Abstract
Objective
A period of particularly high risk for suicide attempts among adolescent inpatients is within 12 months after discharge. However, little is known about longitudinal trajectories of suicidal ideation in this high-risk group and how these relate to post-hospitalization suicide attempts and rehospitalizations. Our objectives were to identify these trajectories and examine their relationships with post-hospitalization psychiatric crises. We also examined predictors of trajectory group membership.
Method
Participants (N=376; ages 13-17; 72% females) were assessed at hospitalization and 3, 6, and 12 months later. Trajectory groups, and their predictors, were identified with latent class growth modeling. We used logistic regression to examine associations between trajectory groups and likelihood of suicide attempts and rehospitalization, controlling for attempt history.
Results
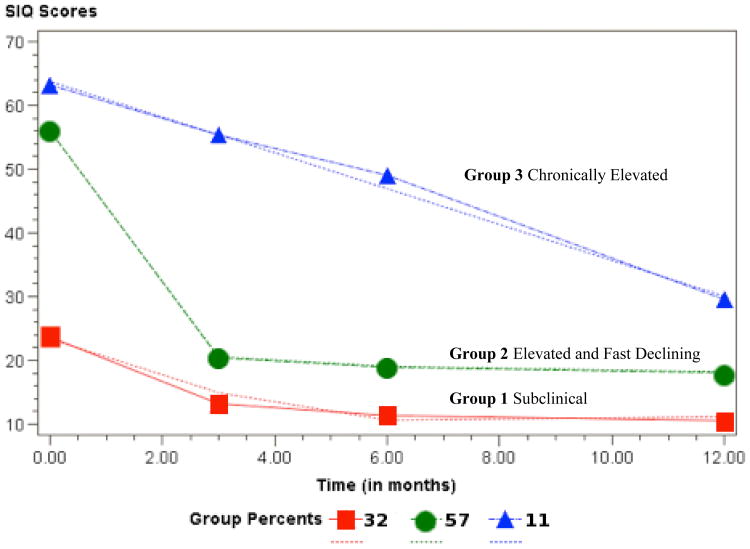
Three trajectory groups were identified: (1) subclinical ideators (31.6%); (2) elevated ideators with rapidly declining ideation (57.4%); and (3) chronically elevated ideators (10.9%). Adolescents in the chronically elevated ideation group had 2.29[(CI=1.08,4.85), p=0.03] and 4.15[(CI=1.65,10.44), p<0.01] greater odds of attempting suicide and 3.23[(CI=1.37,7.69), p=0.01] and 11.20[(CI=4.33,29.01), p<0.001] greater odds of rehospitalization relative to rapidly declining and subclinical groups, respectively. Higher baseline hopelessness was associated with persisting suicidal ideation.
Conclusions
Results suggest that suicidal ideation severity at hospitalization may not be an adequate marker for subsequent suicidal crises. It is important to identify adolescents vulnerable to persisting suicidal ideation, as they are at highest risk of psychiatric crises. Addressing hopelessness may facilitate faster declines in ideation after hospitalization. Results also highlight a need for consistent monitoring of these adolescents' suicidal ideation after discharge.
Keywords: suicidal ideation, longitudinal, suicide attempt, adolescents, hopelessness
Suicide is among the leading causes of death among adolescents in the United States (Centers for Disease Control and Prevention, 2012a). Precursors to suicide are also of significant concern. Within the last year, approximately 16% and nearly 8% of high school students surveyed nationally reported serious suicidal thoughts and suicide attempts, respectively (Centers for Disease Control and Prevention, 2012b). The transition to adolescence marks a sensitive developmental period during which suicidal ideation and behaviors are on the rise. According to a recent, nationally representative study, the prevalence of suicidal ideation increases rapidly between ages 12 and 17 while the rates of plans and attempts are rising increasingly between the ages of 12 and 15 and then more slowly until age 17 (Nock et al., 2013). This increase is attributed in part to important developmentally normative events (e.g., greater cognitive ability of thinking about and planning a suicide), limitations in self-self-regulation of emotions and capacity for problems solving, as well as greater prevalence of psychopathology, particularly mood disorders and substance abuse (see review by Bridge, Goldstein, & Brent, 2006; King, 1997). It is particularly important to understand suicidal phenomena among psychiatrically hospitalized adolescents. Psychiatrically hospitalized adolescents are a particularly vulnerable group as they are at high risk for repeated suicide attempts, especially within the first year of hospitalization (Goldston et al., 2001; King, Kerr, Passarelli, Foster, & Merchant, 2010; King et al., 1995). In addition, a recent study of previously hospitalized teens who were followed for six months found that a significant percentage of these teens were at a high risk for suicide risk-related events, such as emergency department visits (23%) and inpatient hospitalizations (28%) (Yen, Weinstock, Andover, Sheets, Selby, & Spirito, 2013). Preventing suicidal behavior among these high-risk teens requires a better understanding of which adolescents are most at risk for repeated suicidal episodes and what factors can improve post-hospitalization functioning.
Surprisingly little is known about longitudinal patterns of suicidal ideation among recently discharged adolescent inpatients and if, and for whom, these patterns change or are relatively stable. Findings from community studies demonstrate that suicidal ideation tends to persist over time, even into adulthood, and is associated with poor functioning in many life domains and suicide attempts (Fergusson, Horwood, Ridder, & Beautrais, 2005; Herba, Ferdinand, van der Ende, & Verhulst, 2007; Lewinsohn, Rohde, & Seeley, 1994; Reinherz, Tanner, Berger, Beardslee, & Fitzmaurice, 2006). Among psychiatric adolescent inpatients, severe suicidal ideation at the time of hospitalization has also been implicated as a strong predictor of post-hospitalization suicide attempts six months to a year later (Huth-Bocks, Kerr, Ivey, Kramer, & King, 2007; King, et al., 2010; King, et al., 1995). Few studies, however, have examined the longitudinal course of suicidal ideation among psychiatrically hospitalized teens and how these trajectories may impact future risk of suicidal behavior. A better understanding of the course of suicidal ideation following a suicidal crisis could have significant implication for improving how to best intervene with these adolescents to minimize subsequent suicidal crises.
To the best of our knowledge, only one study investigated the course of suicidal ideation among psychiatrically hospitalized adolescents who were followed for 18 months (Prinstein et al., 2008). It is noteworthy that the sample included suicidal and non-suicidal adolescents, and thus the findings may not directly apply to adolescents hospitalized for acute suicide risk. The authors found that there was a sharp decrease in suicidal ideation during the first six months after hospitalization, which then gradually reemerged between nine and eighteen months after hospitalization. The significance of these fluctuations is that increases in suicidal ideation were associated with subsequent increases in the risk of a suicide attempt. Moreover, of significance is that specific factors in this study maintained elevated suicidal ideation. Specifically, higher depressive symptoms and higher levels of non-suicidal self-injury measured at the time of hospitalization were found to be associated with less pronounced decreases in suicidal ideation right after hospitalization. In contrast, externalizing disorders (conduct and oppositional defiant disorders) were associated with more of a decrease in suicidal ideation over time. Interestingly, the decreasing pattern of suicidal ideation within six months of hospitalization was also found in a recent study of suicidal inpatient adolescents whose retrospective ratings of weekly suicidal ideation over a course of six months showed a reduction in suicidal thinking during the follow-up (Selby, Yen, & Spirito, 2013).
An important question that has not been addressed is whether there are different trajectory groups among previously hospitalized adolescents, as opposed to the single trajectory that was recently reported by Prinstein and colleagues (2008) to describe fluctuations in suicidal ideation. For example, some adolescents may follow a decreasing and then increasing pathway, as described in Prinstein et al.'s study, while others may follow a continuously decreasing pathway. There may also be a subgroup that has a more stable or chronic pattern of suicidal ideation. In fact, a study involving adolescents from the community, assessed at age 14, 15, and 17, identified three different suicidal ideation trajectory subgroups –no ideation, decreased ideation, and persistent or increased ideation –rather than a single group (Reuter, Holm, McGeorge, & Conger, 2008). These authors examined the association between the three trajectories and risk of suicidal behavior across a 10-year period, reporting that adolescent females in the increasing ideation group and males in the decreasing ideation group had the highest probability of attempting suicide. It is unclear, however, the extent to which these findings would be directly relevant to psychiatrically hospitalized teens who tend to experience more severe suicidal ideation, are at higher risk for suicidal behaviors, and for whom mapping a more short-term course of ideation might be of greater significance given that they are particularly vulnerable to suicidal behavior after hospitalization. In addition, this study did not explore what factors predicted membership in the three trajectory groups that were identified.
Mapping the course of suicidal ideation post hospitalization may have an advantage over considering suicidal ideation only at the time of hospitalization: A better understanding of longitudinal patterns of suicidal ideation following hospitalization, and the degree to which this course is uniform or different among subgroups, may help inform which adolescents are at the greatest risk of post-hospitalization suicidal behavior. The purpose of this study was to examine if acutely suicidal inpatient adolescents who had been recently discharged follow different suicidal ideation trajectories post hospitalization, and the extent to which these trajectories were associated with future suicide attempts and psychiatric rehospitalization; we examined if this effect would hold over and above history of prior suicide attempts, which is the strongest predictor of suicidal behavior (Bridge et al, 2006; Goldston et al, 1999). We hypothesized that there will be at least two distinct trajectory groups: a decreasing suicidal ideation group and a persistent or chronic group. In addition, we also anticipated there may be a third group that is following a decreasing and then increasing pathway, as described in Prinstein et al.'s (2008) study. We expected that teens in the persistent or chronic suicidal ideation group would be at greatest risk for suicidal behavior and for rehospitalization. Moreover, recent evidence suggests that suicidal ideation at the time of hospitalization is a significant predictor of suicidal behavior one year later for adolescent girls, but not boys (King, Jiang, Czyz, & Kerr, under review), providing additional support for considering the severity of suicidal ideation beyond index hospitalization to improve identification of all at-risk adolescents. To this effect, we examined if the influence of group trajectories on likelihood of suicide attempts and rehospitalization would be moderated by sex. We also examined the moderating effect of multiple suicide attempt history, as teens who attempt suicide more than once have the highest risk for future suicide attempts after hospitalization relative to suicide ideators or one-time attempters (D'Eramo, Prinstein, Freeman, Grapentine, & Spirito, 2004; Goldston, et al, 1999; Miranda et al, 2008). Finally, we explored what risk and protective factors assessed at the time of hospitalization predict membership in suicidal ideation trajectories. We build on previous studies by considering the influence of several important correlates of suicidal thoughts and behavior, including adolescents' sex, multiple suicide attempt status, depressive symptoms, externalizing problems, substance use, hopelessness, history of parental psychopathology, history of physical and sexual abuse, and family and peer connectedness (Borowsky, Ireland, & Resnick, 2001; Bridge, et al, 2006; King & Merchant, 2008; Lewinsohn, Rohde, & Seeley, 1996).
Methods
Participants
Participants were 376 adolescents who had been psychiatrically hospitalized due to acute suicidal ideation or attempt and were subsequently followed for one year. The sample was drawn from a randomized clinical trial of a psychosocial intervention—Youth-Nominated Support Team-II—for suicidal adolescents following hospitalization (King, Klaus, Kramer, Venkataraman, Quinlan, & Gillespie). The original study included 448 adolescents, ages 13 to 17. Inclusion criteria were adolescent or parent reports of recent (within 4 weeks) suicidal ideation that was either unrelenting or accompanied by a specific plan (“Did you think about killing yourself many times in the last four weeks?” or “Did you plan exactly how you would kill yourself?”) or recent suicide attempt, both taken from the Diagnostic Interview Schedule for Children (DISC-IV) (Shaffer, Fisher, Lucas, & NIMH DISC Editorial Board, 1998). Exclusion criteria included severe cognitive impairment, direct transfer to a medical unit or a residential placement, distances of more than one hour that preclude travel, and unavailability of a legal guardian. A detailed description of the study design and participant recruitment and retention are available in the original study (King et al. 2009).
Adolescents were included in the present study if they had baseline data for suicidal ideation and completed at least one follow-up assessment three, six, or 12 months after hospitalization. Participants were predominantly female (72%) with a mean age of 15.6 years (SD= 1.31). The racial/ethnic composition of the sample was approximately 83% Caucasian, 7% African-American, 0.5% Asian-American/Pacific Islander, 2% Hispanic, 0.5% Native American, and 7% “Other” or not identified. The annual income of adolescents' families ranged from less than $15,000 (6% of families) to more than $100,000 (17% of families), with the median annual family income between $40,000 and $59,000. Further, 10% of participants lived in families where at least one parent received public assistance. Participants with and without follow-up data did not differ significantly on important demographic variables (i.e. sex, age, race, use of public assistance), the primary predictors of interest, baseline suicidal ideation, and suicide attempt history. In addition, adolescents assigned to YST-II, versus usual care only, did not have a significantly different rate of suicide attempts during the 12-month follow-up.
Procedures
Participants were recruited from a university hospital or a private hospital in the midwestern region of the United States. Study eligibility criteria were determined based on hospital admission records, and adolescents meeting study criteria were approached to participate. Parents or guardians of eligible adolescents provided written informed consent and adolescents provided informed assent. Participants were assessed during or within one week of hospitalization, and follow-up data (3, 6, and 12 months later) were collected at an outpatient office adjacent to the hospital or in the participants' homes. Participating adolescents and parents were compensated $30 and $20, respectively, for completing each assessment. The study was approved by the participating university's Institutional Review Board.
Measures
Suicide Attempts
Lifetime multiple attempt status, assessed at baseline, and suicide attempts at each of the follow-up points were assessed using suicide attempt items from the DISC–IV (Shaffer, et al., 1998). The presence of suicide attempts was assessed with the question “Have you ever, in your whole life, tried to kill yourself or made a suicide attempt?” (yes/no). The time frame was adapted to capture the appropriate assessment window at each follow-up assessment.
Suicidal Ideation
Severity of suicidal ideation was assessed with the Suicidal Ideation Questionnaire-Junior (SIQ-JR) (Reynolds, 1988), a 15-item self-report questionnaire that measures frequency of a range of suicidal thoughts. Frequency of suicidal thoughts is rated on a 7-point scale ranging from “I never had this thought” to “almost every day.” Total score can range from 0 to 90, with a published clinical cut-off score of 31. The SIQ-JR has solid, well-documented psychometric properties (Reynolds, 1988, 1992) and has been found to predict suicidal thoughts and attempts 6 months after psychiatric hospitalization in a sample of adolescents (King, Hovey, Brand, & Ghaziuddin, 1997). The internal consistency for the sample was 0.92.
Psychiatric Rehospitalization
A dichotomous variable was created (yes/no) based on two questions inquiring if a participant was in a psychiatric hospital or a general hospital for psychiatric or emotional problems since the last assessment. The time frame was adapted to capture the appropriate assessment window at each of the follow-up assessments. A positive response to either question was coded “yes.”
Depressive Symptoms
The Children's Depression Rating Scale-Revised (CDRS-R) (Poznanski & Mokros, 1996) was used to measure depressive symptoms within the previous two weeks. The CDRS-R is a semi-structured interview that assesses a broad range of depressive symptoms grouped into 17 areas, such as Appetite Disturbance, Sleep Disturbance, Social Withdrawal, or Depressed Feelings. Items are rated on a 5- or a 7-point scale and scores range from 17 to 113. The measure has strong psychometric properties in studies with adolescents (e.g., Emslie et al., 1997; Shain, Naylor, & Alessi, 1990). Inter-interviewer reliability for total scores, assessed prior to data collection, was high (mean alpha across raters of .98).
Hopelessness
The Beck Hopelessness Scale (BHS) (Beck & Steer, 1988) is a 20-item, true/false self-report questionnaire that was used to assess negative attitudes about the future. Scores range from 0 to 20, with higher scores indicating greater hopelessness. Example items include “I don't expect to get what I really want” and “My future seems dark to me.” The BHS has been shown to predict eventual suicides in adult psychiatric inpatients and outpatients in the original sample and has also demonstrated strong psychometric properties in adolescent samples (Goldston, et al., 2001). The internal consistency for the sample was 0.91.
Externalizing Symptoms
The externalizing problems scale from Youth Self-Report (YSR) (Achenbach, 1991) was used to assess externalizing behavior problems (delinquent and aggressive behaviors). YSR is a 119-item, questionnaire that assesses a variety of emotional and behavioral problems in adolescents. It is a widely used measure with strong psychometric properties; its two scales (internalizing and externalizing) have demonstrated strong psychometric properties, including internal consistency, test-retest reliability, and criterion and construct validity (Achenbach, 1991; Thurber & Hollingsworth, 1992). The externalizing problems scale has items such as “I destroy my own things” and “I disobey my parents.” Adolescents rate each item by selecting responses from 0 (not true) to 2 (Very true or often true). The externalizing subscale for the study sample was 0.86.
Substance Use
The Personal Experiences Questionnaire (PESQ) (Winters, 1991, 1992) is a 41-item self-report questionnaire used to screen for abuse of alcohol or other substances in adolescents. Sample items include “How often have you used alcohol or other drugs at home” and “How often have you made excuses to teachers about your alcohol or drug use?” The problem severity scale used in this study consists of 18 items assessing the frequency with which adolescents engage in behaviors related to alcohol and drug abuse using a four-point scale (never to often); scores range from 18 to 72. It showed adequate reliability and validity for identifying problem substance use in the original sample (Winters, 1992). The internal consistency for the study sample was 0.94.
Connectedness
Perception of connectedness was measured with items from the Perceived Emotional/Personal Support Scale (PEPPS) (Slavin, 1991), which assesses the degree to which respondents perceive their relationships as close, confiding, satisfying, and supportive. Participants listed initials of up to three people in each relationship domain (family members, friends, and non-family adults) and, using a four-point scale ranging from “hardly at all” to “very much, rated how much they talk to each person about personal concerns, how close they feel to the person, and how satisfied they are with the help and support the person gives them. Three connectedness subscales corresponding to each relationship domain were created by averaging all ratings within each relationship category, with higher scores indicating greater connectedness. PEPPS has reasonably high test-retest reliability and internal consistency for the subscales (.83 for family, .91 for peer, and .89 for non-family adult) in an adolescent sample (Slavin, 1991). The internal consistency in this sample was 0.84 and 0.85 for family and peer connectedness, respectively.
Family Psychiatric History
The Family History Screen (FHS) (Weissman et al., 2000) was used to assess psychiatric histories of adolescent' biological parents. Information was obtained from a biological parent or legal guardian. The FHS has 24 items and has demonstrated acceptable validity and reliability. A dichotomous variable indicative of parental psychopathology was created based on positive responses to two questions asking if either parent:(1) “ever had an emotional problem or mental illness” and (2) “had ever sought treatment with a psychiatrist, psychologist, social worker, doctor, or other health professional because of a mental health problem.” Chronbach alpha for these FHS items is 0.80 for fathers and 0.78 for mothers.
History of Physical and Sexual Abuse
History of physical and sexual abuse was assessed with two items from the Schedule for Affective Disorders and Schizophrenia for School-Age Children (KSADS-PL) (Kaufman et al., 1997). More specifically, the items were drawn from the KSADS-PL Post-Traumatic Stress Disorder module including screening questions about experience of different traumatic events. KSADS-PL is a structured diagnostic interview based on the DSM-IV. Interviewers were trained mental health professionals who completed 20 hours of training in KSADS-PL; inter-rater reliability was established with a senior diagnostician prior to study onset. Each of the two abuse history variables was dichotomous.
Data Analysis
Latent class growth modeling (LCGM) was used to identify distinct latent trajectories of suicidal ideation across time (4 time points: baseline, 3-, 6-, and 12- months after hospitalization) as well as predictors of belonging to each latent growth class. Data were analyzed using the PROC TRAJ procedure (Jones & Nagin, 2007; Jones, Nagin, & Roeder, 2001) in SAS (version 9.2). This analytic approach identifies different latent trajectory classes, where individuals in a given class follow a distinct pattern of change over time, and simultaneously examines predictors of class membership within the same modeling framework. Unlike standard growth modeling procedures, this analysis does not assume a particular type or number of trajectories a priori but rather examines what trajectory classes are in the available data. In addition, it does not expect that individuals change in the same direction across time; instead, participants are allowed to follow different growth patterns with varying strength and direction of change over time, forming discrete trajectory classes (Andruff, Carraro, Thompson, Gaudreau, & Louvet, 2009).
We initially fitted models without any risk factors included to explore possible trajectory classes (allowing for linear, quadratic, or cubic trends in any given class) to identify the best-fitting and most parsimonious preliminary model. The Bayesian information criterion (BIC) was used to select the best fitting model from a series of models including different numbers of trajectories. BIC performs very well as an indicator for deciding on the number of classes in mixture modeling (Nylund, Asparouhov, & Muthen, 2007). We then simultaneously entered into the model key risk and protective factors measured at hospitalization (sex, history of multiple suicide attempts, depressive symptoms, substance use, externalizing problems, hopelessness, social connectedness measured separately for family and friends, parental psychiatric history, and physical and sexual abuse history). These risk factors were entered to determine predictors of membership in the identified trajectory groups. To minimize multicolinearlity, all continuous predictors were centered. Given that the original sample came from an intervention study, we also controlled for the potential effect of intervention; however, the intervention had only a modest positive effect on suicidal ideation that was time-limited (found for multiple suicide attempters during the initial 6 weeks after hospitalization) and no effect on the likelihood of suicide attempt (King et al. 2009).
To obtain the most parsimonious model, backward selection was used by deleting the least significant risk factors one at a time, while including and then leaving out sex (due to there being more girls than boys; however, there was no difference between models with and without gender included). The significance level was set at p < 0.05, and multi-parameter Wald tests implemented in PROC TRAJ were used to examine the omnibus importance of a given risk factor in determining overall class membership.
To examine the degree to which the distinct trajectory groups identified in the LCGM were associated with the likelihood of suicide attempts and psychiatric rehospitalization during the follow-up, logistic regression was used. In both models, sex, multiple attempt history, and treatment group were entered in the first step of logistic regression, trajectory group was entered in the second step, and each two-way interaction between the latent group variable and sex and then multiple attempt status was entered in step 3. Intervention group was included as a covariate but was removed from the final model because it was not a significant predictor and results did not vary with it in the models.
Results
Characteristics of the Sample
Baseline and follow-up SIQ scores, in addition to sample size at each assessment time point, are provided in Table 1. Female adolescents had significantly higher SIQ scores than males at each assessment time point, and adolescents with multiple suicide attempt histories also tended to have higher SIQ scores with the exception of the 12-month assessment time point. The following are means (M) and standard deviations (SD) of additional baseline characteristics: depressive symptoms (M=60.85; SD=12.97); externalizing problems (M=21.40; SD=9.69); substance abuse (M=28.15; SD=11.57); hopelessness (M=8.74; SD=5.78); family connectedness (M=8.29; SD=2.12); and friend connectedness (M=9.90; SD=1.90). History of mental health problems was endorsed for mothers of 160 (43%) participants and for fathers of 103 (27%) adolescents; for 55% of adolescents (n = 207), at least one parent had a history of mental health problems. History of physical abuse was reported by 75 (20%) of the sample while sexual abuse was reported by 85 (23%) of participants. Prior to baseline, 91 (24%) of adolescents had not attempted suicide, 135 (36%) had made one attempt, and 150 (40%) had a history of two or more attempts. In addition, 63 adolescents (17%) made at least one suicide attempt during the follow-up; adolescents with multiple attempt histories were more likely to attempt suicide (23% vs. 14%), χ2 (1, N=354) = 4.27, p = 0.04. Moreover, 135 (36%) of adolescents were psychiatrically rehospitalized at least once during the follow-up; these adolescents were more likely to have history of multiple suicide attempts (54% vs. 40%), χ2 (1, N=294) = 5.43, p=0.02. Sex did not differentiate who attempted suicide or was rehospitalized during the follow-up.
Table 1. Suicidal ideation at baseline and follow-up for total sample and subgroups defined by sex and multiple suicide attempt status.
| Overall | Sex | Multiple Attempt Status | |||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| M (SD) | Females M (SD) | Males M (SD) | pa | No M (SD) | Yes M (SD) | pa | |
| Suicidal Ideation | |||||||
| baseline | (n=376) 46.53 (20.87) | (n=272) 47.64 (21.01) | (n=104) 43.63 (20.30) | 0.09 | (n=226) 43.60 (20.84) | (n=150) 50.95 (20.19) | 0.001 |
| 3 months | (n=341) 22.28 (17.83) | (n=244) 24.44 (18.93) | (n=97) 16.84 (13.33) | <0.001 | (n=205) 20.32 (16.73) | (n=136) 25.23 (19.07) | 0.02 |
| 6 months | (n=313) 20.09 (16.50) | (n=224) 21.55 (16.74) | (n=89) 16.40 (15.36) | 0.01 | (n=191) 18.18 (14.98) | (n=122) 23.07 (18.30) | 0.01 |
| 12 months | (n=345) 17.06 (14.04) | (n=252) 18.02 (14.61) | (n=93) 14.46 (12.06) | 0.02 | (n=214) 16.57 (13.61) | (n=131) 17.86 (14.74) | 0.42 |
Notes:
Two-sample t-test assuming unequal variances (two-sided)
Latent Class Growth Models
The best fitting model included three distinct classes (BIC: -5547.88), providing a better fit relative to models with a different number of classes, such as two- (BIC: -5600.73) or four-class models (BIC: -5548.81). As shown in Figure 1, the three distinct latent groups were: (1) a quadratic trend group with sub-clinical suicidal ideation (n=119; 31.6%); (2) a cubic trend group with high suicidal ideation at hospitalization but sharp decline three months later (n=216; 57.4%); and (3) a linear trend group with high suicidal ideation at baseline that was elevated throughout the follow-up (n=41; 10.9%). There were 77 females (64.7%) and 42 males (35.3%) in Group 1,161 females (74.5%) and 55 males (25.5%) in Group 2, and 34 females (82.9%) and 7 males (17.1%) in Group 3. There were 34 (28.6%), 94 (43.5%), and 22 (53.7%) multiple suicide attempters in Group 1, 2, and 3, respectively.
Figure 1. Latent trajectory classes.
Note: SIQ=Suicidal Ideation Questionnaire
Bivariate Analysis
Several risk and protective factors were added to the model to identify predictors of latent growth class membership. Almost all predictors were significant in bivariate analyses: sex (F=3.62, p=0.03); multiple suicide attempt status (F=5.59, p=0.004); depressive symptoms (F=18.65, p<0.0001); externalizing problems (F=11.12, p<.0001); hopelessness (F=18.03, p<.0001); substance abuse (F=4.08, p=0.02); history of physical abuse (F=3.32, p=0.04) and history of sexual abuse (F=3.43, p=0.03). Parental history of mental health problems, connectedness with family, and connectedness with friends were not statistically significant. We also adjusted for potential effect of the intervention; it was a non-significant predictor.
Table 2 shows the relative importance of the significant bivariate predictors in differentiating between trajectory classes. Relative to Group 2, Group 1 membership was associated with less severe baseline depressive symptoms, externalizing problems, hopelessness, and substance abuse in addition to lower likelihood of being female, history of multiple suicide attempts, and history of sexual abuse. The same pattern was observed when comparing adolescents in Group 1 relative to Group 3, however substance abuse and history of abuse history no longer differentiated these two groups. Relative to Group 3, membership in Group 2 was associated with less severe baseline hopelessness and lower likelihood of physical abuse history.
Table 2. Bivariate predictors of latent trajectory class membership.
| Group 1 relative to Group 2 | Group 1 relative to Group 3 | Group 2 relative to Group 3 | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Variables | B (SE) | p | B (SE) | p | B (SE) | p |
| Sex (male) | 0.52 (0.31) | 0.01 | 1.33 (0.54) | 0.01 | 0.82 (0.54) | n.s. |
| Multiple attempters (yes) | −0.80 (0.30) | 0.01 | −1.28 (0.43) | 0.003 | −0.49 (0.41) | n.s. |
| Depressive symptoms | −0.08 (0.01) | <0.001 | −0.10 (0.02) | <0.001 | −0.02 (0.02) | n.s. |
| Externalizing problems | −0.09 (0.02) | <0.001 | −0.08 (0.02) | 0.001 | 0.01 (0.02) | n.s. |
| Hopelessness | −0.24 (0.05) | <0.001 | −0.35 (0.06) | <0.001 | −0.11 (0.04) | 0.01 |
| Substance abuse | −0.04 (0.02) | 0.01 | −0.01 (0.02) | n.s | 0.03 (0.02) | 0.08 |
| Physical abuse history (yes) | −0.21 (0.37) | n.s. | −0.11 (0.45) | 0.01 | −0.90 (0.42) | 0.03 |
| Sexual abuse history (yes) | −1.05 (0.40) | 0.01 | −0.88 (0.51) | 0.09 | 0.18 (0.44) | n.s. |
Notes: Group 1 = Subclinical ideators; Group 2 =Elevated but rapidly declining; Group 3 = Chronically elevated; Reference group in paranthases; Family connectendess, peer connectedness, and parental psychiatric history were not significant predcitors of latent class membership
Multivariate Analysis
All predictors and intervention group were subsequently entered into a full model. Backward selection was used to simplify the model by deleting the least significant risk factors one at a time to obtain the most parsimonious model; there was no difference between models with and without sex and intervention group included. Using multi-parameter Wald tests to examine the omnibus importance of a given risk factor in determining overall class membership, the following were significant predictors of class membership and were included in the final model (see Table 3): depressive symptoms (F=8.17, p<0.001); externalizing problems (F=6.11, p=0.002); and hopelessness (F=15.73, p<0.0001). As described in Table 3, relative to Group 1, participants with more severe baseline depressive symptoms, externalizing problems, and hopelessness were more likely to follow the Group 3 trajectory. Similarly, the same three predictors differentiated Group 2 from Group 1, with more severe scores predicting membership in Group 2 relative to Group 1. However, the only predictor that differentiated membership in Group 3 relative to Group 2 was more severe hopelessness; the more severe hopelessness at baseline, the more likely adolescents were to follow the trajectory of Group 3.
Table 3. Multivariate predictors of latent trajectory class membership.
| Latent SI Trajectory | Baseline Predictors | B | SE (B) | p |
|---|---|---|---|---|
| (Group 1 as reference) | ||||
| Group 2 (Elevated and Fast Declining) | Depressive symptoms | 0.06 | 0.02 | <0.001 |
| Externalizing problems | 0.08 | 0.02 | <0.001 | |
| Hopelessness | 0.20 | 0.04 | <0.001 | |
| Group 3 (Chronically Elevated) | Depressive symptoms | 0.07 | 0.02 | <0.001 |
| Externalizing problems | 0.07 | 0.03 | 0.02 | |
| Hopelessness | 0.31 | 0.06 | <0.001 | |
|
| ||||
| Latent SI Trajectory | Baseline Predictors | B | SE (B) | p |
|
| ||||
| (Group 3 as reference) | ||||
| Group 2 (Elevated and Fast Declining) | Depressive symptoms | −0.01 | 0.02 | n.s |
| Externalizing problems | 0.02 | 0.02 | n.s | |
| Hopelessness | −0.11 | 0.04 | 0.01 | |
Notes: SI=Suicidal ideation; N=370
Logistic Regression Models
Suicide Attempt
Overall, the latent trajectory group variable was a significant predictor of suicide attempts at follow-up (p=0.01), over and above multiple suicide attempt history and sex, demonstrating incremental validity (χ2 = 9.26, p=0.01). As shown in Table 4, relative to Group 1, Group 3 was associated with a four-fold increase in likelihood of a suicide attempt [(OR=4.15; CI=1.65, 10.44), p=0.002]. Adolescents in Group 3 were also approximately 2 times more likely to make a suicide attempt compared to adolescents in Group 2 (OR=2.29; CI=1.08, 4.85), p=0.03. In contrast, adolescents in Group 2 were not more likely to make a suicide attempt relative to Group 1. The effect of trajectory group was not moderated by history of multiple suicide attempts. Due to a limited sample size of males in Group 3 with follow-up suicide attempt data, we did not have sufficient variability to fully examine if sex was a significant moderator.
Table 4. Logistic regression predicting post-hospitalization suicide attempts and rehospitalization.
| Suicide Attempta | Psychiatric Rehospitalizationb | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Variables | Odds ratio | CI (lower, upper) | p | Odds ratio | CI (lower, upper) | p |
| Sex (female) | 0.85 | (0.45, 1.61) | n.s | 1.00 | (0.57, 1.75) | n.s |
| Multiple Attempters (yes) | 1.61 | (0.91, 2.83) | n.s | 1.37 | (0.82, 2.29) | n.s |
| Latent SI Trajectories | ||||||
| (Group 1) | ||||||
| Group 2 | 1.81 | (0.88, 3.74) | n.s | 3.52 | (1.93, 6.40) | <0.001 |
| Group 3 | 4.15 | (1.65, 10.44) | 0.002 | 11.20 | (4.33, 29.01) | <0.001 |
| (Group 2) | ||||||
| Group 3 | 2.29 | (1.08, 4.85) | 0.03 | 3.23 | (1.37, 7.69) | 0.008 |
Notes: SI=Suicidal ideation; Reference group in parentheses;
N=350;
N=289
Psychiatric Rehospitalization
The latent trajectory group variable was also a significant predictor of psychiatric rehospitalization (p<0.001), over and above multiple suicide attempt history and sex, demonstrating incremental validity (χ2 = 38.69, p<0.001). Relative to Group 1, Group 3 was associated with an 11-fold increase in likelihood of being psychiatrically rehospitalized during the follow-up [(OR=11.20; CI=4.33, 29.01), p<0.001]. Adolescents in Group 3 were also approximately three times more likely to be rehospitalized compared to those in Group 2 [(OR=3.23; CI=1.37, 7.69), p<0.008]. Unlike what we observed for suicide attempts, adolescents in Group 2 were 3.5 times more likely to be rehospitalized relative to Group 1 [(OR=3.52; CI=1.93, 6.40), p<0.001]. The effect of trajectory group was not moderated by multiple suicide attempt history. Again, due to limitations in sample size, we were not able to examine if sex was a moderator.
Discussion
We examined a longitudinal course of suicidal ideation among suicidal adolescent inpatients followed for one year. We hypothesized that these adolescents would have different trajectories of suicidal ideation, as opposed to a single course of ideation that assumes change in the same direction across time as has been examined previously (Prinstein, et al., 2008). To the best of our knowledge, this is the first study that has examined district trajectories of suicidal ideation, and their impact on suicide attempts and rehospitalizations, in a sample of inpatient suicidal adolescents. Consistent with our expectations, the course of suicidal ideation post hospitalization was not uniform for all adolescents but was better represented by three distinct trajectories.
The most common trajectory was characterized by high suicidal ideation at the time of hospitalization, which rapidly declined below clinical levels within three months of hospitalization. The second most common trajectory was characterized by a course of elevated suicidal ideation at time of hospitalization, but at sub clinical levels, that also decreased during the follow-up, with the most striking decline again occurring within three months of hospitalization. This pattern of substantial decrease in suicidal thinking after hospitalization is consistent with other studies of adolescent inpatients showing a decrease in suicidal ideation shortly after hospitalization (King, et al., 2009; Prinstein, et al., 2008). However, one group of authors (Prinstein, et al., 2008) also reported a gradual reemergence of suicidal ideation between nine and eighteen months after hospitalization. Even though our study did not have an additional assessment between months six and 12, the trend across the trajectory groups in our study indicates a pattern of relatively stable or decreasing ideation that did not increase at month 12 as might be expected based on previous results. The difference in the sample composition, wherein the current study focused on adolescents with a recent acute suicidal episode while the Prinstein et al.'s study also included non-suicidal inpatients, could be accounting for this discrepancy.
A key finding in our study was that a smaller, but significant, proportion of adolescents followed a trajectory characterized by persistent or chronic suicidal ideation. Adolescents in this group experienced similarly high levels of suicidal ideation at baseline as the youths following the fast declining trajectory, but their rate of decline was significantly slower. In fact, the severity of suicidal ideation characterizing the chronic group was significantly elevated through month six of the follow-up and was not far below clinical levels even 12 months after hospitalization. One possible pathway for persisting suicidal thoughts may be cognitive vulnerability characterized by hopelessness. High level of hopelessness was the only factor differentiating the chronic ideation group from the elevated but fast declining group. The idea that holding negative expectations about the future may be maintaining suicidal thoughts is also supported by a previous study of depressed psychiatric adult patients, where declines in hopelessness preceded declines in suicidal ideation (Sokero et al., 2006). It is also possible that enduring suicidal thoughts may be maintained by a related ruminative process that prolongs negative mood and impedes faster declines in suicidal thinking. Indeed, rumination, or tendency to repeatedly think about one's distress and associated circumstances, is associated with increases in suicidal ideation and also longer and more severe depressed mood (Smith & Alloy, 2009).
Adolescents in the chronic trajectory group were significantly more likely than teens in the other two groups to attempt suicide. In contrast, adolescents in the fast declining group were no more likely to attempt suicide than teens in the subclinical group. In addition, of significance is that trajectory group membership uniquely contributed to suicide attempts over and above a key risk factor, history of multiple suicide attempts, demonstrating incremental validity. An interesting question is whether prolonged suicidal thinking can habituate a person toward suicidal behavior, much like suicide attempts and other painful and fearsome experiences have been proposed to do by way of acquired capacity for suicidal behavior, a key component of the Interpersonal-Psychological Theory of Suicidal Behavior (Joiner, 2005; Van Orden et al., 2010). Acquired capacity for suicidal behavior is conceptualized by the theory as fearlessness about physical pain and death itself acquired through repeated risky behaviors or painful and provocative experiences (e.g., non-suicidal self-injury, abuse) that habituate a person toward self-injury and suicidal behavior. The theory proposes that acquired capacity for suicide erodes the basic human instinct of self-preservation, thus making suicidal behavior more likely. It is possible that prolonged rehearsal of suicidal thoughts lowers the threshold for engaging in suicidal behavior via a similar process of habituation that produces acquired capacity.
Adolescents in the chronic suicidal ideation group were also more likely to be psychiatrically rehospitalized during the follow-up relative to adolescents in the subclinical and the fast declining groups. In addition, when comparing the fast declining with the subclinical group, the former had greater odds of being psychiatrically rehospitalization. Although adolescents in the fast declining group were no more likely to attempt suicide than the subclinical group, they nevertheless experienced more severe suicidal ideation at baseline and throughout the follow-up, which might have rendered them more likely to experience psychiatric crises requiring hospitalization. Unfortunately, we were unable to explore gender as a moderating variable for attempts and rehospitalizations due to the limited sample size of males in the chronic group. This question deserves more attention in future research. However, we found that the effect of trajectory group membership on suicide attempts or rehospitalization did not vary based on history of multiple suicide attempts. This finding highlights that all adolescents hospitalized for acute suicide risk with persisting suicidal thoughts are at high-risk for psychiatric crises regardless of previous suicide attempt history.
Finally, we explored which baseline risk and protective factors differentiated adolescents following the distinct trajectories. This information could contribute to identifying adolescents who might experience a more persistent course of suicidal ideation after hospitalization and who are more at risk for subsequent psychiatric crises. Almost all baseline factors considered were significant predictors in bivariate analyses. However, only depressive symptoms, externalizing problems, and hopelessness remained significant when all predictors were considered simultaneously. In general, higher scores on these predictors were associated with higher initial levels of ideation and more severe suicidal ideation trajectories. However, as already described, the only baseline predictor that differentiated the fast declining and chronic ideation groups was high level of hopelessness. One possible explanation for why some established risk factors in this study (e.g., social connectedness) did not predict trajectory group membership is the difficulty of distinguishing high-risk subgroups within an already high-risk population of suicidal adolescents, even based on well-documented risk factors (Yen et al., 2013). Moreover, according to the Interpersonal-Psychological Theory of Suicidal Behavior (Joiner, 2005; Van Orden et al., 2010), suicidal desire, which may manifest as suicidal ideation, arises from thwarted belongingness (e.g., low levels of social connectedness) and perceived burdensomeness. As such, it is possible that social connectedness in combination with perceived burdensomeness might have had a greater impact on suicidal ideation trajectories.
Implications
The present findings have important implications for identifying and intervening with adolescents most at risk for suicidal crises post hospitalization. Our findings suggest that suicidal ideation at the time of hospitalization may not be an adequate marker of suicide attempt risk and highlight the limitations of considering average changes in suicidal ideation; These approaches can overlook subgroups of suicidal adolescents who are most vulnerable to suicidal crises after hospitalization. The most common patterns of suicidal ideation are characterized by a decreasing trend in ideation, with the most significant decrease occurring within the first three months after hospitalization. This is consistent with average scores of suicidal ideation at each follow-up time point, showing a significant decline in ideation at three months and continuing to decrease thereafter, although less drastically. However, adolescents most likely to attempt suicide and be rehospitalized were similar to the most average group at hospitalization, but followed a distinct trajectory of persisting suicidal ideation, highlighting the importance of identifying and intervening with adolescents vulnerable to this pattern of ideation.
Our findings also have significant relevance for the critical need to closely monitor persisting suicidal ideation among recently discharged psychiatric inpatients as it may place these youths at an especially high risk for suicide attempts. In addition, the impact of prolonged suicidal ideation and associated suicidal crises may have negative effects on important developmental opportunities in the social, emotional, and cognitive domains that are critical to the adolescent developmental period. Our data suggests that one possible pathway for addressing these adolescents' vulnerability to persisting suicidal thinking is by way of reducing their sense of hopelessness. It is also possible that persisting suicidal ideation and higher levels of hopelessness are indicative of an underlying cognitive vulnerability, such as tendency to ruminate, that ultimately renders these youths more at risk for suicidal behavior. More research considering mechanisms that maintain suicidal ideation is needed to inform how to improve these youths' post-hospitalization functioning.
It is noteworthy that the majority of adolescents who experienced a significant decrease in suicidal ideation within three months of hospitalization continued to report sub clinical levels of suicidal thoughts for the duration of the follow-up. Although the rapidly declining group had a lower risk of suicide attempts, they nevertheless were at risk for psychiatric rehospitalizations. It is possible that the presence of even less severe suicidal thinking following hospitalization places these youths at risk for future psychiatric crises warranting stabilization. As such, continued monitoring of all previously suicidal adolescents is recommended. In addition, our findings suggest that addressing key vulnerability factors that predict the course of suicidal ideation, particularly hopelessness, could shorten the duration of severe suicidal thoughts after hospitalization and thus may prevent continued suicidal crises. With relatively few longitudinal studies having examined hopelessness in psychiatrically hospitalized adolescents, more research attention is needed in this area.
Study Limitations
There are several important limitations of this study. The predominantly female and Caucasian sample from one region of the United States has limited generalizability to other adolescent groups. In addition, participants were psychiatrically hospitalized suicidal adolescents and findings may not apply to adolescents from outpatient clinics or from the community or to adolescents with high levels of suicidal ideation who were not hospitalized; these adolescents might follow different trajectories or their distribution on the trajectories might be different than found in this study. However, due to the high-risk nature of this population and its vulnerability to suicidal crises, the study's focus on hospitalized suicidal adolescents is also its strength. Another limitation is that we did not examine additional potentially important predictors of trajectory groups. In particular, due to limited data, we were unable to fully examine sex as a predictor and we did not examine the influence of non-suicidal self-injury (NSSI). NSSI is an important correlate of suicidal behavior (e.g., Nock, Joiner, Gordon, Lloyd-Richardson, & Prinstein, 2006). Future studies should address this gap and explore additional predictors of suicidal ideation trajectories. More diverse adolescent samples should also be utilized in future work to explore the role of demographic variables such as age and race/ethnicity. The present study also has some measurement limitations: a) we used a brief screen to assess family psychiatric history that relied on one informant (usually the mother), did not assess diagnostic criteria, did not differentiate between different forms of mental illness, its timing or severity, or which parent had the mental illness; b) the measure of externalizing problems was based on youth self-report, which might have underestimated the extent of these problems. Finally, the degree to which subclinical suicidal ideation of the rapidly declining trajectory group might have been inflated at follow-up is uncertain. More specifically, one of the answer choices for the suicidal ideation measure, “I had this thought before but not in the past month,” makes it difficult to assess the exact timing of suicidal ideation and whether or not it occurred between assessment time points (e.g. within last six weeks) or in more distant past. Despite these limitations, this study has addressed an important gap in the literature and has important strengths including a prospective design and a large sample of acutely suicidal adolescents.
Conclusion
The majority of adolescents with elevated suicidal ideation at baseline experienced a significant decline in suicidal thoughts within three months after hospitalization; however, a significant proportion of youths continued to experience high levels of ideation throughout the entire follow-up. These teens were at the highest risk of attempting suicide and psychiatric rehospitalization, even when suicide attempt history was taken into account. Hopelessness emerged as a key predictor of persisting suicidal ideation, highlighting its potential role in facilitating declines in suicidal thinking post hospitalization. Results suggest that severity of suicidal ideation at the time of hospitalization may not be an adequate marker for subsequent suicidal crises. Instead, it may be important to identify adolescents who are vulnerable to persisting suicidal ideation, as they are at the highest risk for suicide attempts.
Acknowledgments
The authors gratefully acknowledge Sanjeev Venkataraman, M.D., and Paul Quinlan, M.D., for administrative and risk management support; and Anne Kramer, MSW, ACSW, Barbara Hanna, Ph.D., and Lois Weisse, R.N., for project management. We also thank our research staff, adolescent inpatient staff, and the adolescent participants and their parents and guardians. Special acknowledgements are due to Brady West, Ph.D. for his statistical consultation. Support for this project was provided by National Institute of Mental Health awards (R01 MH63881, K24MH77705) to Cheryl King, Ph.D.
Contributor Information
E.K. Czyz, Email: ewac@umich.edu.
C.A. King, Email: kingca@umich.edu.
References
- Achenbach TM. Manual for the Youth Self-Report and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Andruff H, Carraro N, Thompson A, Gaudreau P, Louvet B. Latent Class Growth Modeling: A Tutorial. Tutorials in Quantitative Methods for Psychology. 2009;5(1):11–24. [Google Scholar]
- Beck AT, Steer RA. Beck Hopelessness Scale Manual. San Antonio, TX: Psychological Corporation; 1988. [Google Scholar]
- Borowsky IW, Ireland M, Resnick MD. Adolescent suicide attempts: risks and protectors. Pediatrics. 2001;107:485–493. doi: 10.1542/peds.107.3.485. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry. 2006;47:372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS). National Center for Injury Prevention and Control. 2012a Available at: http://www.cdc.gov/injury/wisqars/index.html.
- Centers for Disease Control and Prevention. Youth Risk Behavior Survailance— United States, 2011. Morbidity and Mortality Weekly Report. 2012a;61(No. 4) [PubMed] [Google Scholar]
- D'Eramo KS, Prinstein MJ, Freeman J, Grapentine WL, Spirito A. Psychiatric diagnoses and comorbidity in relation to suicidal behavior among psychiatrically hospitalized adolescents. Child Psychiatry & Human Development. 2004;35:21–35. doi: 10.1023/b:chud.0000039318.72868.a2. [DOI] [PubMed] [Google Scholar]
- Emslie GJ, Rush AJ, Weinberg WA, Kowatch RA, Hughes CW, Carmody T, Rintelmann J. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Archives of General Psychiatry. 1997;54:1031–1037. doi: 10.1001/archpsyc.1997.01830230069010. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Suicidal behaviour n adolescence and subsequent mental health outcomes in young adulthood. Psychological Medicine. 2005;35:983–993. doi: 10.1017/s0033291704004167. [DOI] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Reboussin BA, Reboussin DM, Frazier PH, Harris AE. Cognitive risk factors and suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:91–99. doi: 10.1097/00004583-200101000-00021. [DOI] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Reboussin DM, Reboussin BA, Frazier PH, Kelley AE. Suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study of risk during the first 5 years after discharge. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:660–671. doi: 10.1097/00004583-199906000-00012. [DOI] [PubMed] [Google Scholar]
- Herba CM, Ferdinand RF, van der Ende J, Verhulst FC. Long-term associations of childhood suicide ideation. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46:1473–1481. doi: 10.1097/chi.0b013e318149e66f. [DOI] [PubMed] [Google Scholar]
- Huth-Bocks AC, Kerr DC, Ivey AZ, Kramer AC, King CA. Assessment of psychiatrically hospitalized suicidal adolescents: self-report instruments as predictors of suicidal thoughts and behavior. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46:387–395. doi: 10.1097/chi.0b013e31802b9535. [DOI] [PubMed] [Google Scholar]
- Joiner T. Why people die by suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Jones BL, Nagin DS. Advances in Group-Based trajectory modeling and an SAS procedure for estimating them. Sociological Methods & Research. 2007;35:542–571. [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research. 2001;29:374–393. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- King CA. Suicidal behavior in adolescence. In: Marris R, Silverman M, Canetto S, editors. Review of Suicidology. New York: Guilfortd Press; 1997. pp. 61–95. [Google Scholar]
- King CA, Hovey JD, Brand E, Ghaziuddin N. Prediction of positive outcomes for adolescent psychiatric inpatients. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:1434–1442. doi: 10.1097/00004583-199710000-00026. [DOI] [PubMed] [Google Scholar]
- King CA, Jiang Q, Czyz EK, Kerr DCR. One-year predictive validityof suicidal ideation for suicide attempts among adolescent psychiatric inpatients under review. [Google Scholar]
- King CA, Kerr DC, Passarelli MN, Foster CE, Merchant CR. One-year follow-up of suicidal adolescents: parental history of mental health problems and time to post-hospitalization attempt. Journal of Youth and Adolescence. 2010;39:219–232. doi: 10.1007/s10964-009-9480-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Klaus N, Kramer A, Venkataraman S, Quinlan P, Gillespie B. The Youth-Nominated Support Team-Version II for suicidal adolescents: randomized controlled intervention trial. Journal of Consulting and Clinical Psychology. 2009;77:880–893. doi: 10.1037/a0016552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Merchant CR. Social and interpersonal factors relating to adolescent suicidality: a review of the literature. Archives of Suicide Research. 2008;12:181–196. doi: 10.1080/13811110802101203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Segal H, Kaminski K, Naylor MW, Ghaziuddin N, Radpour L. A prospective study of adolescent suicidal behavior following hospitalization. Suicide and Life-Threatening Behavior. 1995;25:327–338. [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Psychosocial risk factors for future adolescent suicide attempts. Journal of Consulting and Clinical Psychology. 1994;62:297–305. doi: 10.1037//0022-006x.62.2.297. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Adolescent suicide ideation and attempts: Prevalence, risk factors, and clinical implications. Clinical Psychology Science and Practice. 1996;3:25–46. [Google Scholar]
- Miranda R, Scott M, Hicks R, Wilcox HC, Harris Munfakh JL, Shaffer D. Suicide attempt characteristics, diagnoses, and future attempts: comparing multiple attempters to single attempters and ideators. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:32–40. doi: 10.1097/chi.0b013e31815a56cb. [DOI] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results From the National Comorbidity Survey Replication Adolescent Supplement. Journal of the American Medical Association Psychiatry. 2013;70:300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Joiner TE, Jr, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Research. 2006;144:65–72. doi: 10.1016/j.psychres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthen BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14:535–569. [Google Scholar]
- Poznanski EO, Mokros HB. Children's Depression Rating Scale-Revised (CDRS- R) Los Angeles, CA: Western Psychological Services; 1996. [Google Scholar]
- Prinstein MJ, Nock MK, Simon V, Aikins JW, Cheah CS, Spirito A. Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. Journal of Consulting and Clinical Psychology. 2008;76:92–103. doi: 10.1037/0022-006X.76.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinherz HZ, Tanner JL, Berger SR, Beardslee WR, Fitzmaurice GM. Adolescent suicidal ideation as predictive of psychopathology, suicidal behavior, and compromised functioning at age 30. American Journal of Psychiatry. 2006;163:1226–1232. doi: 10.1176/ajp.2006.163.7.1226. [DOI] [PubMed] [Google Scholar]
- Rueter MA, Holm K, McGeorge CR, Conger RD. Adolescent suicidal ideation subgroups and their association with suicidal plans and attempts in young adulthood. Suicide and Life-Threatening Behavior. 2008;38:564–575. doi: 10.1521/suli.2008.38.5.564. [DOI] [PubMed] [Google Scholar]
- Reynolds WM. Suicidal Ideation Questionnaire: Professional manual. Odessa, FL: Psychological Assessment Resources; 1988. [Google Scholar]
- Reynolds WM. Measurement of suicidal ideation in adolescents; Paper presented at the American Association of Suicidology Annual Conference; Chicago, IL. 1992. [Google Scholar]
- Selby EA, Yen S, Spirito A. Time varying prediction of thoughts of death and suicidal ideation in adolescents: Weekly ratings over 6-month follow-up. Journal of Clinical Child & Adolescent Psychology. 2013;42:481–495. doi: 10.1080/15374416.2012.736356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas C NIMH DISC Editorial Board. DISC-IV Diagnostic Interview Schedule for Children (Youth informant and parent informant interviews): Epidemiologic version. New York: Joy and William Ruane Center to Identify and Treat Mood Disorders, Division of Child Psychiatry Columbia University; 1998. [Google Scholar]
- Shain BN, Naylor M, Alessi N. Comparison of self-rated and clinician-rated measures of depression in adolescents. American Journal of Psychiatry. 1990;147:793–795. doi: 10.1176/ajp.147.6.793. [DOI] [PubMed] [Google Scholar]
- Slavin LA. Validation studies of the PEPSS, a measure of perceived emotional support for use with adolescents. Journal of Adolescent Research. 1991;6:316–335. [Google Scholar]
- Smith JM, Alloy LB. A roadmap to rumination: a review of the definition, assessment, and conceptualization of this multifaceted construct. Clinical Psychology Review. 2009;29:116–128. doi: 10.1016/j.cpr.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokero P, Eerola M, Rytsala H, Melartin T, Leskela U, Lestela-Mielonen P, Isometsa E. Decline in suicidal ideation among patients with MDD is preceded by decline in depression and hopelessness. Journal of Affective Disorders. 2006;95:95–102. doi: 10.1016/j.jad.2006.04.028. [DOI] [PubMed] [Google Scholar]
- Thurber S, Hollingsworth DK. Validity of the Achenbach and Edelbrock Youth Self-Report with hospitalized adolescents. Journal of Clinical Child Psychology. 1992;21:249–254. [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychological Review. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: the family history screen. Archives of General Psychiatry. 2000;57:675–682. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- Winters KC. Personal Experience Screen Questionnaire (PESQ) Manual. Los Angeles, CA: Western Psychological Services; 1991. [Google Scholar]
- Winters KC. Development of an adolescent alcohol and other drug abuse screening scale: Personal Experience Screening Questionnaire. Addictive Behaviors. 1992;17:479–490. doi: 10.1016/0306-4603(92)90008-j. [DOI] [PubMed] [Google Scholar]
- Yen S, Weinstock LM, Andover ES, Sheets E, Selby EA, Spirito A. Prospective predictors of adolescent suicidality: 6 month post hospitalization follow-up. Psychological Medicine. 2013;43:983–993. doi: 10.1017/S0033291712001912. [DOI] [PMC free article] [PubMed] [Google Scholar]