Individuals with rosacea express high baseline levels of cathelicidin and kallikrein 5 (KLK5) (Yamasaki, et al, 2007). The significance of elevated KLK5 is that this trypsin-like serine protease controls the cleavage of the cathelicidin precursor protein into LL-37 (Yamasaki et al, 2007; Yamasaki et al, 2006). LL-37 is both pro-inflammatory and angiogenic (Koczulla et al, 2003; Lande et al, 2004; Morizane et al, 2012). Based on these findings, we hypothesized that inhibition of KLK5 may improve the clinical signs of rosacea by decreasing LL-37 production.
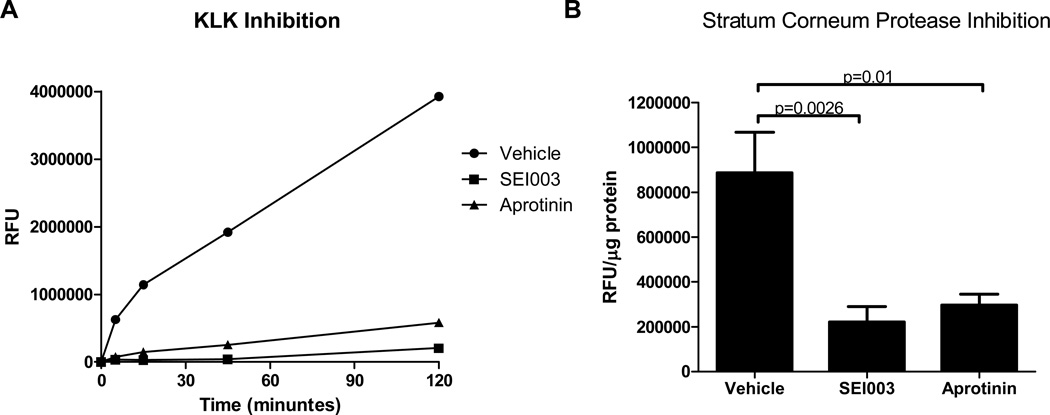
To test this hypothesis, we studied the effects of a known inhibitor of trypsin-like serine protease, ε-aminocaproic acid (ACA). ACA is FDA-approved for systemic administration to enhance hemostasis in cases of fibrinolytic bleeding, and is well-tolerated in humans intravenously in doses up to 3 g/kg. To determine if ACA might be useful in rosacea, ACA was first tested in vitro using an Enzcheck Protease Assay Kit (Invitrogen) against the proteolytic activity of tissue kallikrein (100 µg/mL, Sigma-Aldrich, St. Louis, MO) or stratum corneum protease activity (SPA) collected from tape-strips (D-100 CuDerm, Dallas, TX) of the facial skin of 6 healthy subjects. SPA was extracted from tape with 20 mM Tris-HCl (pH 8.0) containing 0.1% TritonX-100. Protease activity was measured at 37°C for 2 hours after treatment with vehicle, ACA (1M), or the known selective inhibitor of trypsin-related enzymes, aprotinin, (50 µg/mL, Sigma-Aldrich).. Aprotinin strongly suppressed SPA, indicating predominance of trypsin-like proteases in the stratum corneum extract. The inhibitory effect of ACA was similar to that of aprotinin (Figure 1). These combined data suggested that ACA could be effective to inhibit stratum corneum trypsin-like proteases such as KLK5.
Figure 1.
In vitro effects of SEI003 and aprotinin on KLK and human total stratum corneum protease activity. (A) Both SEI003 and aprotinin inhibit KLK activity compared to vehicle alone. SEI003 completely blocks KLK activity for the first 45 minutes of the assay. (B) Compared to vehicle alone, SEI003 and aprotinin both significantly decrease stratum corneum protease activity.
Having confirmed that ACA was an effective inhibitor of SPA in vitro, we next sought to determine whether topical application of a cream formulation containing equal weight of cream and ACA solution (2M), decreased SPA in patients with rosacea. If active, this formulation, called SEI003, would permit us to test the hypothesis that inhibition of SPA improves rosacea. We therefore conducted a proof-of-concept, randomized, double-blind, placebo-controlled study on 11 adult patients with papulopustular rosacea (clinicaltrials.gov identifier NCT01398280). The study was conducted at the University of California San Diego (UCSD) dermatology clinic in accordance with the Declaration of Helsinki and the regulations of the UCSD Institutional Review Board (reference number 100867). Written informed consent was obtained from all participants. The study was conducted between July 2011 and December 2012, and included fifteen subjects with papulopustular rosacea randomized 2:1 to receive either SEI003 (the treatment group) or the base cream homogenized with an equal weight of the ACA vehicle (the placebo group). Subjects, study coordinators and those performing clinical assessments were blinded. Of the 11 patients originally assigned to the treatment group, three subjects voluntarily withdrew from the study (one patient reported scheduling conflicts and two others were no longer interested in participating), and one was withdrawn from the study after starting doxycycline for ocular rosacea. The study numbers of participants who withdrew from the study were reassigned to new subjects after patient 11 was enrolled. All four patients originally assigned to the placebo group completed the study in its entirety. Patients were instructed to apply their assigned medication to their entire face twice daily for the 12-week duration of the study. Clinical assessments including the Investigator’s Global Assessment (IGA) and the summed total of the 5-point Clinician’s Erythema Assessment (CEA) score of five different target sites (left cheek, right cheek, nose, chin, glabella), as well as digital photography were completed at baseline. These procedures were repeated 2, 6, 9 and 12 weeks after the baseline visit along with safety monitoring and tape strip sampling for SPA.
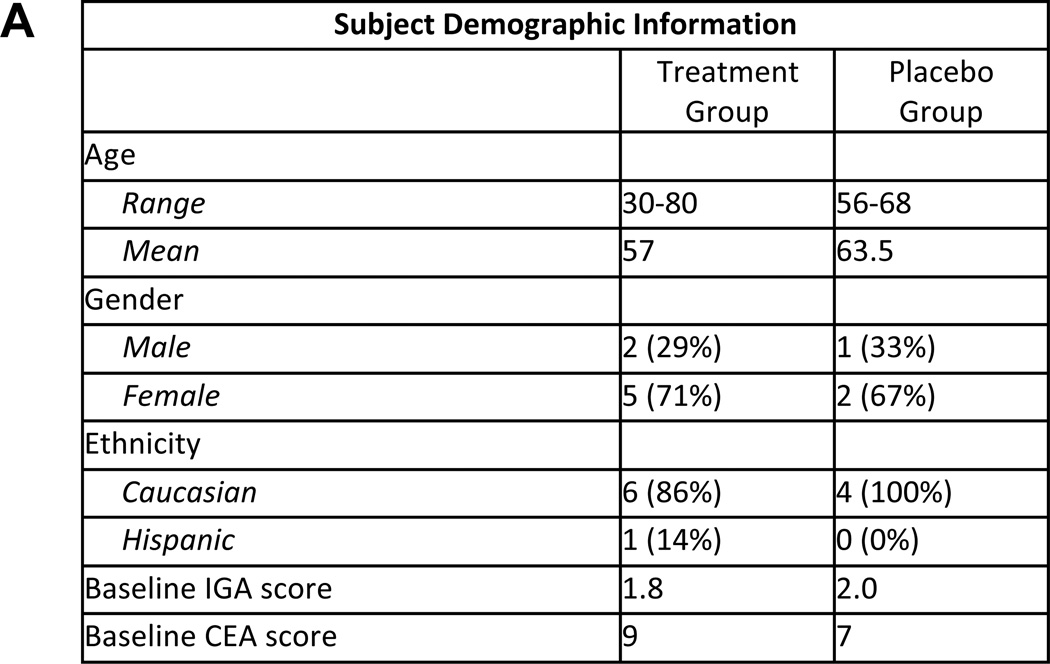
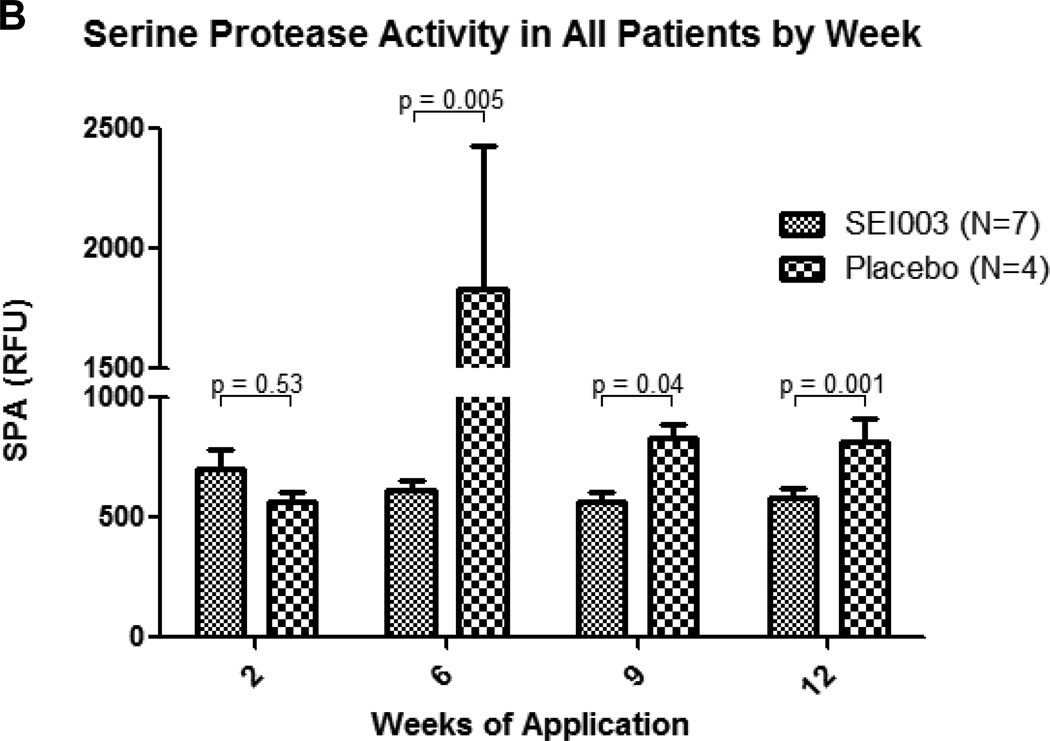
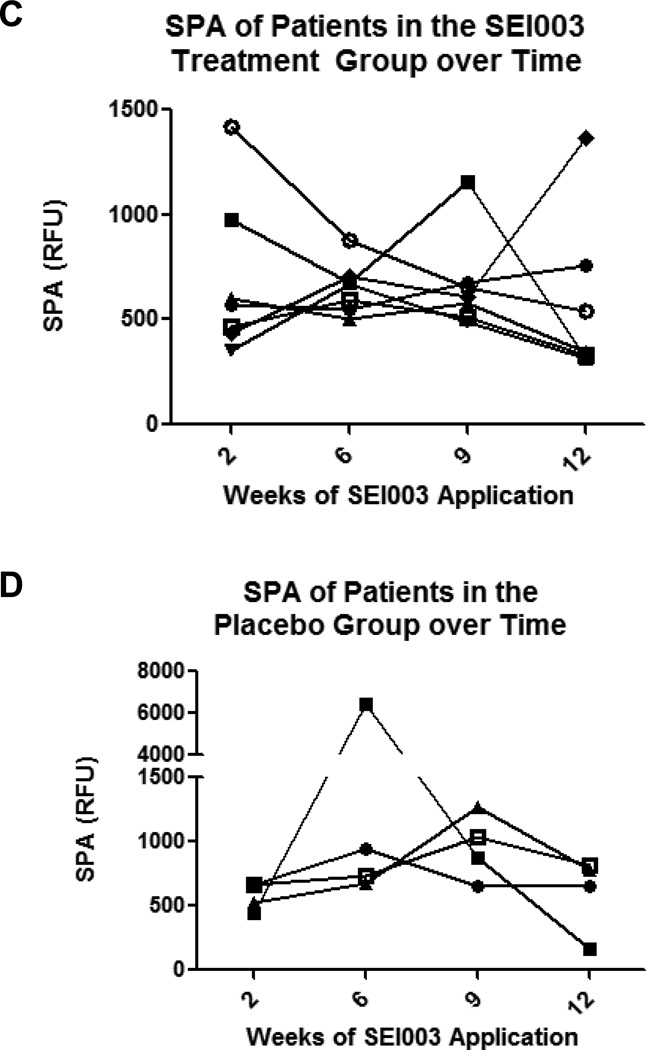
The average age and baseline IGA and CEA scores for subjects in the two groups were similar (Figure 2A). The average of the SEI003 treatment group had significantly lower SPA compared to the placebo group at weeks 6, 9 and 12 after start of therapy. A two-way ANOVA comparing the SPA of subjects in the two groups at all visits showed that treatment group (p = 0.002), time (p = 0.002), and the interaction between time and treatment group (p = 0.001) all had a significant effect on subjects’ SPA (Figure 2B). As this was a small pilot study, and to better illustrate the individual response of SPA over the course of the study, SPA levels were also plotted for each subject over time. SPA levels of the two subjects with the highest baseline SPA had the most pronounced decrease (Figure 2C). In contrast, SPA levels of subjects in the placebo group remained relatively stable during the course of the study (Figure 2D).
Figure 2.
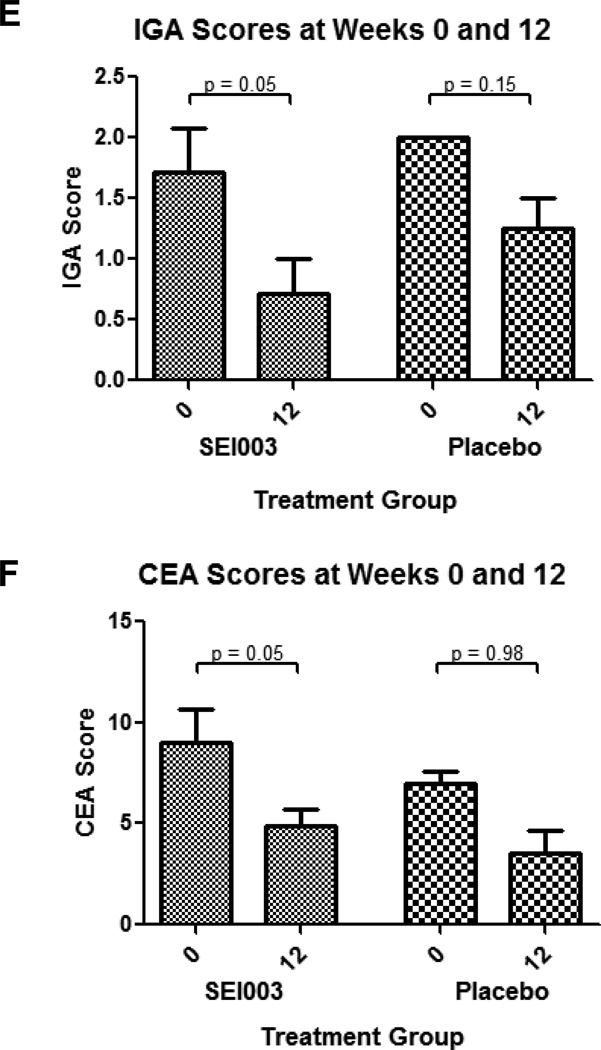
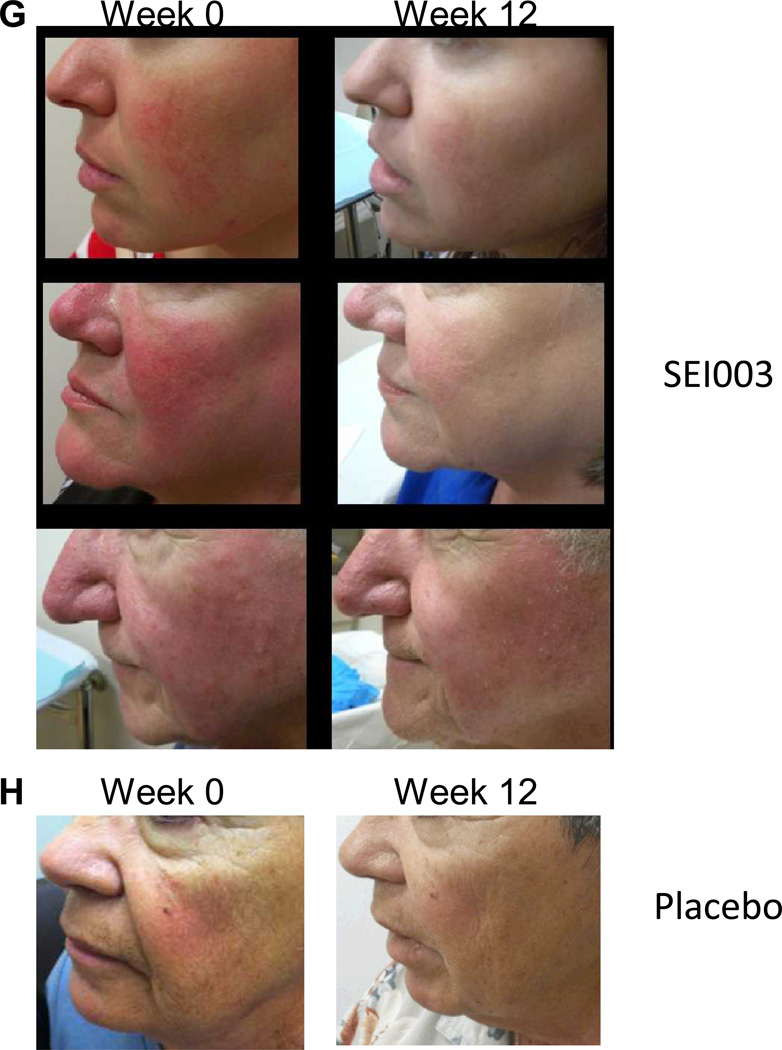
Response of rosacea patients to SEI003 treatment. (A) Demographic data for participants completing the trial. (B) SPA levels were not significantly different in the treatment groups at week 2, however differences at week 6, 9 and 12 were statistically significant. (C) SPA levels of individual subjects in the treatment group tended to decrease over time. (D) SPA levels of individual subjects in the placebo group remained relatively unchanged over time. (E) IGA scores decreased throughout the study for participants in both groups, however scores were only significant for time and the interaction between time and treatment group. (F) CEA scores also trended down as participants progressed through the study, however a two-way ANOVA of CEA scores for participants in both groups was significant only for time. (G) Decreased erythema is seen in patients in the treatment group at week 12. (H) Decreased erythema is also appreciated in this control subject over time, however this finding is less pronounced in these patients. Error bars represent mean +/− standard error of the mean. Treatment group n = 7, control group n = 4.
Overall improvements in IGA and CEA scores were seen in subjects in both the placebo and SEI003 groups over the 12-week course of the study. Although there were no significant differences in IGA and CEA scores between the two groups at any time point, a correlation between activity to inhibit SPA and clinical improvement was seen as IGA and CEA scores of subjects in the SEI003 group differed significantly at week 12 compared to baseline (p=0.05, Figure 2E, F). This significant change was not seen in the placebo group (p=0.15, Figure 2E; p=0.98, Figure 2F). These findings are likely related to the small sample size and short duration of the study, as well as a placebo effect from the base cream. Digital photographs taken of participant’s faces at the beginning of each visit showed the pronounced improvement in rosacea symptoms in some patients receiving SEI003 (Figure 2G and 2H). Interestingly, the two subjects with the highest baseline SPA values were among the subjects with the most noticeable changes on digital photography, and both are pictured in Figure 2G. No adverse events were reported during the study.
Previous studies have correlated high KLK5 activity with rosacea disease state (Yamasaki et al, 2007). Recent studies of known rosacea treatments suggest that clinical improvements correlate with decreases in this protease cascade, suggesting that KLK5 plays a key role in mediating the inflammatory response seen in rosacea by its ability to activate cathelicidin. A recent open-label study of 15% azelaic acid gel showed that rosacea patients with high baseline SPA had a significant reduction in their SPA by week 16 of treatment, and this correlated with clinical improvement (Coda et al, 2013). Our data show a similar trend, with subjects with the highest baseline SPA correlating with maximal improvement. In another recent study, the antibiotic doxycycline was found to indirectly inhibit SPA and block LL-37 generation in vitro (Kanada et al, 2012). Subsequently, a report of a multi-center clinical trial showed that the therapeutic benefits of doxycycline when taken as a formulation consisting of both immediate release and delayed release beads also correlated with decreased protease activity and LL-37 (Huang et al, 2013). Our study agrees with the associations observed in these other studies, and further suggests that direct targeted inhibition of SPA can result in a reduction of erythema and inflammatory papules in some patients with rosacea.
In conclusion, this pilot study shows early clinical evidence that directly supports a causative role for high protease activity in the pathogenesis of rosacea. Although we failed to show clear evidence of clinical benefit over placebo for this formulation of serine protease inhibitor, this study was designed only as a proof of concept trial with a small number of patients. This work supports the KLK-cathelicidin inflammation hypothesis and the need for adequately powered clinical trial of the therapeutic benefit of direct targeting of SPA in the treatment and control of rosacea.
ACKNOWLEDGMENTS
In vitro analysis described in this work was supported in part by the United States National Institute of Health (NIH) grant R01- AR052728 to RLG. Neither Therapeutics, Inc. nor Skin Epibiotics, Inc. provided any financial compensation for the study or to any members of the study team with the exception of EH, who left his position at UCSD for employment opportunities at these companies part-way through the study.
Abbreviations used
- ACA
ε-aminocaproic acid
- KLK
kallikrein
- SPA
serine protease activity
- IGA
Investigator’s Global Assessment
- CEA
Clinician’s Erythema Assessment
- UCSD
University of California San Diego
REFERENCES
- 1.Coda AB, Hata T, Miller J, Audish D, Kotol P, Two A, Shafiq F, Harper JC, Del Rosso JQ, Gallo RL. Cathelicidin, KLK5 and serine protease activity is inhibited during treatment of rosacea with azelaic acid 15% gel. J Am Acad Dermatol. doi: 10.1016/j.jaad.2013.05.019. advance online publication 18 July 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang E, DiNardo A, Gallo R, et al. Surface cathelicidin expression is a predictor of treatment success in papulopustular rosacea. J Invest Dermatol. 2013;133(S1):S23. (Abstr.) [Google Scholar]
- 3.Kanada KN, Nakatsuji T, Gallo RL. Doxycycline indirectly inhibits proteolytic activation of tryptic kallikrein-related peptidases and activation of cathelicidin. J Invest Dermatol. 2012;132:1435–1442. doi: 10.1038/jid.2012.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koczulla R, von Degenfeld G, Kupatt C, et al. An angiogenic role for the human peptide antiobitic LL-37/hCAP-18. J Clin Invest. 2003;111:1165–1172. doi: 10.1172/JCI17545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lande R, Gregorio J, Facchinetti V, et al. Plasmacytoid dendritic cells sense self-DNA coupled with antimicrobial peptide. Nature. 2007;449:564–569. doi: 10.1038/nature06116. [DOI] [PubMed] [Google Scholar]
- 6.Morizane S, Yamasaki K, Muhleisen B, et al. Cathelicidin antimicrobial peptide LL-37 in psoriasis enables keratinocyte reactivity against TLR9 ligands. J Invest Dermatol. 2012;132:135–143. doi: 10.1038/jid.2011.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamasaki K, Di Nardo A, Bardan A, et al. Increased serine protease activity and cathelicidin promotes skin inflammation in rosacea. Nat Med. 2007;13:975–980. doi: 10.1038/nm1616. [DOI] [PubMed] [Google Scholar]
- 8.Yamasaki K, Schauber J, Coda A, et al. Kallikrein mediated proteolosis regulates the antimicrobial effects of cathelicidins in skin. FASEB J. 2006;20:2068–2080. doi: 10.1096/fj.06-6075com. [DOI] [PubMed] [Google Scholar]