Abstract
Background
Continuous femoral nerve block has been shown to decrease opioid use, improve postoperative pain scores, and decrease length of stay. However, several studies have raised the concern that continuous femoral nerve block may delay patient ambulation and increase the risk of falls during the postoperative period.
Questions/purposes
This study sought to determine whether continuous femoral nerve block with a single-shot sciatic block prevented early ambulation after total knee arthroplasty (TKA) and whether the technique was associated with adverse effects.
Methods
Between January 2011 and January 2013, 77 consecutive patients undergoing primary TKAs at an orthopaedic specialty hospital received a continuous femoral nerve block for perioperative analgesia. The femoral block was placed preoperatively with an initial bolus and 76 (99%) patients received a single-shot sciatic nerve block performed at the same time. Fifty-eight percent (n = 45) received an initial bolus of 0.125% bupivacaine and 42% (n = 32) received 0.25% bupivacaine. All 77 patients received 0.125% bupivacaine infusion postoperatively with the continuous femoral nerve block. All patients were provided a knee immobilizer that was worn while they were out of bed and was used until 24 hours after removal of the block. All patients also used a front-wheeled walker to assist with ambulation. All 77 patients had complete records for assessing the end points of interest in this retrospective case series, including distance ambulated each day and whether in-hospital complications could be attributed to the patients’ nerve blocks.
Results
Thirty-five patients (45%) ambulated for a mean distance of 19 ± 22 feet on the day of surgery. On postoperative Days 1 and 2, all 77 patients successfully ambulated a mean of 160 ± 112 and 205 ± 123 feet, respectively. Forty-eight patients (62%) had documentation of ascending/descending stairs during their hospital stay. No patient fell during the postoperative period, required return to the operating room, or readmission within 90 days of surgery. One patient experienced a transient foot drop related to the sciatic nerve block, which resolved by postoperative Day 1.
Conclusions
Continuous femoral nerve block with dilute bupivacaine (0.125%) can be successfully used after TKA without preventing early ambulation. By taking active steps to prevent in-hospital falls, including the use of a knee immobilizer for ambulation while the block is in effect, patients can benefit from the analgesia provided by the block and still ambulate early after TKA.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The recent introduction of the Patient Protection and Affordable Care Act has made hospital and surgeon reimbursement subject to penalty if patients are not satisfied with the quality of their care after surgery [11]. With more than 50% of patients citing postoperative pain as their primary fear before surgery [19], and pain control being one of several important quality measures involved in the Patient Protection and Affordable Care Act, there is a compelling argument for the surgeon and anesthesiologist to focus on postoperative pain control after major surgeries such as TKA.
Continuous femoral nerve block has been shown to decrease opioid use and improve postoperative pain scores [3, 5, 6, 8, 9, 14, 15, 18]. These blocks have also been shown to decrease length of stay and complications and increase early knee flexion [3, 5, 6, 8, 14, 15, 18]. However, several studies have raised the concern that continuous femoral nerve block may delay patient ambulation and increase the risk of falls during the postoperative period [10, 16]. To date, few studies specifically address the effect of continuous femoral nerve block on early ambulation after TKA [4, 14, 15].
The primary objective of this study was to determine whether continuous femoral nerve block, as a component of multimodal analgesia, prevented early ambulation after TKA. The secondary objective was to report other adverse effects such as patient falls with the use of a continuous femoral nerve block.
Patients and Method
After institutional review board approval, we retrospectively reviewed a consecutive series of 77 patients treated with continuous femoral nerve block after primary TKA at a single location. All TKAs were performed at an academic orthopaedic specialty hospital between January 2011 and January 2013 by a single surgeon (CLP). All patients at this location receive a continuous femoral nerve block, unless the patient declined a block or if it was contraindicated by allergy. Because no patients during this period had contraindications or refused a block, all were included for review. Patients’ records were reviewed for admission date, discharge date, discharge location, age, primary diagnosis, surgical anesthetic type, nerve block type and concentration, American Society of Anesthesiologists (ASA) score, total anesthesia time, height, weight, anesthesiologist, ambulation distances, stairs ascended, falls, reoperations, and any other block-associated complications.
The cross-section of patients was similar to the overall practice of the surgeon in regard to age, sex, and height but differed in weight and body mass index (Table 1). Forty-four underwent general anesthesia (57%) and 33 spinal anesthesia (43%) with all 77 receiving a continuous femoral nerve block and 76 (99%) a single-shot sciatic block. The primary diagnosis was osteoarthritis in 94%. The median ASA score was 2 (range, 1–3) and the average total operating room time was 132 ± 29 minutes. Fifty-eight percent (n = 45) received an initial bolus of 0.125% bupivacaine and 42% (n = 32) received 0.25% bupivacaine. All 77 patients received 0.125% bupivacaine infusion postoperatively with the continuous femoral nerve block. The electronic medical record contained specific documentation of each time the patient ambulated with the therapist and the distances achieved on each attempt for all patients.
Table 1.
Patient characteristics
| Variable | Cross-section | Overall practice* | p value |
|---|---|---|---|
| Number of patients | n = 77 (22%) | n = 345 | |
| Age (years) | 62 ± 11 (range, 18–88) | 63 ± 11 (range, 26–91) | 0.31 |
| Sex | |||
| Male | 27 (35%) | 38% | 0.63 |
| Female | 50 (65%) | 62% | |
| Height (inches) | 67 ± 4 (range, 60–79) | 67 ± 4 (range, 49–77) | 0.70 |
| Weight (lbs) | 189 ± 45 (range, 110–322) | 210 ± 59 (range, 106–425) | 0.008 |
| Body mass index (kg/m2) | 30 ± 7 (range, 20–53) | 33 ± 8 (range, 16–56) | 0.01 |
* All primary TKAs performed by the surgeon from January 2011 to January 2013 at two facilities.
All 77 patients received continuous femoral nerve block as part of an established multimodal analgesia protocol that also included a single-injection sciatic nerve block at the level of the popliteal fossa. The pharmacologic components of this protocol included scheduled doses of pregabalin, celecoxib, and acetaminophen with oxycodone administration as needed.
Anesthesia and perioperative pain management at this location are under direct supervision of a single anesthesiologist (JDS). All nerve blocks were placed preoperatively using ultrasound guidance (Fig. 1). Patients received detailed instruction on the risks and benefits of peripheral nerve block before surgery and anesthesia. The continuous femoral nerve block catheters were positioned deep to the fascia iliaca and 1 cm lateral to the femoral nerve. All patients received an initial injection of preservative-free bupivacaine (30 mL) followed by an infusion of bupivacaine 0.125% at a rate of 5 mL/hour for 48 hours. All sciatic nerve blocks were also placed using ultrasound guidance. These blocks were performed using a single injection of 0.125% bupivacaine (30 mL) approximately 1 cm medial to the sciatic nerve within the popliteal space. Before surgery, each patient was tested for temperature and light touch sensation over the anterior thigh and foot to confirm sensory loss in the distributions of the femoral and sciatic nerves.
Fig. 1.
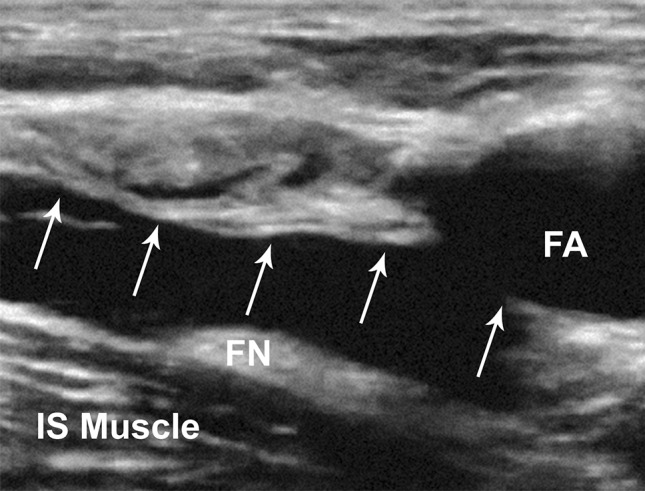
An ultrasound image inferior to the inguinal ligament shows a hypoechoic space deep to the fascia iliaca (demonstrated by white arrows) created by the injection of bupivacaine. The femoral artery (FA) and femoral nerve (FN) are visible. After injection, the FN is visible on the surface of the iliopsoas (IS) muscle.
Intraoperatively, patients received either a spinal or general anesthetic based on the preferences of the patient and the attending anesthesiologist. All surgeries were performed through a midline anterior incision and a medial parapatellar approach by the senior author (CLP). All total knee operations were performed according to a standard protocol using the same surgical technique and implant design (Biomet Vanguard; Biomet Inc, Warsaw, IN, USA) [15]. During the procedure, 30 mL of 0.25% bupivacaine without epinephrine was injected posterior to the capsule after all bony cuts were completed. At the end of the procedure, a sterile dressing was applied as well as a cryotherapy pad and knee immobilizer.
On the day of surgery and twice daily thereafter, a physical therapist consulted on each patient in an attempt to have them stand and ambulate. A knee immobilizer and front-wheeled walker were used during ambulation as a precaution for possible quadriceps weakness. The knee immobilizer was continued until 72 hours after surgery (24 hours after the block was removed). All patients were also evaluated for motor function in the distribution of the sciatic nerve before ambulation. Those patients with weakness in the tibial or peroneal nerve distribution were not allowed to ambulate until motor function had recovered. In addition to scheduled physical therapy, patients were allowed to ambulate as desired with the assistance of the floor nurse; however, because distance during these sessions was not recorded, this was not included in the analysis. The electronic record was reviewed to identify specific rehabilitation events such as the time of first ambulation, the distances ambulated, the ability to ascend stairs, and the incidence of patient falls or other complications related to ambulation.
For patients who did not ambulate on the day of surgery, the record was also examined to determine if a cause for this was recorded. If patients reported increased pain at rest or with ambulation, the floor nurse first documented the presence of continued sensory loss in the distribution of the femoral nerve before administering additional oral analgesics. If no sensory change was evident in the femoral nerve distribution, the anesthesiologist was consulted to restore effective block by supplemental catheter bolus or replacing the catheter when necessary. While in bed, the knee immobilizer was loosened or removed at the patient’s request with explicit instructions not to attempt ambulation without the knee immobilizer in place. All patients were placed on a continuous passive motion machine for up to 6 hours a day with patient-controlled range of up to 0° to 90°.
The continuous femoral nerve block catheter was removed 48 hours after discharge from the postanesthesia care unit in all patients. Patients continued to use a knee immobilizer until sensation over the anterior thigh had returned to normal and they could demonstrate active knee extension. If the patient was discharged before the morning of postoperative Day 3, they were instructed to wear their knee immobilizer during ambulation until the morning of the third day or until complete return of anterior thigh sensation.
The length of hospital stay was recorded for each patient. For any patient whose length of stay exceeded 3 days, the electronic record was examined to determine whether any medical or surgical complication resulted in prolonged hospitalization. Patients were seen 2 weeks after surgery in the clinic for removal of skin staples and assessment of quadriceps function. The electronic records for the postoperative visits were also reviewed to document any block-related complications.
Summary statistics were reported as means ± SD. Statistics were performed using commercially available software (STATA® Version 12.1; Statacorp, LP, College Station, TX, USA).
Results
On the day of surgery, 35 patients (45%) ambulated for a mean distance of 19 ± 22 feet. For the remaining 42 patients (55%), there was no documented attempt at ambulation. On postoperative Day 1, all 77 patients successfully ambulated. The mean total distance ambulated for postoperative Day 1 was 160 ± 112 feet. Likewise, on postoperative Day 2, all patients were able to ambulate a mean of 205 ± 123 feet. Ambulation distances on postoperative Day 3 were a mean 80 ± 70 feet; however, only five patients (6%) remained hospitalized long enough to complete more than one session of physical therapy. Thus, ambulation for postoperative Day 3 was not included in the analysis. Forty-eight patients (62%) had documentation of ascending/descending stairs during their hospital stay. On the day of surgery, one patient was able to ascend nine stairs. Three patients climbed stairs (17 ± eight stairs) by postoperative Day 1 and 33 patients climbed stairs (nine ± nine stairs) by postoperative Day 2.
There were no postoperative falls nor any other complications requiring return to the operating room or readmission to the hospital within the first 90 days. At the 2-week postoperative visit, all but one returning patient (n = 76) could ambulate without the need for staff assistance and all patients could perform full active knee extension. One patient returned to an outside physician for their 2-week followup appointment because of geographic inaccessibility, so quadriceps function was not documented at that time. This patient returned for a 6-week followup and presented with normal sensation and quadriceps function. One patient manifested motor weakness in the distribution of the peroneal nerve (foot drop) on the day of surgery that resolved by postoperative Day 1. There were no reports of motor weakness in the distribution of the sciatic nerve for any patient after the day of surgery and no complications were attributable to the use of the femoral or sciatic nerve blocks.
Discussion
Previous studies have demonstrated that femoral nerve block can provide decreased opioid use, improved postoperative pain scores, and decreased length of stay while avoiding many of the complications associated with other techniques such as continuous epidural analgesia [3, 5, 6, 8, 14, 15, 18]. However, concerns remain that femoral nerve block will prevent early ambulation and increase the number of patient falls after surgery [1, 7, 10, 12]. In our cohort, all patients were able to ambulate by postoperative Day 1 and 45% (35 of 77) of patients were able to ambulate on the day of surgery. In this small retrospective series, we observed no falls or serious complications related to use of the blocks, although we took active steps to prevent falls, including the use of a knee immobilizer for ambulation while the block was in effect.
As a retrospective case series, our study has characteristic limitations in its design. The major limitation of this study is the small size of the series, which was too small to quantify uncommon events such as falls or permanent nerve injury and thus, the safety of this analgesic approach cannot be compared with more traditional opioid-based techniques based on this study alone. In addition, despite the favorable outcomes in our series when compared with earlier trials [8, 14, 15], our study lacks a control group and thus, we are unable to compare the beneficial effect of our multimodal pain management protocol with traditional opioid-based techniques. Another concern is selection bias. The majority of TKAs performed by the senior surgeon during the study period (78%), including the high-risk patients, were performed at a separate tertiary care facility and not at the study site where the patients in this series received their care; thus, this study population was different from the overall population of primary TKAs in some important ways, including weight and body mass index (Table 1), and this likely resulted in some selection bias. However, the variability in anesthesia care at our tertiary care center would have introduced considerable variability in the technique and anesthetic concentrations used. Hence, we chose to include only patients from our orthopaedic specialty hospital because all patients at this facility had direct oversight from a single anesthesiologist and received the same multimodal pain control with dilute bupivacaine (0.125%) continuous femoral nerve catheters performed under ultrasound guidance, which decreased confounding factors.
Among existing publications, there is considerable disparity about the effect of femoral nerve block on early ambulation after TKA. Although some authors have reported mean ambulation distances of 102 to 337 feet in the first 2 days after surgery [4, 14, 15], others note substantial limitations in early ambulation. For example, Seet et al. [16] reported no ambulation until at least 60 hours after surgery. Similarly, Kandasami et al. [10] reported that 70% of their patients were unable to mobilize until postoperative Day 2 (Table 2). An important component of our treatment protocol facilitating ambulation is the use of dilute bupivacaine with the intention of preserving motor function. It is well known that bupivacaine exhibits a dose-response effect that progresses from analgesia to dense motor block as its concentration is increased and although it is desirable to use motor-sparing concentrations of bupivacaine, the duration of action of such concentrations is limited [13]. Thus, we used a continuous femoral nerve block infusion to control both the duration and density of block effect. Despite our use of dilute local anesthetic infusions, we continued to use, and strongly recommend to those considering such a protocol, the precaution of having patients wear a knee immobilizer and ambulate with a front-wheeled walker during the early postoperative period.
Table 2.
Comparisons in the literature of patients undergoing TKA and receiving femoral nerve block for postoperative multimodal pain management
| Study | Type of study | Number of patients | Mean length of stay (days; range) | Mean days before ambulation* | Mean ambulation (POD 0–3) |
|---|---|---|---|---|---|
| Current study | Retrospective case series | 77 | 2.7 (2–5) | 1 | 116 ft |
| Nader et al. (2012) [14] | Randomized controlled trial | 62 | NR | 1 | 120 ft |
| Sharma et al. (2010) [17] | Retrospective cohort | 970 | 3.9 (2–21) | NR | NR |
| Carli et al. (2010) [4] | Randomized controlled trial | 40 | 5 | 2 | 187 ft |
| Seet et al. (2006) [16] | Randomized controlled trial | 60 | 6.5 | 2.7 | NR |
| Peters et al. (2006) [15] | Retrospective cohort | 100 | 3 | NR | 102 ft |
* For 100% of patients; POD = postoperative day; NR = not reported.
Early ambulation is an important component for optimal recovery after TKA. We believe our outcomes to be noteworthy in that all patients were able to ambulate on postoperative Day 1 and thereafter. Our findings suggest that continuous femoral nerve block using low-dose bupivacaine does not prevent ambulation in the early postoperative period. In this series, patients had documented sensory effects in the distribution of the femoral nerve but were not adversely affected by any associated motor block. This may be attributed to use of a knee immobilizer while the block is in place along with training and diligence of the floor staff.
The overall complication rate of femoral nerve catheters has generally ranged from 1.5% to 8.0% [7, 10, 17, 20]. This risk can be reduced through the use of ultrasound guidance, which decreases the risk of vascular or other mechanical injury during insertion [2]. Moreover, the risk of postoperative falls with continuous femoral nerve block has been reported to be 0.7% to 3.0% with reoperation required in up to 0.4% of cases [7, 10, 17, 20]. In our group of patients, there were no reported falls despite having all patients ambulate at least twice daily. However, our study did not include adequate numbers to address this issue specifically.
Although several previous publications have warned surgeons about the detrimental effects on postoperative ambulation, this analysis demonstrates that continuous femoral nerve block with dilute bupivacaine (0.125%) can be successfully used in conjunction with multimodal analgesia after TKA in a way that does not prevent early ambulation. By taking active steps to prevent in-hospital falls, including the use of a knee immobilizer for ambulation while the block is functioning, patients can benefit from the analgesia provided by the block and still ambulate early after TKA.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Atkinson HD, Hamid I, Gupte CM, Russell RC, Handy JM. Postoperative fall after the use of the 3-in-1 femoral nerve block for knee surgery: a report of four cases. J Orthop Surg (Hong Kong). 2008;16:381–384. doi: 10.1177/230949900801600324. [DOI] [PubMed] [Google Scholar]
- 2.Baldi C, Bettinelli S, Grossi P, Fausto A, Sardanelli F, Cavalloro F, Allegri M, Braschi A. Ultrasound guidance for locoregional anesthesia: a review. Minerva Anestesiol. 2007;73:587–593. [PubMed] [Google Scholar]
- 3.Capdevila X, Barthelet Y, Biboulet P, Ryckwaert Y, Rubenovitch J, d’Athis F. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999;91:8–15. doi: 10.1097/00000542-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Carli F, Clemente A, Asenjo JF, Kim DJ, Mistraletti G, Gomarasca M, Morabito A, Tanzer M. Analgesia and functional outcome after total knee arthroplasty: periarticular infiltration vs continuous femoral nerve block. Br J Anaesth. 2010;105:185–195. doi: 10.1093/bja/aeq112. [DOI] [PubMed] [Google Scholar]
- 5.Chelly JE, Greger J, Gebhard R, Coupe K, Clyburn TA, Buckle R, Criswell A. Continuous femoral blocks improve recovery and outcome of patients undergoing total knee arthroplasty. J Arthroplasty. 2001;16:436–445. doi: 10.1054/arth.2001.23622. [DOI] [PubMed] [Google Scholar]
- 6.De Ruyter ML, Brueilly KE, Harrison BA, Greengrass RA, Putzke JD, Brodersen MP. A pilot study on continuous femoral perineural catheter for analgesia after total knee arthroplasty: the effect on physical rehabilitation and outcomes. J Arthroplasty. 2006;21:1111–1117. doi: 10.1016/j.arth.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Feibel RJ, Dervin GF, Kim PR, Beaule PE. Major complications associated with femoral nerve catheters for knee arthroplasty: a word of caution. J Arthroplasty. 2009;24:132–137. doi: 10.1016/j.arth.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Ilfeld BM, Mariano ER, Girard PJ, Loland VJ, Meyer RS, Donovan JF, Pugh GA, Le LT, Sessler DI, Shuster JJ, Theriaque DW, Ball ST. A multicenter, randomized, triple-masked, placebo-controlled trial of the effect of ambulatory continuous femoral nerve blocks on discharge-readiness following total knee arthroplasty in patients on general orthopaedic wards. Pain. 2010;150:477–484. doi: 10.1016/j.pain.2010.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jamison RN, Ross MJ, Hoopman P, Griffin F, Levy J, Daly M, Schaffer JL. Assessment of postoperative pain management: patient satisfaction and perceived helpfulness. Clin J Pain. 1997;13:229–236. doi: 10.1097/00002508-199709000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Kandasami M, Kinninmonth AW, Sarungi M, Baines J, Scott NB. Femoral nerve block for total knee replacement—a word of caution. Knee. 2009;16:98–100. doi: 10.1016/j.knee.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Lansky D, Nwachukwu BU, Bozic KJ. Using financial incentives to improve value in orthopaedics. Clin Orthop Relat Res. 2012;470:1027–1037. doi: 10.1007/s11999-011-2127-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lareau JM, Robbins CE, Talmo CT, Mehio AK, Puri L, Bono JV. Complications of femoral nerve blockade in total knee arthroplasty and strategies to reduce patient risk. J Arthroplasty. 2012;27:564–568. doi: 10.1016/j.arth.2011.06.028. [DOI] [PubMed] [Google Scholar]
- 13.Liu SS, Ware PD, Allen HW, Neal JM, Pollock JE. Dose-response characteristics of spinal bupivacaine in volunteers. Clinical implications for ambulatory anesthesia. Anesthesiology. 1996;85:729–736. doi: 10.1097/00000542-199610000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Nader A, Kendall MC, Wixson RL, Chung B, Polakow LM, McCarthy RJ. A randomized trial of epidural analgesia followed by continuous femoral analgesia compared with oral opioid analgesia on short- and long-term functional recovery after total knee replacement. Pain Med. 2012;13:937–947. doi: 10.1111/j.1526-4637.2012.01409.x. [DOI] [PubMed] [Google Scholar]
- 15.Peters CL, Shirley B, Erickson J. The effect of a new multimodal perioperative anesthetic regimen on postoperative pain, side effects, rehabilitation, and length of hospital stay after total joint arthroplasty. J Arthroplasty. 2006;21:132–138. doi: 10.1016/j.arth.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 16.Seet E, Leong WL, Yeo AS, Fook-Chong S. Effectiveness of 3-in-1 continuous femoral block of differing concentrations compared to patient controlled intravenous morphine for post total knee arthroplasty analgesia and knee rehabilitation. Anaesth Intensive Care. 2006;34:25–30. doi: 10.1177/0310057X0603400110. [DOI] [PubMed] [Google Scholar]
- 17.Sharma S, Iorio R, Specht LM, Davies-Lepie S, Healy WL. Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res. 2010;468:135–140. doi: 10.1007/s11999-009-1025-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998;87:88–92. doi: 10.1097/00000539-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Warfield CA, Kahn CH. Acute pain management. Programs in US hospitals and experiences and attitudes among US adults. Anesthesiology. 1995;83:1090–1094. doi: 10.1097/00000542-199511000-00023. [DOI] [PubMed] [Google Scholar]
- 20.Wasserstein D, Farlinger C, Brull R, Mahomed N, Gandhi R. Advanced age, obesity and continuous femoral nerve blockade are independent risk factors for inpatient falls after primary total knee arthroplasty. J Arthroplasty. 2012 Dec 19 [Epub ahead of print]. [DOI] [PubMed]


