Abstract
Hospitalizations among nursing home residents are frequent, expensive, and often associated with further deterioration of resident condition. The literature indicates that a substantial fraction of admissions is potentially preventable and that nonprofit nursing homes are less likely to hospitalize their residents. However, the correlation between ownership and hospitalization might reflect unobserved resident differences rather than a causal relationship. Using national minimum data set assessments linked with Medicare claims, we use a national cohort of long-stay residents who were newly admitted to nursing homes within an 18-month period spanning January 1, 2004 and June 30, 2005. After instrumenting for ownership status, we found that IV estimates of the effect of nonprofit ownership on hospitalization are at least as large as the non-instrumented effects, indicating that selection bias does not explain the observed relationship. We also found evidence suggesting the lower rate of hospitalizations among nonprofits was due to a different threshold for transfer.
Keywords: Ownership, Nursing homes, Quality, Long-term care, Hospitalization
Introduction
Hospitalization of nursing home residents
Reducing hospitalizations among nursing home residents has remained an important policy objective for several decades due to both the high costs and adverse clinical complications of hospital care in this vulnerable population. Given the frailty of the nursing home population, it is not surprising that hospitalizations are common. Reviews of the literature Castle and Mor (1996) and Grabowski et al. (2008) found high but variable hospitalization rates depending on the population and time period studied. A recent report by the Commonwealth Fund (2012) suggested a hospitalization rate of 20 % per 6 months. In the hospital setting, nursing home residents commonly acquire iatrogenic and nosocomial infections and experience functional and cognitive decline (Ouslander et al. 2000). Frequent hospitalization of frail residents can be emotionally upsetting and raise the likelihood of medical errors from poor care coordination (Mor et al. 2010). In addition to clinical consequences, hospital admissions also have significant financial costs. For example, Grabowski et al. (2007) found that the cost of hospital admissions for New York State nursing home residents totaled $972M in 2004, a 29 % real increase since 1999. Nationally, the rate at which post-acute patients are rehospitalized within 30 days of initial discharge to a skilled nursing facility (SNF) has been rising and the Medicare cost of these rehospitalizations was $4.34B in 2006 (Mor et al. 2010).
Further, a large body of literature shows that many hospitalizations may be avoidable through treatment that could be provided within the nursing home. Using an ambulatory-care sensitive conditions (ACSC) definition of avoidability, Grabowski et al. (2007) deemed 23 % of hospitalizations to be potentially avoidable, while a chart review approach used by Ouslander et al. (2010) rated 67 % of admissions as avoidable. Some of these potentially avoidable admissions represent cases where earlier identification or better treatment of problems in the nursing home setting could have avoided the deterioration in patient condition that necessitated hospitalization. Others represent providers’ discretionary choices about whether to hospitalize in response to a given clinical situation. Even a small proportionate decline in avoidable hospitalizations could yield significant clinical and economic benefits.
Facility ownership and hospitalizations among long-stay residents
The literature examining resident and provider characteristics predicting hospitalization has been reviewed by Grabowski et al. (2008) and previously by Castle and Mor (1996). A consistent finding is lower hospitalization rates among residents of non-profit nursing homes. The more recent review identified twenty estimates of this relationship, of which twelve found a significantly lower hospitalization rate in nonprofit nursing homes, seven found no relationship, and only one found lower hospitalization rate in for-profits. However, this literature has not addressed whether observed differences are causal, and therefore cannot distinguish between three possible reasons for a negative correlation between nonprofit ownership and hospitalization:
Selection bias. Unobserved resident differences account for the observed association, with the residents of nonprofit homes being at lower risk of admission.
Quality of care. By identifying and treating conditions in a way that reduces the clinical need for hospital care, nonprofits improve the clinical trajectory of their residents.
Different hospitalization thresholds. Nonprofits, even with similar residents at admission and similar post-admission health trajectories, hospitalize less because they are more willing and able to treat certain conditions “in house”. This different threshold might be enabled by greater resources or services available in nonprofit facilities.
The first explanation does not imply a causal relationship. The second and third explanations imply causal relationships but different underlying mechanisms. Therefore, establishing the existence and nature of any causal relationship underlying the correlation between ownership and hospitalization is necessary to design appropriate policy and practice responses.
We use national minimum data set (MDS) assessments linked with Medicare claims to create a national cohort of long-stay residents who were newly admitted to nursing homes within an 18-month period spanning January 1, 2004 and June 30, 2005. Because of the concern that unobservables such as patient health will be correlated with the admission to a nonprofit and the quality of care, we instrument for nonprofit status using the differential distance (DD) to nearest nonprofit nursing home relative to the nearest for-profit to examine the effect of ownership on hospitalization.
Background
Approximately two-thirds of nursing homes are for-profit while one-fourth are nonprofit. The remaining nursing homes (6 %) are government-owned. For-profit nursing homes are presumed to set output, quality and inputs to maximize profits. In a competitive market, profit-maximizing behavior would generally be expected to yield desirable outcomes (the delivery of the array and quality of services most valued by consumers given the costs of efficient production). However, if nursing home residents cannot accurately observe quality, the profit motive can result in lower quality than would be chosen by a hypothetical, fully-informed resident. Clearly, certain aspects of quality are more observable than others to patients and their families, even with public report cards and regulatory oversight (Werner et al. 2009a; Zhang and Grabowski 2004). Unobservable dimensions may include workforce quality (Cawley et al. 2006) and process and outcome measures unreported on government report card websites such as locomotion, bladder incontinence, and infections (Werner et al. 2009b).
Unlike their for-profit counterparts, nonprofits cannot distribute profits to individual equity holders. In return, nonprofits are granted several advantages, including exemption from income and property taxes and access to tax-deductible donations and bonds. Given that nonprofit and government providers lack a defined shareholder, these firms may have less incentive to maximize profits and a greater incentive to maximize other objectives such as unobservable aspects of quality and the provision of public goods (Hansmann 1980; Newhouse 1970).
The decision to hospitalize, which we assume is made by the nursing home via a physician order (Freiman and Murtaugh 1993; Ouslander et al. 2011), is a function of resident welfare and preferences, provider preferences, and the financial implications for the provider. A profit-maximizing firm would be expected to weight these factors based on how they affect profits directly or indirectly (e.g., through reputation effects), while a non-profit provider might balance these factors differently. Hospitalization decisions can also be a function of the resources and capabilities of the facility to deal with different clinical situations in-house such as physician involvement, skilled staffing levels (e.g., physician assistant, nurse practitioner, RN), and the availability of ancillary services (e.g., infusion therapy). However, those resources and capabilities may also be chosen endogenously based on how the facility weights the factors noted above in its decisions.
A large literature has considered the role of ownership in health care, with studies in a number of sectors including hospitals (Sloan 2000), health plans (Town et al. 2004), dialysis centers (Brooks et al. 2006), and home health agencies (Grabowski et al. 2009). Nursing home ownership has received particular attention. In a review of 38 studies published between 1990 and 2002, Hillmer et al. (2005) concluded that quality was lower in for-profit nursing homes. Similarly, a meta-analysis of 82 studies published over the period 1962 through 2003 by Comondore et al. (2009) suggested nonprofit nursing homes deliver higher quality care. However, this previous literature is based on cross-sectional comparisons of nonprofit and for-profit nursing homes that fail to account for the possibility that there may be unobservable differences across long-stay residents receiving care at different types of facilities. As Konetzka (2009) wrote in an editorial accompanying the Comondore study, “no review or meta-analysis can overcome the empirical limitations common to all studies reviewed—we still do not know whether not-for-profit status is the reason for higher quality care” (p. 356).
Data and methods
The study uses individual-level data from the MDS for nursing home resident assessment, medicare claims and enrollment records, and the medicaid analytic extract (MAX). At the facility level, the primary data source was the online survey certification and reporting (OSCAR) system. We also included data at the zip-code level. Each of these sources is described briefly.
The MDS resident assessment instrument has nearly 400 data elements, including cognitive function, communication/hearing problems, physical functioning, continence, psychosocial well-being, mood state, activity and recreation, disease diagnoses, health conditions, nutritional status, oral/dental status, skin conditions, special treatments, and medication use. Evaluations of the reliability of the MDS provided at least adequate values on most scales (Mor et al. 2003, 2011; Morris et al. 1990; Phillips et al. 1997).
We merged the medicare standard analytic file [inpatient and skilled nursing facility (SNF) files] and eligibility data from the Medicare enrollment record with MDS data using the Health Insurance Claim (HIC) number of Medicare beneficiaries. Match rates between MDS records of residents 65 and older exceeded 95 %. The Medicare enrollment file contains gender, date of birth, survival status, managed care participation, Part A and B eligibility and “buy in” status. Medicaid eligibility information was merged from the MAX. Zip code level information on per capita income and the percent of elderly individuals living below the federal poverty level from the Census 2000 aggregates was merged to individuals based on prior zip of residence.
The OSCAR database provides information on nursing home characteristics and results from survey inspections, and can be linked to the MDS through the facility provider number with nearly 100 % match rates. Completed on the day of the inspection, data include ownership, structure (e.g. number of beds), staffing (by job category), observed deficiencies, and availability of various services. A profile of the facility’s residents on the day of the inspection is provided which includes census (by payer), functional deficits, nursing care needs, and receipt of “high tech” nursing care.
To construct the DD instrument (described in detail below), we geo-coded all certified nursing homes that currently operate in the U.S. as well as residents’ prior zip code. Using this geo-referenced database, we calculated the distance from a particular nursing home to a particular resident’s prior residence as approximated by the centroid of the zip code area from which the resident was admitted.
National MDS data were used to identify a cohort of residents newly admitted to 13,874 unique nursing homes between January 1, 2004 and June 30, 2005. This “inception” cohort approach allows us to focus on whether individuals select a nonprofit or a for-profit facility contingent upon the geographic proximity of selection options, without having the choice be influenced by relationships built through a prior nursing home stay. New admission status was defined as no prior nursing home admission in the MDS records going back to 1999. Furthermore, given our interest in examining long-stay patient outcomes, our final analytic file was restricted to those who had a cumulative stay of at least 90 days during the 120 day period following the initial admission (n = 278,848). About 60 % of this cohort was initially admitted following an acute hospitalization while the remaining 40 % were admitted from community settings. Hospitalization within 90 and 180 days was then tracked using the MDS assessment occurring nearest to 90 days post-initial admission as the baseline time.
In the prior literature, the effect of nonprofit ownership on hospitalization in the literature has generally been estimated by a reduced form equation including a dummy variable measuring ownership type, coded as 1 for nonprofit ownership and 0 for for-profit ownership. The basic specification is:
| (1) |
where Y refers to hospitalization for person i in nursing home j in state s, NFP is a dummy variable for nonprofit ownership status, X includes an intercept and a set of exogenous controls, ν is a state fixed effect, and ε is the residual. Relatively few facilities are government-owned (6 %) and many of these facilities serve particular populations (e.g., Veterans Affairs beneficiaries) or serve as safety net providers (e.g., many city or county facilities). Therefore, for many prospective residents government facilities may not be close substitutes for private facilities. Our primary analyses exclude government-owned facilities and their residents, but we present a sensitivity analysis that includes these facilities.
The possibility of informative censoring due to death or loss to follow-up exists. Some residents may die in the nursing home without hospitalization within 90 or 180 days. Among all long-stay patients in our study sample, 7.1 % died without a hospitalization within 90 days of baseline and 10.5 % died without a hospitalization within 180 days of baseline. If we ignored this censoring, it could introduce bias into the measurement of the outcomes. To account for this, we estimate multinomial models that account for censoring. Thus, we model three 90 and 180 day outcomes: hospitalization, death, and neither hospitalization nor death. If a person is hospitalized before death, the person is coded as hospitalized.
A set of exogenous variables at the person, facility, zip code and state level were included as controls in this study. At the person level, we control for age, gender, race, education, marital status, Medicaid eligibility, diabetes, congestive heart failure, hip fracture, Alzheimer’s, other dementia, stroke, manic depression, schizophrenia, emphysema/COPD, cancer, shortness of breath, number of medications in prior 7 days, and a cognitive performance scale (CPS). These person-level health measures were obtained from the MDS admission assessment and thus cannot be influenced by the care of the facility directly. At the facility level, we controlled for occupancy rate, number of beds, urban/rural status, hospital-based facility and chain membership. At the zip-code level, we controlled for per capita income and the elderly poverty rate. We also controlled for state fixed effects.
We first estimate Eq. 1 using a multinomial logit model. However, this approach may suffer from bias due to the suspected endogeneity of ownership status and nursing home quality. The error term in Eq. 1 is likely to include unobserved health status that may be correlated with ownership status. If less (more) healthy people tend to choose nonprofits, the OLS coefficient on nonprofit ownership on hospitalization rates will underestimate (overestimate) the true causal relationship. As such, we next estimate an instrumental variables model. Assume that nonprofit status NFP has the following reduced form:
| (2) |
where DD is the DD between the nearest nonprofit and for-profit nursing homes, X is the same set of variables that appeared in the quality equation, ν is a state fixed effect, and μ is the residual.
The differential selection of individuals into nonprofit nursing homes by health status may reflect both demand and supply side factors. For example, if less healthy individuals have a propensity to demand care from nonprofits, this negative selection may relate to the higher value that sicker individuals place on nonprofit status as a signal that the promised level of quality will be delivered (i.e., patients in worse health have more to gain from higher quality nonprofit care). On the supply side, nonprofits may be more willing to admit sicker, more costly patients. Although Medicare SNF payment is case-mix adjusted, the system uses a relatively narrow set of patient conditions in adjusting payments.
If unobserved health is similarly correlated with ownership choice and quality, the error terms ε and μ will be correlated, violating the assumptions underlying the linear regression model. However, we can still generate a consistent estimate of the effect of nonprofit status on quality if we can identify a variable DD that is correlated with nonprofit status but not ε, the error term in the quality equation. Given DD, we can calculate an IV estimate of the effect of nonprofit status on quality.
We assume that DD between the nearest nonprofit and for-profit will predict entry into a nonprofit nursing home. A large health services literature establishes the importance of distance in the choice of provider (e.g., Brooks et al. 2006; Hirth et al. 2003; McClellan et al. 1994) and research also suggests that distance matters in the choice of nursing home (e.g., Shugarman and Brown 2006; Zwanziger et al. 2002). In the studies that most closely mirror the distance-based instrument used in this study, Brooks et al. (2006) found the relative proximity to for-profit and nonprofit dialysis facilities to be the strongest predictor of the type of facility chosen, and that use of this measure as an IV eliminated the relationship between ownership and patient survival that existed in the observational data. Similarly, Grabowski et al. (2013) used DD as an instrument to examine ownership and post-acute SNF quality and found that nonprofits provided higher quality after instrumenting for ownership.
We also expect DD to be uncorrelated with unobserved factors that may influence outcomes. This assumes that individuals choose a place of residence without regard to the proximity of nonprofit and for-profit nursing homes. The relatively low rate of elderly migration supports this assumption (U.S. Census Bureau 2003). Moreover, although Norton and Staiger (1994) found that hospitals chose organization type endogenously with characteristics of the local population, the wide and historical variability of nonprofit prevalence geographically helps support the validity of our instrument in the nursing home context. That is, the relative proportions of nonprofit and for-profit nursing homes have been relatively static within-markets over time (Grabowski and Stevenson 2008). The relative share of nonprofits in different parts of the country is rooted in historical factors such as the age of the city and different patterns of voluntarism and charitable provision that have little to do with the technology and third party payment systems that characterize the current health care environment (Stevens 1989). The conversions across for-profit and nonprofit ownership (roughly 75 in each direction per year) and the limited entry and exit over time do not create major changes in the presence of ownership types in the majority of local markets. As such, we hypothesize that the DD measure is predetermined for potential nursing home residents and unrelated to unobserved quality of care. In the next section, we report a falsification test to validate this assumption.
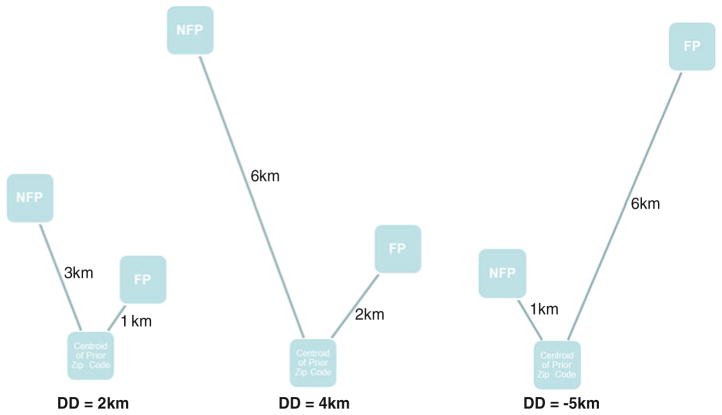
To construct a DD measure for nursing home residents, we calculated the distance using the great circle formula from the centroid of the resident’s zip code prior to nursing home admission, as reported in the Medicare enrollment record, to the exact geo-address of the nearest nonprofit and for-profit facilities based on the latitude and longitude. The differential measure was then calculated as the distance to the nearest nonprofit minus the distance to the nearest for-profit. The resulting measure’s interpretation is how much farther the resident would have to re-locate to be admitted to the nearest nonprofit facility (see Fig. 1 for examples). A negative value indicates that the nearest facility is a nonprofit.
Fig. 1.
Examples of differential distance (DD) calculation between nearest nonprofit (NFP) and for-profit (FP) nursing homes
In the estimation of our IV models, we account for the fact that both our endogenous regressor (ownership status) and our outcomes of interest (90 and 180 day hospitalization, death or neither) are binary or multinomial measures. Recent methodological papers have stressed the potential for bias when standard two-stage least squares IV methods are employed (e.g., Bhattacharya et al. 2006; Terza et al. 2008). Even in cases such as ours with a large sample, this bias is not attenuated. Assuming a valid instrument, the two-stage residual inclusion (2SRI) method has been shown to provide unbiased estimates (Terza et al. 2008). In 2SRI, the endogenous variables are not replaced by first-stage predictors but rather the first-stage residuals are included as an additional regressor in the second stage. In our application, we estimate the first stage using least squares and the second stage using a multinomial logit. In the results section, we present marginal effects at the mean for the key outcomes. The full multinomial results are available upon request. Bhattacharya et al. (2006) use simulations to show that a bivariate probit model may perform better than some IV models in the non-linear context. Therefore, as a sensitivity analysis we estimated the model using bivariate probit, finding very similar results to the 2SRI approach. Full results are also available upon request.
In grouped data such as ours, a concern involves the likely presence of heteroskedasticity. When the true specification of the residual variance-covariance matrix follows such a structure, Moulton (1990) has shown that estimates of the standard errors will be biased downwards. A straightforward and unrestrictive approach to addressing this issue is to adjust the standard errors using the Huber–White robust estimator clustered at the zip-code level.
Tables 1 and 2 summarize the variables used in our analysis. Roughly 29 % of the long-stayers reside in nonprofit facilities. The average age is 82.4 years, roughly two-thirds are female, 84 % are white, 26 % are married, and 53 % are Medicaid-eligible. In terms of outcomes, 17.9 % of the sample is hospitalized within 90 days and 7.2 % dies (without hospitalization); 27.8 % of the sample is hospitalized within 180 days and 10.5 % dies. The average DD was 5.92 km (3.68 miles), suggesting the typical resident had to travel 5.92 additional kilometers to the nearest nonprofit facility relative to the nearest for-profit.
Table 1.
Descriptive statistics: long-stay residents (N = 278,848)
| Variable | Mean | Std. Dev. |
|---|---|---|
| Nonprofit | 0.285 | 0.451 |
| Differential distance in km (nearest NFP minus nearest FP) | 5.916 | 16.939 |
| Age at initial admission (cohort qualification) | 82.439 | 7.696 |
| Patient gender (per MDS) | 0.683 | 0.465 |
| White | 0.844 | 0.363 |
| High school graduate | 0.403 | 0.490 |
| More than high school | 0.230 | 0.421 |
| Missing education | 0.013 | 0.115 |
| Married | 0.264 | 0.441 |
| Per capita income in origin zip code | 20846.780 | 8386.667 |
| Poverty rate in origin zip code | 10.693 | 7.094 |
| Occupancy rate | 0.876 | 0.113 |
| Total number of beds | 136.688 | 75.358 |
| Urban facility | 0.757 | 0.429 |
| Hospital-based facility | 0.025 | 0.156 |
| Chain-owned facility | 0.608 | 0.488 |
| Days between admission and initial MDS assessment | 11.362 | 3.050 |
| Diabetes mellitus | 0.267 | 0.442 |
| Congestive heart failure | 0.171 | 0.376 |
| Hip fracture | 0.078 | 0.269 |
| Alzheimer’s disease | 0.063 | 0.243 |
| Aphasia | 0.037 | 0.189 |
| Cerebrovascular accident(stroke) | 0.192 | 0.394 |
| Dementia other than Alzheimer’s | 0.113 | 0.317 |
| Multiple sclerosis | 0.002 | 0.049 |
| Manic depression (bipolar disease) | 0.013 | 0.112 |
| Schizophrenia | 0.012 | 0.108 |
| RUGs 5.12 nursing CMI based on FR 2004 proposed repayment rule | 0.871 | 0.256 |
| Days between admission and baseline assessments | 81.181 | 14.246 |
| Emphysema/COPD | 0.131 | 0.338 |
| Cancer | 0.029 | 0.167 |
| Shortness of breath | 0.084 | 0.277 |
| Number of medications in last 7 days | 9.670 | 4.322 |
| Morris additive ADL scale 0–28 | 13.968 | 7.801 |
| Max level pressure ulcer seen | 0.416 | 1.011 |
| CPS scale, Fries/Morris 92 | 2.441 | 1.580 |
| Comorbidity index, CHESS(0 to 5) 0 = not at all unstable, 5 = highly | 1.512 | 1.123 |
| Medicaid-eligible per MAX at baseline | 0.526 | 0.499 |
Table 2.
Summary of long-stay outcomes (N = 278,848)
| Mean | Std. dev. | |
|---|---|---|
| Neither hospitalized, nor died in 90 days | 74.93 | 0.433 |
| Hospitalized (before death) in 90 days | 17.9 | 0.383 |
| Died in 90 days | 7.17 | 0.258 |
| Neither hospitalized, nor died in 180 days | 61.64 | 0.486 |
| Hospitalized (before death) in 180 days | 27.82 | 0.448 |
| Died in 180 days | 10.54 | 0.307 |
| ADL decline 4+ points | ||
| Positive | 11.65 | 0.321 |
| Negative | 67.61 | 0.468 |
| Missing | 12.88 | 0.335 |
| Dead | 7.86 | 0.269 |
| Pressure ulcer worsen | ||
| Positive | 5.76 | 0.233 |
| Negative | 73.38 | 0.442 |
| Missing | 12.09 | 0.326 |
| Dead | 8.77 | 0.283 |
To differentiate between the three alternative reasons for a negative correlation between nonprofit ownership and hospitalization rate in the observational data, two versions of the ordinary multinomial logit and 2SRI models are estimated. First, to distinguish between selection bias (reason 1) and a causal relationships (reasons 2 and 3), the multinomial models are estimated for three outcomes (any hospitalization, death without hospitalization, and neither death nor hospitalization). If a negative relationship seen in the ordinary logit is driven by selection of healthier residents into nonprofits, the magnitude of the effect should be smaller in the 2SRI results. Conversely, if less healthy residents tend to select nonprofits, the negative relationship should become even stronger in the 2SRI results.
Second, to distinguish between the two possible causal mechanisms behind the negative relationship, we expand the multinomial models by dividing the hospitalization outcome into two separate outcomes reflecting whether the initial hospital transfer in the period was deemed a potentially preventable or non-preventable hospitalization. To define preventable hospitalizations, we used the Agency for Healthcare Research and Quality’s Prevention Quality Indicators (PQIs), which measure quality of care for “ambulatory care sensitive conditions” (ACSCs). ACSCs are conditions for which hospitalizations can potentially be prevented by good outpatient care or by early intervention which prevents complications or the development of more severe disease (http://www.qualityindicators.ahrq.gov/modules/pqi_overview.aspx). If the driving force behind a causal relationship is improved quality of care leading to a better clinical trajectory (reason 2), we would expect to see a disproportionate reduction in preventable hospitalizations. Conversely, a reduction that does not occur disproportionately among preventable hospitalizations would favor a different hospitalization threshold (reason 3) as the causal mechanism because a different threshold for managing conditions in house could occur in either ACSC or non-ACSC hospitalizations.
Effect of differential distance: specification tests
Problems with weak instruments are well-known (Staiger and Stock 1997; Stock and Yogo 2005) and Bound et al. (1995) have argued that the use of instruments that jointly explain little variation in the endogenous regressors can do more harm than good. The DD instrument meets the standard of Staiger and Stock, with the F-statistics far exceeding the threshold of 10. The first-stage estimates suggest that a one kilometer increase in the DD between the nearest nonprofit and for-profit led to a 0.5 % point decrease in the likelihood of choosing a nonprofit with a t statistic of 33.2 (Table 3) and an F statistic of 233.32.
Table 3.
First-stage results, regression of nonprofit ownership on differential distance
| Full sample | Those who travelled more than 100 km from origin zip code | |
|---|---|---|
| Differential distance (NFP–FP) | −.0050691 (−33.17) | −.0002435 (−1.18) |
| R2 | 0.2171 | 0.2264 |
| Observations | 278,848 | 4,999 |
Regression includes all the covariates reported in Table 1 and state fixed effects
Robust t statistics clustered at the zip code level are reported in parentheses
In addition to the assumption regarding the instruments being strongly associated with the endogenous variable, IV also assumes the instrument must not be correlated with the second stage error term. If it is still correlated, then the instrumented variable will still be endogenous. Although it is impossible to confirm the null hypothesis that the instrument is uncorrelated with the error term in the quality equation, a standard practice is to report whether the instrument is correlated with those observed factors that affect the second-stage error term. Thus, we divide the variables used within this study by those observations that are above or below the median in DD (Table 4). As expected, nonprofit status is 24.5 % points higher for those patients with distances below the median. The other patient-level measures are very similar across the two groups, suggesting the samples are balanced, mitigating concerns that large unobserved differences exist between populations located relatively close to facilities of different ownership types.
Table 4.
Person-level characteristics by differential distance (DD) between nearest nonprofit and nearest for-profit (N = 278,848)
| Variable | DD<Median | DD>Median |
|---|---|---|
| Nonprofit | 0.407 | 0.162 |
| Age at initial admission (cohort qualification) | 82.624 | 82.254 |
| Patient gender (per MDS) | 0.684 | 0.683 |
| White | 0.844 | 0.844 |
| High school graduate | 0.408 | 0.397 |
| More than high school | 0.238 | 0.221 |
| Missing education | 0.014 | 0.013 |
| Married | 0.260 | 0.267 |
| Per capita income in origin zip code | 21440.180 | 20250.430 |
| Poverty rate in origin zip code | 10.434 | 10.953 |
| Occupancy rate | 0.885 | 0.866 |
| Total number of beds | 144.322 | 129.017 |
| Urban facility | 0.791 | 0.722 |
| Hospital-based facility | 0.035 | 0.015 |
| Chain-owned facility | 0.566 | 0.651 |
| Days between admission and initial MDS assessment | 11.222 | 11.503 |
| Diabetes mellitus | 0.264 | 0.271 |
| Congestive heart failure | 0.164 | 0.177 |
| Hip Fracture | 0.077 | 0.080 |
| Alzheimer’s | 0.058 | 0.068 |
| Aphasia | 0.038 | 0.036 |
| Cerebrovascular accident(stroke) | 0.188 | 0.197 |
| Dementia other than Alzheimer’s | 0.108 | 0.118 |
| Multiple sclerosis | 0.003 | 0.002 |
| Manic depression (bipolar disease) | 0.013 | 0.013 |
| Schizophrenia | 0.012 | 0.012 |
| RUGs 5.12 nursing CMI based on FR 2004 proposed repayment rule | 0.866 | 0.875 |
| Days between admission and baseline assessments | 81.099 | 81.265 |
| Emphysema/COPD | 0.125 | 0.138 |
| Cancer | 0.028 | 0.029 |
| Shortness of breath | 0.080 | 0.087 |
| Number of meds in last 7 days | 9.626 | 9.714 |
| Morris additive ADL scale 0–28 | 13.978 | 13.958 |
| Max level pressure ulcer seen | 0.418 | 0.414 |
| CPS scale, Fries/Morris 92 | 2.430 | 2.452 |
| Comorbidity index, CHESS(0 to 5) 0 = not at all unstable, 5 = highly | 1.516 | 1.507 |
| Medicaid-eligible per MAX at baseline | 0.509 | 0.544 |
As a final specification check, we conducted a falsification test of our instrument, which we draw from the identification strategy of a recent study. Doyle (2011) used people treated in Florida who did not reside there (“vacationers”) as a means of addressing selection of individuals into high and low cost areas in studying the relationship between spending and health care outcomes. We adapt this idea by examining individuals who enter a nursing home far from their primary residence. The concentration of non-profit nursing homes around their primary residence should not affect entry into a NFP for those individuals who enter a nursing home near a family member living elsewhere or while on vacation or at a secondary residence. For this “vacationer” sub-sample, the first stage should be small and insignificant. If it is negative and significant, it suggests that where individuals live relative to the nearest NFP and FP is correlated with unmeasured quality. We define this vacationer sub-sample as individuals entering a nursing home over 100 km (N = 4,999 or 1.92 % of full sample) away from their primary residence. The results suggest a weak first-stage estimate of the DD instrument for the vacationer sub-samples (column 2 in Table 3). The first-stage estimate is roughly 4 % as large as the result from the full sample. Thus, this falsification check does not support the idea that an individual’s place of residence relative to the nearest NFP and FP is correlated with other (unmeasured) factors that predict quality of care.
Results
The estimates of the effect of profit status on any hospitalization are presented in Table 5, including both the standard model that treats profit status as exogenous, and the IV model that treats profit status as endogenous (N = 278,848). Results are presented as marginal effects at the mean. In the multinomial logit model, residents in nonprofit facilities are 1.9 % points less likely to be hospitalized within 90 days and 3.0 % points less likely to be hospitalized within 180 days. Thus, when we fail to account for the endogeneity of ownership status, our results replicate most of those in the literature by suggesting that residents in nonprofits are less likely to be hospitalized.
When we account for endogenous ownership in the IV models, the relationship remains negative and becomes larger. Residents in nonprofit facilities are 3.09 % points less likely to be hospitalized within 90 days and 4.85 % points less likely to be hospitalized within 180 days. This indicates that the observed relationship between nonprofit ownership and lower hospitalization rates is not driven by selection of healthier patients into nonprofits. Rather, it suggests that less healthy patients may be selecting nonprofits causing the relationship in the non-IV models to actually underestimate the true causal relationship. To test whether the IV results differed significantly from the ordinary results, we conducted Durbin–Wu–Hausman tests based on linear probability versions of the models. These tests suggest that the IV results were not significantly different (p = .260 for 90 day hospitalization; p = .119 for 180 day hospitalization). Nonetheless, the fact that the IV results are even more negative than the results from the models that assume ownership is exogenous support the existence of a causal relationship.
The second set of models splits hospitalizations based on whether they were considered preventable under the AHRQ criteria. Just under one fourth of all 90 and 180 day hospitalizations were considered preventable. For both the 90 and 180 day outcomes, the models treating ownership as exogenous showed significantly fewer hospitalizations, both preventable and non-preventable, among nonprofits, but the marginal effects were larger for those hospitalizations not classified as preventable. The IV models accentuated these differences with the marginal effects for preventable hospitalizations becoming insignificant and close to zero. This suggests that the quality of care explanation (reason 2) for the negative correlation between nonprofit ownership and hospitalization is not driving the relationship. Under that explanation, we would have expected a disproportionate decline in preventable hospitalizations. Thus, different thresholds for hospitalizing (vs. managing the resident’s condition in-house) (reason 3) appears to be the more likely explanation. However, it is not clear why the impact would be disproportionate on non-preventable hospitalizations and more detailed analyses of the conditions leading to hospitalization would be warranted. To corroborate this finding, we performed a descriptive analyses of OSCAR data from 2000–2010 (results available upon request). Controlling for patient acuity, Medicaid share, staffing measures, for-profits have more total and preventable hospitalizations, and consistent our main analyses, the difference is larger for total hospitalizations than for preventable hospitalizations (Table 6).
Table 6.
Long-stay regression results for potentially preventable and unpreventable hospitalizations: marginal effects of being treated in a nonprofit home instead of a for-profit home
| Outcome | 90 Day hospitalization
|
180 Day hospitalization
|
||||
|---|---|---|---|---|---|---|
| Distribution of outcomes | Marginal effects without instrument | Marginal effects with instrument | Distribution of outcomes | Marginal effects without instrument | Marginal effects with instrument | |
| Nothing | 75.23 | 0.0194*** (9.866) | 0.0351*** (3.463) | 61.64 | 0.0297*** (12.45) | 0.0493*** (4.007) |
| Unpreventable hospitalization | 13.54 | −0.0133*** (−8.069) | −0.0313*** (−3.818) | 21.93 | −0.0214*** (−10.40) | −0.0491*** (−4.631) |
| Death | 7.10 | −0.000358 (−0.428) | −0.00450 (−1.054) | 10.54 | −0.000140 (−0.120) | −0.00136 (−0.213) |
| Preventable hospitalization (Ambulatory Care Sensitive) | 4.12 | −0.00576*** (−6.837) | 0.000735 (0.143) | 5.89 | −0.00811*** (−7.539) | 0.00114 (0.176) |
| Observations | 278,848 | 278,848 | 278,848 | 278,848 | ||
To examine the robustness of our primary model specification, we ran a series of alternate models (Table 7). As a first check, we found that the results are robust to the exclusion discharges to hospital-based nursing homes. The concern is that hospital-based nursing homes might selectively attract patients from the hospital to which they are affiliated (David et al. 2011; Stearns et al. 2006).
Table 7.
Specification checks (N = 278,848 unless otherwise noted)
| Hospitalized within 90 days | Hospitalized within 180 days | |
|---|---|---|
| Base line model | −0.0309*** (−3.269) | −0.0485*** (−4.107) |
| Excluded hospital based nursing homes (N = 271,904) | −0.0272*** (−2.871) | −0.0439*** (−3.717) |
| Urban NHs only (N = 210,981) | −0.0464*** (−3.182) | −0.0723*** (−3.866) |
| Rural NHs only (N = 67,867) | −0.0183 (−1.564) | −0.0319** (−2.160) |
| Include health referral region fixed effects | −0.0278*** (−2.759) | −0.0443*** (−3.492) |
| Include government facilities (N = 296,249) | −0.0290*** (−2.989) | −0.0439*** (−3.604) |
| Binary DD measure (above/below) median | −0.0285*** (−3.117) | −0.0508*** (−4.375) |
| Logged values of DD measure | −0.0371*** (−4.764) | −0.0605*** (−6.181) |
| Exclude NHs in same zip code as resident prior address (N = 196,309) | −0.0543*** (−2.922) | −0.0690*** (−2.828) |
| Supply of NH beds included in the model (N = 267,934) | −0.0340*** (−3.282) | −0.0542*** (−4.154) |
Results are presented as marginal effects. Full multinomial results available upon request. Models include all the covariates reported in Table 1 and state fixed effects unless otherwise noted. Robust t-statistics clustered at the zip code-level are reported in parentheses. DD Differential distance, NH nursing home
Another concern is that the exclusion of discharges to government nursing homes may have biased the results. When we added discharges to government facilities and included a corresponding instrument for DD to a government provider relative to the next nearest facility, the nonprofit findings were sustained as well.
Another potential issue is that the effects we observed might be concentrated in certain markets. When we estimated our models conditional on urban and rural markets, the findings were stronger in urban markets but the sign remained negative in rural markets (and significant for the 180 day measure despite the substantially smaller sample). The primary models include state fixed effects. However, one concern is that unobserved factors at the market level may be correlated with both ownership and quality of care. For example, more concentrated nursing home markets might have less access to nonprofit nursing homes and lower quality of care due to reduced competition. To address this concern, we substituted hospital referral region (HRR) fixed effects for state fixed effects in our model. With HRR fixed effects, both the 90 and 180 day results are very similar to those in the baseline model. We also ran a check in which we included a measure of the local supply of nursing home beds, which did not alter our primary conclusions.
We also experimented with different forms of the DD instrument including a binary measure (above/below median) and logged values (log of distance to nearest nonprofit minus log distance to nearest for-profit) to account for skewed values. The results were again quite robust.
Finally, because we approximated the resident’s prior residence by the centroid of the zip code area from which the resident was admitted, the DD instrument will have the greatest measurement error when a nursing home is located in that same zip code. When we exclude those cases in which a nursing home was located in their zip code of prior residence, the results have the same sign and significance but larger effect magnitudes than our baseline estimates.
In summary, the specification checks suggest the hospitalization results are very robust.
Conclusion
A large literature has documented a relationship between nursing home ownership status and hospitalization, a measure with significant clinical and cost implications. These studies treat ownership as exogenous, although there are reasons to suspect that firms jointly choose their ownership form and quality of care (Sloan 2000). We lay out three possible reasons for the correlation between nonprofit ownership and lower hospitalization rates and are able to reject selection bias as the root of correlation. Our results show that—after instrumenting for endogenous ownership—the negative correlation is at least as strong in the instrumented models. Although we do not formally reject the validity of the non-instrumented results, it appears that any bias that exists is downward (i.e., nonprofits receive an unfavorable selection of residents in terms of likelihood of needing hospitalization). Therefore, we conclude that the observed relationship likely reflects an underlying causal relationship.
To begin assessing the nature of this causal relationship, we differentiated between potentially preventable and non-preventable hospitalizations. Because the decline in hospitalization is not concentrated among those transfers deemed “preventable” through better ambulatory care, the pattern of results is more consistent with nonprofits having a greater willingness or ability to manage certain cases in-house rather than with nonprofits delivering care that results in a better clinical trajectory per se. It is somewhat puzzling that the lower hospitalization rate observed for nonprofits is actually larger for hospitalizations not deemed preventable particularly because the more prevalent use of RNs by non-profit facilities should serve to both reduce the threshold for hospitalization and to identify early signs of patient illness that would stimulate early medical intervention. However, no necessary reason exists for why hospitalization differences driven by varying admission thresholds (as opposed to varying quality of ambulatory care) could not be larger for “unpreventable” indications. Further, defining which admissions are preventable is an inherently imprecise exercise, as indicated by the extreme sensitivity to methodology. For example, 23 % of admissions were classified as potentially preventable using an ACSC approach (Grabowski et al. 2007) versus 67 % using a chart review approach (Ouslander et al. 2010). This highlights the fact that the empirical validity of these expert-opinion designations of preventability has not been conclusively demonstrated in the nursing home context. Most research on nursing home hospitalizations has not differentiated between preventable and non-preventable causes, and constructs such as ambulatory-care sensitive conditions have been developed primarily in the community setting.
Several other pieces of evidence are consistent with the idea that there exists discretion in the hospitalization “threshold”. First, descriptive analyses of the OSCAR data from 2000–2010 show that nonprofits provide more direct care staff hours per resident day (4.03 vs. 3.22), have a higher skill mix (37.6 % of nursing hours are RNs vs. 27.9 %) and are likely to have more financial resources via a more favorable payer mix (51.8 % Medicaid vs. 65.4 %). It would be useful to examine other measures of resources (e.g., availability of therapeutic services and on-site diagnostic testing) that would indicate greater capacity to substitute services in the nursing home for those delivered in an inpatient setting. Second, the responsiveness of hospitalization to resources and incentives also is suggestive of discretionary threshold. Earlier research suggests higher hospitalization and re-hospitalization rates in states with more generous “bed-hold” policies (under which nursing homes receive payments when a resident is hospitalized to ensure that the bed is still available once the resident is discharged) (Grabowski et al. 2010; Gruneir et al. 2007; Intrator et al. 2007; Unruh et al. 2013), and higher hospitalization rates in states with lower Medicaid nursing home payment rates (Intrator et al. 2007)
In conclusion, hospitalizations among nursing home residents are clinically and economically significant, and our research indicates that the correlation between ownership and hospitalization found in the prior literature does not appear to arise from the selection of favorable residents into nonprofits. Further, the data suggest that nonprofit nursing homes may have a lower propensity to transfer residents to a hospital.
Table 5.
Long-stay regression results: marginal effects of being treated in a nonprofit home instead of a for-profit home (N = 278,848)
| Outcome | Least squares | 2SRI |
|---|---|---|
| Hospitalized within 90 days | −0.019*** (−10.46) | −0.0309*** (−3.269) |
| Hospitalized within 180 days | −0.030*** (−13.13) | −0.0485*** (−4.107) |
Results are presented as marginal effects. Full multinomial results available upon request. Models include all the covariates reported in Table 1 and state fixed effects. Robust t statistics clustered at the zip code-level are reported in parentheses
Contributor Information
Richard A. Hirth, Email: rhirth@umich.edu, University of Michigan School of Public Health, 1415 Washington Heights, Ann Arbor, MI 48109-2029, USA
David C. Grabowski, Harvard University, Cambridge, MA, USA
Zhanlian Feng, Research Triangle Institute, Research Triangle Park, NC, USA. Brown University, Providence, RI, USA.
Momotazur Rahman, Brown University, Providence, RI, USA.
Vincent Mor, Brown University, Providence, RI, USA.
References
- Bhattacharya J, Goldman D, McCaffrey D. Estimating probit models with self-selected treatments. Statistics in Medicine. 2006;25:389–413. doi: 10.1002/sim.2226. [DOI] [PubMed] [Google Scholar]
- Bound J, Jaeger DA, Baker RM. Problems with instrumental variables estimation when the correlation between the instruments and the endogenous explanatory variable is weak. Journal of the American Statistical Association. 1995;90:443–450. [Google Scholar]
- Brooks JM, Irwin CP, Hunsicker LG, Flanigan MJ, Chrischilles EA, Pendergast JF. Effect of dialysis center profit-status on patient survival: A comparison of risk-adjustment and instrumental variable approaches. Health Services Research. 2006;41:2267–2289. doi: 10.1111/j.1475-6773.2006.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle NG, Mor V. Hospitalization of nursing home residents: A review of the literature, 1980–1995. Medical Care Research and Review. 1996;53:123–148. doi: 10.1177/107755879605300201. [DOI] [PubMed] [Google Scholar]
- Cawley J, Grabowski DC, Hirth RA. Factor substitution in nursing homes. Journal of Health Economics. 2006;25:234–247. doi: 10.1016/j.jhealeco.2005.06.004. [DOI] [PubMed] [Google Scholar]
- Comondore VR, Devereaux PJ, Zhou Q, Stone SB, Busse JW, Ravindran NC, et al. Quality of care in for-profit and not-for-profit nursing homes: Systematic review and meta-analysis. BMJ British Medical Journal. 2009;339:b2732. doi: 10.1136/bmj.b2732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David G, Rawley D, Polsky D. Integration and task allocation: Evidence from patient care. Cambridge: National Bureau of Economic Research; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle JJ. Returns to local-area healthcare spending: Evidence from health shocks to patients far from home. American Economic Journal Applied Economics. 2011;3:221–243. doi: 10.1257/app.3.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freiman MP, Murtaugh CM. The determinants of the hospitalization of nursing home residents. Journal of Health Economics. 1993;12:349–359. doi: 10.1016/0167-6296(93)90017-9. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Feng Z, Hirth R, Rahman M, Mor V. Effect of nursing home ownership on the quality of post-acute care: An instrumental variables approach. Journal of Health Economics. 2013;32:12–21. doi: 10.1016/j.jhealeco.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, Feng Z, Intrator O, Mor V. Medicaid bed-hold policy and Medicare skilled nursing facility rehospitalizations. Health Services Research. 2010;45:1963–1980. doi: 10.1111/j.1475-6773.2010.01104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, Huskamp HA, Stevenson DG, Keating NL. Ownership status and home health care performance. Journal of Aging and Social Policy. 2009;21:130–143. doi: 10.1080/08959420902728751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, O’Malley AJ, Barhydt NR. The costs and potential savings associated with nursing home hospitalizations. Health Affairs. 2007;26:1753–1761. doi: 10.1377/hlthaff.26.6.1753. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Stevenson DG. Ownership conversions and nursing home performance. Health Services Research. 2008;43:1184–1203. doi: 10.1111/j.1475-6773.2008.00841.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of nursing home hospitalization: A review of the literature. Medical Care Research and Review. 2008;65:3–39. doi: 10.1177/1077558707308754. [DOI] [PubMed] [Google Scholar]
- Gruneir A, Miller SC, Intrator O, Mor V. Hospitalization of nursing home residents with cognitive impairments: The influence of organizational features and state policies. The Gerontologist. 2007;47:447–456. doi: 10.1093/geront/47.4.447. [DOI] [PubMed] [Google Scholar]
- Hansmann HB. The role of nonprofit enterprise. The Yale Law Journal. 1980;89:835–901. [Google Scholar]
- Hillmer MP, Wodchis WP, Gill SS, Anderson GM, Rochon PA. Nursing home profit status and quality of care: Is there any evidence of an association? Medical Care Research and Review. 2005;62:139–166. doi: 10.1177/1077558704273769. [DOI] [PubMed] [Google Scholar]
- Hirth RA, Chernew ME, Turenne MN, Pauly MV, Orzol SM, Held PJ. Chronic illness, treatment choice and workforce participation. International Journal of Health Care Finance and Economics. 2003;3:167–181. doi: 10.1023/a:1025332802736. [DOI] [PubMed] [Google Scholar]
- Intrator O, Grabowski DC, Zinn J, Schleinitz M, Feng Z, Miller S, et al. Hospitalization of nursing home residents: The effects of states’ Medicaid payment and bed-hold policies. Health Services Research. 2007;42:1651–1671. doi: 10.1111/j.1475-6773.2006.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konetzka RT. Do not-for-profit nursing homes provide better quality? BMJ British Medical Journal. 2009;339:b2683. doi: 10.1136/bmj.b2683. [DOI] [PubMed] [Google Scholar]
- McClellan M, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. JAMA. 1994;272:859–866. [PubMed] [Google Scholar]
- Mor V, Angelelli J, Jones R, Roy J, Moore T, Morris J. Inter-rater reliability of nursing home quality indicators in the US. BMC Health Services Research. 2003;3:20. doi: 10.1186/1472-6963-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Affairs (Millwood) 2010;29:57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Intrator O, Unruh MA, Cai S. Temporal and Geographic variation in the validity and internal consistency of the Nursing Home Resident Assessment Minimum Data Set 2.0. BMC Health Services Research. 2011;11:78. doi: 10.1186/1472-6963-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JN, Hawes C, Fries BE, Phillips CD, Mor V, Katz S, et al. Designing the national resident assessment instrument for nursing homes. Gerontologist. 1990;30:293–307. doi: 10.1093/geront/30.3.293. [DOI] [PubMed] [Google Scholar]
- Moulton BR. An illustration of a pitfall in estimating the effects of aggregate variables on micro units. The Review of Economics and Statistics. 1990;72:334–338. [Google Scholar]
- Newhouse JP. Toward a theory of nonprofit institutions: An economic model of a hospital. American Economic Review. 1970;60:64–74. [Google Scholar]
- Norton EC, Staiger DO. How hospital ownership affects access to care of the uninsured. Rand Journal of Economics. 1994;25:171–185. [PubMed] [Google Scholar]
- Ouslander JG, Lamb G, Perloe M, Givens JH, Kluge L, Rutland T, et al. Potentially avoidable hospitalizations of nursing home residents: Frequency, causes, and costs: [see editorial comments by Drs. Jean F. Wyman and William R. Hazzard, pp 760–761] Journal of the American Geriatrics Society. 2010;58:627–635. doi: 10.1111/j.1532-5415.2010.02768.x. [DOI] [PubMed] [Google Scholar]
- Ouslander JG, Lamb G, Tappen R, Herndon L, Diaz S, Roos BA, et al. Interventions to reduce hospitalizations from nursing homes: Evaluation of the INTERACT II collaborative quality improvement project. Journal of the American Geriatrics Society. 2011;59:745–753. doi: 10.1111/j.1532-5415.2011.03333.x. [DOI] [PubMed] [Google Scholar]
- Ouslander JG, Weinberg AD, Phillips V. Inappropriate hospitalization of nursing facility residents: A symptom of a sick system of care for frail older people. Journal of the American Geriatrics Society. 2000;48:230–231. doi: 10.1111/j.1532-5415.2000.tb03919.x. [DOI] [PubMed] [Google Scholar]
- Phillips CD, Morris JN, Hawes C, Fries BE, Mor V, Nennstiel M, et al. Association of the resident assessment instrument (RAI) with changes in function, cognition, and psychosocial status. Journal of the American Geriatrics Society. 1997;45:986–993. doi: 10.1111/j.1532-5415.1997.tb02971.x. [DOI] [PubMed] [Google Scholar]
- Shugarman LR, Brown JA. Nursing home selection: How do consumers choose? volume I: Findings from focus groups of consumers and information intermediaries (Prepared for office of disability, aging and long-term care policy, office of the assistant secretary for planning and evaluation) U.S. Department of Health and Human Services; Washington, DC: 2006. Contract #HHS-100-03-0023. [Google Scholar]
- Sloan FA. Not-for-profit ownership and hospital behavior. Amsterdam: Elsevier Science; 2000. [Google Scholar]
- Staiger D, Stock JH. Instrumental variables regression with weak instruments. Econometrica. 1997;65:557–586. [Google Scholar]
- Stearns SC, Dalton K, Holmes GM, Seagrave SM. Using propensity stratification to compare patient outcomes in hospital-based versus freestanding skilled-nursing facilities. Medical Care Research and Review. 2006;63:599–622. doi: 10.1177/1077558706290944. [DOI] [PubMed] [Google Scholar]
- Stevens R. Sickness and in wealth. New York: Basic Books; 1989. [Google Scholar]
- Stock JH, Yogo M. Testing for weak instruments in linear IV regression. Cambridge: Cambridge University Press; 2005. [Google Scholar]
- Terza JV, Basu A, Rathouz PJ. Two-stage residual inclusion estimation: Addressing endogeneity in health econometric modeling. Journal of Health Economics. 2008;27:531–543. doi: 10.1016/j.jhealeco.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terza JV, Bradford WD, Dismuke CE. The use of linear instrumental variables methods in health services research and health economics: A cautionary note. Health Services Research. 2008;43:1102–1120. doi: 10.1111/j.1475-6773.2007.00807.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Town R, Feldman R, Wholey D. The impact of ownership conversions on HMO performance. International Journal of Health Care Finance and Economics. 2004;4:327–342. doi: 10.1023/B:IHFE.0000043761.95636.96. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Internal migration of the older population: 1995–2000. U.S. Department of Commerce; 2003. [Google Scholar]
- Unruh MA, Grabowski DC, Trivedi AN, Mor V. Medicaid bed-hold policies and hospitalization of long-stay nursing home residents. Health Services Research. 2013;48:1617–1633. doi: 10.1111/1475-6773.12054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner RM, Konetzka RT, Kruse GB. Impact of public reporting on unreported quality of care. Health Services Research. 2009;44:379–398. doi: 10.1111/j.1475-6773.2008.00915.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner RM, Konetzka RT, Stuart EA, Norton EC, Polsky D, Park J. Impact of public reporting on quality of postacute care. Health Services Research. 2009;44:1169–1187. doi: 10.1111/j.1475-6773.2009.00967.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Grabowski DC. Nursing home staffing and quality under the nursing home reform act. Gerontologist. 2004;44:13–23. doi: 10.1093/geront/44.1.13. [DOI] [PubMed] [Google Scholar]
- Zwanziger J, Mukamel DB, Indridason I. Use of resident-origin data to define nursing home market boundaries. Inquiry. 2002;39:56–66. doi: 10.5034/inquiryjrnl_39.1.56. [DOI] [PubMed] [Google Scholar]