Abstract
Purpose:
Prostate cancer survivors (PCSs) may experience persistent symptoms following treatment. If PCSs and spouses differ in their perceptions of symptoms, that incongruence may cause mismanagement of symptoms and reduced relationship quality. The purpose of this study was to examine symptom incongruence and identify the PCS and spouse characteristics associated with symptom incongruence in older couples coping with prostate cancer.
Methods:
Participants in the study were older PCSs (>60 yrs) and their spouses (N=59 couples). Symptom incongruence was determined by comparing patient and spouse independent ratings of the severity of his cancer-related symptoms. Predictor variables included PCS age, time since diagnosis, PCS comorbidity, PCS and spouse depressive symptoms, and spouse caregiving strain.
Results:
PCS and spouse ratings of his symptom severity and the amount of incongruence over his symptoms varied significantly across couples. Overall, couples rated a moderate level of PCS symptom severity, but PCSs and their spouses significantly differed in their perceptions of PCS symptom severity with spouses rating severity higher (t = −2.66, df =51, p < 0.01). PCS younger age and high spouse caregiver strain accounted for 29% of incongruence in perceptions of PCS symptom severity.
Conclusions:
This study is among the first to show that PCSs and spouses may perceive cancer-related persistent symptoms differently. Among this older sample, younger PCS age and spouse caregiver strain were associated with incongruence in symptoms perceptions in couples. These and other factors may inform future interventions aimed at preserving relationship quality in older couples who have experienced prostate cancer.
Keywords: relationship, survivorship, quality of life, supportive care, depression
INTRODUCTION
Treatment of localized and regional prostate cancer is frequently successful with over 90% of men surviving at least five years, but many experience persistent symptoms well after treatment. Sexual dysfunction, urinary and/or bladder problems and fatigue are the most commonly reported symptoms among many that result from prostate cancer treatments [1]. Not only do symptoms adversely impact prostate cancer survivor’s (PCS) QOL and functioning, but they also affect his spouse, the quality of his marital relationship and could alter his treatment and his prognosis [2-4].
Spouses of PCSs are affected by her husband’s symptoms because they can directly impact aspects of the marital relationship (i.e., sexual dysfunction) and the distress caused by symptoms can strain the marriage [5-7]. Because spouses are often the primary caregivers for PCSs, they are also the most likely family member to help manage his symptoms. When a PCS and spouse perceive symptoms differently, the incongruence in perceptions may lead to PCS feelings of invalidation, poor relationship quality and problems with decision-making, and this has been demonstrated in prior studies of chronic illnesses and caregiving [8-10]. In cancer survivors, incongruence in perception of symptoms has been associated with declining health, depression and an increased risk of poor adjustment to prostate cancer in the PCS [11,9,12] and increases relationship strain and marital dissatisfaction within the couple [13,14]. From studies of incongruence in couples facing illnesses other than prostate cancer, differences in patient and spouse characteristics, such as physical (e.g., age and comorbidities) or emotional health (e.g., depression and caregiving strain), are linked to incongruent symptom assessment [11,9]; however, we know little about predictors of symptom incongruence specific to couples coping with prostate cancer.
Most prior research on long-term symptoms in PCSs has focused on the PCS’s report of symptoms. However, the relational context of the couple is important to the overall health and quality of life of the PCS, even in the presence of bothersome symptoms. There is little information about symptom incongruence among couples coping with prostate cancer, including the characteristics of each partner that might be associated with incongruence. Understanding the factors that influence symptom incongruence between PCS and spouses could identify couples at risk of incongruence, inform the design of interventions, and explore how effective interventions work. Traditional couple methods and those most often used in studies of patient-spouse incongruence (e.g. percent agreement, difference scores) are limited in what they can tell us about incongruence. Multilevel modeling (MLM) is an innovative approach for assessing couple incongruence and for determining which member of the couple is scoring higher or lower. In contrast to studies that use a difference score or average score, MLM simultaneously creates a latent couple average and latent couple incongruence score, corrected for measurement error. In addition, it allows the researcher to predict individual variability around these true scores [15].
We had the unique opportunity to explore patterns (e.g., degree and directionality) and predictors of incongruence using baseline data from PCSs and spouses who were enrolled in a randomized trial of partnered exercise training. The purpose of this secondary analysis was to use MLM to determine the degree and directionality of symptom incongruence between PCSs and spouses and to explore the PCS and spouse characteristics associated with symptom incongruence.
METHODS
Sample
Participants in this study were PCSs who had completed primary cancer treatment and their spouses who lived in the same residence. Couples were participants in a randomized trial of exercise that is described in detail elsewhere [16]. The present study examined baseline data that was collected prior to randomization to study groups. Complete data on all variables was available for 59 out of 62 enrolled couples and used for analysis. PCSs were eligible to participate in the study if they received treatment for histologically confirmed prostate cancer of any stage, were not currently undergoing radiation therapy or chemotherapy for prostate cancer, were aged 60 or over and were currently residing with a spouse (or co-residing partner) willing to participate. Procedures for the trial and the study reported here were approved by a university IRB board.
Measures
PCS Symptom Severity was measured with a 15-item list of symptoms specific to persons with cancer [17] and covering the following symptom types: vasomotor, neuropathic, neurocognitive, urinary, and cardio-respiratory. This instrument has demonstrated clinical validity and reliability in people undergoing cancer treatment [18]; though in our sample of men who were mostly post-treatment perceived symptoms could also reflect those that persist long term. For any symptom that was considered present in the past 7 days, the severity of each symptom was then rated with a 5-level Likert-type scale (1 = not present / not at all severe to 5 = extremely severe) and the average severity was then calculated. Higher average scores indicate more severe symptoms with a possible range of 1-5. In addition to completion of the checklist by the PCS, the spouse completed the checklist based on observations of the partner’s symptoms.
PCS and/or Spouse Predictors of Symptom Incongruence. We focused on characteristics of both the PCS and spouse that may predict symptom incongruence within couples. We were limited in our selection and number of independent variables to those that were measured in the parent trial and based on the available sample size. As this was an exploratory study, we chose to focus on individual characteristics that have been found to be associated with incongruence in other populations, in particular, the physical (age [19,20], clinical history [11] and comorbidities [11,9]) health of the patient and emotional health of each partner (depressive symptoms [21,22] and caregiver strain [23,24]). An a priori power analysis was not performed, but rather the number of predictors entered into HLM models were limited in order to maximize statistical power.
Depressive symptoms was evaluated by the Center for Epidemiological Studies-Depression (CES-D) [25]. The 20-item CES-D scale has been widely used and demonstrates good internal consistency (Cronbach’s α=.86 - .92), sensitivity, specificity and validity. Both PCSs and spouses rated their own depressive symptoms, with scores that range from 0-60 and higher scores indicating greater depressive symptoms.
Caregiver Strain was measured using the role overload scale which assesses the extent to which spouse’s time and energy are exhausted by the demands of caring for their partner [26]. The 3-item scale has good internal consistency (Cronbach’s α=.71 to .78), high reliability, and evidence of construct validity with patient physical function and family member depression [23]. Scores range from 3-12 and higher scores indicate greater caregiver strain.
Current comorbidity was characterized by the 18-item Charlson Comorbidity Index [27], with scores ranging from 0-37 and higher scores indicating more chronic medical conditions. Risk of comorbidity associated with obesity was characterized by body mass index (BMI; kg/m2). Charlson scores for PCSs were included as a potential predictor of symptom incongruence based on previous research.
Age was included as a potential predictor of symptom incongruence because previous research has shown that the way that couples cope with chronic illness may vary across the lifespan, where older couples tend to adapt better to the illness experience than younger couples [19,20].
Demographics and clinical information including age, education, employment, length of relationship and cancer specific information for PCSs were gathered by self-report.
Statistical Analysis
Zero-order correlations were run between dependent and independent variables to guide selection of predictors and examine potentially interdependent variables. HLM 7 [28] was used to examine couple incongruence in PCS symptom severity using full information maximum likelihood (FIML) estimation. This analytic approach determines the heterogeneity of variance in patient-spouse incongruence in patient symptom severity and identifies variables associated with this incongruence. A couple incongruence model similar to the incongruence models described by Barnett et al [29] and Lyons et al [30] will illustrate the similarities and differences in perceptions of patients and spouses. Due to the inability to calculate parallel scales as originally suggested by Raudenbush and colleagues [28], the alternative “known variance” approach described by Cano et al [31] was used. This approach estimates measurement error using the formula ([1 – Reliability] X observed variance).
The following model is fit separately to the symptom data for each couple j:
| (1) |
Severityij represents the symptom severity score i in couple j. The Level 1 or within-couple model expresses the outcome as a function of a dummy variable that indicates whether the score was reported by the patient or the spouse, plus a residual term r that captures measurement error in the outcome scores. The predictor is coded −0.5 for the patient and +0.5 for the spouse. Under this formulation, the model intercept (β0j) represents the expected value of the outcome SEVERITY when the predictor INDICATOR is zero, which is the couple average; the model slope (β1j) represents the incongruence or gap between the two members of the couple.
The first step involves an examination of the unconditional Level 2 or between-couple model, which provides estimates of the population averages for couple symptom severity and couple incongruence and the variability around those averages. A chi-square test is performed to test whether the variances are significantly different from zero. When they are, significant heterogeneity exists across couples and predictors are introduced to explain the heterogeneity.
Second, the conditional Level 2 model adds predictors to explain the heterogeneity across couples in average symptom severity and incongruence in symptom severity as follows:
The effect of PCS and spouse characteristics on symptom severity are captured by the coefficients γ02 through γ06, while the effect of PCS and spouse characteristics on symptom incongruence are captured by the coefficients γ12 through γ16. Predictor variables were mean centered, where appropriate, for ease of interpretation.
RESULTS
Sample
Couples in this analysis (N=59) were together an average of 42 years, with men older and in poorer health than their spouses (Table 1). The participants reflected the largely Caucasian demographic in Oregon, were well educated and consistent with their age, most were also retired. For PCSs, men were mostly within 10 years of cancer diagnosis with less than half (44%) having received radiation therapy, one-quarter currently on androgen deprivation therapy (ADT), and few participants that received chemotherapy. A small fraction of men (13%) had metastatic disease, but were not actively receiving treatment at the time of study enrollment.
Table 1.
Baseline demographic and clinical characteristics of prostate cancer survivors (PCS) and their spouses.
| PCS (N=59) | Spouse (N=59) | ||
|---|---|---|---|
|
| |||
| Characteristic | Mean (SD) or % of sample |
Mean (SD) or % of sample |
p-value* |
|
| |||
| Age (yrs.) | 71.6 (7.4) | 68.0 (7.7) | <0.01 |
| Race (% Caucasian) | 92% | 92% | 0.45 |
| Ethnicity (% Non-Hispanic) | 95% | 93% | 0.50 |
| Education (% above high school) | 85% | 75% | 0.45 |
| Employment status | |||
| % Retired | 71% | 59% | |
| % Working full or part-time | 25% | 22% | 0.02 |
| % Homemaker | 0% | 15% | |
| % Unemployed | 3% | 3% | |
| Marital status (% married) | 100% | — | |
| Length of relationship (years) | 42.2 (14.0) | — | |
| Comorbidity Index | 3.0 (2.4) | 1.3 (1.8) | <0.01 |
| BMI (kg/m2) | 28.8 (3.9) | 29.0 (6.8) | 0.87 |
|
| |||
| Patient characteristics | |||
|
| |||
| Time since diagnosis (yrs.) | 5.5 (3.9) | N/A | |
| Received chemotherapy (%) | 2% | N/A | |
| Received radiation therapy (%) | 44% | N/A | |
| Currently on ADT (%) | 27% | N/A | |
| Metastatic disease (%) | 13% | N/A | |
Abbreviations: ADT = androgen deprivation therapy; N/A = not applicable
p-value to test for significant differences between patient and spouse using paired t-tests for continuous data or chi-squares tests for categorical data
Average Symptom Severity
The average PCS symptom severity scores were higher when rated by spouses (2.75, SD = 0.60) than when rated by PCSs (2.51, SD = 0.60). The difference was statistically significant (t = −2.66, df =51, p < 0.01).
Correlations between PCS Symptom Severity and Potential Independent Variables
The zero-order correlations between the independent variables (PCS age, time since diagnosis, PCS comorbidity, PCS depressive symptoms, spouse depressive symptoms, and spouse caregiver strain) and each PCS and spouse ratings of PCS symptom severity are shown in Table 2. Correlations indicate that older age and higher levels of depressive symptoms were associated with greater PCS symptom severity. Spouses were more likely to report the PCS as having greater symptom severity when the PCS had higher levels of depressive symptoms, and the spouse herself, reported higher depressive symptoms and higher levels of caregiver strain. Finally, there was a significant, moderate correlation between PCS and spouse depressive symptoms.
Table 2.
Zero-Order Correlations Among Independent Variables and Prostate Cancer Survivor (PCS) Symptom (Sx) Severity (as reported by both PCS and spouses (SP)) (N=59 Couples)
| Variables | PCS Age |
Time Since Diagnosis |
PCS Co- morbidity |
PCS Depressive Sx |
SP Depressive Sx |
SP Caregiver Strain |
|---|---|---|---|---|---|---|
| Dependent | ||||||
|
| ||||||
| PCS Sx Severity (PCS Report) |
.29* | .10 | .21 | .35** | .29* | .03 |
| PCS Sx Severity (SP Report) |
−.01 | .18 | .20 | .30* | .27* | .33* |
|
| ||||||
| Independent | ||||||
|
| ||||||
| PCS Age | ||||||
| Time Since Diagnosis | .32* | |||||
| PCS Comorbidity | .05 | −.13 | ||||
| PCS Depressive Sx | .05 | .16 | .18 | |||
| SP Depressive Sx | .19 | .34** | −.03 | .27* | ||
| SP Caregiver Strain | .22 | .18 | .06 | .23 | .33* | |
p < 0.05
p < 0.01
p < 0.001
HLM Level 1 Model: Patient-Spouse Symptom Incongruence
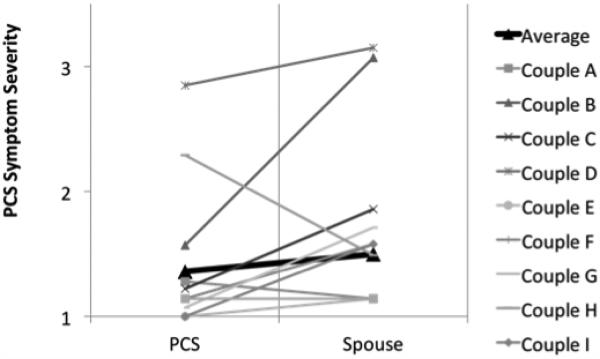
Level 1 results (Table 3) showed that, on average, couples rated the PCS’s symptom severity as 2.61 (p < 0.001), indicating a moderate level of severity (1-5 scale). The average incongruence score for PCS symptom severity was 0.26 (p < 0.01). The positive direction indicates that, on average, spouses rated PCS symptom severity higher than did PCSs. There was significant variability around the average couple mean for PCS symptom severity χ2 = 334.21, p < 0.001 and the average couple incongruence χ2 = 130.91, p< 0.001 which is illustrated using a sample of 10 couples (Fig 1). Although the couple average indicated a moderate level of symptom severity, the Level 1 model showed significant variability within couples in both steepness and direction of slope.
Table 3.
Level 1 Model: Couple Means and Prostate Cancer Survivor (PCS)-Spouse Incongruence of PCS Symptom Severity
| Symptom Severity |
||
|---|---|---|
| Parameter | Coefficient | SE |
| Fixed effects | ||
| Couple Mean (intercept) | 2.61*** | 0.07 |
| Incongruence (slope)a | 0.26** | 0.09 |
|
| ||
| Variance Component | df | |
|
| ||
| Random effects | ||
| Couple Mean | 0.25*** | 51 |
| Incongruence | 0.26*** | 51 |
Positive incongruence scores indicate that the spouse is rating PCS symptom severity as higher than the PCS; negative incongruence scores indicate that the PCS is rating PCS symptom severity as higher than the spouse.
p < 0.05
p < 0.01
p < 0.001.
Fig 1.
Couple ratings of symptom severity for prostate cancer survivors (PCS) as reported by each the PCS and his spouse in a sample of 10 couples. Average mean for PCS symptom severity ratings is shown in the bold, black line.
HLM Level 2 Model: Predicting PCS-Spouse Symptom Incongruence
A Level 2 model introduced independent variables of PCS age, PCS comorbidity, PCS depressive symptoms, spouse depressive symptoms, and spouse caregiver strain into models to explain variability in couple average ratings of PCS symptom severity and incongruence between PCS and spouse in ratings of PCS symptom severity. Results (table 4) showed that PCS depressive symptoms were significantly associated with couple mean ratings of PCS symptom severity, controlling for other variables in the model, and the variables together accounted for 32% of the variance in couple mean ratings of PCS symptom severity. PCS age and spouse caregiver strain were significantly associated with incongruence, controlling for other variables, and the model explained 29% of the incongruence in ratings of PCS symptom severity. Couples were significantly more likely to experience more incongruence in how they rated PCS symptom severity when PCS age was lower (60-70 yrs.) and the spouse reported higher levels of caregiver strain.
Table 4.
Level 2 Model: Fixed Effect Results Predicting Prostate Cancer Survivor (PCS)-Spouse (SP) Incongruence in PCS Symptom Severity
| Parameter | Couple Mean | Incongruence | ||
|---|---|---|---|---|
|
| ||||
| Independent Variable (Predictor) | Coefficient | SE | Coefficient | SE |
| Intercepta | 2.61*** | 0.06 | 0.27** | 0.08 |
| PCS Age | 0.01 | 0.01 | −0.03* | 0.01 |
| PCS Comorbidity | 0.04 | 0.03 | 0.01 | 0.03 |
| PCS Depressive Symptoms | 0.02* | 0.01 | −0.01 | 0.01 |
| SP Depressive Symptoms | 0.01 | 0.01 | −0.01 | 0.01 |
| SP Role Overload | 0.01 | 0.03 | 0.12** | 0.05 |
Model controls for time since diagnosis.
p < 0.05
p < 0.01
p < 0.001
DISCUSSION
In a sample of older couples who have shared the experience of prostate cancer treatment, there was significant variability among couples in how the PCS and his spouse rated the severity of his symptoms and whether or not the PCS and his spouse were different in their ratings. Higher levels of depressive symptoms in the PCS or spouse were correlated with either of them reporting higher levels of PCS symptom severity, consistent with previous research [31]. However, when using MLM to determine which characteristics predicted the degree of incongruence between the PCS and his spouse over PCS symptom severity, depressive symptoms in the PCS or spouse did not contribute to whether or not they were different (incongruent) in their ratings of overall symptom severity, when controlling for other factors. Rather, factors associated with the couple being incongruent in assessing symptoms were his younger PCS age relative to older peers and the level of caregiving strain reported by his spouse.
Prior studies of incongruence between cancer patients and spouses have reported inconsistent findings with some studies suggesting low incongruence [32-35] and others suggesting high incongruence [36,37]. Within couples in our study, we found spouses rated PCS symptoms significantly higher than did PCSs themselves, a finding that is consistent with other studies that observe incongruence between family members and cancer patients over how much a patient’s physical function is changing or how severe the patient’s symptoms are [38,33,39,40]. Incongruence in symptoms in cancer survivors has been associated with poorer health, depression and a higher risk of poor adjustment to cancer among the survivors [11,9,12], though earlier studies did not consider what might be contributing to the incongruent perceptions so that a basis for intervention could be considered. In couples coping with heart disease or who have faced any type of cancer, incongruence is associated with higher levels of relationship strain and marital dissatisfaction for both partners [13,14]. In the single study specific to couples coping with prostate cancer, Merz recently reported that positively correlated appraisal of urogenital symptoms between PCS and spouses was associated with better health-related quality of life (HRQOL), less stress, better coping ability, and greater stability in the relationship compared to a lower HRQOL reported by couples who had incongruent perceptions of how bothersome his symptoms were [41]. The clinical relevance of incongruence using our symptom measure is uncertain since our study was the first use of this instrument to evaluate incongruence. Future longitudinal studies where incongruence predicts outcomes over time using our symptom checklist could provide an indication of the meaningfulness of varying magnitudes of incongruence.
Differences in patient and spouse characteristics, such as physical or emotional health, could lead to incongruent symptom assessment. Within the caregiving literature, spouses who are extremely burdened or depressed may perceive the patient to be more impaired than he or she actually is [21,22]. Symptom incongruence has been found to be higher when caregiver strain from providing care is high [23,24]. In our study, when spouses felt more overwhelmed by their role as caregivers the degree of disagreement between her and her husband over the severity of his symptoms increased. While spouses who felt more overwhelmed reported more depressive symptoms, her level of strain may have more strongly influenced her to perceive the severity of her husband’s symptoms higher than either her or his depressive symptoms. The low level of depressive symptoms among our sample may also explain why they failed to contribute to the model.
In addition to caregiver strain, we found that incongruence between the couple over PCS symptoms was more likely when the PCS was younger. Among our older sample, young-old PCSs (60-70 yrs.) reported less symptom severity than old-old PCSs (>70 yrs.), yet couples with younger men were at greater risk for incongruent perceptions. In our study, young-old PCS were closer to diagnosis, more likely to have had prostate cancer surgery and just as likely to have received other therapy (radiation and/or ADT) as old-old PCS yet they reported less severe symptoms, suggesting that they could be minimizing or concealing their symptoms, have had less time since treatment to adapt to their symptoms, or simply experiencing fewer age-related symptoms. Incongruence among young-old couples could also be a reflection of the developmental differences found between middle-aged and older couples that indicate middle-aged couples are more at risk for poor psychological and relational well-being in the face of chronic illness compared to older couples [42], though there have been no studies that have quantitatively evaluated age and symptom incongruence in couples with a history of prostate cancer. While our study presents only preliminary evidence of potential age differences in symptom incongruence among older couples, future research is warranted about whether younger couples are more likely to be incongruent or inconsistent in recognizing and evaluating symptoms of prostate cancer treatment.
Our study has several strengths. To our knowledge, ours is the first study to use MLM to examine the patterns and predictors of incongruence in symptom assessment among couples coping with prostate cancer. The aim of our study was to examine symptom incongruence and predictors of symptom incongruence among couples coping with prostate cancer. Analytic approaches other than MLM are useful for either identifying the pattern of incongruence or examining the predictors of incongruence, but cannot simultaneously address both objectives. By examining PCS and spouse characteristics associated with incongruence, we can begin to identify those couples at greatest risk for disparate perceptions of the severity of symptoms experienced by PCSs. The study also has limitations, some of which were imposed by the design of this study as a secondary data analysis. Specifically, the cross sectional data cannot imply causation between predictors and incongruence, the potential predictor variables were constrained by the choice of instruments included in the RCT as opposed a priori selection of predictors, and the sample size limited the number of predictor variables included in our models. Despite these limitations, age and caregiver strain were significant predictors of incongruence. However, it is probable that other characteristics that we did not include in the model contribute to incongruence, such as shared characteristics of the couple (e.g., length of relationship, time spent in shared activities, relationship quality) or communication patterns, and these should be explored in future studies. Another potential limitation was our use of a general cancer symptom checklist rather than a measure of symptoms specific to prostate cancer. Though our checklist included symptoms common across cancer types (i.e., cognitive trouble, fatigue) and in PCS (i.e., incontinence), it is possible that our observations may not extend to symptoms we did not measure, like loss of libido. Nor does it allow for examination of incongruence for individual symptoms. Future research should build on this work by employing MLM to examine incongruence for symptoms specific to prostate cancer.
While incongruence within couples over patient symptoms can threaten relationship quality and increase the risk of poor health in each partner, incongruence may increase [37] or decrease over time [40] suggesting that incongruence is amenable to interventions. Among couples in our study, when the husband was younger or when the spouse felt high caregiving strain, spouses were more likely to disagree over his symptoms. Future interventions aiming to preserve relationship quality among couples coping with prostate cancer might consider targeting younger couples and approaches that manage strain from caregiving. However, it is also clear that additional descriptive studies are warranted first and should consider whether other factors such qualities of the marital relationship and couple communication influence incongruence. Caregiving strain among spouses in our study was positively correlated with her depressive symptoms that were in turn associated with PCS depressive symptoms. These interdependencies within the couple underscore the rationale and justification for taking a dyadic approach to the prostate cancer experience and point to couples-based approaches that could simultaneously lessen the physical, emotional and relationship costs of prostate cancer.
Acknowledgements
The work was supported by funding from the National Cancer Institute 1R21 CA137272 to KWS (Principal Investigator) and KSL (Co-Investigator).
Footnotes
Disclosures: None
REFERENCES
- 1.Hsiao CP, Loescher LJ, Moore IM. Symptoms and symptom distress in localized prostate cancer. Cancer Nurs. 2007;30(6):E19–32. doi: 10.1097/01.NCC.0000300163.13639.bc. [DOI] [PubMed] [Google Scholar]
- 2.Clark JA, Talcott JA. Symptom indexes to assess outcomes of treatment for early prostate cancer. Med Care. 2001;39(10):1118–1130. doi: 10.1097/00005650-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Chang VT, Thaler HT, Polyak TA, Kornblith AB, Lepore JM, Portenoy RK. Quality of life and survival: the role of multidimensional symptom assessment. Cancer. 1998;83(1):173–179. doi: 10.1002/(sici)1097-0142(19980701)83:1<173::aid-cncr23>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 4.Dandapani SV, Sanda MG. Measuring health-related quality of life consequences from primary treatment for early-stage prostate cancer. Semin Radiat Oncol. 2008;18(1):67–72. doi: 10.1016/j.semradonc.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim Y, Kashy D, Wellisch D, Spillers R, Kaw C, Smith T. Quality of Life of Couples Dealing with Cancer: Dyadic and Individual Adjustment among Breast and Prostate Cancer Survivors and Their Spousal Caregivers. Ann Behav Med. 2008;35(2):230–238. doi: 10.1007/s12160-008-9026-y. [DOI] [PubMed] [Google Scholar]
- 6.Northouse LL, Mood DW, Montie JE, Sandler HM, Forman JD, Hussain M, Pienta KJ, Smith DC, Sanda MG, Kershaw T. Living with prostate cancer: patients’ and spouses’ psychosocial status and quality of life. J Clin Oncol. 2007;25(27):4171–4177. doi: 10.1200/JCO.2006.09.6503. [DOI] [PubMed] [Google Scholar]
- 7.Resendes LA, McCorkle R. Spousal responses to prostate cancer: an integrative review. Cancer Invest. 2006;24(2):192–198. doi: 10.1080/07357900500524652. [DOI] [PubMed] [Google Scholar]
- 8.Franks P, Fiscella K, Shields CG, Meldrum SC, Duberstein P, Jerant AF, Tancredi DJ, Epstein RM. Are patients’ ratings of their physicians related to health outcomes? Ann Fam Med. 2005;3(3):229–234. doi: 10.1370/afm.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miaskowski C, Zimmer EF, Barrett KM, Dibble SL, Wallhagen M. Differences in patients’ and family caregivers’ perceptions of the pain experience influence patient and caregiver outcomes. Pain. 1997;72(1-2):217–226. doi: 10.1016/s0304-3959(97)00037-7. [DOI] [PubMed] [Google Scholar]
- 10.Sunny L, Hopfgarten T, Adolfsson J, Steineck G. Economic conditions and marriage quality of men with prostate cancer. BJU Int. 2007;99(6):1391–1397. doi: 10.1111/j.1464-410X.2007.06807.x. [DOI] [PubMed] [Google Scholar]
- 11.Sneeuw KC, Aaronson NK, Sprangers MA, Detmar SB, Wever LD, Schornagel JH. Comparison of patient and proxy EORTC QLQ-C30 ratings in assessing the quality of life of cancer patients. J Clin Epidemiol. 1998;51(7):617–631. doi: 10.1016/s0895-4356(98)00040-7. [DOI] [PubMed] [Google Scholar]
- 12.Boehmer U, Clark JA. Communication about prostate cancer between men and their wives. J Fam Pract. 2001;50(3):226–231. [PubMed] [Google Scholar]
- 13.Coyne JC, Smith DA. Couples coping with a myocardial infarction: A contextual perspective on wives’ distress. J Personal Soc Psychol. 1991;61:404–412. doi: 10.1037//0022-3514.61.3.404. [DOI] [PubMed] [Google Scholar]
- 14.Zakowski SG, Harris C, Krueger N, Laubmeier KK, Garrett S, Flanigan R, Johnson P. Social barriers to emotional expression and their relations to distress in male and female cancer patients. Br J Health Psychol. 2003;8(Pt 3):271–286. doi: 10.1348/135910703322370851. [DOI] [PubMed] [Google Scholar]
- 15.Maguire MC. Treating the dyad as the unit of analysis: A primer on three analytic approaches. J Marriage Fam. 1999;61:213–223. [Google Scholar]
- 16.Winters-Stone KM, Lyons KS, Nail LM, Beer TM. The Exercising Together project: Design and recruitment for a randomized, controlled trial to determine the benefits of partnered strength training for couples coping with prostate cancer. Contemp Clin Trials. 2012;33(2):342–350. doi: 10.1016/j.cct.2011.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walker BL, Nail LM, Larsen L, Magill J, Schwartz A. Concerns, affect, and cognitive disruption following completion of radiation treatment for localized breast or prostate cancer. Oncol Nurs Forum. 1996;23(8):1181–1187. [PubMed] [Google Scholar]
- 18.Nail L, Jones L, Greene D, DL S, Jensen R. Use and perceived efficacy of self-care activities in patients receiving chemotherapy. Oncol Nurs Forum. 1991;18:883–887. [PubMed] [Google Scholar]
- 19.Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychol Bull. 2007;133(6):920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- 20.Harden JK, Northouse LL, Mood DW. Qualitative analysis of couples’ experience with prostate cancer by age cohort. Cancer Nurs. 2006;29(5):367–377. doi: 10.1097/00002820-200609000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Pruchno RA, Burant CJ, Peters ND. Typologies of caregiving families: Family congruence and individual well-being. Gerontologist. 1997;37(2):157–167. doi: 10.1093/geront/37.2.157. [DOI] [PubMed] [Google Scholar]
- 22.Zweibel N, Lydens LA. Incongruent perceptions of older adult/caregiver dyads. Fam Relat. 1990;39:63–67. [Google Scholar]
- 23.Broberger E, Tishelman C, von Essen L. Discrepancies and similarities in how patients with lung cancer and their professional and family caregivers assess symptom occurrence and symptom distress. J Pain Symptom Manage. 2005;29:572–583. doi: 10.1016/j.jpainsymman.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 24.Porter LS, Keefe FJ, McBride CM, Pollak K, Fish L, Garst J. Perceptions of patients’ self-efficacy for managing pain and lung cancer symptoms: correspondence between patients and family caregivers. Pain. 2002;98:169–178. doi: 10.1016/s0304-3959(02)00042-8. [DOI] [PubMed] [Google Scholar]
- 25.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Measure. 1977;1:385–401. [Google Scholar]
- 26.Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 27.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 28.Raudenbush SW, Bryk AS, Congdon R. 2nd SSI; Lincolnwood, IL: 2004. Hierarchical linear and nonlinear modeling. [Google Scholar]
- 29.Barnett RC, Marshall NL, Raudenbush SW, Brennan RT. Gender and the relationship between job experiences and psychological distress: A study of dual-earner couples. J Personal Soc Psychol. 1993;64:794–806. doi: 10.1037//0022-3514.64.5.794. [DOI] [PubMed] [Google Scholar]
- 30.Lyons KS, Zarit SH, Sayer AG, Whitlatch CJ. Caregiving as a dyadic process: Perspectives from caregiver and receiver. J Gerontol Psyc Sci. 2002;57B:P195–P204. doi: 10.1093/geronb/57.3.p195. [DOI] [PubMed] [Google Scholar]
- 31.Cano A, Johansen AB, Franz A. Multilevel analysis of couple congruence on pain, interference, and disability. Pain. 2005;118(3):369–379. doi: 10.1016/j.pain.2005.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dar R, Beach C, Barden P, Cleeland CS. Cancer pain in the marital system: a study of patients and their spouses. J Pain Symp Manage. 1992;7:87–93. doi: 10.1016/0885-3924(92)90119-3. [DOI] [PubMed] [Google Scholar]
- 33.Kristjanson LJ, Nikoletti S, Porock D, Smith M, Lobchuk M, Pedler P. Congruence between patients’ and family caregivers’ perceptions of symptom distress in patients with terminal cancer. J Palliat Care. 1998;14(3):24–32. [PubMed] [Google Scholar]
- 34.Kurtz ME, Kurtz JC, Given CC, Given B. Concordance of cancer patient and caregiver symptom reports. Cancer Prac. 1996;4:185–190. [PubMed] [Google Scholar]
- 35.Sigurdardottir V, Brandberg Y, Sullivan MD. Criterion-based validation of the EORTC QLQ-C36 in advanced melanoma: the CIPS questionnaire and proxy raters. Qual Life Res. 1996;5:375–386. doi: 10.1007/BF00433922. [DOI] [PubMed] [Google Scholar]
- 36.Lin C-C. Congruity of cancer pain perceptions between Taiwanese patients and family caregivers: Relationship to patients’ concerns about reporting pain and using analgesics. J Pain Symptom Manage. 2001;21:18–26. doi: 10.1016/s0885-3924(00)00230-x. [DOI] [PubMed] [Google Scholar]
- 37.Lobchuk MM, Kristjanson LJ, Degner LF, Blood P, Sloan J. Perceptions of symptom distress in lung cancer patients: I. Congruence between patients and primary family caregivers. J Pain Symptom Manage. 1997;14:136–146. doi: 10.1016/s0885-3924(97)00022-5. [DOI] [PubMed] [Google Scholar]
- 38.Elliott BA, Elliott TE, Murray DM, Braun BL, Johnson KM. Patients and family members: The role of knowledge and attitudes in cancer pain. J Pain Symptom Manage. 1996;12:209–220. doi: 10.1016/0885-3924(96)00124-8. [DOI] [PubMed] [Google Scholar]
- 39.Lobchuk MM, Degner LF. Patients with cancer and next-of-kin response comparability on physical and psychological symptom well-being. Cancer Nurs. 2002;25:358–374. doi: 10.1097/00002820-200210000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Sneeuw KC, Aaronson NK, Sprangers MA, Detmar SB, Wever LD, Schornagel JH. Comparison of patient and proxy EORTC QLQ-C30 ratings in assessing the quality of life of cancer patients. J Clin Epidemiol. 1998;51:617–631. doi: 10.1016/s0895-4356(98)00040-7. [DOI] [PubMed] [Google Scholar]
- 41.Merz EL, Malcarne VL, Ko CM, Sadler M, Kwack L, Varni JW, Sadler GR. Dyadic concordance among prostate cancer patients and their partners and health-related quality of life: Does it matter? Psychol Health. 2011;26(6):651–666. doi: 10.1080/08870441003721251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carter JH, Lyons KS, Stewart BJ, Archbold PG, Scobee R. Does age make a difference in caregiver strain? Comparison of young versus older caregivers in early-stage Parkinson’s disease. Movement Dis. 2010;25(6):724–730. doi: 10.1002/mds.22888. [DOI] [PubMed] [Google Scholar]