Abstract
Introduction: Ceramide-containing moisturizers may offer benefits as an adjunct to acne treatment. Methods: An expert panel of 11 Canadian dermatologists, including an international clinical scientist, used the following modified Delphi process: 1) A systematic literature review for acne treatment, dry skin, irritation, depletion of ceramides in acne, and benefits of moisturizers and ceramide-containing moisturizers was conducted; 2) panel members gave their opinion on the resulting statements, taking into account their treatment practices; 3) a panel meeting was held during the 2011 Canadian Dermatology Update to determine final statements; 4) the panel reviewed the final document. Results: The panel reached the following consensus (11/11): 1) A very important reason for nonadherence to acne treatment is dry skin and irritation; 2) skin barrier dysfunction may contribute to acne; 3) dry skin and irritation commonly results from topical acne treatment; 4) dry skin and irritation commonly results from systemic retinoid therapy; 5) moisturizers can improve dryness and irritation resulting from acne treatment; 6) ceramide-containing moisturizers may enhance adherence and complement existing acne therapies; 7) adjunctive therapy with moisturizers should be considered in acne-treated patients. Conclusion: The panel proposes that adjunctive therapy with moisturizers, particularly ceramide-containing moisturizers, should be considered in acne-treated patients.
Acne vulgaris is a chronic inflammatory dermatosis that consists clinically of open and closed comedones, papules, pustules, and nodules.1 It is a common skin disease, affecting 40 to 50 million individuals of all races and ethnicities.2–4 Acne vulgaris traditionally is thought to be related to hormonal factors producing excess sebum production leading to open and closed comedones, papules, pustules, and cysts. New developments have looked at additional pathogenic factors, such as altered sebum lipid quality, regulation of steroidogenesis in the skin, interaction with neuropeptidases, androgen activity, and nutrition.5
There are multiple acne therapies, including systemic and topical retinoids, antibacterials, systemic and topical antibiotics, and benzoyl peroxide (BPO).6–9
Many of the medications that are typically used can cause skin irritation and dry skin conditions and may lead to nonadherence and thus treatment failure.10–13 Other reasons for nonadherence may be the complexity of the treatment and unattractive aspect of the treatment products. Optimal skin care, such as the concomitant use of moisturizers including ceramide-containing moisturizers as an adjunct to acne treatment, may offer therapeutic benefits. A modified Delphi panel procedure was used to explore this further.
ROLE OF THE PANEL
An expert panel was established to explore possible benefits to the use of moisturizers and ceramide-containing moisturizers for acne patients. The panel comprised 11 nationally recognized dermatologists, who practice in Canada in medical dermatology, including an advisor with an international clinical and scientific background in this field. The group included: Chuck W. Lynde, MD, FRCPC; Anneke Andriessen, PhD; Benjamin Barankin, MD, FRCPC; Gillian de Cannes, MD, FRCPC; Wayne Gulliver, MD, FRCPC; Richard Haber, MD, FRCPC; Catherine McCuaig, MD, FRCPC; Poonam Rajan, MD, DABD, FRCPC (C); Sandra P. Skotnicki, MD, FRCPC; Richard Thomas, MD, FRCPC; Jack Toole, MD, FRCPC; Ron Vender, MD, FRCPC.
The panel population is representative of the healthcare providers likely to assess and to treat patients with acne. The care described by the panel may be better than typical acne skin care because panel members treat a high proportion of patients with acne and are well-trained in this area. However, selecting a panel composed of opinion leaders was deemed appropriate to ensure that a high quality of care is established.
METHODS
The procedure. A systematic literature review was carried out on PubMed and Google for topical acne treatment and skin irritation as well as dry skin conditions, depletion of ceramides in acne patients’ skin, and possible benefits of the use of moisturizers in general and ceramide-containing moisturizers in particular (Table 1). Further, a secondary analysis of related citations and references was conducted. The following keywords were used: topical acne treatment, adherence, concordance, efficacy, safety, tolerability, dry skin, skin irritation, moisturizers and acne, ceramide-containing moisturizers and acne, depletion of ceramides and acne, adjunctive treatment with ceramide-containing moisturizers.
TABLE 1.
Websites and key words used for the systematic literature review
| A systematic literature review was carried out on the use of moisturizes and treatment of acne, using the following keywords: topical acne treatment, adherence, concordance, efficacy, safety, tolerability, dry skin, skin irritation, moisturizers an acne, ceramide-containing moisturizers and acne, depletion of ceramides and acne adjunctive treatment with ceramide-containing moisturizers. The panel searched published studies, which met the following criteria: publications in English, Germ; French or Dutch; with human subjects including reviews, reports, and meta-analyses | |
|---|---|
| DATABASES SEARCHED | DETAILS |
| COCHRANE Database | Cochrane Dermatology—website: www.doctor411network.com/Alabama/Cochrane-dermatology.html |
| MEDSCAPE | http://www.medscape.com/home |
| MEDLINE | Pubmed; http://www.pubmed.de/data/nlm.link.html |
| EMBASE | Excerpta Medica DataBase; in DIMDI database; www.elsevier.com/locate/dermven |
| CINAHL | Cumulative Index to Nursing and Allied Health Literature: www.cinahl.com/library/journals.htmwww.trcc.commnet.edu/library/guides/.../Cinahl_search_guide.htm |
| National Library of Medicine (acne, dry skin, skin irritation) | www.nlm.nih.gov/medlineplus/ency/article/003250.htm |
| AAD and supported by the AAD | http://www.aad.org/public/publications/pamphlets/acne.htmwww.aad.org/public/publications/pamphlets/acne.html health.yahoo.com/skinconditions.../acne.../healthwise— hw107895.html www.cigna.com/healthinfo/hw107895.html |
| TVS | The Tissue Viability Society (TVS)—Glanville Centre, Salisbury District Hospital, Salisbury SP2 8BJ, UK www.tvs.org.uk |
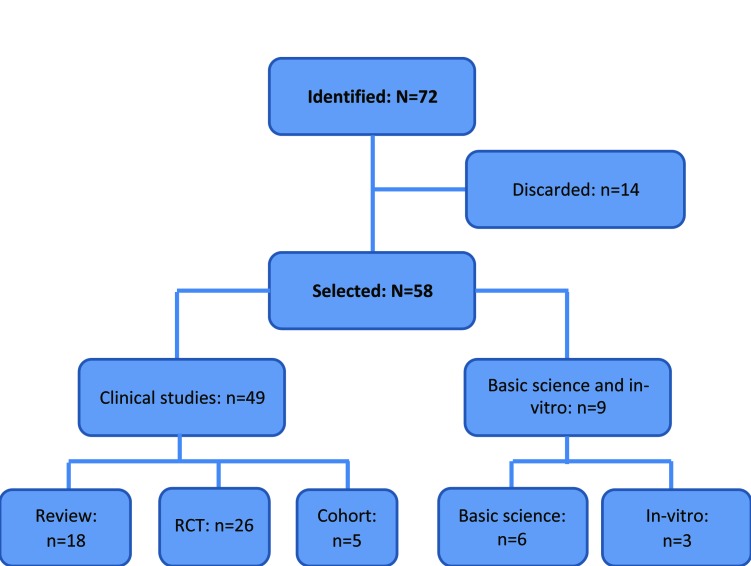
Results of the literature search. Seventy-two studies were identified, 58 of which were selected for the panel discussion (Figure 1). The results were checked for the inclusion criteria and trial quality using a standardized literature evaluation form. Existing systematic reviews (e.g., Cochrane) and other guidelines served as additional steering for the body of evidence used. Pooling of the studies was not attempted due to the lack of common outcome measures and endpoints. A limitation was that most studies looked at acne treatment and did not specifically consider the evaluation of moisturizers as an adjunct therapy. The discarded studies were mostly poor quality or were reviews of already included studies. The literature search findings were categorized according to the level of evidence (Table 2). The results showed that in general, dry skin and skin irritation in acne treatment are reasons for acne patients not to adhere to treatment leading to poor outcomes.10-19
Figure 1.
Literature search: Identified and selected studies
TABLE 2.
The levels of evidence are based on Cochrane59 methodology
| LEVELS OF EVIDENCE | DEFINITION |
|---|---|
| 1 | Evidence obtained from a systematic review of all relevant randomized controlled trials. |
| 2 | Evidence obtained from at least one properly designed randomized controlled trial. |
| 3.1 | Evidence obtained from well-designed, pseudo-randomized controlled trials |
| 3.2 | Evidence obtained from comparative studies with concurrent controls and allocation not randomized, cohort studies, case-control studies, or interrupted time series with a control group. |
| 3.3 | Evidence obtained from comparative studies with historical control, two or more single arm studies, or interrupted time series without a parallel control group. |
| 4 | Evidence obtained from case studies, either post-test or pretest/ post-test |
Research suggests that lipid bilayer deficiencies compromise skin barrier integrity, with dry skin being the most common adverse effect.6-14 Furthermore, acne patients have a deficiency in total ceramides and free sphingosine.5,20-25 Therefore, skin barrier dysfunction, coupled with various triggering events, may contribute to the signs and symptoms of acne.3,5,22-25 There is evidence of benefits of the use of moisturizers as well as application of ceramides containing moisturizers.18,21,26-32 The goal of use of moisturizers is to improve skin condition reducing irritation and inflammation.33-39 This may result in a more rapid improvement in the acne and skin condition than could be achieved in other circumstances and also improve patient adherence and treatment efficacy34 In vitro and in vivo studies showed a strong antimicrobial effectiveness of skin-identical phytosphingosine produced by ceramides.36-39 Both in vitro and in vivo, the phytosphingosine-containing product showed excellent clinical results in the context of skin care in acne, based on both anti-inflammatory and antimicrobial activity.37-41
These results demonstrate the potential of ceramide containing products to enhance or complement existing acne therapies acting as an active cosmetic ingredient. The findings were summarized as follows: reasons for nonadherence to topical acne treatment (Table 3), skin irritation as a result of topical acne treatment (Table 4), skin barrier dysfunction in acne (Table 5), benefits of moisturizers (Table 6), and moisturizers for acne (Table 7).
TABLE 8.
Results of the panel discussion
| # | STATEMENTS DISCUSSED BY THE PANEL | VOTE: N=11 |
|---|---|---|
| 1 | Very important reason for nonadherence to acne treatment is dry skin and skin irritation | 11/11 |
| 2 | Dry skin and skin irritation commonly results from topical acne treatment | 11/11 |
| 3 | Dry skin and skin irritation commonly results from systemicretinoids | 11/11 |
| 4 | Skin barrier dysfunction may contribute to the signs and symptoms of acne | 11/11 |
| 5 | Moisturizers can improve skin dryness and skin irritation resulting from acne treatment | 11/11 |
| 6 | Ceramide-containing moisturizers may enhance adherence and complement existing acne therapies | 11/11 |
| 7 | Adjunctive therapy with moisturizers should be considered in acne-treated patients | 11/11 |
TABLE 3.
Reasons for nonadherence to topical acne treatment
| # | AUTHORS/JOURNAL | TITLE | NONADHERENCE | EVIDENCE LEVEL |
|---|---|---|---|---|
| 1 | Tan JK, Balagurusamy M, Fung K et al. J Cutan Med Surg. 2009;13(4):204-208. | Effect of quality of life impact and clinical severity on adherence to topical acne treatment. | Adherence was significantly positively correlated with improved quality of life. | 2 |
| 2 | Gollnick H, Cunliffe W, Berson D, et al. J Am Acad Dermatol. 2003;49(1 Suppl):S1-S37. | Global Alliance to Improve Outcomes in Acne. Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. | Simplify treatment and make it more comfortable causing less irritation and dryness. | 2 |
| 3 | Yentzer BA, Baldwin H, Shalita A, et al. J Drugs Dermatol. 2010;9:S92-S95. | Optimizing patient adherence: update on combination acne therapy—teens and beyond. | Improving treatment making it more comfortable with less skin irritation. | 2 |
| 4 | Koo J. Skinmed. 2003;2:229-233. | How do you foster medication adherence for better acne vulgaris management? | Complicated treatment regimen for children together with the chronic nature of the disease and skin irritation lead to poor medication adherence. | 2 |
| 5 | Carroll CL, Feldman SR, Camacho FT, et al. J Am Acad Dermatol. 2004;51:212-216. | Adherence to topical therapy decreases during the course of an 8-week psoriasis clinical trial: commonly used methods of measuring adherence to topical therapy overestimate actual use. | Patients explain that failing to properly use their medications is in part due to forgetfulness and frustration with skin irritation. | 2 |
TABLE 4.
Dry skin and skin irritation related to topical acne treatment
| # | AUTHORS/JOURNAL | TITLE | DRY SKIN AND SKIN IRRITATION | EVIDENCE LEVEL |
|---|---|---|---|---|
| 1 | Drealos ZD, Callender V, Young C, Sunil SD. Cutis. 2008;82:281-284. | The effect of vehicle formulation on acne medication tolerability. | Dryness and peeling and irritation occur in topical treatment with BPO and retinoids. | 2 |
| 2 | Thiboutot DM, Weiss J, Bucko A, et al. J Am Acad Dermatol. 2007;57:791-799. | Adapalene-benzoyl peroxide, a fixed-dose combination for the treatment of acne vulgaris: results of a multicenter, randomized double-blind, controlled study. | AEs reported were dry skin, erythema and desquamation. Similar adverse event frequency and tolerability profile for combination gel vs. adapalene monotherapy. | 2 |
| 3 | Andres P, Pernin C, Poncet M. Cutis. 2008;81:278-284. | Adapalene-benzoyl peroxide once-daily, fixed-dose combination gel for the treatment of acne vulgaris: a randomized, bilateral (split-face), dose-assessment study of cutaneous tolerability in healthy participants. | Adapalene 0.1%-BPO 5% caused more irritation than BPO 5% or 10% monotherapy. | 1 |
| 4 | Troielli PA, Asis B, Bermejo A, et al. Skinmed. 2010;8:17-22. | Community study of fixed-combination adapalene 0.1% and benzoyl peroxide 2.5% in acne. | Erythema, scaling, itching, burning, and stinging were all reported. | 2 |
| 5 | Gollnick HP, Draelos Z, Glenn MJ, et al. Br J Dermatol. 2009;161:1180-1189. | Adapalene-benzoyl peroxide, a unique fixed-dose combination topical gel for the treatment of acne vulgaris: a transatlantic, randomized, double-blind, controlled study in 1,670 patients. | AEs dry skin, erythema and desquamation. Adapalene-BPO showed significantly greater efficacy than monotherapies. | 2 |
| 6 | Gold LS, Tan J, Cruz-Santana A, et al. Cutis. 2009;84:110-116. | A North American study of adapalene-benzoyl peroxide combination gel in the treatment of acne. | AEs reported were dry skin, erythema, and desquamation.Comparable safety of adapalene-BPO to monotherapies and gel vehicle. | 2 |
| 7 | Poulin Y, Sanchez NP, Bucko A, et al. Br J Dermatol. 2011 Apr 1; [Epub ahead of print]. | A 6-month maintenance therapy with adapalene-benzoyl peroxide gel prevents relapse and continuously improves efficacy among severe acne vulgaris patients: results of a randomized controlled trial | AEs reported were dry skin, erythema, and desquamation for adapalene-BPO. | 2 |
| 8 | Zouboulis CC, Fischer TC, Wohlrab J, Barnard J, Alio AB. Cutis. 2009;84:223-229. | Study of the efficacy, tolerability, and safety of 2 fixed-dose combination gels in the management of acne vulgaris. | RCT: Combination therapies adapalene-BPO and BPO/clin: application site dryness, desquamation, burning, erythema, and pruritus occurred and were less common in subjects using clindamycin. | 2 |
| 9 | Loesche C, Pernin C, Poncet M. Eur J Dermatol. 2008;18:524-526. | Adapalene 0.1% and benzoyl peroxide 2.5% as a fixed-dose combination gel is as well tolerated as the individual components alone in terms of cumulative irritancy. | Study analyzed tolerability only; no significant difference in irritation indices for adapalene-BPO vsmonotherapies. With erythema and desquamation as the most frequent AEs | 2 |
TABLE 5.
Skin barrier dysfunction and acne treatment
| # | AUTHORS/JOURNAL | TITLE OF STUDY | SKIN BARRIER DYSFUNCTION AND ACNE TREATMENT | LEVEL OF EVIDENCE |
|---|---|---|---|---|
| 1 | Kurokawa I, Dan by FW, Ju Q, et al. Exp Dermatol. 2009;18(10):821-832. | New developments in our understanding of acne pathogenesis and treatment. | Skin barrier dysfunction coupled with various triggering events contributes to the signs and symptoms of acne. | 2 |
| 2 | Pavicic T, Wollenweber U, Farwick, et al. Int J Cosmet Sci. 2007;29(3):181-190. | Anti-microbial and -inflammatory activity and efficacy of Phytosphingosine (PS): an in vitro and in vivo study addressing acne vulgaris. | In acne-affected skin, PS is depleted leading to an impaired skin barrier, inflammation, and infection. | 2 |
| 3 | Jeremy AH, Holland DB, Roberts SG, Thomson KF, Cunliffe WJ. J Invest Dermatol. 2003:121(1): 20-27. | Inflammatory events are involved in acne lesion initiation. | In acne-affected skin, Phytosphingosine is depleted, making the skin prone to inflammation. | 2 |
| 4 | Yamamoto A, Takenouchi K, Ito M. Arch Dermatol Res. 95;287(2):214-218. | Impaired water barrier function in acne vulgaris. | In acne, lower amounts of ingolipids were observed corresponding with diminished WBF. | 2 |
| 5 | Madison KC. J Invest Dermatol. 2003;121(2):231-241. | Barrier function of the skin: “la raison d’etre” of the epidermis | Skin barrier dysfunction mechanisms are described. | 3 |
| 6 | Johnson AW. In: Draelos ZD, ed. Procedures in Cosmetic Dermatology Series: Cosmeceuticals. 1st ed. Philadelphia: Elsevier; 2005:97-102 | Cosmeceuticals: Function and the skin barrier. | Cholesterol, ceramides and fatty acid are important components of lipid bilayers. | 3 |
| 7 | Elias PM, Hatnano Y, Williams ML. J Alter Clin Immunol. 2008;121:1337-1343. | Skin barrier dysfunction mechanisms in inflammatory dermatosis. | Skin barrier dysfunction leading to inflammation. | 1 |
TABLE 6.
Benefits of moisturizers for acne
| # | AUTHORS/JOURNAL | TITLE OF STUDY | BENEFITS OF MOISTURIZERS FOR ACNE | LEVEL OF EVIDENCE |
|---|---|---|---|---|
| 1 | Feldman SR, Chen DM. J Drugs Dermatol. 2011;10(6):605-608. | How patients experience and manage dryness and irritation from acne treatment. | 41 percent of subjects reported using moisturizers to counteract dryness and redness and benefitted from a moisturizer. | 3 |
| 2 | Yamamoto A, Takenouchi K, Ito M. Arch Dermatol Res. 1995;287:214-218. | Impaired water barrier function in acne vulgaris. | A dysfunctional skin barrier has been shown to provoke increased transepidermal water loss (TEWL), resulting in pronounced cutaneous dehydration. | 2 |
| 3 | Bouwstra J Pilgram G, Gooris G, Körten H, Ponec M. Skin Pharmacol Appl Skin Physiol. 2001;14 Suppl 1:52-62. | New aspects of the skin barrier organization. | It is shown that a balanced application of SC-identical lipids, such as pure ceramides or a combination thereof with cholesterol and fatty acids should replenish any low levels of stratum corneum lipids. | 2 |
| 4 | Shalita AR, Smith JG, Parish LC, Sofman MS, Chalker DK. Int J Dermatol. 1995;34(6):434-437. | Topical nicotinamide compared with clindamycin gel in the treatment of inflammatory acne vulgaris | Moisturizing is important for acne-prone skin. Moisturizers keep skin hydrated and balanced and often serves as a vehicle for antioxidants and nutrients, as well as treatments for acne. However, oily skin should be treated with the gentlest and lightest oil-free moisturizers. | 3 |
| 5 | Draelos ZD. Dermatol Clin. 2000;18(4):597-607. | Therapeutic moisturizers. | Moisturizers keep skin hydrated and balanced and reduces skin irritation. | 3 |
| 6 | Lynde CW. Skin Therapy Lett. 2001;6(13):3-5. | Moisturizers: what they are and how they work. | Moisturizers keep skin hydrated and repair skin barrier damage due to topical treatment. | 3 |
TABLE 7.
Benefits of ceramides containing moisturizers for acne
| # | AUTHORS/JOURNAL | TITLE OF STUDY | BENEFITS OF MOISTURIZERS FOR ACNE | LEVEL OF EVIDENCE |
|---|---|---|---|---|
| 1 | Pavicic T, Wollenweber U, Farwick M, Korting HC. Int J Cosmet Sci. 2007;29(3):181-190. | Anti-microbial and -inflammatory activity and efficacy of phytosphingosine: an in vitro and in vivo study addressing acne vulgaris. | Both in vitro and in vivo the phytosphingosine containing product showed excellent clinical results in acne, based on anti-inflammatory and anti-microbial activity, enhancing or complementing existing acne therapies. | 2 |
| 2 | Yamamoto A, Takenouchi K, Ito M. Arch Dermatol Res. 1995;287(2):214-218. | Impaired water barrier function in acne vulgaris. | In acne lower amounts of sphingolipids correspond with a diminished water barrier function (WBF). An impaired WBF caused by decreased amounts of ceramides may be responsible for comedo formation, since barrier dysfunction is accompanied by hyperkeratosis of the follicular epithelium. | 2 |
| 3 | Imokawa G. In: Leyden JJ, Rawlings AV, eds. Skin Moisturization. 1st ed. New York: Marcel Dekker; 2002:267-302. | Ceramides as natural moisturizing factors and their efficacy in dry skin. | Ceramides are instrumental in the skin barrier function. Topical ceramides help improve skin barrier function in acne-affected skin. | 2 |
| 4 | Bouwstra J, Pilgram G, Gooris G, Koerten H, Ponec M. Skin Pharmacol Appl Skin Physiol. 2001;14 Suppl 1:52-62. | New aspects of the skin barrier organization. | A balanced application of stratum corneum identical lipids, pure ceramides or a combination thereof with cholesterol and fatty acids replenish low levels of stratum corneum lipids. | 2 |
| 5 | Del Rosso JQ. Cosmetic Dermatol. 2007;20(8):485-490 | The role of skin care and maintaining proper barrier function in the management of rosacea. | The amount of ceramides present in the stratum corneum decreases drastically, because keratinocytes have a reduced ability to synthesize certain classes are reduced, especially the quantity of phytosphingosine-based ceramides like Ceramide 3. | 2 |
| 6 | Draelos ZD. Plast Reconstr Surg. 2010;125(2):719-724. | Active agents in common skin care products. | The use of a ceramide-containing moisturizing cream and cleanser in conjunction with fluocinonide cream 0.05% reduced disease duration, time to disease clearance. | 3 |
| 7 | Loden M. Am J Clin Dermatol. 2003;4(11):771-778. | Role of topical emollients and moisturizers in the treatment of dry skin barrier disorders. | A ceramide-dominant lipid mixture decreased transepidermal water loss. | 3 |
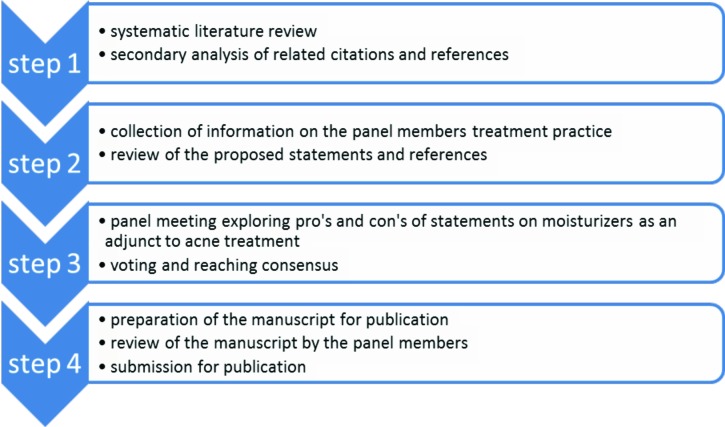
MODIFIED DELPHI METHOD
After this literature review, a modified Delphi method was used to collect further information on treatment practice. Panel members gave their opinions on the statements that resulted from the search regarding their individual practice in caring for acne patients and the use of moisturizers and ceramide-containing moisturizers. A panel reviewed the document and statements and selected studies. A meeting was then held with the same panel members who previously reviewed the document during the Canadian Dermatology Update 2011 conference in Montreal to explore pros and cons of moisturizes and ceramide-containing moisturizers for acne patients.
The advisor guided the meeting, where the panel members reviewed a summary of all responses, reached a consensus as to the meaning of each question, and then provided a final response and wording about their treatment of patients with acne using moisturizers.
A modified Delphi process was also used to determine the final statements. The final document and statements were edited and reviewed by the panel after the meeting (Figure 2).
Figure 2.
Procedure: Modified Delphi Method
STATEMENTS FOR THE PANEL DISCUSSION
The initial statements were put together as a result of a literature search, secondary analysis of related citations, and references. The panel addressed these in the meeting. They were asked to give their opinions, looking at the issues from a clinical perspective, and were given the opportunity to adapt the statements, after which the panel voted. Consensus was reached when 9 of the 11 dermatologist who participated in the panel agreed with the statement. At the end of the meeting, the panel reached a full (11/11) consensus on all seven modified statements. On the rationale of why to use a moisturizer for acne, the following was discussed and agreed: 1) moisturizers in acne patients help repair the defective moisture barrier function, help prepare the skin for treatment, and protect against further damage; 2) when moisturizers have incorporation of ceramides, components of the intercellular lipids, they are capable of protecting the skin. These moisturizers replenish ceramides and help repair the skin barrier.
DISCUSSION
The panel agreed that there is evidence to support that a very important reason for nonadherence to acne treatment is dry skin and skin irritation.8,16-29,42 They further agreed that dry skin and skin irritation commonly results from topical acne treatment and from systemic retinoids.43-58
The panel recognized that skin barrier dysfunction may contribute to the signs and symptoms of acne.3-5,20-25 Pathogenic factors, such as altered sebum lipid quality regulation of steroidogenesis in the skin, interaction with neuropeptidases, androgen activity, and nutrition, contribute to acne development.3,22 In acne-affected skin, the barrier function is impaired and decreased water binding leads to a decrease in skin moisture and a reduction in skin surface lipids (ceramides).5,22 Phytosphingosine occurs naturally in the stratum corneum, both in its free form and as a part of the major fraction of ceramides. It plays a crucial role in permeability barrier function and cutaneous antimicrobial defense. In acne-affected skin, phytosphingosine is depleted, leading to an impaired skin barrier, inflammation, and infection.22 Furthermore, the lower amounts of sphingolipids were observed corresponding with a diminished water barrier function. This situation is proposed to lead to comedo formation, since barrier dysfunction is accompanied by hyperkeratosis of the follicular epithelium.5,22 Cholesterol, ceramides, and fatty acid are important components of lipid bilayers. Ceramides play a crucial role in the stratum corneum structure and the regulation of skin barrier homeostasis.36 Most skin barrier disorders in inflammatory dermatosis are therefore characterized by a decreased ceramide content.30-32
The skin type and stage of disease has to be taken into consideration when choosing the vehicle for topical treatments. The efficacy and safety/tolerability of topical treatments are largely influenced by the choice of vehicle. A delivery technology, which provides a controlled release of ceramides and other ingredients slowly over time, may allow the ingredients to better penetrate into the skin, preventing moisture loss. The ceramide-containing cleansers and moisturizers used in acne-prone skin are to be noncomedogenic , nonirritating, and fragrance-free.
The panel members agreed that moisturizers can improve skin dryness and skin irritation resulting from acne treatment. They further agreed that ceramide-containing moisturizers may enhance adherence and complement existing acne therapies. The panel therefore proposes that adjunctive therapy with moisturizers and ceramides containing moisturizers should be considered in acne-treated patients.
A cohort study is initiated to evaluate the clinical efficacy of moisturizers in acne patients.
CONCLUSION
The goal for the use of moisturizers and ceramide-containing moisturizers as an adjunctive acne therapy is to improve skin condition, reducing irritation and inflammation. This may result in a more rapid improvement in the acne and skin condition than could be achieved in other circumstances and improved adherence to the prescribed therapy.
Footnotes
DISCLOSURE:The panel consisted of 11 nationally recognized dermatologists who practice in Canada in medical dermatology. The meeting was held during the Canadian Dermatology Update 2011 conference in Montreal. The participating panel members received a stipend.
REFERENCES
- 1.Katsambas A, Dessinioti C. New and emerging treatments in dermatology: acne. Dermatol Titer. 2008;21:86–95. doi: 10.1111/j.1529-8019.2008.00175.x. [DOI] [PubMed] [Google Scholar]
- 2.White GM. Recent findings in the epidemiologic evidence, classification, and subtypes of acne vulgaris. J Am Acad Dermatol. 1998;39:S34–S37. doi: 10.1016/s0190-9622(98)70442-6. [DOI] [PubMed] [Google Scholar]
- 3.Gollnick H. Current concepts of the pathogenesis of acne: implications for drug treatment. Drugs. 2003;63:1579–1596. doi: 10.2165/00003495-200363150-00005. [DOI] [PubMed] [Google Scholar]
- 4.Perkins AC, Cheng CE, Hillebrand GG, et al. Comparison of the epidemiology of acne vulgaris among Caucasian, Asian. Continental Indian and African American women. J Eur Acad Dermatol Venereol. 2011;25(9):1054–1060. doi: 10.1111/j.1468-3083.2010.03919.x. [DOI] [PubMed] [Google Scholar]
- 5.Kurokawa I, Danby FW, Ju Q, et al. New developments in our understanding of acne pathogenesis and treatment. Exp Dermatol. 2009;18:821–832. doi: 10.1111/j.1600-0625.2009.00890.x. [DOI] [PubMed] [Google Scholar]
- 6.Leyden JJ. A review of the use of combination therapies for the treatment of acne vulgaris. J Am Acad Dermatol. 2003;49:S200–S210. doi: 10.1067/s0190-9622(03)01154-x. [DOI] [PubMed] [Google Scholar]
- 7.Wolf JE, Jr, Kaplan D, Kraus SJ, et al. Efficacy and tolerability of combined topical treatment of acne vulgaris with adapalene and clindamycin: a multicenter, randomized, investigator-blinded study. J Am Acad Dermatol. 2003;49:S211–S217. doi: 10.1067/s0190-9622(03)01152-6. [DOI] [PubMed] [Google Scholar]
- 8.Abdel-Naser MB, Zouboulis CC. Clindamycin phosphate/tretinoin gel formulation in the treatment of acne vulgaris. Expert Opin Pharmacother. 2008;9:2931–2937. doi: 10.1517/14656566.9.16.2931. [DOI] [PubMed] [Google Scholar]
- 9.Wolf JE., Jr. Potential anti-inflammatory effects of topical retinoids and retinoid analogues. Adv Ther. 2002;19:109–118. doi: 10.1007/BF02850266. [DOI] [PubMed] [Google Scholar]
- 10.Yentzer BA, Ade RA, Fountain JM, et al. Simplifying regimens promotes greater adherence and outcomes with topical acne medications: a randomized controlled trial. Cutis. 2010;86:103–108. [PubMed] [Google Scholar]
- 11.Koo J. How do you foster medication adherence for better acne vulgaris management? Skinmed. 2003;2:229–233. doi: 10.1111/j.1540-9740.2003.02037.x. [DOI] [PubMed] [Google Scholar]
- 12.Carroll CL, Feldman SR, Camacho FT, et al. Adherence to topical therapy decreases during the course of an 8-week psoriasis clinical trial: commonly used methods of measuring adherence to topical therapy overestimate actual use. J Am Acad Dermatol. 2004;51:212–216. doi: 10.1016/j.jaad.2004.01.052. [DOI] [PubMed] [Google Scholar]
- 13.Yentzer BA, Baldwin H, Shalita A, et al. Optimizing patient adherence: update on combination acne therapy—teens and beyond. J Drugs Dermatol. 2010;9:S92–S95. [Google Scholar]
- 14.Feneran AN, Kaufman WS, Dabade TS, Feldman SR. Retinoid plus antimicrobial combination treatments for acne. Clin Cosmet Investig Dermatol. 2011;4:79–92. doi: 10.2147/CCID.S13873. 2011 Jul 1. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tan JK, Balagurusamy M, Fung K, et al. Effect of quality of life impact and clinical severity on adherence to topical acne treatment. J Cutan Med Surg. 2009;13(4):204–208. doi: 10.2310/7750.2009.08055. [DOI] [PubMed] [Google Scholar]
- 16.Lee IA, Maibach HI. Pharmionics in dermatology: a review of topical medication adherence. Am J Clin Dermatol. 2006;7(4):231–236. doi: 10.2165/00128071-200607040-00004. [DOI] [PubMed] [Google Scholar]
- 17.Bucks D, Sarpotdar P, Yu K, et al. The development and optimization of a fixed combination of clindamycin and benzoyl peroxide aqueous gel with minimal irritation and enhanced bioavailability. J Drugs Dermatol. 2009;8(7):634–638. [PubMed] [Google Scholar]
- 18.Leyden JJ, Grossman R, Nighland M. Cumulative irritation potential of topical retinoid formulations. J Drugs Dermatol. 2008;7(8 SuppI):S14–S18. [PubMed] [Google Scholar]
- 19.Bucks DAW, Pillai RS, McCall-Perez F. Advances in formulation technologies: creating highly effective and well-tolerated topical dermatologicals. Skin & Aging. 2010 July. [Supplement]. [Google Scholar]
- 20.Motta S, Sesana S, Monti M, et al. A domain mosaic model of the skin barrier function. Arch Dermatol. 1994;130:452–456. [PubMed] [Google Scholar]
- 21.Chamlin SL, Kao J, Frieden IJ, et al. Ceramide-dominant barrier repair lipids alleviate childhood atopic dermatitis. J Am Acad Dermatol. 2002;47(2):198–208. doi: 10.1067/mjd.2002.124617. [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto A, Takenouchi K, Ito M. Impaired water barrier function in acne vulgaris. Arch Dermatol Res. 1995;287:214–218. doi: 10.1007/BF01262335. [DOI] [PubMed] [Google Scholar]
- 23.Madison KC. Barrier function of the skin: “la raison d’etre” of the epidermis. J Invest Dermatol. 2003;121(2):231–241. doi: 10.1046/j.1523-1747.2003.12359.x. [DOI] [PubMed] [Google Scholar]
- 24.Johnson AW. Cosmeceuticals: function and the skin barrier. In: Draelos ZD, editor. Procedures in Cosmetic Dermatology Series: Cosmeceuticals. 1st ed. Philadelphia: Elsevier.; 2005. pp. 97–102. [Google Scholar]
- 25.Bouwstra J, Pilgram G, Gooris G, et al. New aspects of the skin barrier organisation. Skin Pharmacol Appl Skin Physiol. 2001;14:52–62. doi: 10.1159/000056391. [DOI] [PubMed] [Google Scholar]
- 26.Draelos ZD. Therapeutic moisturizers. Dermatol Clin. 2000;18(4):597–607. doi: 10.1016/s0733-8635(05)70210-2. [DOI] [PubMed] [Google Scholar]
- 27.Kraft JN, Lynde CW. Moisturizers: what they are and how they work. Skin Therapy Lett. 2001;6(13):3–5. [PubMed] [Google Scholar]
- 28.Jensen JM, Folster-Holst R, Baranowsky A, et al. Skin barrier function. J Invest Dermatol. 2004;122:1423–1431. doi: 10.1111/j.0022-202X.2004.22621.x. [DOI] [PubMed] [Google Scholar]
- 29.Del Rosso JQ. Newer topical therapies for the treatment of acne vulgaris. Cutis. 2007;80(5):400–410. [PubMed] [Google Scholar]
- 30.Del Rosso JQ. The role of skin care and maintaining proper barrier function in the management of rosacea. Cosmetic Dermatol. 2007;20(8):485–488. [Google Scholar]
- 31.Draelos ZD. Active agents in common skin care products. Plast Reconstr Surg. 2010;125(2):719–724. doi: 10.1097/PRS.0b013e3181c83192. [DOI] [PubMed] [Google Scholar]
- 32.Draelos ZD. The effects of ceramide-containing skin care products on eczema resolution duration. Cutis. 2008;81:87–91. [PubMed] [Google Scholar]
- 33.Loden M. Role of topical emollients and moisturizers in the treatment of dry skin barrier disorders. Am J Clin Dermatol. 2003;4(11):771–778. doi: 10.2165/00128071-200304110-00005. [DOI] [PubMed] [Google Scholar]
- 34.Feldman SR, Chen DM. How patients experience and manage dryness and irritation from acne treatment. J Drags Dermatol. 2011;10(6):605–608. [PubMed] [Google Scholar]
- 35.Del Rosso JQ. Understanding skin cleansers and moisturizers: the correlation of formulation science with the art of clinical use. Cosmet Dermatol. 2003;16:19–31. [Google Scholar]
- 36.Castiel-Higounenc I, Chopard M, Ferraris C. Stratum corneum lipids: specificity, role, deficiencies and modulation. Oleagineux, Corps Gras, Lipides. 2004;11:401–106. [Google Scholar]
- 37.Imokawa G. Ceramides as natural moisturizing factors and their efficacy in dry skin. In: Leyden JJ, Rawlings AV, editors. Skin Moisturization. 1st ed. New York: Marcel Dekker; 2002. pp. 267–302. [Google Scholar]
- 38.Tanno O, Ota Y, Kitamura N, et al. Nicotinamide increases biosynthesis of ceramides as well as other stratum corneum lipids to improve the epidermal permeability barrier. Br J Dermatol. 2000;143:524–531. doi: 10.1111/j.1365-2133.2000.03705.x. [DOI] [PubMed] [Google Scholar]
- 39.Ghering W, Gloor M. Effect of topically applied dexpanthenol on epidermal barrier function and stratum corneum hydration. Arzneim-Forsch/Drug Res. 2000;50:659–663. doi: 10.1055/s-0031-1300268. [DOI] [PubMed] [Google Scholar]
- 40.Ebner F, Heller A, Rippke F, et al. Topical use of dexpanthenol in skin disorders. Am J Clin Dermatol. 2002;3:427–433. doi: 10.2165/00128071-200203060-00005. [DOI] [PubMed] [Google Scholar]
- 41.Pavicic T, Wollenweber U, Farwick M, Korting C. Anti-microbial and -inflammatory activity and efficacy of phytosphingosine: an in vitro and in vivo study addressing acne vulgaris. J Cosmet Sci. 2007;29:181–190. doi: 10.1111/j.1467-2494.2007.00378.x. [DOI] [PubMed] [Google Scholar]
- 42.Jeremy AHT, Holland DB, Roberts SG, et al. Inflammatory events are involved in acne lesion initiation. J Invest Dermatol. 2003;121:20–27. doi: 10.1046/j.1523-1747.2003.12321.x. [DOI] [PubMed] [Google Scholar]
- 43.Gollnick HP, Draelos Z, Glenn MJ, et al. Adapalene-benzoyl peroxide, a unique fixed-dose combination topical gel for the treatment of acne vulgaris: a transatlantic, randomized, double-blind, controlled study in 1670 patients. Br J Dermatol. 2009;161:1180–1189. doi: 10.1111/j.1365-2133.2009.09209.x. [DOI] [PubMed] [Google Scholar]
- 44.Loesche C, Pernin C, Poncet M. Adapalene 0.1% and benzoyl peroxide 2.5% as a fixed-dose combination gel is as well tolerated as the individual components alone in terms of cumulative irritancy. Eur J Dermatol. 2008;18:524–526. doi: 10.1684/ejd.2008.0488. [DOI] [PubMed] [Google Scholar]
- 45.Drealos ZD, Callender V, Young C, Sunil SD. The effect of vehicle formulation on acne medication tolerability. Cutis. 2008;82:281–284. [PubMed] [Google Scholar]
- 46.Andres P, Pernin C, Poncet M. Adapalene-benzoyl peroxide once-daily, fixed-dose combination gel for the treatment of acne vulgaris: a randomized, bilateral (split-face), dose-assessment study of cutaneous tolerability in healthy participants. Cutis. 2008;81:278–284. [PubMed] [Google Scholar]
- 47.Thiboutot DM, Weiss J, Bucko A, et al. Adapalene-benzoyl peroxide, a fixed-dose combination for the treatment of acne vulgaris: results of a multicenter, randomized double-blind, controlled study. J Am Acad Dermatol. 2007;57:791–799. doi: 10.1016/j.jaad.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 48.Troielli PA, Asis B, Bermejo A, et al. Community study of fixed-combination adapalene 0.1% and benzoyl peroxide 2.5% in acne. Skinmed. 2010;8:17–22. [PubMed] [Google Scholar]
- 49.Gold LS, Tan J, Cruz-Santana A, et al. A North American study of adapalene-benzoyl peroxide combination gel in the treatment of acne. Cutis. 2009;84:110–116. [PubMed] [Google Scholar]
- 50.Poulin Y, Sanchez NP, Bucko A, et al. A 6-month maintenance therapy with adapalene-benzoyl peroxide gel prevents relapse and continuously improves efficacy among severe acne vulgaris patients: results of a randomized controlled trial. Br J Dermatol. doi: 10.1111/j.1365-2133.2011.10344.x. 2011 Apr 1. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 51.Zouboulis CC, Fischer TC, Wohlrab J, et al. Study of the efficacy tolerability, and safety of 2 fixed-dose combination gels in the management of acne vulgaris. Cutis. 2009;84:223–229. [PubMed] [Google Scholar]
- 52.Shalita AR, Smith JG, Parish LC, et al. Topical nicotinamide compared with clindamycin gel in the treatment of inflammatory acne vulgaris. Int J Dermatol. 1995;34(6):434–437. doi: 10.1111/j.1365-4362.1995.tb04449.x. [DOI] [PubMed] [Google Scholar]
- 53.Zouboulis CC, Derumeaux L, Decroix J, et al. A multicentre, single-blind, randomized comparison of a fixed clindamycin phosphate/tretinoin gel formulation (Velac) applied once daily and a clindamycin lotion formulation (Dalacin T) applied twice daily in the topical treatment of acne vulgaris. Br J Dermatol. 2000;143:498–505. doi: 10.1111/j.1365-2133.2000.03701.x. [DOI] [PubMed] [Google Scholar]
- 54.Thiboutot D, Gollnick H, Bettoli V, et al. Global Alliance to Improve Outcomes in Acne. New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol. 2009;60(5 Suppl):Sl–S50. doi: 10.1016/j.jaad.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 55.Gollnick H, Cunliffe W, Berson D, et al. Global Alliance to Improve Outcomes in Acne. Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2003;49(1 Suppl):SlSS7. doi: 10.1067/mjd.2003.618. [DOI] [PubMed] [Google Scholar]
- 56.Schlessinger J, Menter A, Gold M, et al. Clinical safety and efficacy studies of a novel formulation combining 1.2% clindamycin phosphate and 0.025% tretinoin for the treatment of acne vulgaris. J Drags Dermatol. 2007;6:607–615. [PubMed] [Google Scholar]
- 57.Eichenfield LF, Wortzman M. A novel gel formulation of 0.25% tretinoin and 1.2% clindamycin phosphate: efficacy in acne vulgaris patients aged 12 to 18 years. Pediatr Dermatol. 2009;26:257–261. doi: 10.1111/j.1525-1470.2008.00862.x. [DOI] [PubMed] [Google Scholar]
- 58.Kircik LH, Peredo MI, Bucko AD, et al. Safety of a novel gel formulation of clindamycin phosphate 1.2%-tretinoin 0.025%: results from a 52-week open-label study. Cutis. 2008;82:358–366. [PubMed] [Google Scholar]