Abstract
Background
Functional exercises are important in the rehabilitation of anterior cruciate ligament deficient and reconstructed individuals but movement compensations and incomplete recovery persist. This study aimed to identify how tasks pose different challenges; and evaluate if different activities challenge patient groups differently compared to controls.
Methods
Motion and force data were collected during distance hop, squatting and gait for 20 anterior cruciate ligament deficient, 21 reconstructed and 21 controls.
Findings
Knee range of motion was greatest during squatting, intermediate during hopping and smallest during gait (P < 0.01). Peak internal knee extensor moments were greatest during distance hop (P < 0.01). The mean value of peak knee moments was reduced in squatting and gait (P < 0.01) compared to hop. Peak internal extensor moments were significantly larger during squatting than gait and peak external adductor moments during gait compared to squatting (P < 0.01). Fluency was highest during squatting (P < 0.01). All patients demonstrated good recovery of gait but anterior cruciate ligament deficient adopted a strategy of increased fluency (P < 0.01). During squatting knee range of motion and peak internal knee extensor moment were reduced in all patients (P < 0.01). Both anterior cruciate ligament groups hopped a shorter distance (P < 0.01) and had reduced knee range of motion (P < 0.025). Anterior cruciate ligament reconstructed had reduced fluency (P < 0.01).
Interpretation
Distance hop was most challenging; squatting and gait were of similar difficulty but challenged patients in different ways. Despite squatting being an early, less challenging exercise, numerous compensation strategies were identified, indicating that this may be more challenging than gait.
Keywords: Clinical biomechanics, Movement analysis, Anterior cruciate ligament, Rehabilitation, Knee joint, Functional exercise, Physiotherapy
1. Introduction
Rehabilitation is recommended for individuals with anterior cruciate ligament (ACL) injury that have a surgical reconstruction (ACLR) and for those that manage their injury conservatively and remain ACL deficient (ACLD). Despite rehabilitation quite a large proportion of ACLR and ACLD individuals demonstrate incomplete recovery; this can result in altered movement strategies and/or inability to return to pre-injury activity (Ardern et al., 2011; Button et al., 2005, 2006; Deneweth et al., 2010; Gobbi and Francisco, 2006; Gustavsson et al., 2006; Myklebust et al., 2003; Orishimo et al., 2010; Salem et al., 2003; Strehl and Eggli, 2007; Zabala et al., 2013). A number of rehabilitation protocols have been published and/or assessed within randomised control trials. These have focused on; perturbation, strengthening and neuromuscular control exercises or generalised programmes that combine the different exercise types within the rehabilitation programmes (Beynnon et al., 2005; Chmielewski et al., 2005; Eitzen et al., 2010; Hartigan et al., 2009; Risberg et al., 2007; White et al., 2013; Wilk et al., 2012). Functional exercises are favoured in rehabilitation to address knee and lower limb strength and motor control because they are closely related to everyday activities and sport. This includes important exercises such as walking (GAIT), double leg squat (DLS) and single leg distance hop (SLDH). Greater insight into the biomechanical differences between GAIT, DLS and SLDH is required so that exercise prescription within rehabilitation can be more targeted. In addition an understanding of biomechanical compensation strategies in ACLR, ACLD compared to healthy controls is required so that rehabilitation can be more specific.
This study addressed the following two aims. Firstly to identify how GAIT, DLS and SLDH exercises pose different knee motion, moment and control challenges to the knee. Secondly to evaluate if these activities challenge ACL deficient (ACLD) and ACL reconstructed (ACLR) individuals differently compared to controls (CONT). There is a wide range of functional exercises but GAIT, DLS and SLDH are being evaluated in the current study because they are presumed to span the early (GAIT), intermediate (DLS) and advanced (SLDH) phases of rehabilitation. This means that they pose different challenges to the knee; single versus double leg stance, range of motion and internal/external moments (Escamilla et al., 2012; Risberg et al., 2007; White et al., 2013; Wilk et al., 2012). Based on the literature we hypothesised that SLDH would be the most challenging task, followed by DLS and then GAIT. The second hypothesis was that ACLD would demonstrate the most compensation strategies that would reflect the challenges posed by each functional exercise.
2. Methods
20 ACLD, 21 ACLR and 21 healthy control (CONT) subjects provided informed consent to participate in this study (demographics are in Table 1). All ACLR had a single bundle gracilis–semitendinosus tendon graft reconstruction, with an ‘anatomical’ tunnel position. Ethical approval for this study was obtained from the South East Wales Research Ethics Committee. Inclusion criteria were that patients were aged between 18 and 50 years, had an ACL rupture that may or may not be accompanied with a meniscal tear or collateral ligament sprain, or a primary ACL reconstruction; had finished their rehabilitation; had no other pathology which affects their movement; had no previous knee surgery and were able to provide informed consent independently. All ACL individuals had an MRI scan and were reviewed by an expert clinician to ensure the inclusion criteria were met.
Table 1.
Mean and standard deviation for demographic variables and time since injury/surgery, muscle strength and patient rated questionnaires for ACLR, ACLD and CONT. *Signifies P < 0.05. SKnExt represents peak torque for the quadriceps muscle, and SKnFlex represents peak torque for the hamstrings. The patient rated questionnaires are the Tampa Scale of Kinaesiophobia (FOI), International Knee Documentation Committee (IKDC) and Cincinnati Sports and Activity Scale (CSAS).
| CONT | ACLR | ACLD | |
|---|---|---|---|
| Age (years) | 26.8 (7.7) | 29.1 (9) | 29.2 (6) |
| Height (m) | 1.75 (0.13) | 1.73 (0.07) | 1.80 (0.08)* |
| Mass (kg) | 77.6 (19.6) | 80.1 (9.5) | 82.9 (12.5) |
| Gender | F: 9 M: 12 | F: 5 M: 16 | F: 3 M: 17 |
| Time since injury (months) | 24.1 (16.9) | 19.6 (55.5) | |
| Time since surgery (months) | 13.5 (9) | ||
| SKnExt (Nm) | 147 (71) | 134 (64) | 115 (42) |
| SKnFlex (Nm) | 86 (40) | 80 (31) | 75 (22) |
| FOI | 32.4 (4.9) | 40.7 (5.1)* | |
| IKDC | 83.3 (10) | 61.5 (12.6)* | |
| CSAS median | 95 | 80 | 75 |
Knee function was scored for ACLD and ACLR using the International Knee Documentation Subjective Knee (IKDC) questionnaire (Irrgang et al., 2001). Fear of re-injury was measured using the modified Tampa Scale of Kinaesiophobia (Kvist et al., 2005). Sports activity level was measured using the Cincinnati Sports and Activity Scale (CSAS) (Barber-Westin et al., 1999). Knee extensor (SKneeExt) and flexor (SKneeFlex) isokinetic strengths (concentric/concentric) were measured at 90°/s on a Biodex System 4 PRO dynamometer (Biodex Medical Systems Inc., USA). This was measured on both legs, but presented for the injured (ACLR and ACLD) and the dominant stance leg (CONT) only.
Standardised instructions were given on how to carry out the activities. For GAIT participants were asked to walk along a 15 metre walkway at their ‘normal’ walking speed. For DLS participants were instructed to squat to their maximum depth and then return to their starting position. For SLDH individuals were asked to hop their maximum single leg hop distance and regain their balance after landing. Participants were asked to perform eight DLS and SLDH trials and five GAIT trials, four successful trials for each activity were analysed. Individuals were given time to rest between SLDH trials. All ACL injured subjects hopped using their injured leg and the controls using their dominant stance leg.
Anthropometric measurements were taken and used for the inverse dynamic calculations. Ground reaction force data were collected using a Kistler force plate (Kistler Instruments Ltd., Winterthur, Switzerland) at 1000 Hz. Kinematic data were collected at 250 Hz using an eight camera VICON MX motion analysis system (Oxford Metrics Group Ltd., Oxford., UK). Reflective markers were placed using the ‘Plug-in-Gait’ full body marker set. Two additional markers were placed on the left and right lateral sides of the iliac crest (LILC and RILC). A static anatomical calibration trial was collected on each participant. The knee axes were aligned using the anatomical calibration trial. In some trials the trunk and hips flexed as such that the markers on the left and right anterior superior iliac crests (LASI and RASI) were occluded; these gaps were filled using the data of the LILC and RILC markers in a custom written programme in ViconBodyBuilder for Biomechanics (version 1.2, Oxford Metrics Group Ltd., Oxford, UK). Inverse dynamics calculations were performed within VICON Nexus software (version 1.6.1 (Oxford Metrics Group Ltd., Oxford., UK)) and data were further processed and analysed in Matlab R2010b (The Mathworks Inc., Natick,USA). This analysis focused on the stance phase of GAIT, the descent and ascent phases of DLS and the landing phase of SLDH.
Performance variables were quantified for each of the activities; gait velocity for GAIT, squat depth for DLS and hop distance (dhop) for SLDH. dhop was calculated as the distance the ankle joint centre travelled along the axis of hopping and normalized to body height. Kinematic and kinetic variables used to evaluate exercise difficulty were knee flexion–extension range of motion (RoMknee), hip flexion–extension range of motion (RoMhip), ankle flexion–extension range of motion (RoMankle), peak internal knee extensor moment (MkneeMax), peak external knee adductor moment (MaddMax), peak internal hip moment (MhipMax), and peak internal ankle moment (MankleMax). In the coronal plane peak external knee adductor moments have been used because this corresponds to terminology most commonly used in the literature. The output variable calculated to assess knee control was fluency. This was calculated by a method adapted from Smeulders et al. (2001). It was defined as the number of times the velocity of the knee position in the coronal plane crossed zero, averaged per second. The inverse of this measure (Period (s): T = 1/f) was used so that a larger value agreed with a more fluent movement.
The data were checked for normality using the Kolmogorov–Smirnov test. The data were transformed when large differences in standard deviations existed using square root or logarithmic adjustment. To address aim 1, a one-way ANOVA with Bonferroni post hoc testing was used to investigate differences between GAIT, DLS and SLDH for the variable representing knee moments and motor control. To address aim 2 a univariate analysis was used to evaluate differences between ACLR and CONT and between ACLD and CONT for the performance, motion, moment and knee control variables. Gait velocity, squat depth and hop distance were used as covariates for each of the activities. An overall alpha level of P < 0.05 was used to signify significance. With Bonferroni adjustment for two comparisons P < 0.025 indicated significance. Not all of the ACLD individuals could do a SLDH. Descriptive data (means and standard deviations) for the demographics and key biomechanical parameters are presented for 12 ACLD that could hop (ACLDhop) and for 8 ACLD that could not hop (ACLDno-hop). These sub-groups were compared by means of descriptive statistics.
3. Results
The ACL groups were matched to CONT for height, mass, age and gender; however matching was not optimal (Table 1). Therefore, hop distance was normalized to height and all peak moments were normalized to height and weight. The ACLR were mean 25.5 (SD 16.9) months and the ACLD were mean 19.6 (SD 55.15) months post-injury. The ACLR subjects were on average 13.5 ± 9 months post-surgery (Table 1). The level of sports participation (CSAS values) was highest for CONT, intermediate for ACLR and lowest in ACLD. There was no significant difference between the ACL groups and CONT for SKnExt (ACLR P = 1.000; ACLD P = 0.318) or SKnFlex (ACLR P = 1.000; ACLD P = 0.958). A higher fear of re-injury (TSK) and lower IKDC score existed for ACLD compared to ACLR (P < 0.05). These findings are summarized in Table 1.
3.1. Comparison of functional exercises
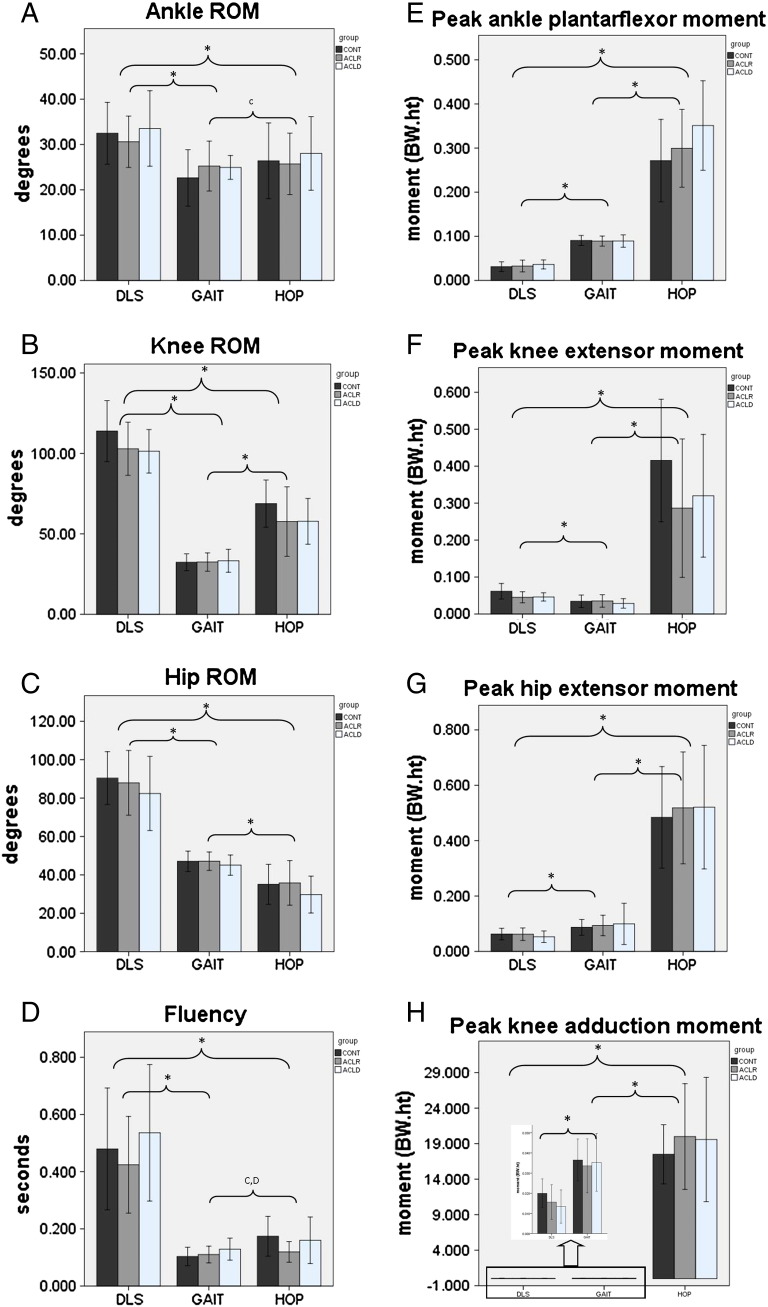
The first aim of this study was to assess differences in joint motion, peak moments, knee fluency and performance between GAIT, DLS and SLDH. The mean values, standard deviations and statistical differences between these exercises are displayed in Fig. 1. The ankle, knee and hip range of motion was greatest during DLS regardless of subject group (P < 0.01). RoMknee was intermediate during SLDH (P < 0.01) and lowest during GAIT (P < 0.01). RoMhip was intermediate during GAIT (P < 0.01) and lowest during SLDH (P < 0.01). There was no statistical difference in RoMankle between GAIT and SLDH (P > 0.05) for ACLR (P = 1.000) or ACLD (P = 0.062) but RoMankle was greater during SLDH than GAIT for CONT (P < 0.01).
Fig. 1.
A–H. Graphs of means and standard deviations for all the biomechanical parameters for each of the functional exercises used in the between activity analysis for GAIT, DLS and HOP. Note that internal moments were used in all cases except for the peak external knee adductor moments because this corresponds to terminology most commonly used in the literature.
*Indicates a statistical significance of P < 0.01 for all ACL groups. CIndicates a statistical significance of P < 0.01 for CONT only. C,DIndicates a statistical significance of P < 0.01 for CONT and ACLD only. In panel H the mean moment for DLS and GAIT has been inserted on an expanded scale.
Peak internal ankle plantar flexor, knee extensor and hip extensor and external knee adductor moments were greatest during SLDH (P < 0.01) regardless of subject group; the difference from the other two activities was substantial, for example MKneeMax during SLDH was larger than during the other exercises by a factor of 8 (Fig. 1). MKneeMax was significantly larger during DLS than GAIT (P < 0.01). MAddMax, MhipMax, and MankleMax were significantly larger during GAIT than DLS (P < 0.01).
Fluency was highest during DLS (P < 0.01) compared to SLDH and GAIT for all groups. Fluency was significantly larger during SLDH than GAIT for CONT and ACLD (P < 0.01) but for ACLR there was no significant difference in fluency between SLDH and GAIT (P = 0.966).
3.2. Biomechanical compensation strategies in ACLR and ACLD
The second aim was to evaluate different biomechanical compensation strategies in ACLR and ACLD compared to CONT for knee motion, moment and control for each of the functional activities. These results are summarized in Table 2.
Table 2.
Mean and standard deviation for all biomechanical parameters for each subject group within an activity. Statistical differences between ACLR and ACLD compared to CONT are presented for each activity. *Indicates a statistically significant difference between subject groups within a functional exercise when P < 0.025, and **indicates a highly statistically significant difference when P < 0.01. Range of motion at the ankle, knee and hip is represented as RoMankle, RoMknee and RoMhip. Note that internal moments were used for; peak knee extensor (MkneeMax), peak hip extensor (MhipMax) and peak ankle plantar flexor moments (MankleMax). External moments were used for peak knee adductor moments (MaddMax) because this corresponds to terminology most commonly used in the literature.
| CONT |
ACLR |
ACLD |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| GAIT | DLS | SLDH | GAIT | DLS | SLDH | GAIT | DLS | SLDH | |
| RoMankle degrees | 22.6 (6.2) | 32.5 (6.8) | 26.4 (8.4) | 25.2 (5.5)** | 30.6 (5.7) | 25.7 (6.8) | 25 (2.7)* | 33.5 (8.3)** | 28.0 (8.1)* |
| RoMknee degrees | 32.4 (5.2) | 113.9 (19.0) | 68.8 (14.7) | 32.5 (5.7) | 102.9 (16.5)** | 57.6 (21.6)* | 33.2 (7.2) | 101.3 (13.5)** | 57.7 (14.2)** |
| RoMhip degrees | 47.1 (5.3) | 90.4 (13.8) | 35.1 (10.4) | 47.1 (4.8) | 87.9 (17) | 35.8 (11.6) | 45 (5.3) | 82.4 (19.3)* | 29.7 (9.6) |
| Fluency seconds | 0.104 (0.030) | 0.490 (0.210) | 0.172 (0.070) | 0.108 (0.028) | 0.430 (0.170) | 0.120 (0.037)** | 0.123 (0.032)** | 0.530 (0.243) | 0.148 (0.072) |
| MankleMax BW ∙ ht | 0.091 (0.011) | 0.031 (0.011) | 0.272 (0.094) | 0.089 (0.011) | 0.033 (0.013) | 0.300 (0.088) | 0.089 (0.014) | 0.036 (0.010)** | 0.355 (0.101)** |
| MkneeMax BW ∙ ht | 0.034 (0.017) | 0.061 (0.021) | 0.416 (0.166) | 0.035 (0.017) | 0.045 (0.015)** | 0.286 (0.187)* | 0.029 (0.013) | 0.046 (0.011)** | 0.320 (0.166) |
| MhipMax BW ∙ ht | 0.087 (0.029) | 0.062 (0.021) | 0.484 (0.183) | 0.094 (0.037) | 0.062 (0.023) | 0.518 (0.202)** | 0.100 (0.076) | 0.053 (0.020)** | 0.521 (0.223)** |
| MaddMax BW ∙ ht | 0.037 (0.010) | 0.020 (0.007) | 0.291 (0.119) | 0.034 (0.013) | 0.016 (0.009)** | 0.303 (0.115) | 0.036 (0.014) | 0.013 (0.008)** | 0.272 (0.068) |
3.2.1. Gait
GAIT performance was evaluated using gait velocity and there was no significant difference between the subject groups (CONT mean 1.473 (SD 0.156); ACLR mean 1.447 (SD 0.169); ACLD mean 1.44 (SD 0.165) P = 0.594). For joint range of motion the ACL groups both used an increased RoMankle, in the region of 2° compared to CONT (ACLR P < 0.01; ACLD P < 0.025). There was no significant difference in RoMknee (P = 0.761) and RoMhip (ACLR P = 0.192; ACLR P = 0.092) compared to CONT. For moments there was no significant difference in MankleMax (P = 0.783), MKneeMax (P = 0.221), MaddMax (P = 0.182) or MhipMax (P = 0.601) in ACL groups compared to CONT. For knee control the ACLD had a higher fluency score than CONT (P < 0.01). There was no significant difference in fluency between ACLR and CONT (P = 0.534).
3.2.2. Double leg squat (DLS)
DLS performance was significantly reduced in both ACLR and ACLD as both groups had reduced knee RoMknee compared to CONT (ACLR P < 0.01; ACLD P < 0.01; Table 2). ACLD had significantly reduced RoMhip (P < 0.025) and increased RoMankle (P < 0.01) compared to CONT. For ACLR there was no significant difference in RoMhip (P = 0.053) or RoMankle (P = 0.577) compared to CONT. For joint moments ACLR and ACLD had reduced MKneeMax (ACLR P < 0.01; ACLD P < 0.01) and MaddMax (ACLR P < 0.01; ACLD P < 0.01) compared to CONT. ACLD used reduced MhipMax (P < 0.01) and increased MankleMax (P < 0.01) compared to CONT. There was no significant difference in MankleMax (P = 0.997) or MhipMax (P = 0.265) for ACLR compared to CONT. There was no significant difference in fluency scores for ACLR (P = 0.130) and ACLD (P = 0.041) compared to CONT.
3.2.3. Single leg distance hop (SLDH)
For SLDH all of the CONT and ACLR subjects were able to hop but only 12 of the ACLD were able. Dhop was used as the performance measure and this was significantly shorter in ACLR compared to CONT. The subgroup of ACLD subjects hopped the shortest distance (CONT mean 73.45 (SD 13.49); ACLR mean 64.03 (SD 24.21) P < 0.01; ACLD mean 52.67 (SD 15.2) P < 0.01). ACLD demonstrated a significantly greater RoMankle (P < 0.025). There was no significant difference in RoMankle for ACLR compared to CONT (P = 0.649). Both ACLR and ACLD had reduced RoMknee compared to CONT (ACLR P < 0.025; ACLD P < 0.01). There was no significant difference in RoMhip between the groups (overall test result P = 0.655). ACLR did not demonstrate any significant difference in MankleMax (P = 0.042) but ACLD had increased MankleMax (P < 0.01) compared to CONT. Both ACLR and ACLD had increased MhipMax (ACLR P < 0.01; ACLD P < 0.01) compared to CONT. There was no statistical difference in MKneeMax (P = 0.297) or MaddMax (P = 0.120) between the ACL groups and CONT. Knee control as represented by fluency scores was significantly reduced in ACLR compared to CONT (P < 0.01) but not for ACLD compared to CONT (P = 0.946).
Not all the ACLD individuals were able to hop so the means and standard deviations for key demographic and biomechanical parameters of the ACLD subjects that could hop (ACLDhop) and those that could not (ACLDno-hop) are presented in Table 3. Although not tested for significance these descriptive results suggest that the ACLDno-hop tended to have a larger mean body mass, higher fear of re-injury and lower IKDC. The ACLDno-hop demonstrated reduced mean values for squat depth and gait velocity.
Table 3.
Mean and standard deviation for key parameters for ACLD that were able to hop (ACLDhop) and those that were unable to hop (ACLDno-hop). Range of knee motion during double leg squat is represented as DLS RoMknee. The questionnaires used are the Tampa Scale of Kinaesiophobia (FOI) and the International Knee Documentation Committee (IKDC).
| Variable | ACLDno-hop | ACLDhop |
|---|---|---|
| Number of subjects | 8 | 12 |
| Height (m) | 1.83 (0.641) | 1.78 (0.73) |
| Age (years) | 31 (7.4) | 28.1 (4.6) |
| Mass (kg) | 90.5 (10.3) | 77.9 (10.7) |
| Gender | M = 8 | F = 4 M = 8 |
| DLS RoMknee (degrees) | 95.79 (12.62) | 104.91 (12.90) |
| Gait velocity (m/s) | 1.39 (0.17) | 1.47 (0.16) |
| FOI | 44.6 (2.4) | 38.5 (5.0) |
| IKDC | 52.3 (7.7) | 66.6 (12.1) |
4. Discussion
4.1. Activity comparison
The first aim of this study was to identify how GAIT, DLS and SLDH exercises pose different motion, moment and control challenges to the lower limb. The results demonstrate that each of these activities challenges the lower limb differently and each of the key biomechanical variables will be discussed.
Joint range of motion for the ankle, knee and hip were largest during DLS, intermediate during SLDH and least during GAIT, with the exception of RoMhip, which was greater in gait than SLDH. The large range of motion during DLS is often considered to make this activity challenging for knee rehabilitation. This larger RoMknee during DLS did result in greater MKneeMax during DLS than GAIT. This happened despite DLS taking place in double limb support and the moments being distributed between two legs. Conversely MankleMax and MhipMax were significantly larger during GAIT than DLS. So the larger ankle, knee and hip RoMs during DLS were influential on the knee but not on the ankle and hip moments. This could be explained by differences in moment arms. The larger MankleMax and MhipMax in GAIT were expected because it is a single leg stance activity and includes push off. The larger MaddMax during GAIT than DLS was expected because of the single leg stance and medio-lateral sway. Overall, peak moments were substantially larger during SLDH and this is therefore the most challenging activity in terms of joint loading.
Finally, to evaluate how each activity challenges knee control, fluency scores were considered as an indicator of knee control. DLS was found to challenge knee control the least, which seems related to the double limb support during this activity. Conversely the landing phase of SLDH and the stance phase of GAIT are single leg support activities and therefore seem more likely to prove a greater challenge to knee control, resulting in more medial–lateral knee movement variability. It was unexpected that the fluency scores for GAIT were lower than for SLDH and this result needs further clarification. This finding may be related to higher co-contraction during SLDH than GAIT (landing phase of SLDH compared to stance phase of GAIT) but it is reasonable to assume that the three activities analysed differ in terms of the movement pattern. Characteristics of these movement patterns are expected to influence fluency making it difficult to directly compare the activities for this parameter. Therefore it is recommended that interpretation of fluency is restricted to evaluating subject group differences and not for comparison across activities.
Overall, it can be concluded that SLDH is the most challenging functional exercise due to the much higher moments and therefore potential joint loading; it also challenges knee control but results in an intermediate range of joint motion. The main challenge of DLS is the high range of joint motion encountered. The relatively high MKneeMax during DLS indicates that this exercise can be used to specifically target the knee whilst gradually increasing squat depth. However, although DLS and GAIT pose different biomechanical challenges to the knee, for integration into the clinical setting it can be concluded that overall they are of similar difficulty.
4.2. Biomechanical compensation strategies in ACLR and ACLD
The second aim of this study was to evaluate if these activities challenge ACLD and ACLR individuals differently compared to CONT. The comparison of key parameters for GAIT, DLS and SLDH between ACL subject groups and CONT confirms that all ACL injured individuals used a range of compensation strategies and despite completed rehabilitation recovery seems incomplete.
Few biomechanical compensation strategies were used by ACLD and ACLR during GAIT indicating a more advanced recovery for this exercise and that it was least challenging. There was no difference in gait velocity between any of the groups, which is a finding reported in other studies (Button et al., 2005, 2008; Zabala et al., 2013). Both ACLD and ACLR used increased ankle RoM during GAIT. The mean difference was 2° so the clinical significance of this finding is uncertain but it is a compensation strategy consistently used by ACLD for all the exercises. During DLS and SLDH this accompanies increased peak internal ankle plantarflexor moments and confirms that ACLD showed less recovery and compensated at the ankle. This current study is the first to demonstrate that ACLD used increased fluency to enhance knee control during GAIT compared to CONT. This could relate to a strategy to “freeze degrees of freedom” (Bernstein, 1967; Higuchi et al., 2002; Verrel et al., 2013). Increased knee control was not accompanied with reduced sagittal knee RoM, but may relate to the subtle alteration in ankle RoM noted above. It is important to highlight that the ACLDno-hop also had lower mean scores on the IKDC questionnaire and high mean score on the fear of re-injury. Surprisingly there was no difference in their fluency from CONT during SLDH, which is a more challenging activity. A likely explanation is that eight ACLD individuals were unable to SLDH, so unlike GAIT not all the individuals were included in the analysis leaving only the better performers of this SLDH activity.
Squat performance was not fully recovered in ACLR and ACLD compared to CONT as demonstrated by the reduced RoMknee, representing reduced squat depth. ACLD were more challenged than ACLR as their DLS was altered most. ACLD also used reduced RoMhip. For both groups the kinematic compensation patterns are reflected in altered moments. ACLD demonstrated increased MankleMax moments whilst using reduced MhipMax, MKneeMax and MaddMax. In line with this ACLR had reduced MKneeMax and MaddMax. There was no difference in fluency scores at the knee for ACL compared to CONT, this is explained because DLS occurs in double leg support and therefore challenges knee control less in the frontal plane. Few studies have investigated squatting compensation strategies in ACLR and ACLD. Reduced MKneeMax and a trend of increased MhipMax have been reported elsewhere (Salem et al., 2003). It can be concluded that despite DLS being classified in the current study as an early rehabilitation exercise and posing low challenge to ACL, these individuals performed it with widespread movement adaptations and had not recovered performance of DLS. It therefore seems to be a more difficult exercise compared to GAIT for these patients after all.
SLDH was the most difficult exercise, especially for ACLD as eight were unable to hop. Both ACL groups had reduced performance, demonstrated by a shorter hop distance. Reduced hop distance has been reported by several other studies evaluating ACLD (Button et al., 2006; Gauffin et al., 1990; Gustavsson et al., 2006; Scavenius et al., 1999). For ACLR, variable recovery of hop distance has been reported; Orishimo et al. (2010) found hop distance to recover, whereas Gokeler et al. (2010) reported that it had not. Taking the reduced hop distance into consideration both ACL groups still used altered strategies. Both ACL groups demonstrated reduced RoMknee but this did not result in reduced MkneeMax for ACL and may indicate increased muscle co-activation; stiffening the knee. Both ACL groups used a strategy of increased MhipMax and ACLD also used increased MankleMax. This is a strategy to increase the role the ankle and hip joints played in controlling the deceleration. This finding is supported by the literature (Oberlander et al., 2012; Rudolph et al., 2000). Knee control as represented by the fluency scores was lower in the ACLR and may represent incomplete recovery of knee control for these subjects. In ACLD there was no difference in fluency compared to CONT; clearly just including ACLD that had the better recovery and could hop resulted in better knee control than may have been expected. Interestingly the cautious execution with increased knee control in ACLR was not accompanied by altered MaddMax. However the altered knee control could result in a shift of the point of internal knee joint loading and lead to other potential soft tissue damage (Andriacchi et al., 2009).
4.3. Clinical implications
DLS and GAIT should be incorporated early in rehabilitation as loading was comparable but these activities have different roles. DLS permits loading over a larger range of motion, from a stable double stance position and specifically targets knee extension whilst gradually increasing squat depth. GAIT loads the knee over a small range of motion but potentially challenges knee control due to the single leg stance. DLS is generally considered a safe exercise for ACLR individuals as it places relatively low stress on the ACL except at higher flexion angles (Escamilla et al., 2012). The large range of knee motion demonstrated in the current study indicates that initially patients should start with a mini squat. The low moments suggest that GAIT and DLS are unlikely to have a strengthening effect beyond the early rehabilitation phase, unless additional loading is added. The continued biomechanical compensation strategies for the ACL subjects demonstrate that patients have not fully recovered DLS and specific rehabilitation techniques are required to address these. Further development of ACLD rehabilitation protocols is needed, as there are currently no specific recommendations for GAIT and DLS exercises (Chmielewski et al., 2005; Hartigan et al., 2009).
SLDH was the most challenging activity and both ACLR and ACLD demonstrated reduced performance and biomechanical compensation strategies. Predictably, SLDH should be used in the advanced rehabilitation stage as it challenges knee joint motion, moments and control. Clearly, general performance measures alone are not sufficient to evaluate recovery and additional biomechanical information is required to inform successful rehabilitation. A recent review has indicated that reduced RoMknee during landing can result in larger ACL forces (Escamilla et al., 2012). This is potentially disadvantageous to the ACLR group and the recommendation is to encourage ACL individuals to land using ‘soft’ landings, which require large knee RoM (Laughlin et al., 2011). Therefore rehabilitation protocols also need to include information on prescribing functional exercise and exercise technique as current methods still seem to result in incomplete recovery and biomechanical compensations.
The main findings of this study were that DLS and GAIT were of similar difficulty but challenged patients in different ways. Despite DLS being an early rehabilitation exercise ACL individuals were still demonstrating reduced performance and altered strategies. This study has highlighted the importance of biomechanics in providing insight into the challenges provided by functional exercises. Further work is required to classify the difficulty of other functional exercises and to develop a framework for functional exercises that can be used in rehabilitation protocols and exercise prescription. In addition identification of compensation strategies that ACL individuals are using can be used to inform rehabilitation training methods.
Conflict of interest statement
The authors listed on this manuscript have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Acknowledgements
We thank Mr. P Rimmer and Miss P Swar for their help with data collection and processing. We are also grateful to Dr. Sparkes for support with the development of the study. We acknowledge NISCHR CRC for their support with subject recruitment and data collection. Dr. Roos is funded by Arthritis Research UK (Grant No 18461). Dr. Button is funded by RCBC and NISCHR, Wales. We would like to thank Cardiff and Vale University Health Board for support with recruitment, in particular Mr. C Wilson, Mr. R Williams, Miss S Gardner, Miss J Parry-Williams and Mr. P Adamson.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial- ShareAlike License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- Andriacchi T.P., Koo S., Scanlan S.F. Gait mechanics influence healthy cartilage morphology and osteoarthritis of the knee. J. Bone Joint Surg. Am. 2009;91(Suppl. 1):95–101.2. doi: 10.2106/JBJS.H.01408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardern C.L., Webster K.E., Taylor N.F., Feller J.A. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br. J. Sports Med. 2011;45:596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- Barber-Westin S.D., Noyes F.R., McCloskey J.W. Rigorous statistical reliability, validity, and responsiveness testing of the Cincinnati knee rating system in 350 subjects with uninjured, injured, or anterior cruciate ligament-reconstructed knees. Am. J. Sports Med. 1999;27:402–416. doi: 10.1177/03635465990270040201. [DOI] [PubMed] [Google Scholar]
- Bernstein N. Pergamon Press; Oxford: 1967. The Co-ordination and Regulation of Movements. [Google Scholar]
- Beynnon B.D., Uh B.S., Johnson R.J., Abate J.A., Nichols C.E., Fleming B.C., Poole A.R., Roos H. Rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs administered over 2 different time intervals. Am. J. Sports Med. 2005;33:347–359. doi: 10.1177/0363546504268406. [DOI] [PubMed] [Google Scholar]
- Button K., van Deursen R., Price P. Measurement of functional recovery in individuals with acute anterior cruciate ligament rupture. Br. J. Sports Med. 2005;39:866–871. doi: 10.1136/bjsm.2005.019984. (discussion 866–71) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Button K., van Deursen R., Price P. Classification of functional recovery of anterior cruciate ligament copers, non-copers, and adapters. Br. J. Sports Med. 2006;40:853–859. doi: 10.1136/bjsm.2006.028258. (discussion 859) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Button K., van Deursen R., Price P. Recovery in functional non-copers following anterior cruciate ligament rupture as detected by gait kinematics. Phys. Ther. Sport. 2008;9:97–104. doi: 10.1016/j.ptsp.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Chmielewski T.L., Hurd W.J., Rudolph K.S., Axe M.J., Snyder-Mackler l. Perturbation training improves knee kinematics and reduces muscle co-contraction after complete unilateral anterior cruciate ligament rupture. Phys. Ther. 2005;85:740–749. (discussion 750–4) [PubMed] [Google Scholar]
- Deneweth J.M., Bey M.J., Mclean S.G., Lock T.R., Kolowich P.A., Tashman S. Tibiofemoral joint kinematics of the anterior cruciate ligament-reconstructed knee during a single-legged hop landing. Am. J. Sports Med. 2010;38:1820–1828. doi: 10.1177/0363546510365531. [DOI] [PubMed] [Google Scholar]
- Eitzen I., Moksnes H., Snyder-Mackler l., Risberg M.A. A progressive 5-week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J. Orthop. Sports Phys. Ther. 2010;40:705–721. doi: 10.2519/jospt.2010.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escamilla R.F., Macleod T.D., Wilk K.E., Paulos l., Andrews J.R. Anterior cruciate ligament strain and tensile forces for weight-bearing and non-weight-bearing exercises: a guide to exercise selection. J. Orthop. Sports Phys. Ther. 2012;42:208–220. doi: 10.2519/jospt.2012.3768. [DOI] [PubMed] [Google Scholar]
- Gauffin H., Pettersson G., Tegner Y., Tropp H. Function testing in patients with old rupture of the anterior cruciate ligament. Int. J. Sports Med. 1990;11:73–77. doi: 10.1055/s-2007-1024766. [DOI] [PubMed] [Google Scholar]
- Gobbi A., Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg. Sports Traumatol. Arthrosc. 2006;14:1021–1028. doi: 10.1007/s00167-006-0050-9. [DOI] [PubMed] [Google Scholar]
- Gokeler A., Hof A.L., Arnold M.P., Dijkstra P.U., Postema K., Otten E. Abnormal landing strategies after ACL reconstruction. Scand. J. Med. Sci. Sports. 2010;20:8. doi: 10.1111/j.1600-0838.2008.00873.x. [DOI] [PubMed] [Google Scholar]
- Gustavsson A., Neeter C., Thomeé P., Silbernagel K.G., Augustsson J., Thomeé R., Karlsson J. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2006;14:778–788. doi: 10.1007/s00167-006-0045-6. [DOI] [PubMed] [Google Scholar]
- Hartigan E., Axe M.J., Snyder-Mackler l. Perturbation training prior to ACL reconstruction improves gait asymmetries in non-copers. J. Orthop. Res. 2009;27:724–729. doi: 10.1002/jor.20754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higuchi T., Imanaka K., Hatayama T. Freezing degrees of freedom under stress: kinematic evidence of constrained movement strategies. Hum. Mov. Sci. 2002;21:831–846. doi: 10.1016/s0167-9457(02)00174-4. [DOI] [PubMed] [Google Scholar]
- Irrgang J.J., Anderson A.F., Boland A.L., Harner C.D., Kurosaka M., Neyret P., Richmond J.C., Shelborne K.D. Development and validation of the international knee documentation committee subjective knee form. Am. J. Sports Med. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- Kvist J., Ek A., Sporrstedt K., Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2005;13:393–397. doi: 10.1007/s00167-004-0591-8. [DOI] [PubMed] [Google Scholar]
- Laughlin W.A., Weinhandl J.T., Kernozek T.W., Cobb S.C., Keenan K.G., O'connor K.M. The effects of single-leg landing technique on ACL loading. J. Biomech. 2011;44:1845–1851. doi: 10.1016/j.jbiomech.2011.04.010. [DOI] [PubMed] [Google Scholar]
- Myklebust G., Holm I., Maehlum S., Engebretsen l., Bahr R. Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury: a follow-up study. Am. J. Sports Med. 2003;31:981–989. doi: 10.1177/03635465030310063901. [DOI] [PubMed] [Google Scholar]
- Oberlander K.D., Bruggemann G.P., Hoher J., Karamanidis K. Reduced knee joint moment in ACL deficient patients at a cost of dynamic stability during landing. J. Biomech. 2012;45:1387–1392. doi: 10.1016/j.jbiomech.2012.02.029. [DOI] [PubMed] [Google Scholar]
- Orishimo K.F., Kremenic I.J., Mullaney M.J., Mchugh M.P., Nicholas S.J. Adaptations in single-leg hop biomechanics following anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2010;18:1587–1593. doi: 10.1007/s00167-010-1185-2. [DOI] [PubMed] [Google Scholar]
- Risberg M.A., Holm I., Myklebust G., Engebretsen l. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys. Ther. 2007;87:737–750. doi: 10.2522/ptj.20060041. [DOI] [PubMed] [Google Scholar]
- Rudolph K.S., Axe M.J., Snyder-mackler l. Dynamic stability after ACL injury: who can hop? Knee Surg. Sports Traumatol. Arthrosc. 2000;8:262–269. doi: 10.1007/s001670000130. [DOI] [PubMed] [Google Scholar]
- Salem G.J., Salinas R., Harding F.V. Bilateral kinematic and kinetic analysis of the squat exercise after anterior cruciate ligament reconstruction. Arch. Phys. Med. Rehabil. 2003;84:1211–1216. doi: 10.1016/s0003-9993(03)00034-0. [DOI] [PubMed] [Google Scholar]
- Scavenius M., Bak K., Hansen S., Norring K., Jensen K.H., Jorgensen U. Isolated total ruptures of the anterior cruciate ligament—a clinical study with long-term follow-up of 7 years. Scand. J. Med. Sci. Sports. 1999;9:114–119. doi: 10.1111/j.1600-0838.1999.tb00219.x. [DOI] [PubMed] [Google Scholar]
- Smeulders M.J., Kreulen M., Bos K.E. Fine motor assessment in chronic wrist pain: the role of adapted motor control. Clin. Rehabil. 2001;15:133–141. doi: 10.1191/026921501672958566. [DOI] [PubMed] [Google Scholar]
- Strehl A., Eggli S. The value of conservative treatment in ruptures of the anterior cruciate ligament (acl) J. Trauma. 2007;62:1159–1162. doi: 10.1097/TA.0b013e31805006e7. [DOI] [PubMed] [Google Scholar]
- Verrel J., Pologe J., Manselle W., Lindenberger U., Woolacott M. Co-ordination of degrees of freedom and stabilisation of task variables in a complex motor skill: expertise related differences in cello bowing. Exp. Brain Res. 2013;224:323–334. doi: 10.1007/s00221-012-3314-2. [DOI] [PubMed] [Google Scholar]
- White K., Di Stasi S.L., Smith A.H., Snyder-Mackler l. Anterior cruciate ligament-specialized post-operative return-to-sports (acl-sports) training: a randomized control trial. BMC Musculoskelet. Disord. 2013;14:108. doi: 10.1186/1471-2474-14-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilk K.E., Kacrina l.C., Kain K.L., Kugas J.R., Andrews J.R. Recent advances in the rehabilitation of anterior cruciate ligament injuries. J. Orthop. Sports Phys. Ther. 2012;42:153–171. doi: 10.2519/jospt.2012.3741. [DOI] [PubMed] [Google Scholar]
- Zabala M.E., Favre J., Scanlan S.F., Donahue J.J., Andriacchi T.P. Three-dimensional knee moments of acl reconstructed and control subjects during gait, stair ascent, and stair descent. J. Biomech. 2013;46:515–520. doi: 10.1016/j.jbiomech.2012.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]