Abstract
Background and Purpose
Individuals with stroke-like symptoms are recommended to receive rapid diagnostic evaluation. Emergency medical services (EMS) transport, compared to private modes, and hospital notification prior to arrival may reduce delays in evaluation. This study estimated associations between hospital arrival modes (EMS or private; with or without EMS pre-notification) and times for completion and interpretation of initial brain imaging in presumed stroke patients.
Methods
Among suspected stroke patients identified and enrolled by the North Carolina Stroke Care Collaborative (NCSCC) registry in 2008-2009, we analyzed data on arrival modes, meeting recommended targets for brain imaging completion and interpretation times (<25 minutes and <45 minutes since hospital arrival, respectively), and patient- and hospital-level characteristics. We used modified Poisson regression to estimate adjusted risk ratios (RR) and 95% confidence intervals (CI).
Results
Of 13,894 eligible patients, 21% had their brain imaging completed and 23% had their brain imaging interpreted by a physician within target times. Arrival by EMS (versus private transport) was associated with both brain imaging completed within 25 minutes of arrival [EMS with pre-notification: RR=3.0, 95% CI=2.1-4.1; EMS without pre-notification: RR=1.9, 95% CI=1.6-2.3] and brain imaging interpreted within 45 minutes [EMS with pre-notification: RR=2.7, 95% CI=2.3-3.3; EMS without pre-notification: RR=1.7, 95% CI=1.4-2.1].
Conclusions
Presumed stroke patients arriving to the hospital by EMS were more likely to receive brain imaging and have it interpreted by a physician in a timely manner than those arriving by private transport. Moreover, EMS arrivals with hospital pre-notification experienced the most rapid evaluation.
Keywords: acute stroke, emergency medical services, in hospital delay time
Introduction
Thrombolytic therapy can improve neurological outcomes in appropriate stroke patients. Intravenous tissue plasminogen activator (tPA) is most beneficial when administered in a qualified acute care facility within 3 hours of symptom onset.1,2 Therefore, it is imperative that stroke patients receive timely emergency medical care and evaluation. Only 2-3% of acute strokes are given thrombolytics,3 which is partly due to both prehospital and in-hospital delays.4 A recent study found that only 23% of acute stroke patients arrived to the emergency department (ED) within 3 hours of symptom onset.5 Even when patients arrive soon after symptom onset, physician evaluation and brain imaging studies are required to determine eligibility for thrombolytics. Consensus guidelines recommend a target time of 25 minutes or less from hospital arrival to computed tomography (CT) scan and another 20 minutes for the CT to be interpreted by a neurologist or other physician.1,6
Emergency medical services (EMS) can significantly benefit acute stroke patients, but only about half of acute stroke patients use EMS.7-12 EMS responders can accurately identify suspect strokes in the field13,14 and notify the receiving facility that a potential stroke patient is en route,15,16 allowing hospitals to prepare and mobilize resources prior to the patient’s arrival. Studies report that EMS utilization is associated with reduced prehospital and in-hospital delays in acute stroke patients.7-9,12,17-24 However, few have explored more advanced levels of EMS care, such as prehospital notification to the receiving facility.25
We examined the associations between hospital arrival mode (EMS versus private transport) and meeting recommended times for completion and interpretation of brain imaging in stroke patients. Further, we compared EMS arrivals by whether or not the receiving hospital was pre-notified.
Methods
Study Population and Data Collection
In 2001, the Paul Coverdell National Acute Stroke Registry (PCNASR) program was established to measure, track, and improve the quality of in-hospital stroke care.12,26 These state-based registries collect data on quality-of-care indicators based on established guidelines. The North Carolina Stroke Care Collaborative (NCSCC) is one of six PCNASR and includes 52 participating acute care hospitals covering 39 of 100 North Carolina counties, representing 61% of all stroke discharges in the state. As previously described,27,28 trained hospital staff prospectively identify presumptive stroke patients ages 18 years and older and collect data on demographics, initial presentation, quality-of-care indicators, in-hospital outcomes, and discharge disposition using a standardized, web-based data collection tool.
We used 2008 and 2009 NCSCC data. During this period, hospitals enrolled 16,179 presumptive stroke patients with an admission diagnosis of ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage, non-specified stroke, or transient ischemic attack. For our study, patients were excluded if they were transfers from another hospital or had an unknown mode of arrival (N=725), had outside brain imaging prior to hospital arrival (N=1,858), were missing hospital arrival time (N=186), had implausible imaging times (N=9), and had imaging delays greater than 24 hours (N=147). The final study size was 13,894 patients.
Study Measures and Variables
Hospital arrival mode was defined as “private” for arrivals by private car, taxi, or other. Information in the medical record was used to classify EMS arrivals by whether or not there was pre-notification to the hospital of a suspected stroke. We calculated delay times from ED or hospital arrival to (1) completion of initial brain imaging and (2) its interpretation by a physician. Imaging completion times were entered from the film printout or the digital image of the radiology report. Imaging interpretation time was defined as the time results were first read by a radiologist, neurologist, ED physician, or any other physician. Times were recorded from various sources including radiology reports, ED notes, and tPA protocol sheets. As a secondary outcome, we examined tPA administration in the subset of eligible patients.
Covariates included age (18-44, 45-64, 65-84, 85+ years), sex, race (White, Black, other), insurance status (Medicare or private insurance, Medicaid only, no insurance), time of day of arrival (7AM-6:59PM, 7-11:59PM, 12-6:59AM), weekend or weekday arrival, documented history of stroke or TIA, presumptive stroke diagnosis (ischemic, hemorrhagic, not-specified, TIA), ambulation at admission (independent or with device, with personal assistance, or unable to ambulate), and patient location at time of symptom onset (not in a healthcare facility, another healthcare facility). Hospital-level characteristics were Joint Commission Primary Stroke Center (JCPSC) certification status, teaching hospital status, and number of beds (<100, 100-300, >300 beds). We defined prehospital delay as the time between when the patient was last known well and hospital arrival, with further categorization by the optimal ≤ 2 hours prehospital delay.
Statistical Analysis
Delays from arrival to brain imaging completion and physician interpretation were compared by arrival mode. Since the distribution of delay times were right skewed, we reported median times (in hours). Per recommended time targets, we calculated crude and covariate-adjusted proportions (risks) of brain imaging completion within 25 minutes of arrival and brain imaging interpretation within 45 minutes of arrival. Crude and adjusted risk ratios (RR) and 95% confidence intervals (CI) comparing arrival modes were estimated using modified Poisson regression with robust variance estimators to account for clustering of patients within hospitals. We adjusted for all covariates to limit potential bias due to confounding and estimated adjusted risks using the distribution of covariates in the total study population. The number needed to treat (NNT) with pre-notification was calculated as the reciprocal of the difference between the risks in the two EMS arrival modes. We repeated analyses restricted to those patients with a prehospital delay of ≤ 2 hours. As a secondary analysis, we fit adjusted regression models comparing tPA administration among ischemic stroke patients who arrived within 2 hours of symptom onset and were identified as having no contraindications.
Since time of brain imaging interpretation was missing for 44% of patients, we conducted a sensitivity analysis using multiple imputation methods to explore potential bias and loss of precision from missing data (see online supplement). Because changes in estimates and loss of precision were minimal, we present results from the complete case analysis only.
Results
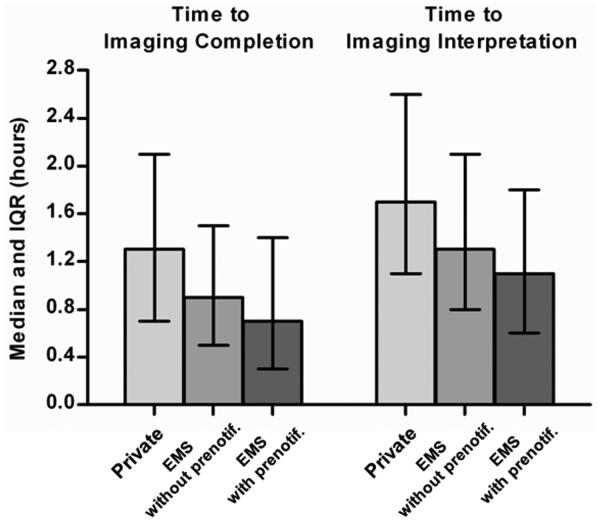
Of the 13,894 study patients, 45% arrived by private transportation, and 55% used EMS. Of the EMS arrivals, the receiving hospital was pre-notified in 58% of cases. Table 1 presents patient and hospital characteristics in the total study population and by arrival mode. The strongest predictors of arrival mode were age, time of day of arrival, presumptive stroke diagnosis, ambulatory status on admission, patient location at onset, and hospital bed size. Shorter prehospital delays were also associated with EMS transport and hospital pre-notification. Overall median time (interquartile range) to initial brain imaging completion was 1.0 hours (0.5 – 1.8 hours) and brain imaging interpretation was 1.4 hours (0.8 – 2.3 hours). On average, delay times were longest in the private transport group and shortest in the EMS with pre-notification group (Figure 1).
Table 1.
Patient- and Hospital-level Covariates by Arrival Mode, North Carolina Stroke Care Collaborative (NCSCC), 2008-2009
| Arrival Mode | ||||||||
|---|---|---|---|---|---|---|---|---|
| Total (N=13,894) |
EMS | |||||||
| Covariates | Private (N=6,300) |
Without pre- notification (N=3,214) |
With pre- notification (N=4,380) |
|||||
|
|
||||||||
| No. | % | No. | % | No. | % | No. | % | |
| Age, years | ||||||||
| 18-44 | 713 | 5% | 419 | 7% | 120 | 4% | 174 | 4% |
| 45-64 | 4,401 | 32% | 2,422 | 38% | 817 | 25% | 1,162 | 27% |
| 65-84 | 6,547 | 47% | 2,850 | 45% | 1,569 | 49% | 2,128 | 49% |
| 85+ | 2,233 | 16% | 609 | 10% | 708 | 22% | 916 | 21% |
| Female Sex | 6,430 | 46% | 3,017 | 48% | 1,405 | 44% | 2,008 | 46% |
| Race | ||||||||
| White | 10,000 | 72% | 4,482 | 71% | 2,281 | 71% | 3,237 | 74% |
| Black | 3,564 | 26% | 1,654 | 26% | 859 | 27% | 1,051 | 24% |
| Other | 270 | 2% | 137 | 2% | 55 | 2% | 78 | 2% |
| missing | 60 | 27 | 19 | 14 | ||||
| Insurance Status | ||||||||
| Medicare or Private | 12,027 | 87% | 5,310 | 85% | 2,828 | 89% | 3,889 | 89% |
| Medicaid only | 601 | 4% | 296 | 5% | 139 | 4% | 166 | 4% |
| None | 1,182 | 9% | 652 | 10% | 219 | 7% | 311 | 7% |
| missing | 84 | 42 | 28 | 14 | ||||
| Time of Day of Arrival | ||||||||
| 7:00AM-6:59PM | 10,258 | 74% | 4,903 | 78% | 2,262 | 70% | 3,093 | 71% |
| 7:00PM-11:59PM | 2,570 | 19% | 1,067 | 17% | 640 | 20% | 863 | 20% |
| 12:00AM-6:59AM | 1,066 | 8% | 330 | 5% | 312 | 10% | 424 | 10% |
| Weekend Arrival | 3,716 | 27% | 1,618 | 26% | 896 | 28% | 1,202 | 27% |
| Prehospital Delay | ||||||||
| ≤ 2 hours | 2,588 | 46% | 804 | 38% | 554 | 44% | 1,230 | 54% |
| > 2 hours | 3,083 | 54% | 1,315 | 62% | 701 | 56% | 1,067 | 46% |
| missing | 8,223 | 4,181 | 1,959 | 2,083 | ||||
| History of Stroke or TIA | 4,946 | 36% | 2,045 | 32% | 1,260 | 39% | 1,641 | 37% |
| Presumptive Stroke Diagnosis | ||||||||
| Ischemic | 4,916 | 35% | 2,141 | 34% | 978 | 30% | 1,797 | 41% |
| Hemorrhagic | 1,329 | 10% | 293 | 5% | 420 | 13% | 616 | 14% |
| TIA | 3,524 | 25% | 1,909 | 30% | 746 | 23% | 869 | 20% |
| Not-specified | 4,125 | 30% | 1,957 | 31% | 1,070 | 33% | 1,098 | 25% |
| Ambulatory Status at Admission | ||||||||
| Independent | 11,997 | 91% | 5,833 | 96% | 2,596 | 87% | 3,568 | 86% |
| Other or Unable | 1,239 | 9% | 259 | 4% | 405 | 14% | 575 | 14% |
| missing | 658 | 208 | 213 | 237 | ||||
| Patient Location at Onset | ||||||||
| Not a Health Care Facility | 12,631 | 92% | 6,076 | 98% | 2,703 | 85% | 3,852 | 89% |
| Another Health Care Facility | 1,075 | 8% | 134 | 2% | 459 | 15% | 482 | 11% |
| missing | 188 | 90 | 52 | 46 | ||||
| JCPSC Certification | 6,974 | 50% | 3,060 | 49% | 1,675 | 52% | 2,239 | 51% |
| Teaching Hospital | 5,164 | 37% | 2,248 | 36% | 1,284 | 40% | 1,632 | 37% |
| Hospital Beds | ||||||||
| < 100 | 789 | 6% | 420 | 7% | 229 | 7% | 140 | 3% |
| 100-300 | 5,794 | 42% | 2,853 | 45% | 1,581 | 49% | 1,360 | 31% |
| > 300 | 7,311 | 53% | 3,027 | 48% | 1,404 | 44% | 2,880 | 66% |
TIA indicates transient ischemic attack; JCPSC, Joint Commission Primary Stroke Center
Figure 1.
Median In-hospital Delay Times (and Interquartile Range, IQR) by Arrival Mode, NCSCC, 2008-2009
Overall, 21% of presumed stroke patients had initial brain imaging completed and 23% had their imaging interpreted by a physician within the recommended 25 and 45 minutes following arrival, respectively. For patients receiving imaging within 25 minutes, 60% had results interpreted within the next 20 minutes. Crude and covariate-adjusted probabilties of meeting these targets (“Risks”) are presented by arrival mode in Table 2 with RRs and 95% CIs comparing EMS arrival types to private transport (referent). In adjusted analyses, patients arriving by EMS were significantly more likely to have imaging completed and interpreted within the target times. Moreover, pre-notification by EMS (versus no pre-notification) was positively associated with imaging completed within 25 minutes of arrival (RR = 1.5; 95% CI = 1.0, 2.3) and imaging interpreted within 45 minutes of arrival (RR = 1.6; 95% CI = 1.3, 2.0). According to estimated NNTs, on average, 8.8 patients arriving by EMS with pre-notification versus without pre-notification would result in one additional patient having imaging completed within 25 minutes of arrival. Similarly, for every 7.7 patients arriving with pre-notification by EMS, one additional patient would have imaging results interpreted by a physician within 45 minutes of arrival.
Table 2.
Associations between Meeting Brain Imaging Target Times and Arrival Mode, NCSCC, 2008-2009
| Brain Imaging completed within 25 minutes |
Brain Imaging interpreted within 45 minutes |
|||||
|---|---|---|---|---|---|---|
|
|
||||||
| Risk | RR | 95% CI | Risk | RR | 95% CI | |
| Crude | ||||||
| EMS with pre-notification | 0.32 | 2.9 | (2.1, 3.9) | 0.34 | 2.5 | (2.1, 3.1) |
| EMS without pre-notification | 0.22 | 1.9 | (1.5, 2.5) | 0.24 | 1.8 | (1.4, 2.3) |
| Private (ref) | 0.11 | 1 | 0.13 | 1 | ||
| Adjusted* | ||||||
| EMS with pre-notification | 0.32 | 3.0 | (2.1, 4.1) | 0.35 | 2.7 | (2.3, 3.3) |
| EMS without pre-notification | 0.21 | 1.9 | (1.6, 2.3) | 0.22 | 1.7 | (1.4, 2.1) |
| Private (ref) | 0.11 | 1 | 0.13 | 1 | ||
RR indicates risk ratio; CI, confidence interval
Adjusted for age, sex, race, health insurance, time of day of arrival, weekend arrival, documented history of stroke/TIA, presumptive stroke diagnosis, ambulatory status at admission, patient location at onset, JCPSC certification, teaching hospital, hospital beds
Imaging completion and interpretation were almost twice as likely to occur within the optimal time windows when patients arrived within 2 hours of symptom onset or last known well. Adjusted relative risks (RRs) were weaker compared to the entire study population; however, absolute risk differences, particularly between EMS with pre-notification and without, were of similar magnitude (Table 3). Intravenous tPA was initiated in 317 of 467 ischemic stroke patients who arrived within 2 hours of symptom onset and were medically eligible for this treatment. In adjusted analyses, patients arriving by EMS with pre-notification were more likely to receive tPA than those arriving by private transport (RR = 1.5; 95% CI = 1.1, 1.9). Moreover, EMS arrival with pre-notification (versus no pre-notification) was significantly associated with higher tPA administration (RR = 1.6; 95% CI = 1.4, 2.0).
Table 3.
Associations between Meeting Brain Imaging Target Times and Arrival Mode among Patients Arriving Within 2 Hours of Stroke Onset, NCSCC, 2008-2009
| Brain Imaging completed within 25 minutes |
Brain Imaging interpreted within 45 minutes |
|||||
|---|---|---|---|---|---|---|
|
|
||||||
| Risk | RR | 95% CI | Risk | RR | 95% CI | |
| Crude | ||||||
| EMS with pre-notification | 0.55 | 2.3 | (1.8, 2.8) | 0.57 | 1.8 | (1.5, 2.1) |
| EMS without pre-notification | 0.34 | 1.4 | (1.1, 1.8) | 0.43 | 1.3 | (1.1, 1.7) |
| Private (ref) | 0.25 | 1 | 0.32 | 1 | ||
| Adjusted* | ||||||
| EMS with pre-notification | 0.52 | 1.9 | (1.6, 2.3) | 0.53 | 1.5 | (1.3, 1.7) |
| EMS without pre-notification | 0.34 | 1.2 | (1.0, 1.6) | 0.43 | 1.2 | (1.0, 1.5) |
| Private (ref) | 0.27 | 1 | 0.35 | 1 | ||
RR indicates risk ratio; CI, confidence interval
Adjusted for age, sex, race, health insurance, time of day of arrival, weekend arrival, documented history of stroke/TIA, presumptive stroke diagnosis, ambulatory status at admission, patient location at onset, JCPSC certification, teaching hospital, hospital beds
Discussion
The immediate evaluation of stroke patients is critical to identify the best course of treatment and ensure timely administration of therapy, yet meeting in-hospital timing goals continues to be a major challenge. In the NCSCC, about one-fifth of suspected stroke patients had their brain imaging completed or interpreted within the recommended times. A recent comprehensive literature review found that only 2 of 20 published studies reported median times to CT scan less than 25 minutes.4 Still, they estimated a 0.1-hour annual decline in CT scan delays from 1994-2005. When compared to CT delays reported in a similar NC patient population from 2005-200828, we observed 0.2-hour shorter average delay times, suggesting a trend of decreasing delays.
Our findings confirm arrival mode is strongly associated with in-hospital delays in stroke evaluation. Further, the proportion of suspect stroke patients having a brain imaging study completed and interpreted in a timely manner was higher with hospital pre-notification by EMS. This is consistent with a previous study that found shorter times to CT with EMS pre-notification.25 To illustrate the public health impact of our findings, given approximately 28,000 stroke discharges from NC hospitals per year,29 an estimated 15,400 would arrive by EMS, and according to our NNT analysis, pre-notification would increase the number of patients having imaging completed within 25 minutes from 4,216 to 4,957, or by 741 patients. Similarly, the number of patients having imaging interpreted within 45 minutes would increase from 4,478 to 5,321, or by 843. Therefore, incorporating pre-notification in large populations could increase timely evaluation in a substantial number of stroke patients.
Our study has several strengths and limitations. NCSCC collects the time of imaging interpretation by a physician, which allowed us to examine a second important source of in-hospital delay. Although current guidelines specifically state a target time,1,6 we are aware of only one other study that has reported on this endpoint.30 Measuring time to brain imaging interpretation is challenging. Although NCSCC personnel are instructed to record the time images are first read by any physician, the sources of this information can vary by site and patient. Data quality and completeness are important considerations for collection and analysis of this measure. Even though interpretation time was missing for about 44% of patients in this study, we were reassured that our sensitivity analysis demonstrated consistent estimates (see online supplement).
We conducted a secondary analysis of the NCSCC, so our study was limited to existing data. Nonetheless, given the extensive information collected, we were able to adjust for confounding by numerous patient and hospital characteristics. However, we could not adjust for stroke severity since it was not adequately measured. Since more severe strokes may have shorter prehospital delays,9 we may have accounted for some confounding by severity in the analysis restricted to patients arriving within 2 hours of onset, where we found positive, although weaker, associations. Hospital participation in the NCSCC is voluntary; thus, our study may not be representative of all hospitals in North Carolina. However, NCSCC hospitals are located in geographic regions across the state and are diverse in terms of size and type.
A main strength of the NCSCC is that patients are enrolled prospectively based on a presumptive stroke diagnosis. Trained hospital personnel examine various information sources including ED discharge diagnoses and physician admission notes for evidence of a suspected stroke. Therefore, we were able to study the in-hospital evaluation of patients with an initial clinical impression of stroke or TIA, regardless of final diagnosis. To show that our results are robust to the exclusion of TIAs, we performed a stroke only analysis and found slightly stronger associations between arrival mode and imaging delay times, while observing the same relationships as with the overall study population.
Our assessment of EMS pre-notification was limited to present or absent; thus, we did not capture additional details communicated to hospitals, such as type of symptoms and prehospital stroke screening results. Moreover, data on the capabilities and resources of EMS agencies and their personnel were also not available. These characteristics are known to vary substantially by region31 and should be explored as potentially modifying factors of the perceived benefits associated with individual EMS actions. Nonetheless, our study addresses an important characteristic of EMS transport of potential stroke patients with implications for policies that influence the role of EMS in stroke systems of care. Our results suggest that implementing hospital pre-notification in EMS protocols may significantly reduce delays in the evaluation of acute stroke patients. Additional analyses suggest a similar impact of EMS pre-notification on rates of tPA administration. Further research is needed on how faster completion of diagnostic procedures translates into improvements in the delivery of acute stroke care.
Conclusions
In the NCSCC from 2008-2009, hospitalized patients with stroke-like symptoms arriving by EMS were more likely to receive brain imaging and have it interpreted by a physician in a timely manner than those arriving by private transport. Moreover, EMS arrivals with pre-notification to the hospital experienced the most rapid evaluation. Nevertheless, the proportion of patients who met recommended target times was only about 20%. Patients arriving soon after symptom onset were more likely to meet these targets, although there were still reductions in hospital delays with EMS pre-notification. These findings support the practice of pre-notification by EMS personnel when transporting suspected stroke patients to the hospital.
Supplementary Material
Acknowledgements
We thank participating hospitals and staff.
Sources of Funding
This study was supported by the Centers for Disease Control and Prevention (CDC) as a Paul Coverdell National Acute Stroke Registry (PCNASR) via a subcontract with the North Carolina Division of Public Health (Contract # 01602-10).
Footnotes
Disclosures
None
References
- 1.Adams HP, Jr., del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the Early Management of Adults With Ischemic Stroke: A Guideline From the American Heart Association/ American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007;38:1655–1711. doi: 10.1161/STROKEAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- 2.Marler JR, Tilley BC, Lu M, Brott TG, Lyden PC, Grotta JC, et al. Early stroke treatment associated with better outcome The NINDS rt-PA Stroke Study. Neurology. 2000;55:1649–1655. doi: 10.1212/wnl.55.11.1649. [DOI] [PubMed] [Google Scholar]
- 3.Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM, et al. Recommendations for Comprehensive Stroke Centers A Consensus Statement From the Brain Attack Coalition. Stroke. 2005;36:1597–1616. doi: 10.1161/01.STR.0000170622.07210.b4. [DOI] [PubMed] [Google Scholar]
- 4.Evenson KR, Foraker RE, Morris DL, Rosamond WD. A comprehensive review of prehospital and in-hospital delay times in acute stroke care. International Journal of Stroke. 2009;4:187–199. doi: 10.1111/j.1747-4949.2009.00276.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reeves MJ, Broderick JP, Frankel M, LaBresh KA, Schwamm L, Moomaw CJ, et al. The Paul Coverdell National Acute Stroke Registry Initial Results from Four Prototypes. American Journal of Preventive Medicine. 2006;31:202–209. doi: 10.1016/j.amepre.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Marler JR, Winters-Jones P, Emr M. National Institute of Neurological Disorders and Stroke; Proceedings of a National Symposium on Rapid Identification and Treatment of Acute Stroke; 1997. pp. 157–158. [NIH publication No. 97-4239] [Google Scholar]
- 7.Kothari R, Jauch E, Broderick J, Brott T, Sauerbeck L, Khoury J, et al. Acute Stroke: Delays to Presentation and Emergency Department Evaluation. Annals of Emergency Medicine. 1999;33:3–8. doi: 10.1016/s0196-0644(99)70431-2. [DOI] [PubMed] [Google Scholar]
- 8.Lacy CR, Suh DC, Bueno M, Kostis JB. Delay in Presentation and Evaluation for Acute Stroke Stroke Time Registry for Outcomes Knowledge and Epidemiology (STROKE) Stroke. 2001;32:63–69. doi: 10.1161/01.str.32.1.63. [DOI] [PubMed] [Google Scholar]
- 9.Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S. Prehospital and emergency department delays after acute stroke: the Genentech Stroke Presentation Survey. Stroke. 2000;31:2585–2590. doi: 10.1161/01.str.31.11.2585. [DOI] [PubMed] [Google Scholar]
- 10.Porteous GH, Corry MD, Smith WS. Emergency medical services dispatcher identification of stroke and transient ischemic attack. Prehospital Emergency Care. 1999;3:211–216. doi: 10.1080/10903129908958939. [DOI] [PubMed] [Google Scholar]
- 11.Schroeder EB, Rosamond WD, Morris DL, Evenson KR, Hinn AR. Determinants of Use of Emergency Medical Services in a Population With Stroke Symptoms The Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke. 2000;31:2591–2596. doi: 10.1161/01.str.31.11.2591. [DOI] [PubMed] [Google Scholar]
- 12.Prehospital and hospital delays after stroke onset–United States, 2005-2006. MMWR Morbidity and Mortality Weekly Report. 2007;56:474–478. [PubMed] [Google Scholar]
- 13.Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS) Stroke. 2000;31:71–76. doi: 10.1161/01.str.31.1.71. [DOI] [PubMed] [Google Scholar]
- 14.Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: Reproducibility and Validity. Annals of Emergency Medicine. 1999;33:373–378. doi: 10.1016/s0196-0644(99)70299-4. [DOI] [PubMed] [Google Scholar]
- 15.Crocco TJ, Grotta JC, Jauch EC, Kasner SE, Kothari RU, Larmon BR, et al. EMS management of acute stroke–prehospital triage. Prehospital Emergency Care. 2007;11:313–317. doi: 10.1080/10903120701347844. [DOI] [PubMed] [Google Scholar]
- 16.Gladstone DJ, Rodan LH, Sahlas DJ, Lee L, Murray BJ, Ween JE, et al. A Citywide Prehospital Protocol Increases Access to Stroke Thrombolysis in Toronto. Stroke. 2009;40:3841–3844. doi: 10.1161/STROKEAHA.108.540377. [DOI] [PubMed] [Google Scholar]
- 17.Bohannon RW, Silverman IE, Ahlquist M. Time to emergency department arrival and its determinants in patients with acute ischemic stroke. Connecticut Medicine. 2003;67:145–148. [PubMed] [Google Scholar]
- 18.Evenson KR, Schroeder EB, Legare TB, Brice JH, Rosamond WD, Morris DL. A comparison of emergency medical services times for stroke and myocardial infarction. Prehospital Emergency Care. 2001;5:335–339. doi: 10.1080/10903120190939463. [DOI] [PubMed] [Google Scholar]
- 19.Harraf F, Sharma AK, Brown MM, Lees KR, Vass RI, Kalra L. A multicentre observational study of presentation and early assessment of acute stroke. British Medical Journal. 2002;325:17. doi: 10.1136/bmj.325.7354.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.John M, Palmer P, Faile E, Broce M. Factors causing patients to delay seeking treatment after suffering a stroke. The West Virginia Medical Journal. 2005;101:12–15. [PubMed] [Google Scholar]
- 21.Menon SC, Pandey DK, Morgenstern LB. Critical factors determining access to acute stroke care. Neurology. 1998;51:427–432. doi: 10.1212/wnl.51.2.427. [DOI] [PubMed] [Google Scholar]
- 22.Rosamond WD, Gorton RA, Hinn AR, Hohenhaus SM, Morris DL. Rapid response to stroke symptoms: the Delay in Accessing Stroke Healthcare (DASH) study. Academic Emergency Medicine. 1998;5:45–51. doi: 10.1111/j.1553-2712.1998.tb02574.x. [DOI] [PubMed] [Google Scholar]
- 23.Rossnagel K, Jungehulsing GJ, Nolte CH, Muller-Nordhorn J, Roll S, Wegscheider K, et al. Out-of-hospital delays in patients with acute stroke. Annals of Emergency Medicine. 2004;44:476–483. doi: 10.1016/j.annemergmed.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 24.Wester P, Radberg J, Lundgren B, Peltonen M. Factors associated with delayed admission to hospital and in-hospital delays in acute stroke and TIA: a prospective, multicenter study. Seek- Medical-Attention-in-Time Study Group. Stroke. 1999;30:40–48. doi: 10.1161/01.str.30.1.40. [DOI] [PubMed] [Google Scholar]
- 25.Abdullah AR, Smith EE, Biddinger PD, Kalenderian D, Schwamm LH. Advance hospital notification by EMS in acute stroke is associated with shorter door-to-computed tomography time and increased likelihood of administration of tissue-plasminogen activator. Prehospital Emergency Care. 2008;12:426–431. doi: 10.1080/10903120802290828. [DOI] [PubMed] [Google Scholar]
- 26.Labarthe DR, Biggers A, LaPier T, George MG. The Paul Coverdell National Acute Stroke Registry (PCNASR): a public health initiative. American Journal of Preventive Medicine. 2006;31:192–195. doi: 10.1016/j.amepre.2006.07.027. [DOI] [PubMed] [Google Scholar]
- 27.George MG, Tong X, McGruder H, Yoon P, Rosamond W, Winquist A, et al. Paul Coverdell National Acute Stroke Registry Surveillance - four states, 2005-2007. MMWR Morbidity and Mortality Weekly Report Surveillance Summaries. 2009;58:1–23. [PubMed] [Google Scholar]
- 28.Rose KM, Rosamond WD, Huston SL, Murphy CV, Tegeler CH. Predictors of Time From Hospital Arrival to Initial Brain-Imaging Among Suspected Stroke Patients: The North Carolina Collaborative Stroke Registry. Stroke. 2008;39:3262. doi: 10.1161/STROKEAHA.108.524686. [DOI] [PubMed] [Google Scholar]
- 29.Huston SL. Burden of Cardiovascular Disease in North Carolina - July, 2010. NC Department of Health and Human Services; Raleigh: 2010. Available at: www.startwithyourheart.com/Default.aspx?pn=CVDBurden. Accessed October 14, 2010. [Google Scholar]
- 30.Katzan IL, Graber TW, Furlan AJ, Sundararajan S, Sila CA, Houser G, et al. Cuyahoga County Operation Stroke speed of emergency department evaluation and compliance with National Institutes of Neurological Disorders and Stroke time targets. Stroke. 2003;34:994. doi: 10.1161/01.STR.0000060870.55480.61. [DOI] [PubMed] [Google Scholar]
- 31.Brice JH, Evenson KR, Lellis JC, Rosamond WD, Aytur SA, Christian JB, et al. Emergency medical services education, community outreach, and protocols for stroke and chest pain in North Carolina. Prehospital Emergency Care. 2008;12:366–371. doi: 10.1080/10903120802100100. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.