Abstract
Background:
Vitiligo is a common, acquired, pigmentary disorder characterized by loss of melanocytes resulting in white spots. This disease carries a lot of social stigma in India.
Objective:
To study the clinico-epidemiological profile of vitiligo patients in Kumaun region of Uttarakhand state in India.
Materials and Methods:
The clinical presentation of vitiligo was examined and analyzed in 762 vitiligo patients attending the Dermatology outdoor of Government Medical College, Haldwani, which is a referral centre for Kumaun region of Uttarakhand state in India.
Results:
Male and female patients were found to be affected almost equally. It was observed that onset of vitiligo was most common in 0-10 years age group, as evidenced by 336 cases out of 762 cases. Acrofacial type of vitiligo (339 cases out of 762) was most commonly observed, followed by vitiligo vulgaris, focal, segmental, mucosal, mixed, and universal vitiligo. The most common site of onset was the lower limbs followed by head and neck, upper limbs, trunk, genitalia, and mucasae. Leucotrichia was observed in 33.5%, Koebner's phenomenon in 26.3%, and a positive family history in 19% of the vitiligo patients. The other common conditions associated were thyroid disorders (8.9%), diabetes (5.3%), and atopic dermatitis (4.9%).
Conclusion:
The study indicates that acrofacial vitiligo is the most common clinical type observed in Kumaun region of Uttarakhand in India. Onset of vitiligo is most common in first decade of life.
Keywords: Clinico-epidemiological profile, Uttarakhand, vitiligo
Introduction
What was known?
Vitiligo vulgaris has been reported as the most common clinical type of vitiligo worldwide, except a single report from Libya where acro-facial vitiligo was found to be the most common clinical type. In most of the studies from India, age of onset of vitiligo is mainly in second and third decade.
Vitiligo is a common, acquired disorder characterized by depigmented cutaneous macules usually devoid of functional melanocytes. These lesions are cosmetically disfiguring and usually cause emotional trauma in both children and adults. Vitiligo affects all races and both sexes almost equally. The population prevalence is estimated to be 0.14-2% in different countries.[1] Vitiligo can develop at any age but the peak incidence is in second or third decade.[2] The precise cause of vitiligo is unknown. Multiple theories have been proposed including theories based on autoimmune, neural, and autocytotoxic phenomenon.[3,4,5,6] The disease has a familial incidence of 1.56-34%.[7,8,9,10,11] Genetic studies suggest a polygenic inheritance pattern.[12] Vitiligo has been reported in association with several endocrinopathies and other disorders of autoimmune nature.[13,14] Our objective in this five year prospective study were to explore the nature of vitiligo in Kumaun region of Uttarakhand state in India and to establish the clinical characteristics of vitiligo and its association with other diseases.
Materials and Methods
The new vitiligo patients who attended the Dermatology outdoor department between January 2006 and December 2010 were included in the study. A complete history including age, sex, duration, site of onset, family history, history of Koebner's phenomenon, and history of associated diseases was elucidated and noted. A complete clinical examination was performed and the sites, area involved, and the pattern of the lesions were noted. The evolution of the disease, as evidenced by the appearance of new lesions and the increase in the size of existing lesions, over the past 3 months was also noted. The vitiligo patients were classified according to recent Bordeaux vitiligo global issues consensus conference classification and consensus nomenclature[15] into three groups, viz. nonsegmental, segmental, and unclassified vitligo. Nonsegmental vitiligo (NSV) was further classified as acrofacial, generalized, universal, mucosal (more than one mucosal sites), and mixed vitiligo. Unclassified vitiligo included focal and mucosal (one site in isolation). Acrofacial vitiligo was defined as multiple, bilateral, symmetrical depigmented macules involving acral region of the extremities and peri-orifacial regions. Vitiligo vulgaris (common vitiligo as per new nomenclature) was defined as scattered macules widely distributed usually symmetrical. Vitiligo was defined as universal if more than 80% body surface area was involved. Mixed vitiligo refers to concomitant occurrence of segmental and NSV. Mucosal vitiligo was defined as involvement of the oral and/or genital mucosae. Segmental vitiligo refers to one or more depigmented macules in a single or multidermatomal configuration. Focal vitiligo was defined as one or more depigmented macules in one area, but not in a dermatomal distribution. The presence of leucotrichia, Koebner's phenomenon was also noted. Screening for autoimmune and endocrine disorders like thyroid diseases, diabetes mellitus, and alopecia areata was also performed by history and clinical examination. Hemogram, peripheral blood smear, blood glucose level, triiodothyronine (T3), thyroxine (T4), thyroid stimulating hormone, and antithyroid antibodies were done in all patients.
Results
A total of 762 vitiligo patients were examined during the study period, accounting for 2.64% of total dermatology outpatients (28842). Three hundred and ninety one patients (51.31%) were male and 371 (48.69%) patients were female, with male:female ratio of 1.05. Duration of the vitiligo at the time of presentation ranged from 1 month to 40 years. The average disease duration at the time of hospital visit was 3.6 years. The most common age group for onset of vitiligo was 0-10 years (31% cases), followed by 11-20 years age group (26.25% cases), as shown in Figure 1. The mean age of onset of vitiligo was 24.4 year in male and 19.7 years in female patients (range 1 month to 72 years). Age of the patients at the time of presentation is also depicted in Figure 1.
Figure 1.
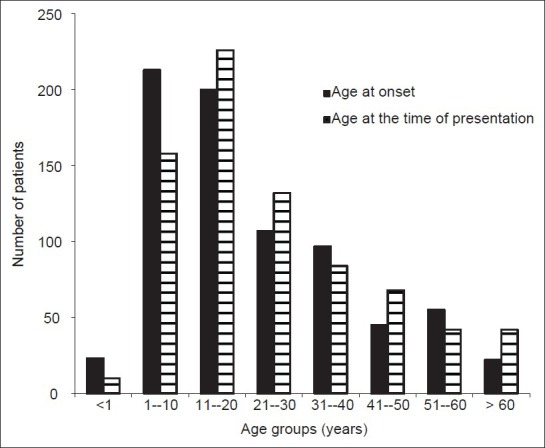
Age at the onset and at the time of presentation of vitiligo
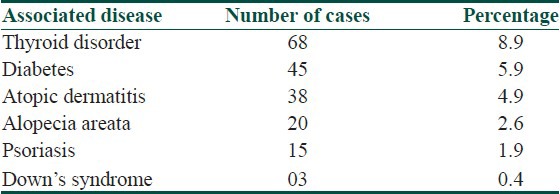
Acrofacial type of vitiligo (339 cases out of 762, 44.5%) was observed to be most common, followed by vitiligo vulgaris, focal, segmental, mucosal, mixed, and universal vitiligo, as shown in Table 1. Four hundred fifty two patients (59.3%) were having active disease as evidenced either by the appearance of new lesions or the increase in the size of the existing lesions, over the past 3 months. It was observed that 465 (61%) patients had a body surface area involvement of less than 2%, 27% had a body surface area involvement of 2-5%, and 12% patients had more than 5% body surface involvement. One hundred and forty five (19%) patients had a positive family history involving one or more than one family members. Leucotrichia was observed in 255 (33.5%) vitiligo patients. Koebner's phenomenon was found in 200 (26.3%) vitiligo patients. Oral mucosal was involved in 58 (7.6%) vitiligo patients and genital mucosa in 26 (3.4%) patients, while both oral and genital mucosae were involved in 48 (6.3%) patients. Site of onset of the vitiligo lesions in the patients is shown in Table 2. The most common site of onset was the lower limbs followed by head and neck upper limbs, trunk, genitalia, and mucosae. Other associated conditions are summarized in Table 3. Thyroid disorders were associated with 68 (8.9%) vitiligo patients. Only 12 out of these 68 vitiligo patients were symptomatic for thyroid disorder. Antithyroid antibodies were found in 27 vitiligo patients. No patient complained of deafness.
Table 1.
Type of vitiligo
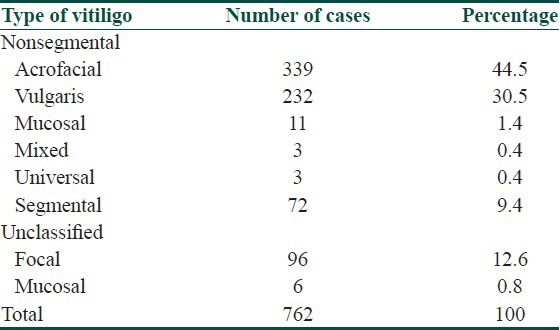
Table 2.
Site of onset of vitiligo
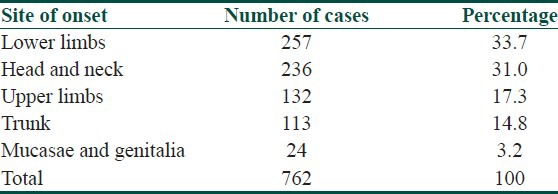
Table 3.
Association of vitiligo with other diseases
Discussion
Vitiligo is characterized by chalky or milky-white colored macules of variable shapes and sizes with or without leucotrichia and lacks any epidermal changes. It is the most common depigmentary disorder having social and psychological aspects. The population prevalence is estimated to be 0.14-2% in different countries based primarily on clinical records of hospitals and dermatology clinics. The results of hospital based data may be biased because of factors like gender, age, educational level, and social factors. Compared with the prevalence of vitiligo in hospital-based studies, data derived from population surveys are more reliable. A recent study from Shaanxi Province, China, showed prevalence of vitiligo only to be 0.093% and stated that the presumed vitiligo prevalence of 1-2% is overestimated.[16] In an extensive survey in India in and around the city of Surat, prevalence of vitiligo was 0.47% in the rural population and 1.78% in the urban population.[17] Men and women were affected equally. Another study from Calcutta, India showed prevalence of 0.5% with equal sex distribution.[18] The variation in the prevalence of vitiligo in India is probably due to the varying ethnic backgrounds of the population in different geographic regions. The incidence of vitiligo in the present study was found to be 2.64%. The incidence of vitiligo reported in other studies is 4% by Dutta and Mandal,[19] 2.9% by Sehgal,[8] and 2.5% by Handa and Kaur.[20]
Vitiligo can develop at any age and is reported from birth to 81 years of age.[21] In most of the studies from India,[9,22] age of onset of vitiligo was mainly in second and third decade; but in our study, 57.2% (436 cases out of 762) of the patients had age of onset of vitiligo in first or second decade, indicating that vitiligo may start at a younger age. However, Howitz et al.[2] reported the age of onset of vitiligo to be between 40 and 60 years. Akrem et al.[23] found that 73.3% vitiligo patients had age of onset beyond 18 years of age. The onset of vitiligo in our patients ranged from 1 month to 72 years of age. The mean age of onset of vitiligo were 24.4 years in male and 19.7 years in female patients comparable to the previous epidemiological data from India,[17] showing mean age of onset among males and females to be 24.8 years and 19.3 years, respectively. The mean age of onset reported from other countries is as low as 10 years (Turkey),[24] 18.8 years (China),[25] 19.3 years (Libya),[10] 28.5 years (Estonia),[26] and as high as 37.7 years (Denmark).[2] A study by Zhang et al.[27] has concluded that onset of vitiligo is possibly affected by genetic backgrounds, common environmental factors and clinical type of vitiligo.
Males and females were affected almost equally in our study, which is similar to various other studies.[1,2,17,18,19,20,25] However, female predominance in some studies[8,24,26] may be presumably explained by more awareness of the women to cosmetic disfigurement and therefore more likely to seek treatment. Age at the time of presentation of vitiligo was corresponding to the age of onset of vitiligo. The duration of the disease varied widely from 1 month to 40 years, with a mean duration of 3.6 years. The long duration of the disease could probably be attributed to its slow progression and asymptomatic nature.
If there are several affected individuals within an extended family, it suggests a genetic component to the cause. The presence of vitiligo in monozygotic twins and the occurrence of HLA-DR4-associated vitiligo in black Americans lend support to this theory.[28,29] In a study from India, the relative risk of vitiligo for first-degree relatives was increased by 4.5 times.[18] Vitiligo is not transmitted in a simple mendelian autosomal dominant or recessive manner. Rather, the transmission seems to be complex and polygenic. Familial occurrence has been reported to vary from as low as to 1.56% reported by Singh et al.[10] (Libya) to as high as to 34% reported from Boisseau-Garsaud et al.[11] (French West Indies). There was family history of vitiligo in 19% of vitiligo cases studied by us which is comparable to various other studies.
Acrofacial vitiligo was the most common clinical type of vitiligo affecting 339 (44.5%) of the patients. This was followed by vitiligo vulgaris, focal, segmental, mucosal, mixed, and universal vitiligo. This pattern of predominance of acrofacial type of vitiligo in our study is contrary to various other studies from India[8,9,19,20,22] and other countries[11,23,24,25,26] in which vitiligo vulgaris has been reported to be the most common type of vitiligo. A single study from Libya by Singh et al.[10] has reported acrofacial vitiligo to be most common type affecting 40.6% vitiligo patients. The studies[30,31] from Benin and Lagos Cities of Nigeria reported localized focal vitiligo to be the most common type of vitiligo affecting 77% and 35% of the vitiligo patients, respectively. The time duration between disease onset and presentation is not mentioned in the study from Benin City.[30] Most patients begin with focal vitiligo and progress to different phenotype of vitiligo as the disease progresses.[25] It is difficult to interpret the mechanism and determinants underlying the clinical patterns of vitiligo. The study by Zhang et al.[27] has indicated that different phenotypes of vitiligo had different pathogenesis and genetic background. As India is a vast country having racial, ethnic, and genetic diversities, predominance of acrofacial vitiligo in clinical patterns of vitiligo can be explained on this basis in this north-western region of the country.
The coexistence of SV and NSV was first reported in a pediatric NSV patient treated with UVB, which left a recalcitrant segmental lesion suggestive of pre-existing SV.[32] Additional cases were subsequently reported, with the term “mixed vitiligo” proposed to designate this form of diseases[33] and a case series subsequently proposed definition criteria.[34] We also observed three patients with mixed vitiligo, two male and one female.
Leucotrichia has been reported in 9-48.4% of the patients with vitiligo.[8,19,20,26,29,35] Significance is attached to this finding as these cases also showed resistance to therapy. It may also be considered as poor prognostic factor. Leucotrichia was seen in 255 (33.5%) of our vitiligo patients. Koebner phenomenon has been reported to occur in up to 33.0% of vitiligo patients.[28] It was seen in 26.3% of our vitiligo patients similar to other studies. However, it was less prevalent in the studies done by Handa et al.[20] and Akay et al.[24] (5% and 7.3%, respectively). Lower limbs were the most common sites for the onset in 257 (33.7%) patients. It is in concordance with many studies[7,19,23] though some studies[8,27] report face as the most common site of onset of vitiligo. Karelson et al.[26] has reported upper limbs as most common site of vitiligo. The exact significance of this observation is difficult to appreciate. Nevertheless, we believe that exposed and trauma-prone sites, such as the lower limbs and hands, may develop vitiligo lesions more easily in genetically predisposed individuals.
Vitiligo has been reported in association with several endocrinopathies and other disorders of autoimmune nature. We observed an association of vitiligo with cutaneous diseases such as atopic dermatitis (4.9%), alopecia areata (2.6%), and psoriasis (1.9%) and with systemic disorders such as diabetes mellitus (5.9%). Three cases of Down syndrome also had vitiligo. Antithyroid antibodies were found in 27 vitiligo patients (not all symptomatic for thyroid dysfunction). Handa and Kaur[20] observed atopic dermatitis in 1.4% of their patients, alopecia areata in 0.4%, bronchial asthma in 0.7%, diabetes mellitus in 0.6%, and thyroid diseases in 0.5%. Kovacs[35] stated that patients with vitiligo have an increased risk of developing autoimmune diseases. He also noted that autoantibodies against different organ systems may be present in vitiligo patients without clinical correlation. None of our patients showed clinically apparent deafness or ocular abnormalities. As the inner ear contains melanocytes and the pigment epithelium of the retina and the choroids are rich in melanocytes, and since vitiligo affects all active melanocytes, auditory and ocular problems may result with vitiligo.[36,37] Sensorineural hypoacusis was found in 37.7% of the vitiligo patients in a recent study by Akay et al.[24]
Conclusion
This clinico-epidemiological study of vitiligo in the Kumaun region of Uttarakhand has shown that acrofacial vitiligo is the most common clinical type observed. The onset of vitiligo is most common in first decade of life and lower limbs are the most common sites of onset. We also observed an association of vitiligo with cutaneous diseases such as atopic dermatitis, alopecia areata, and psoriasis and with systemic disorders such as thyroid disorder and diabetes mellitus.
What is new?
Acrofacial vitiligo is the most common clinical type observed in Kumaun region of Uttarakhand, India, in contrary to other reports where vitiligo vulgaris has been reported to be most common clinical type of vitiligo. We found the age of onset of vitiligo most common in first decade of life in contrary to other reports where second or third decade is reported to be most common age of onset of vitiligo.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Majumder PP. Genetics and prevalence of vitiligo vulgaris. In: Hann SK, Nordlund JJ, editors. Vitiligo. Oxford: Blackwell Science Ltd; 2000. pp. 18–20. [Google Scholar]
- 2.Howits J, Brodthagen H, Schwarts M, Thomsen K. Prevalence of vitiligo. Epidemiological survey the Isle of Bornholm, Denmark. Arch Dermatol. 1977;113:47–52. doi: 10.1001/archderm.113.1.47. [DOI] [PubMed] [Google Scholar]
- 3.Cui J, Arita Y, Btstryn J. Cytolytic antibodies to melanocytes in vitiligo. J Invest Dermatol. 1993;100:812–5. doi: 10.1111/1523-1747.ep12476636. [DOI] [PubMed] [Google Scholar]
- 4.Yu HS, Kao CH, Yu CL. Co-existence and relationship of antikeratinocyte and antimelanocyte antibodies in patients with non segmental type vitiligo. J Invest Dermatol. 1993;100:823–8. doi: 10.1111/1523-1747.ep12476728. [DOI] [PubMed] [Google Scholar]
- 5.Al’ Abadie, Senior MS, Bleehen SS, Gaekrodger DJ. Neuropeptide and neuronal marker studies in vitiligo. Br J Dermatol. 1994;131:160–5. doi: 10.1111/j.1365-2133.1994.tb08486.x. [DOI] [PubMed] [Google Scholar]
- 6.Lerner AB. On the etiology of vitiligo and grey hair. Am J Med. 1971;51:141–7. doi: 10.1016/0002-9343(71)90232-4. [DOI] [PubMed] [Google Scholar]
- 7.Lerner AB. Vitiligo. J Invest Dermatol. 1959;32:285–310. [PubMed] [Google Scholar]
- 8.Sehgal VN. A clinical evaluation of 202 cases of vitiligo. Cutis. 1974;14:439–45. [Google Scholar]
- 9.Koranne RV, Sehgal VN, Sachdev KG. Clinical profile of vitiligo in North India. Indian J Dermatol Venereal Leprol. 1986;52:81–2. [PubMed] [Google Scholar]
- 10.Singh M, Singh G, Kanwar AJ, Belhaj MS. Clinical pattern of vitiligo in Libya. Int J Dermatol. 1985;24:233–5. doi: 10.1111/j.1365-4362.1985.tb05768.x. [DOI] [PubMed] [Google Scholar]
- 11.Garsaud AM, Garsaud P, Cales-Quist D. Epidemiology of vitiligo in the French West Indies (Isle of Martinique) Int J Dermatol. 2000;39:18–20. doi: 10.1046/j.1365-4362.2000.00880.x. [DOI] [PubMed] [Google Scholar]
- 12.Sun X, Xu A, Wei X, Ouyang J, Lu L, Chen M, et al. Genetic epidemiology of vitiligo: A study of 815 probands and their families from south China. Int J Dermatol. 2006;45:1176–81. doi: 10.1111/j.1365-4632.2006.02907.x. [DOI] [PubMed] [Google Scholar]
- 13.Dawber RPR. Clinical association of vitiligo. Postgrad Med J. 1970;46:276. doi: 10.1136/pgmj.46.535.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allison JR, Curtis AC. Vitiligo and pernicious anemia. Arch Dermatol. 1955;72:407. doi: 10.1001/archderm.1955.03730350009002. [DOI] [PubMed] [Google Scholar]
- 15.Ezzedine K, Lim HW, Suzuki T, Katayama I, Hamzavi I, Lan CC, et al. Revised classification/nomenclature of vitiligo and related issues: The vitiligo global issues consensus conference. Pigment Cell Melanoma Res. 2012;25:E1–13. doi: 10.1111/j.1755-148X.2012.00997.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu T, Gao T, Wang A, Jin Y, Li Q, Li C. Vitiligo prevalence study in Shaanxi province, China. Int J Dermatol. 2007;46:47–51. doi: 10.1111/j.1365-4632.2006.02848.x. [DOI] [PubMed] [Google Scholar]
- 17.Mehta NR, Shaha KC, Theodore C, Vyas V, Patel A. Epidemiological study of vitiligo in Surat area, South Gujarat. Indian J Med Res. 1973;61:145–54. [PubMed] [Google Scholar]
- 18.Das SK, Mazumdar PP, Chakraborty R, Majumdar TK, Haldar B. Epidemiological profile in Calcutta. India Genet Epid. 1985;2:71–8. doi: 10.1002/gepi.1370020107. [DOI] [PubMed] [Google Scholar]
- 19.Dutta AK, Mandal SB. A clinical study of 650 cases of vitiligo and their classification. Indian J Dermatol. 1969;14:103–5. [PubMed] [Google Scholar]
- 20.Handa S, Kaur I. Vitiligo: Clinical findings in 1436 patients. J Dermatol. 1999;26:653–7. doi: 10.1111/j.1346-8138.1999.tb02067.x. [DOI] [PubMed] [Google Scholar]
- 21.Ortonne J, Moscher D, Fitzpatrick T. Hypomelanotic disorders in vitiligo and other hypomelanoses of hair and skin. Plenum. 1983;15:129–310. [Google Scholar]
- 22.Sarin RC, Kumar AJ. A clinical study of vitiligo. Indian J Dermatol Venereal Leprol. 1977;43:311–4. [PubMed] [Google Scholar]
- 23.Akrem J, Baroudi A, Aichi T, Houch F, Hamdaoui MH. Profile of vitiligo in the south of Tunisia. Int J Dermatol. 2008;47:670–4. doi: 10.1111/j.1365-4632.2008.03695.x. [DOI] [PubMed] [Google Scholar]
- 24.Akay BN, Bozkir M, Anadolu T, Gullu S. Epidemiology of vitiligo, associated autoimmune diseases and audiological abnormalities: Ankara study of 80 patients in Turkey. J Eur Acad Dermatol Venereol. 2010;24:1144–50. doi: 10.1111/j.1468-3083.2010.03605.x. [DOI] [PubMed] [Google Scholar]
- 25.Liu JB, Li M, Yang S, Gui JP, Wang HY, Du WH, et al. Clinical profile of vitiligo in China: An analysis of 3742 patients. Clin Exp Dermatol. 2005;30:327–31. doi: 10.1111/j.1365-2230.2005.01813.x. [DOI] [PubMed] [Google Scholar]
- 26.Karelson M, Kimgo K, Salum T, Kõks S, Silm H. An Adult's Vitiligo in Estonia: Study of 155 patients. Open Dermatol J. 2009;3:68–72. [Google Scholar]
- 27.Zhang XJ, Liu JB, Gui JP, Li M, Xiong QG, Wu HB, et al. Characteristics of genetic epidemiology and genetic models for vitiligo. J Am Acad Dermatol. 2004;51:383–90. doi: 10.1016/j.jaad.2003.12.044. [DOI] [PubMed] [Google Scholar]
- 28.Hann SK, Chun WH, Park PK. Clinical characteristics of progressive vitiligo. Int J Dermatol. 1997;36:353–55. doi: 10.1046/j.1365-4362.1997.00162.x. [DOI] [PubMed] [Google Scholar]
- 29.Cho S, Kang HC, Hahm J. Characteristics of vitiligo in Korean children. Pediatr Dermatol. 2000;17:189–93. doi: 10.1046/j.1525-1470.2000.01749.x. [DOI] [PubMed] [Google Scholar]
- 30.Onunu AN, Kubeyinje EP. Vitiligo in the Nigerian African: A study of 351 patients in Benin City, Nigeria. Int J Dermatol. 2003;42:800–2. doi: 10.1046/j.1365-4362.2003.01908.x. [DOI] [PubMed] [Google Scholar]
- 31.Ayanlowo O, Olumide YM, Akinkugbe A, Ahamneze N, Otike-Odibi BI, Ekpudu VI, et al. Characteristics of Vitiligo in Lagos, Nigeria. West Afr J Med. 2009;28:118–21. [PubMed] [Google Scholar]
- 32.Gauthier Y, Cario Andre M, Taieb A. A critical appraisal of vitiligo etiologic theories. Is melanocyte loass a melanocytorrhagy? Pigment Cell Res. 2003;16:322–32. doi: 10.1034/j.1600-0749.2003.00070.x. [DOI] [PubMed] [Google Scholar]
- 33.Mulekar SV, Al Issa A, Asaad M, Ghwish B, Al Eisa A. Mixed vitiligo. J Ctan Med Surg. 2006;10:104–7. doi: 10.2310/7750.2006.00018. [DOI] [PubMed] [Google Scholar]
- 34.Ezzedine K, Gauthier Y, Leaute-Labreze C, Marquez S, Bouchtnei S, Jouary T, et al. Segmental vitiligo associated with generalized vitiligo (mixed vitiligo): A retrospective case series of 19 patients. J Am Acad Dermatol. 2011;65:965–71. doi: 10.1016/j.jaad.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 35.Kovacs OS. Vitiligo. J Am Acad Dermatol. 1998;38:647–66. doi: 10.1016/s0190-9622(98)70194-x. [DOI] [PubMed] [Google Scholar]
- 36.Wolff D. Melanin in the ear. Arch Otolaryngol. 1931;14:195–211. [Google Scholar]
- 37.Albert DM, Wagoner MD, Pruett RC, Norlund JJ, Lerner AB. Vitiligo and disorder of retinal pigment epithelium. Br J Opthalmol. 1983;67:153–6. doi: 10.1136/bjo.67.3.153. [DOI] [PMC free article] [PubMed] [Google Scholar]


