Abstract
Purpose
Despite previous studies the management of Rockwood type III acromioclavicular (AC) dislocations remains controversial and the debate continues about whether patients with Rockwood type III AC injuries should be treated conservatively or operatively. In this study, we will review the current literature and present an overview of the outcome of conservative versus operative treatment of Rockwood type III dislocations.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines was used to conduct this review. A systematic search was performed in the Pubmed, Cochrane library, Embase, Scopus and Cumulative Index to Nursing and Allied Health Literature databases. Titles and abstracts were screened using predefined criteria and articles were critically appraised on relevance and validity.
Results
After critical appraisal eight articles were included in the study. The objective and subjective shoulder function outcome was better in the operative group, especially in young adults, though the rate of complications and radiographic abnormalities were higher. The rehabilitation time was shorter in the conservative group, however the cosmetic outcome was worse.
Conclusions
This review showed no conclusive evidence for the treatment of Rockwood type III AC dislocations. Overall, physically active young adults seem to have a slight advantage in outcome when treated operatively.
Keywords: Acromioclavicular, Rockwood, III/3, Conservative, Operative, Dislocation
Introduction
The management of Rockwood grade III acromioclavicular (AC) dislocations remains controversial. Conservative treatment shows excellent results and a painless shoulder function. However, the dislocation is not actively reduced and will maintain in a prominent position in the majority of the patients. Furthermore, some patients suffer from chronic instability and pain [1, 2]. These shortcomings might be prevented when treated operatively. With surgical treatment the dislocation, with the upstanding collar bone, can be actively reduced to achieve anatomical correction and the best function and shape of the shoulder. However, this treatment might compromise the function of the shoulder [1, 3].
In most cases the choice of treatment depends on the preference of the treating surgeon or the choice of the patients: young active patients prefer surgery and elderly patients prefer conservative treatment. Choice of treatment is even geographically determined. In Germany the majority are treated surgically in contrast to the United States of America where conservative treatment is preferred [4].
Also in the literature, there is still no consensus regarding the treatment of Rockwood type III AC dislocations. The difficulty lies in the different definitions of grade III AC dislocations used in the current studies. There are multiple classifications for the description of AC dislocations. Common classifications for AC dislocations are the Allman [5], Tossy et al. [6] and Rockwood et al. [7] classifications. Allman and Tossy et al. describe three grades of AC dislocation. The more recent classification of Rockwood et al. classified the AC dislocations into six types. Allman’s and Tossy’s classification grades I and II correspond with Rockwood’s type I and II. Rockwood, however, made a further subdivision of Allman’s and Tossy’s grade III into Rockwood type III–VI.
Types I and II are widely accepted as best managed conservatively [3, 8] and there seems to be a consensus that type IV–VI should be treated operatively [7, 9–11]. The best treatment for Rockwood type III dislocations is, despite numerous trials and reviews, still unclear. Some advocate surgical treatment in young physically active adults to maintain good power [12, 13], others prefer conservative treatment because of the lower complication rate and recovery time [1, 14] and other studies showed no difference in outcome between the conservatively and operatively treated patients [9, 15].
Several studies have aimed to investigate the best treatment for type III AC dislocations, conservative versus operative treatment [16–19]. However, no distinction was made in these studies between the different classifications of type III dislocations. This results in several types of AC dislocations within a single study group which gives a skewed result of the outcome of type III dislocations.
Despite previous have studies the debate continues whether patients with Rockwood type III AC injuries should be treated conservatively or operatively. In this study, we will review the current literature and present an overview of the outcome of conservative versus operative treatment of Rockwood type III dislocations.
Materials and Methods
Search and selection
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines was used to conduct this review [20]. On the 24th of April 2013 we conducted an extensive systematic search of the published literature in the Pubmed, Cochrane library, Embase, Scopus and Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases. We used the search terms ‘acromio’ and ‘clavicular’ for domain and ‘operative’ and ‘conservative’ for determinant and all variations and combinations of these terms in the title and abstract. Furthermore we added the search term ‘III/three/3’ in all text fields to be able to specify the search without limiting it. All studies meeting the search terms were included.
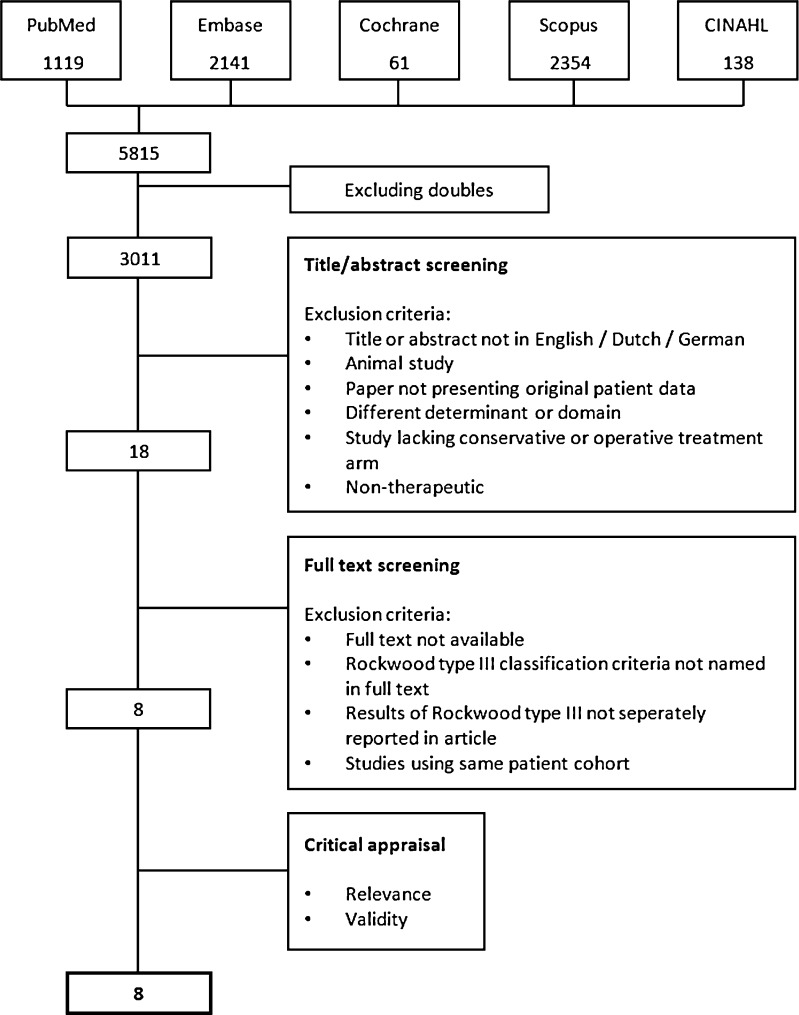
Prior to the selection of relevant articles, all double articles were excluded. Two reviewers (KK, AG) independently assessed methodological quality and extracted outcome data. First, title and abstract were screened and articles were excluded by the exclusion criteria shown in Fig. 1. Second, full text copies were obtained and screened of all potentially relevant studies using the criteria shown in Fig. 1. Discrepancies in this exclusion process between the two reviewers was resolved by consensus. The references of the remaining articles were identified using Web of Science and screened using the same criteria.
Fig. 1.
Flowchart
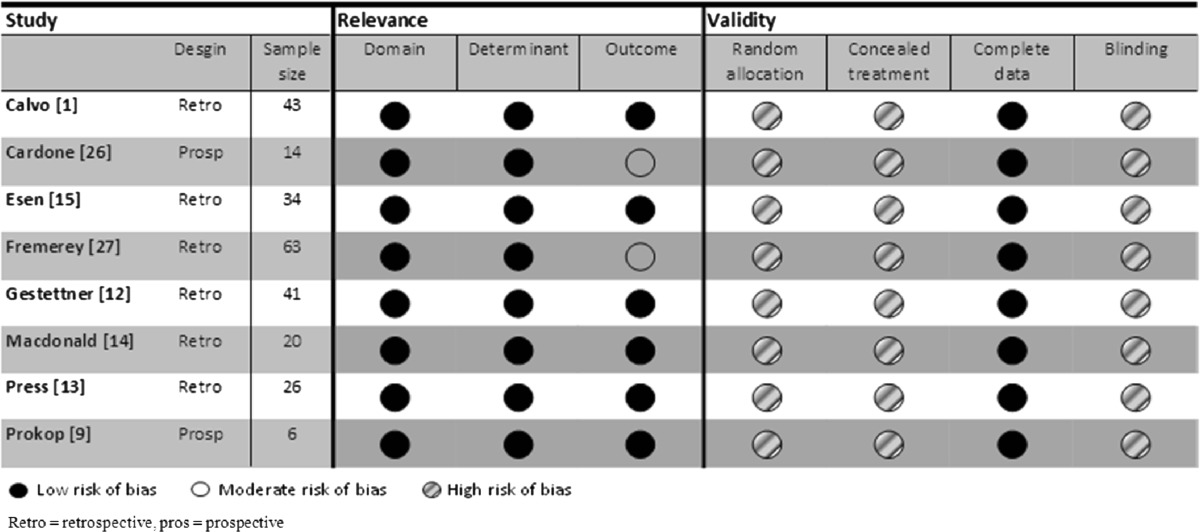
The articles were independently appraised by two authors (KK, AG) on relevance and validity. Appraisal was performed using the criteria of the Centre for Evidence Based Medicine of the University of Oxford [21]. Articles including more types of Rockwood AC dislocations were selected when the results of the Rockwood type III AC dislocation was separately presented.
Outcomes of interest
In order to evaluate all published literature we were interested primarily in all objective clinical outcomes (e.g. Constant-Murley score [22], Imatani score [23], Poigenfurst score [15], ULCA score [24], Taft score [25]), radiological assessments and complication rates and secondly all subjective outcomes (e.g. health related quality of life, pain, shoulder function, cosmetic outcome, return to previous work/sport/activities).
Data analysis
The preferred analysis was to pool the results of the studies. Homogeneity will be determined with eyeballing. In the case of incomparable outcomes or study groups we will combine comparable patients from different study groups in order to achieve a significant number of patients and perform subgroup analyses. Statistical analysis was performed using SPSS version 20.0 (SPSS Inc. Chicago, Illinois, USA) for Windows. A p-value <0.05 was considered significant.
Results
Search strategy results
Initially 5,815 articles were retrieved from the databases. After excluding doubles and applying the inclusion and exclusion criteria 18 articles were relevant for full text screening. After screening and critically appraising the full text of the remaining articles (Table 1), eight studies were eligible for this study (Fig. 1) [1, 9, 12–15, 26, 27]. None of the articles were randomised trials, six were retrospective cohort studies [1, 12–15, 27] and two were prospective cohort studies [9, 26].
Table 1.
Critical appraisal study designs
In the absence of homogeneity between the studies, we were not able to pool all the results of the studies. However, to be able to make evident assumptions of the results, we combined patients from different studies with comparable outcomes.
Study characteristics
Amalgamated, 142 patients were managed operatively and 105 patients conservatively. Age ranged from 16 to 68 years in the operative group and 14–69 years in the conservative group. The mean follow-up time differed between study groups. With the exception of one study [14], all studies had a minimum follow-up time of 12 months. The follow-up time ranged from 6.3 to 122.8 months in the operative group and 5.7–78 months in the conservative group. A wide range of surgical techniques were described. In three studies the biodegradable PDS cord was used to stabilise the AC-junction [9, 26, 27]. In two studies the (modified) Weaver and Dunn technique was applied [13, 15]. In the remaining three studies the operative procedure was performed with Bosworth screw fixation, or Steinmann or Knowles pinning [14], an AC-hookplate [12] and the modified Phemister procedure [1]. Postoperative management comprised a sling or bandage.
The conservative treatments consisted of immobilisation management with a sling or bandage. In both groups the treatment was extended with analgesics and physiotherapy when indicated. All these findings are presented in Table 2.
Table 2.
Study characteristics
| Study | Design | Population (n) | Gender (♂/♀) | Mean age (years) | Mean follow-up (months) | Surgical technique | Conservative technique | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Surg | Cons | Surg | Cons | Surg | Cons | Surg | Cons | ||||
| Calvo et al. [1] | Retro | 32 | 11 | 27/5 | 11/0 | 39.6 | 34.5 | 122.8 | 40.5 | Modified Phemister | Sling 2 wks, physio afterwards |
| Cardone et al. [26] | Prosp | 8 | 6 | 8/0 | 6/0 | 26.7 | 29 | 44.8 | 29.5 | Open reduction, PDS banding | Sling until comfortable, physio |
| Esen et al. [15] | Retro | 17 | 17 | 12/5 | 12/5 | 46.9 | 40.4 | 36.1 | 29.6 | Modified Weaver & Dunn | AC-bandage, physio from start |
| Fremerey et al. [27] | Retro | 32 | 31 | UK | UK | 35.9 | 33.7 | 6.1 yrs | 6.5 yrs | PDS banding | Link bandage 4–6 wks/sling 6–12 days, physio when comfortable |
| Gstettner et al. [12] | Retro | 24 | 17 | UK | UK | 37.2 | 36.2 | 32.1 | 36.8 | AC Hook plate | Sling, physio when comfortable |
| Macdonald et al. [14] | Retro | 10 | 10 | 10/0 | 10/0 | 25 | 31.7 | 6.3 | 5.7 | Bosworth screw, Steinmann/Knowles pin | Sling immobilisation |
| Press et al. [13] | Retro | 16 | 10 | 12/4 | 9/1 | 30.7 | 49.6 | 32.3 | 33.4 | Weaver & Dunn | Sling, physio when comfortable |
| Prokop et al. [9] | Prosp | 3 | 3 | 2/1 | 3 | 37 | 30.3 | 16 | 19.3 | PDS banding | Gilchrist bandage, physio when comfortable |
retro retrospective, prosp prospective, surg surgical, cons conservative, UK unknown, physio physiotherapy
Subgroup analysis
Shoulder function
In four studies [1, 9, 12, 15] the objective shoulder function was assessed using an objective scoring system, the Constant score [22], Imatani score [23], Poigenfurst score [15], and Taft score [25]. With the scoring systems patients were scored for pain, function, movement, strength and radiological findings. Because different scoring systems were used we were not able to combine the results and statistically analyse the summarised outcomes in the operatively and conservatively treated patients. The majority of the studies [1, 9, 15] showed comparable results, i.e. no significant difference between the treatment groups. Gstettner et al. [12] presented a significant difference in Constant score in favour of the operative group, i.e. excellent versus good shoulder function (Table 3).
Table 3.
Objective shoulder scoring systems
| Study | Scoring system | Max. points | Operative score (SD) | Operative mean outcome | Conservative score (SD) | Conservative mean outcome | P-value |
|---|---|---|---|---|---|---|---|
| Calvo et al. [1] | Imatani score | 100 | 93.7 (±9.9) | Excellent | 94.1 (±12) | Excellent | 0.71 |
| Esen et al. [15] | Poigenfurst score | Excellent | 7 Excellent, 10 good | Good | 9 Excellent, 8 good | Excellent | 0.492 |
| Gstettner et al. [12] | Constant score | 100 | 90.4 (12.9) | Excellent | 80.7 (17.4) | Good | 0.029* |
| Prokop et al. [9] | Taft score | 12 | 10.7 | Excellent | 10.3 | Excellent | NA |
NA not available, SD standard deviation
*Statistically significant (p <0.05)
In three studies [13, 14, 26] a subjective shoulder function was assessed using a questionnaire, with the items pain, function, stiffness, and cosmetic outcome. The minimum score was one (poor outcomes) and the maximum score was four (excellent outcome). The surgically treated patients scored a higher mean average (3.13) in comparison with the conservative group (2.77; p = 0.406). The difference in subjective shoulder function is mainly caused by the scores of the cosmetic outcome and deformity, which were better in the operative group in the individual studies.
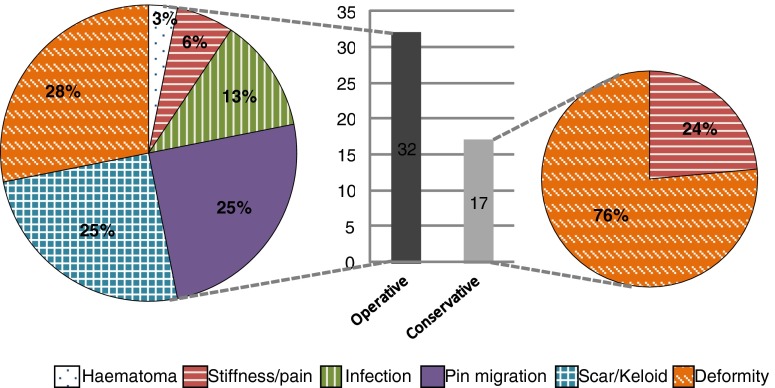
Complications
The complication rate was presented in seven studies [1, 9, 12, 13–15, 27]. Altogether, 49 complications were reported, 32 in the operative and 17 in the conservative group. The most frequently observed complications were deformities, pin migration and a keloid or unattractive scar (Fig. 2). Obviously, infections, pin migration and scar or keloid were only present in the surgical patient group.
Fig. 2.
Complication rate
A complication was considered clinically relevant when a surgical revision or other additional treatment was indicated. All six patients with this indication were first managed surgically, which suggests that almost 19 % of the complications in the surgical treatment group are considered clinically relevant.
Radiological outcomes
The radiological outcomes, degree of reduction, osteoarthritis, and calcifications, were examined in three studies [1, 12, 27]. The incidence of osteoarthritis and calcification of the ligament, was higher in the operative group, however not significant (1.412, p = 0.312; 1.966, p = 0.161). In the individual studies, Calvo et al. [1] described a significantly higher incidence of AC osteoarthritis and CC-ligament ossification and a higher number of complete reduction of the dislocation in the operative treatment group. This corresponds with the results of the studies of Gstettner et al. [12] and Fremerey et al. [27], which both showed better anatomical recovery in the operative treatment group.
Cosmetic outcome
Four studies reported the deformities and cosmetic outcomes [1, 13, 14, 25]. The overall evident deformities and the cosmetic complaints about deformities were significantly higher in the conservative treatment group than operative treatment group, respectively, 84 % and 18 % (p < 0.001).
Rehabilitation time
Various outcomes, such as time to return to work, to sports, and recreational activities, were used in the studies to measure the rehabilitation time. In order to evaluate the rehabilitation time we aimed to combine the outcomes into time to return to the normal daily activities. However, all studies used different outcome measurements. Cardone et al. [26] showed that the time to return to the pre-injury sports level was in favour of the surgical group (18.8 versus 26.2 weeks), despite the fact that these patients had a longer rehabilitation time before they were able to return to their sports training at all (6.3 versus 2.4 weeks). Gstettner et al. [12] demonstrated that 4/19 (21 %) patients in the operative treatment group versus 4/15 (27 %) patients in the conservative treatment group were not able to return to their previous sports level. Furthermore, 1/24 (4.1 %) of the surgically managed patients and 3/17 (17.6 %) of the conservatively managed patients were not able to return to their former level of activity at work. In the study of Press et al. [13] a significantly longer rehabilitation time for work and recreational activities was seen in the surgical group, respectively, 2.6 versus 0.8 months (p = 0.04) and 6.4 versus 3.5 months (p = 0.02).
Discussion
Despite the fact that many studies have been published regarding the treatment of type III AC dislocations no consensus has yet been reached. A major flaw in the published studies is the lack of use of the Rockwood classification of AC joint injuries [12]. Furthermore, the majority of the studies investigating Rockwood type III include several types of Rockwood injuries or incompatible types of other classifications. This might decrease the informative value of the results in these studies considerably.
In this study we reviewed the current literature and aimed to outline the outcome of conservative versus operative treatment of solely Rockwood type III AC dislocations.
We have performed a broad search on domain and determinant in the title and abstract and have extended the search by adding the search term 'three' and its synonyms in all text fields. We are convinced that adding this search term will not compromise or narrow the search, but decrease the number of articles in any way. In contrast to previous meta-analyses and reviews [16–19, 28] we also included German articles. The management of AC injuries has been investigated thoroughly in Germany, therefore including these studies provides a more valid reflection of the current literature.
The most important outcome is the objective shoulder function. In order to evaluate the objective shoulder function multiple objective scoring tools have been developed: Constant-Murley score [22], Imatani score [23], Poigenfurst score [15], ULCA score [24], Taft score [25]. Unfortunately, none of these scoring systems are comparable for analysis because the scores of the different elements in the categories between the scoring system do not match. The majority of the studies showed no difference in the objective shoulder function between the two treatment groups, this is in line with the results of previous reviews [16, 18]. One study [12] showed a significant difference in the objective shoulder function in favour of the operative treatment group, i.e. excellent versus good. However it is unclear what the clinical relevance is in outcome between good and excellent and this is relevant in order to draw conclusions based on this result.
All studies observed a higher complication rate in the operative treatment group, which is an obvious consequence of the invasive procedure. In six surgically treated patients a surgical revision or additional treatment was indicated, and therefore clinically relevant. However, the indication for this decision is not mentioned in the studies. These reoperations might prolong the rehabilitation period and enhance the medical costs.
The radiographic assessments in the studies showed more radiographic abnormalities, e.g. osteophytes, arthrosis/arthritis and calcifications, after surgical treatment. Though Gstettner et al. [12] reported that the radiographic abnormalities were only clinically symptomatic in one out of the 41 patients. This suggests that a higher number of radiographic abnormalities in the surgical group might not be a valid argument for conservative treatment. This is in accordance with previous studies, which demonstrated that radiological abnormalities after surgery were often not clinically relevant in patients [2, 23, 28–31].
Nowadays, the cosmetic outcome is becoming more and more an important factor. As presented in the results above the cosmetic outcome, defined as a permanent prominent dislocation of the shoulder, is worse in the conservative treatment group. However, complete anatomical correction is not always achieved with surgery [1, 27]. One should consider the preference of a better cosmetic outcome against the higher complication rate in surgically treated patients.
As in previous reviews [32, 33], the studies were not consistent regarding the rehabilitation time. Cardone et al. [26] and Gstettner et al. [12] presented a better rehabilitation time in the surgically treated patients, especially in the young and physically active adults [26]. Press et al. [13] showed a significantly longer rehabilitation time for the surgical patients. This was also associated with a longer immobilisation period which is according to protocol after the surgical procedure.
There are several open surgical techniques for the treatment of AC dislocations [11, 16–18, 25, 32, 34]. The studies included in this review all used open surgical procedures [1, 9, 12–15, 26, 27]. A novel minimally-invasive technique, presented by Gille et al. [35], showed good results without any complications. Because the outcome after surgery might depend on the chosen surgical treatment, it is important to evaluate the influence of the different surgical treatment on the outcome. Therefore a study which evaluates solely the outcome after different surgical procedures in patients with AC dislocations would be justified.
Furthermore, we have to remark that the follow-up time in the included studies might be too short to evaluate the long-term outcomes of the function of the shoulder or long-term complications. Moreover, the studies do not present any data of the time between the start of physiotherapy or exercises to strengthen the shoulder and the follow-up measurement of the function of the shoulder. These activities are meant to improve the shoulder function and therefore adjustment for the period that a patient received the therapy would be appropriate.
There are a couple of limitations in our study. No randomised trials regarding the treatment of Rockwood type III have been published yet. The critical appraisal showed a poor internal validity of the studies and the results of this review are based on level three and four studies. Though we have to bear in mind that these studies are the best available evidence. We only included studies which reported the results of the Rockwood type III AC dislocation separately. Studies which included patients with Rockwood type III, but did not describe the results of type III solely, were not evaluated; this might limit the results of our study.
Furthermore, due to the different scoring systems, we were not able to compare the outcomes of the objective shoulder function in the studies, which we consider as the most important outcome of AC joint injuries.
Moreover, different surgical techniques and conservative treatments were used in the studies. These treatments might also have an influence on the outcome; this should be investigated in an evidence-based manner.
In conclusion, this review showed no conclusive evidence for the treatment of Rockwood type III AC dislocations. Physically active young adults seem to have a slight advantage in outcome when treated operatively. In order to provide evidence for the best treatment in patients with Rockwood type III AC dislocations a randomised trial should be performed with a generalised study population and a long-term follow-up.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Calvo E, Lopez-Franco M, Arribas IM. Clinical and radiological outcomes of surgical and conservative treatment of type III acromioclavicular joint injury. J Shoulder Elbow Surg. 2006;15:300–305. doi: 10.1016/j.jse.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 2.Taft TN, Wilson FC, Oglesby JW. Dislocation of the acromioclavicular joint. J Bone Joint Surg Am. 1987;15:300–305. [PubMed] [Google Scholar]
- 3.Rolf O, Hann von Weyhern A, Ewers A, Boehm TD, Gohlke F. Acromioclavicular dislocation Rockwood III-V: results of early versus delayed surgical treatment. Arch Orthop Trauma Surg. 2008;128:1153–1157. doi: 10.1007/s00402-007-0524-3. [DOI] [PubMed] [Google Scholar]
- 4.Sehmisch S, Sturmer EK, Zabka K, et al. Results of a prospective multicenter trial for treatment of acromioclavicular dislocation. Sportverletz Sportschaden. 2008;22(3):139–145. doi: 10.1055/s-2008-1027541. [DOI] [PubMed] [Google Scholar]
- 5.Allman FLJ. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg. 1967;49A:774–784. [PubMed] [Google Scholar]
- 6.Tossy JD, Mead NC, Sigmond HM. Acromio-clavicular separations: Useful and practical classification for treatment. Clin Orthop. 1963;28:111–119. [PubMed] [Google Scholar]
- 7.Rockwood C, Williams G, Young D. Acromioclavicular injuries. In: Rockwood C, Green D, Bucholz R, Heckman J, editors. Fractures in adults. 4. Philadelphia: Lippincott-Raven; 1996. pp. 1341–1413. [Google Scholar]
- 8.Hootman JM. Acromioclavicular dislocation: Conservative or surgical therapy. J Athl Train. 2004;39(1):10–11. [PMC free article] [PubMed] [Google Scholar]
- 9.Prokop A, Helling H, Andermahr J, Mönig S, Rehm K. AC-gelenksprengungen typ tossy III. Der Orthopäde. 2003;32(5):432–436. doi: 10.1007/s00132-002-0419-5. [DOI] [PubMed] [Google Scholar]
- 10.Post M. Current concepts in the diagnosis and management of acromioclavicular dislocations. Clin Orthop Relat Res. 1985;200(200):234–247. [PubMed] [Google Scholar]
- 11.Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am. 1972;54(6):1187–1194. [PubMed] [Google Scholar]
- 12.Gstettner C, Tauber M, Hitzl W, Resch H. Rockwood type III acromioclavicular dislocation: Surgical versus conservative treatment. J Shoulder Elbow Surg. 2008;17(2):220–225. doi: 10.1016/j.jse.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 13.Press J, Zuckerman JD, Gallagher M, Cuomo F. Treatment of grade III acromioclavicular separations: operative versus nonoperative management. Bull Hosp Jt Dis. 1997;56(2):77–83. [PubMed] [Google Scholar]
- 14.MacDonald PB, Alexander MJ, Frejuk J, Johnson GE. Comprehensive functional analysis of shoulders following complete acromioclavicular separation. Am J Sports Med. 1988;16(5):475–480. doi: 10.1177/036354658801600508. [DOI] [PubMed] [Google Scholar]
- 15.Esen E, Özturk A, Doğramaci Y, Kanatli U, Bölökbași S. Comparison of surgical treatment and conservative approach for type III acromioclavicular dislocations. Turkiye Klinikleri J Med Sci. 2011;31(1):109–114. [Google Scholar]
- 16.Phillips AM, Smart C, Groom AF. Acromioclavicular dislocation. conservative or surgical therapy. Clin Orthop Relat Res. 1998;353(353):10–17. [PubMed] [Google Scholar]
- 17.Smith TO, Chester R, Pearse EO, Hing CB. Operative versus non-operative management following Rockwood grade III acromioclavicular separation: A meta-analysis of the current evidence base. J Orthop Trauma. 2011;12(1):19–27. doi: 10.1007/s10195-011-0127-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spencer EE., Jr Treatment of grade III acromioclavicular joint injuries: A systematic review. Clin Orthop Relat Res. 2007;455:38–44. doi: 10.1097/BLO.0b013e318030df83. [DOI] [PubMed] [Google Scholar]
- 19.Tamaoki MJ, Belloti JC, Lenza M, Matsumoto MH, Gomes Dos Santos JB, Faloppa F. Surgical versus conservative interventions for treating acromioclavicular dislocation of the shoulder in adults. Cochrane Database Syst Rev. 2010;8:CD007429. doi: 10.1002/14651858.CD007429.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D, Alessandro L, Tetzlaff J, Altman DG, for the PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Available at: http://www.cebm.net/index.aspx?o=1157. Accessed 16 September 2013
- 22.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 23.Imatani RJ, Hanlon JJ, Cady GW. Acute, complete acromioclavicular separation. J Bone Joint Surg Am. 1975;57(3):328–332. [PubMed] [Google Scholar]
- 24.Amstutz HC, Sew Hoy AL, Clarke IC. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981;155:7–20. [PubMed] [Google Scholar]
- 25.Taft TN, Wilson FC, Oglesby JW. Dislocation of the acromioclavicular joint. An end-result study. J Bone Joint Surg Am. 1987;69(7):1045–1051. [PubMed] [Google Scholar]
- 26.Cardone D, Brown JN, Roberts SN, Saies AD, Hayes MG. Grade III acromioclavicular joint injury in Australian rules football. J Sci Med Sport. 2002;5(2):143–148. doi: 10.1016/s1440-2440(02)80035-4. [DOI] [PubMed] [Google Scholar]
- 27.Fremerey RW, Lobenhoffer P, Ramacker K, Gerich T, Skutek M, Bosch U. Acute acromioclavicular joint dislocation–operative or conservative therapy? Unfallchirurg. 2001;104(4):294–299. doi: 10.1007/s001130050730. [DOI] [PubMed] [Google Scholar]
- 28.Larsen E, Bjerg-Nielsen A, Christensen P. Conservative or surgical treatment of acromioclavicular dislocation. A prospective, controlled, randomized study. J Bone Joint Surg Am. 1986;68:552–555. [PubMed] [Google Scholar]
- 29.Thelen E, Rehn J. Acromioclavicularsprengungen – Ergebnisse nach operativer und konservativer Versorgung in 162 Fällen. Unfallheilkunde. 1976;79:417–422. [PubMed] [Google Scholar]
- 30.Reichkendler M, Rangger C, Dessl A, Ulmer H. Vergleich und Ergebnis von Schultereckgelenkverletzungen II. und III. Grades. Unfallchirurg. 1996;99:778–783. doi: 10.1007/s001130050055. [DOI] [PubMed] [Google Scholar]
- 31.Park JP, Arnold JA, Coker TP, Harris WD, Becker DA. Treatment of acromioclavicular separations. Am J of Sports Med. 1980;8(4):251–256. doi: 10.1177/036354658000800407. [DOI] [PubMed] [Google Scholar]
- 32.Bannister GC, Wallace WA, Stableforth PG, Hutson MA. The management of acute acromioclavicular dislocation. A randomized prospective controlled trial. J Bone Joint Surg Br. 1989;71:848–850. doi: 10.1302/0301-620X.71B5.2684990. [DOI] [PubMed] [Google Scholar]
- 33.Sehmisch S, Stürmer EK, Zabka K, Losch A, Brunner U, Stürmer KM, Bauer G. Ergebnisse einer prospectiven Multicenterstudie zur Behandlung der Schultereckgelenksprengung. Sportverl Sportschad. 2008;22:139–145. doi: 10.1055/s-2008-1027541. [DOI] [PubMed] [Google Scholar]
- 34.Adam FF, Farouk O. Surgical treatment of chronic complete acromioclavicular dislocation. Int Orthop. 2004;28(2):119–122. doi: 10.1007/s00264-003-0520-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gille J, Heinrichs G, Unger A, Riepenhof H, Herzog J, Kienast B, Oheim R. Arthroscopic-assisted hook plate fixation for acromioclavicular joint dislocation. Int Orthop. 2013;37(1):77–82. doi: 10.1007/s00264-012-1691-6. [DOI] [PMC free article] [PubMed] [Google Scholar]