Abstract
Vascular calcification can be categorized into two different types. Intimal calcification related to atherosclerosis and elastin-specific medial arterial calcification (MAC). Osteoblast-like differentiation of vascular smooth muscle cells (VSMCs) has been shown in both types; however, how this relates to initiation of vascular calcification is unclear. We hypothesize that the initial deposition of hydroxyapatite-like mineral in MAC occurs on degraded elastin first and that causes osteogenic transformation of VSMCs. To test this, rat aortic smooth muscle cells (RASMCs) were cultured on hydroxyapatite crystals and calcified aortic elastin. Using RT-PCR and specific protein assays, we demonstrate that RASMCs lose their smooth muscle lineage markers like alpha smooth muscle actin (SMA) and myosin heavy chain (MHC) and undergo chondrogenic/osteogenic transformation. This is indicated by an increase in the expression of typical chondrogenic proteins such as aggrecan, collagen type II alpha 1(Col2a1) and bone proteins such as runt-related transcription factor 2 (RUNX2), alkaline phosphatase (ALP) and osteocalcin (OCN). Furthermore, when calcified conditions are removed, cells return to their original phenotype. Our data supports the hypothesis that elastin degradation and calcification precedes VSMCs' osteoblast-like differentiation.
Keywords: Matrix Mineralization, Osteoblast-like differentiation, Osteogenesis, Phenotype, Vascular calcification
Introduction
There are two distinctive types of vascular calcification: intimal atherosclerotic plaque calcification and medial elastin-specific arterial calcification (MAC). Intimal calcification occurs in the context of atherosclerosis, associated with lipids, macrophages, and vascular smooth muscle cells; whereas, medial calcification can exist independently of atherosclerosis and is associated with elastin and vascular smooth muscle cells[1]. In this study we mainly focused on the mechanisms of MAC. It has been accepted for decades that the pathology of vascular calcification resembles physiological bone mineralization in that it shows the presence of bone proteins and osteo-chondrogenic cells [2, 3]. However, mere presence of osteogenic cells and bone protein expression in the calcified arterial tissue does not warrant the role of osteogenesis in the initiation of elastin calcification. The scientific knowledge gap still exists about the cause-and-effect relationship between the elastin-specific medial calcification and osteoblast-like differentiation of vascular smooth muscle cells (VSMCs). It is still unclear if there exists a chronological occurrence between the osteoblast-like differentiation of VSMCs and passive deposition of hydroxyapatite on elastin, or if both processes occur simultaneously causing the eventual calcification of arteries.
Based on our previous in vivo data [4, 5], we hypothesize that the initial mineral deposition on elastin precedes the osteoblast-like differentiation of VSMCs, which is a pathological response to elastin degradation and early arterial calcification. To test this hypothesis, we exposed rat aortic smooth muscle cells (RASMCs) to calcified conditions, by culturing them on hydroxyapatite and calcified elastin. We show when exposed to a calcific environment, healthy RASMCs transform to osteoblast-like cells; removal of calcific environment restores the native phenotype of SMCs.
Materials and methods
Cell culture and treatment
Primary rat aortic smooth muscle cells (RASMCs) were isolated from rat aorta according to published protocol[6]. Passage numbers 5 to 8 were used for all experiments. Cells were cultured in 60 mm tissue culture petri dish (2×106 cells/well) in Dulbecco's Modified Eagle Medium (Cellgro-Mediatech, Manassas, VA), containing 10% fetal bovine serum (Cellgro-Mediatech, Manassas, VA), 100 units/ml penicillin and 100 units/ml streptomycin (Cellgro-Mediatech, Manassas, VA) in a humidifier incubator (Innova® CO-170) at 37 °C, with 5% CO2. Media was replenished every 3 days. Hydroxyapatite powder (average size <200 um) was purchased from Aldrich Chemical Company (Milwaukee, WI). One mg of hydroxyapatite was coated onto 60 mm tissue culture Petri dish. Here the coating process was achieved by first placing a hydroxyapatite suspension in sterile phosphate-buffered saline (PBS) on a Petri dish and then drying it overnight under sterile cell culture hood. For control group, the RASMCs were cultured in a Petri dish without hydroxyapatite coating. To better mimic the calcified pathological situation, RASMCs were also cultured in a Petri dish with a coating of calcified porcine aortic elastin fibers (10 mg per well) while a coating with non-calcified elastin served as a control. The calcified porcine aortic elastin fibers were prepared in vitro based on a modified protocol[7] and the average size for both the pure and calcified elastin fiber were less than 200 μm (passed through 200 μm sieve). Briefly purified elastin was suspended in a calcifying solution (Tris-HCl buffer PH7.4; KCl 55 mmol/l; KH2PO4 35 mmol/l; CaCl2 35 mmol/l) for 7 days with shaking at 37°C. Poorly crystalline hydroxyapatite was deposited on elastic fibers. The calcium deposition was characterized by alizarin red stain and scanning electron microscope (SEM, Hitachi's SU6600) with energy dispersive X-ray spectrometer (EDX) and quantified by atomic absorption spectroscopy (Perkin-Elmer Model 3030, Norwalk, CT). Cells were grown on top of calcified matrix for 1 day and 7 days. To study the RASMCs' fate after removing calcified conditions, the cells were first cultured for 7 days on calcified matrix (specifically both hydroxyapatite and calcified elastin) followed by isolation and placement on a 60 mm tissue culture Petri dish without calcified matrix for an additional 7 days, or 14 days total as referred to below (n=12 per group total, 3 for RNA isolation, 3 for protein isolation, 3 for cell immunofluorescence and another 3 for staining for alkaline phosphatase). The experiments were repeated twice.
Gene expression
At each time point, cell monolayers were scraped and homogenized (n=3 per group) using a homogenizer (PowerGen Model 125 Homogenizer, Fisher Scientific, Atlanta, GA). The total RNA from the cells was isolated using the RNeasy Mini Kit (Qiagen, MD). The concentration of the extracted RNA was quantified by UV spectroscopy using Take3 Micro-Volume Plates from BioTek (Winooski, VT). One microgram of RNA was reverse transcribed to cDNA by High Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA) using a Mastercycler gradient (Eppendorf Scientific, Inc., Westbury, NY). The cDNA samples were further amplified on a Rotor gene 3000 thermal cycler (Corbett Research, Mortlake, NSW, Australia) for real - time polymerase chain reaction (PCR). The primers sequences for β-2microglobulin (β2-MG)[5], alpha smooth muscle actin (SMA)[8], myosin heavy chain (MHC)[9], aggrecan[10], collagen type II alpha 1(Col2a1)[11], alkaline phosphatase (ALP)[5], Runt-related transcription factor 2 (RUNX-2)[5] and osteocalcin[5] are listed in Table 1. Gene expression in each sample was normalized to the expression of β2-MG as housekeeping gene and compared with control samples (for the hydroxyapatite study group, the control was the cells grown on standard culture plates while for the calcified elastin group, the control was the cells grown on non-calcified elastin coated culture plates) using the 2-ΔΔCT method[12] as follows: ΔΔCT= (CT target gene-CT β-2 MG) study – (CT target gene-CT β-2 MG) control.
Table 1.
PCR primers used in the RT-PCR study.
| Name | References | Forward primer | Reverse primer |
|---|---|---|---|
| β2 MG | Lee et al[5]. | CGTGATCTTTCTGGTGCTTGTC | ACGTAGCAGTTGAGGAAGTTGG |
| SMA | Simionescu et al[8] | ACTGGGACGACATGGAAAAG | CATACATGGCAGGGACATTG |
| MHC | Low et al[9]. | AAGCAGCTCAAGAGGCAG | AAGGAACAAATGAAGCCTCGTT |
| Aggrecan | Agung et al[10]. | TAGAGAAGAAGAGGGGTTAGG | AGCAGTAGGAGCCAGGGTTAT |
| Clo2a1 | Zhang et al[11]. | TCCTAAGGGTGCCAATGGTGA | AGGACCAACTTTGCCTTGAGGAC |
| OCN | Lee et al[5]. | TATGGCACCACCGTTTAGGG | CTGTGCCGTCCATACTTTCG |
| ALP | Lee et al[5]. | TCCCAAAGGCTTCTTCTTGC | ATGGCCTCATCCATCTCCAC |
| RUNX2 | Lee et al[5]. | CAACCACAGAACCACAAGTGC | CACTGACTCGGTTGGTCTCG |
Immunofluorescence
The cells were fixed in 4% paraformaldehyde (Affymetrix, Cleveland, OH) for 15 minutes at room temperature, treated with 1% bovine serum albumin (Sigma, St. Louis, MO)/0.2% Triton X-100 (MP Biomedicals, Solon, OH)/PBS for 1 hour at room temperature to block non-specific binding. The primary antibodies used include: mouse monoclonal Anti- SMA at 1:200 dilutions (Sigma, St. Louis, MO), mouse monoclonal [1C10] to smooth muscle Myosin heavy chain I at 1:200 dilution (Abcam, Cambridge, MA) and mouse anti-collagen type I at 5 μg/ml (Developmental Studies Hybridoma Bank, Iowa City, IA). After overnight incubation at 4 °C, cells were stained for 2 hours at room temperature in the dark with AlexaFlour 594 donkey anti-mouse IgG secondary antibody (Molecular Probes, Eugene, OR) diluted to 10 μg/ml. All well plates were mounted in VECTASHIELD HardSet Mounting Medium (VECTOR LABORATORIES, INC, Burlingame, CA) with DAPI (4′, 6-diamidino-2-phenylindole dihydrochloride) blue fluorescent nuclear stain (Molecular Probes, Eugene, OR) and examined by fluorescence microscopy.
Protein isolation
Cell monolayers were washed once with PBS and isolated in a mammalian extraction buffer. To prepare the buffer, 1 tablet of protease inhibitor cocktail (Roche Diagnostics, Indianapolis, IN) was added to 10ml of SoluLyse-M™ Mammalian Protein Extraction Reagent (Genlantis, San diego, CA). SoluLyse-M™ reagent (500 μl) was added into the 60 mm tissue culture petri dishes. Cells were incubated for 10 minutes at 25 °C with gentle rotation and then homogenized and centrifuged at 14,000 × g for 5 minutes. The supernatant was collected (preserved in -20°C freezer) and assayed for different proteins of interest. The total cellular protein was quantified by Pierce® BCA protein assay kit (Thermo scientific, Rockford, IL).
Western blotting
Ten micrograms of protein from each sample and molecular weight standards (Precision Plus Protein™ Kaleidoscope Standards, Bio Rad Life Science, Hercules, CA), were loaded in duplicate on 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis gels. After electrophoresis, the proteins were electro-transferred to Immobilon-P membranes (Millipore Corporation, Bedford, MA). Membranes were blocked in 2% nonfat dry milk (LabScientific, Inc., New Jersey) for 1 hour at room temperature and then probed with primary antibody overnight at 4°C. Primary antibodies used include: mouse monoclonal Anti- SMA at 1:1000 dilution (Sigma, St. Louis, MO), mouse monoclonal [1C10] to smooth muscle Myosin heavy chain I at 1:1000 dilution (Abcam, Cambridge, MA) and rabbit monoclonal [EP2978Y] to beta 2 Microglobulin (Abcam, Cambridge, MA). The proteins were detected by enhanced chemiluminescence according to the manufacturer's recommendations (Roche, Indianapolis, IN) and analyzed by densitometry using Image J software. The optical densities of the bands were reported as relative density units (RDU) comparing to the control groups. Beta 2 Microglobulin antibodies were used as the loading control and the target protein's band densities were first normalized by beta 2 Microglobulin.
ALP assay – colorimetric quantification and cell stain
Cell lysates were analyzed for alkaline phosphatase (ALP) using p-nitrophenyl phosphate (PNPP) as a substrate and diethanolamine buffer. Two PNPP tablets (Thermo scientific, Rockford, IL) were dissolved in 10 ml diethanolamine substrate buffer (Pierce, Rockford, IL). PNPP solution (200 μl) and protein samples (40 μl) were added into each well of the 96-well plate. The plate was incubated at room temperature for 30 minutes or until sufficient color developed. The reaction was stopped by adding 50 μl of 2N NaOH to each well. The absorbance was measured at 405 nm. Alkaline phosphatase was calculated using a p-nitrophenol (MP Biomedicals Inc, Solon, Ohio) standard curve and was normalized to the total protein content. Additionally, cells in culture were stained to corroborate the expression of ALP by the cells. Cells were stained with premixed BC IP/NBT solution (Sigma Aldrich, St. Louis, MO). The premixed BCIP/NBT solution contains 0.48 mM NBT (nitro blue tetrazolium), 0.56 mM BCIP (5-bromo-4-chloro-3-indolyl phosphate), 10 mM Tris HCl, 59.3 mM MgCl2, and pH ∼9.2. Cells were incubated in the staining solution in the dark for 1 hour at room temperature and then washed.
Osteocalcin Assay- Enzyme-linked immunosorbent assay (ELISA)
The total cellular protein samples were analyzed for osteocalcin using a Rat Osteocalcin ELISA Kit (Biomedical Technologies Inc., Stoughton, MA) following the manufacturer's instructions. 25 μl of total protein sample, rat osteocalcin serial standards(1.0, 2.5, 5.0, 10 and 20 ng/ml) and rat serum controls were pipetted into osteocalcin antibody coated well plate strips followed by 100 μl of osteocalcin antiserum(second antibody, goat polyclonal) at 37 °C for 2.5 hours. Donkey anti-goat IgG peroxidase conjugate was used as secondary antibody and 3, 3′, 5, 5′-Tetramethylbenzidine (TMB) was used as the peroxidase substrate. Levels of osteocalcin were calculated by rat osteocalcin standard curve and then normalized to total protein concentration.
Statistical Analysis
Results are expressed as means ± standard error of the mean (SEM). Statistical analyses of the data were performed using single-factor analysis of variance. Differences between means were determined using the least significant difference with an α value of 0.05. Asterisks in figures denote statistical significance (P < 0.05) for each group compared with controls.
Results
Characterization of calcified elastin
Calcified elastin was prepared in vitro and the calcium level in the calcified elastin fiber was detected as 15 ± 2 μg/mg using atomic absorption spectroscopy. The calcium deposition was evenly distributed over the porcine elastin fiber as seen by alizarin red stain, which stains calcium red while no staining was seen in the control pure elastin (Fig. 1A). The morphology of calcified elastin, as studied by scanning electron microscopy, showed globular calcific deposits. These were confirmed as calcium phosphates by Energy-dispersive X-ray spectroscopy (Fig. 1B and C).
Fig. 1.

Characterization for calcified elastin. A: Alizarin red staining for pure elastin (PE, left) and calcified elastin (CE, right). Calcium was stained red. Scale bar: 50μm. B: Scanning electron microscope (SEM) image for pure elastin (PE, left) and calcified elastin (CE, right). C: Energy-dispersive X-ray spectroscopy (EDX) pseudo colored image for Ca and P element distribution (Ca purple and P red). Mineral deposition is labeled with red arrows.
RASMCs lose smooth muscle lineage markers under calcified conditions
We analyzed gene and protein level expression of two typical smooth muscle lineage markers: alpha smooth muscle actin (SMA)[13] and myosin heavy chain (MHC)[14] in two different simulated calcified conditions: (1) pure hydroxyapatite; (2) calcified elastin. These markers were studied at two time points (day 1 and day 7) to see the changes compared to the control groups. Cellular localization based on immunofluorescence stain of SMA showed that both hydroxyapatite and calcified elastin groups had similar SMA expression at day 1 as controls; however, at day 7 they exhibited very low expression of SMA protein (Fig. 2A). Similarly, immunofluorescence stain for MHC also showed little change at day 1 but a significant decrease was observed at day 7 (Fig. 2B).
Fig. 2.

Expression of SMA and MHC in RASMCs cultured on hydroxyapatite and calcified elastin at day 1 and day 7. A and B: Immunofluorescence stains of SMA and MHC respectively (red fluorescence). Nuclei were stained blue by DAPI. Scale bar: 100μm. Abbreviations: HA-hydroxyapatite; PE: pure elastin; CE: calcified elastin. D1: day 1; D7: day 7. C and D: SMA and MHC gene expression respectively as measured by RT-PCR. E: protein expression measured by western blot followed by densitometry as relative density units (RDU) and expressed as relative percentage ratio comparing to control groups (For HA treatment group the control was normal media while for CE treatment group the control was PE). The band density was first normalized by loading control protein-β2 MG. Results are presented as mean ± SEM (* p<0.05).
Furthermore, both hydroxyapatite and calcified elastin treated groups showed decrease in the gene expression (quantified by RT-PCR) and protein expression (detected by western blot) of SMA and MHC at day 7. Compared to respective control groups, SMA gene expression decreased by 48 ± 18% in hydroxyapatite groups and 53 ± 5% in calcified elastin groups (Fig. 2C). Similarly, MHC gene expression decreased by 64 ± 19% in hydroxyapatite groups and 60 ± 13% in calcified elastin groups (Fig. 2D). Western blotting results confirmed the down-regulation of translation of both SMC markers. Compared to respective control groups, the SMA protein expression decreased by 56 ± 2 % in hydroxyapatite groups and 48 ± 2% in calcified elastin groups (Fig. 2E). The MHC protein expression decreased by 52 ± 6% in hydroxyapatite groups and 53 ± 2% in calcified elastin groups (Fig. 2E).
RASMCs develop an osteogenic/chondrogenic phenotype under calcified conditions
We then analyzed expression of three typical osteogenic markers: Runt-related transcription factor 2 (RUNX2) [15, 16], Alkaline phosphatase (ALP) and osteocalcin (OCN)[13, 14, 17, 18] and two typical chondrogenic markers: aggrecan and collagen type II alpha 1(Col2a1) to see whether RASMCs develop an osteogenic/chondrogenic phenotype with the stimuli of hydroxyapatite and calcified elastin. At day 1, we found significant upregulation of RUNX2 gene under mineralized conditions, which is the earliest transcription factor involved in osteogenesis. No other osteogenic markers were changed at day 1 as compared to controls (Fig. 3A). Compared to respective control groups, RUNX2 gene expression increased by 87 ± 43% in hydroxyapatite groups and 116 ± 19% calcified elastin groups at day 7. Similarly, at day 7, ALP gene expression increased by 41 ± 20% in hydroxyapatite groups and 188 ± 21% in calcified elastin groups while OCN gene expression increased by 111 ± 30% in hydroxyapatite groups and 54 ± 21% in calcified elastin groups (Fig. 3A).
Fig. 3.
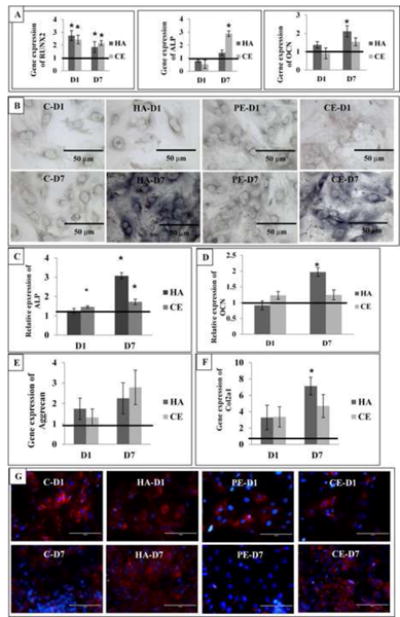
Expression of osteogenic/chondrogenic markers in RASMCs cultured on hydroxyapatite and calcified elastin elastin at day 1 and day 7. A: gene expression of RUNX2, ALP and OCN. B: Histochemical staining of ALP activity in cells in four groups (C-control, HA-hydroxyapatite, PE-pure elastin, CE-calcified elastin). Scale bar: 50μm. C: ALP protein quantification. D: OCN protein quantification. OCN was determined by ELISA assay and expressed as ng osteocalcin/mg protein. The relative protein expression for both ALP and OCN has been calculated compared to respective control groups. E: Gene expression of chondrogenic markers – aggrecan. F: Gene expression of chondrogenic markers – Col2a1. G: Immunofluorescence stains for collagen type I (red fluorescence). Nuclei were stained blue by DAPI. Scale bar: 100μm. Results are presented as mean ± SEM (* p<0.05).
Histochemical staining for ALP revealed intense purple coloration in both hydroxyapatite and calcified elastin groups indicating greater ALP activity compared to control groups (Fig. 3B). Additionally, quantification of cellular ALP activity showed an increase by 207 ± 35 % in hydroxyapatite groups and 72 ± 9 % in calcified elastin groups at day 7 (Fig. 3C). Osteocalcin protein expression increased by 97 ± 13 % in hydroxyapatite groups and 23 ± 12 % in calcified elastin groups respectively at day 7 (Fig. 3D). The ALP and OCN protein expression in calcified elastin groups was much less elevated might because of relative lower concentration of hydroxyapatite in elastin group, specifically one mg of of HA in hydroxyapatite versus only ∼150 μg in elastin group (10 mg of calcified elastin with mineral deposition of 15 ± 2 μg Ca/mg tissue) (Fig. 3C, 3D). It is also possible that HA crystal structure in two groups is different and that can cause variation in relative expression.
For the chondrogenic markers, at day 7, compared to respective control groups, Aggrecan gene expression increased by 125 ± 76% in hydroxyapatite groups and 179 ± 84% in calcified elastin groups(Fig. 3E); Col2a1 gene expression increased by 613 ± 108% in hydroxyapatite groups and 370 ± 141% in calcified elastin groups (Fig. 3F).
RASMCs show up-regulation of Collagen Type I under calcified conditions
Immunofluorescent detection of collagen type I showed an intense signal both for hydroxyapatite and calcified elastin treated group at day 7 (Fig. 3G). The increase of collagen type I expression under calcified conditions, indicated more synthetic phenotype of RASMCs under mineralized conditions.
RASMCs restore their original phenotype after removal of calcified matrix
In an independent set of experiments, RASMCs were cultured on calcified matrix for 7 days and then were cultured for another 7 days without the calcified matrix to study cellular behavior after removing calcified matrix. After 14 days (7 days post reversal) both hydroxyapatite and calcified elastin treated group showed dramatic restoration of VSMCs markers (comparable to control groups: for the hydroxyapatite study group, the control was the cells grown on standard culture plates while for the calcified elastin group; the control was the cells grown on non-calcified elastin coated culture plates at day 14) as detected by immunofluorescence (Fig. 4A, 4B) and RT-PCR and western blotting (Fig. 4C, 4D). All the earlier mentioned osteogenic/chondrogenic markers including RUNX2, ALP, OCN, aggrecan and col2a1 decreased gene expression at day 14 and restored close to normal level (Fig. 5A, 5B). The protein expression of ALP and OCN also decreased comparing to day 7 although still remained elevated comparing to the normal control levels (Fig. 5C). Histochemical staining for ALP restored to normal level comparing to the controls (Fig. 5D). Collagen type 1 expression also restored close to normal level (Fig. 5E). These results indicate that the phenotypic transition from smooth muscle cells to osteoblast-like cells is reversible with reversal of calcification.
Fig. 4.

Expression of SMA and MHC in RASMCs after removal of calcified matrix. Cells were cultured on calcified matrix for 7 days, then removed and cultured in normal cell culture plate for additional 7 days (total 14 days of culture) A: Immunofluorescence stains of SMA (red fluorescence). B: Immunofluorescence stains of MHC (red fluorescence). Nuclei were stained blue by DAPI. Scale bar: 100μm. Abbreviations: C-control, HA-hydroxyapatite; PE: pure elastin; CE: calcified elastin. D14: day 14. C: SMA and MHC gene expression measured by RT-PCR. D: protein expression measured by western blot followed by densitometry as relative density units (RDU) and expressed as relative percentage ratio comparing to control groups (For HA treatment group the control was normal media while for CE treatment group the control was PE). The band density was first normalized by loading control protein-β2 MG. Results are presented as mean ± SEM (* p<0.05).
Fig. 5.

Expression of osteogenic/chondrogenic markers in RASMCs after removal of calcified matrix. Cells were cultured on calcified matrix for 7 days, then removed and cultured in normal cell culture plate for additional 7 days (total 14 days of culture) A: gene expression of RUNX2, ALP and OCN. B: gene expression of aggrecan and Col2a1. C: protein quantification of ALP and OCN. D: Histochemical staining of ALP activity in cells at in four groups(C, HA, PE, CE). Original magnification, 400×. Scale bar: 50μm. E: Immunofluorescence stains for collagen type I (red fluorescence). Nuclei were stained blue by DAPI. Scale bar: 100μm. Results are presented as mean ± SEM (* p<0.05).
Discussion
Our data shows that, in response to the calcified matrix, for both hydroxyapatite crystals and calcified aortic porcine elastin, RASMCs lose their smooth muscle lineage markers, specifically alpha smooth muscle actin (SMA) and myosin heavy chain (MHC). In addition, RASMCs undergo chondroblast/osteoblast-like differentiation confirmed by an increase in expression of typical bone-markers such as Runt-related transcription factor 2 (RUNX2), alkaline phosphatase (ALP), osteocalcin (OCN), aggrecan, and collagen type II alpha 1(Col2a1). RASMCs also turn synthetic as indicated by increased expression of collagen type I. Interestingly, this phenotypic transition was reversible and RASMCs restored their original linage upon reversal of calcification.
Putative relationship between osteoblast-like transformation of VSMCs and vascular calcification is still under debate and the cause-and-effect relationship between these two processes is unclear. It has been reported that the vascular calcification process can be caused by osteoblast-like differentiation of VSMCs[19]. Chronic kidney disease (CKD) related vascular calcification has often been associated with increase serum Ca and P levels[20]. Elevated phosphate conditions could cause osteogenic/chondrogenic differentiation of VSMC [13, 21]. In rat models of renal failure, animals with severe calcification showed the presence of chondrocyte-like cells. Mature cartilage tissue and major chondrogenic factors were found in the calcified vessels[22]. Osteoblast-like differentiation of VSMCs was also reported in the aortae of transgenic mice, ubiquitously expressing Msx2 (encodes an osteoblast-specific transcription factor), that were fed with a high-fat diet. High-fat diets led to vascular calcification in these transgenic mice but not in their non-transgenic littermates[23]. In type-2 diabetes related medial calcification, BMP-2/Mxs2/Wnt signaling has been established[24]. Studies in patients with type 2 diabetes showed that medial calcification is a cell-mediated process characterized by a phenotypic change of VSMCs to osteoblast-like cells[25]. Based on these studies, it is thought that chondrogenic/osteogenic transformation of VSMCs is the earliest step in vascular calcification.
Alternatively, there are many studies support that medial elastin-specific calcification can occur due to degraded elastin without osteoblastic differentiation of VSMCs. In early 1970s, Urry has shown that elastin has a specific calcium binding site serving as the neutral nucleation site for calcium [26]. We previously showed that pure aortic elastin when implanted subdermally in rats undergoes calcification with bone-protein expression occurring only in the later stages of mineral propagation[5]. In circulatory rat model, we confirmed that matrix metalloproteinases (MMPs) mediated degradation of elastin, leads to elastic-lamina calcification in absence of cell-associated calcification [4]. Price et al. have shown that in the presence of serum factors, arterial elastin calcifies in vitro in absence of cells[27]. Furthermore, VSMCs have shown osteoblast-like behavior in vitro when exposed to elastin peptides along with TGF-beta, therefore suggesting a causative role of elastin degradation in VSMCs mediated calcification [17]. Recently Murshed et al found in a MGP-deficient (Mgp−/−) mice model, chondro/osteogenic markers are not up-regulated in the arteries prior to the initiation of calcification[28]. One recent study found that calcium phosphate deposition was a passive phenomenon and it was responsible for the osteogenic changes for the VSMCs[29]. All these studies indicate that initial vascular calcification may be formed without osteoblastic differentiation of VSMCs.
Our study was designed to investigate the effect of calcified matrix on RASMCs' phenotypic change. We hypothesize that the initial mineral deposition on elastin precedes the osteoblast-like differentiation which is a pathological response to elastin degradation and early arterial calcification. Our results showed that RASMCs lose their smooth muscle lineage markers like SMA and MHC (Fig. 2) and undergo chondrogenic/osteogenic transformation (Fig. 3) under calcified conditions. It is unclear as to how calcified matrix triggers this response in RASMCs and further study is needed to test this. Calcium and phosphorus levels in the media were similar in controls and calcified matrix groups (data not shown), thus osteoblast-like transformation seen on our studies was not due to higher amounts of free ions as shown by others[13, 20, 21]. We speculate that RASMCs synthesize small quantities of bone proteins (they come from same mesenchymal origin of osteoblasts). These proteins in healthy state do not accumulate in the vessel media; however, calcified elastin matrix can bind to these synthesized proteins[30, 31] and increase local concentration causing RASMCs to turn to osteoblast-like cells. Interestingly, our work, for the first time shows that upon removal of calcified conditions, cells have the ability to revert back to SMC-like cell behavior. When calcified matrix was removed from culture conditions, SMA and MHC expression increased to normal levels, whereas osteogenic/chondrogenic markers decreased to normal levels (Fig. 4, Fig. 5). This is important as we can then envision demineralizing strategies to remove mineral from arteries and bring homeostasis to the arterial structures.
To summarize, there are possibilities of two distinctly different, yet interconnected mechanisms to demonstrate the cause-and-effect relationship between chondro/osteoblast-like differentiation of VSMCs and medial elastin-specific calcification as shown in Fig. 6. Model A: chondro/osteoblast-like differentiation of VSMCs precedes medial elastin-specific calcification. Many factors could induce VSMCs into osteoblast-like cells, such as elevated level of phosphate, lipids, inflammatory cytokines and others[32]. Those differentiated osteoblast-like VSMCs synthesize bone proteins such as osteocalcin, alkaline phosphatase to initiate mineral deposition. This may be true in patients with chronic kidney disease and type-2 diabetes where increase incidences of vascular medial calcification has been found[20, 25]. Model B: Medial elastin-specific calcification precedes chondro/osteogenic differentiation of VSMCs. In ageing patients or in patients with diseases like aortic aneurysm and arteriosclerosis, increased matrix metalloproteiases activity can lead to accelerated elastic fiber degradation. This degradation would expose calcium binding sites in elastin and allow initial mineral deposition[26]. This early mineral deposits may anchor calcium binding proteins such as osteocalcin. This local increase in bone proteins may lead to transformation of SMCs to osteoblast-like cells. It is also possible that these two processes occur simultaneously and add mutually. Our current data mostly supported Model B, that is, the first calcium deposition on elastin appear prior to the osteoblast-like differentiation of RASMCs. Interestingly based on our data of reversal of osteogenic markers, we hypothesize that demineralization of calcified arteries will return homeostasis in arteries. In fact, recently we have shown that local delivery of chelating agent such as ethylene diamine tetraacetic acid (EDTA) led to regression of arterial calcification in rats[33].
Fig. 6.

Model of putative links between medial elastin-specific calcification and chondro/osteoblast-like differentiation of VSMCs in the artery. A: chondro/osteoblast-like differentiation of VSMCs precedes medial elastin-specific calcification. Elevated levels of phosphate, lipids, inflammatory cytokines and many other factors could induce chondro/osteoblast-like differentiation of VSMCs. B: Medial elastin-specific calcification precedes chondro/osteoblast-like differentiation of VSMCs. The elastin degradation happens due to inflammatory conditions and matrix metalloproteinases. This in turn exposes calcium binding sites on elastin causing first calcific deposits. This early calcification leads to osteoblast-like differentiation in VSMCs that can further augment calcification process.
Limitations of Current Study
There are some limitations to our studies. First, we used reagent grade synthetic hydroxyapatite to mimic the ectopic deposition of mineral in vascular calcification, which might not be ideal to represent the real pathologic condition of vascular calcification, which shows poorly crystalline hydroxyapatite crystals and other calcium phosphate minerals. We also used porcine aortic elastin that was allowed to calcify in vitro. It indeed showed poorly crystalline hydroxyapatite deposits along the elastin fibers. Finally, we did the studies only for two time points: day 1, and day 7. It is still unknown if longer exposure of RASMCs to calcified conditions would prevent reversal to normal phenotype. More physiologic or animal studies are needed to further test the hypothesis that medial elastin-specific calcification occurs first followed by cellular changes to osteoblast like cells to augment mineral deposits.
Conclusions
In conclusion, our results demonstrate that hydroxyapatite and calcified elastin induce chondrogenic and osteoblast-like differentiation of rat aortic smooth muscle cells, and these studies support that elastin degradation and calcification may occur prior to osteoblast-like transformation of VSMCs.
Research Highlights.
Rat aortic smooth muscle cells (RASMCs) when cultured on calcified matrix undergo osteoblast-like differentiation.
RASMCs down-regulate smooth muscle lineage markers and up-regulate osteogenic protein markers under calcified conditions.
Once the calcified matrix is removed, smooth muscle cells restore their original phenotype.
Acknowledgments
The authors would like to thank Dr. Martine LaBerge at department of bioengineering of Clemson University (Clemson, SC) for the gift of rat aortic smooth muscle cells, Dr. Jeoung Soo Lee at department of bioengineering of Clemson University for help with molecular biology analysis such as RT-PCR, western blotting and immunofluorescence, Dr. Haijun Qian at Clemson University Electron Microscopy Laboratory for the SEM work, and Andrew Holman for manuscript edits. This work was partially supported by NIH P20GM103444 grant and Hunter Endowment to Dr. Naren Vyavahare.
List of Abbreviations
- VSMCs
vascular smooth muscle cells
- RASMCs
rat aortic smooth muscle cells
- β2-MG
β-2microglobulin
- SMA
alpha smooth muscle actin
- MHC
myosin heavy chain
- Col2a1
collagen type II alpha 1
- RUNX2
runt-related transcription factor 2
- ALP
alkaline phosphatase
- ELISA
enzyme-linked immuno sorbent assay
- DAPI
4′,6-Diamidino-2-Phenylindole, Dihydrochloride
- TMB
tetramethylbenzidine
- HA
hydroxyapatite
- CE
calcified elastin
- PE
pure elastin
- CKD
chronic kidney disease
- MMPs
matrix metalloproteinases
Footnotes
Disclosures: All authors state that they have no conflicts of interest.
Authors' roles: Study design: YL, AS and NV. Study conduct: YL, AS, NN and AG. Data collection: YL. Data analysis: YL, AS and NV. Data interpretation: YL, AS and NV. Drafting manuscript: YL. Revising manuscript content: YL, AS, NN, AG and NV. Approving final version of manuscript: YL, AS, NN, AG and NV. YL and NV take responsibility for the integrity of the data analysis.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Proudfoot D, Shanahan CM. Biology of Calcification in Vascular Cells: Intima versus Media. Herz. 2001;26:245–251. doi: 10.1007/pl00002027. [DOI] [PubMed] [Google Scholar]
- 2.Bini A, Mann KG, Kudryk BJ, Schoen FJ. Noncollagenous Bone Matrix Proteins, Calcification, and Thrombosis in Carotid Artery Atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology. 1999;19:1852–1861. doi: 10.1161/01.atv.19.8.1852. [DOI] [PubMed] [Google Scholar]
- 3.Dhore CR, Cleutjens JPM, Lutgens E, Cleutjens KBJM, Geusens PPM, Kitslaar PJEHM, Tordoir JHM, Spronk HMH, Vermeer C, Daemen MJAP. Differential Expression of Bone Matrix Regulatory Proteins in Human Atherosclerotic Plaques. Arteriosclerosis Thrombosis, and Vascular Biology. 2001;21:1998–2003. doi: 10.1161/hq1201.100229. [DOI] [PubMed] [Google Scholar]
- 4.Basalyga DM, Simionescu DT, Xiong W, Baxter BT, Starcher BC, Vyavahare NR. Elastin Degradation and Calcification in an Abdominal Aorta Injury Model: Role of Matrix Metalloproteinases. Circulation. 2004;110:3480–3487. doi: 10.1161/01.CIR.0000148367.08413.E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee JS, Basalyga DM, Simionescu A, Isenburg JC, Simionescu DT, Vyavahare NR. Elastin Calcification in the Rat Subdermal Model Is Accompanied by Up-Regulation of Degradative and Osteogenic Cellular Responses. The American Journal of Pathology. 2006;168:490–498. doi: 10.2353/ajpath.2006.050338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stegemann JP, Nerem RM. Altered response of vascular smooth muscle cells to exogenous biochemical stimulation in two-and three-dimensional culture. Experimental cell research. 2003;283:146–155. doi: 10.1016/s0014-4827(02)00041-1. [DOI] [PubMed] [Google Scholar]
- 7.Mavrilas D, Apostolaki A, Kapolos J, Koutsoukos PG, Melachrinou M, Zolota V, Dougenis D. Development of bioprosthetic heart valve calcification in vitro and in animal models: morphology and composition. Journal of Crystal Growth. 1999;205:554–562. [Google Scholar]
- 8.Simionescu A, Simionescu DT, Vyavahare NR. Osteogenic Responses in Fibroblasts Activated by Elastin Degradation Products and Transforming Growth Factor-β1: Role of Myofibroblasts in Vascular Calcification. The American Journal of Pathology. 2007;171:116–123. doi: 10.2353/ajpath.2007.060930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Low RB, White SL, Low ES, Neuville P, Bochaton-Piallat ML, Gabbiani G. Age dependence of smooth muscle myosin expression by cultured rat aortic smooth muscle cells. Differentiation. 1999;65:151–159. doi: 10.1046/j.1432-0436.1999.6530151.x. [DOI] [PubMed] [Google Scholar]
- 10.Agung M, Ochi M, Yanada S, Adachi N, Izuta Y, Yamasaki T, Toda K. Mobilization of bone marrow-derived mesenchymal stem cells into the injured tissues after intraarticular injection and their contribution to tissue regeneration. Knee Surgery Sports Traumatology Arthroscopy. 2006;14:1307–1314. doi: 10.1007/s00167-006-0124-8. [DOI] [PubMed] [Google Scholar]
- 11.Zhang M, Zhou Q, Li CG, Holz J, Tang D, Sheu TJ, Li TF, Shi Q, Wang YJ. IGF-1 regulation of type II collagen and MMP-13 expression in rat endplate chondrocytes< i> via</i> distinct signaling pathways. Osteoarthritis and Cartilage. 2009;17:100–106. doi: 10.1016/j.joca.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 12.Livak KJ, Schmittgen TD. Analysis of Relative Gene Expression Data Using Real-Time Quantitative PCR and the 2< sup>- ΔΔCT</sup> Method. methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 13.Steitz SA, Speer MY, Curinga G, Yang HY, Haynes P, Aebersold R, Schinke T, Karsenty G, Giachelli CM. Smooth Muscle Cell Phenotypic Transition Associated With Calcification: Upregulation of Cbfa1 and Downregulation of Smooth Muscle Lineage Markers. Circulation Research. 2001;89:1147–1154. doi: 10.1161/hh2401.101070. [DOI] [PubMed] [Google Scholar]
- 14.Giachelli CM, Speer MY, Li X, Rajachar RM, Yang H. Regulation of Vascular Calcification: Roles of Phosphate and Osteopontin. Circulation Research. 2005;96:717–722. doi: 10.1161/01.RES.0000161997.24797.c0. [DOI] [PubMed] [Google Scholar]
- 15.Franceschi RT. The Developmental Control of Osteoblast-Specific Gene Expression: Role of Specific Transcription Factors and the Extracellular Matrix Environment. Critical Reviews in Oral Biology & Medicine. 1999;10:40–57. doi: 10.1177/10454411990100010201. [DOI] [PubMed] [Google Scholar]
- 16.Ducy P, Zhang R, Geoffroy V, Ridall AL, Karsenty G. Osf2/Cbfa1: A Transcriptional Activator of Osteoblast Differentiation. Cell. 1997;89:747–754. doi: 10.1016/s0092-8674(00)80257-3. [DOI] [PubMed] [Google Scholar]
- 17.Simionescu A, Philips K, Vyavahare N. Elastin-derived peptides and TGF-β1 induce osteogenic responses in smooth muscle cells. Biochemical and Biophysical Research Communications. 2005;334:524–532. doi: 10.1016/j.bbrc.2005.06.119. [DOI] [PubMed] [Google Scholar]
- 18.Oshima A, Tanabe H, Yan T, Lowe GN, Glackin CA, Kudo A. A novel mechanism for the regulation of osteoblast differentiation: Transcription of periostin, a member of the fasciclin I family, is regulated by the bHLH transcription factor, twist. Journal of Cellular Biochemistry. 2002;86:792–804. doi: 10.1002/jcb.10272. [DOI] [PubMed] [Google Scholar]
- 19.Demer LL, Tintut Y. Vascular Calcification: Pathobiology of a Multifaceted Disease. Circulation. 2008;117:2938–2948. doi: 10.1161/CIRCULATIONAHA.107.743161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moe SM, Chen NX. Mechanisms of Vascular Calcification in Chronic Kidney Disease. Journal of the American Society of Nephrology. 2008;19:213–216. doi: 10.1681/ASN.2007080854. [DOI] [PubMed] [Google Scholar]
- 21.Jono S, McKee MD, Murry CE, Shioi A, Nishizawa Y, Mori K, Morii H, Giachelli CM. Phosphate Regulation of Vascular Smooth Muscle Cell Calcification. Circulation Research. 2000;87:e10–e17. doi: 10.1161/01.res.87.7.e10. [DOI] [PubMed] [Google Scholar]
- 22.Neven E, Dauwe S, De Broe ME, D'Haese P, Persy V. Endochondral bone formation is involved in media calcification in rats and in men. Kidney International. 2007;72:574–581. doi: 10.1038/sj.ki.5002353. [DOI] [PubMed] [Google Scholar]
- 23.Shao JS, Cheng SL, Pingsterhaus JM, Charlton-Kachigian N, Loewy AP, Towler DA. Msx2 promotes cardiovascular calcification by activating paracrine Wnt signals. Journal of Clinical Investigation. 2005;115:1210–1220. doi: 10.1172/JCI24140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Towler DA. Angiogenesis and marrow stromal cell fates: roles in bone strength. Osteoporosis international. 2003;14:46–53. doi: 10.1007/s00198-003-1473-5. [DOI] [PubMed] [Google Scholar]
- 25.Chen NX, Duan D, O'Neill KD, Moe SM. High glucose increases the expression of Cbfa1 and BMP-2 and enhances the calcification of vascular smooth muscle cells. Nephrology Dialysis Transplantation. 2006;21:3435–3442. doi: 10.1093/ndt/gfl429. [DOI] [PubMed] [Google Scholar]
- 26.Urry DW. Neutral Sites for Calcium Ion Binding to Elastin and Collagen: A Charge Neutralization Theory for Calcification and Its Relationship to Atherosclerosis. Proceedings of the National Academy of Sciences. 1971;68:810–814. doi: 10.1073/pnas.68.4.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Price PA, Si Chan W, Jolson DM, Williamson MK. The Elastic Lamellae of Devitalized Arteries Calcify When Incubated in Serum: Evidence for a Serum Calcification Factor. Arteriosclerosis, Thrombosis, and Vascular Biology. 2006;26:1079–1085. doi: 10.1161/01.ATV.0000216406.44762.7c. [DOI] [PubMed] [Google Scholar]
- 28.Khavandgar Z, Roman H, Li J, Lee S, Vali H, Brinckmann J, Davis EC, Murshed M. Elastin haploinsufficiency impedes the progression of arterial calcification in MGP-deficient mice. Journal of Bone and Mineral Research. 2013 doi: 10.1002/jbmr.2039. [DOI] [PubMed] [Google Scholar]
- 29.Villa-Bellosta R, Millan A, Sorribas V. Role of calcium-phosphate deposition in vascular smooth muscle cell calcification. American Journal of Physiology - Cell Physiology. 2011;300:C210–C220. doi: 10.1152/ajpcell.00229.2010. [DOI] [PubMed] [Google Scholar]
- 30.Hoang QQ, Sicheri F, Howard AJ, Yang DS. Bone recognition mechanism of porcine osteocalcin from crystal structure. Nature. 2003;425:977–980. doi: 10.1038/nature02079. [DOI] [PubMed] [Google Scholar]
- 31.Reinholt FP, Hultenby K, Oldberg A, Heinegård D. Osteopontin--a possible anchor of osteoclasts to bone. Proceedings of the National Academy of Sciences. 1990;87:4473–4475. doi: 10.1073/pnas.87.12.4473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Speer MY, Giachelli CM. Regulation of cardiovascular calcification. Cardiovascular Pathology. 2004;13:63–70. doi: 10.1016/S1054-8807(03)00130-3. [DOI] [PubMed] [Google Scholar]
- 33.Lei Y, Grover A, Sinha A, Vyavahare N. Efficacy of Reversal of Aortic Calcification by Chelating Agents. Calcif Tissue Int. 2013:1–10. doi: 10.1007/s00223-013-9780-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


