Abstract
Purpose
Arthroscopic lateral clavicle resection (LCR) is increasingly used, compared to an open approach, but literature does not clearly indicate which approach is preferable. The goal of this study was to compare function and pain between patients who underwent lateral clavicle resection using an open approach and patients treated using an arthroscopic approach.
Methods
Patients who underwent LCR between January 2008 and December 2011 were reviewed. After exclusion, 149 shoulders (143 patients) were eligible for analysis: 41 open and 108 arthroscopic. Disabilities of arm, shoulder and hand (DASH) questionnaire and visual analogue scale (VAS) score were used to assess shoulder function and pain. Complications, operative time, length of hospitalization and resection distance were compared.
Results
At a mean follow-up of three years, patients in the open group had significantly less pain by VAS (mm) (Mdn 10, IQR 23) compared with arthroscopic patients (Mdn 20, IQR 50) (p = 0.036). Operative time (minutes) was significantly less for the open approach (Mdn 24.0, IQR 12) compared with arthroscopic (Mdn 38.0, IQR 15) (p < 0.001). Resection distance (mm) was larger for the open approach (Mdn 7.1, IQR 7.0) compared with the arthroscopic approach (Mdn 3.2, IQR 3.1) (p = 0.006), but was not associated with outcome. No significant differences were found for DASH score, complication rate or length of hospitalization.
Conclusions
Both arthroscopic and open approaches for LCR provide excellent outcome in patients with acromioclavicular pain. Less residual pain was found for the open approach, which has shorter operating time and is likely more cost effective.
Keywords: Arthroscopic, Open, Resection, Acromioclavicular, Clavicle
Introduction
Lateral clavicle resection (LCR) is a generally accepted and effective surgical procedure, predominantly performed for symptomatic acromioclavicular (AC) osteoarthritis, but also for osteolysis and symptomatic posttraumatic changes of the acromioclavicular joint (ACJ) [1]. Over the last decade a transition has occurred from the use of an open to an arthroscopic approach [2]. This transition may partly be explained by the likeliness of acromioclavicular instability after open resection due to excessive resection of the clavicle or capsular damage [3, 4]. Besides, a trend towards using minimal invasive surgery is seen in general [2].
So far, few studies on patient-related outcomes comparing these approaches have been published, all showing excellent results in function and pain for both approaches [5–9]. Although one study found a better pain score outcome in favour of an arthroscopic approach [8], no relevant differences were found in other studies [5–7, 9]. Thus, a preferable approach based on patient-related outcome measures can, so far, not be determined [5–8]. When both surgical interventions prove to have similar outcome, a future shift towards the least expensive procedure can be expected, because in times of economic recession, budget cuts are demanded while quality of treatment must be maintained.
The objective of the present study was to compare function and pain of patients with acromioclavicular pain that underwent lateral clavicle resection using an open approach with patients treated using an arthroscopic approach. Secondary objectives were to compare operation time, duration of hospitalization, occurrence of complications and resection distance. We hypothesize that there is no difference in patient-related outcome measures.
Patients and methods
Study design and study population
A retrospective cohort study was combined with a cross-sectional questionnaire survey (level of evidence III). All patients who underwent excision of the lateral clavicle for acromioclavicular pain in the period January 2008 to December 2011 in our hospital were liable for inclusion. Exclusion criteria were age under 18 years, previous surgery on the same shoulder, preoperative diagnosis of glenohumeral osteoarthritis and simultaneous adjuvant procedures other than caudal acromioplasty during surgical intervention.
Procedure
The institution’s database was searched for patients who underwent excision of the lateral clavicle using an open or arthroscopic procedure between January 2008 and December 2011. The patient files were requested for retrospective analysis. Objective outcome variables available in the patient files were extracted. All patients were informed about the proposed study by letter and invited to participate. Instructions and information about the study were included, along with a questionnaire and reply envelope. If patients rejected participation, they were asked to return the blank questionnaire along with the arguments for rejection. If no reply was received or no arguments for rejection were included in the reply, patients were contacted by telephone to identify the reason for rejection.
Surgical procedure
In the open approach, an incision is made over the AC joint, after which the deltopectoral fascia and anterior deltoid origin are dissected and taken down. The dissection should be limited to that necessary to expose the bone for resection. The superior AC joint ligament is incised and elevated subperiosteally, so that continuity of its posterior half and the posterior AC joint capsule are preserved, which are the primary restraints to posterior subluxation at the ACJ [10–12]. Enough bone is removed so that the tip of an index finger can be placed in the newly created AC space without impingement on cross-arm abduction.
The indirect arthroscopic approach is performed using posterior, anterior and midlateral portals. Caudal acromioplasty is performed based on pre-operative clues of impingement, intra-operative findings in the subacromial space or the need to create space in order to visualize the ACJ. A needle is placed into the joint from above to localize the ACJ arthroscopically. Electrocautery is used to incise the inferior capsule and to demarcate the distal clavicle from anterior to posterior. Care is taken to avoid disturbance of the superior ACJ capsule and ligaments. A burr is used to shave the clavicle beginning inferiorly. The bone is resected until the surgeon believes the appropriate amount is removed; this is approximately half a centimeter, although the amount of resection is not measured. By viewing from the other portals the sufficient amount of resection is confirmed.
Dependent variables
Shoulder function was assessed using the disabilities of arm, shoulder and hand (DASH) questionnaire, which was found to be reliable and valid in Dutch [13]. Scores range from 0 to 100, and a higher score indicates greater disability. Pain in the preceding week was assessed by visual analogue scale (VAS) (0–100 mm, 0 being no pain, and 100 maximum pain). Secondary outcome measures were extracted from the patient files: wound infection, postoperative bleeding, bony regrowth in the operation site, acromioclavicular joint instability, postoperative frozen shoulder, re-operation of the AC joint, length of hospitalization and operative time. The AC distance on the preoperative (anterior posterior) radiograph of the clavicle was measured between the two closest visual bone structures of the acromion and clavicle, in millimeters. Where available, postoperative AC distance was also measured between the two closest points to quantify the amount of resection. Measurements were made by two of the authors (ND and JK) on digital preoperative radiographs of the ACJ, with the built-in measurement tools of the institution’s radiography software (Agfa IMPAX 6.0, Agfa-Gevaert, Belgium). Postoperative measurements were made in a similar fashion. An interobserver reliability analysis was not performed.
Independent variables
Age and sex of the subjects were available in the institution’s database. Body mass index (BMI) at the time of the operation was extracted from the patient files if available. If not, the current BMI was used, obtained as part of the questionnaire. For the occurrence of prior trauma, the period from initial contact for the shoulder symptoms until the day of surgery was screened for a mentioned trauma as noted by the attending orthopedic surgeon or resident. To determine the dominant side, a question was included in the questionnaire. Any adjuvant procedures were extracted from the operative report, including cuff repair, biceps tendon tenodesis or tenolysis, labral repair, removal of a corpus liberum and excision of a tendon calcification in the arthroscopic group. In the open group adjuvant procedures included diagnostic arthroscopy and rotator cuff repair. Caudal acromioplasty as an adjuvant procedure was included in all groups. The confounding effect of concomitant pathology was minimized by excluding all other adjuvant surgical procedures.
Statistical analysis
Age, BMI, length of hospitalization, operation time, follow-up period, VAS score and DASH score were checked for normality by exploring z-values for skewness and kurtosis, histograms, Q-Q plots, box plots and the results of the Kolmogorov-Smirnov test for the open and arthroscopic groups separately. For normally distributed variables mean and standard deviation (SD) were determined, while for not normally distributed variables median and interquartile range (IQR) were determined. The variables that were not normally distributed were log-transformed. If they appeared normally distributed after transformation, further parametric analyses were performed using the log-transformed values. For the variables that were not normally distributed after transformation, further analysis was performed using a non-parametric test. Age and follow-up period appeared normally distributed; BMI, operative time and pre- and postoperative AC distance appeared so after being log-transformed. Non-parametric tests were necessary for DASH score, VAS score, length of hospitalization and resection distance. Chi-square tests were performed for dichotomous and categorical variables as the occurrence of complications and re-operation of the acromioclavicular joint. Statistical analyses were performed with IBM SPSS Statistics 20.0 (IBM Corporation, Armonk, NY, USA) and p < 0.05 was accepted as being significant.
Results
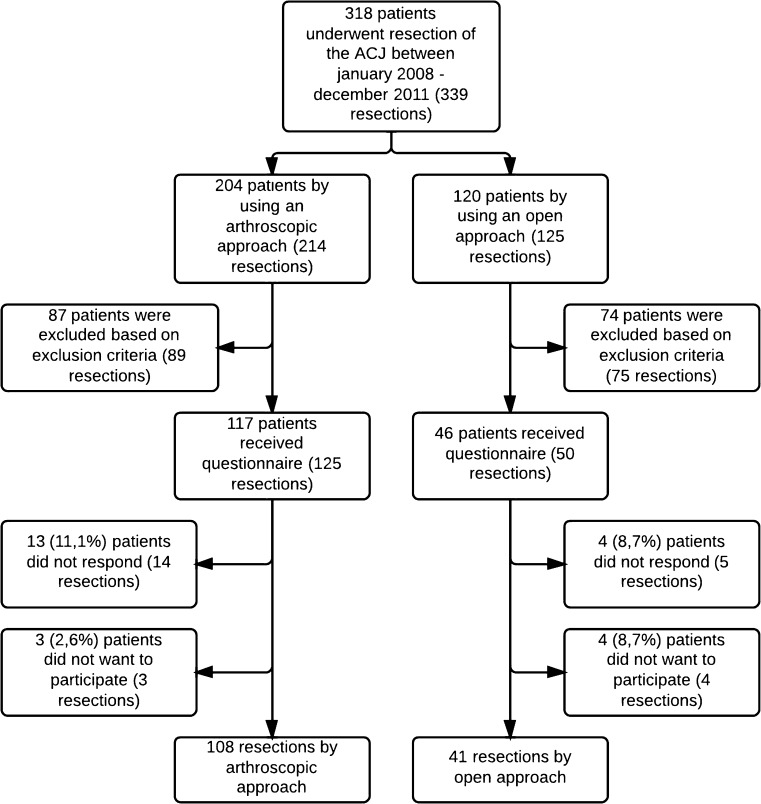
In the three-year period, 318 patients were eligible for inclusion. After exclusion, 143 patients remained, totalling 149 shoulders in the group (Fig. 1). Non-response analysis showed no significant differences in gender, age, BMI and the occurrence of preoperative trauma between the patients that did and did not respond.
Fig. 1.
Patient selection
Overall, the mean follow-up was 2.8 (SD 1.0) years for the arthroscopic group and 3.6 (SD 1.0) years in the open group and was significantly different (p < 0.001). Patient characteristics were comparable between the two approaches (Table 1).
Table 1.
Patient characteristics for both approaches
| Characteristic | Arthroscopic approach | Open approach | p-value |
|---|---|---|---|
| Total (n) | 108 | 41 | |
| Male | 40 (37.0 %) | 15 (36.6 %) | 0.959 |
| Dominant side | 55 (50.9 %) | 22 (53.7 %) | 0.766 |
| Smoker | 29 (27.1 %) | 13 (32.5 %) | 0.519 |
| Preoperative trauma | 15 (13.9 %) | 5 (12.2 %) | 0.857 |
| Age (mean and SD) | 53.8 (9.8) | 53.1 (9.2) | 0.694 |
| BMI (median and IQR) | 25.0 (5.0) | 26.0 (6.0) | 0.443 |
SD standard deviation, BMI body mass index, IQR interquartile range
When looking at the primary outcome variables, no significant differences in DASH score were observed. VAS score at final follow-up was significantly higher for the arthroscopic group (20 mm, compared to 10 mm in the open group). With respect to the secondary outcome variables, length of resection was larger (7.1 mm compared to 3.2 mm) and operative time was less (24 compared to 38 minutes) for the open approach. The percentage of caudal acromioplasties performed was significantly higher in the arthroscopically treated group (93.5 %, versus 24.4 % in the open group, p < 0.001). The number of complications and length of hospitalization were not significantly different (Table 2).
Table 2.
Primary and secondary outcome variables for both approaches
| Characteristic | Arthroscopic approach | Open approach | p-value |
|---|---|---|---|
| Total (n) | 108 | 41 | |
| Adjuvant acromioplasty | 101 (93.5 %) | 10 (24.4 %) | <0.001 |
| Primary outcome variables | |||
| DASH score (median and IQR) | 22.0 (41) | 21.0 (33) | 0.165 |
| VAS (median and IQR) in mm | 20 (50) | 10 (23) | 0.036 |
| Secondary outcome variables | |||
| Complication | 11 (10.2 %) | 3 (7.3 %) | 0.592 |
| Frozen shoulder | 9 (8.3 %) | 1 (2.4 %) | 0.199 |
| Postoperative bleeding | 1 (0.9 %) | 0 (0.0 %) | 0.536 |
| Surgical site infection | 1 (0.9 %) | 2 (4.9 %) | 0.127 |
| Bony regrowth | 0 (0.0 %) | 0 (0.0 %) | |
| Instability | 0 (0.0 %) | 0 (0.0 %) | |
| Re-surgery | 4 (3.7 %) | 1 (2.4 %) | 0.702 |
| Preoperative distance (with postoperative radiograph) (median and IQR) in mm | 1.7 (1.1) (n = 41) | 2.4 (2.0) (n = 15) | 0.092 |
| Postoperative distance (median and IQR) in mm | 5.4 (3.25) (n = 41) | 10.1 (5.30) (n = 15) | 0.001 |
| Length of resection (median and IQR) in mm | 3.2 (3.10) (n = 41) | 7.1 (7.00) (n = 15) | 0.006 |
| Operative time (median and IQR) in minutes | 38.0 (15) | 24.0 (12) | <0.001 |
| Hospitalization (median and IQR) in days | 1.00 (1.00) | 2.00 (1.00) | 0.270 |
DASH disabilities of arm, shoulder and hand questionnaire, IQR interquartile range, VAS visual analog scale
Interpretation
The aim of this retrospective cohort study was to compare shoulder function and residual pain after LCR using an arthroscopic approach and with LCR using an open approach. The results indicate that residual pain at final follow-up is less for patients who underwent LCR by an open approach. The data also show that operation time is less and resection distance is larger for the open group.
Primary outcome variables
Shoulder function by means of DASH score was not different between the two approaches. A significantly better VAS score at final follow-up was found for the open group. To our knowledge, this is the first comparative study in which the open approach scores are slightly better then the arthroscopic approach, thus a critical evaluation is needed.
In 2010, after reviewing 17 studies, Pensak et al. [9] concluded that both approaches are safe and beneficial for the treatment of recurrent AC pain, but the arthroscopic approach was associated with higher success rate than the open approach, with a good or excellent outcome in 79 % for the open approach (n = 287) and 91 % for the arthroscopic approach (n = 142). Four comparative studies were found in the literature, which found no difference in shoulder function at final follow-up between LCR by an open and arthroscopic approach, although different questionnaires were used [5–8]. The data in the present study support these findings. For VAS pain score, no difference was found in most studies [5–7]. Only one of these studies did correct for concomitant pathology; with the exclusion of adjuvant procedures, Robertson et al. [8] found a lower VAS score for the arthroscopic group, in contrast with the results of the present study. However, they did not perform analyses for a correlation between resection length and residual pain. Length of resection might present a direction for explaining these findings. In the methods, a resection of approximately half a centimeter was described. In the present study, bone removal was significantly less in the arthroscopic group in comparison to the open group, with medians of 3.2 mm and 7.1 mm, respectively. It can be argued that more resection results in less bony contact or pressure and thus less pain. On the other hand, too much resection might damage the capsule, increasing the risk of acromioclavicular instability and accompanying symptoms. In one study, a resection length greater than 10 mm was found to be associated with more postoperative pain [14] and another study recommended a resection not larger than 10 mm to preserve acromioclavicular stability [15]. Although in the present study perceived pain was significantly less and resection distance was significantly larger for the open approach, no significant association was found between pain and resection distance in additional regression analyses. Postoperative radiography was not a standard procedure, therefore the measured distances might represent a relatively small sample, in which there were residual shoulder complaints, demanding additional imaging. Because of this, results cannot be generalized.
Additionally, the optimal length of resection is subject to discussion. A 5-mm distal clavicle resection was found to be sufficient for eliminating bony contact, and even a resection of 2.5–5.0 mm could be adequate, if care is taken to excise a greater depth of bone in the inferior-posterior quadrant [16]. Flatow et al. [6] compared removal in the open and arthroscopic approach, and measured 18 and 17 mm, respectively. The large difference in bone removal compared to the present study may be partly explained by the year in which the study was performed (1992)—older reports recommend a minimum resection of 2 cm [17–19], whereas newer studies show that even resections of 5 mm can still impair joint stability [4, 10, 12, 20]. Several studies show an equal amount of resection between the approaches, but it might be harder to estimate the resected amount in arthroscopy [5, 8, 14].
Secondary outcome variables
The occurrence of complications was not significantly different between the approaches (10.2 % and 7.3 % for the arthroscopic and open approaches, respectively). Few studies have compared complications between both approaches and different complications have been mentioned [5, 6, 8, 14, 17]. In general, both approaches give few complications, with surgical site infection (SSI) rates of 0.0–4.3 %, and stiffness of the shoulder in 0–33 % of the patients [3]. Our SSI rate was 2 % and prevalence of frozen shoulder was 6,7 %, which are average compared to other studies. The larger proportion of patients with postoperative frozen shoulder in the arthroscopy group might be related to the intra-articular procedure or the longer operative time, although this finding was not significant.
When differences in patient-related outcomes between approaches are negligible, costs of operation and rehabilitation can be considered. Operative time was significantly less for the open procedure, mainly because of the absence of a diagnostic arthroscopy in the open group and the difference in additional acromioplasty. Nonetheless, we also believe the open approach is faster. The study by Robertson et al. [8], in which all patients in the open group had a diagnostic arthroscopy at the time of LCR, found no differences in operation time. To our knowledge, no other studies have compared operation time, length of hospitalization or direct costs between open and arthroscopic LCR. Despite the little amount of data available, it appears that the open approach is more or less equal to the arthroscopic approach, except for operative time for this group of patients. When comparing the surgical costs of the two approaches, the longer operative time and extra disposable equipment cause an estimated two- to threefold higher amount of total costs for the arthroscopic approach, e.g. in our hospital, costs were 990 versus 390 euro for arthroscopic and open approaches, respectively (Table 3). Because complication rate and days of hospitalization were not different between the groups, these were not taken into account. As this study was not designed as a cost-effectiveness study, presented costs are merely an indication.
Table 3.
Costs in Euro of open and arthroscopic procedures in our hospital
| Material | Open | Arthroscopic |
|---|---|---|
| Tray | 108 | 117 |
| Disposable arthroscopy materiala | 426 | |
| Other materialb | 41 | 63 |
| Operative time (10/min) | 244 | 386 |
| Total | 393 | 992 |
aDisposable cassette, burr, trocar, shaver blade, etc.
bGloves, scalpel, needles, iodine, saline, adhesives, etc.
Limitations and strengths
To our knowledge, this is the fifth study directly comparing the open and arthroscopic approach for LCR.
The retrospective nature of the present study accounts for some limitations. No randomization of patients was performed, so surgeon diagnostics, preference or experience on either technique may have played a role in determining the approach. The procedures were carried out by eight experienced orthopaedic surgeons. Four surgeons solely performed open procedures while the other four performed both open and arthroscopic ACJ resections. The reason for performing open or arthroscopic resection was not mentioned in the patient files and may have caused patient selection, although this is not endorsed by differences in patient characteristics. The higher amount of caudal acromioplasties performed in the arthroscopic group may have influenced the primary outcome variables and operative time. Furthermore, no baseline DASH score or VAS score were recorded, and patients were not seen for physical examination at final follow-up. Because of this lack in physical follow-up, we could not use a more shoulder specific questionnaire such as the Constant score. Most indications for LCR were AC osteoarthritis, but there were four patients with posttraumatic degeneration of the ACJ as well (one in the arthroscopic group and three in the open group). We did not correct for pre-operative indication. Furthermore, it was impossible to correct for intra-operative findings in the open group, because a diagnostic arthroscopy was not performed in all cases.
Lastly, the follow-up period was longer for the open approach which may have biased postoperative VAS pain score in favour of the open approach. However, it can be considered unlikely that a difference in 0.8 years after a follow-up of 2.8 years for the arthroscopic group would have affected the outcome in VAS pain score. Because of these limitations, care must be taken in generalizing the results. Nonetheless, the possible bias by concomitant pathology has been reasonably minimized by excluding surgical interventions with adjuvant procedures, creating a cohort as homogenous as possible. Also, the sample size can be considered relatively large [7, 8].
Conclusion
In conclusion, this study adds to the negligible difference in patient-related outcome measures between the open and arthroscopic approach for LCR. Pain was less at final follow-up for the open approach group. Apart from shorter operating time and greater length of resection for ACJ resection using the open approach, secondary outcome variables showed no differences between the groups.
For orthopaedic practice it seems that, for patients with no expected additional pathology, using an open approach for AC resection leads to good to excellent results but takes less expensive equipment and operating time compared to an arthroscopic approach. However, a careful evaluation of possible other pathologies, and, in those cases, considering an arthroscopic approach or an adjuvant diagnostic arthroscopy remains warranted. Future studies comparing the arthroscopic and open approach for LCR should include cost-effectiveness analyses and exploration of associations between resection length and residual pain.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Rios CG, Mazzocca AD. Acromioclavicular joint problems in athletes and new methods of management. Clin Sports Med. 2008;27:763–788. doi: 10.1016/j.csm.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 2.Himal HS. Minimally invasive (laparoscopic) surgery. Surg Endosc. 2002;16:1647–1652. doi: 10.1007/s00464-001-8275-7. [DOI] [PubMed] [Google Scholar]
- 3.Chronopoulos E, Gill HS, Freehill MT, Petersen SA, McFarland EG. Complications after open distal clavicle excision. Clin Orthop Relat Res. 2008;466:646–651. doi: 10.1007/s11999-007-0084-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Renfree KJ, Wright TW. Anatomy and biomechanics of the acromioclavicular and sternoclavicular joints. Clin Sports Med. 2003;22:219–237. doi: 10.1016/S0278-5919(02)00104-7. [DOI] [PubMed] [Google Scholar]
- 5.Elhassan B, Ozbaydar M, Diller D, Massimini D, Higgins LD, Warner JJ. Open versus arthroscopic acromioclavicular joint resection: a retrospective comparison study. Arthroscopy. 2009;25:1224–1232. doi: 10.1016/j.arthro.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 6.Flatow EL, Cordasco FA, Bigliani LU. Arthroscopic resection of the outer end of the clavicle from a superior approach: a critical, quantitative, radiographic assessment of bone removal. Arthroscopy. 1992;8:55–64. doi: 10.1016/0749-8063(92)90136-Y. [DOI] [PubMed] [Google Scholar]
- 7.Freedman BA, Javernick MA, O'Brien FP, Ross AE, Doukas WC. Arthroscopic versus open distal clavicle excision: comparative results at six months and one year from a randomized, prospective clinical trial. J Shoulder Elbow Surg. 2007;16:413–418. doi: 10.1016/j.jse.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Robertson WJ, Griffith MH, Carroll K, O'Donnell T, Gill TJ. Arthroscopic versus open distal clavicle excision: a comparative assessment at intermediate-term follow-up. Am J Sports Med. 2011;39:2415–2420. doi: 10.1177/0363546511419633. [DOI] [PubMed] [Google Scholar]
- 9.Pensak M, Grumet RC, Slabaugh MA, Bach BR., Jr Open versus arthroscopic distal clavicle resection. Arthroscopy. 2010;26:697–704. doi: 10.1016/j.arthro.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 10.Branch TP, Burdette HL, Shahriari AS, Carter FM, Hutton WC. The role of the acromioclavicular ligaments and the effect of distal clavicle resection. Am J Sports Med. 1996;24:293–297. doi: 10.1177/036354659602400308. [DOI] [PubMed] [Google Scholar]
- 11.Buttaci CJ, Stitik TP, Yonclas PP, Foye PM. Osteoarthritis of the acromioclavicular joint: a review of anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil. 2004;83:791–797. doi: 10.1097/01.PHM.0000140804.46346.93. [DOI] [PubMed] [Google Scholar]
- 12.Matthews LS, Parks BG, Pavlovich LJ, Jr, Giudice MA. Arthroscopic versus open distal clavicle resection: a biomechanical analysis on a cadaveric model. Arthroscopy. 1999;15:237–240. doi: 10.1016/S0749-8063(99)70027-7. [DOI] [PubMed] [Google Scholar]
- 13.Veehof MM, Sleegers EJ, van Veldhoven NH, Schuurman AH, van Meeteren NL. Psychometric qualities of the Dutch language version of the disabilities of the arm, shoulder, and hand questionnaire (DASH-DLV) J Hand Ther. 2002;15:347–354. doi: 10.1016/S0894-1130(02)80006-0. [DOI] [PubMed] [Google Scholar]
- 14.Eskola A, Santavirta S, Viljakka HT, Wirta J, Partio TE, Hoikka V. The results of operative resection of the lateral end of the clavicle. J Bone Joint Surg Am. 1996;78:584–587. doi: 10.2106/00004623-199604000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Boehm TD, Kirschner S, Fischer A, Gohlke F. The relation of the coracoclavicular ligament insertion to the acromioclavicular joint: a cadaver study of relevance to lateral clavicle resection. Acta Orthop Scand. 2003;74:718–721. doi: 10.1080/00016470310018261. [DOI] [PubMed] [Google Scholar]
- 16.Edwards SL, Wilson NA, Flores SE, Koh JL, Zhang LQ. Arthroscopic distal clavicle resection: a biomechanical analysis of resection length and joint compliance in a cadaveric model. Arthroscopy. 2007;23:1278–1284. doi: 10.1016/j.arthro.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Neer CS (1983) Impingement lesions. Clin Orthop Relat Res 173:70–77 [PubMed]
- 18.Rockwood CA, Young DC. Disorders of the acromioclavicular joint. In: Rockwood CA, Matsen FA, editors. The shoulder. Philadelphia: WB Saunders; 1990. pp. 413–476. [Google Scholar]
- 19.Rowe CR. Trends in treatment of complete acromioclavicular dislocations. In: Bateman JE, Walsh RP, editors. Surgery of the shoulder. Toronto: RC Decker; 1984. pp. 73–78. [Google Scholar]
- 20.Corteen DP, Teitge RA. Stabilization of the clavicle after distal resection: a biomechanical study. Am J Sports Med. 2005;33:61–67. doi: 10.1177/0363546504268038. [DOI] [PubMed] [Google Scholar]