Abstract
A changing undergraduate demographic and the need to help students develop advanced critical thinking skills in neuroanatomy courses has prompted many faculty to consider new teaching methods including clinical case studies. This study compared primarily conventional and inquiry-based clinical case (IBCC) teaching methods to determine which would produce greater gains in critical thinking and content knowledge. Results showed students in the conventional neuroanatomy course gained less than 3 national percentile ranks while IBCC students gained over 7.5 within one academic term using the valid and reliable California Critical Thinking Skills Test. In addition to 2.5 times greater gains in critical thinking, IBCC teaching methods also produced 12% greater final exam performance and 11% higher grades using common grade performance benchmarks. Classroom observations also indicated that IBCC students were more intellectually engaged and participated to a greater extent in classroom discussions. Through the results of this study, it is hoped that faculty who teach neuroanatomy and desire greater critical thinking and content student learning outcomes will consider using the IBCC method.
Keywords: inquiry-based clinical case teaching (IBCC), neuroanatomy pedagogy, active learning, critical thinking
Teaching an undergraduate neuroanatomy course can be challenging because it tends to require a more systemic approach rather than a regional or topographic perspective as is often the case in many anatomy courses. Moreover, the ways in which neuroanatomy teaching is organized and the diverse anatomical levels taught (ranging from microscopic to macroscopic to gross anatomy) require a different instructional approach. The challenge is further compounded by the observation that many students seem to suffer from “neurophobia.” Jozefowicz coined this term to describe student “fear of the neural sciences and clinical neurology that is due to students’ inability to apply their knowledge of basic sciences to clinical situations” (Jozefowicz, 1994). Students often consider neuroscience material to be highly complex and many struggle throughout these courses. Given these challenges, many educators are seeking pedagogical methods that go beyond the conventional lecture/laboratory method of teaching neuroscience generally and neuroanatomy specifically (Lynd-Balta, 2006; Krontiris-Litowitz, 2008; Svirko and Mellanby, 2008).
National agencies have called for significant improvements in teaching and assessment methods in science, technology, engineering, and mathematics (STEM) courses (American Association for the Advancement of Science, 2009; National Research Council, 2002, 2006; Business-Higher Education Forum & American Council on Education, 2003). The goal is to promote critical thinking and relate learning to real world scenarios rather than rely mainly on rote memorization of scattered facts. According to Bloom’s Taxonomy of Educational Objectives (Bloom and Krathwohl, 1956) instructors should strive to create learning environments that give students opportunities to apply, analyze, synthesize, and evaluate information – in other words use advanced cognitive processing like critical thinking. Critical thinking can be defined as a process of purposeful self-regulatory judgment that drives problem solving and decision making (Facione, 2010). At the core of critical thinking are the component skills of analysis, interpretation, inference, explanation, evaluation, and self-regulation (Facione, 2000). The ability to think critically is also pivotally important to personal and professional success for both students and faculty (Facione, 2009). The pervasive importance of critical thinking is illustrated by a national survey which showed that 93% of college faculty consider analytical and critical thinking to be among the most essential skills students can develop, and while 87% of students believe college experiences prepare them to think, a paltry 6% of graduates can actually demonstrate significant gains in critical thinking (Association of American Colleges and Universities, 2005). An increasing number of national reports further underscores a growing concern about the ineffectiveness of some higher education teaching practices and resulting decreased performance of U.S. students relative to other countries (Gröschner et al., 2010). The goal then for teaching any course like neuroanatomy should be to provide engaging, relevant learning experiences in an environment that encourages intellectual risk-taking and development of critical thinking and content knowledge over time (Quitadamo et al., 2008).
Given the vast array of instructional approaches available and potential workload issues that revolve around course preparation, it can be difficult to choose methods that clearly connect critical thinking with science teaching methods. The difficulty of making data-based instructional choices is further compounded by a general lack of studies that clearly show which teaching methods produce critical thinking gains. Most studies overly rely on anecdotal evidence including academic performance (e.g., GPA), undergraduate and alumni surveys of student and faculty attitudes and perception, percent entry into STEM programs, and post-graduation marketability and employment rates (Kinkel and Henke, 2006; Russell et al., 2007). In addition, there has been a lack of empirical studies that have investigated anatomy teaching methods in relation to learning and critical thinking (Terrell, 2006; Collins, 2008). Ultimately, what is needed is a practical teaching approach that improves critical thinking skills and connects teaching and learning to solving real world problems (Quitadamo et al., 2008), such as those found in clinical settings.
One teaching method that is designed to foster critical thinking is inquiry-based teaching. Generally speaking, inquiry-based instruction incorporates elements of undergraduate research to promote student inquiry and discovery in an authentic context (Blumenfeld et al., 1991; Sclove, 1995). For example, the Community-Based Inquiry (CBI) method consists of several elements that include authentic inquiry related to community need, case study exercises aligned to major course themes, peer evaluation and individual accountability, and lecture/content discussion focused on key concepts (Sundberg, 2003; Pukkila, 2004). Studies have shown that inquiry-based instruction in general science courses can improve student critical thinking (Ernst and Monroe, 2006; Quitadamo and Kurtz, 2007; Quitadamo et al., 2008); however it remains unclear whether inquiry-based instruction that incorporates clinical cases (IBCC) can be successfully implemented in more specialized content courses such as neuroanatomy and whether similar critical thinking gains can be achieved. Case studies have been shown to be an important tool for gaining insight into neurological conditions and serve as an effective teaching method in neuroscience courses (Meil, 2007; Kennedy, 2013). Moreover, case studies, in particular those that use real life scenarios to explore particular content topics, also appear to help develop student critical thinking skills as they acquire new content knowledge (Chaplin, 2009; Noblitt et al., 2010). Given that both inquiry and case study methods independently appear to improve critical thinking, it seems likely that a combination of the two in the context of clinical relevance should produce greater critical thinking gains than either alone.
The purpose of this study was to discover whether an IBCC approach could be implemented in an undergraduate neuroanatomy course and whether IBCC could produce greater student critical thinking gains as compared to conventionally-taught sections of the same course.
MATERIALS AND METHODS
Participants
This study took place at a regional university in the Pacific Northwest. Three sections of an undergraduate Human Neuroanatomy course over two successive years were included in the study (n = 85). One section comprised of conventional didactic lecture that included some alternative assessment methods like oral exams was assigned as a conventional group (n = 27); and two sections that implemented an IBCC approach were assigned as the experimental group (n = 58). Neither conventional nor IBCC sections included a full lab section; however, both courses included one class period in the human cadaver lab. All students included in the study provided IRB-sanctioned informed consent for their participation on the first day of class. Only students who completed both the critical thinking pre- and post-tests were statistically analyzed for critical thinking (n = 42). All students enrolled in the courses were analyzed for exam and course grade performance (n = 85).
Study Context
This study followed the general approach described previously for Community-Based Inquiry (Quitadamo et al., 2008) but included a major focus on clinical case studies. All course sections were taught in similarly appointed modern classrooms and common laboratory facilities. Each lecture was taught for 90 minutes two days a week. The same instructor taught all course sections included in the conventional and IBCC groups. The same course textbook was also used in all course sections. Conventional and IBCC groups differed primarily by the instructional method used. The conventional group used a standard didactic lecture format whereby the instructor covered a range of common neuroanatomy material including general anatomy of the central nervous system, cranial nerves, neuropathology, basic sensory and motor system structure and function, etc. Identical topics were also covered in the IBCC group using more unconventional methods. Little emphasis was placed on student-driven scientific inquiry in the conventional group and with the exception of oral exams there were no activities used that explicitly addressed critical thinking skills. A comparison of methods used in IBCC and conventional groups is described in Table 1.
Table 1.
Methods used in IBCC and conventional groups. The +, +/−, and − symbols refer to full, partial, or no use of method, respectively.
| Method | Conventional | IBCC |
|---|---|---|
| Lecture | + | + |
| Human cadaver lab | + | + |
| Small groups | − | + |
| Clinical case studies | − | + |
| Oral & written exams | +/− | + |
| Peer and self-evaluation | − | + |
| Critical thinking framework | − | + |
Description of the IBCC Method
The IBCC teaching method consisted of three elements that were intended to work together with the express purpose of promoting gains in content knowledge and critical thinking. These elements included: 1) clinical case studies aligned to major content themes, 2) group work that included peer evaluation and individual accountability, and 3) lecture/content discussion. All three elements were integrated and used as a framework (Sundberg, 2003; Pukkila, 2004) focused on promoting the development of critical thinking through clinical application.
On the first day of lecture, the IBCC instructor informed the students that their course performance would be evaluated using a combination of clinical case studies, small group work with peer evaluations, and oral exams in addition to conventional written midterm and final exams. The criteria for completing IBCC assignments were further explained at that time. Students were grouped into small “clinical teams” of three to four students by the second week of classes.
Clinical case studies were used during lecture to increase student understanding of functional neuroanatomy and to facilitate collaborative learning. Approximately four to five lecture periods were devoted to case study work during the term. Each case study exercise was designed around a major theme in neuroanatomy (e.g., cranial nerve function) and intended to explicitly reinforce critical thinking and development of anatomical knowledge (Meester, 2011). The focus of each clinical case was based on real clinical cases, as listed in Blumenfeld's Neuroanatomy through Clinical Cases (Blumenfeld, 2002). Each clinical case followed a slightly modified version of the interrupted case method (Herreid, 2005) where students worked in their clinical teams and submitted all answers in writing. Each exercise consisted of multiple parts (usually two to three) that were completed sequentially. The choice to use collaborative teams with IBCC was based on existing literature (Jones and Carter, 1998; Springer et al., 1999) that has shown writing in small groups measurably improves undergraduate critical thinking skills (Quitadamo and Kurtz, 2007).
Each student team was required to work through assigned cases in a clinical manner to identify important questions and variables, state hypotheses, integrate important content information (supported by lecture), analyze data, and draw reasoned clinical conclusions on possible diagnoses and the involved neuroanatomy. See Appendix I for an example clinical case. Throughout each clinical case, the instructor monitored each group and posed additional Socratic questions (Elder and Paul, 2004) aimed at clarifying the student’s initial questions and/or answers from groups and individual students. Teams then reflected on the instructor’s comments and revised their work prior to turning in their written answers. This reflection and revision strategy was used in an attempt to develop student critical thinking (Brookfield, 1987) and metacognitive awareness (Donovan and Bransford, 2005).
Peer evaluations and self-reflection were another element of the IBCC model that provided individual accountability within each clinical team. This was done to help students reflect on and evaluate their own performance, maximize individual contributions to the group, and ensure students received credit proportional to their contributions. A peer evaluation rubric was used to assess team members based on their contributions, quality of work, effort, attitude, focus on tasks, work with others in the group, problem solving and group efficacy. Peer evaluation has been shown to be an effective tool to assess contributions of individual group members (Weimer, 2008).
The third element in the IBCC instructional model was converting the conventional lecture to a discussion highlighted by Socratic questioning (Elder and Paul, 2004). As with conventional lectures, discussions were largely content-driven, but were modified to explicitly support the current clinical case within a course framework of critical thinking. The scientific method, inquiry as a process, and Socratic questioning were emphasized. Students in both courses were encouraged to visualize anatomy as a three-dimensional mental picture and applying that knowledge in a broader context.
Finally, the IBCC students participated in a mid-term and final-exam that had both written and oral components. The written portion of the exams were primarily multiple choice, similar to the conventional group exams but with clinical cases added. Like the conventional group, the oral portion of the exams consisted of students labeling neuroanatomical structures, stating functional connections and making clinical connections from slides that were presented by the instructor via a PowerPoint presentation. The choice to incorporate clinical case questions during exams was supported by the literature that shows anatomy should be taught and learned within a clinically meaningful context (Weatherall, 2006), and that assessment should focus on tasks that resemble realistic clinical problems and reward integration and application (Ramsden, 2003).
RESULTS
A quasi-experimental pretest/posttest control group design was used to determine critical-thinking gains in IBCC and conventional groups. This design was chosen because intact groups were used and it was not feasible to randomly assign students between course sections. In the absence of a true experimental design, this design was the most useful because it minimizes threats to internal and external validity (Campbell and Stanley, 1963). Given the study design and ability to more accurately estimate error, a repeated-measures ANOVA test was used to statistically test for pretest/posttest differences in critical thinking. Pretest sensitivity and selection bias were potential concerns, but minimized via the use of the valid and reliable California Critical Thinking Skills Test (CCTST) that has been evaluated for sensitivity (Facione, 1990). The CCTST is a well established, discipline neutral, critical thinking assessment (Facione, 1990; Facione and Facione, 2004) that has been used in both educational and workplace settings. Specifically, the CCTST is designed to determine a student’s ability to analyze arguments, determine validity of deductive and inductive arguments, evaluate reasoning, analyze data presented in charts and diagrams and engage them in real world issues.
Critical Thinking Performance
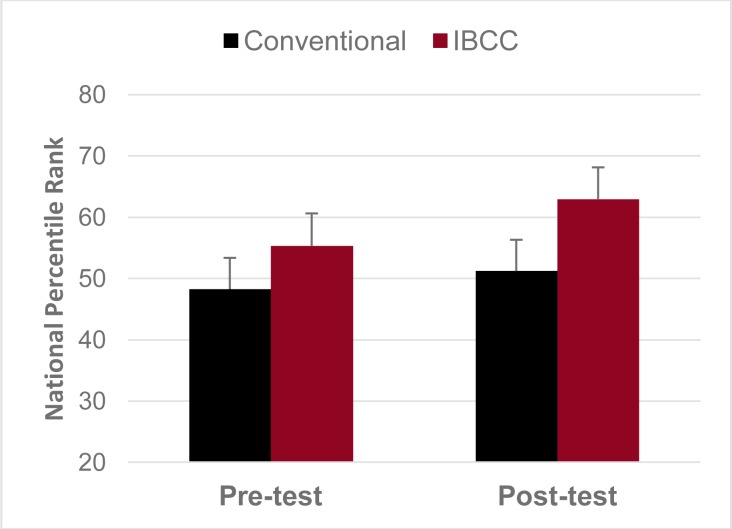
Student critical thinking skills were assessed using an online version of the CCTST. Students in the conventional group had somewhat lower initial critical thinking (M=48.26, S.E.= 6.41) and showed modest critical thinking gains (2.95 national percentile gain) as compared to the IBCC group that had slightly higher initial critical thinking (M=55.35, S.E.=5.1) and larger critical thinking gains (7.52 national percentile gain). On average, IBCC students showed over 2.5 times greater critical thinking gains than did conventionally-taught students. See Table 1 and Figure 1 for a summary of results.
Figure 1.
Comparison of critical thinking performance for conventional and IBCC neuroanatomy course sections. Numbers represent critical thinking national percentile rank as measured by the California Critical Thinking Skills Test.
A more detailed analysis revealed differences in the following component skills of critical thinking. IBCC students showed 6.5-fold greater analysis, 3.3-fold greater inference, and 3-fold greater interpretation skills than students in the conventional group.
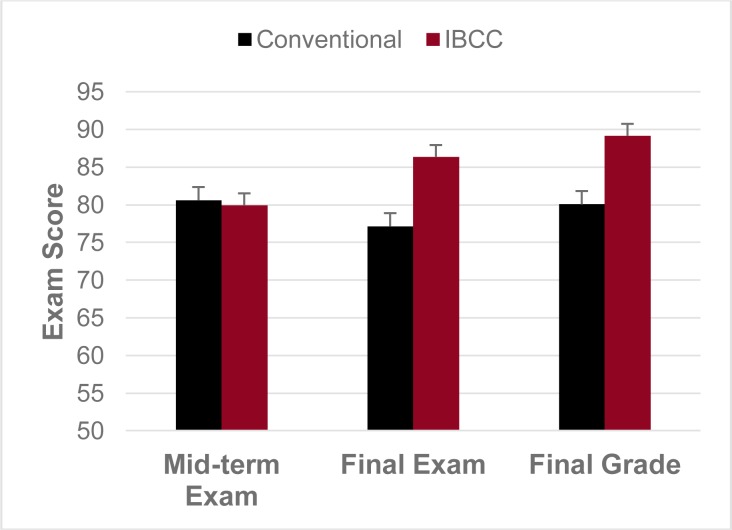
Exam Performance
Students in the conventional and IBCC groups had highly similar mid-term exam scores (M=80.58, S.E.=1.78 and M=79.91, S.E.=1.61, respectively). However, IBCC students demonstrated higher (p=.05) final exam scores (M=86.33, S.E.=1.76) than the conventional group (M=77.12, S.E.=2.67). IBCC students also received significantly (p=0.001) higher final grades (M=89.14, S.E.=1.25) than students in the conventional group (M=80.05, S.E.=1.7). Altogether, IBCC students had 12% higher final exam and 11% higher final grade scores than conventionally-taught students. See Table 2 and Figure 2 for a summary of results.
Table 2.
Summary of critical thinking and content gains. Comparison of critical thinking, mid-term and final exam scores and final course grades for conventional and IBCC courses.
| Conventional (N=27) | IBCC (N=42) | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| CCTST Score Pre-test | 48.26 | 6.41 | 55.35 | 5.1 |
| CCTST Score Post-test | 51.21 | 6.69 | 62.87 | 5.27 |
| Mid-term Exam | 80.58 | 1.78 | 79.91 | 1.61 |
| Final Exam | 77.12 | 2.67 | 86.33 | 1.76 |
| Final Course Grade | 80.05 | 1.7 | 89.14 | 1.25 |
Figure 2.
Profile of course exam and grade performance between conventional and IBCC course sections. Numbers represent scores on a scale from 0–100. Exam content assessed with each exam was highly comparable between conventional and IBCC courses.
Student Reaction
In order to assess reaction to the IBCC approach, students were explicitly instructed to comment on the IBCC model in their Self-evaluation paper. All students in the IBCC courses completed the Self-evaluation, with 95% of students indicating that the IBCC approach was a valuable learning experience. Specifically, the vast majority of students (>90%) indicated that the IBCC approach helped them to integrate course information, increase content knowledge, enhance interest of course material, and stimulate critical thinking. Generally, students commented that they found the IBCC approach to be an enjoyable and engaging way to learn neuroanatomy.
DISCUSSION
The purpose of this study was to discover whether an IBCC instructional approach would elicit greater gains in critical thinking than conventional lecture/laboratory instruction in an undergraduate neuroanatomy course. Results indicated that students experiencing IBCC instruction showed greater overall gains in critical thinking, greater specific gains in analysis, inference, and interpretation skills, performed better on content exams, and received significantly higher grades. To our knowledge, there have been no prior studies that directly assessed critical thinking gains as it relates to teaching neuroanatomy. Further, the significantly higher grades of the IBCC group are consistent with the notion that application of anatomical knowledge in a clinically relevant manner is an effective method for enhancing student learning and understanding of anatomy (Woods et al., 2006; Bergman et al., 2008; Collins, 2008; Ward and Walker, 2008). Specifically, clinical case studies serve to connect student experiences to textbook content, making them more relevant to student daily life. This increases student engagement and reinforces clinical principles and critical thinking (Meil, 2007; Walton, 2008; Noblitt et al., 2010; Kennedy, 2013). Collectively, the results of this study indicate that IBCC students outperform conventionally-taught students and show greater gains in overall critical thinking.
Faculty considering whether to use IBCC may wonder about their specific role, and if time and energy spent implementing the method will produce better clinicians and scientists. Aside from engaging in meaningful diagnostic exercises and learning to think critically, it is also important that students learn to appreciate the scientific and clinical process. The instructor must play a pivotal role in IBCC, modeling a range of good scientific and clinical behaviors from how to problem solve to drawing conclusions based on evidence. A clear emphasis is placed on the value of clinical discovery, not just rote memorization of facts. Moreover, the instructor emphasizes the importance of active and deep learning (Pandey and Zimitat, 2007) by highlighting the clinical relevance of the material with a focus on the meaning of content rather than just the content itself.
Faculty trying IBCC for the first time may find that some students become frustrated over the first 2–4 weeks of the term because they are asked to do more than memorize. Whereas others have found students may remain skeptical and develop negative attitudes of new instructional methods for some time (Sundberg and Moncada, 1994), our results indicate IBCC students rapidly become acclimated after about three weeks as clinical cases begin and beneficial relationships between clinical practices and critical thinking become more clear. Although this study did not assess student reaction via a formal survey, responses from the student self-evaluation papers clearly indicated that students regarded the IBCC approach as a positive learning experience. Generally, students found the use of clinical cases to be an enjoyable aspect of the course. In addition, classroom observations indicated that IBCC students were more intellectually engaged and participated to a greater extent in classroom discussions than students in the conventional teaching group. Learning how to use critical thinking as the course framework (Pukkila, 2004) and clearly connecting this to real-world contexts (Meester, 2011) appears to be a major element in the success of the IBCC approach. This may explain why students in the IBCC group showed higher overall and specific critical thinking gains and significantly higher course scores than the conventional group.
Some practical considerations for adopting the IBCC approach include clearly defining for students what kinds of critical thinking behaviors and skills are expected, and developing explicit examples of how critical thinking relates to clinical conditions (Meester, 2011). Time spent evaluating and providing meaningful feedback on student’s clinical cases is another potential concern of faculty. In this study, implementation of IBCC did not take more time and effort per se; rather, it required faculty to re-conceptualize how they spent their instructional time and adopt different primary objectives. For example, students were informed ahead of time that each member of their clinical group would receive the lowest common grade for their clinical case. As a result, students tended to self regulate group behavior and productivity. Rubric evaluations, which would be time-consuming if faculty completed one for every student, were provided for each clinical group. Group members then discussed strengths and weaknesses of their submission and worked collaboratively to address them. Successful implementation requires training on inquiry-based objectives to faculty and teaching assistants, how to evaluate student work using a rubric, reinforcement of the Socratic teaching method, and collaborative learning. Moreover, faculty and teaching assistants must understand how an inquiry-based clinical case model is different, why it is being used, and what they can expect from students (Sundberg et al., 2000; Quitadamo et al., 2008).
A limitation of this study is that it did not evaluate content knowledge via a standardized content exam. However, students in the IBCC group showed significantly higher final comprehensive exam scores and final course grades. Future research may want to specifically compare content knowledge of students in both conventional and IBCC groups via a standardized content exam. It is important to note that the IBCC instructor covered the same amount of lecture content as he had in the conventionally taught course. Perceived lack of content knowledge is a common criticism of teaching methods that focus on thinking process, although recent studies have shown no content knowledge penalties manifest (Sundberg, 2003), especially if content is directly linked to reasoning skills (Fencl, 2010). Overall, the curriculum, teaching, and assessment must encourage the learning of clinically meaningful anatomy (Collins, 2008).
In conclusion, results of this study are encouraging for faculty who seek better alternatives to conventional teaching pedagogies if their goal is to improve student critical thinking, class engagement and content knowledge. Based on previous literature on effective anatomy teaching and the results presented here, we conclude that IBCC helps improve student’s critical thinking skills in an undergraduate neuroanatomy course. IBCC is an instructional method that has the potential to improve essential learning outcomes like critical thinking and clinical reasoning, which in turn enhance the cognitive performance and competitiveness of students and future clinicians. As the search for better ways to teach and learn neuroscience continues, IBCC warrants consideration as an effective neuroscience instructional method.
APPENDIX I.
Appendix I includes a sample three-part clinical case study appropriate for use with the IBCC method. Each case study was based on authentic clinical cases, as listed in Blumenfeld's Neuroanatomy through Clinical Cases (Blumenfeld, 2002).
Sample Case: Delayed Unresponsiveness After Head Injury
Part One
Chief Complaint: A 52-year-old man was found to be progressively unresponsive the morning after a head injury.
Patient History:
The night before admission, patient WJ fell down a flight of cement stairs at 1:00 AM, following a domestic altercation. He struck his left temporal area and lost consciousness for about 12 minutes. By the time the police and paramedics arrived, however, he was fully awake, smelled of alcohol, and refused medical treatment. He was arrested on domestic violence charges and spent the night in jail. In the morning, officers found him difficult to arouse, thrashing about incoherently. He had vomited and defecated in the cell overnight. He was transported to the emergency room for evaluation.
Past Medical History:
Unremarkable
Past Surgical History:
Surgery for appendicitis around age 26.
Medications:
None
Social & Family History:
Not recorded
Physical Examination:
WJ’s general appearance was disheveled, with several stains on his shirt. There was a left forehead abrasion; no raccoon eyes.
Neurological Examination:
Mental Status: the patient was unresponsive to commands. Not speaking and occasionally trashed on the stretcher in agitated, semi purposeful fashion. Shortly after arriving in the emergency room, the patient became completely unresponsive.
Cranial Nerve Function: left pupil was dilated and fixed (no response to light). Right pupil normal constricting in response to light.
Motor and Sensory exam: Withdrew left arm and left leg purposefully from painful stimulation. Right arm and leg did not move in response to pain.
Gait: not tested
Questions
Working in your clinical teams, please answer the following questions as completely and thoroughly as possible. You may use your textbook, atlas or any other resource at your disposal to answer these questions.
Evaluate the symptoms & signs and prioritize them in order of importance. Please provide a rationale for your thinking.
Please define hyperreflexia. Briefly discuss the relevance of this symptom.
Evaluate the clinical symptoms, what is the most likely diagnosis? What are some other possibilities? Please explain.
What diagnostic test(s) could you order to help narrow down a diagnosis? Please provide a rationale for your choice.
Damage to which possible neuroanatomical pathways could account for the patient’s symptoms? Please explain.
Could this be an upper or lower motor neuron lesion? Please explain your choice & why this is an important distinction?
Part Two
Because of the patients change in clinical status, an urgent head CT was ordered. Provide the students with an appropriate CT image.
Questions:
Working in your clinical teams, please answer the following questions as completely and thoroughly as possible. You may use your textbook, atlas or any other resource at your disposal to answer these questions.
Analyze this image and label some key anatomical structures & regions.
What anatomical orientation is this image?
Contrast this CT image with what an MRI of the same image would look like.
What do you notice about this image? What are some of the possible causes?
Based on this new information, what is your diagnosis?
How does it compare to the one you made in part one?
What course of treatment would you recommend? Please provide a rationale for your choice.
Part Three
Working in your clinical teams, briefly reflect on your learning process and knowledge base. Discuss what you believe to be your team’s strengths and weaknesses as it relates to the material.
Questions:
What strategies did you use to work on this clinical case? Where they effective? How could you improve them on the next clinical case?
Evaluate your knowledge of brain anatomy (what level of confidence do you have about your knowledge of the relevant neuroanatomy, etc.).
What areas do you need to review or study further?
Footnotes
This work was supported by the National Science Foundation grant, Using Community-Based Inquiry to Build Faculty Capacity and Student Critical Thinking (DUE-1023093). The authors thank Dr. Martha Kurtz, Dr. James Johnson, and Dr. Carin Thomas for project collaboration and Kristy Kappenman and Page Wooller for assessment and research support.
REFERENCES
- American Association for the Advancement of Science . Vision and change in undergraduate biology education: a call to action. Washington, D.C.: 2009. [Google Scholar]
- Association of American Colleges and Universities . Liberal education outcomes: a preliminary report on student achievement in college. Washington, D.C.: 2005. [Google Scholar]
- Bergman EM, Prince KJ, Drukker J, van der Vleuten CP, Scherpbier AJ. How much anatomy is enough. Anat Sci Educ. 2008;1:184–188. doi: 10.1002/ase.35. [DOI] [PubMed] [Google Scholar]
- Bloom BS, Krathwohl DR. Taxonomy of educational objectives: the classification of educational goals by a committee of college and university examiners. Hanbook 1: Cognitive Domains. New York, NY: Longman, Green; 1956. [Google Scholar]
- Blumenfeld PC, Soloway E, Marx RW, Krajcik JS, Guzdial M, Palincsar A. Motiviating project-based learning: sustaining the doing, supporting the learning. Educ Psychol. 1991;26:369–398. [Google Scholar]
- Blumenfeld H. Neuroanatomy through clinical Cases. Sunderland, MA: Sinauer Associates Inc; 2002. [Google Scholar]
- Brookfield SD. Developing critical thinkers: challenging adults to explore alternative ways of thinking and acting. San Francisco, CA: Jossey-Bass; 1987. [Google Scholar]
- Business-Higher Education Forum & American Council on Education . Building a nation of learners: the need for changes in teaching and learning to meet global challenges. Washington, D.C.: 2003. [Google Scholar]
- Campbell DT, Stanley JC. Experimental and quasi-experimental designs for research. Boston, MA: Houghton Mifflin Company; 1963. [Google Scholar]
- Chaplin S. Assessment of the impact of case studies on student learning gains in an introductory biology course. J Coll Sci Teach. 2009;39:72–78. [Google Scholar]
- Collins JP. Teaching and learning anatomy. Student BMJ. 2008;337:a1753. doi: 10.1136/bmj.a1310. [DOI] [PubMed] [Google Scholar]
- Donovan S, Bransford JD, editors. How students learn: Science in the classroom. Washington, D.C.: National Academy Press; 2005. [Google Scholar]
- Elder L, Paul R. The miniature guide on the art of asking essential questions for students and teachers. Dillon Beach, CA: Foundation for Critical Thinking; 2004. [Google Scholar]
- Ernst J, Monroe M. The effects of environment-based education on student’s critical thinking skills and disposition toward critical thinking. Environ Educ Res. 2006;12:429–443. [Google Scholar]
- Facione PA. The California critical thinking skills test: college level. Technical report #1. Experimental validation and content validity. Millbrae, CA: Insight Assessment; 1990. [Google Scholar]
- Facione PA. The disposition toward critical thinking: its character, measurement, and relationship to critical thinking skill. Informal Logic. 2000;20:61–84. [Google Scholar]
- Facione PA, Facione NC. Insight assessment. 2004. Test of everyday reasoning.
- Facione PA. Critical thinking; what it is and why it counts. 2009 Update. Millbrae, CA: Insight Assessment; 2009. [Google Scholar]
- Facione PA. Think critically. New Jersey: Prentice Hall; 2010. [Google Scholar]
- Fencl HS. Development of students' critical-reasoning skills through content-focused activities in a general education course. J Coll Sci Teach. 2010;39:56–62. [Google Scholar]
- Gröschner A, Heinz JLK, Seidel T. Measures and indicators for inquiry-based science teaching as published from 2005–2009: a research review. Munich: TUM; 2010. [Google Scholar]
- Herreid CF. The interrupted case method. J Coll Sci Teach. 2005;35:4–5. [Google Scholar]
- Jones GM, Carter G. In: Small groups and shared constructions. In: Teaching science for understanding: a human constructivist view. Mintzes, editor. San Diego, CA: Academic Press; 1998. pp. 261–279. [Google Scholar]
- Jozefowicz R. Neurophobia: the fear of neurology among medical students. Arch Neurol. 1994;51:328–329. doi: 10.1001/archneur.1994.00540160018003. [DOI] [PubMed] [Google Scholar]
- Kennedy S. Using case studies as a semester-long tool to teach neuroanatomy and structure-function relationships to undergraduates. J Undergrad Neurosci Educ. 2013;12:A18–22. [PMC free article] [PubMed] [Google Scholar]
- Kinkel DH, Henke SE. Impact of undergraduate research on academic performance, educational planning and career development. J Nat Res Life Sci Educ. 2006;35:194–201. [Google Scholar]
- Krontiris-Litowitz J. Using truncated lectures, conceptual exercises, and manipulatives to improve learning in the neuroanatomy classroom. Adv Physiol Educ. 2008;32:152–156. doi: 10.1152/advan.00103.2007. [DOI] [PubMed] [Google Scholar]
- Lynd-Balta E. Using literature and innovative assessments to ignite interest and cultivate critical thinking skills in an undergraduate neuroscience course. CBE – Life Sci Educ. 2006;5:167–174. doi: 10.1187/cbe.05-08-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meil WM. The use of case studies in teaching undergraduate neuroscience. J Undergrad Neurosci Educ. 2007;5:A53–62. [PMC free article] [PubMed] [Google Scholar]
- Meester LD. Learning anatomy for use beyond the classroom: a guide for medical students. McMaster University Medical Journal. 2011;8:45–48. [Google Scholar]
- National Research Council . BIO 2010, undergraduate education to prepare biomedical research scientists. Washington, DC: The National Academic Press; 2002. [Google Scholar]
- Noblitt L, Vance DE, DePoy-Smith ML. A comparison of case study and conventional teaching methods for improvement of oral communication and critical-thinking skills. J Coll Sci Teach. 2010;39:26–32. [Google Scholar]
- Pukkila PJ. Introducing student inquiry in large introductory genetics classes. Genetics. 2004;166:11–18. doi: 10.1534/genetics.166.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey P, Zimitat C. Medical students learning of anatomy: memorization, understanding and visualization. Med Educ. 2007;41:7–14. doi: 10.1111/j.1365-2929.2006.02643.x. [DOI] [PubMed] [Google Scholar]
- Quitadamo IJ, Kurtz MJ. Learning to improve: using writing to increase critical thinking performance in general education biology. CBE Life Sci Educ. 2007;6:140–154. doi: 10.1187/cbe.06-11-0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quitadamo IJ, Faiola CL, Johnson JE, Kurtz MJ. Community-based inquiry improves critical thinking in general education biology. CBE-LSE. 2008;7:327–337. doi: 10.1187/cbe.07-11-0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsden P. Learning to teach in higher education. London: Routledge Falmer; 2003. [Google Scholar]
- Russell SH, Hancock MP, McCullough J. Benefits of undergraduate research experiences. Science. 2007;316:548–549. doi: 10.1126/science.1140384. [DOI] [PubMed] [Google Scholar]
- Sclove RE. Putting science to work in communities. Chron High Educ. 1995;41:B1–B3. [Google Scholar]
- Springer L, Donovan SS, Stanne ME. Effects of small-group learning on undergraduates in science, mathematics, engineering, and technology: a meta-analysis. Rev Educ Res. 1999;69:21–51. [Google Scholar]
- Sundberg M, Moncada GJ. Creating effective investigative laboratories for undergraduates. Bioscience. 1994;44:698–704. [Google Scholar]
- Sundberg MD. Strategies to help students change naïve alternative conceptions about evolution and natural selection. Reports of the National Center for Science Education. 2003;23:23–26. [Google Scholar]
- Sundberg MD, Armstrong JE, Dini ML, Wischusen EW. Some practical tips for instituting investigative biology laboratories. J Coll Sci Teach. 2000;29:353–359. [Google Scholar]
- Svirko E, Mellanby J. Attitudes to e-learning, learning style, and achievement in learning neuroanatomy by medical students. Med Teach. 2008;30:219–227. doi: 10.1080/01421590802334275. [DOI] [PubMed] [Google Scholar]
- Terrell M. Anatomy of learning: instructional design principles for the anatomical sciences. Anat Rec B New Anat. 2006;289:252–260. doi: 10.1002/ar.b.20116. [DOI] [PubMed] [Google Scholar]
- Walton KLW. Use of case studies and data analysis to improve critical thinking skills in a one-semester anatomy and physiology course. FASEB J. 2008;22:767. 6. [Google Scholar]
- Ward PJ, Walker JJ. The influence of study methods and knowledge processing on academic success and long-term recall of anatomy learning by first-year veterinary students. Anat Sci Educ. 2008;1:68–74. doi: 10.1002/ase.12. [DOI] [PubMed] [Google Scholar]
- Weatherall DJ. Science in the undergraduate curriculum during the 20th century. Med Educ. 2006;40:195–201. doi: 10.1111/j.1365-2929.2006.02399.x. [DOI] [PubMed] [Google Scholar]
- Weimer M. Feedback forms for peer assessment in groups. Retrieved from Faculty Focus website. 2008. http://www.facultyfocus.com/articles/educational-assessment/feedback_form/.
- Woods NN, Neville AJ, Levinson AJ, Howey EH, Oczkowski WJ, Norman GR. The value of basic science in clinical diagnosis. Acad Med. 2006;81:S124–S127. doi: 10.1097/00001888-200610001-00031. [DOI] [PubMed] [Google Scholar]