Abstract
The main objective of this study was to compare the reporting of health status and symptom severity, for a set of core symptoms related to imatinib therapy, between chronic myeloid leukemia patients and their treating physicians. Patients were asked to complete a questionnaire including questions on symptom severity and health status. The symptoms assessed were: abdominal discomfort, diarrhea, edema, fatigue, headache, muscle cramps, musculoskeletal pain, nausea and skin problems. The physicians were asked to complete a questionnaire for each of their patients entering the study. Four hundred twenty-two patients were included in the study. All respective paired physicians (n=29) completed the questionnaire, and thus the analyses are based on 422 patient-physician dyads. Agreement on symptom ratings ranged from 34% (for muscle cramps) to 66% (for nausea). For all symptoms, patients reported higher severity more often than their physicians. The three symptoms whose severity was most frequently underestimated by physicians were fatigue (51%), muscle cramps (49%) and musculoskeletal pain (42%). Health status was overestimated by physicians in 67% of the cases. Physicians and their patients with chronic myeloid leukemia often disagree in their ratings of the patients’ symptom severity. Most typically, physicians tend to underestimate symptom severity and overestimate the overall health status of their patients. Current findings support the use of patient-reported outcome measures as a possible means to enhance the management of patients with chronic myeloid leukemia.
Introduction
The treatment of chronic myeloid leukemia (CML) has changed dramatically with the advent of molecularly targeted therapies (i.e., tyrosine kinase inhibitors).1 Imatinib was the first tyrosine kinase inhibitor approved by the United States Food and Drug Administration for the treatment of CML patients. It has provided major survival advantages compared to previous interferon-based therapies.2 While survival of patients who respond to imatinib is not different from that of the general population,3 it is important to consider that these patients require lifelong therapy that affects their health-related quality of life.4,5 The most frequently reported long-term adverse effects of imatinib therapy include edema, nausea, muscle cramps, and musculoskeletal pain.6
More recently, other so-called “second generation” tyrosine kinase inhibitors (i.e., dasatinib and nilotinib) have been approved for first-line use in CML patients, based on results from two large randomized trials.7,8 This makes the choice of tyrosine kinase inhibitor to be used as first-line therapy a major challenge. While imatinib, dastinib and nilotinib have different toxicity profiles,9 they have been reported to produce similar outcomes in terms of progression-free survival and overall survival at 24 months.10,11
It has, therefore, been suggested that, regardless of which drug is used as first-line therapy, timely management of side effects, changing the tyrosine kinase inhibitor when required, is a critical factor for optimal management of patients.9 In this scenario, close monitoring of burdensome symptoms experienced by patients is essential to facilitate a timely switch to other available tyrosine kinase inhibitors. Instrumental to the physician’s ability to consider alternative treatment strategies, however, is an accurate estimation of symptom severity and overall health status of their patients.
Data from studies conducted in malignant solid tumors have shown that physicians tend to rate symptoms as being less severe than do their patients.12–15 Also, patients’ self-reported symptoms have been shown to reflect daily health status better than do physician-reported symptoms.13 These types of findings formed the rationale for the National Cancer Institute-sponsored initiative to create a version of the Institute’s Common Terminology Criteria for Adverse Events (PRO-CTCAE) that can be completed by patients themselves, providing direct feedback from patients on their symptom experience during treatment.16 However, no study has investigated possible discrepancies between patient- and physician-reporting in the CML setting. Given the lifelong therapy needed for these patients, a possible mismatch in such reporting could have important clinical implications.
The main objective of this study was to compare the reporting of health status and symptom severity, for a set of core symptoms related to first-line imatinib therapy, between patients and their treating physicians. Secondary objectives were to investigate whether patient-reported or physician-reported symptoms better reflect patients’ overall health status, and to identify factors that may predict discrepancies between patients’ versus physicians’ ratings of symptom severity.
Methods
Study population and procedures
We approached consecutive CML patients as part of a larger project on cancer survivorship involving 26 Departments of Hematology.4 To avoid any risk of convergence in item ratings, the study was designed to avoid that patients and their treating physicians were aware of each other’s ratings. Physicians invited their patients to participate at the earliest follow-up visit following approval of the study in their center. The physicians were asked to complete a questionnaire for each of their patients entering the study. This was done as close in time as possible to the time that the patient was asked to complete his/her questionnaire. The study was approved by all Ethic Committees of each participating center and all patients provided written informed consent.
Data collection and variables examined
The questionnaire administered to patients and physicians included a checklist of nine core symptoms: abdominal discomfort, diarrhea, edema, fatigue, headache, muscle cramps, musculoskeletal pain, nausea and skin problems.17 Symptom severity was rated as: “not at all”, “a little”, “quite a bit” and “very much”. Respondents were also asked to complete a single question on overall health status from the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36):18 “In general would you say your health is¿” with the response options: “excellent”, “very good”, “good”, “fair” and “poor”. This question was included because it has been shown to be a valid measure of self-rated overall health.19
Additional patients’ variables collected included age, gender, dose of imatinib, and duration of care by the participating physician. Additional physicians’ variables included age, gender, number of CML patients under direct management, overall number of years in practice and years of experience in treating CML patients, and how long each of their patients in the study had been under their management (i.e., 1, 2, 3 or more than 3 years). The date of questionnaire completion by both the patients and physicians was also recorded.
Statistical analysis
We computed differences in ratings for each symptom scale previously described and the overall health status as measured by the SF-36 questionnaire. Differences ranged from −3 to +3 and −4 to +4 for symptoms and overall health status ratings, respectively, with a negative, null or positive value representing physicians’ underestimation, agreement or overestimation of the patients’ rating. For descriptive purposes, we grouped such differences in five classes,14 representing proportions of agreement (difference=0) and either minor or major disagreement (difference =|1| and ≥|2|, respectively). We also investigated the association between patient-rated and physician-rated symptoms and overall health status (patient-reported) by Kendall τb. Furthermore, we used a multilevel logistic regression analysis to investigate potential patient-related and physician-related predictors of physicians’ underestimation of patients’ symptom (α=0.05). The multilevel approach was chosen to account for the clustered nature of the data (i.e., each physician could evaluate more than one patient).20 We applied Bonferroni correction to adjust for multiple testing. All analyses were performed with SAS Version 9.2 (SAS Institute Inc).
Further details on the Methods of this study and a list of collaborators and participating centers are available in the Online Supplementary Appendix.
Results
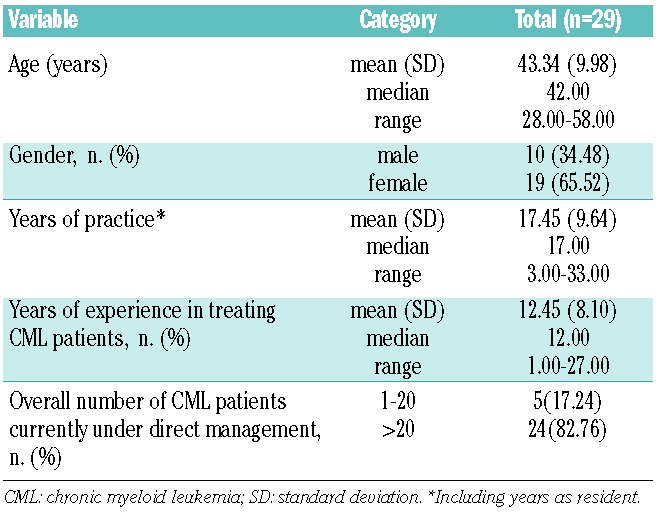
Four hundred twenty-two patients returned the questionnaire to the GIMEMA Data Center, out of the 448 who consented to participate. Socio-demographic and clinical characteristics of the sample have been reported previously.4 Briefly, the median age of the patients was 57 years (range, 19 to 87 years) and 91% of them started with imatinib at a standard dose of 400 mg/day. The median time in treatment with imatinib was 5 years (range, 3 to 9 years). All respective paired physicians (n=29) completed the questionnaire, and thus the analyses are based on 422 patient-physician dyads. Eighty-four percent of patients were in treatment with the same physician for 3 or more years. Additional physicians’ characteristics are reported in Table 1.
Table 1.
Physicians’ characteristics.
Symptoms and overall health status: patients’ versus physicians’ ratings
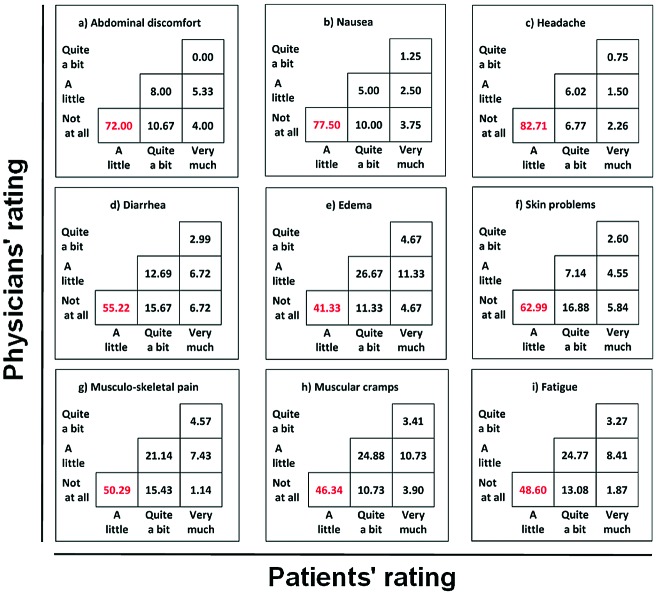
Agreement on symptom ratings ranged from 34% (for muscle cramps) to 66% (for nausea). For all symptoms, patients reported higher severity more often than their physicians. The three symptoms whose severity was most frequently underestimated by physicians were fatigue (51%), muscle cramps (49%) and musculoskeletal pain (42%). The majority of discrepancies were within one point (i.e., minor disagreement). For edema, skin problems, musculoskeletal pain, muscle cramps and fatigue, differences of two points (i.e., major disagreement) were also noted in at least 10% of evaluations.
Agreement on overall health status rating was observed in 26% of cases. However, health status was overestimated by physicians in 67% of the cases (Figure 1).
Figure 1.
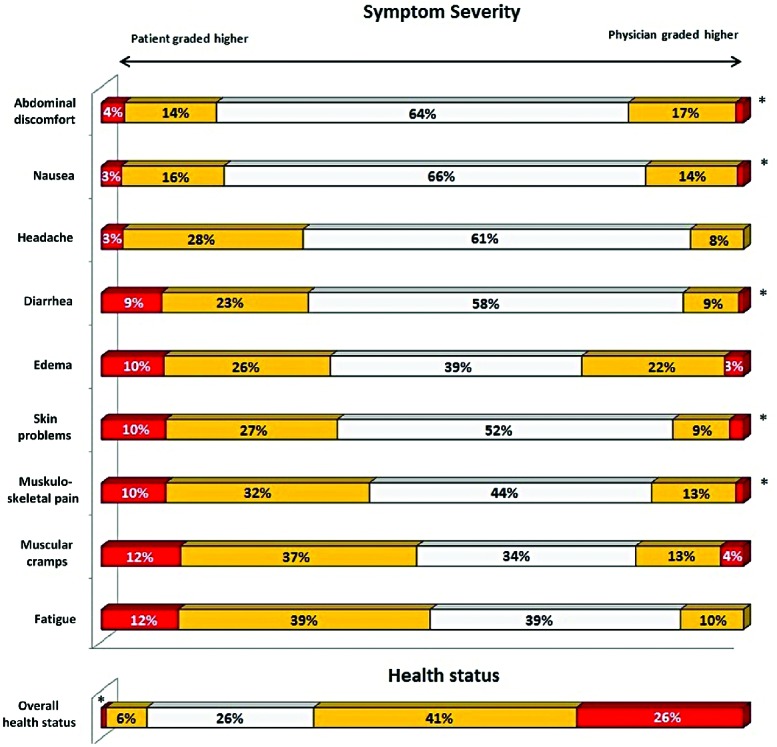
Agreement and disagreement between patients and physicians on symptoms and health status. The respondents were asked to report the severity of each symptom with the following possible answers: “not at all”, “a little”, quite a bit” and “very much”. Possible answers to the question on overall health status were: “excellent”, “very good”, “good”, “fair” and “poor “
We also calculated the absolute number of discrepant symptom ratings. Three or more discrepancies in symptom ratings were observed in more than 80% of the paired evaluations.
The pattern of physicians’ underestimation of symptom severity is shown in Figure 2. When physicians underestimated symptom severity, this was most frequently the case at the lower end of symptom severity. In the majority of cases, physicians rated the symptom as not being present while patients rated the same symptom as being of mild intensity (i.e., a little).
Figure 2.
Physicians’ underestimation by symptom severity. For each symptom, the table shows the distribution of physicians’ underestimation by each permissible pair of scores. Each cell shows the joint frequency of physicians’ score (vertical ratings) versus patients’ score (horizontal ratings). The levels of underestimation are represented on the diagonals from left to right. For example, the main diagonal represents the possible pairs of the smallest score difference (−1).
Association between symptom burden and overall health status based on patient-reported versus physician-reported symptoms
The correlation between symptom burden and overall health status was higher when based on patient-reported rather than physician-reported symptoms. Fatigue was the symptom most correlated with overall health status for both patients and physicians. However, the strength of association between fatigue and health status was greater for patients’ reports (Kendall τb =0.43; 95% CI = 0.354 to 0.500), compared to physicians’ reports (Kendall τb =0.27; 95% CI= 0.186 to 0.348). Figure 3 depicts the strength of these associations.
Figure 3.
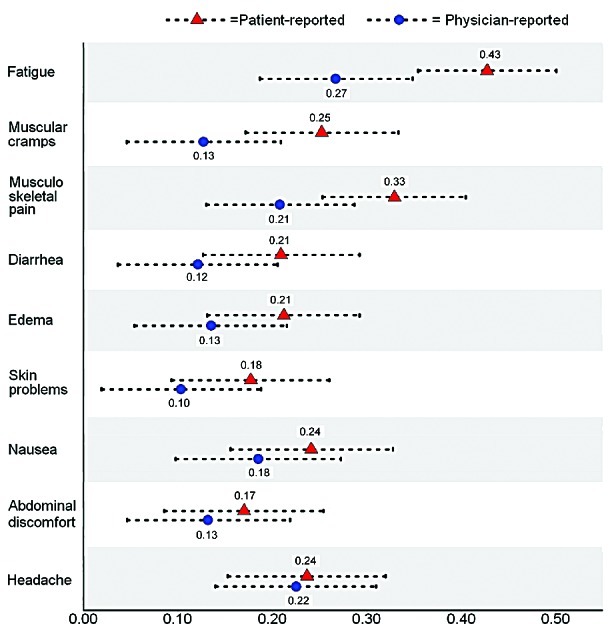
Strength of association between patient-reported versus physician-reported symptoms and health status. The figure shows Kendall’s τ-b correlation coefficients of patient-reported overall health status with patients’ symptoms, reported either by themselves or their physician (dotted lines= 95% confidence intervals). The higher the coefficient, the stronger the relationship between overall health status and the corresponding symptom.
Factors predicting physicians’ underestimation of symptom severity
No statistically significant associations were found between physicians’ characteristics (i.e., gender, years of experience in treating CML patients and number of patients under direct management) or patients’ characteristics (i.e., gender, age, current imatinib dose) and physicians’ underestimation of their patients’ symptom severity. Similarly, the timing of questionnaire completion (i.e., time elapsed between the physician and the patient completing the questionnaire) and the duration of care by the corresponding physician were not associated significantly with the probability of underestimating symptom burden (data not shown in tabular form).
Discussion
The main finding of this study is that physicians and their CML patients often disagree in their ratings of the patients’ symptom severity. Our data also indicate that, most typically, physicians tend to underestimate symptom severity and overestimate the overall health status of their patients.
The symptom most frequently underestimated by physicians in our study was fatigue. This is in line with what has been observed in similar studies conducted on patients with solid tumors receiving conventional chemotherapies.14 It was previously reported that fatigue is the main factor impairing the health-related quality of life of CML patients21 and thus, failure to recognize its severity can have important clinical implications. Guidelines suggesting strategies to manage fatigue in patients receiving active treatments are available and these can be of help to physicians treating CML patients.22
Our findings are all the more striking in that the large majority of patients (more than 80%) had been managed by the same physician for at least 3 years, and were typically attending regular follow-up visits on a monthly basis.
A more detailed analysis of the pattern of discrepancies, when physicians’ underestimated their patients’ symptom severity, revealed that these were most commonly at the low end of the symptom scale. In the majority of cases, physicians evaluated the symptom as not being present whereas their patients rated the symptom as being of mild intensity. Although one might be tempted to argue that such discrepancies in ratings at the lower end of symptom severity are less important, earlier work has shown that even relatively mild symptoms can have a considerable impact on the health-related quality of life of CML patients, given the lifelong nature of the therapy.21,23 Also, physicians’ failure to note the presence of mild symptoms can have major clinical implications. For example, it could lead to underestimation of the risk that patients will (temporarily) discontinue treatment due to the side effects. Full adherence to therapy is crucial to maximize clinical response to imatinib therapy24,25 and recognizing the presence of low-grade side effects is critical for optimal management of patients. Previous studies have, in fact, suggested that avoiding unpleasant side effects is the main cause of intentional non-adherence in CML.26
Although we attempted to identify factors that could predict physicians’ underestimation of their patients’ symptoms, no patient-related or physician-related variables were found to be statistically significant in our multivariate model. This is consistent with previous studies conducted in other malignancies,14 and future work is needed to identify factors that can predict such discrepancies in symptom ratings.
Current findings suggest that the routine collection of patient-reported symptom data in daily clinical practice may facilitate greater awareness in physicians of their patients’ symptom burden, which in turn may enhance the management of patients with CML. For example, it might contribute to better treatment choices when considering timely switching to another tyrosine kinase inhibitor. A number of controlled clinical trials have demonstrated that providing physicians (and nurses) with summaries of patient-reported symptom and health-related quality of life information can enhance communication and timely recognition of problems.27–29 At the very least, patients’ self-reports should be used to complement information derived from current standard physician-reporting of toxicity and improve accurate identification of patients who are truly intolerant to therapy. To this end, two patient-reported outcome measures specifically devised for CML patients have just been published: the MD Anderson Symptom Inventory (MDASI)-CML30 and the European Organization for Research and Treatment of Cancer (EORTC) QLQ-CML24.31 Implementation of these standard questionnaires in clinical research and practice could enhance physicians’ ability to capture the burden of the disease and treatment from the unique patient’s perspective.
Our study has limitations. Although being a large multicenter study, it was conducted in a single country. Also, the cross-sectional design did not allow investigation of a possible effect of repeated measures on the agreement between the ratings of patients and their physicians. Thus replication of our results in longitudinal, multinational studies would give more support to the generalizability of the current findings. Finally, our results can only be generalized to patients receiving imatinib. Although there is no reason to believe that the results would be different for patients receiving other tyrosine kinase inhibitors, this needs to be confirmed empirically.
This study also has a number of strengths. It is based on a large sample of patients recruited in an observational setting, and the participation rate of both patients and physicians was very high. Thus we are confident that our results are generalizable to the larger population of CML patients currently treated in daily clinical practice. Also, given the design of the study, patients and physicians were not aware of each other’s ratings, thus the risk of artificially inflated agreement levels was minimized.
In conclusion, our results indicate that physicians tend to underestimate the severity of long-term side effects of imatinib therapy. We would recommend introducing patient-reported symptom assessment into clinical practice as a means of improving physicians’ awareness of their patients’ symptom burden, and facilitating timely changes in treatment and management of the patients, if necessary.
Acknowledgment
We are very grateful to all patients who participated in this study and we acknowledge the essential contribution of the “Associazione Italiana contro le Leucemie, Linfomi e Mieloma (AIL)” which provided logistic and administrative support for this project.
Footnotes
The online version of this article has a Supplementary Appendix.
Funding
This study was supported by the “Associazione Italiana contro le Leucemie, Linfomi e Mieloma (AIL)” and in part by Novartis. Novartis had no role in the design or conduct of the study; collection, management, analysis or interpretation of data; or preparation, review, or approval of the manuscript.
Authorship and Disclosures
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Kris MG, Benowitz SI, Adams S, Diller L, Ganz P, Kahlenberg MS, et al. Clinical cancer advances 2010: annual report on progress against cancer from the American Society of Clinical Oncology. J Clin Oncol. 2010;28(36):5327–47 [DOI] [PubMed] [Google Scholar]
- 2.O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F, et al. Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2003;348(11):994–1004 [DOI] [PubMed] [Google Scholar]
- 3.Gambacorti-Passerini C, Antolini L, Mahon F-X, Guilhot F, Deininger M, Fava C, et al. Multicenter independent assessment of outcomes in chronic myeloid leukemia patients treated with imatinib. J Natl Cancer Inst. 2011;103(7):553–61 [DOI] [PubMed] [Google Scholar]
- 4.Efficace F, Baccarani M, Breccia M, Alimena G, Rosti G, Cottone F, et al. Health-related quality of life in chronic myeloid leukemia patients receiving long-term therapy with imatinib compared with the general population. Blood. 2011;118(17):4554–60 [DOI] [PubMed] [Google Scholar]
- 5.Phillips KM, Pinilla-Ibarz J, Sotomayor E, Lee MR, Jim HS, Small BJ, et al. Quality of life outcomes in patients with chronic myeloid leukemia treated with tyrosine kinase inhibitors: a controlled comparison. Support Care Cancer. 2013;21(4):1097–103 [DOI] [PubMed] [Google Scholar]
- 6.Druker BJ, Guilhot F, O’Brien SG, Gathmann I, Kantarjian H, Gattermann N, et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006;355(23):2408–17 [DOI] [PubMed] [Google Scholar]
- 7.Saglio G, Kim DW, Issaragrisil S, le Coutre P, Etienne G, Lobo C, et al. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med. 2010;362(24):2251–9 [DOI] [PubMed] [Google Scholar]
- 8.Kantarjian H, Shah NP, Hochhaus A, Cortes J, Shah S, Ayala M, et al. Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2010;362(24):2260–70 [DOI] [PubMed] [Google Scholar]
- 9.Marin D. Initial choice of therapy among plenty for newly diagnosed chronic myeloid leukemia. Hematology Am Soc Hematol Educ Program. 2012:115–21 [DOI] [PubMed] [Google Scholar]
- 10.Kantarjian HM, Hochhaus A, Saglio G, De Souza C, Flinn IW, Stenke L, et al. Nilotinib versus imatinib for the treatment of patients with newly diagnosed chronic phase, Philadelphia chromosome-positive, chronic myeloid leukaemia: 24-month minimum follow-up of the phase 3 randomised ENESTnd trial. Lancet Oncol. 2011;12(9):841–51 [DOI] [PubMed] [Google Scholar]; Erratum in:; Lancet Oncol. 2011;12(11):989 [Google Scholar]
- 11.Kantarjian HM, Shah NP, Cortes JE, Baccarani M, Agarwal MB, Undurraga MS, et al. Dasatinib or imatinib in newly diagnosed chronic-phase chronic myeloid leukemia: 2-year follow-up from a randomized phase 3 trial (DASISION). Blood. 2012;119(5):1123–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fromme EK, Eilers KM, Mori M, Hsieh YC, Beer TM. How accurate is clinician reporting of chemotherapy adverse effects? A comparison with patient-reported symptoms from the Quality-of-Life Questionnaire C30. J Clin Oncol. 2004;22(17):3485–90 [DOI] [PubMed] [Google Scholar]
- 13.Basch E, Jia X, Heller G, Barz A, Sit L, Fruscione M, et al. Adverse symptom event reporting by patients vs clinicians: relationships with clinical outcomes. J Natl Cancer Inst. 2009;101(23):1624–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Basch E, Iasonos A, McDonough T, Barz A, Culkin A, Kris MG, et al. Patient versus clinician symptom reporting using the National Cancer Institute Common Terminology Criteria for Adverse Events: results of a questionnaire-based study. Lancet Oncol. 2006;7(11):903–9 [DOI] [PubMed] [Google Scholar]
- 15.Basch E. The missing voice of patients in drug-safety reporting. N Engl J Med. 2010;362(10):865–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Cancer Institute U.S. Department of Health and Human Services. Division of Cancer Control and Population Sciences, Patient-Reported Outcomes Version of the Common Terminology Criteria for Adverse Events (PRO-CTCAE). http://outcomes.cancer.gov/tools/pro-ctcae_fact_sheet.pdf (accessed may 28, 2012).
- 17.Efficace F, Breccia M, Baccarani M, Alimena G, Lambertenghi Deliliers G, Specchia G, et al. Development and feasibility of a patient-reported symptom checklist for chronic myeloid leukemia patients [abstract]. Haematologica 2010;95(Suppl 2):S189 [Google Scholar]
- 18.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83 [PubMed] [Google Scholar]
- 19.Bjorner J, Fayers P, Idler E. Self-rated Health, in Assessing Quality of Life in Clinical Trials. 2nd ed. Fayers P, Hays R, editors. New York: Oxford University Press; 2005. p. 309–23 [Google Scholar]
- 20.Suarez-Almazor ME, Conner-Spady B, Kendall CJ, Russell AS, Skeith K. Lack of congruence in the ratings of patients’ health status by patients and their physicians. Med Decis Making. 2001;21(2):113–21 [DOI] [PubMed] [Google Scholar]
- 21.Efficace F, Baccarani M, Breccia M, Cottone F, Alimena G, Lambertenghi Deliliers G, et al. Chronic fatigue is the most important factor limiting health-related quality of life of chronic myeloid leukemia patients treated with imatinib. Leukemia. 2013;27(7):1511–9 [DOI] [PubMed] [Google Scholar]
- 22.National Comprehensive Cancer Network (NCCN) Practice Guidelines in Oncology. Cancer-related fatigue. V.1.2013. [Google Scholar]
- 23.Pinilla-Ibarz J, Cortes J, Mauro MJ. Intolerance to tyrosine kinase inhibitors in chronic myeloid leukemia: definitions and clinical implications. Cancer. 2011;117(4):688–97 [DOI] [PubMed] [Google Scholar]
- 24.Marin D, Bazeos A, Mahon FX, Eliasson L, Milojkovic D, Bua M, et al. Adherence is the critical factor for achieving molecular responses in patients with chronic myeloid leukemia who achieve complete cytogenetic responses on imatinib. J Clin Oncol. 2010;28(14):2381–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Noens L, van Lierde MA, De Bock R, Verhoef G, Zachée P, Berneman Z, et al. Prevalence, determinants, and outcomes of nonadherence to imatinib therapy in patients with chronic myeloid leukemia: the ADAGIO study. Blood. 2009;113(22):5401–11 [DOI] [PubMed] [Google Scholar]
- 26.Eliasson L, Clifford S, Barber N, Marin D. Exploring chronic myeloid leukemia patients’ reasons for not adhering to the oral anticancer drug imatinib as prescribed. Leuk Res. 2011;35(5):626–30 [DOI] [PubMed] [Google Scholar]
- 27.Velikova G, Booth L, Smith AB, Brown PM, Lynch P, Brown JM, et al. Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol. 2004;22(4):714–24 [DOI] [PubMed] [Google Scholar]
- 28.Detmar SB, Muller MJ, Schornagel JH, Wever LD, Aaronson NK. Health-related quality-of-life assessments and patient-physician communication: a randomized controlled trial. JAMA. 2002;288(23):3027–34 [DOI] [PubMed] [Google Scholar]
- 29.Hilarius DL, Kloeg PH, Gundy CM, Aaronson NK. Use of health-related quality-of-life assessments in daily clinical oncology nursing practice: a community hospital-based intervention study. Cancer. 2008;113(3):628–37 [DOI] [PubMed] [Google Scholar]
- 30.Williams LA, Gonzalez AG, Ault P, Mendoza TR, Sailors ML, Williams JL, et al. Measuring the symptom burden associated with the treatment of chronic myeloid leukemia. Blood. 2013;122(5):641–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Efficace F, Baccarani M, Breccia M, Saussele S, Abel G, Caocci G, et al. International development of an EORTC questionnaire for assessing health-related quality of life in chronic myeloid leukemia patients: the EORTC QLQ-CML24. Qual Life Res. 2013. September 13 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]