Abstract
Purpose
The treatment of elderly KBD knee remains a significant clinical challenge, and clinical data are lacking. This study aimed to prospectively determine the functional outcomes of total knee arthroplasty (TKA) in adult patients with severe Kashin-Beck disease (KBD) of the knee.
Method
Fifteen cases that included 18 occurrences of KBD of the knee were treated by primary knee arthroplasty and followed up for at least two years. Clinical assessments for each patient were performed at time zero (pre-operatively), one, three, six and 12 months and yearly thereafter. The efficacy measures included the visual analogue scale (VAS) pain score, Hospital for Special Surgery (HSS) score, and Functional Score for Adult Tibetans with Kashin-Beck Disease (FSAT-KBD) as well as radiographic findings.
Results
All patients were followed for a mean length of 32.47±10.05 months. All force lines in the lower limbs had been improved significantly. No radiographic evidence of loosening or changes in component positioning was observed at the last follow up. The VAS decreased significantly during the first six months after surgery and was maintained until the last follow up (p < 0.01). Similar trends were found in both HSS and FSAT-KBD, which increased significantly post-operatively (p < 0.01).
Conclusion
Knee arthroplasty can reduce pain and improve function in patients with severe KBD of the knee. Additional studies will be necessary to confirm our findings.
Keywords: Kashin–Beck disease, Arthroplasty, Knee
Introduction
Kashin-Beck disease (KBD) is a chronic disease endemic to China, Siberia and North Korea [1]. The primary clinical symptoms of KBD in the elderly include symmetrical multiple joint pain, enlarged and shortened fingers, and deformed, enlarged joints with limited motion in the extremities, along with a high rate of late-stage disability [2, 3]. The degree of knee and elbow pain is relatively more serious than that of shoulders, hips, wrists and ankles, with the knee being the joint most seriously affected [4]. As a result, pain and functional limitations of the knee are usually the main factors affecting the lives and abilities of KBD patients [5].
The treatment of KBD in the elderly remains a significant clinical challenge, and clinical data for this disease are lacking. Current treatment options are mainly derived from experiences in the area of osteoarthritis (OA) treatment [6]. Non-steroidal anti-inflammatory drugs (NSAIDs) and other analgesics have been found to provide predictable and sustained relief from pain in elderly KBD patients but did little to improve joint function [7]; moreover, the gastrointestinal and cardiovascular risks associated with NSAIDs often limit their long-term use in many elderly patients [8]. Intra-articular injections of hyaluronic acid have been shown to provide good pain relief in the early and middle stages of KBD, but the relief is poor in patients whose KBD has progressed to severe damage and deformity [9–11]. Physical therapy can relieve pain and improve mobility, thereby improving the functional and even the socioeconomic status of KBD patients [12], but KBD requires long-term treatment to achieve results. No data are available regarding the degree to which physical therapy may improve the function of severe knee KBD that has progressed to deformity. Osteotomy with impaction can correct the initial angular deformities and improve the function of lower limbs in KBD patients [13], but it’s more suitable for young and middle-aged KBD patients with deformities in limbs than elderly KBD patients with severe articular cartilage degeneration.
Total knee arthroplasty (TKA) is one of the most effective surgical procedures for improving physical function and relieving pain in patients with severe osteoarthritis (OA) of the knee. National TKA registries report survival rates of nearly 95 % at ten years and just below 90 % at 20 years in patients with OA [14, 15]. These good results after TKA are also achieved in most patients with severe OA [16–18]. Few studies have reported clinical data on TKA in patients with advanced stage KBD of the knee. In this prospective study, we evaluated the efficacy of TKA for the treatment of elderly knee KBD patients with Kellgren–Lawrence radiographic grade IV [19] and provide clinical evidence for further treatment of KBD of the knee.
Patients and methods
This study was undertaken at the Department of Orthopaedic Surgery at West China Hospital, Sichuan University. It was approved by the Human and Ethics Committee for Medical Research at Sichuan University in accordance with the Helsinki Declaration. Informed consent was obtained for all patients prior to their inclusion in the study.
We reported on 15 patients (18 knees) who underwent TKA between 2008 and 2011 and were followed for an average of more than two years postoperatively. The detailed data on the 15 cases are shown in Table 1. All patients were from Aba Prefecture, Sichuan Province, China, where the average prevalence of KBD among adults was 41.0 %, according to a recent investigation [20]. At the time of screening, patients underwent a medical history evaluation; complete physical examination, including laboratory assessments; and examination of the target knee and other affected joints and radiographs including the target knee and AP-view long-leg films. The clinical diagnosis of KBD was performed by at least two senior orthopaedic surgeons from the Orthopaedics Department or by senior physicians from the Rheumatology Department at West China Hospital, West China Medical School, Sichuan University, based on previously described clinical criteria [21, 22]. The diagnostic grade criteria for grading were as follows: grade I, multiple symmetrical joint enlargement of fingers or other limbs, usually accompanied by slight muscular atrophy and pain; grade II°, worse symptoms than a grade I patient, usually with significant enlargement of interphalangeal joints and shortened fingers; and grade III, progression from a grade II patient, usually with significant dystrophie limbs or dwarfism.
Table 1.
Clinical features of the 15 patients
| Case | Age(years)/sex | Side (R/L) | KBD grade | NBJLI (n) | BMI (kg/m2) | Disease duration(years) | Varus angle (°) before surgery | Follow-up period (months) | Complications after surgery |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 57/F | R | II | 6 | 28.48 | 8 | 9.0 | 29 | None |
| 2 | 63/F | R | II | 6 | 19.95 | 15 | 5.5 | 29 | None |
| 3 | 69/F | R | I | 4 | 18.75 | 23 | 16.8 | 62 | None |
| 4 | 74/F | R | I | 8 | 24.22 | 9 | 12.5 | 42 | None |
| 5 | 55/F | L | I | 6 | 29.30 | 20 | 13.7 | 32 | None |
| 6 | 61/F | R/L | II | 10 | 23.93 | 30 | 12.5/9.8 | 28 | None |
| 7 | 66/M | L | I | 8 | 31.49 | 5 | 13.7 | 42 | None |
| 8 | 80/F | R | I | 8 | 24.56 | 40 | 2.5 | 26 | Onea |
| 9 | 64/F | L | III | 6 | 26.41 | 10 | 9.9 | 24 | None |
| 10 | 76/F | R/L | I | 8 | 27.77 | 6 | 6.6/4.3 | 27 | None |
| 11 | 77/F | R | I | 6 | 25.80 | 20 | 2.2 | 32 | None |
| 12 | 65/F | R/L | II | 8 | 27.45 | 22 | 18.8/16.3 | 37 | None |
| 13 | 59/F | R | I | 6 | 20.38 | 7 | 6.2 | 23 | None |
| 14 | 62/M | L | II | 8 | 19.63 | 15 | 3.3 | 28 | None |
| 15 | 67/F | R | I | 10 | 22.46 | 17 | 9.1 | 26 | None |
| Average | 66.33 | 7.2 | 24.71 | 16.47 | 32.47 |
KBD Kashin-Beck disease, BMI body mass index, NBJI the number of big limb joints involved, R right, L left
aThis patient suffered pulmonary infection after the first stage of hip joint replacement, which resolved within one week after extended antibiotic therapy, and the patient then successfully underwent TKA treatment
Patients were considered eligible for inclusion if they were symptomatic for at least six months prior to enrolment, experienced a pain intensity of more than 60 mm on a 100-mm visual analogue pain scale (VAS; 0 mm representing no pain and 100 mm representing severe pain) in the target knee while walking on the floor, were able to walk no more than 200 metres due to knee pain, and had a Kellgren-Lawrence radiographic grade of IV in the target knees. Patients were excluded from the study if they had any unstable medical condition, such as abnormal vital signs, inflammation or infection. These exclusion criteria were based on our experience using TKA in the treatment of OA.
Surgical procedure
Health education was provided to the patients after their hospital admission, and they were then given pre-operative oral analgesics. Patients with medical conditions, such as ischemic heart disease, congestive heart failure, or chronic obstructive airway disease, were seen by a medical specialist or anaesthetist.
TKA under tourniquet was performed on the diseased knees by the two senior total joint replacement surgeons. The knee joint was accessed through a medial parapatellar approach, then osteophytes and intra-articular soft tissues were cleared. Bone cuts in the distal femur were made perpendicular to the mechanical axis with 3° valgus and 4° extorsion angles using an intramedullary alignment system. The proximal tibia was cut perpendicular to the mechanical axis of the tibia with a 3° caster angle using extramedullary alignment rods. The soft tissues around the knee were carefully balanced to allow optimum knee kinematics. Patellofemoral tracking was balanced with trial components in situ and if necessary with a lateral release or medial reefing procedure. Once the definitive components had been selected, they were cemented into place with polymethyl methacrylate cement. The tourniquet was deflated prior to closure to allow adequate haemostasis, a drain was placed, and the leg was dressed in extension.
Of the 18 TKAs, four were performed with spinal anaesthesia combined continuous epidural anaesthesia, five with tracheal intubation plus combined intravenous inhalational anaesthesia, and nine with general anaesthesia combined with a femoral nerve block. Among the 15 cases, three cases of bilateral knee joint involvement were treated with staged TKA procedures performed approximately seven days apart. One case also had severe ipsilateral hip damage and another case had severe contralateral hip damage; these patients underwent hip replacements first, followed by TKA after an interval of approximately seven days. All TKAs were performed with Scorpio (Stryker Howmedica Osteonics, Allendale, NJ) bone cement prosthesis.
Postoperative treatment and rehabilitation program
Intravenous prophylactic antibiotics (cefazolin 2.0 g) were routinely administered 30 minutes pre-operatively and once post-operatively. All patients were given oral NSAIDs or an intramuscular injection of pethidine hydrochloride for pain relief. A quadriceps relaxation process was encouraged after anaesthesia recovery to help prevent venous thrombosis. Drains were usually removed within 24 hours, and the patient was encouraged to walk on the second postoperative day under the guidance of the physical therapist. X-rays were performed after the drains were removed.
Postoperative assessments
Follow-up appointments with clinical and radiographic evaluation were scheduled regularly at two and four weeks and three, six, and 12 months postoperatively and then annually. The radiographic data were assessed every year. During each follow up, all radiographic and/or soft tissue complications were recorded at the review clinics. Clinical efficacy measures were reported by the patients while the radiographic results were analysed by the surgeon.
Outcome measures included complications during perioperative period, VAS scores, Hospital for Special Surgery scores (HSS) [23], Functional Score for Adult Tibetans with Kashin-Beck Disease (FSAT-KBD) [24] and radiographic results at each follow up. The FSAT-KBD scale, developed by orthopaedic experts in our department for the specific lifestyle of Tibetans, is a highly reliable, validated instrument for the assessment of changes in KBD symptoms and disability in Tibet [24]. The FSAT-KBD instrument consists of 12 questions (Table 2). Each question is measured on a four-point categorical scale (1 = impossible/< 100 m/crutches to 4 = no problem/none). The maximum total possible score for the FSAT-KBD is 48, with a minimum possible total FSAT-KBD score of 12.
Table 2.
The functional score for adult Tibetans with Kashin-Beck Disease
| Items | Four-point categorical scale | |||
|---|---|---|---|---|
| Dressing | □ No problem | □ Slight problem | □ Severe problem | □ Impossible |
| Combing | □ No problem | □ Slight problem | □ Severe problem | □ Impossible |
| Making Ciba | □ No problem | □ Slight problem | □ Severe problem | □ Impossible |
| Eating | □ No problem | □ Slight problem | □ Severe problem | □ Impossible |
| Picking cow manure | □ No problem | □ Slight problem | □ Severe problem | □ Impossible |
| Lift the load (>10 kg) | □ No problem | □ Slight problem | □ Severe problem | □ Impossible |
| Hunkering | □ No problem | □ Slight problem | □ Severe problem | □ Impossible |
| Squatting | □ No problem | □ Slight problem | □ Severe problem | □ Impossible |
| Standing | □ No problem | □ Slight problem | □ Severe problem | □ Impossible |
| Up/down ladder | □ No problem | □ Slight problem | □ Severe problem | □ Impossible |
| Walking distance | □ No problem | □ > 2000 m | □ < 500 m | □ < 100 m |
| Support | □ None | □ Single stick | □ Single crutch | □ Crutches |
| 1 = impossible/< 100 m/crutches to 4 = no problem/none | ||||
Statistical analysis
Statistical analyses were conducted with the SPSS Version 16.0 software (SPSS Inc., Chicago, IL, USA). The distributions of all measurement variables were tested with the Kolmogorov-Smirnov test before any other statistical analyses were performed. The continuous data are presented as the mean ± standard deviation (SD). Comparisons of variables between baseline and any endpoint were analysed using the paired-T test when the distribution was normal, otherwise the Wilcoxon signed-rank test was used. A p value less than 0.05 was considered significant and less than 0.01 to be highly significant for all the statistical tests.
Results
Perioperative complications
The mean length of time to walking postoperatively was two days (range, one to three days). Postoperative recovery was uneventful, except for one 80-year-old patient who developed a pulmonary infection after the first stage of hip joint replacement. The infection resolved within one week after extended antibiotic therapy and encouragement to cough and breathe deeply. After resolution of the infection, the patient successfully underwent TKA on the target knee and was discharged in good health five days postoperatively. No wound infections, wound-healing disorders, or deep vein thrombosis were noted.
Clinical efficacy measures
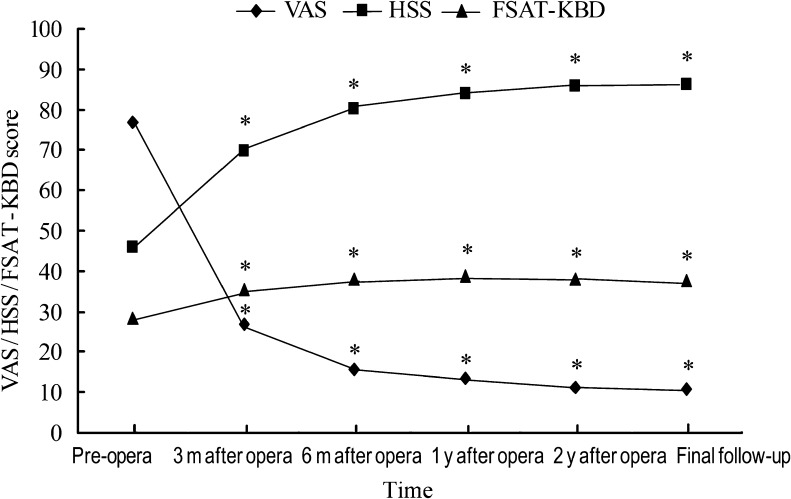
The patients were followed for an average of 32.47 ± 10.05 months. A significant reduction was observed in knee pain score along with a significant improvement in function as measured by VAS, HSS and FSAT-KBD scores after receiving TKA treatment (Fig. 1).
Fig. 1.
The visual analogue scale (VAS), Hospital for Special Surgery (HSS), and Functional Score for Adult Tibetans with Kashin-Beck Disease (FSAT-KBD) scores for each endpoint. * p < 0.001 compared with pre-operation
The VAS score was significantly reduced from 76.94 ± 5.81 mm before surgery to 26.94 ± 5.04 mm three months after TKA (p < 0.01), which continued to decrease to 15.83 ± 4.49 mm at six months postoperatively (p < 0.01 vs. baseline). After six months, the knee pain was almost fully relieved, and this was sustained through the final follow-up (reaching a minimum of 10.83 ± 3.82).
The HSS score was significantly improved from 45.78 ± 7.11 before surgery to 69.94 ± 6.04 three months after TKA (p < 0.01), which continued to increase to 80.17 ± 4.35 at six months postoperatively (p < 0.01 vs. baseline). The HSS score was sustained and reached a peak of 86.33 ± 3.02 at the final follow up. At the final follow up, of the 18 knees treated, 17 rated excellent (80–100) and rated good (70–80), according to the HSS scoring system.
The FSAT-KBD score displayed an astonishingly similar trend to the HSS score, improving from 28.50 ± 3.27 at baseline to 35.56 ± 2.89 three months postoperatively (p < 0.01), which continued to increase to 38.16 ± 2.75 at month 6 (p < 0.01 vs. baseline). The HSS score reached its peak (38.77 ± 2.30) at one year after surgery.
Radiographic assessment
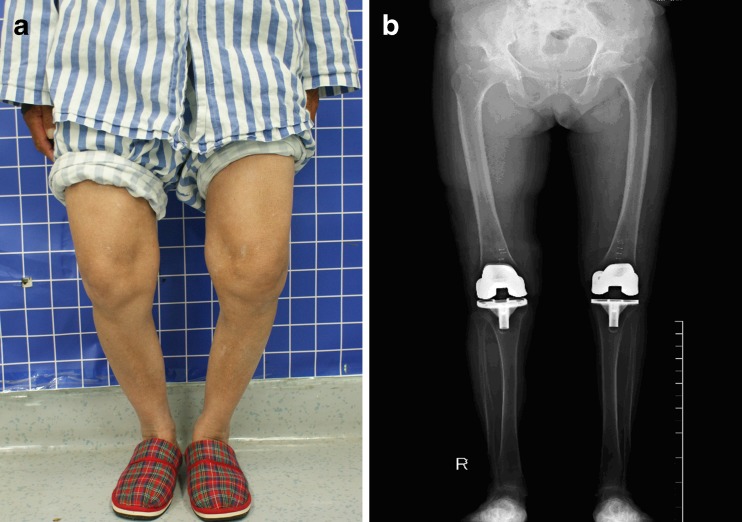
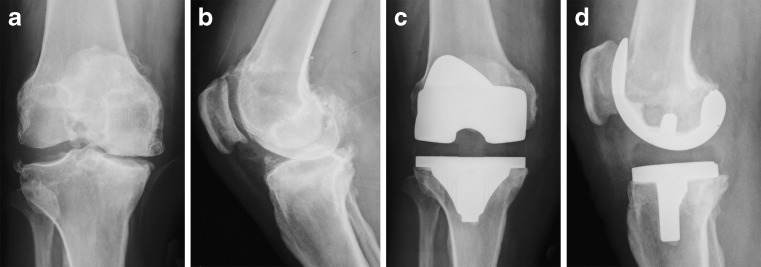
Postoperative X-rays showed that all prosthesis components in the knees were well fixed, and a significant improvement of limb alignments was achieved in all patients (Fig. 2). Long-leg film analysis (Syngo Imaging V31, Siemens AG Medical Solutions, Germany) revealed that the mean value of varus deformity in the coronal plane was adjusted from 9.6° (range 2.2–18.8°) before surgery to 2.4° (range 0.3–6.9°) after TKA. One patient had a valgus angle of 0.9° in the left knee after surgery. There was no radiographic evidence of loosening, change, or fracture in component positioning at the final follow up (Fig. 3).
Fig. 2.
A 65-year-old woman with Kashin-Beck disease (KBD) of the knees. a Both knees with varus and inflexion deformity before total knee arthroplasty (TKA) operation. b Accurate limb alignments were achieved after TKA operation
Fig. 3.
A 69-year-old woman with Kashin-Beck disease (KBD) of the right knee received total knee arthroplasty (TKA). a, b The X-ray film before operation showed the knee joint was characterised by severe joint narrowing, marked osteophyte formation at the joint margin, as well as sclerosis of subchondral bone at the femoral condyle and tibial plateau. c, d Four years after surgery, there was no radiographic evidence of loosening or change in component positioning
Discussion
KBD is a disabling osteoarticular disease involving growth cartilage [25, 26], usually leading to joint damage, pain, deformity and serious limitations in joint motion in the later stages of the disease. Currently, more than one million people, mostly adults, are affected by KBD in an endemic area that spans from southeastern Siberia, crosses northern China, and ends in central Tibet. However, the clinical data regarding treatment of elderly KBD patients are lacking.
Based on our experience treating OA patients, we prospectively evaluated the efficacy of TKA for the treatment of severe knee involvement in elderly KBD patients. We found that TKA could not only significantly relieve the pain of the target knee but could also significantly improve the function of the knee as well as the overall living and working ability. This was supported by the rapidly decreased VAS score and the rapidly improved HSS as well as FSAT-KBD scores six months after TKA. Up to the final follow up, the VAS score was significantly reduced and the HSS and FSAT-KBD scores were significantly increased, suggesting that TKA provides efficacious and long-lasting treatment of knee pain and functional limitations due to KBD.
TKA is one of the most effective surgical procedures for improving physical function and relieving pain in patients with osteoarthritis (OA) of the knee. Even in severe osteoarthritis, good results are achieved in most patients after TKA [16–18]. In our study, all TKAs were performed for severe KBD of the knee with K-L grade IV. However, good clinical results were achieved postoperatively in all patients, and no radiographic evidence of loosening, change, or fracture in component positioning was observed at the final follow up, which is consistent with the above reports [16–18].
Few studies have reported clinical results for TKA in patients with advanced stage KBD of the knee. Yang et al. [27] reported four cases of KBD of the knee in patients that received TKA treatment. The four cases were followed up for 1.5 to five years, with three patients reporting good and one case reporting fair (60–70 points) results, according to HSS scoring. The same team [28] later published (in a retrospective study) the results of an extended series of 23 patients (27 knees) managed with primary TKA with an average of 28 months of follow up. There was no radiographic evidence of loosening, change, or fracture in component positioning at the last follow up. The final HSS score averaged 82.6, and 18 knees (66.67 %) rated excellent, seven knees (25.93 %) rated well and two knees (7.40 %) rated fair, similar to what was observed in our study. The portion that rated excellent and good in our study was higher than the Yang et al. study (100 % vs. 92.6 %), which may be because our department was the centre of joint reconstruction in Southwest China, and has senior surgeons with more experience, standard operating procedures and a more rigorous rehabilitation program after discharge.
Clinically, KBD in the elderly usually exhibits symmetrical multi-joint enlargement, which is sometimes accompanied by muscular atrophy and severe joint distortion [2–4]. These observations were confirmed by the 50 % of KBD patients in our study who had no less than eight joints involved. The scales commonly used for the overall evaluation of limb function mainly include the Rosser Index [29], Barthel Index [30] and the Stanford Health Assessment Questionnaire (HAQ) [31]. However, these function scales were inappropriate for evaluating KBD patients’ limb function as these scales were based on Western and urban residents’ life and work habits, while most KBD patients in the Aba Prefecture in our study lived in mountainous regions and their life and work was mainly based on herding and agriculture[32, 33]. The FSAT-KBD scale, developed by orthopaedic experts in our department, has been validated as a reliable, validated instrument for the assessment of changes in KBD symptoms and disability in Tibet [24]. Therefore, we included the FSAT-KBD as a second measure of daily living and working ability in the rehabilitation process after TKA. This study showed that the FSAT-KBD score increased three to six months after TKA, with a similar trend in HSS score, suggesting that TKA can rapidly improve the overall function of limbs. The slight reduction after one year could be explained by the fact that the conditions of other joints worsen over time, which has been reported in another study [4].
The limited number of patients enrolled in this study precludes any definitive conclusion about the efficacy of TKA for treating KBD of the knee. That may be ascribed to the following factors. First, the study was suspended from 2008 to 2009 under difficult circumstances due to the Wenchuan great earthquake in May of 2008. Second, due to limited resources at the sites where this study was conducted, not all patients in the area were able to undergo TKA treatment. However, to our knowledge, this study includes the largest sample size and the longest follow up among all prospective research for evaluating TKA in the treatment of severe KBD of the knees. Because of the limitations of our open-label and small sample size study, other larger randomised, long-term, prospective studies are needed to confirm our findings.
Conclusion
Considering the promising results of this study, TKA can be regarded as useful for the treatment of severe KBD of the knee and is associated with good to excellent clinical and radiographic outcomes in short-term follow up. More extensive studies are needed to confirm the findings of our study.
Acknowledgments
This research was funded by the China National Science & Technology Pillar Program during the eleventh 5-year plan period (2007BAI 25B04). The authors would like to thank the local government in Aba Prefecture for their support and cooperation in the collection of data.
Conflict of interest
The authors declare that they have no conflicts of interest.
Contributor Information
Zong-Ke Zhou, Email: zongke@126.com.
Fu-Xing Pei, Email: peifuxing@vip.163.com.
References
- 1.Hinsenkamp M. Editorial: Kashin-Beck disease. Int Orthop. 2001;25(3):133. doi: 10.1007/s002640000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schepman K, Engelbert RH, Visser MM, et al. Kashin Beck disease: more than just osteoarthrosis: a cross-sectional study regarding the influence of body function—structures and activities on level of participation. Int Orthop. 2011;35:767–776. doi: 10.1007/s00264-010-1043-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hinsenkamp M, Rippens F, Begaux F, et al. Anatomic distribution of radiographic abnormalities in Kashin-Beck disease. Int Orthop. 2001;25(3):142–146. doi: 10.1007/s002640100236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Y, Zhou Z, Shen B, et al. Clinical features of Kashi-Beck disease in adults younger than 50 years of age during a low incidence period: severe elbow and knee lesions. Clin Rheumatol. 2013;32:317–324. doi: 10.1007/s10067-012-2115-0. [DOI] [PubMed] [Google Scholar]
- 5.Zhou Z, Shen B, Pei F, et al. Relation between affected big joints and classification of Kashin–Beck disease in adult of Tibet (Article in Chinese) Chin J Bone Joint Surg. 2009;2:352–356. [Google Scholar]
- 6.Yang J. The discussion on the mediation for adult Kashin-Beck disease (Article in Chinese) Chin J Endemiol. 2005;24:87–90. [Google Scholar]
- 7.Luo R, Liu G, Liu W, et al. Efficacy of celecoxib, meloxicam and paracetamol in elderly Kashin-Beck disease (KBD) patients. Int Orthop. 2011;35:1409–1414. doi: 10.1007/s00264-010-1062-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bjordal JM, Ljunggren AE, Klovning A, et al. Non-steroidal anti-inflammatory drugs, including cyclo-oxygenase-2 inhibitors, in osteoarthritic knee pain: meta-analysis of randomised placebo controlled trials. BMJ. 2004;329:1317. doi: 10.1136/bmj.38273.626655.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu P, Guo X, Jin W, et al. Curative effects of intra-articular injections of sodium hyaluronate to treat Kashin–Beck disease (Article in Chinese) Chin J End. 2004;23:588–590. [Google Scholar]
- 10.Yu Y, Guo D, Huang L, et al. Intra-articular injections of solium hyaluronicfor treating Kashin-beck knee (Article in Chinese) Chin J Ctrl Endem Dis. 2011;26:185–187. [Google Scholar]
- 11.Tang X, Pei FX, Zhou ZK, et al. A randomized, single-blind comparison of the efficacy and tolerability of hyaluronate acid and meloxicam in adult patients with Kashin-Beck disease of the knee. Clin Rheumatol. 2012;31:1079–1086. doi: 10.1007/s10067-012-1979-3. [DOI] [PubMed] [Google Scholar]
- 12.Mathieu F, Suetens C, Begaux F, et al. Effects of physical therapy on patients with Kashin-Beck disease in Tibet. Int Orthop. 2001;5:191–193. doi: 10.1007/s002640000206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu F, Wang Z, Hinsenkamp M. Knee osteotomy in 195 advanced cases of Kashin-Beck disease. Int Orthop. 1998;22:87–91. doi: 10.1007/s002640050215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knutson K, Robertsson O (2010) The Swedish Knee Arthroplasty Register (www.knee.se). Acta Orthop 81:5–7 [DOI] [PMC free article] [PubMed]
- 15.Paxton EW, Furnes O, Namba RS, et al. Comparison of the Norwegian knee arthroplasty register and a United States arthroplasty registry. J Bone Joint Surg Am. 2011;93(Suppl 3):20–30. doi: 10.2106/JBJS.K.01045. [DOI] [PubMed] [Google Scholar]
- 16.Carr AJ, Robertsson O, Graves S, et al. Knee replacement. Lancet. 2012;379:1331–1340. doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 17.Stroh DA, Delanois R, Naziri O, et al. Total knee arthroplasty in patients over 80 years of age. J Knee Surg. 2011;24:279–283. doi: 10.1055/s-0031-1284729. [DOI] [PubMed] [Google Scholar]
- 18.Hamel MB, Toth M, Legedza A, et al. Joint replacement surgery in elderly patients with severe osteoarthritis of the hip or knee: decision making, postoperative recovery, and clinical outcomes. Arch Intern Med. 2008;168:1430–1440. doi: 10.1001/archinte.168.13.1430. [DOI] [PubMed] [Google Scholar]
- 19.Kellgren JH, Lawrence JS. Radiographic assessment of osteoarthritis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li F, Deng J, Zhou D, et al. Analysis on monitoring data of Kashin-Beck disease in Sichuan Province in 2005 (Article in Chinese) J Prev Med Inf. 2005;21:666–668. [Google Scholar]
- 21.Guo X. Diagnostic, clinical and radiological characteristics of Kashin Beck disease in Shaanxi Province, PR China. Int Orthop. 2001;25:147–150. doi: 10.1007/s002640100248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mathieu F, Begaux F, Lan ZY, et al. Clinical manifestations of Kashin–Beck disease in Nyemo Valley, Tibet. Int Orthop. 1997;21:151–156. doi: 10.1007/s002640050139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Insall JN, Ranawat CS, Aglietti P, et al. A comparison of four models of total knee replacement prostheses. J Bone Joint Surg Am. 1976;58:754–765. [PubMed] [Google Scholar]
- 24.Huang Q, Zhou Z, Shen B, et al. The primary validation study of Kashin-Beck Disease affected big joints function assessing system for adult Tibetans in Rangtang County (Article in Chinese) Chin J Evid-based Med. 2010;10:1041–1044. [Google Scholar]
- 25.Pasteels JL, Fu-De L, Hinsenkamp M, et al. Histology of Kashin-Beck lesions. Int Orthop. 2001;25:151–153. doi: 10.1007/s002640000190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zheng J, Wu C, Ma W, et al. Abnormal expression of chondroitin sulphate N-acetylgalactosaminyltransferase 1 and Hapln-1 in cartilage with Kashin-Beck disease and primary osteoarthritis. Int Orthop. 2013;37:2051–2059. doi: 10.1007/s00264-013-1937-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang L, Tu Z, Zhou J, et al. Surgical treatment on adult Kaschin-Beck disease (article in Chinese) Chin J Joint Surg (electronic edition) 2009;3:33–35. [Google Scholar]
- 28.Yang L, Gao D, Tu Z, et al. Stabilized prosthesis after total knee arthroplasty for the adult Kaschin-Beck disease with mixed deformities (article in Chinese) Chin J Bone Joint Surg. 2009;3:33–35. [Google Scholar]
- 29.Rosser R, Watts V. The measurement of hospital output. Int J Epidemiol. 1972;1:361–368. doi: 10.1093/ije/1.4.361. [DOI] [PubMed] [Google Scholar]
- 30.Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 31.Bruce B, Fries JF. The Stanford Health Assessment Questionnaire: a review of its history, issues, progress, and documentation. J Rheumatol. 2003;30:167–178. [PubMed] [Google Scholar]
- 32.Hinsenkamp M, Mathieu F, Claus W, et al. Effects of physical environment on the evolution of Kashin-Beck disease in Tibet. Int Orthop. 2009;33:1085–1088. doi: 10.1007/s00264-009-0738-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Malaisse F, Haubruge E, Mathieu F, et al. Ethno-agricultural approach to the rural environment in the prevention of Kashin-Beck disease. Int Orthop. 2001;25:170–174. doi: 10.1007/s002640000215. [DOI] [PMC free article] [PubMed] [Google Scholar]