Abstract
Background
Revision THAs are expected to increase; however, few studies have characterized the prognosis of revision THAs in younger patients.
Questions/purposes
We performed a case-control study to evaluate intermediate-term survivorship, complications, and hip and activity scores after revision THAs in patients 55 years and younger, compared these outcomes with the results of primary THAs in a matched patient population, and evaluated risk factors for failed revisions.
Methods
Ninety-three patients (103 hips) had a minimum of 4 years after revision THA, died, or had rerevision surgery. They were matched with 98 patients (103 hips) with primary THAs. Survivorship, complications, and clinical outcomes were compared between the groups using t-tests. Risk factors for failure also were assessed with chi-square analysis.
Results
At mean followup of 6.7 years, 71 revision THAs (69%) survived, compared with 102 (99%) primary THAs (odds ratio [OR], 45.9; 95% CI, 16.5–128.4; p < 0.001). Complications occurred in 29% of the revision group and 6% of the primary group (OR, 6.64; 95% CI, 4.14–10.67; p < 0.001). After revision THA, the average improvement in Harris hip score was 19.2 compared with 34.4 after primary THA (p < 0.001). The UCLA activity score improved by an average of 0.87 after revision compared with 2.36 after primary THA (p < 0.001). Conventional polyethylene was associated with failure after revision THA (OR, 2.98; 95% CI, 1.87–4.76; p = 0.004).
Conclusions
At intermediate-term followup, young patients undergoing revision THAs had markedly higher failure and complication rates and more modest clinical improvements compared with patients in a matched cohort who had primary THAs.
Level of Evidence
Level III, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
THA has been highly effective in the treatment of end-stage osteoarthritis. Its use, particularly among younger patients, has increased substantially and is expected to continue to increase [5, 13, 14]. Additionally, the prevalence of revision THAs is expected to increase. Younger age at the time of the primary THA has been shown to increase the risk of revision [4, 12, 18]. Projections suggest that revision procedures will more than double between 2005 and 2030 [4].
Previous studies have reported outcomes of revision THA [2, 7, 8], and historically, these outcomes have been limited in young patients [11, 15, 16]. There have been high rates of mechanical loosening and revision rates have ranged from 10% to 20% [11, 15, 16]. However, these reports are outdated. They focus predominantly on early-generation cemented implants, with a paucity of information regarding the outcome of contemporary procedures [11, 15, 16]. Specifically, the literature is lacking studies dedicated to characterizing the function and survivorship of revision hip arthroplasties with modern cementless implants in young patients.
We therefore evaluated intermediate-term survivorship, complications, and hip and activity scores, after revision THAs in patients 55 years and younger, compared these outcomes with the results of primary THAs in a matched patient population, and evaluated risk factors for failed revisions.
Patients and Methods
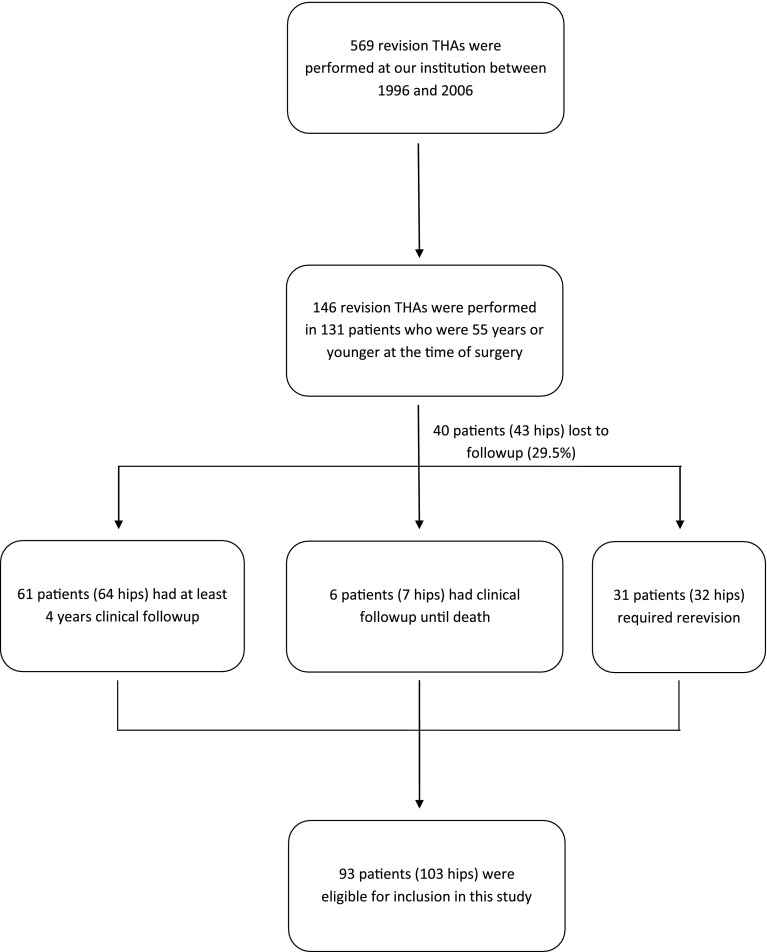
We performed a case control study in which survivorship, complication rate, Harris hip score, and UCLA activity score in patients aged 55 years or younger who had revision THAs were compared with a matched cohort of patients 55 years or younger who had primary THAs. After approval by our institutional review board, we identified patients 55 years or younger who underwent revision THAs at our institution between 1996 and 2006 through our institution’s joint arthroplasty registry. Revision THA was defined as the exchange of one or more components of an existing THA. Hips that were revised for infection, failed hemiarthroplasty, failed hemiresurfacing arthroplasty, and failed surface replacement arthroplasty were excluded. Patients were followed for a minimum of 4 years or until rerevision or death. Ninety-three patients (103 hips) of the 146 who were 55 years or younger, had at least 4 years clinical followup, had rerevisions, or died (70.5%) (Fig. 1). Forty patients (43 hips) were lost to followup (29.5%).
Fig. 1.
The flow chart shows the identification of eligible patients for this study.
We reviewed operative reports for surgical details, including type of revision performed, surgical approach, implant information, and polyethylene liner type. Clinical charts were examined for demographic information, primary hip disease, BMI, medical comorbidities, previous hip surgeries, reason for revision, incidence of postoperative complications, or need for additional surgery. Complications included infection, wound complications, periprosthetic fracture, dislocation, recurrent instability, or venous thromboembolism (deep vein thrombosis or pulmonary embolus). Further revisions of any type, including resection arthroplasty, were considered failures.
Overall, there were 61 women and 32 men (Table 1). The average age of these patients at the time of revision was 45.2 years (range, 22–55 years). Their average BMI was 28.8 kg/m2 (range, 17.7–54.7 kg/m2). Thirty-one percent of the patients had a BMI greater than 30 kg/m2. Sixteen patients (17%) had systemic lupus erythematosus, nine (10%) had rheumatoid arthritis, four (4%) had end-stage renal disease, two (2%) had sickle cell anemia, and one (1%) had HIV. These patients had an average of 1.5 previous hip surgeries (range, 1–5). Seventeen hips (17%) had previous revisions. The most common preoperative diagnosis was aseptic loosening (57 hips, 55%) (Table 2). All revisions were performed through a posterior approach. Most were acetabular revisions alone (41 hips, 40%). Thirty-two percent (33 hips) were head and liner exchanges. Femoral revisions alone were done in 18 hips (18%), and complete acetabular and femoral revisions were done in 11 hips (11%). All acetabular revisions used cementless fixation and were fixed with an average of three screws (range, 1–7 screws)). Trabecular metal acetabular components were used in 25 acetabular revisions (61%) (Table 3). Cementless femoral components were used in 27 of 29 femoral revisions (93%), which were all fully porous coated. Femoral heads and polyethylene liners were exchanged in every revision. The median head size was 32 mm (range, 22–40 mm). Highly cross-linked polyethylene was used at the time of revision in 67 hips (65%). Postoperatively, all patients were prescribed posterior hip precautions for 3 months. Abduction bracing was used at the discretion of the operating surgeon.
Table 1.
Comparison of revision and primary THA groups
| Parameter | Revision THA 93 patients (103 hips) | Primary THA 98 patients (103 hips) | p value |
|---|---|---|---|
| Average age | 45.2 years | 44.3 years | 0.41 |
| Average followup | 6.7 years | 6.6 years | 0.99 |
| Average BMI | 28.8 | 28.5 | 0.72 |
| Comorbidities | |||
| Lupus | 17% | 14% | 0.58 |
| Rheumatoid arthritis | 10% | 7% | 0.53 |
| End-stage renal disease | 4% | 6% | 0.57 |
| Sickle cell anemia | 2% | 2% | 0.96 |
| HIV/AIDS | 1% | 1% | 0.97 |
| % Highly cross-linked polyethylene (overall) | 65% | 68% | 0.66 |
| Mean improvement in scores | |||
| Harris hip score | Pain 12.6 | Pain 18.7 | 0.01 |
| Total 19.2 | Total 34.4 | < 0.001 | |
| UCLA activity score | 0.87 | 2.36 | < 0.001 |
| Overall complication rate | 29% | 6% | < 0.001 |
| Rate of instability | 15% | 3% | 0.002 |
| Survivorship | 69% | 99% | < 0.001 |
Table 2.
Reasons for revision surgery in the revision group
| Reason for revision | % of hips |
|---|---|
| Aseptic loosening | 55 |
| Osteolysis with well-fixed implants | 29 |
| Instability | 7 |
| Component failure, including fractured stem, liner dissociation | 4 |
| Other | 5 |
Table 3.
Components in revision THAs
| Components | Number of hips |
|---|---|
| Acetabular components | |
| Zimmer Trilogy® | 36 |
| Zimmer Trabecular MetalTM | 35 |
| Smith & Nephew ReflectionTM | 4 |
| (Smith & Nephew) Richards Contour Cage† | 2 |
| Howmedica Osteonics RestorationTM Gap Reinforcement Ring | 2 |
| Howmedica Osteonics | 1 |
| DePuy Protrusio Cage | 1 |
| Femoral components | |
| DePuy Solution System® | 15 |
| Zimmer VerSys® Beaded Fullcoat | 13 |
| Zimmer ZMR® | 3 |
| Smith & Nephew EchelonTM | 3 |
| Smith & Nephew SpectronTM | 1 |
| DePuy S-ROM® | 1 |
| Stryker GMRSTM Global Modular Replacement System | 1 |
| Howmedica Osteonics RestorationTM | 1 |
| DePuy Prodigy® | 1 |
| Zimmer VerSys® Heritage® | 1 |
| Unknown existing stem reimplanted | 2 |
| % highly cross-linked polyethylene | 65% |
* Zimmer Inc., Warsaw, IN, USA; †Smith & Nephew Inc, Andover, MA, USA; ‡Stryker Howmedica Osteonics, Rutherford, NJ, USA; §DePuy Orthopaedics Inc, Warsaw, IN, USA.
A separate query of our institution’s joint arthroplasty registry was performed to identify a control group of patients who underwent primary THAs (Table 1). There were 98 patients (103 hips) who 55 years or younger and followed for at least 4 years or until revision surgery. We reviewed the medical records for these patients in a manner similar to that described above. Patients who had primary THAs then were matched to patients who had revision surgery based on age, sex, BMI, primary hip disease, Charnley classification, and pertinent medical comorbidities. More specifically, age was matched within 5 years, sex was matched exactly, and BMI was matched within 5 kg/m2. Patients also were matched according to their primary hip diagnosis (ie, osteoarthritis, inflammatory arthritis, osteonecrosis, etc), Charnley classification, and the presence of one or more of the following comorbid conditions: sickle cell anemia, rheumatoid arthritis (including juvenile rheumatoid arthritis), systemic lupus erythematosus, end-stage renal disease, or HIV/AIDS. Of the 307 patients (354 primary THAs) meeting the matching criteria, 305 patients (346 hips) had at least 4 years clinical followup (97.7%). Eight hips were lost to followup (3.2%), which was significantly less than the loss to followup for the revision group (p < 0.001). One of the authors (MAA) who was not involved in the care of the patients performed this matching process in blinded fashion with respect to clinical outcomes. Eligible control patients were listed alphabetically using Microsoft Excel (Microsoft Inc, Redmond, WA, USA). The patients were reviewed consecutively, and the first patient encountered who could be matched to each revision patient according to the previously described criteria was selected.
Clinical outcomes were measured using the Harris hip score and UCLA activity score. These scores were obtained preoperatively and at final followup. Patients either presented to our clinic for routine evaluation or were contacted by mail or telephone for updates on their clinical status. Followup was completed predominantly in person (94.7%). Correspondence by telephone or mail was used to obtain followup for 5.3% of patients. Patient outcomes were evaluated by changes in the Harris hip score and UCLA activity score. Postoperative changes in these scores were calculated for each patient, and the average change in each group was determined.
Survivorship was calculated as the percentage of hips without reoperation for any reason at the time of final followup. A two-tailed t-test was used to assess differences in age, followup duration, and improvement in Harris hip score and UCLA activity score between the primary and revision groups. Chi-square analysis was used to evaluate differences in complications, instability, and rerevision between the two groups. Additionally, potential for type of revision, history of previous revision, total number of previous hip surgeries, and presence of comorbidities as risk factors for failure in the revision group were assessed using the chi-square test.
Results
Survivorship was markedly lower in the revision THA than in the matched primary THA group. Of the 103 revision hips in the study group, 71 hips (69%) survived an average of 6.7 years (range, 2–13 years). The most common reason for failure was aseptic loosening (12 hips, 38%). Thirty-four percent of all failures (11 hips) were rerevised for the same diagnosis as the initial revision (Table 4). In contrast, survivorship was 99% among matched primary THAs (odds ratio (OR), 45.97; 95% CI, 16.46–128.41; p < 0.001), with the sole failure being attributable to instability
Table 4.
Data for patients with failed revision THAs
| Patient number | Age (years) | Gender | Comorbidities | Preoperative diagnosis | Type of revision | Highly cross-linked polyethylene? | Reason for failure | Time after revision (months) | Type of rerevision |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 45 | M | None | Instability | Head/liner exchange | Yes | Instability | 110 | Acetabular and femoral |
| 2 | 46 | F | None | Loosening | Acetabular and femoral | Yes | Loosening | 54 | Acetabular |
| 3 | 23 | F | Sickle cell anemia | Loosening | Acetabular | No | Infection | 23 | Explant |
| 4 | 25 | M | None | Osteolysis | Head/liner exchange | No | Loosening | 76 | Acetabular |
| 5 | 47 | F | Systemic lupus erythematosus | Osteolysis | Acetabular | Yes | Loosening | 12 | Acetabular |
| 6 | 47 | F | Systemic lupus erythematosus | Loosening | Femoral | Yes | Loosening | 98 | Acetabular |
| 7 | 22 | F | None | Osteolysis | Head/liner exchange | No | Instability | 1 | Head/liner exchange |
| 8 | 53 | F | None | Instability | Head/liner exchange | Yes | Instability | 17 | Acetabular |
| 9 | 53 | F | Systemic lupus erythematosus | Liner Dissociation | Head/liner exchange | No | Instability | 1 | Acetabular |
| 10 | 23 | F | Juvenile Rheumatoid Arthritis | Osteolysis | Head/liner exchange | No | Liner Dissociation | 58 | Head/liner exchange |
| 11 | 53 | F | None | Liner Dissociation | Head/liner exchange | No | Loosening | 114 | Acetabular |
| 12 | 31 | F | None | Instability | Head/liner exchange | No | Gluteus medius tendon tear | 56 | Head/liner exchange |
| 13 | 45 | F | Systemic lupus erythematosus | Loosening | Acetabular | Yes | Instability | 1 | Head/liner exchange |
| 14 | 43 | F | None | Loosening | Femoral | No | Osteolysis | 110 | Head/liner exchange |
| 15 | 44 | F | None | Loosening | Femoral | No | Osteolysis | 169 | Head/liner exchange |
| 16 | 49 | M | None | Loosening | Femoral | No | Loosening | 156 | Femoral |
| 17 | 46 | F | Rheumatoid Arthritis | Loosening | Acetabular | No | Infection | 81 | Explant |
| 18 | 46 | F | Systemic lupus erythematosus, renal failure | Wear | Head/liner exchange | Yes | Fractured Liner | 22 | Acetabular |
| 19 | 54 | F | Rheumatoid Arthritis | Instability | Acetabular | Yes | Instability | 9 | Head/liner exchange |
| 20 | 42 | F | None | Osteolysis | Acetabular | Yes | Loosening | 10 | Acetabular |
| 21 | 44 | F | Systemic lupus erythematosus | Osteolysis | Head/liner exchange | No | Instability | 13 | Acetabular |
| 22 | 49 | F | Systemic lupus erythematosus | Loosening | Acetabular and femoral | Yes | Instability | 41 | Acetabular |
| 23 | 44 | M | None | Loosening | Femoral | No | Infection | 40 | Explant |
| 24 | 52 | F | Systemic lupus erythematosus | Leg length discrepancy | Head/liner exchange | No | Instability | 69 | Acetabular |
| 25 | 50 | M | None | Loosening | Acetabular | Yes | Loosening | 22 | Acetabular |
| 26 | 54 | F | None | Osteolysis | Head/liner exchange | No | Osteolysis | 88 | Acetabular |
| 27 | 48 | F | Rheumatoid arthritis | Fractured stem | Femoral | Wear | 97 | Head/liner exchange | |
| 28 | 44 | F | None | Loosening | Acetabular | Yes | Instability | 9 | Head/liner exchange |
| 29 | 34 | F | None | Loosening | Acetabular | Yes | Loosening | 132 | Acetabular |
| 30 | 40 | M | None | Loosening | Acetabular | Yes | Loosening | 11 | Acetabular |
| 31 | 51 | F | None | Loosening | Acetabular | Yes | Loosening | 92 | Femoral |
| 32 | 37 | M | None | Osteolysis | Head/liner exchange | No | Loosening | 61 | Acetabular |
Complications were more frequent in the revision THA group than in the matched primary THA group. Overall, 30 complications (29%) occurred in the 103 hips in the revision group. One or more dislocations occurred in 15% (16 hips). Six percent of primary THAs (6 hips) had complications (OR, 6.64; 95% CI, 4.14–10.67; p < 0.001), including 3% with instability (OR, 5.68; 95% CI, 2.97–10.87; p = 0.002).
Hip and activity scores improved more in the primary THA group than in the revision THA group. The average change in Harris hip score after revision was 19.2 (range, −40 to 60). The Harris hip pain subscore had a mean improvement of 12.6 (range, −20 to 44). The UCLA activity score improved by 0.87 (range, −6 to 8). Matched primary THAs, at mean followup of 6.6 years (range, 4–13 years), had an average improvement of 34.4 in the Harris hip score (range, −19 to 83), which was greater than the improvement after revision (p < 0.001). Mean improvement of the Harris hip pain subscore was 18.7 (range, −20 to 44), which also was significantly greater than the change after revision (p = 0.01). The UCLA activity score also improved more after primary THA (mean, 2.36; range, −2 to 8) than after revision (p < 0.001).
Use of conventional polyethylene at the time of revision was associated with failure (OR 2.98; 95% CI, 1.86–4.76; p = 0.004). However, type of revision (p = 0.48), head size less than 32 mm (p = 0.39), history of previous revision (p = 0.12), number of previous hip surgeries (p = 0.25), and presence of comorbidities (p = 0.27) were not associated with failure.
Discussion
The projected increase in revision THAs underscores the importance of understanding the durability (and causes of failure) of this procedure in young patients. Such information is essential for guiding surgeon and patient expectations. Our study showed that, when compared with primary THA, revision THA is associated with decreased survivorship, more complications, and more modest improvements in clinical outcome measures at intermediate-term followup.
This study is limited because it is a single institution study and it is difficult to know whether these results are generalizable, given the paucity of current studies on this topic for comparison. This patient population was treated at a high-volume tertiary care center and therefore may represent comparatively more severe revision cases than the average young patient undergoing revision THA. This population also might have higher burdens of comorbidity than what may be seen in the average arthroplasty practice, which could contribute to our results. Second, nearly 30% of eligible patients in the revision group were lost to followup, which was significantly higher than the loss to followup among eligible patients in the control group. The outcomes in these patients—positive or negative—could affect our results. The heterogeneity of types of revision procedures performed in this cohort also may be a limitation, although this was evaluated in our analysis and no association between revision type and risk for failure was found. Another potential confounder is the effect of older technologies. For example, conventional polyethylene is known to have increased wear rates leading to osteolysis and eventual aseptic loosening [6, 10, 17]. Our study spans a 10-year period, including several years before the introduction of highly cross-linked polyethylene. It is possible that the inclusion of procedures using older materials known to have poorer performance limits our results. We found that the use of conventional polyethylene at the time of revision had an association with failure. Changes in surgical implants and techniques, such as highly cross-linked polyethylene, alternative bearings, use of larger-diameter heads, and newer enhanced in-growth surfaces, occur often and potentially confound the results of observational studies such as ours.
This study provides an important update to the literature regarding revision THAs in young patients. Historically, revision THAs have had high rates of failure in young patients. Strömberg et al. [16] reported a 21% rerevision rate after revision THA with a first-generation cementing technique in patients younger than 55 years, predominantly owing to aseptic loosening. The same group reported outcomes of revision THAs with a second-generation cementing technique in the same patient age group and reported a 14% failure rate at 7 years, also predominantly for aseptic loosening [15]. Another report on cemented acetabular revision in young patients had a rerevision rate of 11%, again mostly attributable to aseptic loosening [11]. These rerevisions were thought to be related to the lack of durable fixation that could withstand the relatively higher levels of activity in this young patient population [15, 16]. Our study, despite modern cementless fixation techniques, also showed a much lower survivorship rate for revision THAs compared with primary THAs at intermediate-term followup.
Some studies have shown higher complication rates after revision THAs. Mahomed et al. [9] reported results of primary and revision THAs in Medicare beneficiaries and reported significantly higher rates of mortality (2.6% versus 1.0%), hospital readmission (10% versus 4.6%), and instability (8.4% versus 3.1%) in revisions. Studies on revision THAs in young patients have had complication rates between 18% and 30%, similar to ours [11, 16].
Limited functional results after revision THA also are consistent with previous reports. At an average followup of 4 years (range, 2–6 years), Strömberg et al. [16] reported that 54% of their patients 55 years or younger had poor clinical outcomes, as defined by the Harris hip score. A study of the Norwegian Arthroplasty Register, which directly compared 531 revision THAs with 1087 primary THA controls, reported poorer self-reported satisfaction and postoperative function among patients with revision THA [2]. Sixty-one percent of patients with revision THAs (median age, 67 years), compared with 84% with primary THAs had good or very good overall postoperative satisfaction [2]. Lübbeke et al. [8] compared outcomes of 85 revision THAs (average patient age, 71 years) with 349 primary THAs and found that Harris hip, WOMAC, and SF-12 scores at 5 years followup were significantly lower after revision [8]. In our study, Harris hip scores and UCLA activity scores showed modest improvements after revision THAs, relative to changes after primary THAs. Despite comparison of a revision cohort with a primary cohort with similar comorbidities, it is possible that the burden of comorbidities in our study groups (34% of patients had systemic lupus erythematosus, rheumatoid arthritis, sickle cell anemia, end-stage renal disease, or HIV) had a negative affect on the outcomes of revision surgery. Previous studies have shown that the presence of significant comorbid medical conditions is associated with poorer outcomes of revision THA [1, 3]. It is unknown whether this proportion of medical comorbidity is unique to our patient cohort or whether it is typical of young patients needing revision THAs, as some patients requiring hip arthroplasty at a young age suffer from diseases such as these that predispose them to early degeneration of the hip.
The only risk factor associated with an increased likelihood of reoperation in the revision THA group was the use of conventional, rather than highly cross-linked polyethylene. Increased wear associated with conventional polyethylene, which leads to progressive osteolysis and ultimately aseptic loosening, typically is thought to be a long-term complication, occurring beyond the average followup for this study. However, this primarily comes from the study of conventional polyethylene in primary THAs. The performance of conventional polyethylene in revision THAs is unclear. A larger and longer-term study may be required to confirm our findings; however, the utility of such a study may be minimal, given the wide commercial availability of highly cross-linked polyethylene. Additionally, the durability of liner cementation makes the use of highly cross-linked polyethylene liners, even in acetabular shells without cross-linked liner options, much more likely than the continued use of conventional polyethylene in revision surgeries [19, 20].
We found that patients undergoing revision THAs experienced decreased survivorship, more complications, and more modest improvements in clinical outcome measures at intermediate-term followup than did a matched cohort of patients undergoing primary THAs. These results are similar to outcomes reported from using older implants and techniques, and these findings suggest that surgeons should take care to set reasonable expectations for young patients undergoing revision THA. Furthermore, strategies are needed to avoid revision THAs in this patient population. More durable primary THAs or perhaps delayed primary THAs using hip-preserving procedures where appropriate, could be a means to this end.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Washington University School of Medicine, Saint Louis, MO, USA.
References
- 1.Davis AM, Agnidis Z, Badley E, Kiss A, Waddell JP, Gross AE. Predictors of functional outcome two years following revision hip arthroplasty. J Bone Joint Surg Am. 2006;88:685–691. doi: 10.2106/JBJS.E.00150. [DOI] [PubMed] [Google Scholar]
- 2.Espehaug B, Havelin LI, Engesaeter LB, Langeland N, Vollset SE. Patient satisfaction and function after primary and revision total hip replacement. Clin Orthop Relat Res. 1998;351:135–148. doi: 10.1097/00003086-199806000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Koenig K, Huddleston JI, 3rd, Huddleston H, Maloney WJ, Goodman SB. Advanced age and comorbidity increase the risk for adverse events after revision total hip arthroplasty. J Arthroplasty. 2012;27:1402–1407. doi: 10.1016/j.arth.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 5.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuzyk PR, Saccone M, Sprague S, Simunovic N, Bhandari M, Schemitsch EH. Cross-linked versus conventional polyethylene for total hip replacement: a meta-analysis of randomised controlled trials. J Bone Joint Surg Br. 2011;93:593–600. doi: 10.1302/0301-620X.93B5.25908. [DOI] [PubMed] [Google Scholar]
- 7.Lie SA, Havelin LI, Furnes ON, Engesaeter LB, Vollset SE. Failure rates for 4762 revision total hip arthroplasties in the Norwegian Arthroplasty Register. J Bone Joint Surg Br. 2004;86:504–509. [PubMed] [Google Scholar]
- 8.Lübbeke A, Katz JN, Perneger TV, Hoffmeyer P. Primary and revision hip arthroplasty: 5-year outcomes and influence of age and comorbidity. J Rheumatol. 2007;34:394–400. [PubMed] [Google Scholar]
- 9.Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2003;85:27–32. doi: 10.2106/00004623-200301000-00005. [DOI] [PubMed] [Google Scholar]
- 10.McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB, Chess DG, Charron KD. Wear rate of highly cross-linked polyethylene in total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2009;91:773–782. doi: 10.2106/JBJS.H.00244. [DOI] [PubMed] [Google Scholar]
- 11.Raut VV, Siney PD, Wroblewski BM. Revision of the acetabular component of a total hip arthroplasty with cement in young patients without rheumatoid arthritis. J Bone Joint Surg Am. 1996;78:1853–1856. doi: 10.2106/00004623-199612000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, Coyte PC, Wright JG. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51:428–436. [PMC free article] [PubMed] [Google Scholar]
- 13.Singh JA, Vessely MB, Harmsen WS, Schleck CD, Melton LJ, 3rd, Kurland RL, Berry DJ. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969–2008. Mayo Clin Proc. 2010;85:898–904. doi: 10.4065/mcp.2010.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Skyttä ET, Jarkko L, Antti E, Huhtala H, Ville R. Increasing incidence of hip arthroplasty for primary osteoarthritis in 30- to 59-year-old patients. Acta Orthop. 2011;82:1–5. doi: 10.3109/17453674.2010.548029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strömberg CN, Herberts P. Cemented revision total hip arthroplasties in patients younger than 55 years old: a multicenter evaluation of second-generation cementing technique. J Arthroplasty. 1996;11:489–499. doi: 10.1016/S0883-5403(96)80099-4. [DOI] [PubMed] [Google Scholar]
- 16.Strömberg CN, Herberts P, Ahnfelt L. Revision total hip arthroplasty in patients younger than 55 years old: clinical and radiologic results after 4 years. J Arthroplasty. 1988;3:47–59. doi: 10.1016/S0883-5403(88)80052-4. [DOI] [PubMed] [Google Scholar]
- 17.Thomas GE, Simpson DJ, Mehmood S, Taylor A, McLardy-Smith P, Gill HS, Murray DW, Glyn-Jones S. The seven-year wear of highly cross-linked polyethylene in total hip arthroplasty: a double-blind, randomized controlled trial using radiostereometric analysis. J Bone Joint Surg Am. 2011;93:716–722. doi: 10.2106/JBJS.J.00287. [DOI] [PubMed] [Google Scholar]
- 18.Wainwright C, Theis JC, Garneti N, Melloh M. Age at hip or knee joint replacement surgery predicts likelihood of revision surgery. J Bone Joint Surg Br. 2011;93:1411–1415. doi: 10.1302/0301-620X.93B10.27100. [DOI] [PubMed] [Google Scholar]
- 19.Wang JP, Chen WM, Chen CF, Chiang CC, Huang CK, Chen TH. Cementation of cross-linked polyethylene liner into well-fixed acetabular shells: mean 6-year follow-up study. J Arthroplasty 2010;25:420–424. [DOI] [PubMed]
- 20.Yoon TR, Seon JK, Song EK, Chung JY, Seo HY, Park YB. Cementation of a metal-inlay polyethylene liner into a stable metal shell in revision total hip arthroplasty. J Arthroplasty. 2005;20:652–657. doi: 10.1016/j.arth.2005.01.019. [DOI] [PubMed] [Google Scholar]