Abstract
Hepatitis being first manifestation of secondary syphilis is rare. Here in we report a case of 39 years old male who was being treated for hepatitis and presented to us subsequently with itchy maculopapular rash. Venereal disease research laboratory (VDRL) titre was 1:16. Treponema pallidum hemagglutination assay (TPHA) was positive. He was treated with intramuscular Benzathine Penicillin. His hepatitis improved rapidly.
Keywords: Secondary syphilis, syphilitic hepatitis, treatment of syphilitic hepatitis
Introduction
What was known?
Only 10% of patients with syphilitic hepatitis have abnormal liver enzyme concentrations, but clinical hepatitis is rare.
Symptomatic secondary syphilis classically presents with mucocutaneous lesions and lymphadenopathy. The incidence of skin involvement is 90%.[1] Although 10% of patients have abnormal liver enzyme concentrations, clinical hepatitis is rare.[2,3,4,5]
Case Report
Thirty nine years old male patient presented to medicine out patient department (OPD) with complaints of low grade fever, anorexia, malaise and pain in upper abdomen of one month duration along with dark coloured urine of 10 days duration. Patient gave history of consuming 40-50 grams of alcohol daily for past 3 years. There was no history of drug abuse or blood transfusion.
Examination disclosed presence of icterus with normal vital signs. Per abdomen examination revealed 2 cm, firm, non tender hepatomegaly without splenomegaly or ascites.
Biochemical analysis revealed increased values of serum bilirubin 3.5 mg/dl (normal 0.0-1.5 mg/dl), serum alanine transaminase (ALT) 357 IU/ml (normal < 50), serum aspartate transaminase (AST) 175 IU/ml (normal < 45) and serum alkaline phosphatase 536 IU/ml (normal 20-135). Screening for Hepatitis A, B, C and E were negative. Ultrasound abdomen revealed hepatomegaly with liver span of 16.4 cm with normal echotexture. Magnetic resonance cholangio pancreatography (MRCP) confirmed hepatomegaly with no space occupying lesion, lymphadenopathy or extra hepatic cholestasis.
The patient was thought to have acute hepatitis probably due to alcohol or non-hepatotropic viruses. Since the patient was showing clinical recovery with regression in serum bilirubin (1 mg/dl), AST (90 IU/ml) and ALT (152 IU/ml) though with rising alkaline phosphatase (711 IU/ml), Patient was asked to review after 1 month with the plan of performing liver biopsy after the resolution of acute phase.
On reporting back he presented to dermatology OPD with intensely itchy rash. Examination revealed multiple erythematous papules and plaques on neck, trunk, palms and soles [Figures 1–4]. Buschke Olendroff sign was positive. There was bilateral, non tender, shotty inguinal lymphadenopathy, congestion of soft palate and posterior pharyngeal wall. Genital, per rectal, ophthalmic and auditory examination was normal.
Figure 1.

Erythematous scaly macules and papules over both palms
Figure 4.
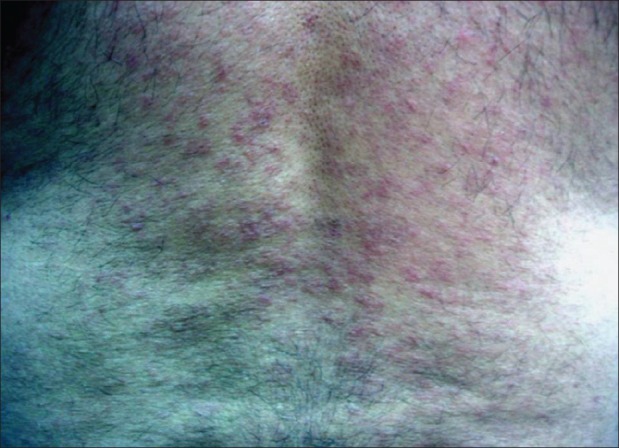
Erythematous macules and papules over back
Figure 2.

Congestion of soft palate
Figure 3.

Erythematous macules and papules over neck
Patient gave history of repeated unprotected heterosexual intercourse with multiple partners during past two years. There were no symptoms suggestive of any sexually transmitted disease.
A provisional diagnosis of secondary syphilis with syphilitic hepatitis was made. VDRL titre was 1:16 and TPHA was positive. Liver biopsy was suggestive of syphilitic hepatitis showing maintained hepatic architecture with Kupffer cell hyperplasia, lymphocytic and neutrophillic infiltration of portal tracts with mild neutrophillic infiltrate in hepatic lobules and no necrosis, granuloma, gumma or Treponema pallidum. Reticulin stain revealed early fibrosis around the portal tracts [Figure 5]. ELISA for HIV was negative. Positron emission tomography (PET) scan revealed hepatomegaly and presence of retroperitoneal, hilar, mediastinal, bilateral axillary, inguinal and external iliac lymph nodes. Patient was treated with 3 doses of intramuscular Benzathine Penicillin 2.4 million units, given weekly. He became asymptomatic with resolution of pruritus and mucocutaneous findings. There was normalization of serum bilirubin, ALT, AST values and reduction in alkaline phosphatase (383 IU/ml).
Figure 5.
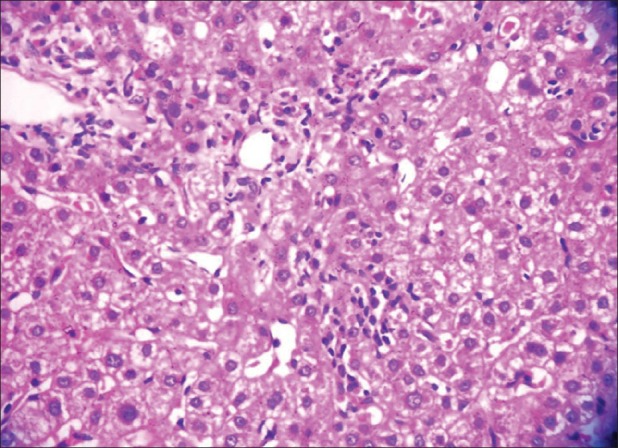
Kupffer cell hyperplasia, lymphocytic and neutrophillic infiltration of portal tracts with mild neutrophillic infiltrate in hepatic lobules
Discussion
Syphilis is typically considered in the differential diagnosis of genital ulcers, generalized lymphadenopathy and a variety of mucocutaneous manifestations, especially in high-risk subjects. Most reviews note skin involvement in approximately 90% of cases[1] and abnormal liver enzyme concentrations in approximately 10%. Rarely, clinical hepatitis usually with cutaneous manifestation has also been described.[2,3,4] Many cases of syphilitic hepatitis have also been reported in HIV infected patients.[5] In Syphilitic hepatitis there is usually disproportionate elevation of the alkaline phosphatase levels.[4,6,7] Elevation in alkaline phosphatase is likely due to pericholangiolar inflammation.[5] Cases may also present with elevated AST and ALT levels.[2,4] Treatment for syphilis results in rapid resolution of biochemical abnormalities.[5,6,7,8]
Our patient presented with signs and symptoms of hepatitis with abnormal liver function tests and prominent elevation in alkaline phosphatase levels. An initial diagnosis of alcohol or a non-hepatotropic virus causing hepatitis was made. The diagnosis of alcoholic hepatitis was erroneously made since patient was known alcoholic and viral markers for hepatitis were negative. However, the diagnosis of secondary syphilis with syphilitic hepatitis was confirmed when later he presented with typical mucocutaneous manifestations of secondary syphilis, high titres of VDRL, positive TPHA, no evidence of fatty changes in liver in ultrasound abdomen, PET scan showing hepatomegaly with multiple lymphadenopathy and liver biopsy suggestive of syphilitic hepatitis. Implication of syphilis as a cause of hepatitis was based on the characteristic liver enzyme pattern, with more prominent elevation in the alkaline phosphatase level, negative serology for hepatotropic viruses and the rapid resolution of symptoms and biochemical abnormalities with therapy.
The purpose of reporting this case is to present an uncommon manifestation of secondary syphilis in the form of hepatitis, its good response to conventional treatment with Benzathine Penicillin and to keep it as a differential diagnosis in young sexually active patients.
What is new?
The diagnosis of hepatitis of undetermined aetiology several weeks preceding the recognition of syphilis, as in our patient, is unusual. Itching can be present in secondary syphilis, however, intense itching described by our patient as “nightmare” is unknown.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Tramont EC. Treponema pallidum (syphilis) In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas and Bennett's Principles and Practice of Infectious Diseases. 5th ed. Philadelphia: Livingstone; 2000. pp. 2474–90. [Google Scholar]
- 2.Tiliakos N, Shamma’a JM, Nasrallah SM. Syphilitic hepatitis. Am J Gastroenterol. 1980;73:60–1. [PubMed] [Google Scholar]
- 3.Agrwal NM, Sassaris M, Brooks B, Akdamar K, Hunter F. The liver in secondary syphilis. South Med J. 1982;75:1136–8. doi: 10.1097/00007611-198209000-00031. [DOI] [PubMed] [Google Scholar]
- 4.Schlossberg D. Syphilitic hepatitis: A case report and review of the literature. Am J Gastroenterol. 1987;82:552–3. [PubMed] [Google Scholar]
- 5.Mullick CJ, Liappis AP, Benator DA, Roberts AD, Parenti DM, Simon GL. Syphilitic hepatitis in HIV-Infected patients: A report of 7 cases and review of the literature. Clin Infect Dis. 2004;39:e100–5. doi: 10.1086/425501. [DOI] [PubMed] [Google Scholar]
- 6.Noto P, Del Nonno F, Licci S, Chinello P, Petrosillo N. Early syphilitic hepatitis in an immunocompetant patient: Really so uncommon? Int J STD AIDS. 2008;19:65–6. doi: 10.1258/ijsa.2007.007037. [DOI] [PubMed] [Google Scholar]
- 7.Campisi D, Whitcomb C. Liver disease in early syphilis. Arch Intern Med. 1979;139:365–6. [PubMed] [Google Scholar]
- 8.Feher J, Somogyi T, Timmer M, Jozsa L. Early syphilitic hepatitis. Lancet. 1975;2:896–9. doi: 10.1016/s0140-6736(75)92129-7. [DOI] [PubMed] [Google Scholar]


