Abstract
Purpose
Several techniques for chronic distal biceps tendon repair have been reported; however, the literature is sparse.
Methods
Seven male patients who underwent chronic distal biceps tendon reconstruction were retrospectively evaluated. All patients had significant retraction necessitating the use of an allograft for reconstruction. The procedure was done through a single incision using suture anchors and a tibialis anterior allograft. In each case, the graft was first fixed to the radial tuberosity with suture anchors, and then the allograft was sutured to the remnant of the native biceps tendon at 60° of elbow flexion. Patients were evaluated with the Mayo Elbow Performance Score (MEPS), Disabilities of Arm, Shoulder and Hand (DASH) scores and elbow range of motion (ROM).
Results
The average time from injury to surgery was 25 (12–56) weeks, and the average follow-up was 16 (minimum 12) months. Average postoperative elbow ROM was as follows: extension 4° (0–12°), flexion 134° (130–140°), pronation 82° (75–85°) and supination 80° (70–85°); average MEPS was 94 (80–100); average DASH score was 6.67 (0–19.8). One patient developed a lateral antebrachial cutaneous neuritis postoperatively that resolved by three months.
Conclusion
Though many reported techniques for chronic distal biceps tendon repair achieve satisfactory outcomes with limited complications, we present a technique with theoretical advantages of a single incision, use of suture anchors, use of a tibialis anterior allograft and tensioning after attachment of the graft to the radial tuberosity. In a series of complicated patients, early results were good to excellent.
Keywords: Single incision, Suture anchors, Chronic, Distal biceps, Repair
Introduction
Distal biceps rupture is a relatively uncommon injury, accounting for 3–10 % of all biceps tendon injuries [1, 2]. The injury typically occurs in middle-aged men engaged in activities that involve an eccentric extension load while the elbow is flexed. Rupture of the distal biceps tendon causes significant loss of supination strength and mild loss of elbow flexion strength [3–6] and is often associated with pain, ecchymosis and cosmetic deformity. However, despite the classic history and physical examination findings, diagnosis and intervention are often delayed for various reasons.
The optimal time for surgical repair following distal biceps rupture is within two weeks of injury, wherein blunt dissection and mobilisation of the biceps tendon down to the radial tuberosity can be done with relative ease [7]. After two weeks, tendon mobilisation is more difficult, and increased dissection is often necessary, potentially leading to higher complication rates. In tears older than six weeks and up to 12 weeks, tissue retraction, loss of elasticity, formation of adhesions and scar and early atrophy can preclude primary reattachment of the tendon to the radial tuberosity [7].
Because of technical difficulty and the frequent impossibility of primary re-attachment, chronic distal biceps ruptures were historically treated nonoperatively. Whereas results were deemed to be acceptable, recent studies of nonoperative treatment demonstrate significantly decreased elbow strength, with 50 % loss in supination peak torque and 30 % loss in flexion peak torque without significant loss in endurance [3, 8]. Non-anatomical surgical repair involving attachment of the ruptured tendon to the brachialis muscle may be successful in restoring elbow flexion strength but does not improve supination strength [1, 9]. Due to these shortcomings, numerous anatomical surgical techniques have been developed to repair chronic distal biceps tendon ruptures. The use of various grafts, including fascia lata [10], semitendinosus [11, 12], flexor carpi radialis (FCR) [13], hamstring [14] and Achilles tendon allograft [4, 15] have been described previously. Though surgical outcomes are reported to be superior to conservative treatment [3], reported complications with surgical intervention include radioulnar synostosis, heterotopic bone formation, neurological injury, donor-site morbidity, infection and graft failure [7, 16].
This study describes a modification of a previously published surgical technique [4] for repairing chronic distal biceps tendon rupture using a single-incision approach with two Mitek G4 suture anchors (Mitek Surgical Products, Inc., Norwood, MA, USA) and tibialis anterior allograft. We hypothesised that our initial series of seven patients would have similar outcomes to those published in the literature.
Materials and methods
Surgical technique
The operation at our institution is performed under regional anaesthesia with the patient in the supine position and the operative arm on an arm board. A nonsterile tourniquet is applied to the upper arm as far proximally as possible. An Esmarch is used to exsanguinate the limb, and the tourniquet is inflated to 250 mmHg. An S-shaped incision starting proximally and medially, crossing the antecubital fossa transversely and finishing distally and laterally in the region of the radial tuberosity is made. Blunt dissection is then used to expose the interval between the pronator (medial) and the brachioradialis (lateral). When developing the plane between the pronator teres and brachioradialis muscles, the forearm should be kept in supination at all times. The lateral antebrachial cutaneous nerve should be identified and preserved. At this time, the biceps muscle and remnant of the tendon is exposed and the surrounding scar tissue released. An Allis clamp is used to control the distal bicep tendon stump and create longitudinal traction. However, because of the chronicity, the tendon stump is often retracted, thickened and small (Fig. 1). Blunt retractors are then placed on either side of the radial tuberosity to expose the native distal biceps tendon insertion site, making sure contact with bone is maintained at all times when placing the retractors to avoid injury to the posterior interosseous nerve (PIN). Keeping the arm in full supination also decreases the likelihood of injury to the PIN. The radial recurrent vessels should also be preserved if possible; however, they can be sacrificed if necessary. At this point, the remaining soft tissue should be removed from the radial tuberosity. After drilling the medial cortex, two Mitek G4 suture anchors are impacted into the radial tuberosity (one proximal and one distal), taking care to stay as medial as possible to better recreate the normal anatomical insertion. Irrigation is used to remove any bony debris to decrease the chance of heterotopic ossification. A tibialis anterior allograft is used to reconstruct the distal biceps tendon. One strand of no. 2 Ethibond suture from each anchor is used to place a Krakow stitch up the given side of the tibialis anterior graft, and the sutures are tied together at about the four centimetre mark.
Fig. 1.
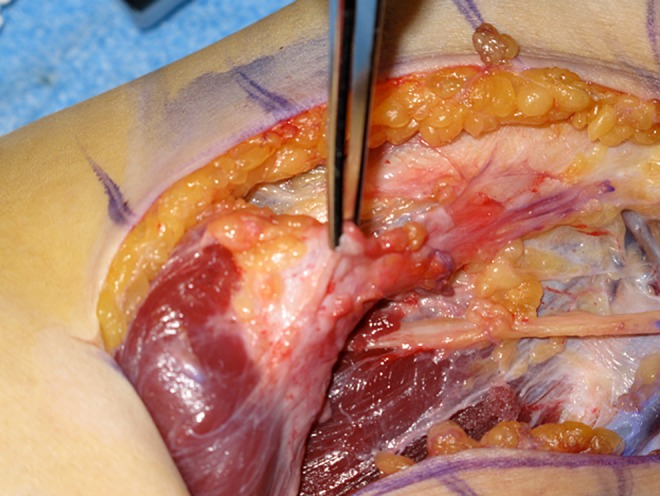
The forceps is holding the chronically torn, shortened biceps tendon that is encased in significant scarring, preventing mobilisation and primary repair to the radial tuberosity
Using the two remaining strands from the anchors, the graft is tensioned back down to the insertion on the radial tuberosity, and knots are tied to secure it (Fig. 2). At this point, we flex the elbow to approximately 60° and attach the tibialis anterior graft to the distal biceps tendon stump using interrupted, nonabsorbable no. 0 Ethibond sutures (Fig. 3). After the allograft is sutured to the distal biceps tendon stump, the graft is doubled back onto itself; figure-of-eight 0 Vicryl sutures are used to increase the strength of the repair (Fig. 4). We also incorporate the allograft into the lacertus attachment if possible. Once this is completed, we make sure we have good tension on the biceps tendon. The tourniquet is released, and haemostasis is achieved with bipolar electrocautery. After the wound is copiously irrigated and haemostasis achieved, the deep layer is closed with interrupted 2–0 Vicryl sutures, followed by a running 3–0 Prolene suture. A dry sterile dressing is applied.
Fig. 2.
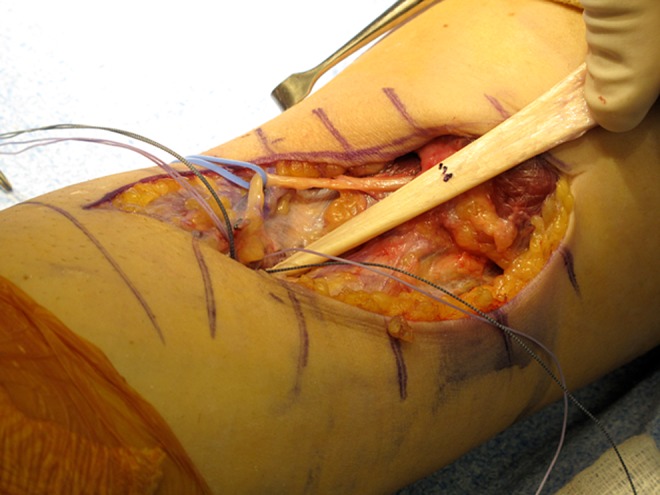
The tibialis anterior allograft is tied and fixed to the radial tuberosity with two suture anchors prior to fixing the allograft to the biceps tendon stump
Fig. 3.
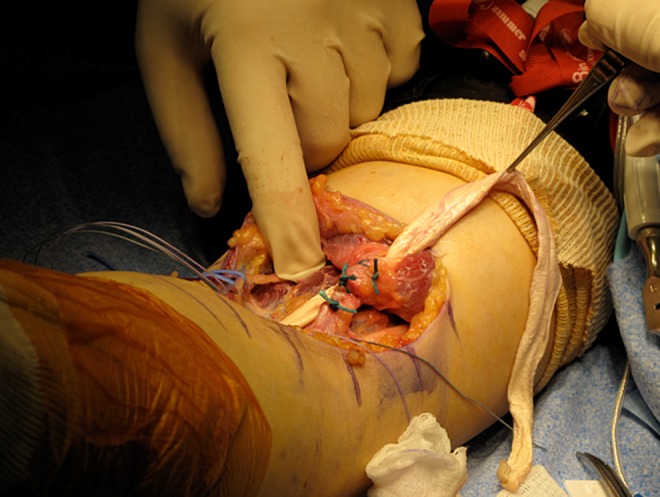
With the elbow flexed at 60°, the proximal end of the tibialis anterior allograft is sutured to the native distal biceps tendon stump using interrupted, nonabsorbable no. 0 Ethibond sutures
Fig. 4.

At the end of the procedure, the remaining tibialis anterior allograft is doubled onto itself to enhance the strength of the repair
Postoperative management
Postoperatively, the arm is placed in a posterior splint at approximately 70° of flexion for one to two weeks and transitioned to a hinged elbow brace for six weeks. Passive range of motion (ROM) from 60–100° in the hinged elbow brace is initiated after splint removal and increased by 10–15° per week, with the goal being full ROM by six to eight weeks postoperatively. Limitations during physical therapy for the first six weeks include no active elbow flexion or forearm supination. At postoperative week six, the patient can begin active and active-assisted elbow flexion without the hinged elbow brace. Progressive strengthening is performed from six to 12 weeks after surgery, with return to full sport or work at six months.
Clinical outcome measures
An institutional review board approved this retrospective case series. Seven patients who underwent the surgical procedure and postoperative rehabilitation protocol were retrospectively evaluated using prospectively collected data. The average age of the seven patients in our cohort was 44 (range 34–59) years. All patients were men, all were right-hand dominant and all were active individuals who required biceps strength. Four patients injured their right elbow and three their left. The average time from injury to surgery was 25 (12–56) weeks, and the average time of final postoperative follow-up was 16 months. Only patients who underwent distal biceps tendon repair after six weeks from original injury were included. Further, only patients who had at least one year of clinical follow-up were included. Primary outcomes were postoperative Mayo Elbow Performance Scores (MEPS), Disabilities of Arm, Shoulder and Hand (DASH) scores and ROM as determined by a hand-held goniometer. Intraoperative and postoperative complications were also evaluated.
Results
The average postoperative ROM of all seven patients was as follows: extension 4° (0–12°), flexion 134° (130–140°), pronation 82° (75–85°) and supination 80° (70–85°). The average postoperative MEPS was 94 (80–100; six excellent, one good). The average DASH score was 6.67 (range 0–19.8). One patient developed lateral antebrachial cutaneous neuritis that resolved without specialised treatment at three months postoperatively. No other intraoperative or postoperative complications occurred.
Discussion
The primary indication for repair of a distal biceps tendon rupture is to prevent and treat chronic pain and weakness. Whereas pain is less common in the chronic injury setting, weakness with elbow flexion and especially supination are common [8, 9]. Thus, repair of a distal biceps rupture is indicated in almost all patients who wish to continue an active lifestyle, especially in the young or those who require heavy use of the upper extremity. The only real contraindications to repair include patients with medical issues precluding surgical intervention and older patients with limited functional goals and no pain [17]. In the chronic setting, however, primary repair can often be difficult, and thus oftentimes an allograft may be required for reconstruction. The purpose of this paper was to describe a modified version of a chronic distal biceps reconstruction in an attempt to double the number of patients in the literature who have undergone chronic distal biceps repair using the above-described technique. Our hypothesis was that results in our initial seven patients in whom a single-incision approach using a tibialis anterior allograft and suture anchors would be similar to results published using other, similar reconstructive techniques. The technique described is a modification of a procedure described by Galatz et al. [17], which was used to treat acute distal biceps tendon ruptures, and by Darlis and Sotereanos [4], who used a similar technique to reconstruct chronic distal biceps ruptures. We varied their technique by using a tibialis anterior tendon allograft instead of an Achilles tendon allograft. Advantages of the technique include the use of suture anchors, the use of a single anterior incision, ease of properly tensioning the repair and minimal dissection required to gain adequate exposure to the radial tuberosity. Biomechanical studies performed by Lemos et al. found fixation with two suture anchors to be significantly superior in regard to peak load compared with bone-tunnel fixation for repairing distal biceps tendon ruptures [18]. Compared with an endobutton, suture anchors have less displacement at ultimate tension load and less stiffness in initial cycles but similar stiffness with repeated cycles [19]. Compared with two-incision techniques, our single-incision technique reduces risk of radioulnar synostosis and heterotopic ossification, the latter being reported in 10–15 % of cases in some series [6, 20]. Although permanent neurological injury, heterotopic ossification and radioulnar synostosis remain a possibility, they were not reported by Galatz et al. [6], Darlis and Sotereanos [4] or the authors of this study. Ultimately, because minimal dissection is required to expose the radial tuberosity, the risk of PIN and radial nerve injury is minimised compared with other single-incision techniques, which use drill holes in the radial tuberosity for reattachment with sutures from the posterior aspect of the radius. The only neurological complication in our series was a single case of lateral antebrachial cutaneous neuritis, which resolved at the three-month follow-up without requiring specialised treatment.
Although the study is limited by a small sample size, its retrospective nature and a lack of muscle-strength testing, in our cohort of seven patients, we achieved good to excellent clinical results with excellent ROM, and average MEPS of 94. In addition, to date we have not seen any rerupture at an average follow-up of 16 months. The study thus doubles the number of patients described in the literature by Darlis and Sotereanos [4], who reported an average MEPS of 97 (six excellent, one good), with no complications and using a very similar technique to treat chronic distal biceps ruptures.
Conclusion
The tibialis anterior graft allows adequate length for doubling the graft upon itself, creating increased strength of repair without risk of donor-site morbidity. The issue of tensioning is simplified via initial attachment of the graft to previously placed suture anchors and subsequent incorporation of the graft into the distal bicep tendon stump. In our experience, this allows more flexibility and precision when tensioning at an exact degree of flexion. On the basis of our experience and the theoretical advantages of the technique, reconstruction of a chronic distal biceps tendon rupture with a single incision, suture anchors and tibialis anterior allograft achieves good to excellent clinical results with minimal complications.
References
- 1.Morrey BF, Askew LJ, An KN, Dobyns JH. Rupture of the distal tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg Am. 1985;67:418–421. [PubMed] [Google Scholar]
- 2.Safran MR, Graham SM. Distal biceps tendon ruptures: incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;404:275–283. doi: 10.1097/00003086-200211000-00042. [DOI] [PubMed] [Google Scholar]
- 3.Baker BE, Bierwagen D. Rupture of the distal tendon of the biceps brachii. Operative versus non-operative treatment. J Bone Joint Surg Am. 1985;67:414–417. [PubMed] [Google Scholar]
- 4.Darlis NA, Sotereanos DG. Distal biceps tendon reconstruction in chronic ruptures. J Shoulder Elbow Surg. 2006;15:614–619. doi: 10.1016/j.jse.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Leighton MM, Bush-Joseph CA, Bach BR. Distal biceps brachii repair. Clin Orthop Relat Res. 1995;317:114–121. [PubMed] [Google Scholar]
- 6.Mariani EM, Cofield RH, Askew LJ, Li G, Chao EY. Rupture of the tendon of the long head of the biceps brachii: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 1988;228:233–239. [PubMed] [Google Scholar]
- 7.Sutton KM, Dodds SD, Ahmad CS, Sethi PM. Surgical treatment of distal biceps rupture. J Amer Acad Orthop Surg. 2010;18:139–148. doi: 10.5435/00124635-201003000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Nesterenko S, Domire ZJ, Morrey BF, Sanchez-Sotelo J. Elbow strength and endurance in patients with a ruptured distal biceps tendon. J Shoulder Elbow Surg. 2010;19:184–189. doi: 10.1016/j.jse.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 9.Freeman CR, McCormick KR, Mahoney D, Baratz M, Lubahn JD. Nonoperative treatment of distal biceps tendon ruptures compared with a historical control group. J Bone Joint Surg Am. 2009;91:2329–2334. doi: 10.2106/JBJS.H.01150. [DOI] [PubMed] [Google Scholar]
- 10.Hovelius L, Josefsson G. Rupture of the distal biceps tendon. Report of five cases. Acta Orthop Scand. 1977;48:280–282. doi: 10.3109/17453677708988769. [DOI] [PubMed] [Google Scholar]
- 11.Hang DW, Bach BR, Jr, Bojchuk J. Repair of chronic distal biceps brachii tendon rupture using free autogenous semitendinosus tendon. Clin Orthop Relat Res. 1996;323:188–191. doi: 10.1097/00003086-199602000-00025. [DOI] [PubMed] [Google Scholar]
- 12.Harryman II DT, Duckworth DG, Moskal MJ, DuMontier TA, Smith KL, Matsen III FA (1999) Chronic distal biceps tendon ruptures reconstruction with autogenous semitendinosis. University of Washington Research Report 8–12.
- 13.Levy HJ, Mashoof AA, Morgan D. Repair of chronic ruptures of the distal biceps tendon using flexor carpi radialis tendon graft. Amer J Sports Med. 2000;28:538–540. doi: 10.1177/03635465000280041501. [DOI] [PubMed] [Google Scholar]
- 14.Hallam P, Bain GI. Repair of chronic distal biceps tendon ruptures using autologous hamstring graft and the Endobutton. J Shoulder Elbow Surg. 2004;13:648–651. doi: 10.1016/j.jse.2004.01.032. [DOI] [PubMed] [Google Scholar]
- 15.Sanchez-Sotelo J, Morrey BF, Adams RA, O'Driscoll SW. Reconstruction of chronic ruptures of the distal biceps tendon with use of an achilles tendon allograft. J Bone Joint Surg Am. 2002;84:999–1005. doi: 10.1302/0301-620X.84B8.12902. [DOI] [PubMed] [Google Scholar]
- 16.Kelly EW, Morrey BF, O'Driscoll SW. Complications of repair of the distal biceps tendon with the modified two-incision technique. J Bone Joint Surg Am. 2000;82:1575–1581. doi: 10.2106/00004623-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Galatz LM, Jani MM, Yamaguchi K. Single anterior incision exposure for distal biceps tendon repair. Tech Shoulder Elbow Surg. 2002;3:63–67. doi: 10.1097/00132589-200203000-00012. [DOI] [Google Scholar]
- 18.Lemos SE, Ebramzedeh E, Kvitne RS. A new technique: in vitro suture anchor fixation has superior yield strength to bone tunnel fixation for distal biceps tendon repair. Amer J Sports Med. 2004;32:406–410. doi: 10.1177/0363546503261720. [DOI] [PubMed] [Google Scholar]
- 19.Spang JT, Weinhold PS, Karas SG. A biomechanical comparison of EndoButton versus suture anchor repair of distal biceps tendon injuries. J Shoulder Elbow Surg. 2006;15:509–514. doi: 10.1016/j.jse.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 20.Karunakar MA, Cha P, Stern PJ. Distal biceps ruptures. A followup of Boyd and Anderson repair. Clin Orthop Relat Res. 1999;363:100–107. doi: 10.1097/00003086-199906000-00013. [DOI] [PubMed] [Google Scholar]


