SUMMARY
Background
Functional dyspepsia (FD), a common functional gastrointestinal disorder, is defined by the Rome III criteria as symptoms of epigastric pain or discomfort (prevalence in FD of 89–90%), postprandial fullness (75–88%), and early satiety (50–82%) within the last 3 months with symptom onset at least 6 months earlier. Patients cannot have any evidence of structural disease to explain symptoms and predominant symptoms of gastroesophageal reflux are exclusionary. Symptoms of FD are non-specific and the pathophysiology is diverse, which explains in part why a universally effective treatment for FD remains elusive.
Aim
To present current management options for the treatment of FD (therapeutic gain/response rate noted when available).
Results
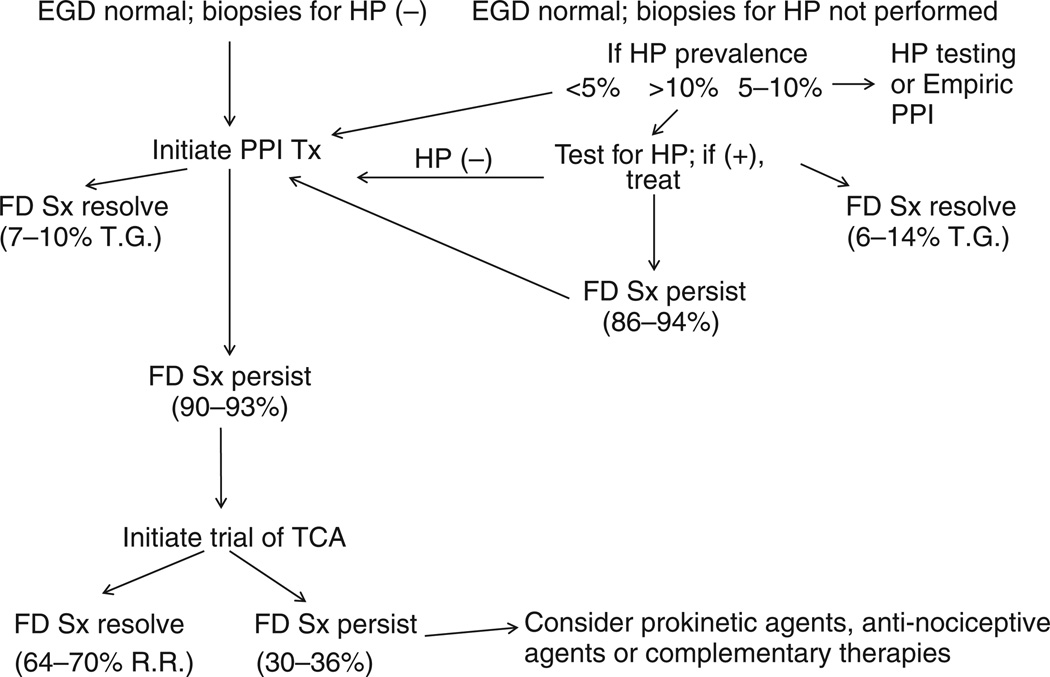
The utility of Helicobacter pylori eradication for the treatment of FD is modest (6–14% therapeutic gain), while the therapeutic efficacy of proton pump inhibitors (PPI) (7–10% therapeutic gain), histamine-type-2-receptor antagonists (8–35% therapeutic gain), prokinetic agents (18–45%), tricyclic antidepressants (TCA) (response rates of 64–70%), serotonin reuptake inhibitors (no better than placebo) is limited and hampered by inadequate data. This review discusses dietary interventions and analyses studies involving complementary and alternative medications, and psychological therapies.
Conclusions
A reasonable treatment approach based on current evidence is to initiate therapy with a daily PPI in H. pylori-negative FD patients. If symptoms persist, a therapeutic trial with a tricyclic antidepressant may be initiated. If symptoms continue, the clinician can possibly initiate therapy with an antinociceptive agent, a prokinetic agent, or some form of complementary and alternative medications, although evidence from prospective studies to support this approach is limited.
INTRODUCTION
Healthcare providers of all specialties routinely evaluate patients for symptoms of dyspepsia. The prevalence of dyspepsia in the general population has been estimated to be 20–40% and the majority of these patients are believed to have FD.1 A systematic review found that the prevalence of FD (after normal upper endoscopy) is 12–15%,2 while the incidence of dyspepsia (most of whom have FD) has been calculated at <1% over 3 months to up to 2.8% per year.3, 4 The natural history of FD has not been well characterised, although the limited available data suggest that approximately 50% of patients remain symptomatic over a 5-year follow-up period.2
Functional dyspepsia, defined by Rome III criteria, is the presence of symptoms thought to originate in the gastroduodenal region in the absence of any organic, systemic, or metabolic disease likely to explain the symptoms.5 In their recent guidelines, the Rome committee introduced two new subcategories for FD - postprandial distress syndrome (PDS) and epigastric pain syndrome (EPS; see Table 1). Recent studies have shown that these two subcategories accurately reflect clinical patients.6, 7 Epigastric pain or discomfort is the hallmark symptom in patients with FD. The word discomfort is important to emphasise, as many patients will not complain of pain, but rather state that they have burning, pressure or fullness in the epigastric area, or cannot finish a normalsized meal (early satiety). Other common symptoms that occur in FD patients include post prandial nausea, belching and abdominal bloating. Frustratingly, symptoms of FD do not consistently predict underlying pathophysiology and do not reliably guide therapy.8–10.
Table 1.
Rome III criteria for functional dyspepsia (modified from reference 5)
| For the two categories noted below, criteria must be fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis. Patients must have one or more of the following symptoms: |
| - Postprandial fullness |
| - Early satiety |
| - Epigastric burning |
| In addition, patients cannot have any evidence of structural disease that is likely to explain symptoms (i.e. upper endoscopy is normal). |
| A. Postprandial distress syndrome |
| Diagnostic criteria must include both the following: |
| - Bothersome postprandial fullness, occurring after ordinary sized meals, at least several times per week |
| - Early satiation that prevents finishing a regular meal, at least several times per week |
| - Other supporting criteria: |
| - Upper abdominal bloating or postprandial nausea or excessive belching can be present |
| - Epigastric pain syndrome may coexist |
| B. Epigastric Pain Syndrome |
| Diagnostic criteria must include all of the following: |
| - Pain or burning localised to the epigastrium, of at least moderate severity at least once per week |
| - The pain is intermittent |
| - Not generalised or localised to other abdominal or chest regions |
| - Not relieved by defecation or passage of flatus |
| - Not fulfilling criteria for biliary pain |
| Supportive criteria: |
| - The pain may be of a burning quality, but without a retrosternal component |
| - The pain is commonly induced or relieved by ingestion of a meal, but may occur while fasting |
| - Postprandial distress syndrome may coexist |
Functional dyspepsia markedly reduces patients’ quality of life and imparts a significant economic burden to the healthcare system.11 This reduction in quality of life is similar to that experienced by patients with mild heart failure and menopause.12 Interestingly, a lower quality of life is in itself an independent risk factor for developing dyspepsia (odds ratio = 2.63; 99% CI 1.86–3.71; 4). The economic impact of FD should not be underestimated. Analysing data from the Leeds UK HELP (Helicobacter pylori eradication in general practice) study, the costs of evaluating and treating dyspepsia were estimated to be 1 billion pounds per year.12 A recent retrospective analysis of health insurance claims of over 275 000 US employees determined that FD patients incurred costs that were $5138 greater than employees without FD.13
The treatment of FD can be confusing to healthcare providers because no medication is currently approved in the US, Canada or the European Union for the treatment of FD. However, recent clinical trials have provided new information on the management of FD.14 The purpose of this narrative review is to evaluate treatment options available for FD patients and provide recommendations using the most recent data from the literature.
METHODS
Literature review
The goal of this article is to provide a narrative review of management options for FD. To accomplish this, a comprehensive search of the published literature using the PubMed database was performed. For Ovid MED-LINE and PubMed (1966 to December 2011) separate searches using the 3 key terms ‘functional dyspepsia’, ‘dyspepsia’ and ‘non-ulcer dyspepsia’ (English language) were combined (using the ‘AND’ operator) with ‘adults’, followed by additional search terms as text terms and (where appropriate) MeSH headings including all of the medications and therapies described in the text. Results focused on human trials, English language, adults and full manuscripts; abstracts were included only if the information was felt to be critical to the manuscript. References within studies that met selection criteria were manually searched for other potentially relevant studies. Studies were excluded from analysis for the following reasons: FD was not specifically defined; the study was retrospective in nature; study duration was less than 4 weeks; a placebo group was not included; total sample size <20 subjects; and randomisation did not occur. Although the Rome III criteria for FD now include subcategories of EPS and PDS, with the exception of acotiamide, the treatment section below did not address management changes in these subcategories, since prospective trials comparing symptom responses in these two subgroups are lacking.
RESULTS
Diet
Diet has been implicated in the pathogenesis of functional gastrointestinal disorders. As nutrient intake modulates upper gastrointestinal sensorimotor function, it is likely that patterns of nutrient intake will influence symptoms in FD and, by corollary, that diet modification may improve FD symptoms. Systematic studies of dyspeptic symptoms both in the general population and in specialised referral centres have revealed that the majority of individuals report induction or worsening of symptoms after meal ingestion.3, 7, 15 However, the possible contribution of specific foods and macronutrients and other dietary habits to the induction and/or exacerbation of dyspeptic symptoms has been poorly studied, often showing conflicting results. Pilichiewicz et al. compared detailed diet diaries in 20 FD patients to 21 healthy controls.16 They found that patients with FD ate fewer meals and consumed less total energy and fat compared to controls. Fullness and bloating were directly related to the amount of fat ingested, while only fullness was inversely related to the amount of carbohydrate ingested. In a recent population-based case-control study, 99 FD patients and 119 controls completed a validated food frequency questionnaire.17 FD patients reported consuming more fat and less carbohydrate than controls. No differences were seen in intake of total calories, fibre, protein or micronutrients. Furthermore, there were no differences in intake of frequently suspected ‘culprit’ foods such as wheat- and lactose-containing foods, caffeinated beverages and fructose-sweetened drinks. Further supporting a potential role of fat in FD symptom generation are studies showing that FD patients more often experience symptoms after intraduodenal infusions of fat.18, 19 In contrast to the above studies, a case-control study of 100 FD subjects did not find that these patients ate substantially differently from healthy controls,20 nor did a recent study of 41 FD patients and 30 healthy controls.21 While the above do not support global alterations in diet as being of primary importance in FD symptom generation, the role of specific food sensitivities and fat require additional study.
It is likely that patients modify their dietary habits to avoid symptoms. Current treatments for FD have generally ignored the potential role of diet. Given the heterogeneous nature of FD, the challenge of a dietary approach lies in the identification of patients who are likely to respond to this therapy. As part of the clinical evaluation of the FD patient, a diary to prospectively assess dyspeptic symptoms in temporal association with eating patterns may be useful. Dietary modifications such as consuming smaller meals with reduced fat intake represent a promising target for FD therapy but have yet to be rigorously studied.
Eradication of Helicobacter pylori
A prior gastrointestinal infection is associated with FD in some patients.22 One of the most common gastric infections, H. pylori can create a cascade of events leading to gastric inflammation and immune activation.3, 5, 8, 9 Thus, it appears plausible that H. pylori could cause FD and as a natural extension of that theory, eradication of H. pylori should improve FD symptoms.9 However, the benefits of H. pylori eradication in the treatment of FD are significantly more limited than in peptic ulcer disease. The most recent Cochrane database meta-analysis reviewed 21 Randomized Controlled Trials (RCTs) evaluating H. pylori eradication and the effects on FD symptoms. Seventeen trials involving 3566 patients reported outcomes in a dichotomous fashion and were grouped together for analysis due to lack of significant heterogeneity between the groups.23 A small but significant symptomatic benefit to eradicating H. pylori in FD patients was found [relative risk reduction (RRR), 10%; 95% CI, 6–14 (therapeutic gain)], with a number needed to treat (NNT) of 14. A recent study of 195 Chinese FD patients (Rome III criteria) with H. pylori found that symptoms of epigastric pain and epigastric burning were more likely to improve with H. pylori treatment compared to placebo (overall response rate of 60.8–65.7% vs. 33.3–31.8% respectively; P < 0.05). However, other dyspeptic symptoms (nausea, belching, early satiety, postprandial fullness) did not improve.24 Finally, a just-published prospective study of 404 Brazilian FD patients using Rome III criteria (70% women; mean age = 46) found that 49% of patients treated with a proton pump inhibitor (PPI) and two antibiotics met the primary endpoint at 12 months (50% improvement in symptoms) compared to 37% of FD patients treated with a daily PPI (P = 0.01;25).
Empiric treatment for presumed (undocumented) H. pylori in FD patients is not recommended due to the low likelihood of achieving symptomatic improvement, concern about widening antibiotic resistance, and the reduced prevalence of H. pylori in many Western countries.26 The American Gastroenterological Association recommends H. pylori test and treat as the initial management strategy for uncomplicated dyspepsia in patients younger than 55 years if the prevalence of infection is >10%. Empiric PPI therapy is recommended as the initial management strategy in these same patients when H. pylori prevalence is low (<5%; 9).
Histamine-type 2 receptor antagonists (H2RAs)
A Cochrane review of RCTs from 1966 to 2006 evaluated the effectiveness of six classes of drugs including histamine H2 receptor antagonists (antacids, histamine H2 antagonists, PPIs, prokinetics, mucosal protecting agents and antimuscarinics) in the improvement of either the individual or global dyspepsia symptom scores in patients with non-ulcer dyspepsia.27 We did not identify additional more recently published RCTs since that review.
Twelve RCTs28–39 compared H2RAs with placebo evaluating a total of 2183 participants. None of these trials involved patients defined as having FD using Rome III criteria. An average of 54% of participants had a statistically significant improvement in dyspeptic symptoms with H2RA therapy compared with 40% in the placebo arm (RRR = 23%; 95% CI = 8–35 therapeutic gain). The NNT with H2RAs to improve one case of dyspepsia was seven subjects (95% CI = 5–21). The median length of follow-up in the trials in this review was 4 weeks with the maximum evaluation time being 12 weeks. Overall, the quality of most trials was poor. There was statistically significant heterogeneity between studies. However, analysis of the type of H2RA, dose of drug, duration of therapy, method of randomisation, concealment of allocation and drop-out rate did not explain this heterogeneity. Since a proportion of FD patients may have gastroesophageal reflux disease (GERD) despite normal endoscopy, reduction in heartburn symptoms may have explained the results of improvement in these trials. Histamine-type 2 receptor antagonists theoretically might also improve symptoms by reducing microscopic gastric or duodenal inflammation due to acid or ameliorating gastroduodenal acid hypersensitivity.
A comparison of PPI therapy to H2RA therapy in a study of 588 participants with nonulcer dyspepsia showed a trend towards a better outcome based on global dyspepsia cure with a PPI, although the difference was not statistically significant.28 Two studies32, 40 showed a trend towards a worse outcome with H2RAs compared to prokinetic agents in regard to global dyspepsia improvement, while one study (n = 104) demonstrated a 33% relative risk reduction in favour of antacids (95% CI = 80 to −23).41 An RCT reported those receiving H2RAs were 2.7 times (95% CI = 1.3–6.0) more likely to have moderate or severe dyspepsia at the end of the trial than those allocated to sucralfate.42
The effect of H2RAs on individual dyspepsia symptoms was assessed in five RCTs.29, 30, 32, 34, 36 Epigastric pain (RRR = 19%; 95% CI = 4–32) and postprandial fullness (RRR = 29%; 95% CI = 0–49) were improved by H2RA therapy compared with placebo with no significant improvement in other individual symptoms.
In summary, participants with FD are more likely to respond to H2RAs than placebo in clinical trials. The effect of these drugs is likely to be small.
Proton pump inhibitors (PPIs)
Following on from their demonstrated success in the treatment of GERD and peptic ulcer, PPIs have been widely employed in the treatment of dyspeptic symptoms and in patients with the diagnosis of FD. However, evidence from RCTs suggests that the efficacy of PPIs in FD is limited and may be confined to those patients who have co-existing reflux symptoms.
Talley et al.43 found a modest benefit of omeprazole 10 or 20 mg once daily over placebo in a 4-week study. The benefit was not found in those with symptoms suggestive of dysmotility. Blum et al.44 compared two doses of omeprazole with ranitidine and placebo in a 2-week study in patients with FD; results were categorised according to H. pylori status. In general, the H. pylorinegative patients had better outcomes. A significant therapeutic gain of omeprazole over placebo was only evident in the H. pylori-positive subgroup. This was explained on the basis of the enhanced antisecretory effect seen with PPIs in the setting of H. pylori infection. However, these results were not confirmed in a later study by Bolling-Sternevald et al., who studied the effects of a higher dose of omeprazole – 20 mg b.i.d. – in FD patients, but excluded those with predominant heartburn. 45 They found a small but statistically significant benefit of omeprazole in a per protocol – but not in an intent-to-treat – analysis, and found no influence of H. pylori status on outcomes.
Wong et al.46 studied the effects of lansoprazole 15 or 30 mg once daily for 4 weeks in Chinese FD patients. They found no benefit of either dose of lansoprazole over placebo; indeed, patients on placebo had a higher rate of complete symptom relief than those on either dose of the PPI. In the US, Peura et al.47 similarly found no significant benefit of lansoprazole 15 or 30 mg once daily over placebo in two parallel 8-week studies in FD patients, having specifically excluded those with a diagnosis of GERD or who had heartburn as their predominant symptom. Patients who had some heartburn were more likely to respond to the PPI than those who did not. Van Zanten et al.48 studied the effect of esomeprazole 40 mg once daily for 8 weeks in FD patients. They also excluded patients who had heartburn or regurgitation as their predominant symptoms. Esomeprazole had no significant benefit over placebo on symptom relief at 8 weeks. Van Rensburg et al.49 randomised FD patients to pantoprazole 20 mg or placebo once daily for 4 weeks. They confined their study to FD patients with ‘ulcer-like’ symptoms. In this selected patient population, pantoprazole had a modest but statistically significant advantage over placebo. Finally, a trial of a high-dose PPI (esomeprazole 80 mg q day) for 1 week was of little value in predicting symptom response at 8 weeks in FD patients.50
A meta-analysis of placebo-controlled RCTs of PPIs in FD included 3725 patients across seven studies.51 Overall, this concluded that PPI treatment was superior to placebo with a NNT of 14.6. In subgroup analyses, they found that the benefit of PPI over placebo was confined to those patients with ‘ulcer-like’ and ‘reflux-like’ dyspepsia; they found no advantage of PPI treatment among patients with ‘dysmotility-like’ or unspecified dyspepsia.
Placebo-controlled RCTs of PPIs in FD have used variable inclusion criteria and outcomes measures. RCTs that studied specific sub-types of dyspepsia found the beneficial effect of PPIs to be confined to patients with ‘reflux-like’ or ‘ulcer-like’ dyspepsia. FD patients with some degree of heartburn have been more likely to respond to PPI treatment. This suggests that, mechanistically, some of the modest beneficial effect of PPI treatment in FD patients may be through the treatment of coexisting reflux symptoms. Alternatively, improving acid-induced injury or acid-induced hypersensitivity to gastric or duodenal mucosa may also contribute to symptom resolution. Overall, the effectiveness of PPI treatment in FD appears modest with a therapeutic gain of approximately 7–10%. Although some patients who carry the diagnosis of FD will respond favourably to PPI treatment, these agents should not be continued in those who do not respond after a reasonable treatment period of 4–8 weeks.
Prokinetic agents
A comprehensive and high quality systematic review and meta-analysis was conducted up to 2005 evaluating the role of prokinetics in FD. Fourteen trials, including 1053 patients, were identified (all but one trial testing cisapride, a mixed 5HT4 agonist and 5HT3 antagonist). The outcome was classified as dyspepsia improvement or not; a significant decrease in dyspepsia was observed with prokinetic therapy vs. placebo (relative risk 0.52; 95% CI, 0.37–0.73). However, the studies were highly heterogeneous casting some doubt on the actual effect size9 and cisapride has been withdrawn from the US market because of cardiac toxicity. The efficacy of domperidone in FD, also unavailable in the USA (except under an IND) but prescribed in Canada, Mexico and elsewhere, remains uncertain as high quality trials are unavailable.
A search since 2005 revealed two high quality RCTs testing the 5HT4 agonist tegaserod in 2667 women with FD.52 Only a very modest benefit was observed with an increase in days with satisfactory relief of 4.6% over placebo (95% CI, 2.29, 6.96). However, patients with severe FD symptoms were more likely to note symptom improvement compared to those with mild symptoms. Despite early promising results,53 itopride was no better than placebo in the Phase III study but is available in Japan.54 Of note, the Phase III studies excluded FD patients with concomitant reflux; post hoc analysis of the Phase II data showed that the presence of reflux was a factor in overall symptom improvement, although sub-analysis of the Holtmann study did not demonstrate that concomitant reflux improved response to therapy.53 Mosapride, available in Japan, was also no better than placebo in a dose finding study.55 A motilin agonist, ABT-229, failed to show superiority over placebo in FD.56 The potent 5HT4 agonist prucalopride is approved in Europe for chronic constipation but has not been properly evaluated in clinical FD trials.57, 58 In summary, although prokinetic agents are conceptually appealing given their potential to improve gastric emptying, and are commonly used throughout the world, the results in FD patients are underwhelming.
Tricyclic antidepressants
Systematic reviews have shown the TCA drugs to be effective in chronic pain syndromes 59 and in irritable bowel syndrome (IBS).60 Clinicians have also used TCAs in FD but the evidence for their efficacy is limited.61 Randomized Controlled Trials in healthy volunteers have shown that TCAs do not influence gastric motor function62 or improve satiety63 after a standard drink test. However, another RCT64 reported that TCAs reduced nausea in healthy volunteers after ingesting a high calorie liquid meal. A crossover randomised placebo-controlled trial of amitriptyline in seven FD patients reported a reduction in gastrointestinal symptoms while subjects were taking the active drug.65 The very small sample size and the crossover design minimise the reported positive outcome. A Japanese RCT evaluated amitriptyline in FD patients who had failed an H2RA or a prokinetic.66 Amitriptyline improved symptoms in 70% compared to 20% of those on placebo. This difference was statistically significant but with only 27 patients the magnitude of effect of TCAs in FD remains uncertain. Finally a Chinese study currently only published in abstract form was included due to the strength of the sample size.67 The authors reported that imipramine was effective in FD patients not responding to PPIs and prokinetics. A total of 107 patients were randomised and treated for 12 weeks with 64% responding in the treatment group and 44% responding in the placebo group. The NNT was 5 but the result was only marginally statistically significant (P = 0.04). In summary, although TCAs appear to make theoretical sense for the treatment of FD, the exceedingly small amount of data that are available makes it difficult to determine whether TCAs are effective in FD. Well-designed, prospective studies are desperately needed to determine whether there is a benefit, and if so, what mechanism of action is responsible for pain relief in FD patients. In particular it needs to be established whether the drug is acting to modulate pain in the nervous system either peripherally or centrally or whether the effects relate to any impact on anxiety and depression which often coexist in FD patients.61
Selective Serotonin Reuptake Inhibitors (SSRIs) and Selective Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs)
Clinicians often use SSRIs to treat symptoms of IBS, a highly prevalent disorder characterised by lower abdominal pain or discomfort. The rationale for this is that SSRIs may improve both central and visceral pain in some patients, in addition to treating co-existing anxiety or depression. Since IBS frequently co-exists with FD, and because FD patients are frequently hypersensitive to gastric distension, using SSRIs to treat the multiple symptoms of FD appears to be a natural extension of their use in IBS.68, 69 Surprisingly, only one study has been published on the use of SSRIs or SNRIs for the treatment of FD. Van Kerkhoven randomised 160 FD patients to receive either venlafaxine (an SNRI) or placebo for the 8-week study period.70 Symptoms, health-related quality of life, anxiety and depression were measured at baseline and up to 20 weeks after the end of medication therapy. No differences were found between venlafaxine and placebo. Based on this single study, no meaningful evidence-based recommendation can be made on the use of SSRIs or SNRIs for the treatment of FD.
Duloxetine, another selective serotonin and norepinephrine reuptake inhibitor (SNRI), warrants brief mention because a small pilot study suggested that it may be efficacious in IBS patients, and there is considerable symptom overlap between FD and IBS.68, 71 However, no trials in FD patients are available for review.
To help determine if antidepressants are truly efficacious in FD, a large, multi-centre, randomised, placebo-controlled study (Functional Dyspepsia Treatment Trial) comparing an SSRI to both a TCA and placebo is now underway and initial results should be available in 2014 (72; Clinical Trial Registration NCT00248651).
Acotiamide
Acotiamide a muscarinic antagonist and cholinesterase inhibitor, improves gastric motility and gastric emptying in rodents and dogs. Two small Phase II studies demonstrated an improvement in FD symptoms in patients treated with acotiamide.73, 74 A multicentre, randomised, placebo-controlled trial in 892 Japanese FD patients with PDS (59% women; mean age = 37 years; Rome III criteria) compared t.d.s. acotiamide (100 mg p.o.) to placebo for 4 weeks.14 The primary efficacy end points were global assessment of overall treatment efficacy (OTE) and elimination of three meal-related symptoms (early satiation, upper abdominal bloating and postprandial fullness). The authors reported that 52.2% of those receiving acotiamide had a global improvement in FD symptoms, compared to 34.8% of those in the placebo group (P < 0.001). Elimination of the three meal-related symptoms occurred in 15.3% of acotiamide patients compared to 9.0% of placebo-treated patients (P = 0.004). No serious adverse events (SAEs) thought secondary to the drug occurred; Adverse events (AEs) were similar between acotiamide (56%) and placebo-treated patients (60.4%; N. S.). These results are intriguing, although future studies need to be longer, multinational and include a large number of patients in a parallel study to identify the mechanism of action.
Anti-nociceptive agents
For FD patients with persistent symptoms who have failed therapeutic trials of agents described above, other anti-nociceptive agents are available, although data supporting their use are quite limited. Gabapentin was initially introduced as an antiepileptic, but has more recently been used in chronic pain syndromes. Pregabalin, which is structurally related to gabapentin, is approved for the management of certain pain disorders and as an adjunct for partial onset seizures and generalised anxiety. Studies suggest that these drugs impact the central processing of pain, and may impact autonomic function. Their most likely mechanism of action is via calcium channels on presynaptic neuronal membranes, and perhaps via modulation of pro-inflammatory pathways. 75 A post hoc analysis of data obtained from six RCTs in patients with generalised anxiety disorder and prominent gastrointestinal symptoms showed that pregabalin was significantly more effective than placebo in treating both anxiety and gastrointestinal symptoms.76
Carbamazepine is an anticonvulsant drug that is also used to treat several pain disorders and psychiatric conditions but has not been tested in FD. Tramadol is an analgesic combining mainly mu-opioid and monoaminergic actions that has been shown to be effective at treating acute visceral (e.g. post-operative) pain. There are no trials in FD patients.
Complementary and alternative medications (CAM)
At least one-third of the US population now uses some form of CAM on a routine basis, while 62% of US adults have used some form of CAM within the preceding 12 months.77, 78 STW 5-II is an herbal preparation containing extracts of bitter candy tuft, matricaria flower, peppermint leaves, caraway, licorice root and lemon balm. Adult patients (n = 120; 71% women; mean age = 44.6 years) meeting Rome I criteria for FD were evenly randomised to one of four different treatment groups (placebo-placebo, drug-drug, placebo-drug, drug-placebo), for a trial which consisted of two separate 4-week blocks of either placebo or STW 5-II (20 drops t.d. s.). The primary outcome variable was patient-rated improvement in gastrointestinal symptoms using a 5-point Likert scale.79 The authors reported that 43.3% of FD patients treated with STW 5-II had complete relief of their symptoms at 8 weeks compared to 3.3% of patients treated with placebo (P < 0.001). No SAEs were reported.
In a multicentre study, 315 FD patients (Rome II criteria; mean age = 49; 67% women) were randomised to STW 5 (20 drops t.d.s.) or placebo for 8 weeks.80 The primary outcome measured was the change in the Gastrointestinal Symptom Score (GIS), a validated questionnaire that measures 10 dyspeptic symptoms using a Likert scale of 0–4. GIS scores significantly improved by 6.9 (±4.8) points in the STW 5 group at week 8, compared to 5.9 (±4.3) in the placebo-treated group (P = 0.04). Adverse events were not different between the two groups, nor were the drop-out rate (11–12%). In a second multicentre study of STW 5, 103 FD patients (Rome II criteria; mean age = 47; 70% women) were randomised to t.d.s. STW 5 (20 drops) or placebo for 28 days.81 The primary outcome measure was a change in GIS scores. Total GIS scores decreased from 11.6 (±4.4) to 5.0 (±4.3) in the STW 5 group compared to a decline in the placebo group scores from 12.0 (±4.7) to 7.5 (±6.6; P = 0.03). Adverse events were not different between the two groups.
Holtmann and colleagues evaluated the efficacy of artichoke leaf extract (ALE; 640 mg t.d.s.) during a 6-week, double-blind, RCTs of 247 FD patients (82; mean age = 47; 64% women). Overall symptom improvement, using a 4-point rating scale each week, was significantly greater in the ALE group than in the placebo group (8.3 ± 4.6 vs. 6.7 ± 4.8; P < 0.01). Quality of life scores, as measured by the Nepean Dyspepsia Index (NDI), were higher in the group treated with ALE compared to those treated with placebo (P < 0.01). One SAE occurred in the placebo group.
Data on other agents are limited. A combination of peppermint oil and caraway oil (90 and 50 mg respectively) given twice daily for 4 weeks to 96 FD patients (67% women; mean age = 51) was more likely than placebo to improve both global dyspeptic symptoms, and the intensity of abdominal pain, using a per-protocol analysis (P < 0.003 for both).83 One study found that banana powder capsules were slightly better than placebo at improving dyspeptic symptoms during an 8-week trial period (n = 46; mean age = 34; 40% women).84 Finally, the antioxidant astaxanthin was found to be no better than placebo in a trial of 132 FD patients meeting Rome II criteria (mean age = 44; 86% women).85
Psychological therapies
The first study to evaluate the role of behavioural therapy in patients with FD involved 103 Swedish patients.86 A total of 52 patients were randomised to the out-patient treatment group which focused on applied relaxation and also on an active self-help programme (63% women; mean age = 37). Patients were asked to attend eight separate 90-min sessions over 3 months. A total of 51 patients were randomised to the control group which only involved recording symptoms. The primary outcome was an improvement in patients’ reports of pain. At week 12, pain intensity (P < 0.04) and pain frequency (P < 0.044) were both reduced in the treatment group compared to the control group, although at 1-year follow-up, there was no significant difference between the treatment group and control group. No AEs were reported, although the drop-out rate in the treatment group was 38% and 49% in the control group.
The role of psychotherapy in FD patients was investigated in 100 Norwegian patients randomised to receive either 10 sessions of cognitive behavioural psychotherapy over 4 months or no treatment (87; mean age 40 years; 59% women). At 1-year follow-up, patients in the behavioural therapy group were more likely than the no-treatment group to have an improvement in days of epigastric pain (P = 0.050), nausea (P = 0.024), heartburn (P = 0.021), constipation (P = 0.047) and diarrhoea (P = 0.002). Five patients stopped therapy in the cognitive psychotherapy group and three patients refused follow-up in the placebo group. No AEs were reported.
In a study of 95 consecutive FD patients who had failed conventional pharmacological therapy, 73 patients (60% women; mean age = 40 years) were randomised to receive either supportive care (seven counselling sessions) or seven sessions of psychodynamic-interpersonal (PI) psychotherapy.88 At the end of treatment, patients undergoing PI noted a greater improvement in total FD symptoms than did controls (P = 0.015). At 1-year follow-up, no-treatment difference existed between the two groups. If patients with severe gastroesophageal reflux were excluded, PI-treated patients felt better than patients treated with supportive therapy (P = 0.037).
A 16-week course of hypnotherapy was compared to supportive therapy plus placebo medication or twice daily ranitidine (150 mg) in a study of 126 FD patients (Rome I; mean age and gender not reported;89). Short-term follow-up (16 weeks) evaluated by a blinded assessor revealed that symptom scores were better in the hypnotherapy group (59% median improvement) compared to the supportive therapy group (41%; P = 0.01) or medical treatment (33%; P = 0.057). Quality of life scores also improved in the hypnotherapy group. Long-term follow-up at 56 weeks found that patients in the hypnotherapy group felt better, were less likely to visit their clinician, and were less likely to have started medications for their FD symptoms compared to the other 2 groups (P < 0.001).
Investigational agents
The absence of an FDA-approved safe and efficacious agent for the treatment of FD has motivated researchers to develop a therapeutic agent capable of normalising pain perception and improving GI neuromuscular function in FD patients. Cholecystokinin (CCK) is a neuropeptide believed to mediate pain in the gut. The CCK antagonist dexloxiglumide reduced dyspeptic symptoms induced by lipid infusion and gastric distension.19 Neurokinin receptors (NK1, NK2, NK3) and N-methyl-d-aspartic acid receptors are expressed in the enteric nervous system and animal studies have demonstrated that specific antagonists have antinociceptive properties, although these results have not been replicated in humans.90, 91 Asimadoline, a kappa-opioid agonist, improved visceral pain in animal models and in a trial involving colonic distention in humans.92, 93 However, in a randomised trial of 40 patients with FD, asimadoline did not improve global symptoms or post nutrient drink symptoms.94 Ghrelin, a 28-amino acid peptide, accelerates gastric emptying in healthy volunteers and patients with diabetic gastroparesis.95, 96 A synthetic intravenous ghrelin agonist (TZP-101) improved gastric emptying in a small study of diabetic patients; a Phase 2B trial of an oral version (TZP-102) is currently underway.97 Both these studies involve patients with diabetic gastroparesis; no data are yet available in FD patients.
CONCLUSIONS
The treatment of FD remains unsatisfactory for many patients. Dietary advice is routinely provided although there are few data available to support clinicians’ recommendations. Eradication of H. pylori improves dyspeptic symptoms in only 7% of patients treated (NNT = 14), while H2RAs are somewhat better, with a calculated NNT of 7. Prokinetic agents are theoretically appealing for FD patients with delayed gastric emptying. However, the results from studies of tegaserod, itopride and mosapride are unimpressive, and since the withdrawal of cisapride, only metoclopramide is currently available in the US; potentially serious side effects limit metoclopramide’s use. Other promotility agents (e.g. domperidone) are available outside the U.S. Complementary agents are commonly used by patients for a number of reasons, including ease of use, the perceived safety compared to prescription pharmacological agents, and the perceived appeal of using a ‘natural’ substance as opposed to a prescription medication. STW-5 has demonstrated benefit in patients with FD, although the mechanism of action is unknown. Hypnotherapy is likely to improve global symptoms in FD patients, although well-trained hypnotherapists are difficult to find and most insurance companies will not pay for this form of therapy.
In the light of these limitations it is not surprising that no agent is approved for the treatment of FD. On the basis of the data contained in this review, a treatment algorithm for FD is proposed (see Figure 1). In areas with H. pylori prevalence >10% patients with a normal endoscopy (without gastric biopsies having been performed) should be tested for H. pylori using either a breath test or stool antigen test, and if positive, treated. Empiric treatment for H. pylori based only on symptoms is not recommended. After H. pylori treatment (assuming that H. pylori has been eradicated), the majority of FD patients will have persistent symptoms, and empiric therapy for 6–8 weeks with a once-daily PPI is reasonable. If symptoms persist then a low-dose TCA may be initiated (e.g. amitriptyline at 10 mg each day with slow escalation to 50 or 75 mg/day; alternatively desipramine at 10–50 mg q day). If symptoms persist, then a trial of a prokinetic agent is reasonable, especially if the patient has concomitant symptoms of nausea and/or postprandial fullness. Alternatively, other anti-nociceptive agents can be used, recognising the lack of evidence from prospective trials to guide clinical care. Finally, if the patient wishes to pursue alternative therapies, then STW-5 can be initiated or a referral to a hypnotherapist may be offered.
Figure 1.
Proposed treatment algorithm for FD. In this algorithm the patient with dyspepsia undergoes an upper endoscopy which, by definition, has to be grossly normal. If biopsies for Helicobacter pylori (HP) were performed and were negative (upper left corner) then the patient should be treated with a daily proton pump inhibitor (PPI). If symptoms (Sx) do not improve after 4–8 weeks, a therapeutic trial with a TCA should be initiated (the percentage of patients with FD symptom resolution is shown in parentheses). If upper endoscopy is grossly normal but gastric biopsies were not obtained for H. pylori, then the algorithm should begin with an assessment of H. pylori prevalence (upper right side). If present, H. pylori should be treated and the occasional patient with H. pylori will experience FD symptom resolution. If the patient is H. pylori-negative, then PPI therapy should be initiated (upper middle of diagram). The percentage of H. pylori-negative FD patients previously treated with a PPI and then a TCA, who will improve with an anti-nociceptive agent or CAM, is unknown. Therapeutic Gain (T.G.) refers to the reported symptom improvement rate above the placebo response (i.e. not including the placebo response). The overall Response Rate (R. R.) refers to the overall response rate which includes the placebo response. For example, on the right hand side of the diagram, the therapeutic gain (T.G.) of treating an FD patient who is H.P (+) has been reported as 6–14%. Alternatively, this portion of the figure could have been labelled using the overall response rate (R.R.) for FD symptom improvement in a patient treated for HP, which is approximately 31–39%, as this includes the placebo response rate which is approximately 25%.
ACKNOWLEDGEMENTS
Dr Howden has served as a speaker for Takeda and GlaxoSmithKline, and a consultant for Takeda. Dr Moayyedi has been an advisory board member for AstraZeneca, and has received research funding from Axcan and AstraZeneca. Dr El-Serag has received research funding by the Houston VA HSR&D Center of Excellence (HFP90-020) and P30 Center Grant DK56338. All research, writing, analyses and editing was performed directly by the authors. Declaration of funding interests: The authors’ time spent researching and preparing this manuscript was supported in part by the National Institute for Diabetes and Digestive and Kidney Disease (NIDDK, U01DK065713)
Footnotes
Declaration of personal interests: Drs Lacy, Talley, Locke, Bouras, DiBaise, Abraham and Prather report no relevant disclosures.
REFERENCES
- 1.Camilleri M, Dubois D, Coulie B, et al. Prevalence and socioeconomic impact of upper gastrointestinal disorders in the United States: results of the US Upper Gastrointestinal Study. Clin Gastroenterol Hepatol. 2005;3:543–552. doi: 10.1016/s1542-3565(05)00153-9. [DOI] [PubMed] [Google Scholar]
- 2.El-Serag HB, Talley NJ. Systematic review: the prevalence and clinical course of functional dyspepsia. Aliment Pharmacol Ther. 2004;19:643–654. doi: 10.1111/j.1365-2036.2004.01897.x. [DOI] [PubMed] [Google Scholar]
- 3.Castillo EJ, Camilleri M, Locke GR, III, et al. A community-based, controlled study of the epidemiology and pathophysiology of dyspepsia. Clin Gastroenterol Hepatol. 2004;2:985–996. doi: 10.1016/s1542-3565(04)00454-9. [DOI] [PubMed] [Google Scholar]
- 4.Ford AC, Forman D, Bailey AG, et al. Initial poor quality of life and new onset of dyspepsia: results from a longitudinal 10-year follow-up study. Gut. 2007;56:321–327. doi: 10.1136/gut.2006.099846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466–1479. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 6.Choung RS, Locke GR, Schleck CD, et al. Do distinct dyspepsia subgroups exist in the community? A population-based study. Am J Gastroenterol. 2007;102:1983–1989. doi: 10.1111/j.1572-0241.2007.01381.x. [DOI] [PubMed] [Google Scholar]
- 7.Bisschops R, Karamanolis G, Arts J, et al. Relationship between symptoms and ingestion of a meal in functional dyspepsia. Gut. 2008;57:1495–1503. doi: 10.1136/gut.2007.137125. [DOI] [PubMed] [Google Scholar]
- 8.Tack J, Bisschops R, Sarnelli G. Pathophysiology and treatment of functional dyspepsia. Gastroenterology. 2004;127:1239–1255. doi: 10.1053/j.gastro.2004.05.030. [DOI] [PubMed] [Google Scholar]
- 9.Talley NJ, Vakil NB, Moayyedi P. American gastroenterological association technical review on the evaluation of dyspepsia. Gastroenterology. 2005;129:1756–1780. doi: 10.1053/j.gastro.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 10.Lacy BE, Cash BD. A 32-year-old woman with chronic abdominal pain. JAMA. 2008;299:555–565. doi: 10.1001/jama.2007.51-a. [DOI] [PubMed] [Google Scholar]
- 11.El-Serag HB, Talley NJ. Health-related quality of life in functional dyspepsia. Aliment Pharmacol Ther. 2003;18:387–393. doi: 10.1046/j.1365-2036.2003.01706.x. [DOI] [PubMed] [Google Scholar]
- 12.Moayyedi P, Mason J. Clinical and economic consequences of dyspepsia in the community. Gut. 2002;50(Suppl. IV):10–12. doi: 10.1136/gut.50.suppl_4.iv10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brook RA, Kleinman NL, Choung RS, et al. Functional dyspepsia impacts absenteeism and direct and indirect costs. Clin Gastroenterol Hepatol. 2010;8:498–503. doi: 10.1016/j.cgh.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Matsueda K, Hongo M, Tack J, et al. A placebo-controlled trial of acotiamide for meal-related symptoms of functional dyspepsia. Gut. 2011 doi: 10.1136/gutjnl-2011-301454. gutnjl-2011-301454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Piessevaux H, De Winter B, Loouis E, et al. Dyspeptic symptoms in the general population: a factor and cluster analysis of symptom groupings. Neurogastroenterol Motil. 2009;21:378–388. doi: 10.1111/j.1365-2982.2009.01262.x. [DOI] [PubMed] [Google Scholar]
- 16.Pilichiewicz AN, Horowitz M, Holtmann GJ, Talley NJ, Feinle-Bisset C. Relationship between symptoms and dietary patterns in patients with functional dyspepsia. Clin Gastroenterol Hepatol. 2009;7:317–322. doi: 10.1016/j.cgh.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 17.Saito YA, Locke GR, Weaver AL, Zinsmeister AR, Talley NJ. Diet and functional gastrointestinal disorders: a population-based case-control study. Am J Gastroenterol. 2005;100:2743–2748. doi: 10.1111/j.1572-0241.2005.00288.x. [DOI] [PubMed] [Google Scholar]
- 18.Barbera R, Feinle C, Read NW. Nutrient specific modulation of gastric mechanosensitivity in patients with functional dyspepsia. Dig Dis Sci. 1995;40:1636–1641. doi: 10.1007/BF02212683. [DOI] [PubMed] [Google Scholar]
- 19.Feinle C, Meier O, Otto B, D’Amato M, Fried M. Role of duodenal lipid and cholecystokinin a receptors in the pathophysiology of functional dyspepsia. Gut. 2001;48:347–355. doi: 10.1136/gut.48.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cuperus P, Keeling PW, Gibnery MJ. Eating patterns in functional dyspepsia: a case control study. Eur J Clin Nutr. 1996;50:520–523. [PubMed] [Google Scholar]
- 21.Carvalho RV, Lorena SL, Almeida JR, Mesquita MA. Food intolerance, diet composition, and eating patterns in functional dyspepsia patients. Dig Dis Sci. 2010;55:60–65. doi: 10.1007/s10620-008-0698-8. [DOI] [PubMed] [Google Scholar]
- 22.Tack J, Demedts I, Dehondt G, et al. Clinical and pathophysiological characteristics of acute-onset functional dyspepsia. Gastroenterology. 2002;122:1738–1747. doi: 10.1053/gast.2002.33663. [DOI] [PubMed] [Google Scholar]
- 23.Moayyedi P, Soo S, Deeks J, et al. Eradication of Helicobacter pylori for non-ulcer dyspepsia. Cochrane Database Syst Rev. 2008;2:CD002096. doi: 10.1002/14651858.CD002096. [DOI] [PubMed] [Google Scholar]
- 24.Lan L, Yu J, Chen YL, et al. Symptom-based tendencies of Helicobacter Pylori eradication in patients with functional dyspepsia. World J Gastroenterol. 2011;17:3242–3247. doi: 10.3748/wjg.v17.i27.3242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mazzoleni LE, Sander GB, Francesconi CF, et al. Helicobacter pylori eradication in functional dyspepsia: HEROES trial. Arch Intern Med. 2011;171:1929–1933. doi: 10.1001/archinternmed.2011.533. [DOI] [PubMed] [Google Scholar]
- 26.Cremonini F, Delgado-Aros S, Talley NJ. Functional dyspepsia: drugs for new (and old) therapeutic targets. Best Pract Res Clin Gastroenterol. 2004;18:717–733. doi: 10.1016/j.bpg.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 27.Moayyedi P, Shelly S, Deeks JJ, et al. Pharmacological interventions for non-ulcer dyspepsia. Cochrane Database Syst Rev. 2006;4:CD001960. doi: 10.1002/14651858.CD001960.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blum AL, Arnold R, Stolte M, Fischer M, Koelz HR. Short course acid suppressive treatment for patients with functional dyspepsia: results depend on Helicobacter pylori status. Gut. 2000;47:473–480. doi: 10.1136/gut.47.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Delattre M, Malesky M, Prinzie A. Symptomatic treatment of nonulcer dyspepsia with cimetidine. Curr Therapeutic Res. 1985;37:980–991. [Google Scholar]
- 30.Gotthard R, Bodemar G, Brodin U, Jonsson KA. Treatment with cimetidine, antacid, or placebo in patients with dyspepsia of unknown origin. Scand J Gastroenterol. 1988;23:7–18. doi: 10.3109/00365528809093840. [DOI] [PubMed] [Google Scholar]
- 31.Hadi S. Clinical investigation of ranitidine in patients with gastritis. Clin Ther. 1989;11:590–594. [PubMed] [Google Scholar]
- 32.Hansen JM, Bytzer P, Schaffalitzky de Muckadell OB. Placebo-controlled trial of cisapride and nizatidine in unselected patients with functional dyspepsia. Am J Gastroenterol. 1998;93:368–374. doi: 10.1111/j.1572-0241.1998.00368.x. [DOI] [PubMed] [Google Scholar]
- 33.Kato M, Watanabe M, Konishi S, et al. Randomized, double-blind, placebo-controlled crossover trial of famotidine in patients with functional dyspepsia. Aliment Pharmacol Ther. 2005;21(Suppl. 2):27–31. doi: 10.1111/j.1365-2036.2005.02470.x. [DOI] [PubMed] [Google Scholar]
- 34.Kelbaek H, Linde J, Eriksen J, Mungaard S, Moesgaard F, Bonnevie O. Controlled clinical trial of treatment with cimetidine for non-ulcer dyspepsia. Acta Med Scand. 1985;213:281–287. doi: 10.1111/j.0954-6820.1985.tb02696.x. [DOI] [PubMed] [Google Scholar]
- 35.Muller P, Hotz J, Franz E, Simon B. Ranitidine in the Treatment of Non-Ulcer Dyspepsia. A placebo-controlled study in the Federal Republic of Germany [Ranitidin in der Behandlung derNon–Ulcer–Dyspepsie. Eine placebo–kontrollierte Studie in der Bundesrepublic Deutschland] Arzneimittelforschung/Drug Res. 1994;10:1130–1132. [PubMed] [Google Scholar]
- 36.Nesland AA, Berstad A. Effect of cimetidine in patients with nonulcer dyspepsia and erosive prepyloric changes. Scand J Gastroenterol. 1985;20:629–635. doi: 10.3109/00365528509089708. [DOI] [PubMed] [Google Scholar]
- 37.Olubuyide IOOA, Ayoola EA, Okubanjo AO, Atoba MA. Non-ulcer dyspepsia in Nigerians: clinical and therapeutic results. Scand J Gastroenterol. 1986;21(Suppl. 124):83–87. doi: 10.3109/00365528609093787. [DOI] [PubMed] [Google Scholar]
- 38.Saunders JH, Oliver RJ, Higson DL. Dyspepsia: incidence of a non-ulcer disease in a controlled trial of ranitidine in general practice. Br Med J (Clin Res Ed) 1994;1986:665–668. doi: 10.1136/bmj.292.6521.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Singal AK, Kumar A, Broor SL. Cimetidine in the treatment of non-ulcer dyspepsia: results of a randomized double-blind, placebo-controlled study. Curr Med Res Opin. 1989;11:390–397. doi: 10.1185/03007998909110140. [DOI] [PubMed] [Google Scholar]
- 40.Carvalhinhos A, Fidalgo P, Freire A, Matos L. Cisapride compared with ranitidine in the treatment of functional dyspepsia. Eur J Gastroenterol Hepatol. 1995;7:411–417. [PubMed] [Google Scholar]
- 41.Casiraghi A, Ferrara A, Lesinigo E. Cimetidine vs antacids in non-ulcer dyspepsia. Curr Ther Res Clin Exp. 1986;39:397. [Google Scholar]
- 42.Misra SP, Dwivedi M, Misra V, Agarwal SK. Sucralfate versus ranitidine in non-ulcer dyspepsia: results of a prospective, randomized, open, controlled trial. Indian J Gastroenterol. 1992;11:7–8. [PubMed] [Google Scholar]
- 43.Talley NJ, Meineche-Schmidt V, Paré P, et al. Efficacy of omeprazole in functional dyspepsia: double-blind, randomized, placebo-controlled trials (the Bond and Opera studies) Aliment Pharmacol Ther. 1998;12:1055–1065. doi: 10.1046/j.1365-2036.1998.00410.x. [DOI] [PubMed] [Google Scholar]
- 44.Blum AL, Arnold R, Stolte M, Fischer M, Koelz HR. Short course acid suppressive treatment for patients with functional dyspepsia: results depend on Helicobacter pylori status. The Frosch Study Group. Gut. 2000;47:473–480. doi: 10.1136/gut.47.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bolling-Sternevald E, Lauritsen K, Aalykke C, Havelund T, Knudsen T, et al. Effect of profound acid suppression in functional dyspepsia: a double-blind, randomized, placebo-controlled trial. Scand J Gastroenterol. 2002;37:1395–1402. doi: 10.1080/003655202762671260. [DOI] [PubMed] [Google Scholar]
- 46.Wong WM, Wong BC, Hung WK, Yee YK, Yip AW, et al. Double blind, randomised, placebo controlled study of four weeks of lansoprazole for the treatment of functional dyspepsia in Chinese patients. Gut. 2002;51:502–506. doi: 10.1136/gut.51.4.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Peura DA, Kovacs TO, Metz DC, Siepmaan N, Pilmer BL, Talley NJ. Lansoprazole in the treatment of functional dyspepsia: two double-blind, randomized, placebo-controlled trials. Am J Med. 2004;116:740–748. doi: 10.1016/j.amjmed.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 48.van Zanten SV, Armstrong D, Chiba N, et al. Esomeprazole 40 mg once a day in patients with functional dyspepsia: the randomized, placebo-controlled “ENTER” trial. Am J Gastroenterol. 2008;101:2096–2106. doi: 10.1111/j.1572-0241.2006.00751.x. [DOI] [PubMed] [Google Scholar]
- 49.van Rensburg C, Berghöfer P, Enns R, Dattani ID, Maritz JF, et al. Efficacy and safety of pantoprazole 20 mg once daily treatment in patients with ulcer-like functional dyspepsia. Curr Med Res Opin. 2008;24:2009–2018. doi: 10.1185/03007990802184545. [DOI] [PubMed] [Google Scholar]
- 50.Talley NJ, Vakil N, Lauritsen K, et al. Randomized-controlled trial of esomeprazole in functional dyspepsia patients with epigastric pain or burning: does a 1-week trial of acid suppression predict symptom response? Aliment Pharmacol Ther. 2007;26:673–682. doi: 10.1111/j.1365-2036.2007.03410.x. [DOI] [PubMed] [Google Scholar]
- 51.Wang WH, Huang JQ, Zheng GF, Xia HH, Wong WM, et al. Effects of proton pump inhibitors on functional dyspepsia: a meta-analysis of randomized placebo-controlled trials. Clin Gastroenterol Hepatol. 2007;5:172–185. doi: 10.1016/j.cgh.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 52.Vakil N, Laine L, Talley NJ, et al. Tegaserod treatment for dysmotility-like functional dyspepsia: results of two randomized, controlled trials. Am J Gastroenterol. 2008;103:1906–1919. doi: 10.1111/j.1572-0241.2008.01953.x. [DOI] [PubMed] [Google Scholar]
- 53.Holtmann G, Talley NJ, Liebregts T, Adam B, Parow C. A placebo-controlled trial of itopride in functional dyspepsia. N Engl J Med. 2006;354:832–840. doi: 10.1056/NEJMoa052639. [DOI] [PubMed] [Google Scholar]
- 54.Talley NJ, Tack J, Ptak T, Gupta R, Giguère M. Itopride in functional dyspepsia: results of two phase III multicentre, randomised, double-blind, placebo-controlled trials. Gut. 2008;57:740–746. doi: 10.1136/gut.2007.132449. [DOI] [PubMed] [Google Scholar]
- 55.Hallerbäck BI, Bommelaer G, Bredberg E, et al. Dose finding study of mosapride in functional dyspepsia: a placebo-controlled, randomized study. Aliment Pharmacol Ther. 2002;16:959–967. doi: 10.1046/j.1365-2036.2002.01236.x. [DOI] [PubMed] [Google Scholar]
- 56.Talley NJ, Verlinden M, Snape W, et al. Failure of a motilin receptor agonist (ABT-229) to relieve the symptoms of functional dyspepsia in patients with and without delayed gastric emptying: a randomized double-blind placebo-controlled trial. Aliment Pharmacol Ther. 2000;14:1653–1661. doi: 10.1046/j.1365-2036.2000.00868.x. [DOI] [PubMed] [Google Scholar]
- 57.Manabe N, Wong BS, Camilleri M. New-generation 5-HT4 receptor agonists: potential for treatment of gastrointestinal motility disorders. Expert Opin Investig Drugs. 2010;19:765–775. doi: 10.1517/13543784.2010.482927. [DOI] [PubMed] [Google Scholar]
- 58.Lacy BE, Loew B, Crowell MD. Prucalopride for chronic constipation. Drugs Today. 2009;45:843–853. doi: 10.1358/dot.2009.45.12.1423115. [DOI] [PubMed] [Google Scholar]
- 59.Saarto T, Wiffen PJ. Antidepressants for neuropathic pain. Cochrane Database Syst Rev. 2007;4:CD005454. doi: 10.1002/14651858.CD005454.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ford AC, Talley N, Schoenfeld PS, Quigley EM, Moayyedi P. Efficacy of antidepressants and psychological therapies in irritable bowel syndrome: systematic review and meta-analysis. Gut. 2009;58:367–378. doi: 10.1136/gut.2008.163162. [DOI] [PubMed] [Google Scholar]
- 61.Talley NJ, Herrick L, Locke GR. Antidepressants in functional dyspepsia. Expert Rev Gastroenterology Hepatol. 2010;4:5–8. doi: 10.1586/egh.09.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Talley NJ, Camilleri M, Chitkara DK, et al. Effects of desipramine and escitalopram on postprandial symptoms induced by the nutrient drink test in healthy volunteers: a randomized, double-blind, placebo-controlled study. Digestion. 2005;72:97–103. doi: 10.1159/000088363. [DOI] [PubMed] [Google Scholar]
- 63.Choung RS, Cremonini F, Thapa P, Zinsmeister AR, Talley NJ. The effect of short-term, low-dose tricyclic and tetracyclic antidepressant treatment on satiation, postnutrient load gastrointestinal symptoms and gastric emptying: a double-blind, randomized, placebo-controlled trial. Neurogastroenterol Motil. 2008;20:220–227. doi: 10.1111/j.1365-2982.2007.01029.x. [DOI] [PubMed] [Google Scholar]
- 64.Bouras EP, Talley N, Camilleri M, et al. Effects of amitriptyline on gastric sensorimotor function and postprandial symptoms in healthy individuals: a randomized, double-blind, placebo-controlled trial. Am J Gastroenterol. 2008;103:2043–2050. doi: 10.1111/j.1572-0241.2008.02021.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mertz H, Fass R, Kodner A, et al. Effect of amitriptyline on symptoms, sleep, and visceral perception in patients with functional dyspepsia. Am J Gastroenterol. 1998;93:160–165. doi: 10.1111/j.1572-0241.1998.00160.x. [DOI] [PubMed] [Google Scholar]
- 66.Otaka M, Jin M, Odashima M, et al. New strategy of therapy for functional dyspepsia using famotidine, mosapride and amitriptyline. Aliment Pharmacol Ther. 2005;21(Suppl. 2):42–6. doi: 10.1111/j.1365-2036.2005.02473.x. [DOI] [PubMed] [Google Scholar]
- 67.Wu JC, Cheong PK, Chan Y, et al. A randomized, double-blind, placebo-controlled trial of low dose imipramine for treatment of refractory functional dyspepsia (FD) Gastroenterology. 2011;140(Suppl. 1):S-50. doi: 10.1016/S2468-1253(18)30303-0. [DOI] [PubMed] [Google Scholar]
- 68.Talley NJ, Dennis EH, Schettler-Duncan VA, et al. Overlapping upper and lower gastrointestinal symptoms in irritable bowel syndrome patients with constipation or diarrhea. Am J Gastroenterol. 2003;98:2454–2459. doi: 10.1111/j.1572-0241.2003.07699.x. [DOI] [PubMed] [Google Scholar]
- 69.Tack J, Caenepeel P, Fischler B, et al. Symptoms associated with hypersensitivity to gastric distention in functional dyspepsia. Gastroenterology. 2001;121:526–535. doi: 10.1053/gast.2001.27180. [DOI] [PubMed] [Google Scholar]
- 70.van Kerkhoven LA, Laheij RJ, Aparicio N, et al. Effect of the antidepressant venlafaxine in functional dyspepsia: a randomize, double-blind, placebo-controlled trial. Clin Gastroenterol Hepatol. 2008;6:746–752. doi: 10.1016/j.cgh.2008.02.051. [DOI] [PubMed] [Google Scholar]
- 71.Brennan BP, Fogarty KV, Roberts JL, et al. Duloxetine in the treatment of irritable bowel syndrome: an open-label pilot study. Hum Psychopharmacol. 2009;24:423–428. doi: 10.1002/hup.1038. [DOI] [PubMed] [Google Scholar]
- 72.Talley NJ, Locke GR, 3rd, Herrick LM, et al. Functional Dyspepsia Treatment Trial (FDTT): a double-blind, randomized, placebo-controlled trial of antidepressants in functional dyspepsia, evaluating symptoms, psychopathology, pathophysiology and pharmacogenetics. Contemp Clin Trials. 2012;33:523–533. doi: 10.1016/j.cct.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tack J, Masclee A, Heading R, et al. A dose-ranging, placebo-controlled, pilot trial of acotiamide in patients with functional dyspepsia. Neurogastroenterol Motil. 2009;21:272–280. doi: 10.1111/j.1365-2982.2009.01261.x. [DOI] [PubMed] [Google Scholar]
- 74.Matsueda K, Hongo M, Tack J, et al. Clinical trial: dose-dependent therapeutic efficacy of acotiamide hydrochloride (Z-338) in patients with functional dyspepsia – 100 mg t.i.d. is an optimal dosage. Neurogastroenterol Motil. 2010;22:618–e173. doi: 10.1111/j.1365-2982.2009.01449.x. [DOI] [PubMed] [Google Scholar]
- 75.Gale JD, Houghton LA. Alpha 2 Delta (α(2)δ) ligands, gabapentin and pregabalin: what is the evidence for potential use of these ligands in irritable bowel syndrome. Front Pharmacol. 2011;2:28. doi: 10.3389/fphar.2011.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stein DJ, Bruce Lydiard R, Herman BK, Mandel FS. Impact of gastrointestinal symptoms on response to pregabalin in generalized anxiety disorder: results of a six-study combined analysis. Int Clin Psychopharmacol. 2009;24:126–132. doi: 10.1097/YIC.0b013e3283249c7b. [DOI] [PubMed] [Google Scholar]
- 77.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 78.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and Alternative Medicine use Among Adults: United States, 2002. Hyattsville, MD: National Center for Health Statistics; 2004. [PubMed] [Google Scholar]
- 79.Madisch A, Holtmann G, Mayr G, Vinson B, Hotz J. Treatment of functional dyspepsia with a herbal preparation. A double-blind, randomized, placebo-controlled, multicenter trial. Digestion. 2004;69:45–52. doi: 10.1159/000076546. [DOI] [PubMed] [Google Scholar]
- 80.von Arnim U, Peitz U, Vinson B, Gundermann KJ, Malfertheiner P. STW 5, a phytopharmacon for patients with functional dyspepsia: results of a multicenter, placebo-controlled double-blind study. Am J Gastroenterol. 2007;102:1268–1275. doi: 10.1111/j.1572-0241.2006.01183.x. [DOI] [PubMed] [Google Scholar]
- 81.Braden B, Caspary W, Borner N, Vinson B, Schneider ARJ. Clinical effects of STW 5 (Iberogast) are not based on acceleration of gastric emptying in patients with functional dyspepsia and gastroparesis. Neurogastroenterol Motil. 2009;21:632–639. doi: 10.1111/j.1365-2982.2008.01249.x. [DOI] [PubMed] [Google Scholar]
- 82.Holtmann G, Adam B, Haag S, et al. Efficacy of artichoke leaf extract in the treatment of patients with functional dyspepsia: a six-week placebo-controlled, double-blind, multicentre trial. Aliment Pharmacol Ther. 2003;18:1099–1105. doi: 10.1046/j.1365-2036.2003.01767.x. [DOI] [PubMed] [Google Scholar]
- 83.May B, Kohler S, Schneider B. Efficacy and tolerability of a fixed combination of peppermint oil and caraway oil in patients suffering from functional dyspepsia. Aliment Pharmacol Ther. 2000;14:1671–1677. doi: 10.1046/j.1365-2036.2000.00873.x. [DOI] [PubMed] [Google Scholar]
- 84.Arora A, Sharma MP. Use of banana in non-ulcer dyspepsia. Lancet. 1990;335:612–613. doi: 10.1016/0140-6736(90)90402-q. [DOI] [PubMed] [Google Scholar]
- 85.Kupcinskas L, Lafolie P, Lignell A, et al. Efficacy of the natural antioxidant astaxanthin in the treatment of functional dyspepsia in patients with or without Helicobacter pylori infection: a prospective, randomized, double-blind, and placebo-controlled study. Phytomedicine. 2008;15:391–399. doi: 10.1016/j.phymed.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 86.Bates S, Sjoden PO, Nyren O. Behavioral treatment of non-ulcer dyspepsia. Scand J Behav Ther. 1988;17:155–165. [Google Scholar]
- 87.Haug TT, Wilhelmsen I, Svebak S, Berstad A, Ursin H. Psychotherapy in functional dyspepsia. J Psychosom Res. 1994;38:735–744. doi: 10.1016/0022-3999(94)90026-4. [DOI] [PubMed] [Google Scholar]
- 88.Hamilton J, Guthrie E, Creed F, et al. A randomized controlled trial of psychotherapy in patients with chronic functional dyspepsia. Gastroenterology. 2000;119:661–669. doi: 10.1053/gast.2000.16493. [DOI] [PubMed] [Google Scholar]
- 89.Calvert EL, Houghton LA, Cooper P, Morris J, Whorwell PJ. Long-term improvement in functional dyspepsia using hypnotherapy. Gastroenterology. 2002;123:1778–1785. doi: 10.1053/gast.2002.37071. [DOI] [PubMed] [Google Scholar]
- 90.Saad RJ, Chey WD. Review article: current and emerging therapies for functional dyspepsia. Aliment Pharmacol Ther. 2006;24:475–492. doi: 10.1111/j.1365-2036.2006.03005.x. [DOI] [PubMed] [Google Scholar]
- 91.Traub RJ, Zhai Q, Ji Y, Kovalenko M. NMDA receptor antagonists attenuate noxious and nonnoxious colorectal distention-induced Fos expression in the spinal cord and the visceromotor reflex. Neuroscience. 2002;113:205–211. doi: 10.1016/s0306-4522(02)00170-7. [DOI] [PubMed] [Google Scholar]
- 92.Sengupta JN, Snider A, Su X, Gebhart GF. Effects of kappa opioids in the inflamed rat colon. Pain. 1999;79:175–185. doi: 10.1016/s0304-3959(98)00175-4. [DOI] [PubMed] [Google Scholar]
- 93.Delvaux M, Beck A, Jacob J, et al. Effect of asimadoline, a kappa opioid agonist, on pain induced by colonic distension in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2004;20:237–246. doi: 10.1111/j.1365-2036.2004.01922.x. [DOI] [PubMed] [Google Scholar]
- 94.Talley NJ, Choung RS, Camilleri M, et al. Asimadoline, a kappa-opioid agonist, and satiation in functional dyspepsia. Aliment Pharmacol Ther. 2008;27:1122–1131. doi: 10.1111/j.1365-2036.2008.03676.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Levin F, Edholm T, Schmidt PT, et al. Ghrelin stimulates gastric emptying and hunger in normal-weight humans. J Clin Endocrinol Metab. 2006;91:3296–3302. doi: 10.1210/jc.2005-2638. [DOI] [PubMed] [Google Scholar]
- 96.Murray CD, Martin NM, Patterson M, et al. Ghrelin enhances gastric emptying in diabetic gastroparesis: a double-blind, placebo-controlled, cross-over study. Gut. 2005;54:1693–1698. doi: 10.1136/gut.2005.069088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ejskjaer N, Vestergaard ET, Hellstrom PM, et al. Ghrelin receptor agonist (TZP-101) accelerates gastric emptying in adults with diabetes and symptomatic gastroparesis. Aliment Pharmacol Ther. 2009;29:1179–1187. doi: 10.1111/j.1365-2036.2009.03986.x. [DOI] [PubMed] [Google Scholar]