Abstract
Infectious prion (PrPRes) material is likely the cause of fatal, neurodegenerative transmissible spongiform encephalopathy (TSE) diseases1. Transmission of TSE diseases, such as chronic wasting disease (CWD), is presumed to be from animal to animal2,3 as well as from environmental sources4-6. Scavengers and carnivores have potential to translocate PrPRes material through consumption and excretion of CWD-contaminated carrion. Recent work has documented passage of PrPRes material through the digestive system of American crows (Corvus brachyrhynchos), a common North American scavenger7.
We describe procedures used to document passage of PrPRes material through American crows. Crows were gavaged with RML-strain mouse-adapted scrapie and their feces were collected 4 hr post gavage. Crow feces were then pooled and injected intraperitoneally into C57BL/6 mice. Mice were monitored daily until they expressed clinical signs of mouse scrapie and were thereafter euthanized. Asymptomatic mice were monitored until 365 days post inoculation. Western blot analysis was conducted to confirm disease status. Results revealed that prions remain infectious after traveling through the digestive system of crows and are present in the feces, causing disease in test mice.
Keywords: Infection, Issue 81, American crows, feces, mouse model, prion detection, PrPRes, scrapie, TSE transmission
Introduction
Transmissible spongiform encephalopathies (TSE) are fatal infectious neurodegenerative disorders that affect wildlife, domestic animals, and humans. The infectious agent of TSE diseases appears to be misfolded or pathogenic isoforms (PrPRes) of prion proteins1. Animal TSE diseases include chronic wasting disease (CWD) in mule deer (Odocoileus hemionus), white-tailed deer (Odocoileus virginianus), elk (Cervus elaphus), and moose (Alces alces); scrapie in sheep and goats; bovine spongiform encephalopathy (BSE) in domestic cattle; transmissible mink encephalopathy in farmed mink; feline spongiform encephalopathy in cats; exotic ungulate spongiform encephalopathy in exotic zoo ruminates of the family Bovidae; and spongiform encephalopathy in nonhuman primates8. The single human TSE disease, variant Creutzfeldt-Jakob disease, is rare and thought to be acquired by consuming PrPRes-contaminated food9. Similarly, BSE can infect humans if contaminated beef is consumed10. Of all the TSE diseases, scrapie and CWD are the only two with self-sustaining epidemics and sources for infection are presumed to be from animal to animal2,3,11 as well as from environmental sources4-6. Research suggests that most TSE diseases require notable extended incubation periods from natural exposure events of PrPRes material to manifestation of clinical signs2-4,6,8 and apparent species barriers minimize, but do not eliminate the potential for, interspecies transmission12-14.
Identifying mechanisms for the spread of infectious prion (PrPRes) material is extremely important for answering questions about how TSE diseases move across the landscape. Experimental investigations have suggested that insects15,16, poultry and pigs17, and American crows (Corvus brachyrhynchos)7,18 are passive carriers or dispersers of PrPRes material. Passage of PrPRes material through the digestive system of crows has recently been documented, demonstrating the role they may play in dispersal of TSE diseases7. These results make it plausible that crows, a scavenger, could encounter, consume, and transport infectious material via feces deposition, to disease-free areas.
The procedures we demonstrate here were used to document passage of PrPRes material through the digestion system of crows and will greatly facilitate the application of these methods to other scavenger and carnivore species-specific models in related future research. In this study conventional methods were used to investigate an unconventional means of trafficking PrPRes material, which could contribute to the spread and overall burden of PrPRes material.
Protocol
Our protocol is adapted from one we previously published7. All procedures involving animals were approved by the Institutional Animal Care and Use Committee of the United States Department of Agriculture (USDA), Animal and Plant Health Inspection Service (APHIS), Wildlife Services (WS), National Wildlife Research Center (NWRC).
1. Crow Gavaging
- Estimate passage time of 'pseudo brain material' through the alimentary tract of American crows.
- Mix 5 ml of cooked and scrambled whole egg with blue dye and gavage 1 crow using a 2 in gavage needle (Figure 1).
- Check crow every 30 min until blue/green-stained feces are no longer being excreted.
Obtain uninfected and terminally ill RML (Chandler strain) -infected C57BL/6 mouse brains.
Generate a 20% wt/vol normal and infected mouse-brain homogenate in a bullet blender homogenizer with 1x phosphate buffered saline (PBS) and glass beads, then centrifuge at 3,000 x g for 1 min to remove larger particulate matter. Remove supernatant and dilute with an equal volume of 1x PBS to generate a 10% wt/vol in sterile PBS. Freeze at -80 °C until needed.
17 hr prior to gavage remove food, but not water, from crow pens.
Randomly allocate crows to treatment groups and orally gavage each crow with 5 ml of either normal or infected mouse brain homogenate using a 2 in gavage needle.
Transfer crows to individual cages and collect and pool all feces within each cage for 4 hr post gavage (Figure 2).
Homogenize pooled feces for each crow in a bullet blender homogenizer with glass beads until a uniform texture is achieved. *Crow feces are mostly liquid and can be mixed easily.
For each crow, dilute 500 µl of fecal homogenate into 9.5 ml 1x PBS for a total volume of 10 ml.
Centrifuge the fecal homogenate for 15 min at 1,400 x g and extract the supernatant.
To minimize the threat of a secondary microbial infection, treat supernatant with 1 µl of 100 units/ml penicillin and 100 µg/ml streptomycin (Invitrogen, NY) per 100 µl of homogenate then place under UV light at room temperature for 20 min to reduce risk of viral and bacterial contamination. After UV exposure, sonicate samples in a 3000 Mp sonicator at setting 70 for 30 sec to disrupt the membrane of any remaining microbes.
2. Mouse Inoculation
- Randomly allocate mice to the following treatment groups (Table 1):
- Group 1 - Positive treatment mice inoculated intraperitoneally (IP) with 1 ml of fecal homogenate from crows orally gavaged with 5ml infected mouse brains.
- Group 2 - Negative treatment mice inoculated IP with 1 ml of fecal homogenate from crows orally gavaged with 5ml normal mouse brains.
- Dilute infected and normal mouse brain homogenate for Groups 3 and 4 to 1:100 w/v in 1x PBS.
- Group 3 - Positive control mice inoculated IP with 1 ml of infected mouse-brain homogenate.
- Group 4 - Negative control mice inoculated IP with 1 ml of normal mouse-brain homogenate.
| Treatment Group | Number of Animals | |
| Group 1 | Scrapie + Crow Feces | 100 |
| Group 2 | Scrapie - Crow Feces | 25 |
| Group 3 | Scrapie + Mouse Brain | 10 |
| Group 4 | Scrapie - Mouse Brain | 5 |
Table 1. Scrapie status of inoculum (positive +, negative -) and number of animals used7.
- Intraperitoneally inoculate mouse:
- Scruff mouse by dorsal neck fur with thumb and index finger and gently rotate to expose ventral side.
- Elevate posterior end of mouse so head is slightly lower.
- Insert 25 G needle 1 cm through skin, 1 cm lateral of midline, and 1-2 cm anterior to the sacroiliac joint using a needle-locking syringe.
- Inject 1 ml inoculate slowly into mouse body cavity.
3. Mouse Monitoring
Monitor mice daily until they express clinical signs of mouse scrapie. Clinical signs may include: kyphosis, ataxia, stiff tail, lack of grooming, emaciation, and lethargy.
Score mice for each of the 6 clinical signs when visible signs are evident, where 0 = none visible, 1 = moderate, and 2 = severe.
Euthanize mice when total daily scores for each sign reach ≥8 for 1 day, ≥ 6 continuously for 3 days, or at 365 days post inoculation (dpi).
Harvest brains immediately following euthanasia and store at -70 °C.
To confirm a scrapie diagnosis, digest brain samples with 3 µl of a 50 µg/ml of proteinase-K solution (PK) diluted as follows: 3.1. µl PK, 12.5 µl of 500 mM EDTA, pH 8, 109.39 µl of 1x PBS for 30 min at 45 °C, then inactivate the PK by adding 8 µl loading buffer and incubating samples at 95 °C for 5 min. Load samples onto a 12% SDS-PAGE gel, electrophorese and transfer to Immobilon PVDF membrane and block with 5% nonfat milk in 0.2% Tween 20 in PBS for 1 hr at room temperature. Then probe with Bar224 anti-PrP monoclonal antibody conjugated to Horseradish peroxidase, diluted in Superblock, for 1 hr at room temperature. Rinse membrane for 1 hr with PBS-0.2% Tween 20. To visualize, incubate Western blot 5 min with chemiluminescent substrate and image on a G-box gel documentation system.
Representative Results
The procedures used demonstrate that the digestive system of crows does not eliminate PrPRes infectivity 4 hr after oral gavage of scrapie brain homogenate7. All twenty crows that were gavaged with PrPRes material subsequently transmitted PrPRes material via feces to mice. Diseased mice were identified by manifestation of clinical mouse-scrapie signs and disease confirmation was completed by Western blot analysis.
Investigation of the retention time of material ingested by crows revealed passage time through the alimentary tract for a gavaged crow to be 4 hr, based on the presence of dye in feces (Figure 1). All feces were collected with disposable pipettes and pooled for each crow (Figure 2). Acute toxicity from untreated crow feces occurred when raw fecal supernatant was injected IP into pilot test mice. By treating fecal inoculate with penicillin and streptomycin, UV light, and sonication we alleviated this problem.
All mice inoculated with either scrapie-positive mouse brain (9/9) or feces from scrapie-inoculated crows (66*/84) developed clinical signs and tested positive by Western blot analysis (Figure 3), illustrating that scrapie readily passed through the digestive system of crows and caused disease. *Eighteen mice died within 3 days of inoculation, likely due to toxicity. All but one (1/23) scrapie-negative inoculated mice were negative by Western blot analysis. We hypothesize that this mouse was inadvertently inoculated with scrapie-positive crow feces instead of feces from a scrapie-negative crow.
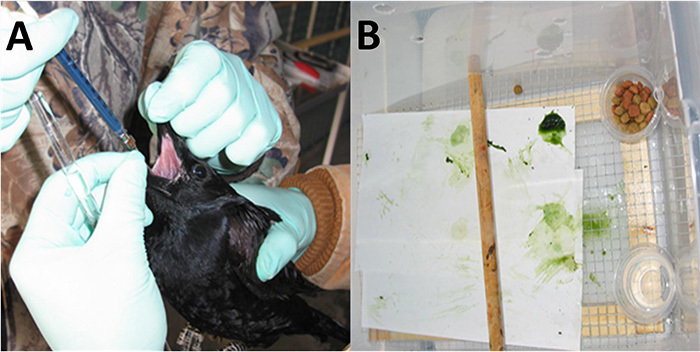 Figure 1. Crow manually restrained and orally gavaged with 5 ml of whole egg mixed with blue dye (A) and blue/green-stained feces 4 hr post gavage (B).Click here to view larger image.
Figure 1. Crow manually restrained and orally gavaged with 5 ml of whole egg mixed with blue dye (A) and blue/green-stained feces 4 hr post gavage (B).Click here to view larger image.
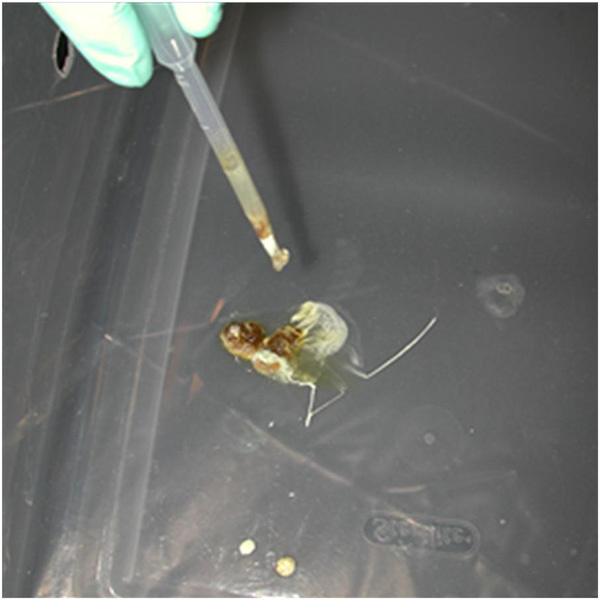 Figure 2. Crow feces collection with pipette prior to homogenization.Click here to view larger image.
Figure 2. Crow feces collection with pipette prior to homogenization.Click here to view larger image.
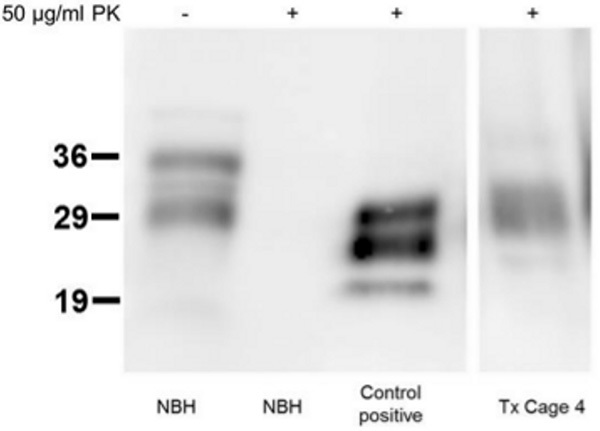 Figure 3. Representative SDS-Page Western blot of mouse brain from bioassay. NBH- normal mouse brain homogenate, scrapie-negative, TX cage 4 - brain from a mouse inoculated with feces from a scrapie-inoculated crow. With (+) and without (-) PK (proteinase K) digestion. Click here to view larger image.
Figure 3. Representative SDS-Page Western blot of mouse brain from bioassay. NBH- normal mouse brain homogenate, scrapie-negative, TX cage 4 - brain from a mouse inoculated with feces from a scrapie-inoculated crow. With (+) and without (-) PK (proteinase K) digestion. Click here to view larger image.
Discussion
We demonstrate a procedure to document passage of PrPRes material through the digestive system of crows. We used conventional methods to determine if crows have the ability to translocate PrPRes material to disease-free geographic areas. Others have evaluated resistance of PrPRes to ruminant19-21 and rodent22,23 digestive fluids, both of which failed to eliminate it. Future application of these techniques should be applied to other carnivores24 as they could also potentially encounter PrPRes material in carrion and transport this material across the landscape facilitating the spread of prion diseases.
We added blue food coloring to our scrambled egg 'pseudo brain' material, providing a simple way to assess approximate passage time of homogenized mouse brain through the alimentary tract of crows. We advise others considering this technique to first inspect existing feces color of study animals and then use food coloring that is most contrasting. This will allow for easy identification of food color stained material that has passed through study animals. We chose to use food coloring to estimate passage time, but others have used florescent pigment25, ferric oxide26, colored plastic markers27, and colored metallic flakes (i.e. glitter)28.
Minimizing the threat of a secondary microbial infection from crow feces and correctly inoculating mice are key starting points for mouse-prion studies that require long incubation periods. If either of these considerations are violated, early mouse mortality is likely to result.
Another possible tool for investigation is serial protein misfolding cyclic amplification or sPMCA to evaluate crow fecal samples over time to establish how long after oral gavage crows pass infectious material, without the need for a mouse bioassay. Recent advances in PMCA fecal analysis by Pulford, et al. indicate that amplification of minute levels of prions can be detected in mammal feces29, suggesting PMCA might also be a useful tool for evaluating avian feces. The mouse bioassay and sPMCA approach could be used to evaluate residual infectivity in feces of crows gavaged with CWD-infected material. A cervidized transgenic mouse line would be required and intracerebral versus intraperitoneal inoculation would give more rapid results.
Avian scavengers, such as crows, vultures, and eagles, could play a role in the spread of TSE diseases, namely CWD in North America. These species could consume CWD-positive tissue from diseased carcasses or entrails (in the case of hunter-killed cervids) and translocate infectious material in their feces to CWD-free areas or populations of cervids. As the practice of feeding grain to cervids, in wild or captive settings, attracts crows which can defecate on the food source and be inadvertently consumed by cervids, is thus a high-risk practice (VerCauteren personal observation). Further, though the odds of CWD-free animals encountering PrPRes material through random feces deposition may be low, areas where crows and thus their feces are concentrated, like below communal roosting sites, could become of high-risk areas for disease transmission since prions are so persistent in the environment30,31.
Disclosures
No conflicts of interest declared.
Acknowledgments
We would like to thank S. Werner for providing the crows used in this study and USDA, APHIS, WS, NWRC animal care staff for animal care and monitoring. Mention or use of a product does not imply USDA endorsement. Funding for this study was provided by USDA, APHIS, Veterinary Services.
References
- Prusiner SB. Novel proteinaceous infectious particles cause scrapie. Science. 1982;216(4542):136–144. doi: 10.1126/science.6801762. [DOI] [PubMed] [Google Scholar]
- Miller MW, Williams ES, et al. Epizootiology of chronic wasting disease in free-ranging cervids in Colorado and Wyoming. Journal of Wildlife Diseases. 2000;36(4):676–690. doi: 10.7589/0090-3558-36.4.676. [DOI] [PubMed] [Google Scholar]
- Miller MW, Williams ES. Horizontal prion transmission in mule deer. Nature. 2003;425(6953):35–36. doi: 10.1038/425035a. [DOI] [PubMed] [Google Scholar]
- Sigurdson CJ, Adriano A. Chronic Wasting Disease. Biochimica et Biophysica Acta. 2007;1772(6):610–618. doi: 10.1016/j.bbadis.2006.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MW, Williams ES, Hobbs NT, Wolfe LL. Environmental sources of prion transmission in mule deer. Emerging Infectious Diseases. 2004;10(6):1003–1006. doi: 10.3201/eid1006.040010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathiason CK, Hays SA, et al. Infectious prions in pre-clinical deer and transmission of chronic wasting disease solely by environmental exposure. PLoS ONE. 2009;4(6):e5916. doi: 10.1371/journal.pone.0005916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VerCauteren KC, Pilon JL, Nash PB, Phillips GE, Fischer JW. Prion remains infectious after passage through digestive system of American crows (Corvus crachyrhunchos) PLoS ONE. 2012;7(10):e45774. doi: 10.1371/journal.pone.0045774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imran M, Mahmood S. An overview of animal prion diseases. Virology Journal. 2011;8(493) doi: 10.1186/1743-422X-8-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts JC, Balachandran A, Westaway D. The expanding universe of prion disease. PLoS PATHOGENS. 2006;2(3):e26. doi: 10.1371/journal.ppat.0020026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce ME, et al. Transmissions to mice indicate that 'new variant' CJD is caused by the BSE agent. Nature. 1997;389(6650):498–501. doi: 10.1038/39057. [DOI] [PubMed] [Google Scholar]
- Ryder S, Dexter G, Bellworty S, Tongue S. Demonstration of lateral transmission of scrapie between sheep kept under natural conditions using lymphoid tissue biopsy. Research in Veterinary Science. 2004;76(2004):211–217. doi: 10.1016/j.rvsc.2003.11.007. [DOI] [PubMed] [Google Scholar]
- Collinge J. The risk of prion zoonoses. Science. 2012;335(6067):411–413. doi: 10.1126/science.1218167. [DOI] [PubMed] [Google Scholar]
- Beringue V, Vilotte JL, Laude H. Prion agent diversity and species barrier. Veterinary Research. 2008;39(47) doi: 10.1051/vetres:2008024. [DOI] [PubMed] [Google Scholar]
- Harrington RD, Baszler T, et al. A species barrier limits transmission of chronic wasting disease to mink (Mustela vison) The Journal of General Virology. 2008;89(4):1086–1096. doi: 10.1099/vir.0.83422-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisniewski HM, Sigurdarson S, Rubenstein R, Kascsak RJ, Carp RI. Mites as vectors for scrapie. Lancet. 1996;347(9008):1114. doi: 10.1016/s0140-6736(96)90310-4. [DOI] [PubMed] [Google Scholar]
- Post K, Riesner D, Walldorf V, Mehlhorn H. Fly larvae and pupae as vectors for scrapie. Lancet. 1999;354(9194):1969–1970. doi: 10.1016/S0140-6736(99)00469-9. [DOI] [PubMed] [Google Scholar]
- Matthews D, Cooke BC. The potential for transmissible spongiform encephalopathies in non-ruminant livestock and fish. Revue Scientifique Et Technique-Office International Des Epizooties. 2003;22(1):283–296. doi: 10.20506/rst.22.1.1393. [DOI] [PubMed] [Google Scholar]
- Jennelle CS, Samuel MD, Nolden CA, Berkley EA Deer carcass decomposition and potential scavenger exposure to chronic wasting disease. Journal of Wildlife Management. 2009;73(5):655–662. [Google Scholar]
- Scherbel C, Pichner R, et al. Degradation of scrapie associated prion protein (PrPSc) by the gastrointestinal microbiota of cattle. Veterinary Research. 2006;37(5):695–703. doi: 10.1051/vetres:2006024. [DOI] [PubMed] [Google Scholar]
- Jeffrey M, Gonzaález L, et al. Transportation of prion protein across the intestinal mucosa of scrapie susceptible and scrapie-resistant sheep. Journal of Pathology. 2006;209(1):4–14. doi: 10.1002/path.1962. [DOI] [PubMed] [Google Scholar]
- Nicholson EM, Richt JA, Rasmussen MA, Hamir AN, Lebepe-Mazur S, Horst RL. Exposure of sheep scrapie brain homogenate to rumen-simulating conditions does not result in a reduction of PrP(Sc) levels. Letters in Applied Microbiology. 2007;44(6):631–636. doi: 10.1111/j.1472-765X.2007.02124.x. [DOI] [PubMed] [Google Scholar]
- Motes C Maluquerde, Grassi J, et al. Excretion of BSE and scrapie prions in stools from murine models. Veterinary Microbiology. 2008;131(1-2):205–211. doi: 10.1016/j.vetmic.2008.02.014. [DOI] [PubMed] [Google Scholar]
- Kruger D, Thomzig A, Lenz G, Kampf K, McBride P, Beekes M. Faecal shedding, alimentary clearance and intestinal spread of prions in hamsters fed with scrapie. Veterinary Research. 2009;40(1):4. doi: 10.1051/vetres:2008042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathiason CK, Nalls AV, et al. Susceptibility of domestic cats to chronic wasting disease. Journal of Virology. 2013;87(4):1947–1956. doi: 10.1128/JVI.02592-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorndal KA. Flexibility of digestive responses in two generalist herbivores, the tortoises Geochelone carbonaria and Geochelone denticulate. Oecologia. 1989;78(3):317–321. doi: 10.1007/BF00379104. [DOI] [PubMed] [Google Scholar]
- Clark RG, Gentle GC. Estimates of grain passage time in captive mallards. Canadian Journal of Zoology. 1990;68(11):2275–2279. [Google Scholar]
- Dierenfeld ES, Koontz FW. Feed intake, digestion and passage of proboscis monkey (Nasalis larvatus) in captivity. Primates. 1992;33(3):399–405. [Google Scholar]
- Thompson AK, Samuel MD, Van Deelen TR. Alternative feeding strategies and potential disease transmission in Wisconsin white-tailed deer. Journal of Wildlife Management. 2008;72(2):416–421. [Google Scholar]
- Pulford B, Spraker TA, et al. Detection of PrPCWD in feces from naturally exposed Rocky Mountain elk (Cervus elaphus nelsoni) using protein misfolding cyclic amplification. Journal of Wildlife Diseases. 2012;48(2):425–433. doi: 10.7589/0090-3558-48.2.425. [DOI] [PubMed] [Google Scholar]
- Hicks RE. Guano deposition in an Oklahoma crow roost. Condor. 1979;81(3):247–250. [Google Scholar]
- Aldous SE. Winter habits of crows in Oklahoma. Journal of Wildlife Management. 1944;73(4):290–295. [Google Scholar]


