Abstract
Background
Previous literature indicates that biases exist in pain ratings. Healthcare professionals have been found to use patient demographic cues such as sex, race, and age when making decisions about pain treatment. However, there has been little research comparing healthcare professionals’ (i.e., physicians and nurses) pain decision policies based on patient demographic cues.
Methods
The current study used virtual human technology to examine the impact of patients’ sex, race, and age on healthcare professionals’ pain ratings. One hundred and ninety-three healthcare professionals (nurses and physicians) participated in this online study.
Results
Healthcare professionals assessed virtual human patients who were male and African American to be experiencing greater pain intensity and were more willing to administer opioid analgesics to them than to their demographic counterparts. Similarly, nurses were more willing to administer opioids make treatment decisions than physicians. There was also a significant virtual human-sex by healthcare professional interaction for pain assessment and treatment decisions. The sex difference (male > female) was greater for nurses than physicians.
Conclusions
Results replicated findings of previous studies using virtual human patients to assess the effect of sex, race, and age in pain decision-making. In addition, healthcare professionals” pain ratings differed depending on healthcare profession. Nurses were more likely to rate pain higher and be more willing to administer opioid analgesics than were physicians. Healthcare professionals rated male and African American virtual human patients as having higher pain in most pain assessment and treatment domains compared to their demographic counterparts. Similarly the virtual human-sex difference ratings were more pronounced for nurses than physicians. Given the large number of patients seen throughout the healthcare professionals’ careers, these pain practice biases have important public health implications. This study suggests attention to the influence of patient demographic cues in pain management education is needed.
Keywords: Healthcare Professionals, Pain Assessment, Pain Treatment, Virtual Technology
Introduction
Previous literature indicates the presence of sex, race, and age biases in both medical and non-medical settings (Anderson et al., 2000). Research has found that there are pain assessment and treatment disparities depending on the patient’s sex, race, and age (Alqudah, et al, 2010; Anderson et al., 2000; Breuer, 2010; Hirsh et al., 2009a; Hirsh et al., 2011). Women and minorities are less likely to receive opioid analgesics than their demographic counterparts, post-surgery, while in emergency rooms, and for cancer pain (Calderone, 1990; Chen & et al., 2008; Cleeland et al., 1994; Faherty & Grier, 1984). Although pain is common in older adults, it is often under-recognized and under-treated compared to pain in younger adults (Gauthier & Gagliese, 2011; Herman, Johnson, Ritchie, & Parmelee, 2009; Horgas & Elliott, 2004).
There are few studies, however, that compare different healthcare professionals’ pain-related decisions and especially how those professionals might be influenced by patient demographic characteristics. Breuer, Cruciani, and Portenoy (2010) examined healthcare providers’ differential rates of medication prescription (i.e., opioid analgesics, non-opioid analgesics, and antidepressants) to chronic pain patients based on the healthcare professionals’ profession (Breuer, Cruciani, & Portenoy, 2010). They found that healthcare providers who specialized in pain management were more comfortable prescribing medication to chronic pain patients than those who did not specialize in pain management. The Breuer study did not, however, examine whether different types of providers are differentially influenced by patient demographic characteristics when making treatment decisions. In fact, we are not aware of any published study that has examined this possibility. This is an important area of inquiry, which may help provide additional information on sex, race, and age disparities in pain management, as well as inform efforts to reduce such disparities and improve pain care through targeted interventions/education.
Virtual human technology provides a novel, experimental, method for examining how patient demographic cues influence providers’ pain management decisions. Virtual humans have good visual fidelity and expressive facial animations and have been rated realistic by laypersons and healthcare professionals (Hirsh, George, & Robinson, 2009b). Hirsh et al. (2009b) found that nurses reported that 70% of the virtual humans” facial expressions were realistic depictions of pain and indicated that they made decisions about the virtual human patients’ pain similar to how they would make decisions about real patients. Virtual human technology has successfully been used to investigate the decision making of laypersons, healthcare trainees, and nurses (Alqudah et al., 2010; Hirsh et al., 2009b; Hirsh et al., 2011; Hirsh et al., 2009b; Stutts et al., 2010; Wandner et al., 2010).
Inconsistencies between the clinical research and experimental research findings regarding pain assessment and treatment may be due to studies being observational in nature and not true experiments that systematically manipulate variables (patient sex, race, and age). The virtual human technology can minimize inconsistencies in pain assessment and treatment by standardizing facial features and pain expressions.
Given the importance of examining how different healthcare professionals treat patients experiencing pain, the inconsistency in pain treatment, and the importance of equitable healthcare delivery, the current study sought to extend the previous literature by examining the common pain decision policies of a larger sample of healthcare professionals.
Method
Participants
We recruited 80 physicians (44 men and 36 women) and 113 nurses (10 men and 103 women) for a total sample of 193. Approximately 71% of participants were female, 69% were Caucasian, 11% were African American, 6% were Hispanic, 10% were Asian, and 4% identified as Other. The average age of the healthcare providers was 44 years (range: 22 to 75), and the average years of professional experience was 15 years (range: 1 to 47). A majority of the healthcare professionals lived in Florida (N=148). All participants provided informed consent and were compensated $50 for their participation. The demographic characteristics for the total sample, as well as for physicians and nurses, are described in Table 1.
Table 1.
Demographic characteristics of the healthcare professionals
| Healthcare Professionals (N= 193) | Physicians (N=80) | Nurses (N=103) | |
|---|---|---|---|
| Sex | |||
| Male | 54 (30%) | 44 (55%) | 10 (10%) |
| Female | 129 (70%) | 36 (455) | 93 (90%) |
| Race | |||
| Caucasian/White | 126 (69%) | 47 (59%) | 79 (77%) |
| African American/Black | 19 (11%) | 7 (9%) | 12 (12%) |
| Hispanic | 10 (6%) | 6 (8%) | 4 (4%) |
| Asian | 18 (10%) | 14 (18%) | 5 (4%) |
| Other | 8 (4%) | 6 (6%) | 3 (3%) |
| Age | Mean: 44.33 SD:11.78 (range:22–75) |
Mean: 47.81 SD: 15.72 (range:28–75) |
Mean:45.25 SD:12.55 (range:22–68) |
| Years Professional Experience | Mean:16.16 SD:12.26 (range:1–47) |
Mean:19.02 SD: 15.26 (range:1–45) |
Mean:16.92 SD:12.88 (range:1–47) |
Procedure
This study was approved by the Institutional Review Board (IRB) at the University of Florida. State registered physicians and nurses were mailed letters inviting them to participate in the study. Those who expressed interest were directed to a secure website to complete the study. After providing consent and completing a demographic questionnaire, the participants observed 32 unique virtual human patient profiles consisting of a text vignette and virtual human video. These patient virtual human profiles have been shown to constitute a reliable and valid approach to examine how patient demographic cues influence providers’ pain management decisions (Hirsh et al., 2009a; Hirsh et al., 2009; Stutts et al., 2010). For each patient profile, participants read a clinical vignette that described the patient as having low back pain. The low back pain vignette read as follows:
Patient presents with lower back pain for the past year of greater than one year duration. Patient reports that the pain began after a work-related lifting incident. The pain is located in the lumbar region of the back. The pain limits patient’s ability to move around freely. Patient reports no prior surgical treatments and has current prescriptions for anti-inflammatory and analgesic medications.
In addition to reading the clinical vignette, participants viewed a 20-second looped video of low and high pain expressing virtual human patients. Each 20-second looped video contained three cues: virtual human-sex (male, female), virtual human-race (Caucasian, African American), and virtual human-age (younger adult, older adult). The virtual human-sex, virtual human-race, and virtual human-age cues were portrayed by changes in the virtual humans ‘s’ appearance (e.g., skin tone, hair length). Pain expression was represented with empirically-validated facial expressions of pain, which consist of changes to specific facial action units (brow lowering, tightening of the orbital muscles, nose wrinkling/upper lip raising, and eye closure) from the Facial Action Coding System (FACS) (Prkachin, 1992). This level of inter-participant standardization and experimenter control of stimuli is an important advantage when studying demographic cue use. Seventy-one percent of the healthcare professionals in this study found the virtual human faces to be realistic depictions of pain. All of the cue combinations were presented twice, resulting in 32 unique virtual human profiles. Figure 1 and Figure 2 present still frame images captured from the virtual human videos.
Figure 1.
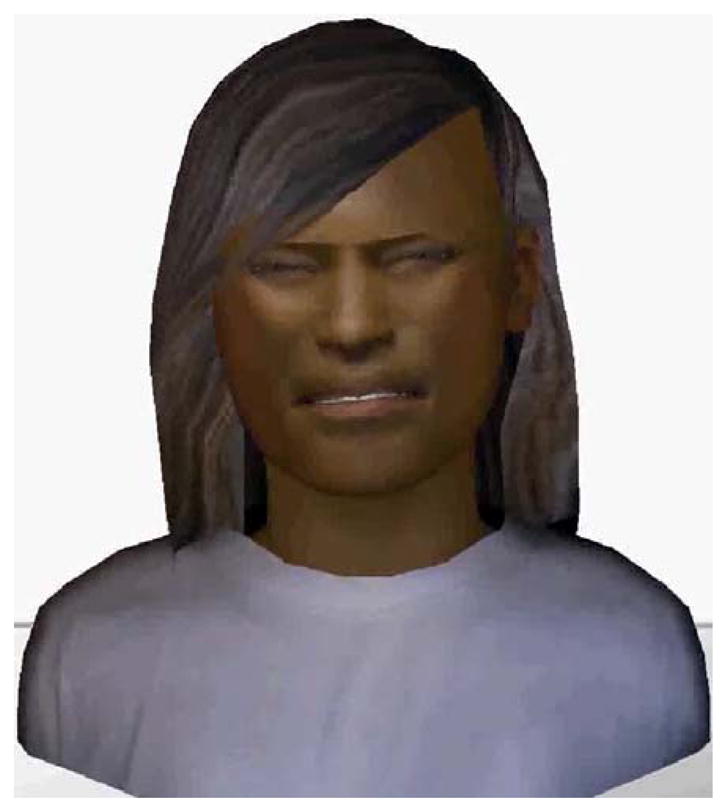
Still frame of virtual human cues representing female sex, African American race, young age, and high pain expression
Figure 2.
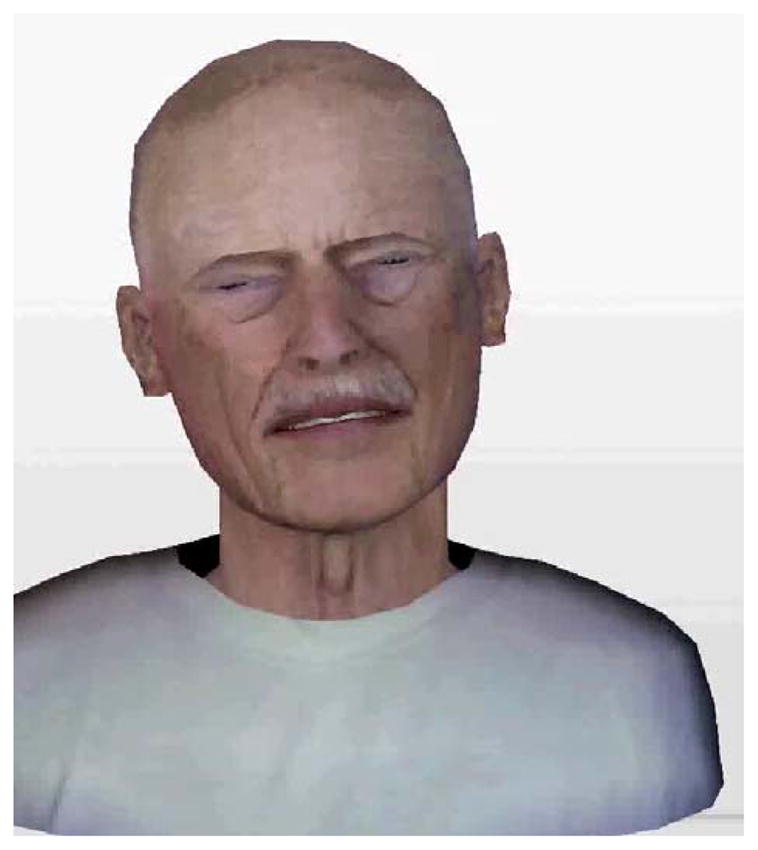
Still frame of virtual human cues representing male sex, Caucasian race, old age, and high pain expression
For each virtual human patient, participants answered 1 pain assessment (pain intensity) and 1 pain treatment (willingness to administer opioids) question. Pain ratings were recorded on separate 100-point VASs. Endpoints ranged from no pain sensation to most intense pain imaginable (pain intensity), and not at all likely to complete certainty (willingness to administer opioid analgesics).
Statistical Analyses
All data analyses were performed using SPSS for Windows (Version 20). Descriptive statistical analyses were conducted to summarize the demographic and background characteristics of the sample. T-test analyses were conducted to determine whether participants could distinguish between the VH patients’ high and low pain expression. Repeated Measures Analysis of Variance (RANOVA) Between-Within design was performed to examine assessment and treatment decisions across different types of healthcare professionals (physicians and nurses) as a function of the virtual human patients’ demographic characteristics (sex, race, and age). The between variable was the type of healthcare professional and the within variables were the virtual human patients’ demographic characteristics.
Results
Low vs. High Pain Expressing Virtual Human Patients
T-test analyses indicated that healthcare professionals rated pain intensity higher and were more willing to administer opioid analgesics to high pain expressing virtual human patients than to low pain expressing virtual human patients. The results are consistent with previous work and provide validation for our pain expression manipulation of the virtual human stimuli. Subsequent analyses were conducted on only the high pain expressing stimuli. Table 2 presents the results of the T-test analyses.
Table 2.
Pain assessment and treatment results of the paired samples T-test
| Decision | Cue | Low-Pain Expression | High Pain Expression | T | Cohen’s d | ||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Pain Assessment | Female African American Young | 28.71 | 19.12 | 57.97 | 21.56 | −22.21*** | −1.44 |
| Female African American Old | 37.76 | 21.80 | 50.87 | 24.80 | −9.29*** | −.56 | |
| Female Caucasian Young | 22.81 | 18.09 | 52.15 | 22.74 | −23.53*** | −1.43 | |
| Female Caucasian Old | 34.81 | 21.66 | 53.64 | 22.73 | −14.52*** | −.85 | |
| Male African American Young | 27.82 | 18.25 | 53.37 | 24.36 | −16.74*** | −1.19 | |
| Male African American Old | 35.07 | 20.61 | 51.75 | 22.17 | −12.78*** | −.78 | |
| Male Caucasian Young | 22.78 | 17.31 | 45.02 | 22.25 | −18.05*** | −1.12 | |
| Male Caucasian Old | 33.63 | 21.59 | 49.91 | 21.50 | −13.21*** | −.76 | |
| Pain Treatment | |||||||
| Female African American Young | 26.40 | 24.76 | 51.68 | 29.53 | −16.85*** | −.93 | |
| Female African American Old | 32.19 | 26.92 | 44.59 | 30.39 | −7.72*** | −.43 | |
| Female Caucasian Young | 21.18 | 23.76 | 44.97 | 30.24 | −15.02*** | −.87 | |
| Female Caucasian Old | 30.54 | 26.16 | 46.09 | 29.08 | −11.33*** | −.56 | |
| Male African American Young | 24.82 | 24.42 | 46.76 | 29.42 | −14.47*** | −.81 | |
| Male African American Old | 30.42 | 25.37 | 44.91 | 29.22 | −10.65*** | −.53 | |
| Male Caucasian Young | 20.86 | 22.83 | 39.72 | 28.99 | −13.98*** | −.72 | |
| Male Caucasian Old | 29.53 | 26.06 | 43.28 | 27.82 | −10.13*** | −.51 | |
Pain Assessment
The results of the ANOVA on pain intensity ratings indicate main effects for virtual human-sex (F(1,180)=20.97, p<.001, pη2=.10), virtual human-race (F(1,180)=21.10, p<.001, pη2=.11), and virtual human-age (F(1,180)=4.16, p=.04, pη2=.023. Participants assessed virtual human patients who were male, African American, or older as having greater pain intensity than female, Caucasian, or younger virtual human patients. Table 3 presents the means and standard errors for the pain assessment main effects.
Table 3.
Descriptive statistics for the pain assessment and treatment main effects
| Mean | Standard Error | |
|---|---|---|
| Pain Assessment | ||
| Profession | ||
| Doctor | 46.31 | 2.14 |
| Nurse | 50.72 | 1.90 |
| Sex | ||
| Male | 47.07 | 1.44 |
| Female | 49.97 | 1.49 |
| Race | ||
| Caucasian | 46.83 | 1.43 |
| African American | 50.20 | 1.52 |
| Age | ||
| Young | 47.69 | 1.46 |
| Old | 49.34 | 1.51 |
| Pain Treatment | ||
| Profession | ||
| Doctor | 33.84 | 2.77 |
| Nurse | 47.74 | 2.46 |
| Sex | ||
| Male | 39.30 | 1.86 |
| Female | 42.28 | 1.93 |
| Race | ||
| Caucasian | 39.22 | 1.85 |
| African American | 42.36 | 1.94 |
| Age | ||
| Young | 40.27 | 1.88 |
| Old | 41.31 | 1.94 |
There was also a significant virtual human-sex by HCP profession interaction (F(1,180)=8.93, p=.003, pη2=.05). The virtual human-sex difference (male > female) was more pronounced for nurses than for physicians. Figure 3 displays the virtual human-sex by profession interaction for pain intensity.
Figure 3.
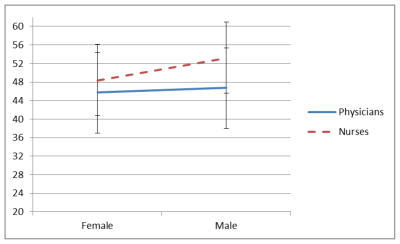
Virtual human-sex by profession interaction for pain intensity
Several significant interactions between the virtual human demographic cues were also observed. A significant virtual human-sex by virtual human-race interaction (F(1,180)=5.17, p = .02, pη2 = .03) indicated that the virtual human-sex difference (male > female) was more pronounced for African American virtual humans than for Caucasian virtual humans. A virtual human-sex by virtual human-age interaction (F(1,180)=17.94, p<.001, pη2 = .09) indicated that the sex difference (male > female) was larger for younger virtual humans than for older virtual humans. Finally, a significant VH-age by VH-race interaction (F(1,180)=50.13, p<.001, pη2 = .22) suggested that there was a more pronounced difference between races (African Americans > Caucasians virtual humans) for younger virtual humans than older virtual humans. Figure 4 displays the virtual human-age by virtual human-race interaction for pain intensity.
Figure 4.
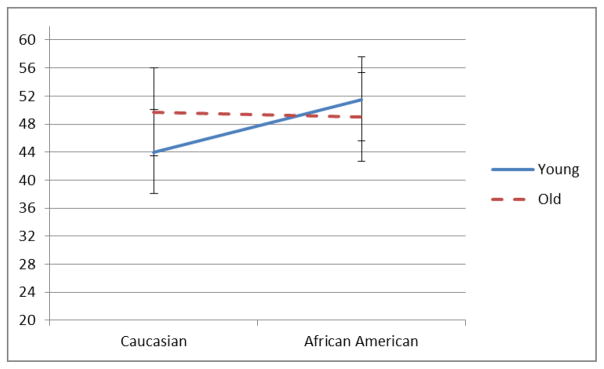
Virtual human-age by virtual human-race interaction for pain intensity
Willingness to Administer Opioid Analgesics
The results of the ANOVA on willingness to administer opioid analgesics to virtual human patients indicate a main effect for virtual human-sex (F(1,180)=14.07, p< .001, pη2 = .07), virtual human-race (F(1,180)=16.02, p<.001, pη2 = .08), and healthcare profession (F(1,180)=14.08, p<.001, pη2 = .07). Participants indicated that they were more willing to administer opioids to male or African American virtual human patients than to female or Caucasian virtual human patients. The main effect for healthcare profession indicates that nurses were more willing to administer opioid analgesics to virtual human patients than were physicians. Table 3 presents the means and standard errors for the pain treatment main effects.
There was also a significant virtual human-sex by HCP profession interaction (F(1,180)=7.16, p=.008, pη2 = .04). The sex difference (male > female) ratings were more pronounced for nurses than physicians. Figure 5 displays the virtual human-sex by profession interaction for willingness to administer opioid analgesics.
Figure 5.
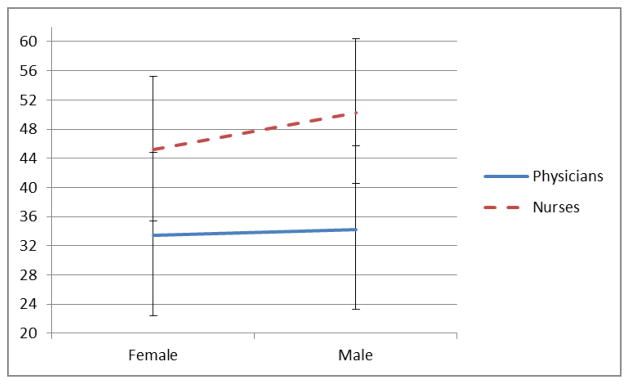
Virtual human-sex by profession interaction for willingness to administer opioid analgesics
A virtual human-sex by virtual human-age interaction (F(1,180)=7.50, p=.007, pη2 = .04) was also observed and indicates that the sex difference (male > female) was more pronounced for older virtual humans than younger virtual humans. Finally, a significant virtual human-age by virtual human-race interaction (F(1,180)=41.00, p<.001, pη2 = .19) indicates that the age difference (young > old for African Americans and old > young for Caucasians) was more pronounced for African American than Caucasian virtual humans. Figure 6 displays the virtual human-sex by virtual human-age interaction for willingness to administer opioids.
Figure 6.
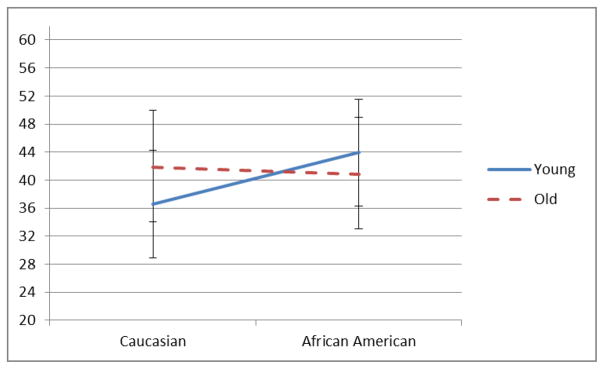
Virtual human-sex by virtual human-age interaction for willingness to administer opioids
Female Sample of Physicians and Nurses
To address a potential sex of provider confound (more female nurses) the RANOVAs were conducted with only female physicians and nurses. The results were similar to the results presented above except for one finding. When assessing female participants, a 3-way interaction (Race X Age X Profession) was significant for pain intensity (F(1,126)=3.83, p =.05, pη2 = .03). The 3-way interaction indicates that for both female physicians and nurses there was a more pronounced race difference (African American > Caucasians) for younger than for older virtual humans. As in the total sample, the nurses’ pain intensity ratings were greater than were the physicians’ ratings.
Caucasian Sample of Physicians and Nurses
To address a potential race of provider confound (more Caucasian nurses and physicians) the RANOVAs were conducted with only Caucasian physicians and nurses. The results were similar to the results presented above. However for pain intensity, there no longer was a main effect for age or for healthcare profession. For willingness to administer opioid analgesics, there no longer was a Sex X Age or Sex X healthcare professional interaction. It is possible that there was not enough power to detect the interactions, or that the minority sample influenced the ability to detect interactions.
Discussion
Recent studies have reported that laypersons, healthcare trainees, and practicing clinicians are influenced by patient sex, race and age when making pain assessment and treatment decisions (Alqudah et al., 2010; Hirsh et al., 2009a; Hirsh et al., 2011; Hirsh et al., 2009b; Stutts et al., 2010; Wandner et al., 2010). However, there has been limited research examining whether different types of healthcare professionals use these cues in pain decision-making. This is an important area of inquiry, especially considering evidence of the existence of pain management disparities, and may inform future research and interventions aimed at reducing disparities and improving pain care.(Anderson et al.) The current study began to address this gap in the literature by using virtual human technology to investigate how patients’ sex, race, and age influence different healthcare professionals’ (i.e., physicians and nurses) pain-related decision-making.
We found meaningful differences in how healthcare professionals make decisions about pain assessment and treatment in general, as well as differences in their pain management decisions across patient demographic groups. Healthcare professionals rated pain higher and were more likely to treat male and African American virtual human patients with opioids than they were female and Caucasian virtual human patients. Healthcare professionals were also more willing to rate pain higher for older than for younger adults. In addition, nurses were more willing to administer opioid analgesics than were physicians.
When specifically looking at the female participants’ or Caucasian participants’ pain management ratings, the results were similar to those of the total participants. Nevertheless, for female participants there was a 3-way way interaction between the race of the virtual human, the age of the virtual human, and the participant’s profession. We did not have any a priori hypothesis about why nurses had a more pronounced race difference in their pain ratings for young than for old virtual humans than their physician counterparts. Similarly, for the Caucasian participants’, we did not have any apriori hypotheses for why we lost some of the two-way interactions. Thus, we are hesitant to interpret these finding and encourage future research to examine these differences to determine if they are reliably observed.
Overall, the results were consistent with previous virtual human patient studies on pain management (Alqudah et al., 2010; Hirsh et al., 2009a; Hirsh et al., 2011; Hirsh et al., 2009b; Stutts et al., 2010; Wandner et al., 2010). However, consistent with clinical research, but inconsistent with previous virtual human results, physicians and nurses rated male virtual humans’ pain higher and were willing to treat their pain more aggressively than female virtual humans (Alqudah et al., 2010; Hirsh et al., 2009a; Hirsh et al., 2011; Hirsh et al., 2009b; Stutts et al., 2010; Wandner et al., 2010). Previous clinical research has suggested that healthcare professionals perceive men as less likely to report pain, or display pain behaviors, unless they are experiencing high levels of pain. Since there is minimal research examining how healthcare professionals rate pain intensity and report willingness to administer opioids when observing standardized facial pain expressions, it is possible that healthcare professionals use different cues to make their pain management decisions than laypeople or healthcare trainees. It is also possible that healthcare professionals’ experience with patients in a clinical setting influences their pain management decisions as opposed to laypeople who base their ratings on personal experiences with pain and non-patients. One explanation for this finding could be due to commonly held gender stereotypes within the United States. For example, if a man reports that he is in pain, it is thought that he must really be in pain if he counters the gender stereotype to be “tough” and not show that he is pain, whereas it is more acceptable for a woman to report that she is in pain (Robinson et al., 2001). Finally, this sample represents an older age cohort than that used in many studies on gender-role stereotypes and may reflect age cohort (of raters) effects related to gender-role expectations of pain (Robinson et al., 2001). More research is needed to examine these potential expected gender role effects.
Consistent with prior virtual human research, but inconsistent with clinical research, the pain intensity of African American virtual human patients’ was rated higher and they were more likely to be treated with opioid analgesics than Caucasian virtual human patients. It is possible that due to cultural differences (race or ethnicity might influence how an individual responds emotionally and behaviorally to pain, interprets the meaning of pain, and conducts pain appraisals), healthcare professionals were more willing to assess and treat pain of African American than Caucasian virtual human patients due to cultural stereotypes. Also, the questions in this study did not ask the dosage of the opioids the healthcare professional was willing to prescribe. As a result, the healthcare professionals might be more willing to prescribe small dosages of opioids to African American virtual human patients, but less likely to prescribe higher dosages. It is also possible that inconsistencies are due to some participants initially having difficulty relating to a virtual human patient, versus an actual patient in the clinic. However, a majority of the participants indicated that the virtual human patients’ pain expression realistically depicted a person’s pain expression.
The current study advanced the literature on pain decision-making by recruiting two different types of healthcare professionals whose professional responsibilities often include pain assessment and treatment. Including both types of healthcare professionals allowed us to examine differences in their general approach to chronic pain management as well as differences in their decision-making for diverse patient groups. Awareness of such group differences could be used by healthcare professional schools and associations to provide targeted training to their constituents to reduce disparities and improve pain care for all patients. This awareness could also lead to increased awareness by individual providers of the patient factors that might influence their clinical decisions.
There are multiple public health implications of the results of this study. First, the study suggests that, similar to the Breuer, Cruciani, and Portenoy (2010) study, different healthcare professions assess and treat pain differently depending on the patients’ demographics (Breuer et al., 2010). Physicians and nurses, who also were able to discriminate between high and low pain expression, may, as part of their general practice, spend relatively less time focusing on the face than on whole body examinations. However, it is important to examine why physicians rate pain intensity lower and are less willing to administer opioid analgesics to patients experiencing pain than are nurses. Differential ratings of pain and willingness to administer opioids could be due to professional group differences in pain management education which, Breuer et al. (2010) suggest, is important for adequate pain management practices for all healthcare professionals (Breuer et al., 2010). Second the healthcare professionals’ use of patient demographic cues when assessing and treating patients is important when considering the large number of patients these providers treat over the course of their careers. Thus, healthcare professionals who are influenced by a patient’s demographic characteristics when making clinical decisions could impact the care of thousands of patients before, during, or after healthcare procedures. Patient care could also be affected if such cue use is communicated, implicitly or explicitly, to other healthcare professionals or trainees during healthcare professional education activities. These issues highlight the importance of including evidence-based pain assessment and treatment education in medical and nursing schools.
This study also points to interesting areas of future research. Future research could examine whether increasing healthcare professionals’ awareness of the non-medical patient factors that influence their decisions actually improves their decision-making. For example, does simply informing healthcare professionals that they use demographic cues to make pain assessment and treatment decisions actually reduce demographic cue use? Such a low intensity intervention might not be enough to change the behavior of healthcare professional, but this is an open empirical question. Thus, future research is needed to determine the necessary and sufficient components of interventions or education tutorials that might improve pain assessment and treatment practices for varying demographic groups.
This study has several limitations. The healthcare professionals who participated might represent a select sample and, thus, might limit the generalizability of our findings. Also, the sample was relatively homogenous, consisting mostly of Caucasian healthcare professionals. Their responses might not be representative of the diverse national professional healthcare population. Finally, despite the virtual human innovation that increases the realism of the stimuli and the task, the study might not have represented a fully ecologically valid clinical scenario.
In summary, this study found that healthcare professionals rated male and African American virtual humans as having higher pain in most pain assessment and treatment domains compared to their demographic counterparts. The study also found that physicians rated pain intensity lower, and were less likely to prescribe opioid analgesics than nurses. The sex and age difference ratings were more pronounced for nurses than physicians. The reasons for the more complex interactions between virtual human-sex, virtual human-race, and virtual human-age are, as yet, not understood. Examination of cultural factors, beliefs and stereotypes about demographic groups are likely to be fruitful areas for further research that might provide more information about these relationships. These results could inform future research, education, and clinical practice by increasing awareness of potential sex, race, and age cue use in assessment and treatment of pain by HCPs.
Research Highlights.
What is already known about the topic? Biases exist in pain ratings and healthcare professionals have been found to use patient demographic cues such as sex, race, and age when making pain management decisions.
What this paper adds? Healthcare professionals’ pain ratings differed depending on healthcare profession (nurses or physicians). Nurses were more likely to rate pain higher and be more willing to administer opioid analgesics than were physicians.
Acknowledgments
Supported in part by grants: National Institute of Dental & Craniofacial Research (R01DE013208) to Dr. Michael Robinson
We thank the National Institute of Dental & Craniofacial Research (R01DE013208) for funding our research.
Footnotes
There were no conflicts of interest in this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alqudah AF, Hirsh AT, Stutts LA, Scipio CD, Robinson ME. Sex and Race Differences in Rating Others’ Pain, Pain-Related Negative Mood, Pain Coping, and Recommending Medical Help. Journal of Cyber Therapy Rehabilitation. 2010;3(1):63–70. [PMC free article] [PubMed] [Google Scholar]
- Anderson KO, Mendoza TR, Valero V, Richman SP, Russell C, Hurley J, Cleeland CS. Minority cancer patients and their providers: pain management attitudes and practice. Cancer. 2000;88(8):1929–1938. [PubMed] [Google Scholar]
- Breuer B, Cruciani R, Portenoy RK. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: a national survey. [Research Support, Non-U.S. Gov’t] Southern Medical Journal. 2010;103(8):738–747. doi: 10.1097/SMJ.0b013e3181e74ede. [DOI] [PubMed] [Google Scholar]
- Calderone KL. The influence of gender on the frequency of pain and sedative medication administered to postoperative patients. Sex Roles. 1990;23:713–725. [Google Scholar]
- Chen EH, et al. Gender disparity in analgesic treatment of emergency deparmtnet patients with acute abdominal pain. Academic Emergency Medicine. 2008;15:414–418. doi: 10.1111/j.1553-2712.2008.00100.x. [DOI] [PubMed] [Google Scholar]
- Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH, Stewart JA, Pandya KJ. Pain and its treatment in outpatients with metastatic cancer. New England Journal of Medicine. 1994;330(9):592–596. doi: 10.1056/NEJM199403033300902. [DOI] [PubMed] [Google Scholar]
- Faherty BS, Grier MR. Analgesic medication for elderly people post-surgery. Nurs Res. 1984;33(6):369–372. [PubMed] [Google Scholar]
- Gauthier LR, Gagliese L. Assessment of pain in older persons. New York: Guilford Press; 2011. [Google Scholar]
- Herman AD, Johnson TM, Ritchie CS, Parmelee PA. Pain management interventions in the nursing home: A structured review of the literature. Journal of the American Geriatrics Society. 2009;57:1258–1267. doi: 10.1111/j.1532-5415.2009.02315.x. [DOI] [PubMed] [Google Scholar]
- Hirsh AT, Alqudah AF, Stutts LA, Robinson ME. Virtual human technology: capturing sex, race, and age influences in individual pain decision policies. Pain. 2009a;140(1):231–238. doi: 10.1016/j.pain.2008.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsh AT, Callander SB, Robinson ME. Patient demographic characteristics and facial expressions influence nurses’ assessment of mood in the context of pain: a virtual human and lens model investigation. [Research Support, N.I.H., Extramural] International Journal of Nursing Studies. 2011;48(11):1330–1338. doi: 10.1016/j.ijnurstu.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsh AT, George SZ, Robinson ME. Pain assessment and treatment disparities: a virtual human technology investigation. Pain. 2009b;143(1–2):106–113. doi: 10.1016/j.pain.2009.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horgas AL, Elliott AF. Pain assessment and management in persons with dementia. Nursing Clinics of North America. 2004;39:593–606. doi: 10.1016/j.cnur.2004.02.013. [DOI] [PubMed] [Google Scholar]
- Prkachin KM. The consistency of facial expressions of pain: a comparison across modalities. Pain. 1992;51(3):297–306. doi: 10.1016/0304-3959(92)90213-U. [DOI] [PubMed] [Google Scholar]
- Robinson ME, Riley JL, Myers CD, Papas RK, Wise EA, Waxenberg LB, Fillingim RB. Gender role expectations of pain: Relationship to sex differences in pain. The Journal of Pain. 2001;2(5):251–257. doi: 10.1054/jpai.2001.24551. [DOI] [PubMed] [Google Scholar]
- Stutts LA, Hirsh AT, George SZ, Robinson ME. Investigating patient characteristics on pain assessment using virtual human technology. European Journal of Pain. 2010;14(10):1040–1045. doi: 10.1016/j.ejpain.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wandner LD, Stutts LA, Alqudah AF, Craggs JG, Scipio CD, Hirsh AT, Robinson ME. Virtual human technology: patient demographics and healthcare training factors in pain observation and treatment recommendations. Journal of Pain Research. 2010;3:241–247. doi: 10.2147/JPR.S14708. [DOI] [PMC free article] [PubMed] [Google Scholar]


