Abstract
Purpose
The objective of this retrospective study was to evaluate the functional results of distal biceps tendon repair using suture anchors via a single-incision approach.
Methods
Forty-nine patients were re-examined at a mean follow-up of 44.2 ± 32.1 months (range, 12–119 months). Subjective and objective criteria included patient’s satisfaction, active range of motion (ROM), maximum isometric strength in flexion (at 45° and 90°), and supination of both arms. Functional scoring included the Morrey elbow score (MES) and the QuickDASH. Furthermore, follow-up radiographs were performed.
Results
Eighty-six percent of patients were highly satisfied or satisfied with their outcome. Compared to contralateral, the active ROM of elbow flexion, extension, and pronation was not affected; however, supination was decreased by 3° (P < 0.001). The isometric maximum strengths showed significant deficits in all tested scenarios (at 45°, P = 0.002; at 90°, P < 0.001; for supination, P < 0.001). The MES and the QuickDASH were 97.2 ± 4.9 and 7.9 ± 13.9, respectively. Heterotopic ossifications (HO) were found in 39 % of patients; however, with respect to scores and strength, no significant differences were seen compared to patients without HO. Moreover, four anchor failures were detected.
Conclusions
Single-incision suture anchor repair provides high patient’s satisfaction and good results with respect to ROM and functional scoring. Nevertheless, based on presented data, the patient has to be informed of postoperative HO and especially for supination strength weakness after surgery. Distal biceps tendon repair should be reserved for experienced upper extremity surgeons to avoid procedure-related complications.
Keywords: Distal biceps repair, Suture anchor, Single incision, Supination strength, Heterotopic ossification
Introduction
Surgical reattachment to the bicipital tuberosity has been recognized nowadays as the treatment of choice for distal biceps tendon ruptures as it leads to improved strength and endurance compared with non-operative treatment [1, 2]. Historically, surgical methods of distal biceps tendon repair involved an extensile anterior single-incision approach with high incidence of neurologic complications [3]. Therefore, double-incision repair methods were developed to decrease the risk of neural complications [4, 5]. However, complications with special respect to heterotopic ossifications (HO) including loss of forearm rotation and radioulnar synostosis were seen in various double-incision techniques [6–8]. Since the late 1990s, the anterior approach has been re-popularized due to the availability and innovations of different fixation devices. Via a single-incision approach, diverse surgical repair techniques using suture anchors, interference screws, and cortical fixation buttons have shown both good clinical results and near pre-injury strength of forearm supination and elbow flexion [9–12]. Nevertheless, the optimal surgical strategy is being controversially discussed in the current literature.
The purpose of the present study was to evaluate our functional results following single-incision suture anchor repair for distal biceps tendon ruptures. The rationale for this repair technique was to provide anatomical reattachment in an effort to restore normal flexion and supination strength.
Methods
Patient population
Between 1998 and 2008, a total of 63 patients underwent suture anchor repair through an anterior single-incision approach. Medical records and radiographs of these patients were reviewed for sex and age at time of surgery, arm dominance, interval between trauma and surgery, and postoperative complications as well. Six patients could not be located and eight were unavailable for review due to time reasons. Thus, 49 patients participated in the present study (22 % lost to follow-up). Except for one female, all patients were male with a mean age of 47.3 ± 9.9 years (range, 20–65 years) at the time of surgery. The dominant arm side was involved in 25 of 49 patients (51 %).
Surgical management
The mean time to surgery was 21.7 ± 31.4 days (range, zero–135). Thirteen different surgeons carried out the operations. All patients were surgically treated under general anaesthesia and a single dose of antibiotics was given pre-operatively for prophylaxis. Patients were positioned supine with the injured arm on a radiolucent table. Depending on the retraction of the tendon stump, the skin incision varied in proximal length for subcutaneous dissection. The lateral antebrachial cutaneous nerve (LACN) of the forearm was identified and carefully retracted. After tendon stump detection, the bicipital tuberosity was exposed by gentle retraction of the surrounding soft tissues and neurovascular protection with the forearm in full supination and decorticated for tendon reattachment. In the ten-year period of treatment evaluated in this study, different types of suture anchor implants were used (Table 1). The positioning of the anchor was intraoperatively checked by biplanar fluoroscopy. Then, the distal biceps tendon stump was debrided and sutured using continuous baseball stitches (Fig. 1). Suture tying was performed with the forearm in full supination and in approximately 30–45° of elbow flexion. Finally, the stability of tendon repair was tested by gentle elbow motion. In five patients with delayed tendon repair (>six weeks), a blunt proximal release of the biceps muscle with flexion of the elbow was satisfactory to enable reattachment to the bicipital tuberosity. No augmentation with tendon autograft or allograft was required.
Table 1.
Numbers and types of suture anchors
| Manufacturer | Anchor implant and sutures types | Patients (n) |
|---|---|---|
| Arthrex (Naples, FL, USA) | 1 × Corkscrew titanium with No. 2 FibreWire | 10 |
| 2 × Corkscrew titanium with No. 2 FibreWire | 24 | |
| 3 × Corkscrew titanium with No. 2 FibreWire | 1 | |
| 2 × Fastak titanium with No. 2 FibreWire | 2 | |
| 1 × Bio-Corkscrew with No. 2 FibreWire | 5 | |
| Depuy Mitek (Norwood, MA, USA) & Ethicon (Somerville, NJ, USA) | 2 × Super-Mitek anchor with No. 2 Ethibond | 6 |
| 3 × Super-Mitek anchor with No. 2 Ethibond | 1 |
Fig. 1.
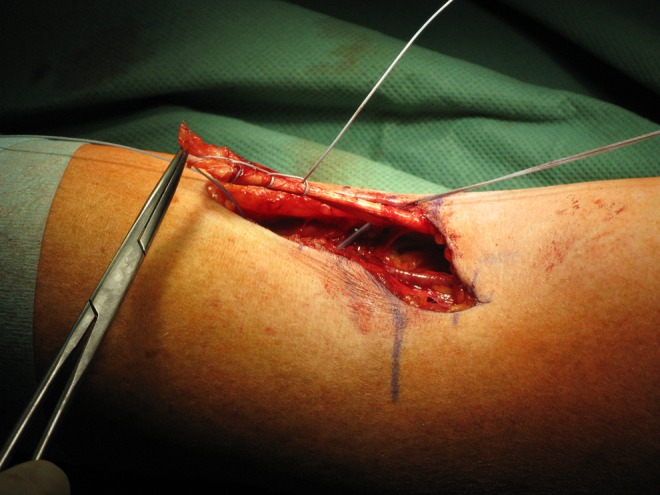
Intraoperative photograph showing distal biceps tendon repair via an anterior s-shaped approach
For postoperative management, the elbow was immobilized in a plaster cast in 90° of flexion for one to two weeks. Passive motion exercises started two days postoperatively. Six weeks after surgery, gradual biceps strengthening was applied. In a delayed surgical intervention, a cast was applied for two to three weeks and no active exercises were allowed to secure tendon repair within this time period. All patients were allowed to resume normal activity without restriction or limitation for three months postoperatively following distal biceps repair.
Outcome evaluation
Personal interviews and elbow scoring was carried out by an independent investigator not involved in the initial surgical management. The mean follow-up was 44.2 ± 32.1 months (range, 12–119 months). Written informed consent was obtained from each patient. The institutional ethics committee approved the study protocol.
For subjective evaluation, patients rated their satisfaction for elbow use on a scale of 1 to 5 (1–highly satisfied; 2–satisfied; 3–moderate; 4–unsatisfied; 5–very unsatisfied). Objective assessment consisted of a physical examination for active range of motion (ROM) of the elbow using a standard goniometer for extension and flexion as well as forearm rotation on both the injured and uninjured side. Moreover, sensomotoric disturbances and postoperative complications were recorded. All patients underwent objective isometric biceps muscle strength testing using the Isoforce Control® (MDS–Medical Device Solutions AG, Oberburg, Switzerland) for the injured and the uninjured upper extremity. The measurements included maximum flexion strength in 45° and 90° of elbow flexion as well as maximum supination strength with the forearm in neutral position. All measurements were performed three times and averaged. For functional outcome scoring, patients completed the Morrey elbow score (MES) and the shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH) [13–15]. To detect HO, anteroposterior and lateral radiographs of the operated elbow were performed in 46 patients. Three patients refused radiographic evaluation and therefore received ultrasound examination.
Statistical analysis
Statistical analysis was performed using Microsoft Excel 2003 and PASW software, version 15.0 (SPSS Inc., Chicago, IL, USA). Data were presented as mean ± standard deviation (SD). The Student’s t-test and Mann–Whitney U-test were used to evaluate the differences between groups where appropriate. A level of P < 0.05 was considered significant.
Results
Patient’s satisfaction
Subjective satisfaction of patients for elbow function was rated as highly satisfied in 15 patients and satisfied in 27 patients, which represents 86 % of the study group. Seven patients were moderately satisfied with their outcome due to decreased flexion and supination strength or scar-related problems.
Objective outcomes
The mean postoperative elbow flexion was 133° (range, 120–140°) compared to 134° (range, 120–145°) of the uninjured side. The mean elbow extension was 1° (range, −5–10°) and 0° (range, −5–10°) on the injured and on the contralateral side, respectively. For supination, the mean values of the operated side were 84° (range, 70–90°) compared to 87° (range, 70–90°) of the uninjured side, representing a significant decrease of 6 % (P < 0.001). The mean pronation was identical with 89° (range, 80–90°) on both arms. There were no significant differences in ROM for flexion (P = 0.09), extension (P = 0.44), and pronation (P = 0.63) when compared with the uninjured arm.
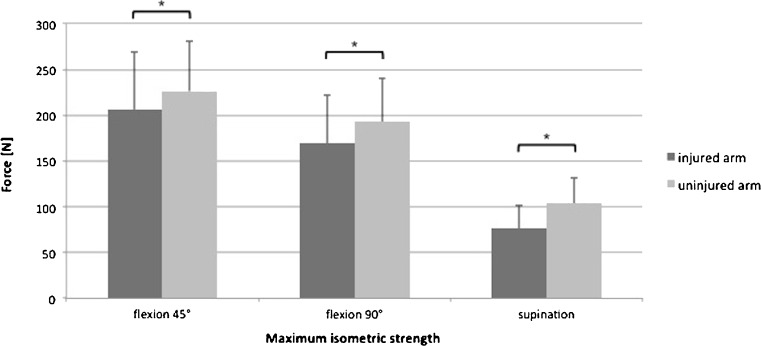
The results of maximum isometric strength testing compared to the uninjured side are presented in Fig. 2. There were significant differences with a mean strength deficit of the operated arm of –9.7 ± 20.3 % (P = 0.002) for elbow flexion at 45°, with –13.7 ± 16.5 % (P < 0.001) for elbow flexion at 90°, and –36.4 ± 35.6 % (P < 0.001) for supination. Mean strength measurements were not statistically different between patients with dominant arm injury and those with non-dominant arm injury (at 45° of elbow flexion, P = 0.07; at 90° of elbow flexion, P = 0.05; for supination, P = 0.84).
Fig. 2.
Maximum isometric strength for both the injured and the uninjured arm
Scores
The mean MES for all 49 patients was 97.2 ± 4.9 points (range, 76.5–100) representing overall 39 excellent outcomes, nine good outcomes, one fair, and no poor outcome. The mean QuickDASH was 7.9 ± 13.9 points (range, 0–59). Related to both scoring systems, no statistical differences were seen between dominant and non-dominant arm injuries (MES, P = 0.36; QuickDASH, P = 0.44).
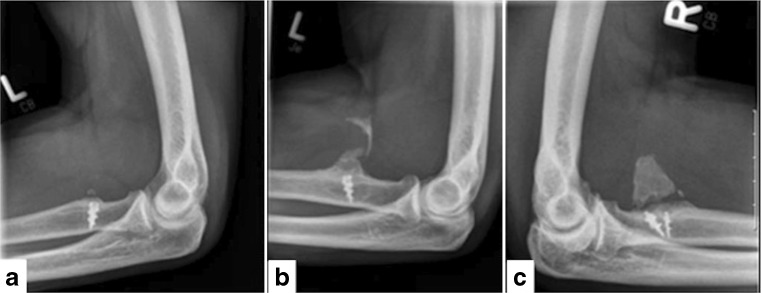
Radiographic evaluation
At the latest follow-up, different types of HO were observed in 19 patients (39 %); in three (6 %) patients minimal HO were seen at the region of bicipital tuberosity, in eight (16 %) patients HO were detected within both the reattached biceps tendon and its distal insertion, and marked HO were located within the reattached tendon in eight (16 %) patients as well (Fig. 3). According to the classification system described by Hastings and Graham [16], all HO seen in this study were graded as type 1 without resultant loss of elbow or forearm ROM. Neither for strength testing (at 45° of elbow flexion, P = 0.22; at 90° of elbow flexion, P = 0.65; for supination, P = 0.65) nor for evaluated scores (MES, P = 0.64; QuickDASH, P = 0.64), differences were seen for patients presenting with HO at the tendinous insertion site when compared to patients without HO (n =30).
Fig. 3.
a–c Classification of three different types of heterotopic ossifications (HO) presented at the bicipital tuberosity and/or within the reattached biceps tendon (a) type 1: HO of insertion site, (b) type 2: HO of insertion site and reattachted distal biceps tendon, (c) type 3: HO of reattached distal biceps tendon
Complications
There was an overall rate of 10.2 % (five of 49 patients) of hardware complications. Initially, one suture anchor had to be revised due to dislocation two days after surgery. In two patients, a dislocation of one suture anchor, and in two other patients, a dislocation of both implanted anchors were observed at final follow-up. Based on the patient’s medical records, we could not reveal any reason for these anchor failures. Interestingly, the patients did not report any acute or insidious onset of pain or biceps muscle weakness within the postoperative course. At the time of survey, these patients reported no complaints due to pain or restrictions in elbow flexion or supination strength.
In three patients, transient altered sensations of the LACN and in two other patients, transient palsies of the posterior interosseous nerve (PIN) were postoperatively apparent, but resolved completely in these cases within four to eight months. At the time of follow-up, nerve deficits did not exist in any case. Overall, there were four (8.2 %) wound complications with a superficial wound infection in three cases and one deep infection that had to be revised surgically (the one patient presenting with a fair MES).
Discussion
The most important finding of the present study was that despite a high patient’s satisfaction rate (86 % of our patients were highly satisfied or satisfied with their postoperative outcome), near preinjury ROM values after surgery and a high functional outcome scoring, but a significant decrease in elbow flexion and supination strengths, and an increased rate of HO was evident.
According to patient’s subjective satisfaction, McKee et al. [12] reported on 96 % very satisfied and somewhat satisfied patients in one of the largest series of 53 patients following single-incision suture anchor repair. This satisfaction rate was slightly higher than in our study group. Khan et al. [17] described that all patients were satisfied following a single-incision suture anchor technique after a mean follow-up of 45 months. In their retrospective review, however, the authors did not differentiate different levels of satisfaction and they surveyed a smaller series of only 17 patients. With special regard to elbow ROM, either single-incision and double-incision repair techniques have shown similar clinical results in the last decade [3]. In detail, the reported mean values range from 1° to 7° for extension and from 126° to 145° for flexion after surgery. In our cohort, the average extension-flexion arc was 1–133° representing no significance in comparison to the uninjured arm. In various studies, mean supination values vary between 62° and 83° following surgery, whereas mean pronation values are reported as widely consistent with 75–85° [3]. In our patients, the mean supination and pronation motions were 84° and 89°, respectively. This reflects comparable results to studies cited above. Even though, we revealed a significant supination deficit of 3° on average compared to the contralateral arm, its clinical relevance seems to be low. Interestingly, patients presenting with HO had no restriction for elbow motion when compared to patients without HO.
The mean MES was 97 points for all patients presenting only one fair result. According to this scoring system, 48 of 49 patients had excellent and good results. These elbow scoring results are comparable to other published studies using the Mayo elbow performance score (MEPS) [18–20]. With an average QuickDASH of 7.9 points, indicating a low level of upper extremity disability, our findings compare favourably with those of the literature [12, 17, 21]. For comparison, Hudak et al. [22] reported on an average DASH score of 6.2 points from a series of healthy individuals. Khan et al. [17] revealed a DASH score of 14.5 points after suture anchor repair, which was slightly inferior to our series. In contrast, Cil et al. [23] and Banerjee et al. [24] reported excellent DASH scores of 3.6 and 1.9 points, respectively.
In multiple outcome studies, objective measurements for flexion and supination strengths were obtained postoperatively. The reported loss of flexion strength ranges between 5 % and 10 % compared to the contralateral arm and between 5 % and 20 % for supination strength, respectively [10, 12, 18, 23, 25]. In our patients, however, we found a higher loss of isometric flexion strength of −9.7 % (at 45° of elbow flexion) and −13.7 % (at 90° of elbow flexion) as well as −36.4 % of isometric supination strength. In a systematic review, Chavan et al. [26] defined a restoration strength of at least 80 % of the contralateral extremity as a satisfactory outcome. Based on this outcome parameter, an unsatisfactory result as a whole in our patients would be stated, even though this deficit is not displayed in the evaluated scores. In addition, it is a debatable point whether maximum isometric supination strength plays a relevant role in routine daily activities. And, it has to be mentioned that different strength measurements (isokinetic and isometric strength, endurance, and grade of strength) for different arm positions have been used in various studies, which complicates an objective comparability [9–12, 18, 21, 25, 27]. Nevertheless, it has to be clearly accentuated that a supination strength deficit of −36 % presented in this study is comparable to those results of nonoperative management [5, 28, 29]. We only can speculate whether our findings in strength measurements may result from an inadequate initial tendon reattachment with suboptimal suture anchor positioning and/or from an inferior compliance in the early postoperative period that facilitates an elongated tendon healing. Indeed, Schmidt et al. [21] have shown that a more anterior reattachment resulting from a single-incision anterior approach causes less forearm supination torque when compared to uninjured controls with a physiological attachment site. In this context, current anatomical studies have demonstrated that some specimens are probably not repairable in an anatomical position using a single-incision technique [30, 31]. In their series, Schmidt et al. [21] found a statistically significant difference in supination strength between injured and uninjured sides presenting a 33 % loss of supination strength with the forearm in 60° of supination. The same authors have biomechanically verified that repairing the distal biceps tendon to a location anteriorly to its anatomic position resulted in a 97 % decrease in biceps supination strength with the elbow in 60° of supination and a 27 % decrease in strength in a neutral position, whereas no significant decrease was found in 60° of pronation [32]. In addition, in 49 % of evaluated patients in our study, the non-dominant arm was involved, which could even be an explanation for reduced strength measurements. This incidence was much higher than the reported demographic data in the literature [1]. As a consequence of the present results, patients have to be informed for possible persistent strength weakness after suture anchor repair via a single-incision approach.
Many authors refer to HO as complications [3, 33]. Chavan et al. [26], however, defined HO as a complication only in case of associated pain or a loss of greater than 30° of motion in any plane. Unlike other single-incision studies, all patients were routinely evaluated for postoperative HO in this study [12, 24]. This might be the reason that we observed such a notable number, i.e. in 39 % of the cases. Greenberg et al. [10] also noted a comparable rate of 35 % of postoperative HO (five of 14 patients) after single-incision cortical button repair. In accordance with previous studies, the prevalence of HO revealed in this study (in all patients graded as type 1 according to Hastings & Graham [16] without functional restrictions) did not affect the functional outcome [10, 18, 21]. However, several studies reported on a significantly lower prevalence between 3 % and 9 % [7, 17, 34]. In the first prospective randomized trial for distal biceps tendon repair, Grewal et al. [35] compared the functional outcome of the single-incision approach using suture anchors versus (n = 47) double-incision technique utilizing transosseous tunnels (n = 44). They noticed only two cases of HO and assumed that the low prevalence of HO was probably due to the postoperative use of Indomethacin, which was prescribed for HO prophylaxis in 61 of 91 patients. Due to our retrospective study design, we were unable to verify whether and how many patients received HO prophylaxis within the ambulatory period. Similarly, the prophylactic use of Indomethacin or nonsteroidal anti-inflammatory drugs (NSAID) is unreported for the majority of recent studies. Due to the high rate of HO seen in this study, the prophylactic use of Indomethacin was now defined as a standard for our postoperative management of distal biceps tendon repair.
Another interesting finding of the present study was a relatively high complication rate, which is in contrast to most studies on distal biceps tendon repair using suture anchors via a single-incision approach. In our research of the literature, anchor failure after distal biceps tendon repair was not previously reported in clinical studies. In our series, the patients could not define a specific event associated with the return of symptoms that may cause these four implant failures. However, the compliance of these patients within the postoperative period could retrospectively not be valuated. Therefore, we only can speculate for a prematurely active load to the repaired distal biceps tendon that results in a gradual anchor pullout. A variety of biomechanical studies determined inferior failure strengths for diverse suture anchor implants when compared to other repair techniques [36–38]. For suture anchor repair, moreover, where the tendon is reattached to the surface of the bicipital tuberosity, Mazzocca et al. [39] pointed out a predisposition for tendon dislocation when compared to techniques where the tendon is inserted within the bicipital tuberosity (Endobutton technique, interference screw fixation).
In the present study, the overall incidence of nerve dysfunctions was 10.2 % (five of 49 patients), but transient in all cases. PIN palsies are considered as major complications by most authors, whereas LACN paresthesia and radial sensory nerve (RSN) paresthesia are regarded as minor complications. It might be that PIN injuries that were seen in this study (4 %) are caused by the fixation technique itself. If the posterior cortex is drilled through or penetrated by the anchor, the PIN may be also at risk of iatrogenic damage during surgical procedure [40]. Other authors also reported PIN injuries (3 %) following suture anchor repair with a comparable incidence [33]. It is stated that the anterior single-incision approach may be at higher risk for palsies of the LACN or the RSN than in double-incision approaches due to a required wider exposure of the bicipital tuberosity [27]. However, in a systematic review, Keener [3] reported on an overall incidence of postoperative nerve complications of 5.7 % for single-incision repair techniques and a comparable incidence of 6.5 % for double-incision muscle-splitting approaches. The two largest series of single-incision suture anchor repair of McKee et al. [12] and John et al. [34] had a reported mean incidence of 5.7 % (three of 53 patients) and 1.9 % (one of 53 patients), respectively. In 2000, Kelly et al. [7] reported on the largest series of 74 patients with primarily repaired distal biceps tendon ruptures following a modified muscle-splitting two-incision technique. The authors described a rate of 8.1 % including the LACN (n = 3), the RSN (n = 2) and the PIN (n = 1). However, El Hawary et al. [27] found transient paresthesia of the LACN in 33 % of their cases after suture anchor repair. Banerjee et al. [24], in a recent study, reported a high rate of nerve deficits (29 %) following cortical button repair including four transient PIN palsies and two persistent lesions of the RSN.
A variety of surgeons performed the distal biceps tendon repair within our study period. The injury’s low incidence and the resulting small experience per surgeon may explain our results at least in parts. As a consequence of these findings, we recommend that distal biceps tendon repair should be performed only by experienced upper extremity surgeons in order to avoid procedure-related pitfalls.
This study has some limitations represented by its retrospective design and the lack of a pre-study power analysis. It has to be stated that the number and variety of used anchors and suture types may be a confounding factor for functional outcome. The variety of used implants is caused by the long inclusion period of ten years. Furthermore, this study did not examine the repair integrity (tendon reattachment site, anchor positioning), which has to be stated as a weakness. In addition, we did not perform a detailed subgroup analysis to correlate different outcome parameters among each other (delayed surgery, presence of HO, hardware failure, etc.). On the other hand, this study has several strengths. It exclusively presents subjective and objective outcome measures including functional scoring as well as radiological evaluation and isometric strength testing of all examined patients. Diverse outcome studies with comparable sample sizes did not perform objective muscle strength testing in all or only in some cases [11, 12, 20, 34]. Moreover, this study comprises one of the largest series of patients following single-incision suture anchor repair with a minimum follow-up of 12 months and a low rate of patients lost to follow-up.
To sum up, single-incision suture anchor repair provides a high patient’s satisfaction and good results with respect to ROM and functional scoring. Nevertheless, the patient has to be informed of postoperative HO, especially for supination strength weakness after surgery. Based on our experience presented in this study, we strongly recommend that distal biceps tendon repair should be reserved for practised upper extremity surgeons to avoid procedure-related complications.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Miyamoto RG, Elser F, Millett PJ. Distal biceps tendon injuries. J Bone Joint Surg Am. 2010;92:2128–2138. doi: 10.2106/JBJS.I.01213. [DOI] [PubMed] [Google Scholar]
- 2.Hetsroni I, Pilz-Burstein R, Nyska M, et al. Avulsion of the distal biceps brachii tendon in middle-aged population: is surgical repair advisable? A comparative study of 22 patients treated with either nonoperative management or early anatomical repair. Injury. 2008;39:753–760. doi: 10.1016/j.injury.2007.11.287. [DOI] [PubMed] [Google Scholar]
- 3.Keener JD. Controversies in the surgical treatment of distal biceps tendon ruptures: single versus double-incision repairs. J Shoulder Elbow Surg. 2011;20:113–125. doi: 10.1016/j.jse.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Boyd HB, Anderson LD. A method for reinsertion of the distal biceps brachii tendon. J Bone Joint Surg Am. 1961;43:1041–1043. [Google Scholar]
- 5.Morrey BF, Askew LJ, An KN, Dobyns JH. Rupture of the distal biceps tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg Am. 1985;67:418–421. [PubMed] [Google Scholar]
- 6.Failla JM, Amadio PC, Morrey BF, Beckenbaugh RD. Proximal radioulnar synostosis after repair of distal biceps brachii rupture by two-incision technique: report of four cases. Clin Orthop Relat Res. 1990;253:133–136. [PubMed] [Google Scholar]
- 7.Kelly EW, Morrey BF, O’Driscoll SW. Complications of repair of the distal biceps tendon with the modified two-incision technique. J Bone Joint Surg Am. 2000;82:1575–1581. doi: 10.2106/00004623-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Rantanen J, Orava S. Rupture of the distal biceps tendon: a report of 19 patients treated with anatomic reinsertion, and a meta-analysis of 147 cases found in the literature. Am J Sports Med. 1999;27:128–132. doi: 10.1177/03635465990270020201. [DOI] [PubMed] [Google Scholar]
- 9.Fenton P, Qureshi F, Ali A, Potter D. Distal biceps tendon rupture: a new repair technique in 14 patients using the biotenodesis screw. Am J Sports Med. 2009;37:2009–2015. doi: 10.1177/0363546509335465. [DOI] [PubMed] [Google Scholar]
- 10.Greenberg JA, Fernandez JJ, Wang T, Turner C. EndoButton-assisted repair of distal biceps tendon ruptures. J Shoulder Elbow Surg. 2003;12:484–490. doi: 10.1016/S1058-2746(03)00173-3. [DOI] [PubMed] [Google Scholar]
- 11.Heinzelmann AD, Savoie FH, 3rd, Ramsey JR, Field LD, Mazzocca AD. A combined technique for distal biceps repair using a soft tissue button and biotenodesis interference screw. Am J Sports Med. 2009;37:989–994. doi: 10.1177/0363546508330130. [DOI] [PubMed] [Google Scholar]
- 12.McKee MD, Hirji R, Schemitsch EH, Wild LM, Waddell JP. Patient-oriented functional outcome after repair of distal biceps tendon ruptures using a single-incision technique. J Shoulder Elbow Surg. 2005;14:302–306. doi: 10.1016/j.jse.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Germann G, Harth A, Wind G, Demir E. Standardisation and validation of the German version 2.0 of the disability of arm, shoulder, hand (DASH) questionnaire. Unfallchirurg. 2003;106:13–19. doi: 10.1007/s00113-002-0456-x. [DOI] [PubMed] [Google Scholar]
- 14.Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7:44. doi: 10.1186/1471-2474-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morrey BF, An KN, Chao EYS. Functional evaluation of the elbow and its disorders. Philadelphia: In: Morrey BF (ed) The elbow and its disorders. WB Saunders; 1985. pp. 73–91. [Google Scholar]
- 16.Hastings H, 2nd, Graham TJ. The classification and treatment of heterotopic ossification about the elbow and forearm. Hand Clin. 1994;10:417–437. [PubMed] [Google Scholar]
- 17.Kahn AD, Penna S, Yin Q, et al. Repair of distal biceps tendon ruptures using suture anchors through a single anterior incision. Arthroscopy. 2008;24:39–45. doi: 10.1016/j.arthro.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 18.Peeters T, Ching-Soon NG, Jansen N, et al. Functional outcome after repair of distal biceps tendon ruptures using the endobutton technique. J Shoulder Elbow Surg. 2009;18:283–287. doi: 10.1016/j.jse.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Eardley WG, Odak S, Adesina TS, Jeavons RP, McVie JL. Bioabsorbable interference screw fixation of distal biceps ruptures through a single anterior incision: a single-surgeon case series and review of the literature. Arch Orthop Trauma Surg. 2010;130:875–881. doi: 10.1007/s00402-009-0974-x. [DOI] [PubMed] [Google Scholar]
- 20.Hartman MW, Merten SM, Steinmann SP. Mini-open 2-incision technique for repair of distal biceps tendon ruptures. J Shoulder Elbow Surg. 2007;16:616–620. doi: 10.1016/j.jse.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 21.Schmidt CC, Diaz VA, Weir DM, Latona CR, Miller MC. Repaired distal biceps magnetic resonance imaging anatomy compared with outcome. J Shoulder Elbow Surg. 2012;21:1623–1631. doi: 10.1016/j.jse.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 22.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH. Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 23.Cil A, Merten S, Steinmann SP. Immediate active range of motion after modified 2-incision repair in acute distal biceps tendon rupture. Am J Sports Med. 2009;37:130–135. doi: 10.1177/0363546508323749. [DOI] [PubMed] [Google Scholar]
- 24.Banerjee M, Shafizadeh S, Bouillon B, et al. High complication rate following distal biceps refixation with cortical button. Arch Orthop Trauma Surg. 2013;133:1361–1366. doi: 10.1007/s00402-013-1819-1. [DOI] [PubMed] [Google Scholar]
- 25.Weinstein DM, Ciccone WJ, II, Buckler MC, et al. Elbow function after repair of the distal biceps brachii tendon with a two-incision approach. J Shoulder Elbow Surg. 2008;17:82–86. doi: 10.1016/j.jse.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 26.Chavan PR, Duquin TR, Bisson LJ. Repair of the ruptured distal biceps tendon: a systematic review. Am J Sports Med. 2008;36:1618–1624. doi: 10.1177/0363546508321482. [DOI] [PubMed] [Google Scholar]
- 27.El Hawary R, Macdermid JC, Faber KJ, Patterson SD, King GJ. Distal biceps tendon repair: comparison of surgical techniques. J Hand Surg [Am] 2003;28:496–502. doi: 10.1053/jhsu.2003.50081. [DOI] [PubMed] [Google Scholar]
- 28.Freeman CR, McCormick KR, Mahoney D, Baratz M, Lubahn JD. Nonoperative treatment of distal biceps tendon ruptures compared with a historical control group. J Bone Joint Surg Am. 2009;91:2329–2334. doi: 10.2106/JBJS.H.01150. [DOI] [PubMed] [Google Scholar]
- 29.Geaney LE, Brenneman DJ, Cote MP, Arciero RA, Mazzocca AD. Outcomes and practical information for patients choosing nonoperative treatment for distal biceps ruptures. Orthopedics. 2010;33:391. doi: 10.3928/01477447-20100429-10. [DOI] [PubMed] [Google Scholar]
- 30.Forthman CL, Zimmerman RM, Sullivan MJ, Gabel GT. Crosssectional anatomy of the bicipital tuberosity and biceps brachii tendon insertion: relevance to anatomic tendon repair. J Shoulder Elbow Surg. 2008;17:522–526. doi: 10.1016/j.jse.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 31.Jobin CM, Kippe MA, Gardner TR, Levine WN, Ahmad CS. Distal biceps tendon repair: a cadaveric analysis of suture anchor and interference screw restoration of the anatomic footprint. Am J Sports Med. 2009;37:2214–2221. doi: 10.1177/0363546509337451. [DOI] [PubMed] [Google Scholar]
- 32.Schmidt CC, Weir DM, Wong AS, Howard M, Miller MC. The effect of biceps reattachment site. J Shoulder Elbow Surg. 2010;19:1157–1165. doi: 10.1016/j.jse.2010.05.027. [DOI] [PubMed] [Google Scholar]
- 33.Cain RA, Nydick JA, Stein MI, et al. Complications following distal biceps repair. J Hand Surg [Am] 2012;37:2112–2117. doi: 10.1016/j.jhsa.2012.06.022. [DOI] [PubMed] [Google Scholar]
- 34.John CK, Field LD, Weiss KS, Savoie FH., 3rd Single incision repair of acute distal biceps ruptures by use of suture anchors. J Shoulder Elbow Surg. 2007;16:78–83. doi: 10.1016/j.jse.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 35.Grewal R, Athwal GS, MacDermid JC, et al. Single versus double-incision technique for the repair of acute distal biceps tendon ruptures: a randomized clinical trial. J Bone Joint Surg Am. 2012;94:1166–1174. doi: 10.2106/JBJS.K.00436. [DOI] [PubMed] [Google Scholar]
- 36.Kettler M, Lunger J, Kuhn V, Mutschler W, Tingart MJ. Failure strengths in distal biceps tendon repair. Am J Sports Med. 2007;35:1544–1548. doi: 10.1177/0363546507300690. [DOI] [PubMed] [Google Scholar]
- 37.Pereira DS, Kvitne RS, Liang M, Giacobetti FB, Ebramzadeh E. Surgical repair of distal biceps tendon ruptures: a biomechanical comparison of two techniques. Am J Sports Med. 2002;30:432–436. doi: 10.1177/03635465020300032101. [DOI] [PubMed] [Google Scholar]
- 38.Siebenlist S, Buchholz A, Zapf J et al (2013) Double intramedullary cortical button versus suture anchors for distal biceps tendon repair: a biomechanical comparison. Knee Surg Sports Traumatol Arthrosc. Jul 6. [Epub ahead of print] [DOI] [PubMed]
- 39.Mazzocca AD, Burton KJ, Romeo AA, et al. Biomechanical evaluation of 4 techniques of distal biceps brachii tendon repair. Am J Sports Med. 2007;35:252–258. doi: 10.1177/0363546506294854. [DOI] [PubMed] [Google Scholar]
- 40.Saldua N, Carney J, Dewing C, Thompson M. The effect of drilling angle on posterior interosseous nerve safety during open and endoscopic anterior single-incision repair of the distal biceps tendon. Arthroscopy. 2008;24:305–310. doi: 10.1016/j.arthro.2007.09.016. [DOI] [PubMed] [Google Scholar]