SUMMARY
Migrainous headache is determined by pathogenetic mechanisms that are also able to affect the peripheral and/or central vestibular system, so that vestibular symptoms may substitute and/or present with headache. We are convinced that there can be many different manifestations of vestibular disorders in migrainous patients, representing true different clinical entities due to their different characteristics and temporal relashionship with headache. Based on such considerations, we proposed a classification of vertigo and other vestibular disorders related to migraine, and believe that a particular variant of migraine-related vertigo should be introduced, namely "epigone migraine vertigo" (EMV): this could be a kind of late migraine equivalent, i.e. a kind of vertigo, migrainous in origin, starting late in the lifetime that substitutes, as an equivalent, pre-existing migraine headache. To clarify this particular clinical picture, we report three illustrative clinical cases among 28 patients collected during an observation period of 13 years (November 1991 - November 2004). For all patients, we collected complete personal clinical history. All patients underwent standard neurotological examination, looking for spontaneous-positional, gaze-evoked and caloric induced nystagmus, using an infrared video camera. We also performed a head shaking test (HST) and an head thrust test (HTT). Ocular motility was tested looking at saccades and smooth pursuit. To exclude other significant neurological pathologies, a brain magnetic resonance imaging (MRI) with gadolinium was performed. During the three months after the first visit, patients were invited to keep a diary noting frequency, intensity and duration of vertigo attacks. After that period, we suggested that they use prophylactic treatment with flunarizine (5 mg per day) and/or acetylsalicylic acid (100 mg per day), or propranolol (40 mg twice a day). All patients were again recommended to note in their diary the frequency and intensity of both headache and vertigo while taking prophylactic therapy. Control visits were programmed after 4, 12 and 24 months of therapy. All patients considerably improved symptoms with therapy: 19 subjects (68%) reported complete disappearance of vestibular symptoms, while 9 (32%) considered symptoms very improved. The subjective judgement was corroborated by data from patients diaries. We conclude that EMV is a clinical variant of typical migraine-related vertigo: a migraineassociated vertigo, headache spell independent, following a headache period, during the lifetime of a patient.
KEY WORDS: Headache, Migraine vertigo, Epigone migraine vertigo, Motion sickness, Aura
RIASSUNTO
La cefalea emicranica è determinata da meccanismi patogenetici che possono interessare anche il sistema vestibolare, periferico e/o centrale, quindi la sintomatologia vestibolare può sostituire e/o manifestarsi insieme alla cefalea. Nei pazienti emicranici ci possono essere diverse manifestazioni di natura vestibolare, che rappresentano delle vere entità cliniche, diverse tra loro per le differenti caratteristiche e relazioni temporali con la cefalea. Su questa base abbiamo proposto una classificazione dei disturbi vestibolari correlati all'emicrania, e tra questi dovrebbe essere introdotta una variante particolare, la "vertigine emicranica epigona" (VEE): questa potrebbe essere un equivalente emicranico tardivo, cioè una vertigine di origine emicranica, che comincia tardivamente nella vita e che sostituisce, come equivalente, una cefalea emicranica preesistente. A questo proposito, riportiamo tre casi esemplificativi, scelti tra 28 pazienti selezionati durante un periodo di 13 anni (novembre 1991 – novembre 2004). Per tutti i pazienti è stata raccolta una dettagliata storia clinica. Tutti sono stati sottoposti ad un esame otoneurologico standard, per la ricerca del nistagmo spontaneo-posizionale, evocato da manovre oculari e provocato da stimolazione termica, usando una video-camera a raggi infrarossi. Abbiamo eseguito anche un head shaking test (HST) e un head thrust test (HTT). E' stata valutata l'oculomotricità, con lo studio dei saccadici e dello smooth pursuit. Per escludere altre patologie neurologiche, è stata effettuata una risonanza magnetica nucleare (RMN) dell'encefalo con gadolinio. Durante i tre mesi dopo la prima visita, i pazienti sono stati invitati a compilare un diario, annotandovi la frequenza, l'intensità e la durata degli attacchi vertiginosi. Al termine di tale periodo, gli abbiamo consigliato di usare una terapia di profilassi con flunarizina (5 mg/die) e/o acido acetilsalicilico (100 mg/die), o con propranololo (40 mg x 2/die). Ancora una volta, abbiamo chiesto ai pazienti di annotare sul loro diario la frequenza e l'intensità sia della vertigine che della cefalea durante il trattamento. Le visite di controllo sono state programmate a 4, 12 e 24 mesi dall'inizio della terapia. In tutti i pazienti si è avuto un miglioramento considerevole della sintomatologia: 19 soggetti (68%) hanno riportato la scomparsa completa della sintomatologia vestibolare, mentre 9 (32%) consideravano i loro sintomi notevolmente migliorati, anche se non completamente risolti. Il giudizio soggettivo era supportato dai dati ricavati dai diari dei pazienti. Possiamo concludere che la VEE è una variante clinica della vertigine correlata all'emicrania: una vertigine emicranica, indipendente dalle crisi algiche, che segue il periodo della cefalea, nel corso della vita del paziente.
Introduction
Headache and vertigo are both very common complaints among internal medicine, neurological and neuro-otological patients; nevertheless, the frequency of the clinical association of vertigo and headache among migraine patients is too high to be justified only by chance 1. It is a common opinion 2 that migrainous headache is determined by pathogenetic mechanisms that are also able to affect peripheral and/or central vestibular structures: the consequence is that vestibular disturbances may substitute and/or present with headache.
Therefore, the hypothesis that migraine vertigo (MV) may be a real clinical entity seems, by now, confirmed 3. In fact, during the last decades some sorts of vertigo and dizziness associated with clinical syndromes typical of migrainous patients have been identified.
In 1961 Bickerstaff 4, for first, collected a series of young females complaining of vertigo, staggering and gait ataxia associated with other neurological disturbances like dysarthria, visual symptoms in both eyes, acroparesthesia, cranial nerve impairment and altered sensorium. In such a group of patients, the latter symptoms were followed by severe, occipital, throbbing headache associated with vomiting. This particular clinical picture was called "basilar artery migraine": it is the expression of functional disturbance of the brainstem, cerebellum and occipital cortex as a probable effect of a transient ischaemia in the distribution area of the basilar artery in migrainous subjects.
Basser, in 1964 5, detected a kind of vertigo, typical of childhood, that he named "benign paroxysmal vertigo of childhood". It is characterized by sudden, recurrent brief vertigo attacks associated with nausea and pallor making the patient unable to move, with a serious inability to stand. Vertigo attacks are not associated with headache or impairment of consciousness. Paediatric patients usually have a clear family history for migraine and often develop true migraine headache after adolescence. Precocious vestibular symptoms are therefore considered as "precursors" of a migrainous headache (precocious canalar equivalent).
A similar manifestation is " benign torticollis of infancy", a clinical picture described by Snyder in 1969 6, that develops during the first four years of life in some subjects with a clear family history of migraine. This manifestation seems to represent a "crisis" of the otolithic system induced by biochemical mechanisms of migrainous origin (precocious otolithic equivalent).
In 1979, Slater 7 described a "benign recurrent vertigo of adults", a vestibular syndrome characterized by recurrent spells of sudden and intense vertigo or unsteadiness associated with vagal symptoms. Such vertigo attacks occur in adults with migraine alternating with headache spells. In such patients, therefore, vertigo substitutes headache as migraine without headache, as described by Whitty 8, during the florid period of recurrent painful spells.
The International Headache Society (IHS), in the classification of the "ad hoc committee" of 1988 9, took in account the practical issue of "migraine related vertigo". Vestibular disturbances occurring in patients suffering from migraine are separated in two groups: neuro-otological disorders that are "due" to migraine and those that are "associated" with it. The first group includes: (1) benign paroxysmal torticollis of infancy, (2) benign paroxysmal vertigo in childhood, (3) basilar artery migraine, (4) benign recurrent vertigo in adults and (5) migrainous infarct resulting in vertigo. The second group includes: (1) motion sickness, (2) Menière's disease and (3) benign paroxysmal positional vertigo. On the other hand, both the IHS and the international literature did not overcome this simple subdivision and did not propose an actual classification of vestibular symptoms that can occur in persons with migraine. In the IHS classification of 2004 10 11 only two vestibular syndromes are listed: basilar type migraine and benign paroxysmal vertigo of childhood.
We are convinced that there are many different manifestations of vestibular disorders in patients with migraine, representing true different clinical entities due to their different characteristics and temporal relationship with headache. Based on such characteristics, our group has proposed a classification of vertigo and other vestibular disorders related to migraine 12. Based on clinical experience acquired while evaluating and treating vestibular disorders occurring in patients with migraine, we believe that a particular variant of migraine-related vertigo should be introduced.
In November 1993, a woman affected by migraine without aura that suffered by intense and frequent headache spells since many years came to our attention. She referred that, during her lifetime, headaches began to decrease, while recurrent vertigo developed. In the patient's history, the temporal sequence of the two symptoms was so striking that it came to our immediate attention. During the following years, we encountered other patients complaining of recurrent vertigo after a period of headache had ceased, or that headache was markedly decreased in frequency and intensity.
To obtain a group of patients that was as clinically homogeneous as possible, we adopted rigorous selection criteria to include such patients in our case study.
The similarity of temporal succession of symptoms, typology of headache and vertigo spells, habitus, absence of any other definite vestibular pathology and negativity of general and neurological investigations that we noticed among our patients, lead us to consider such patients homogeneous enough to be grouped into a new nosological entity that we called "Epigone migraine vertigo" (EMV), from "epigonous" a term that means "borne after".
Such a pathology could therefore represent a type of late migraine equivalent that can be defined as a "recurrent vestibular disorder occurring in migrainous subjects, appearing late in their lives, substituting headache spells when the latter disappear or considerably reduce in frequency and strength, when (for women) patients are still in their fertile age or sometimes at menopause".
To clarify this particular clinical picture we report three illustrative clinical cases.
Case 1: GS, female, 41 years old, date of visit 10.02.1995
Motion sickness since the age of 4 years, partially improved after puberty. Springtime vasomotorial rhinitis. No general disorders in personal pathological history. Mother and grandmother with migraine without aura, maternal aunt with migraine with aura.
Headache.
Migraine headache without aura since the age of 20 years. Acute headache spells lasting from 3 to 8 hours, often throbbing, unilateral, with periorbital pain, always with phono/photophobia and nausea. Frequency: 3-5 episodes each month, always during pre-menstrual period. Headache got only partially better using common analgesics, more often ceasing spontaneously with sleep. Maximal intensity and frequency between 20 and 25 years. When the patient was 28, at the time of her first pregnancy, her headache completely disappeared.
Vertigo.
Immediately after her pregnancy, during the 13 years before the visit, the patient started complaining of postural disturbances associated with instability in the upright position and nausea; each episode lasted from 6 to 48 hours, had an acute onset and a complete resolution, without any residual symptoms. Frequency: 2-4 episodes each year. During the month prior to the visit she had 5 episodes of imbalance, associated with nausea and vomiting and inability to stand, lasting 6-12 hours. Such episodes were just a little bit shorter but more intense than the former, and symptoms were worsened by any movement. Postural symptoms often improved with sleep. She came to visit because of worsening of symptoms.
Investigations.
Cerebral magnetic resonance imaging (MRI), high resolution computed tomography (CT) scan, epiaortic Doppler sonography, electroencephalogram (EEG) and serologic tests were normal as were audiometric, vestibular and neurological exams. Audiological and vestibular tests remained negative during the follow-up period.
Therapy.
Vestibular symptoms completely disappeared using migraine prophylactic drugs (acetylsalicylic acid 100 mg plus flunarizine 5 mg per day) during 4 years follow up.
Comments.
Patient suffers from migraine without aura with high familial history. Headache disappeared with pregnancy and vestibular symptoms (imbalance and subjective rotatory vertigo) started immediately after it. The nine months of pregnancy represent, therefore, the free interval during which both symptoms were absent. After this period, migraine headache evolved into migraine-associated vertigo (late equivalent). Absence of other definite vestibular pathologies that could explain symptoms, negativity of audio-vestibular investigations and disappearance of symptoms with migraine prophylaxis confirmed diagnosis of EMV.
Case 2: ER, female, 47 years old, date of visit 24.03.1995
Motion sickness started during early childhood, hypotension since adolescence; no other significant subsequent pathology. Mother and maternal aunt suffered from migraine without aura; a son who suffered from paroxysmal torticollis of infancy at the age of 28 months.
Headache.
Migraine headache since the age of 10 years; acute, throbbing headache crisis, with phono/photophobia and vomiting. Headache worsened with physical activity, it was rarely unilateral, it lasted from 2 to 48 hours and the maximal frequency of spells (2-3 per week) was between the age of 20 and 30 years. Only few episodes were preceded by visual aura involving both eyes (scotomata and flickering lights). Since June 1992 headaches became milder, very rare, only sometimes related with menstrual cycle.
Vertigo.
July 1992: first rotational vertigo with vomiting and inability to stand, lasted 10 hours, started acutely and rapidly ceased without signs. A similar rotational attack, 6 hours long, occurred one month later. Since September 1992, 2-4 episodes per month of marked dizziness associated with nausea and intolerance to standing, lasting from 2 to 4 hours. Nearly half of vestibular crises were preceded by visual aura lasting 10-15 minutes.
Investigations.
Cerebral MRI, epiaortic colour Doppler sonography, EEG and serological tests were normal. Neurologic examination and audiometry were normal. First vestibular testing showed a small amplitude down-beating nystagmus that was more pronounced in the sitting position. With the patient on a left lateral position, there was a small amplitude, persistent, right beating nystagmus. During follow up, after therapy, down-beating nystagmus was even less pronounced, while right-beating positional nystagmus disappeared.
Therapy.
During 2 years prophylactic treatment with acetylsalicylic acid 100 mg plus flunarizine 5 mg, daily, recurrent postural disturbance was no longer present.
Comments.
Patient had migraine with aura (fulfilling IHS criteria) with a clear familial component. She did not suffer from any other otologic or general pathology. Vestibular disturbances appeared immediately after the headache period was almost completely over; between the two symptoms there was no, therefore, any free interval. It has to be remarked that visual aura was more frequent before vertigo than before headache. Using migraine prophylactic treatment, dizziness and postural instability disappeared.
Case 3: AMG, female, 45 years old, date of visit 18.07.1996
Two normal pregnancies in patient's history; marked motion sickness during childhood; hypotension, as a current general pathology. Father suffering from migraine with aura, paternal grandmother and a daughter suffering from migraine without aura.
Headache.
Since puberty the patient suffered from migraine headache, often intense, unilateral and with a periorbital localization; pain was throbbing, accompanied by nausea and photophobia, exacerbated by physical activity.
Headache spells lasted 5-6 hours and were resistant to common analgesics, sometimes withdrawing with vomiting. When headache occurred during the menstrual period it was associated with bilateral aural fullness and tinnitus. Only a few headache spells lasted more than 12 hours. Frequency of attacks: 1-3 episodes each month. Only between the ages of 19 and 25 years did the patient have more than one spell per month. Eighteen months before the visit, at the beginning of the menopausal period, the patient referred a gradual reduction of headache intensity and frequency, until its disappearance.
Vertigo.
Since 18 months, patient suffered from rotational vertigo that, during the first 3 months, were of the subjective type, associated with nausea and lasted from 30 min to 2 hours; vertigo spells occurred more than once a week and were followed by light and diffuse headache that could last many hours.
Investigations.
Cerebral MRI with gadolinium, colour Doppler sonography, serological tests, neurologic examination were negative. Audiometry and vestibular exams were normal both at the first visit and during the followup period.
Therapy.
During 3 years of prophylactic treatment with flunarizine 5 mg BID (she did not receive acetylsalicylic acid because of gastric intolerance) vestibular symptoms practically disappeared; only a light and rare sense of instability, during the menstrual period, persisted.
Comments.
Patient suffered from migraine without aura and had a clear familial component for migraine. She did not suffer from any definite vestibular pathology that could explain vestibular symptoms. Headache gradually decreased at the beginning of the menopausal period, with the appearance of vestibular disturbances. Only during the first three months from the appearance of vertigo were vestibular symptoms followed by light headache. Afterwards, with the worsening of vertigo, the residual headache disappeared. Both headache and vertigo improved with vomiting. The effectiveness of prophylactic treatment confirmed a diagnosis of EMV.
Materials and methods
To have a higher probability to include in our case study only patients suffering from migraine-related vertigo, we adopted the following selection criteria:
subject suffering from migraine as identified by IHS criteria;
recurrent vertigo and/or postural disturbances;
onset of vestibular symptoms after the disappearance (or remarkable reduction) of headache;
absence of audiologic and vestibular symptoms and signs having reference to definite neuro-otological pathologies;
negative neurological examination and cerebral MRI;
absence of any vascular pathology or vascular risk factor;
effectiveness of migraine prophylactic treatment (disappearance or marked reduction of vestibular symptoms);
at least 2 years of follow-up.
Considering these standards for inclusion, we collected 28 patients during an observation period of 13 years, roughly November 1991- November 2004.
Inclusion criteria and purpose of the study were already determined since the first cases, and were maintained during the entire collection period. Therefore, our study was prospective. We collected a homogeneous group of patients sharing some characteristics that are specific for such a pathology.
The strict selection criteria allows us to affirm that patients with a different vestibular pathology would not have been included in the present case study.
For all patients we collected complete personal clinical history, including family, remote and near pathological history. Particular attention was given in collecting the history regarding headache and vestibular disturbances.
We looked into the migrainous habitus searching for migrainous manifestations in infancy (benign vertigo, paroxysmal torticollis and motion sickness).
Firstly, we made us sure that patients suffered from headache fulfilling migraine criteria as stated by the IHS. Afterwards, concerning headache, we determined: a) age of onset, duration and frequency; b) presence or absence of aura; c) family history.
Regarding vestibular symptoms, we determined: a) age of onset; b) type of vestibular symptom (rotational objective or subjective vertigo or postural troubles); c) duration, intensity and frequency of spells; d) presence or absence of associated vagal symptoms; e) temporal trend of symptoms.
Afterwards, we defined the temporal relationships between headache and vertigo periods over the patient's lifetime; we asked patients to point out one of the following possible temporal relationships: a) between headache and vertigo periods there was a symptom free interval; b) the two symptoms came one after the other, without any interval; c) vertigo gradually took place together with headache. Moreover, we asked to females if the passage of one symptom into the other coincided with the menopausal period.
Furthermore, we asked all patients if at the time of the beginning of the period of vertigo their headache was: a) completely vanished; b) residual but reduced; c) only fairly reduced; d) nearly unchanged.
The persistence of a moderately reduced or unchanged headache lead us to exclude such patients from the study. Finally, during follow-up, we asked patients if, using prophylactic treatment, their vestibular symptoms were: a) completely vanished, b) residual but reduced; c) only fairly reduced; d) unmodified. The persistence of an unmodified (or only partially reduced) vertigo led to exclusion from the study.
We also asked patients if they had ever had audiological symptoms such as hearing loss, unilateral or bilateral tinnitus or fullness, together with vertigo or independently of from it.
Oto-microscopy was performed for all patients in addition to pure tone audiometry and impedance testing.
All patients underwent standard neurotological examination. Vestibular spontaneous-positional nystagmus was checked in seven positions (sitting, supine, right side, left side, head hanging, right and left Dix-Hallpike's) using an infrared video camera. Gaze evoked nystagmus was also checked with the same modalities. Moreover, we performed a head shaking test (HST) and a horizontal head thrust test (HTT) to test vestibulo-ocular reflex (VOR) to higher frequencies with respect to caloric stimuli.
Caloric induced nystagmus was investigated using Fitzgerald-Hallpike's technique. To calculate labyrinthine and directional preponderance, we applied Jongkeens' formulae considering, as a reference parameter, the slow phase angular velocity of caloric-induced nystagmus. Reference normative data were those indicated by Baloh 13. Ocular motility was tested looking at horizontal and vertical saccades velocity, accuracy and latency and horizontal and vertical smooth pursuit gain 14. Both ocular motility and caloric nystagmus were recorded using computed electronystamography.
All patients underwent a neurological visit to exclude other significant neurological pathologies that could justify both headache and vertigo. Moreover, for all patients, we carried out haematological workup, especially concerning vascular risk factors, as well as colour Doppler sonography of carotid and vertebral arteries and brain MRI with gadolinium.
During the three months after the first visit, patients were asked to keep a diary noting frequency, intensity and duration of vertigo attacks. In case of crises they should use only symptomatic drugs (antiemetics, anxiolytics).
After that period, we prescribed prophylactic treatment with flunarizine and acetylsalicylic acid. The suggested doses for flunarizine and acetylsalicylic acid were, respectively, 5 mg and 100 mg per day.
If patients could not take acetylsalicylic acid for a gastric or other pathology, they were prescribed only flunarizine at 10 mg per day. On the other hand, if patients had some contraindications to flunarizine (obesity, depression) and/ or significant side effects (i.e. drowsiness), they were treated only with acetylsalicylic acid at 100 mg BID.
Moreover, if patients could not take either drug, we prescribed, as prophylactic therapy, propranolol at 40 mg BID. All patients were again asked to record in their diary the frequency and intensity of both headache and vertigo while taking prophylactic therapy.
Control visits were programmed after 4, 12 and 24 months of therapy. Informed consent was obtained from all patients.
Results
Subjects
Our case study of patients affected by EMV includes 28 subjects (23 females and 5 males): their mean age, at the first visit to our clinic, was 43 years, with a minimal age of 18 and a maximal age of 64 (SD: 11.9, mode: 45). The mean age at the onset of headache was 18 years (min: 8, max: 38; SD 7.4, mode 15); the mean age at the onset of vestibular symptoms was 38 years (min: 16; max 55; SD: 11, mode: 46). Thus, EMV occurs after a mean headache period of 20 years. In more of 70% of patients vertigo started between 26 and 46 years, but among them, in half of cases, its onset peak is concentrated into the fourth decade (40-46 years). There was no difference between females and males concerning the age of onset of headache and vertigo or the interval between the periods of the two symptoms.
Headache
Twenty-two patients (78%) had migraine without aura and 6 (22%) suffered from migraine with aura. No patient suffered from any other type of migraine included in the definitions of the IHS. Among the 6 patients affected by migraine with aura, in one patient visual aura anticipated EMV spells more often than those of headache. In another patient migraine with aura first changed into migraine without aura (roughly along a period of 2 years) and was then substituted by EMV (without aura). Among the remaining 4 patients, as vertigo began headache disappeared together with the aura in three, and it markedly decreased in one.
Twenty-two of 28 patients affirmed to have or to have had motion sickness during their lifetime, at least during infancy. Twenty-five subjects out of 28 had a clear family history of migraine.
Vertigo and dizziness
Vestibular disturbances in our patients were very different in terms of type, duration and frequency. We found that patients suffered both from objective and subjective rotational vertigo and postural imbalance. Vestibular symptoms were very different among subjects, while in the same patient they presented more similar in terms of quality, varying only in duration and intensity. In fact, 17 patients (61%) always reported the same type of vertigo: 10 subjects (36%) had only objective rotational vertigo, 4 (14%) had only postural disturbances and 3 (11%) had only subjective crises of rotational vertigo. In the remaining 11 patients (39%), at least two types of vestibular symptoms were associated; only in three patients did vestibular disturbances manifest with all the three kinds of vestibular symptoms (objective and subjective vertigo and postural disturbance). In any case, objective rotational vertigo, alone or associated, was referred by more than half of patients: in fact, true objective vertigo was reported by 18 patients: vertigo alone, in 10 patients, vertigo alternating with subjective crises or postural imbalance, was seen in 8 subjects.
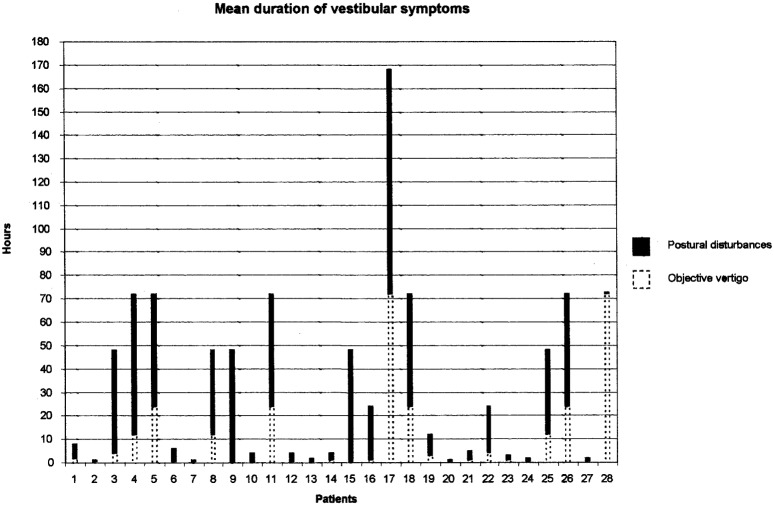
The duration of the individual crisis was highly variable (Fig. 1): objective vertigo lasted, on the average, 15 hours (min 1/2 hour - max 3 days), while postural disturbances usually were longer, with a mean duration of 73 hours (min 1 hour – max 10 days). The mean duration of postural spells was reached by only a few subjects who had particularly prolonged crises. In individual patients also, duration of crises was variable, and was always shorter for objective spells compared to subjective ones. Accompanying vagal symptoms were present in all patients together with stronger crises; they were less severe in 11 patients (only nausea) and more pronounced (nausea and vomiting) in 18 of the 28 subjects.
Fig. 1.
Reported duration of vestibular crisis in our case study: for each patient, the mean duration of postural disturbances (black histogram) and objective vertigo (dotted histogram) is given.
Almost all patients reported that head movements worsened both vestibular and neurovegetative symptoms. Most patients returned to a relative well-being after the attack had ceased; a few subjects (7 of 28) had transient residual unsteadiness for a few days.
The mean frequency of spells (considering period of maximum incidence) varied from a minimum of one crisis every 6 months to a maximum of 5 spells each month. Only 2 patients were diagnosed as having a possible vestibular migraine, whether the other 26 had a diagnosis of Menière's disease, vestibular neuritis, benign paroxysmal positional vertigo and psychogenic vertigo. Twenty of 28 patients complained of kinetosis during adult life, childhood or both, and 17 suffered from hypotension.
Headache versus vertigo
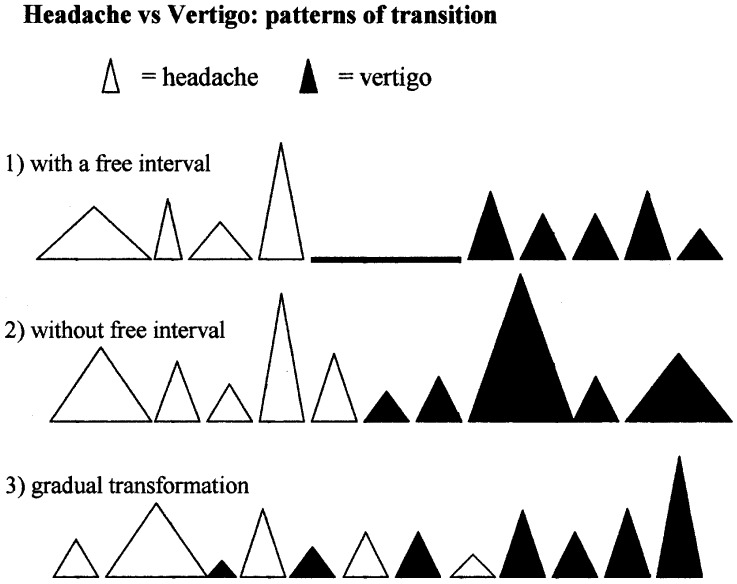
In our case studies, the shift of headache into vestibular symptoms, over a patient's lifetime, occurred according to three different patterns (Fig. 2): 1) with a variable free interval from both symptoms; 2) headache shifted directly into vertigo without a free interval; 3) headache gradually changed into vertigo with a period during which both symptoms are present.
Fig. 2.
Headache vs. vertigo: patterns of transitions of the two symptoms over the course of a lifetime. Height and width of triangles indicate, respectively, the strength and duration of headache or vertigo spells.
Transition with a free interval was reported by 8 patients (28.5%); in one case, the free interval coincided with pregnancy and, in other two, with menopause. Twelve patients (43%) reported the second modality of transformation, i.e. direct transformation of headache into vertigo: in 4 cases transformation occurred during menopause. Finally, 8 patients (28.5%) referred the gradual shift of the two symptoms, sensing a partial overlap. These patients therefore noticed a gradual reduction of headache and, at the same time, the worsening of vestibular disturbances until there persistence (or clear prevalence) of vertigo. Half of these patients noticed that the shift of the two symptoms occurred during menopause.
Among the 23 females in our case study, in 10 cases (43.5%) headache shifted into vertigo at menopause or immediately after it. In one case, such a shift occurred after pregnancy and in the remaining 12 cases (52%) it occurred during the fertile age.
Residual headache
Once headache changed into vertigo, 16 patients (57%) reported that headache completely ceased, while 12 subjects (43%) noticed substantial improvement of this headache (only a light headache often limited to menstrual period) that became a minor disturbance compared with vertigo.
It should be noted that while in the group of patients with gradual transformation of the two symptoms, a light headache was still present in 6 of 8 subjects; in the group of patients with a symptom- free interval, such a residual symptom was present in only 6 of 20 cases.
Audiological symptoms
Bilateral (6) or unilateral (2) fullness was reported by 8 patients, during almost all vertigo attacks; these symptoms ceased as vertigo disappeared. Five patients reported tinnitus that also continued after a vertigo spell in only one case. Three patients had associated tinnitus and fullness.
Audiometry and impedance testing
Twenty-one of 28 patients had normal audiometric and impedance exams. Three subjects had mild conductive hearing loss (1 tympanosclerosis, 2 myringosclerosis) and three had a high frequency sensorineural hearing loss.
Vestibular testing
Only 4 patients had a spontaneous-positional nystagmus. One patient, at the first visit, had a pluri-positional downbeating nystagmus associated with a right-beating nystagmus in the left lateral position: at follow-up visits, during prophylactic treatment, right horizontal nystagmus disappeared while down-beating nystagmus remained, even if reduced in amplitude. One patient had down-beating nystagmus in all clinical positions that remained unchanged during follow-up. Another subject had a slight geotropic, persistent nystagmus on the left and right lateral positions: this sign disappeared after one year of follow-up (this patient also had unilateral labyrinthine weakness). One patient had a horizontal spontaneous left beating nystagmus only on the right lateral position that decreased in amplitude with time. Moreover, during caloric tests 19 patients (68%) showed a significant vagal reaction with nausea and vomiting. Only one patient had a unilateral labyrinthine failure (associated with a spontaneous nystagmus of the central type) and one subject had unilateral labyrinthine weakness, without spontaneous-positional nystagmus. None of our patients was evaluated during the acute phase of vertigo.
Pharmacological prophylaxis
All 28 patients were treated using a prophylactic regimen: 22 took acetylsalicylic acid 100 mg per day and flunarizine 5 mg per day; 3 patients took propranolol 40 mg BID, because of contraindication to both acetylsalicylic acid and flunarizine; 3 patients took only flunarizine at a dose of 5 mg BID because of contraindication to acetylsalicylic acid.
Symptoms considerably improved in all patients with therapy (failed improvement was an exclusion criteria). Nineteen subjects (68%) reported the complete disappearance of vestibular symptoms, while 9 (32%) considered their symptoms very much improved even if not completely resolved.
Subjective judgement was corroborated by data extracted from diaries during the three months before and after the beginning of prophylactic therapy. Four patients were excluded from the case series due to unsatisfactory response to therapy (therapeutic failure was considered as a marker of a diagnostic error).
Discussion and conclusions
In the literature there is no mention of the existence of a structured survey of EMV: a type of vertigo, migrainous in origin, starting late in lifetime that substitutes, as an equivalent, a pre-existing migrainous headache. On the other hand, several authors have noted that some migraine patients, suffering from headache in a young or adult age, also suffered from recurrent vertigo later in their lives.
In 1985, Hood and Kayan 15 stated: "we have recently seen a number of patients at the National Hospital Queen Square of London, whose migrainous attacks ceased after middle age, giving way to recurrent attacks of vertigo". A belated transformation of headache into vertigo in migrainous women at menopause was also reported by Harker in 1996 16; the author wrote: "many older women, who had severe migraine headache earlier in their lives that had become much milder after menopause, postmenopausally, however, begin to experience episodic vertigo, sometimes with accompanying mild headache".
Similarly, in 1961 Atkinson 17 observed a temporal relationship between migraine headache and Menière's disease: "a frequent story told by the Menière's patient is that he suffered from migraine all his life, but that when the dizzy attacks began, his headache ceased". Such a correlation was confirmed by Toglia in 1981 18: "attacks of vertigo typical of Menière's disease may replace, usually later in life, the attacks of migraine".
Even if occasional and brief, these literature annotations prompted us to look for such patients in daily clinical activity: subjects suffering from vestibular migraine in which vertigo could represent a late equivalent of their migraine headache. The first patient satisfying these criteria was found in November 1993.
Examining the previous reports of patients in our survey, not only was no temporal relationship noted between headache and vertigo, but a diagnosis of vestibular migraine was not presumed in 26 of 28 cases.
The extended suffering of these patients lead us to two considerations: 1) the diagnosis of vestibular migraine is too often neglected by general practitioners and, sometimes, by neuro-otologists as well; 2) patients with vestibular migraine do not have improvement of symptoms with drugs other than those indicated in migraine prophylaxis. Therefore, also for EMV, we agree with Dieterich and Brandt 19 when they state that in subjects suffering from vestibular migraine there are "difficulties in defining the disease and frustrating attempts to treat these patients". During 9 years of EMV case selection, we never encountered patients suffering from any type of primary headache (cluster, tension or occasional headache) other than migraine and whose vestibular symptoms manifested in substitution of headache. Hence, EMV could represent a typical manifestation solely of primary migraine headache.
Particularly interesting is the clinical fact that in spite of the long duration of vestibular symptoms before diagnosis (at least 10 years in 6 patients and three years in 16 cases), none or our patients had another transformation of the vestibular disturbance into headache or into another migraine equivalent; therefore, vestibular symptoms of patients with EMV appear to represent the last delayed manifestation of their migrainous habitus. Hence, EMV does not seem to be a temporary conversion, but rather a definite conversion of migrainous symptoms.
With the intent of comparing benign paroxysmal vertigo of childhood and EMV, we can affirm that the former is the first kind of migrainous vertigo that will often give rise, later, to migraine headache 20, whereas the latter is the last manifestation of a migrainous vertigo that will substitute migraine headache. Therefore, the two forms of vertigo could be, respectively, the first and the last migraine equivalent, as shown in migraine classification that we proposed in 2003 12.
In our EMV survey we collected 25 cases of migraine without aura and 3 with aura: such a distribution seems to represent the reported prevalence of the two forms in migraine population. Thus, the presence or absence of an aura does not seem to favour the evolution towards EMV. Moreover, among our patients there was a clear prevalence of females over males, thus reflecting the female prevalence of migraine headache.
Ten of 23 females (43.5%) in our case study had transformation of migraine headache into EMV during or immediately after menopause; in the remaining 13 women, such a transformation manifested during the fertile age. Menopause therefore seems to be a facilitating and not a decisive factor for the transformation of migraine headache into EMV. Almost all patients experienced recurrent attacks of vertigo, belatedly and unexpectedly manifested, as more severe and disabling than the previous headache. In patients with EMV, current or pre-existing motion sickness, hypersensitivity to rapid head movements and an intense vagal reaction to vestibular instrumental stimuli (caloric and rotational) were very common complaints; they showed particular hypersensitivity and, consequently, intolerance to vestibular stimulation. When not experiencing a crisis, in spite of the large number of attacks of vertigo or postural disturbances that patients referred, neuro-otologic investigation was, very often, negative.
Among our patients we found a remarkable polymorphism of vestibular symptoms (objective and subjective vertigo, dizziness); various types of symptoms were also reported also by the same patients in different occasions. Many of the characteristics of EMV are thus very similar to those reported by Dieterich and Brandt 19 for 90 patients with vertigo related to migraine.
In young patients suffering from migraine, recurrent episodes of vertigo, both quantitatively and qualitatively polymorphic, also long-lasting and without associated relevant clinical cochleo-vestibular signs, diagnosis of migraine-associated vestibulopathy is very probable, in agreement with Baloh's statement 21: "when recurrent attacks begin at an early age in a patient with normal hearing and migraine there are a few diagnosis other than migraine that need to be considered"; the same consideration goes for EMV.
We conclude that EMV is a clinical variant of typical migraine-related vertigo: a migraine-associated vertigo, headache spell independent, following the headache period, over the course of a lifetime.
References
- 1.Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular migraine. J Neurol. 2009;256:333–338. doi: 10.1007/s00415-009-0149-2. [DOI] [PubMed] [Google Scholar]
- 2.Cutrer FM, Baloh RW. Migraine-associated dizziness. Headache. 1992;32:300–304. doi: 10.1111/j.1526-4610.1992.hed3206300.x. [DOI] [PubMed] [Google Scholar]
- 3.Neuhauser H, Lempert T. Vertigo and dizziness related to migraine: a diagnostic challenge. Cephalalgia. 2004;24:83–91. doi: 10.1111/j.1468-2982.2004.00662.x. [DOI] [PubMed] [Google Scholar]
- 4.Bickerstaff ER. Basilar artery migraine. Lancet. 1961;1:15–17. [Google Scholar]
- 5.Basser LS. Benign paroxysmal vertigo of childhood. Brain. 1964;87:141–152. doi: 10.1093/brain/87.1.141. [DOI] [PubMed] [Google Scholar]
- 6.Snyder CH. Paroxysmal torticollis in infancy. Am J Dis Child. 1969;117:458–460. doi: 10.1001/archpedi.1969.02100030460013. [DOI] [PubMed] [Google Scholar]
- 7.Slater R. Benign recurrent vertigo. J Neurol Neurosurg Psychiatry. 1979;42:363–367. doi: 10.1136/jnnp.42.4.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitty CWM. Migraine without headache. Lancet. 1967;2:283–285. doi: 10.1016/s0140-6736(67)90115-8. [DOI] [PubMed] [Google Scholar]
- 9.Headache Classification Committee of the International Headache Society, author. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia. 1988;8(suppl 7):1–96. [PubMed] [Google Scholar]
- 10.Headache Classification Subcommittee of the International Headache Society, author. The international classification of headache disorders. Cephalalgia. 2004;24(suppl 1):1–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 11.Farri A, Enrico A, Farri F. Headaches of otolaryngological interest: current status while awaiting revision of classification. Practical considerations and expectations. Acta Otorhinolaryngol Ital. 2012;32:77–86. [PMC free article] [PubMed] [Google Scholar]
- 12.Pagnini P, Verrecchia L, Giannoni B, et al. La vertigine emicranica (VE) Acta Otorhinolaryngol Ital. 2003;23:19–27. [PubMed] [Google Scholar]
- 13.Baloh RW, Honrubia V. Clinical Neurophysiology of the Vestibular System. New York: Oxford University Press; 2001. pp. 152–171. [Google Scholar]
- 14.Tirelli G, Rigo S, Bullo F, et al. Saccades and smooth pursuit eye movements in central vertigo. Acta Otorhinolaryngol Ital. 2011;31:96–102. [PMC free article] [PubMed] [Google Scholar]
- 15.Hood JD, Kayan A. Neurotology and migraine. In: Blau NJ, editor. Migraine. Philadelphia: FA Davis Company; 1985. pp. 597–624. [Google Scholar]
- 16.Harker LA. Migraine-Associated Vertigo. In: Baloh RW, Halmagyi GM, editors. Disorders of the Vestibular System. New York: Oxford University Press; 1996. pp. 407–417. [Google Scholar]
- 17.Atkinson M. Migraine and Menière's disease. Archives of Otolaryngology. 1962;75:46–51. doi: 10.1001/archotol.1962.00740040228008. [DOI] [PubMed] [Google Scholar]
- 18.Toglia JU, Thomas D, Kuritzky A. Common migraine and vestibular function: electronystagmographic study and pathogenesis. Ann Otol Rhinol Laryngol. 1981;90:267–271. doi: 10.1177/000348948109000315. [DOI] [PubMed] [Google Scholar]
- 19.Dieterich M, Brandt T. Episodic vertigo related to migraine (90 cases): vestibular migraine? J Neurol. 1999;246:883–892. doi: 10.1007/s004150050478. [DOI] [PubMed] [Google Scholar]
- 20.Lanzi G, Balottin U, Fazzi E, et al. Benign paroxysmal vertigo of childhood: a long-term follow-up. Cephalalgia. 1994;14:458–460. doi: 10.1046/j.1468-2982.1994.1406458.x. [DOI] [PubMed] [Google Scholar]
- 21.Brantberg K, Trees N, Baloh RW. Migraine-associated vertigo. Acta Otolaryngologica. 2005;125:276–279. doi: 10.1080/00016480510003165. [DOI] [PubMed] [Google Scholar]