Abstract
Purpose
The objective of this study was to evaluate the results achieved after revision with plates of humeral nonunions secondary to failed intramedullary nailing.
Methods
We retrospectively evaluated 32 patients with humeral nonunions secondary to failed intramedullary nailing, treated by internal fixation with plates between 1998 and 2012. Nonunions were diaphyseal in 19 cases, they were located in the proximal humeral metaphysis in nine cases, and in the distal humeral metaphysis in four cases. There were 11 atrophic nonunions and 21 oligotrophic nonunions. Initial treatment was performed with static locked nails in 12 cases, nails with expansive locking systems in 11 cases, and using thin elastic nails in nine cases. The nails were placed antegrade in 18 cases and retrograde in 14 cases. Time between initial surgery and revision surgery averaged 14.5 months. In seven diaphyseal nonunions, the intramedullary nail was left in-situ. Bone graft was added in 25 cases.
Results
Follow-up averaged 35 months. Union was achieved in all cases, after an average of 3.8 months. Disabilities of the Arm, Shoulder and Hand (DASH) score at last follow-up averaged 14 points, and Constant’s score averaged 82 points. The analogue scale of pain averaged 0.8 points. Out of seven patients with radial nerve compromise, six recovered completely and one needed tendon transfers.
Conclusions
Revision with plates after failed intramedullary humeral nailing achieved union and good predictable objective and subjective results in all cases. Adequate implant selection and meticulous surgical technique are necessary to achieve successful osteosynthesis and bony union.
Keywords: Nonunion, Humerus, Intramedullary nails, Plates
Introduction
Intramedullary (IM) nailing has proven to be a valid therapeutic option for the stabilisation of humerus fractures, as long as the indications are appropriate and surgical technique is performed adequately for their placement [1–4]. Nevertheless, several problems have been identified with their use, including less axial and rotational stability than plates, migration, and problems with the insertion site [1]. Clinical results achieved using locked IM nails has not been as consistent as those obtained with similar systems used in the lower extremities [2, 3]. Humeral nonunions secondary to failed IM nailing are difficult to treat, and the percentage of nonunions reported after IM varies between 0 % and 50 % [5–8]. There is literature reporting that IM nails are associated with a higher risk of restriction in shoulder range of motion and a more frequent need for implant removal than when compression plates are used [9]; and there are reports stating that results after surgical treatment of diaphyseal humerus nonunions are worse in patients treated previously with IM nailing, than in those patients with no previous surgical treatment or those treated initially with plates [3, 10]. Exchanging nails when a humerus fracture treated with a nail fails to unite has not been associated with good results [2].
The objective of this study was to evaluate the results achieved after revision with plates of humerus nonunions secondary to failed IM nailing.
Methods
Thirty-two patients with humeral nonunions secondary to failed IM nailing and treated by internal fixation with plates between 1998 and 2012 were retrospectively evaluated. All nonunions were secondary to closed fractures. They were daiphyseal in 19 cases; they were located in the proximal humerus metaphysis in nine cases and in the distal metaphysis in four cases. Twenty-one nonunions were oligotrophic and 11 atrophic. Initial treatment was performed using static locked nails in 12 cases, nails with expansive locking systems in 11 cases (Seidel nails in eight cases and Hacketal nails in three cases), and using thin elastic nails in nine cases (Ender nails in six cases, and titanium elastic nails in three cases); in three cases initial stabilisation was accompanied by cerclage wire at the fracture site. The nails were placed antegrade in 18 cases and retrograde in 14 cases. Time between the previous surgery using a nail and revision surgery averaged 14.5 months (range, 5–54). Nine patients had had iterative operations prior to the placement of the nail that needed to be revised (average 1.9, range 1–5). Preoperative Constant’s score averaged 48 points (range, 12–92). Thirteen patients had elbow functional loss (two had complete elbow stiffness, and in the remaining 11 range of motion loss averaged 25° in flexion [range, 15–50], and 36° in extension [range, 10–85]). Three nonunions were infected. Three patients had complete radial nerve palsy, and five patients recalled having had postoperative radial nerve neurapraxia during their previous surgical procedure, but with complete recovery at the time of their revision surgery.
Henry’s anterolateral approach [11] was used in the nine nonunions located in the proximal humeral metaphysis, and the stabilisation was achieved using locked 90° blade-plates in five cases [12], with conventional blade plates in three cases, and with a 4.5-mm LCP plate in one case. In the four nonunions located in the distal humeral metaphysis, the paratricipital approach described by Alonso-Llames was used [13]; three of these nonunions were stabilised using two 3.5-mm reconstruction plates and one with a 4.5-mm LCP plate and a 3.5-mm reconstruction plate [14]. Regarding the 19 diaphyseal nonunions, the approach used was lateral, and the stabilisation was performed using 4.5-mm LC-DCP plates in nine cases (in three cases using “wave plate” osteosynthesis) [15, 16] (Fig. 1), with 4.5-mm LCP plates in seven cases, and with 3.5 mm LCP plates in three cases. In seven diaphyseal nonunions, the IM nail from the previous surgery was not removed (they were all placed deep in the humeral canal, and it was considered that the risk of further complications at the time of their removal was high), in these cases the osteosynthesis with plates was performed leaving the nail in-situ; in three of these cases the plates were placed using minimally invasive percutaneous plate osteosynthesis technique (Fig. 2); the length of the plates used in diaphyseal nonunions averaged 11.5 holes (range, ten to 13).
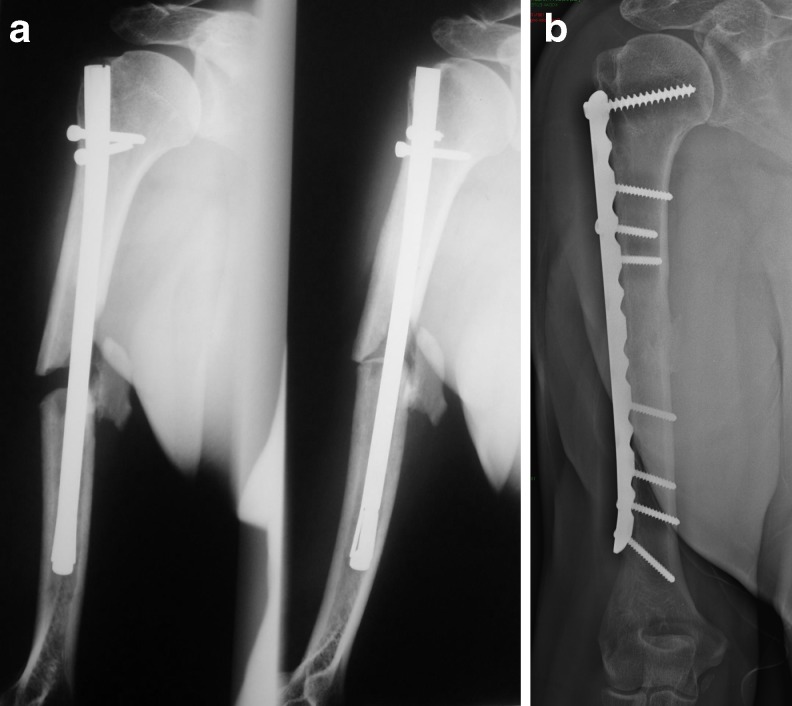
Fig. 1.
a A 56-year-old male, 14 months after antegrade IM nailing with distal expansive locking system. Traction X-rays evidenced diastasis at the nonunion site, and distal cortical thinning due to windshield wiper effect of the loose nail. b Bony union after IM nail removal, decortication, radial nerve release, and stabilisation with a long 4.5-mm LC-DCP plate and autogenous cancellous iliac crest bone graft
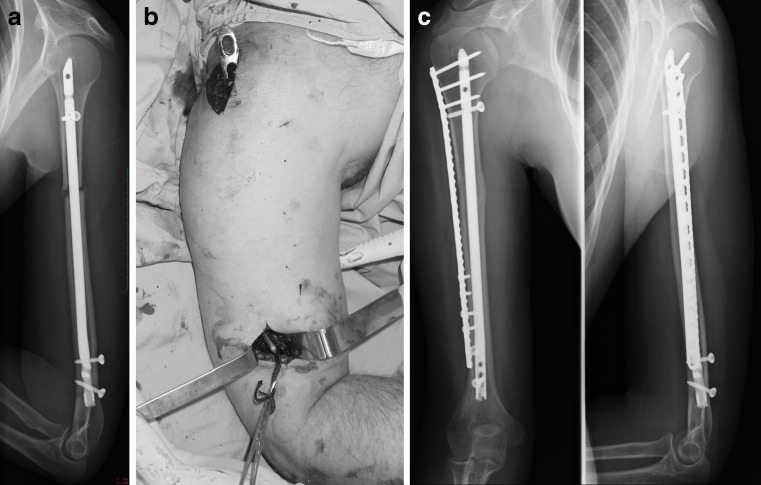
Fig. 2.
a A 26-year-old female, 11 months after retrograde locked IM nailing. b Minimally invasive lateral percutaneous plate osteosynthesis. c Stabilised with a 3.5-mm LCP plate, placed bridging the nonunion. No bone graft was used and the radial nerve was protected throughout plate insertion, achieving union and complete function with no pain
Bone graft was added in 25 cases, in 23 cases autogenous iliac crest bone graft was used (in eight of these cases that had infection or history of previous infection 2 grams of vancomicin powder was used with the graft) [17], and in the other two cases morsellised criopreserved bone allograft with 2 grams of vancomicin powder was used. In one proximal humeral metaphyseal infected nonunion, the reconstruction was performed in two stages; in the first stage thorough debridement and placement of a cement spacer with antibiotics was carried out, and in a second stage, the cement spacer was removed and a locked 90° blade-plate and bone allograft were inserted [18, 19]. In the two remaining infected nonunions, the lesions were located in the distal humeral methaphysis, and reconstruction was performed in one surgical procedure, using two 3.5-mm reconstruction plates, associated with wide debridement and autogenous iliac crest cancellous bone graft mixed with 2 grams of vancomicin powder. In diaphyseal nonunions the radial nerve was identified and protected; and in humerus distal third nonunions the ulnar nerve was identified, protected and transposed anteriorly subcutaneously in two cases.
Results
Follow-up averaged 35 months (range, 12–94). Bony union was achieved in all cases, after an average of 3.7 months (range, 2–7.5). Disabilities of the Arm, Shoulder and Hand score at last follow-up averaged 14 points (range, 0–33). Constant’s score at last follow-up averaged 82 points (range, 56–100). The analogue scale of pain averaged 0.8 points (range, 0–3.5). The two patients with complete pre-operative elbow stiffness had significant ROM improvement, recovering a flexion of 110° and 120°, and an extension loss of 15° and 35°, respectively; of the remaining patients six had elbow ROM limitation, all in extension, averaging 22 (range, ten to 45). Of the three patients that had complete preoperative nerve palsy, two had complete recovery (three and five months after neurolysis and epineurotomy performed during nonunion revision surgery); in the third patient, complete radial nerve section was found at revision surgery, which was performed 14 months after nail placement, and tendon transfers were performed eight months after humeral union was achieved. Another four patients had radial nerve neurapraxia after their revision surgery; two of them had had previous history of radial nerve neurapraxia after their initial humerus fracture treatment, when the IM nail was inserted. All four of these patients had complete nerve recovery before the fourth postoperative month. There was no need for implant removal in any of the 33 cases.
Discussion
Different treatment alternatives have been reported for the revision of failed humerus IM nailing. Exchanging nails has not been associated with good results in these cases [2]. The use of external fixators for revision of failed humerus IM nailing can be associated with re-fractures, pin tract infections, septic arthritis, and nerve lesions [20, 21]; they represent voluminous constructions and the extremity needs to be protected after their removal to decrease the chances of re-fracture. In the series we report, revision with plates after failed humerus nailing achieved good objective and subjective results, as well as union, in all 32 cases; patients final functional limitations were secondary to lesions already present before the revision surgery. The main limitations of this study are its retrospective nature, inclusion of metaphyseal and diaphyseal humeral nonunions and having no control group; but we consider that the rarity of this particular entity and the fact that good predictable results were achieved and a good follow-up was possible make the study worth reporting.
The mechanisms by which it is considered that exchange IM nailing works in femoral and tibial nonunions include additional stability acquired by the placement of a wider nail (improving the bone-nail interface), bone graft from reaming, and increased blood supply induced by reaming and periosteal reaction [22]. One aspect to consider in humerus IM nailing failure is the inadequate primary stability of the fixation, which is responsible for the failure of the implants to maintain the compression achieved intraoperatively; this has been reported in clinical series [5, 23] and in biomechanical studies [24, 25]. In our series, 20 patients were initially stabilised with IM nails with expansive locking systems or thin elastic nails, which were not effective in maintaining compression at the fracture site, and subsequently evolved to nonunion.
Humeral nonunions secondary to failed IM nails can be associated with cortical thinning due to the “windshield-wiper” effect, and bone loss at the nonunion site, decreasing the chances of success if nail exchange is performed [2]. Preoperative X-rays should evaluate the nonunion type and location, size and bone quality of the segments to be stabilised, amount of bony erosion resulting from the windshield-wiper effect (Fig. 1a), and shoulder and elbow joints. The amount of bone loss associated with loose humeral nails, the rotational and distraction strengths (gravity) to which humeral nonunions are subjected, the morbidity associated with intramedullary nail insertion sites, and the low percentage of success reported by nail exchange in humerus nonunions, differentiate these nonunions from similar pathologies in lower extremities [3, 5, 15].
In 1996, Wu [26] proposed associating a staple in nonunions treated with intramedullary nails. In addition, Emmerson and Sher in 1998 [27], Gerber et al. in 2003 [15], Ring and Jupiter in 2003 [10], and Nadkarni et al. in 2008 [28] reported on the placement of different types of plates, leaving the IM nail in-situ; in all their cases the combined osteosynthesis was performed to increase rotational stability at the nonunion, reporting excellent results and union in all cases. When the IM nail protrudes at its entry point, it should be removed; but, when the nails are placed deep in the medullary canal, they can be difficult to find and remove, and during their removal there is risk of additional rotator cuff lesion. In theses cases, leaving the nail and adding a plate is a valid treatment alternative. When the decision is made to leave the nail in place and to introduce a plate to increase stability, it is important to evaluate (a) type of IM nail used (to determine if it has a locking system, and if it protrudes proximally or distally), (b) type of nonunion (to determine if there is bone contact and the extension of the bone defect), and (c) the amount of the medullary canal occupied by the IM nail (to determine the length of the plate, type and direction of the screws to be used). Union and good functional results were achieved in the six cases of our series in which the plate was placed leaving the IM nail in-situ.
Implants with good purchase in the humeral head were used in nonunions extending into the proximal humeral metaphysis [12, 29]. In diaphyseal nonunions long plates were used, restoring good bone contact between the affected segments, and bridging the area affected by previous implants. The use of long plates allowed increasing the pull-out resistance of the implants, by increasing their working length and flexibility [15]. The use of LCP plates has the advantage of allowing improved fixation in the thin humerus cortexes resulting from the windshield effect after loose IM nails, as well as in those cases in which the nail is left in-situ, by using monocortical screws in the areas where the nail occupies most of the medullary canal and which do not allow placement of bicortical screws. In distal metaphyseal nonunions, stabilisation with double plates achieved union and good functional results in the four cases of our series, and good results with its use have been reported [14].
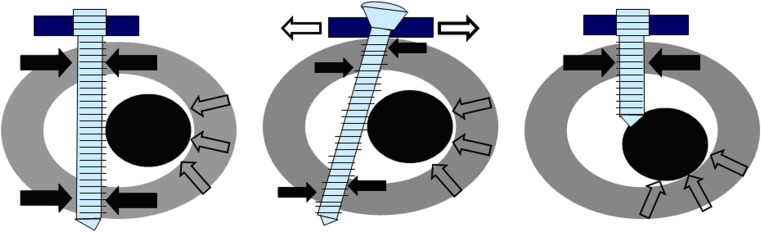
Atrophic nonunions are not avascular [30], and treatment strategies in nonunions should focus on stimulating osteogenesis and angiogenesis [31]. In our series of patients, osteoperiosteal decortication as described by Judet [32] was performed in all cases (except those three in which minimally invasive percutaneous plate osteosynthesis was performed), and bone graft was associated in 25 cases, achieving bony union in all cases. The use of new generation IM nails, that allow locking the screws to the nail, will probably help improve the interface between bone and IM nail, and help increase the stability of these constructions by decreasing loss of compression achieved intraoperatively. A similar effect is achieved by the plates placed without removing the IM nail, as the screws act by compressing the loose nail against the humeral cortex, improving bone–nail interface, and increasing stability of the construction (Fig. 3).
Fig. 3.
Graphics demonstrating the mechanism by which screws (whether compressive bicortical or locked [unicortical or bicortical]) act by compressing the loose nail against the opposite cortex, improving nail–bone interface and increasing the stability of the construction
Success in achieving union and good functional results in humerus nonunions after failed IM nailing is based in many biological and mechanical factors; and although implant selection and surgical technique are important factors to be considered [33, 34], they are only two of the many aspects that must be evaluated and considered before approaching this pathology. Avoiding unnecessary surgical procedures and performing adequate surgical techniques in the initial treatment of humeral fractures are basic concepts that reduce incidence of nonunion after IM humeral nailing [1]. Most failures are due to inadequate surgical indication, implant selection, or surgical technique. In our series, revision with plates alter failed IM humeral nailing achieved union and good objective and subjective results in all patients.
References
- 1.Anglen JO, Archdeacon MT, Cannada LK, Herscovici D, Jr, Ostrum RF. Avoiding complications in the treatment of humeral fractures. Instr Course Lect. 2009;58:3–11. [PubMed] [Google Scholar]
- 2.Brinker MR, O’Connor DP. Exchange nailing of ununited fractures. J Bone Joint Surg Am. 2007;89:177–188. doi: 10.2106/JBJS.F.00742. [DOI] [PubMed] [Google Scholar]
- 3.McKee MD, Miranda MA, Riemer BL, Blasier RB, Redmond BJ, Sims SH, Waddell JP, Jupiter JB. Management of humeral nonunion after the failure of locking intramedullary nails. J Orthop Trauma. 1996;10:492–499. doi: 10.1097/00005131-199610000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Rommens PM, Kuechle R, Bord T, Lewens T, Engelmann R, Blum J. Humeral nailing revisited. Injury. 2008;39:1319–1328. doi: 10.1016/j.injury.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 5.Dujardin FH, Mazirt N, Tobenas AC, Duparc F, Thomine JM. Failure of locked centro-medullary nailing in pseudarthrosis of the humeral diaphysis. Rev Chir Orthop Reparatrice Appar Mot. 2000;86:773–780. [PubMed] [Google Scholar]
- 6.Svend-Hansen H, Skettrup M, Rathcke MW. Complications using the Seidel intramedullary humeral nail. Outcome in 31 patients. Acta Orthop Belg. 1998;64:291–295. [PubMed] [Google Scholar]
- 7.Bain G, Sandow M. Treatment of humeral shaft fractures with the Seidel intramedullary nail. Joint Surg Br. 1992;748(1):39. doi: 10.1111/j.1445-2197.1996.tb01145.x. [DOI] [PubMed] [Google Scholar]
- 8.Farragos AF, Schemitsch EH, McKee MD. Complications of intramedullary nailing for fractures of the humeral shaft: a review. J Orthop Trauma. 1999;13:258–267. doi: 10.1097/00005131-199905000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Kurup H, Hossain M, Andrew JG. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures in adults. Cochrane Database Syst Rev. 2011;15(6):CD005959. doi: 10.1002/14651858.CD005959.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ring D, Jupiter J. Humerus nonunion after intramedullary rod fixation. Locking compression plate without removing the nail. Tech Orthop. 2004;18:356–359. doi: 10.1097/00013611-200312000-00009. [DOI] [Google Scholar]
- 11.Henry AK. Extensile exposure. 2. Edinburgh: Churchill Livingstone; 1973. [Google Scholar]
- 12.Allende C, Allende BT. The use of a new locking 90 degree blade plate in the treatment of atrophic proximal humerus nonunions. Int Orthop. 2009;33:1649–1654. doi: 10.1007/s00264-008-0686-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alonso-Llames M. Bilaterotricipital approach to the elbow. Its application in the osteosynthesis of supracondylar fractures of the humerus in children. Acta Orthop Scand. 1972;43:479–490. doi: 10.3109/17453677208991270. [DOI] [PubMed] [Google Scholar]
- 14.Allende C, Allende BT. Post-traumatic distal humerus nonunion: open-reduction and internal fixation: long term results. Int Orthop. 2009;33:1289–1294. doi: 10.1007/s00264-008-0650-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gerber A, Marti R, Jupiter J. Surgical management of diaphyseal humerus nonunion after intramedullary nailing: Wave-plate fixation and autologous bone grafting without nail removal. J Should Elb Surg. 2003;12:309–313. doi: 10.1016/S1058-2746(03)00044-2. [DOI] [PubMed] [Google Scholar]
- 16.Ring D, Jupiter JB, Quintero J, Sanders RA, Marti RK. Atrophic ununited diaphyseal fractures of the humerus with a bony defect. Treatment by wave plate osteosynthesis. J Bone Joint Surg. 2000;82-B:867–871. doi: 10.1302/0301-620X.82B6.10124. [DOI] [PubMed] [Google Scholar]
- 17.Chan YS, Ueng SW, Wang CJ, Lee SS, Chen CY, Shin CH. Antibiotic-impregnated autogenic cancellous bone grafting is an effective and safe method for the management of small infected tibial defects: a comparison study. J Trauma. 2000;48:246–255. doi: 10.1097/00005373-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Allende C. Cement spacers with antibiotics for the treatment of posttraumatic infected nonunion and bone defects of the upper extremity. Tech Hand Upper Extrem Surg. 2010;14:241–247. doi: 10.1097/BTH.0b013e3181f42bd3. [DOI] [PubMed] [Google Scholar]
- 19.Allende C, Mangupli M, Bagliardelli J, Diaz P, Allende BT. Infected nonunions of long bones of the upper extremity: staged reconstruction using polymethylmethacrylate and bone graft impregnated with antibiotics. Chir Organi Mov. 2009;93:137–142. doi: 10.1007/s12306-009-0046-y. [DOI] [PubMed] [Google Scholar]
- 20.Lammens J, Bauduin G, Driesen R, Moens P, Stuyck J, De Smet L, Fabry G. Treatment of nonunion of the humerus using the Ilizarov external fixator. Clin Orthop Relat Res. 1998;353:223–230. doi: 10.1097/00003086-199808000-00026. [DOI] [PubMed] [Google Scholar]
- 21.Patel VR, Menon DK, Pool RD, Simonis RB. Nonunion of the humerus after failure of surgical treatment. Management using the Ilizarov circular fixator. J Bone Joint Surg. 2000;82-B:977–983. doi: 10.1302/0301-620X.82B7.10180. [DOI] [PubMed] [Google Scholar]
- 22.Schemitsch EH, Kowalski MJ, Swiontkowski MF. Soft-tissue blood flow following reamed versus undreamed locked intramedullary nailing: a fractured sheep tibia model. Ann Plast Surg. 1996;36:70–75. doi: 10.1097/00000637-199601000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Thomsen NOB, Mikkelsen JB, Svendsen RN, Skovgaard N, Jensen CH, Jorgensen U. Interlocking nailing of humeral shaft fractures. J Orthop Sci. 1998;3:199–203. doi: 10.1007/s007760050042. [DOI] [PubMed] [Google Scholar]
- 24.Dalton JE, Salkeldn SL, Satterwhite YE, Cook SD. A biomechanical comparison of intramedullary nailing systems for the humerus. J Orthop Trauma. 1993;7:367–374. doi: 10.1097/00005131-199308000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Schoffer A, Hearn TC, Malisano L, Powell JN, Kellam JF. Comparison of torsional strength of humeral intramedullary nailing: a cadaveric study. J Orthop Trauma. 1994;8:414–421. doi: 10.1097/00005131-199410000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Wu CC. Humeral shaft nonunion treated by a Seidel interlocking nail with a supplementary staple. Clin Orthop. 1996;326:203–208. doi: 10.1097/00003086-199605000-00024. [DOI] [PubMed] [Google Scholar]
- 27.Emmerson KP, Sher JL. A method of treatment of nonunion of humeral shaft fractures following treatment by locked intramedullary nail: a report of three cases. Injury. 1998;29:550–552. doi: 10.1016/S0020-1383(98)00109-0. [DOI] [PubMed] [Google Scholar]
- 28.Nadkarni B, Srivastav S, Mittal V, Agarwal S. Use of locking compression plates for long bone nonunions without removing existing intramedullary nail: review of literature and our experience. J Trauma. 2008;65:482–486. doi: 10.1097/TA.0b013e31817c9905. [DOI] [PubMed] [Google Scholar]
- 29.Ring D, McKee MD, Perrey BH, Jupiter JB. The use of a blade plate and autogenous cancellous bone graft in the treatment of ununited fractures of the proximal humerus. J Should Elb Surg. 2001;10:501–507. doi: 10.1067/mse.2001.118414. [DOI] [PubMed] [Google Scholar]
- 30.Reed AA, Joyner CJ, Brownlow HC, Simpson AH. Human atrophic fracture non-unions are not avascular. J Orthop Res. 2002;20:593–599. doi: 10.1016/S0736-0266(01)00142-5. [DOI] [PubMed] [Google Scholar]
- 31.Garcia P, Pieruschka A, Klein M, Tami A, Histing T, Holstein JH, Scheuer C, Pohlemann T, Menger MD. Temporal and spatial vascularization patterns of unions and nonunions: role of vascular endothelial growth factor and bone morphogenetic proteins. J Bone Joint Surg. 2012;94:49–58. doi: 10.2106/JBJS.J.00795. [DOI] [PubMed] [Google Scholar]
- 32.Ramoutar DN, Rodrigues J, Quah C, Boulton C, Moran CG. Judet decortication and compression plate fixation of long bone non-union: is bone graft necessary? Injury. 2011;42:1430–1434. doi: 10.1016/j.injury.2011.03.045. [DOI] [PubMed] [Google Scholar]
- 33.Connor P, Flatow E. Complications of internal fixation of proximal humerus fractures. Instr Course Lect. 1997;46:25–37. [PubMed] [Google Scholar]
- 34.King AR, Moran SL, Steinmann SP. Humeral nonunion. Hand Clin. 2007;23:449–456. doi: 10.1016/j.hcl.2007.09.003. [DOI] [PubMed] [Google Scholar]