Abstract
Purpose
We investigated the functional and radiological outcomes of conservatively treated simple traumatic elbow dislocations and subsequent incidence of cubitus valgus development in children.
Methods
Eleven patients (one female, ten male; mean age 9.8 years, range seven to 12 years) who presented to our hospital with simple elbow dislocations and were conservatively treated between July 2008 and September 2010 were included in the study. All were posterolateral closed dislocations. None of the patients had accompanying elbow fractures. All patients had pre- and postoperative radiographic examinations. The carrying angle of the involved elbow was measured and compared to the contralateral non-injured elbow during follow-up. The incidence and severity of cubitus valgus development was assessed. The functional and clinical outcomes were evaluated using the Mayo Elbow Performance Scale. The mean monitoring period was 24.3 months (range 19–30 months).
Results
All patients had satisfactory good and excellent results (85–100 points; mean 96.8 points) according to the Mayo Elbow Performance Scale. The final average elbow flexion was 137° (range, 130–145°) and average extension was 8.6° (range 0–20°) with full supination and pronation in traumatic elbow. Four patients (36.4 %) had an average increase (cubitus valgus) of 14.5° (10–20°) in carrying angle compared to the other elbow.
Conclusions
While isolated traumatic dislocation of the elbow is uncommon among children, it can be successfully treated by urgent closed reduction, proper fixation of the elbow and appropriate timely rehabilitation. However, it should be considered that some patients may develop cubitus valgus deformity in a later period. Therefore, each patient with a simple traumatic elbow dislocation should be followed, and the parents should be informed of the potential for any deformity development.
Keywords: Children, Cubitus, Dislocation, Elbow, Elbow joint, Valgus
Introduction
Traumatic elbow dislocations are rare and uncommon injuries among children [1]. They account for approximately 3–6 % of all elbow injuries experienced by children [2, 3].
The elbow carrying angle develops as a response to the forearm pronation, and keeps the upper extremity away from the side of the pelvis during walking. The carrying angle increases starting with the newborn, and reaches a peak value by the age of 15, which is the closing age for growth plates around the elbow. The annual rate of increase of the carrying angle is 0.42° for boys and 0.60° for girls [4]. In a Turkish study, the mean elbow carrying angle of the dominant extremity in six-year-old boys was 12.41° while it was measured 12.85° in girls. The corresponding values of 14-year old teenagers were 18.17° for boys and 18.10° for girls [5].
Extreme increase in the carrying angle is associated with elbow instability and pain during exercise or throwing sports [6]. It may also decrease elbow function and make the elbow vulnerable to dislocation [7]. Knowing the mean carrying angle and standard deviation for a certain age would help us identify the cosmetically acceptable limits of the deformity that occurred [8]. The extreme increase in the carrying angle of the elbow is referred to as cubitus valgus.
Elbow valgus deformity (cubitus valgus) is mostly associated with nonunion of lateral condylar physeal fractures [3]. However, there is no report in the literature for development of valgus deformity following simple elbow dislocations.
We evaluated the conservative treatment of traumatic simple elbow dislocations and its clinical, functional and radiological outcomes in children. Our objective was to determine incidence and severity of cubitus valgus deformity following simple elbow dislocations, which we presume might be a sequelae from growth stimulation of the medial condylus after the dislocation.
Patients and methods
We retrospectively evaluated the functional and clinical results of 11 patients (one female, ten male; mean age 9.8 years; range seven to 12 years) who presented to our hospital with traumatic simple elbow dislocation and were conservatively treated with long-arm splint between July 2008 and September 2010. All were isolated dislocations, so-called simple dislocations (Fig. 1a). One of the patients (9 %) had an accompanying ipsilateral distal radial fracture. None of them had obvious vascular-neurological problems during presentation. The cause of all elbow dislocations was a fall. In all patients, the dislocation was closed and posterolateral. In the patient with a distal radial fracture, the elbow dislocation was reduced, followed by the reduction of the radial fracture. After the procedure, the reduction and range of joint motion were evaluated, showing normal vascular-neurological results. The carrying angle of both elbows were measured clinically and recorded before splinting and at latest follow-up examination. Then, with the forearm in mid-pronation position, a posterior long-arm splint was used in all patients to help keep the remaining intact medial tissues in place when the elbow was flexed 90°. The concentric reduction was documented with direct lateral radiography (Fig. 1b). For each patient, the injured elbow was examined by computed tomography (CT) and magnetic resonance imaging (MRI) during initial presentation and in order to detect possible additional osseous and soft-tissue lesions. The procedures were repeated during follow-up, because of our observation of increase in valgus angles.
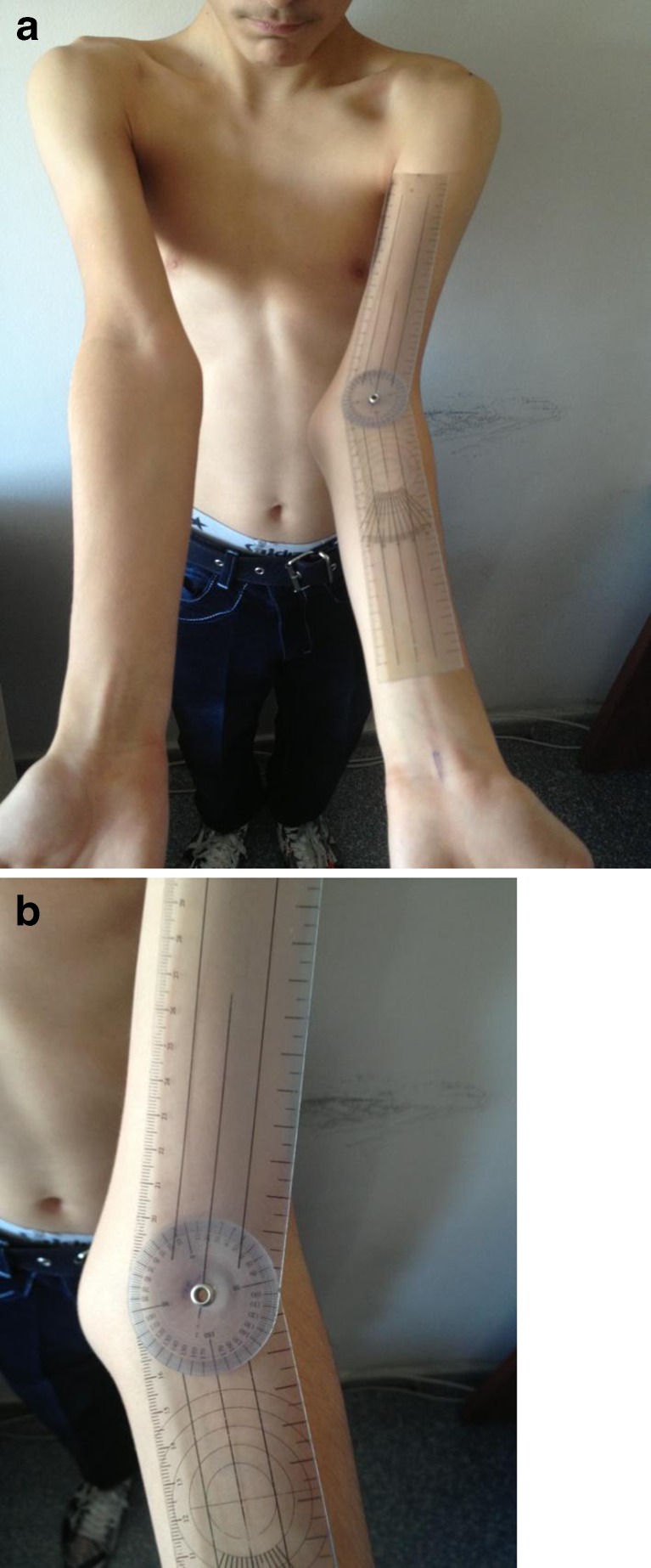
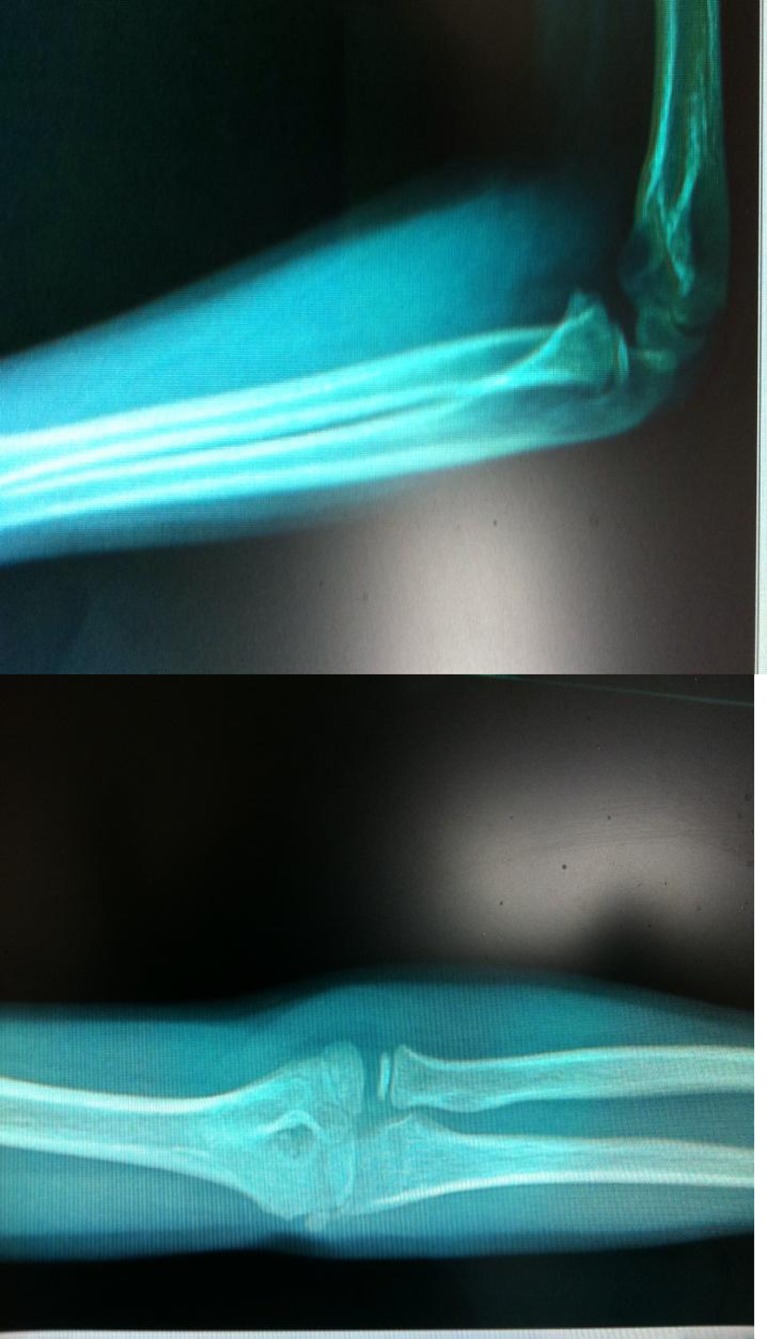
Fig. 1.
a AP and Lateral X-rays of an 11-year-old boy with simple traumatic left elbow dislocation (pre-reduction). b. Lateral X-rays of an 11-year-old boy with simple traumatic left elbow dislocation (post-reduction)
The patients were monitored at the emergency observation unit following the reduction for one day. With an average duration of splint immobilization for 3.3 (three to four) weeks, postoperative controls were performed at weeks one, three, four and six, and then they were scheduled for examination every three months. The carrying angle of each patient was measured in comparison to the other elbow during follow-up. Elbow angulation is clinically measured by the carrying angle. Radiologically it is referred to as the humero-ulnar angle [9]. The carrying angle is the angle between the centreline of the forearm and centreline of the arm when the elbow is fully extended and flexed at zero degrees and the wrist is in neutral position, and the forearm is in full supination [10]. The measurement was performed as described by Balasubramanian et al. [4] when elbow joint was in full extension, with the forearm supinated and hand/wrist in neutral position using a goniometer. The elbow was maintained at neutral, forearm in full supination and the wrist at neutral. An orthopaedic goniometer was placed with its hinge in the centre of the cubital crease (midway between the medial and lateral humeral condyles). The tips of the two axes of its arms were directed such that one was toward the lateral edge of the acromion (easily palpable in children) and the other toward the midpoint of the radial and ulnar styloid. The angle was measured off the dial at the centre of the goniometer, to the nearest degree (as that was the lowest count of the goniometer). This angle corresponded to the acute angle between the axis of the arm and the axis of the fully supinated and extended forearm held neutral at the elbow [4] (Fig. 2a and b).
Fig. 2.
Photos of the same patient as in Fig. 1 demonstrating 20° of cubitus valgus deformity
In the patient with an ipsilateral distal radial fracture, the long-arm splint was removed and replaced with a short-arm splint at week three, and active range of motion exercises were initiated. Range of motion exercises were started at three weeks in all patients. Considering the risk of developing joint stiffness and myositis ossificans, forcible exercises were avoided until week six. None of our patients developed myositis ossificans. They had full range of motion during follow-up. The mean follow-up was 24.3 months (range 19–30). The clinical and functional results were assessed for all patients during follow-up following the monitoring period, and scored according to the Mayo elbow performance scoring system [5]. A score of 75 and over was considered satisfactory [11]. The radiological results were evaluated by direct radiography. The carrying angles were measured and compared to the carrying angle of the intact elbow. And they were also compared to the carrying angle measurements performed immediately after the trauma. We evaluated the difference in carrying angles between the normal and the dislocated elbows and between the measurements after the trauma and at final follow-up. We used Student’s t-test for statistical evaluation of the change in carrying angles. All analyses were performed using SPSS II Version 17.0 (SPSS, Inc, Chicago, IL, USA). Student’s t-test was performed to assess differences of carrying angles between the post-reduction first day and last follow-up.
Results
All dislocations were posterolateral. The right upper limb was dominant in ten of the patients (91 %). Three patients (27 %) had right elbow injury, and eight (73 %) had left elbow injury. None of the patients had skin injury and excessive edema around the elbow. The reductions were performed without sedation in emergency room. The range of elbow motion was full and stable in all cases after the reduction. No other potential complications including joint stiffness, permanent nerve injury, posttraumatic arthrosis, chronic pain, myositis ossificans and recurrent dislocation were observed during final controls (Figs. 3 and 4).
Fig. 3.
AP and Lateral X-rays of the same patient as in Figs. 1 and 2 during follow-up in the 26th month
Fig. 4.
CT and MR images of the same patient
One patient had an ipsilateral distal radial fracture accompanied with the posterolateral elbow dislocation. The patient first underwent closed reduction for elbow dislocation. Then, the distal radial fracture was reduced, and a posterior long-arm cast splint was used. The fracture healed without any complications. The patient had no pain and the range of motion of was full during final control (Table 1).
Table 1.
Patient measurements
| Patient | Flex/ ext (°) | Pron/ Supin (°) | Right-hand side (CA) | Left-hand side (CA) | Difference before and after trauma | |||
|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | |||||
| 1 | 130 | 20 | 75/75 | 12 | 30 | 11 | 11 | 18 |
| 2 | 135 | 10 | 70/75 | 12 | 12 | 10 | 30 | 20 |
| 3 | 140 | 20 | 70/75 | 10 | 10 | 10 | 20 | 10 |
| 4 | 135 | 0 | 75/75 | 9 | 9 | 10 | 10 | 0 |
| 5 | 145 | 10 | 75/80 | 10 | 11 | 10 | 20 | 10 |
| 6 | 145 | 0 | 80/80 | 12 | 12 | 15 | 15 | 0 |
| 7 | 140 | 5 | 70/80 | 10 | 10 | 10 | 12 | 2 |
| 8 | 140 | 0 | 70/75 | 12 | 12 | 12 | 12 | 0 |
| 9 | 135 | 10 | 75/75 | 13 | 13 | 9 | 10 | 1 |
| 10 | 130 | 0 | 70/75 | 13 | 13 | 13 | 13 | 0 |
| 11 | 135 | 15 | 75/80 | 11 | 10 | 11 | 12 | 1 |
CA carrying angle
Four patients (36 %) had clinically obvious increase in carrying angles of the elbow (cubitus valgus) (Fig. 2a and b).
During evaluation of the carrying angles of the elbow following removal of the splint, the mean angle was 11.2° (9–13°) on the right side, and 12° (9–15°) on the left side. During the final control, the mean carrying angle was 11.7° (9–15°) for intact elbows versus 16.5° (10–30°) for traumatised elbows. In four cases (36 %) who developed cubitus valgus deformity, an average increase of 14.5° (10–20°) was observed in carrying angles of the elbow compared to the other elbow and the posttraumatic measurements (Table 1). The p value was found to be 0.038 after statistical analysis using the Student’s t-test, i.e. the mean increase in carrying angle of the related limb was statistically significant.
The appearance of the elbow when compared to the intact elbow had a negative psychological impact on the child and his/her parents.
The clinical results were evaluated according to the Mayo elbow performance scoring system. The mean score of the patients was 96.8 points (85–100), with satisfactory results (good and excellent) in all patients (Table 2).
Table 2.
Posttraumatic measurements
| Patient | Sex | Age (years) | Dominant side | Trauma side | Mayo performance score | Monitoring period (months) | Instability | Pain |
|---|---|---|---|---|---|---|---|---|
| 1 | Male | 10 | R | R | 95 | 28 | No | No |
| 2 | Male | 11 | R | L | 85 | 25 | No | No |
| 3 | Male | 11 | R | L | 85 | 22 | No | No |
| 4 | Male | 10 | R | L | 100 | 30 | No | No |
| 5 | Male | 10 | L | L | 100 | 27 | No | No |
| 6 | Male | 10 | R | R | 100 | 20 | No | No |
| 7 | Male | 12 | R | L | 100 | 23 | No | No |
| 8 | Male | 10 | R | R | 100 | 24 | No | No |
| 9 | Male | 8 | R | L | 100 | 25 | No | No |
| 10 | Male | 9 | R | L | 100 | 24 | No | No |
| 11 | Female | 7 | R | L | 100 | 19 | No | No |
Postreduction direct radiography, CT and MRI examinations showed no pathology in bones or epiphyseal plate.
Discussion
Elbow dislocations are classified and defined according to the position of the proximal radio-ulnar joint in relation to the distal humerus [2, 12]. As seen in our series, this type of dislocation usually occurs as a result of a fall when the forearm is in supination and the elbow is in extension or partial flexion [1, 13]. Elbow dislocations usually are associated with a combination of axial compressive force, supination moment and valgus moment. The soft tissue ring is damaged from lateral to the medial during displacement of the elbow [14]. Almost all simple dislocations are conservatively treated with closed reduction. Acceptable outcomes have been reported with use of either a sling or casting with early elbow range of motion [15]. All of our patients were diagnosed with simple dislocation, and they underwent conservative treatment.
Most elbow dislocations in children are posterior or posterolateral dislocations. A study by Rasool et al. reported that 66 % of dislocations were either posterolateral or posterior, which was repeated by Roberts et al. who achieved 64 % [7, 12]. In a study by Carlioz et al., the rate was 100 % [6, 16]. All of our patients had posterolateral dislocations.
The simple elbow dislocations were reported in the non-dominant left elbow to be 58 % and 54 % in Joseffson et al. [17] and De Haan et al. [12], respectively. It was noteworthy that the dislocation was in the non-dominant left elbow in seven of our patients (70 %). The left side was dominant and traumatised in one patient. Although there has been no comment why non-dominant elbow was mostly injured in the literature, we think that there might have been lower muscular development which made them more susceptible for dislocation.
As simple dislocations are uncommon, evaluation of direct radiographs is crucial to avoid overlooking any fracture in the elbow area. An elbow dislocation observed in an infant should alarm the orthopaedist for potential transphyseal fracture or other fractures. A study by Rasool et al. reported that fractures associated with the dislocated elbow were not accurately diagnosed in 24 % of cases [18]. We performed a very careful evaluation of the direct radiographies for all patients before and after the reduction to identify any potential fractures as well as careful review of the CT and MRI examinations. No fracture was identified in the following period.
One of the factors that affects the outcomes in elbow dislocation is the period between the time of injury and the reduction. The longer this period, the lower the chance to obtain a satisfactory result [11, 19]. Our patients underwent closed reduction at latest within two hours after the event without any need for general/local anaesthesia. Since the period between the trauma and the reduction procedure was short, no excessive oedema was observed in the elbows. We believe that absence of oedema in the elbow facilitated the reduction and follow-up. By subjective means, there was a sudden decrease in pain after the reduction. With decreased pain, it was easier and better to communicate with the children, and perform vascular-neurological evaluation. Based on this, we concluded that elbow dislocations were easier to reduce as soon as they were diagnosed, and further examinations and tests could be easily performed as we earned our patients’ trust by immediately decreasing their pain.
Since compartment syndrome development was reported after elbow dislocations, the patients remained in the emergency observation unit for medical observation for 24 hours following the reduction. When clinical examinations showed no development of compartment syndrome, they were discharged and scheduled for control examinations.
It is uncommon to have recurrent dislocation and instability in simple elbow dislocations following closed reduction and splint use [15, 20]. None of our patients experienced recurrent dislocation or any instability.
Our main objective in elbow dislocations should be to have functional therapy and assure the shortest possible immobilization time. The short immobilization time by splint is closely associated with obtaining a better range of motion. Protzmann indicated that shorter immobilization time in elbow dislocations resulted in lower extension loss in the elbow and lower rate of impairment [12]. Furthermore, Mehlhoff identified a strong relation between shorter immobilization period and less extension loss [21]. The elbows of our patients were immobilized for an average of three weeks using long-arm splints. No statistically significant relation was identified between immobilization period and development of cubitus valgus.
Since joint range of motion is negatively affected after injuries around the elbow area, rehabilitation is crucial. It was reported that forcible manipulations to obtain joint range of motion increased the risk of myositis ossificans [5, 11]. Early active motion should be initiated as early as possible in traumatic elbow [22]. Prolonged immobility, delay in initiating early functional motion and strong early active physiotherapy have been reported to cause myositis ossificans in children [23].
The carrying angle varies with age, and it varies from person to person. Therefore, any comparison should be made to the opposite side, not to the normal standard [24]. The elbow carrying angle increases in both genders as the person ages, and it is statistically larger on the dominant limb [25]. There was no statistically significant difference between the dominant and non-dominant elbow angles in our study. However, a statistically significant difference (p = 0.038) was found between the injured elbow and the intact one in four patients. We considered it important to have a statistically significant difference although our follow-up period was short and the number of cases was small.
As a result of growth plate deformity on the distal end of humerus, the elbow carrying angles may change [26]. Cubitus valgus deformity mostly occurs due to nonunion of lateral condylar physeal fractures [3]. Even though our patients had no osseous problems, cubitus valgus deformity developed. There is restricted data on this subject in the literature.
There was no soft tissue or bony problems on the MRI of their injured elbow taken during the last follow-up. Although there was not any problem clinically or radiologically, the cubitus valgus was developed in some patients' elbows. It could be a sequelae from growth stimulation of the medial condylus after the dislocation.
Since there is a natural valgus angle present in the elbow, cubitus valgus deformity can be cosmetically tolerated. Most cubitus valgus deformities are not clinically problematic. But the increase in elbow carrying angle seems to be an independent factor of ulnar neuropathy that develops in the absence of trauma [19]. No neurologic problem was observed in our patients during their final control.
In cases where valgus angle shows an extreme increase associated with symptoms, corrective osteotomy may be performed, although seen rarely. None of our patients developed any severe deformity that required surgical intervention.
In conclusion, although isolated traumatic dislocation of the elbow is uncommon among children, it can be successfully treated by urgent closed reduction, proper fixation of the elbow and proper and timely rehabilitation.
Functionally we obtained satisfactory outcomes in our patients. We believe that all dislocations being closed, lack of any accompanying fractures around the elbow, timely initiation of proper rehabilitation, and non-development of myositis ossificans had a positive impact on our outcomes.
However, cubitus valgus deformity is one of the problems that develops in a later period disturbing the parents. The patient and the parents should be informed of the potential for any deformity development. Since it occurs more frequently than what is estimated, we believe that it must be clearly indicated in the consent form after the intervention in order to avoid any legal issues in the future.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Herring JA (2002) Upper extremity injuries. In: Tachdjian‘s pediatric orthopaedics. Vol. 3, 3rd ed. Philadelphia: W.B. Saundersp. 2191-2194
- 2.Park CP, Ahmad CS. Dynamic contributions of the flexor-pronator mass to elbow valgus stability. J Bone Joint Surg. 2004;86-A:2268. doi: 10.2106/00004623-200410000-00020. [DOI] [PubMed] [Google Scholar]
- 3.Wilkins KE. Fractures and dislocations of the elbow region. In: Rockwood CA, Wilkins KE, King RE, editors. Fractures in children 4th. Philadelphia: Lippincott-Raven; 1996. pp. 600–887. [Google Scholar]
- 4.Balasubramanian P, Madhuri V, Muliyil J. Carrying angle in children: a normative study. J Pediatr Orthop B. 2006;15:37–40. doi: 10.1097/01202412-200601000-00008. [DOI] [PubMed] [Google Scholar]
- 5.An KN, Chao EY. Functional evaluation of the elbow. In: Morrey BF, editor. The elbow and its disorders. 2. Philadelphia: Saunders; 1993. pp. 85–97. [Google Scholar]
- 6.Hildebrand KA, Patterson SD, King GJ. Acute elbow dislocations: simple and complex. Orthop Clin North Am. 1999;30(1):63–79. doi: 10.1016/S0030-5898(05)70061-4. [DOI] [PubMed] [Google Scholar]
- 7.Yilmaz E, Karakurt L, Belhan O, Bulut M, Serin E, Avci M. Variation of carrying angle with age, sex, and special reference to side. Orthopedics. 2005;28:1360–1363. doi: 10.3928/0147-7447-20051101-16. [DOI] [PubMed] [Google Scholar]
- 8.Spinner RJ, O’Driscoll SW, Davids JR, Goldner RD. Cubitus varus associated with dislocation of both the medial portion of the triceps and the ulnar nerve. J Hand Surg Am. 1999;24:718–726. doi: 10.1053/jhsu.1999.0718. [DOI] [PubMed] [Google Scholar]
- 9.Godfarb CA, Patterson JM, Sutter M, Krauss M, Steffen JA, Galatz L. Elbow radiographic anatomy: measurement techniques and normative data. Shoulder Elbow Surg. 2012;21(9):1236–1246. doi: 10.1016/j.jse.2011.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chein-Wei Chang MD, Yi-Chian Wang MD, Chang-Hung Chu MD. Increased carrying angle is a risk factor for nontraumatic ulnar neuropathy at the elbow. Clin Orthop Relat Res. 2008;466:2190–2195. doi: 10.1007/s11999-008-0308-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bulut G, Erken HY, Tan E, Ofluoğlu O, Yıldız M. Treatment of medial epicondyle fracturs accompanying elbow dislocations in children. Acta Orthop Traumatol Turc. 2005;39(4):334–340. [PubMed] [Google Scholar]
- 12.De Haan J, Schep NW, Zengerink I, van Buijtenen J, Tuinebreijer WE, den Hartog D. Dislocation of the elbow: a retrospective multicentre study of 86 patients. Open Orthop J. 2010;17(4):76–79. doi: 10.2174/1874325001004020076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Durakbasa O, Küçükyazici O, Tuygun H, Okan N, Görgeç M. Surgical treatment of elbow fracture–dislocations seen in children and adolescents. Acta Orthop Traumatol Turc. 2003;37(4):304–308. [PubMed] [Google Scholar]
- 14.O’Driscoll SW, Morrey BF, Korinek S, An KN. Clin Orthop Relat Res. 1992;280:186–197. [PubMed] [Google Scholar]
- 15.Jockel CR, Katolik LI, Zelouf DS. Simple medial elbow dislocations: a rare injury at risk for early instability. J Hand Surg Am. 2013;38(9):1768–1773. doi: 10.1016/j.jhsa.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 16.Carlioz H, Abols Y. Posterior dislocation of the elbow in children. J Pediatr Orthop. 1984;4(1):8–12. doi: 10.1097/01241398-198401000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Josefsson PO, Johnell O, Gentz CF. Long-term sequelae of simple dislocation of the elbow. J Bone Joint Surg Am. 1984;66(6):927–930. doi: 10.2106/00004623-198466060-00014. [DOI] [PubMed] [Google Scholar]
- 18.Rasool MN. Dislocations of the elbow in children. J Bone Joint Surg Br. 2004;86(7):1050–1058. doi: 10.1302/0301-620X.86B7.14505. [DOI] [PubMed] [Google Scholar]
- 19.Michelsson JE, Rauschning W. Pathogenesis of experimental heterotopic bone formation following temporary forcible exercising of immobilized limbs. Clin Orthop Relat Res. 1983;176:265–272. [PubMed] [Google Scholar]
- 20.De Haan J, Schep NW, Tuinebreijer WE, Patka P, den Hartog D. Simple elbow dislocations: a systematic review of the literature. Arch Orthop Trauma Surg. 2009;130:241–249. doi: 10.1007/s00402-009-0866-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mehlhoff TL, Noble PC, Bennett JB, Tullos HS. Simple dislocation of the elbow in the adult. Results after closed treatment. J Bone Joint Surg. Am. 1988;70(2):244–249. [PubMed] [Google Scholar]
- 22.De Haan J, Schep NW, Zengerink I, van Buijtenen J, Tuinereijer WE, den Hartog D. Dislocation of the elbow: a retrospective multicentre study of 86 patients. Open Orthop J. 2010;17(4):76–79. doi: 10.2174/1874325001004020076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lieber J, Zundel SM, Luithle T, Fuchs J, Kirschner HJ. Acute traumatic posterior elbow dislocation in children. J Pediatr Orthop B. 2012;21(5):474–481. doi: 10.1097/BPB.0b013e328354b08c. [DOI] [PubMed] [Google Scholar]
- 24.Herring JA (2002) Tachdjian’s Pediatric Orthopaedics. Vol 3. 3rd ed. Philadelphia, Pa: WB Saunders Co 2164-2168
- 25.Tükenmez M, Demirel H, Perçin S, Tezeren G. Measurement of the carrying angle of the elbow in 2,000 children at ages six and fourteen years. Acta Orthop Traumatol Turc. 2004;38(4):274–276. [PubMed] [Google Scholar]
- 26.Jain AK, Dhammi IK, Arora A, Singh MP, Luthra JS. Cubitusvarus: problem and solution. Arch Orthop Trauma Surg. 2000;120:420–425. doi: 10.1007/s004029900102. [DOI] [PubMed] [Google Scholar]