Abstract
Purpose:
This study aimed to clarify the existing service provision of stroke-specific vocational rehabilitation (VR) in one English county, in order to facilitate future service development.
Method:
Using soft systems methodology, services in Health, Social Care, Department of Work and Pensions, the voluntary and private sectors, which were identified as supporting return to work after stroke, were mapped using a mixed-methodology approach.
Results:
A lack of a sanctioned VR pathway meant access to support relied on brokered provision and tacit knowledge. The timing of an intervention was complex and there was a substantial degree of unmet need for mild stroke patients. VR was seen as “non-essential” due to competing commissioning priorities. Service providers from all sectors lacked training and cross-sector partnerships were tenuous and provider roles unclear.
Conclusions:
Stroke-specific VR should be delivered by an integrated, cross-sector multi-disciplinary team and integrated commissioning between health and other sectors is necessary. Although early intervention is important, support later on in the recovery process is also necessary. Service providers need adequate training to meet the needs of stroke survivors wishing to return to work and better awareness of best practice guidelines. Business cases which demonstrate the efficacy and cost-effectiveness of VR are vital.
Implications for Rehabilitation
The timeliness of a vocational rehabilitation (VR) intervention is complex; services need to be responsive to the changing needs of the stroke survivor throughout their recovery process and have better mechanisms to ensure re-entry into the stroke pathway is possible.
Return to work is a recognised health outcome; health services need to develop better mechanisms for interagency/cross sector working and liaison with employers and not assume that VR is beyond their remit. Therapists and non-health service providers should receive sufficient training to meet the needs of stroke survivors wishing to return to work. Rehabilitation teams must decide how to implement national guidance within existing resources and what training is needed to deploy SSVR.
The lack of a sanctioned pathway results in disorganised and patchy provision of VR for stroke survivors; mild stroke patients can fall through the net and receive little or no support. The journey back to work commences at the point of stroke. Mechanisms for identifying acute stroke survivors who were working at onset and for assessing the impact of the stroke on their work need to be put in place. The entire MDT has a role to play. In the absence of a VR specialist, even patients without obvious disability should be referred for ongoing rehabilitation with detailed work assessment and signposted to employment specialists e.g. disability employment advisors EARLY after stroke.
Health-based VR interventions can influence work return and job retention. However, therapists must routinely measure work outcomes to inform their business case and be encouraged to demonstrate these outcomes to local commissioners. Commissioners should consider emerging evidence of early VR interventions on reduced length of stay, health and social care resource use and the wider health benefits of maintaining employment.
Keywords: Mapping, soft systems analysis, stroke, vocational rehabilitation
Background
Every year 110,000 people in England suffer a stroke, a quarter of whom are of working age [1,2]. Keeping people with long term conditions in work is now a recognised health outcome [2,3] as there is a strong association between worklessness and both physical and mental health issues [4]. In addition, the economic impact in terms of lost income and productivity for stroke survivors and their families is immense. Societal costs, including health and social care and informal care-giving are estimated at £9 billion a year [5]. For many stroke survivors, the primary goal is to return to work (RTW) and regain financial independence [5] yet there has been little research into aspects of life after stroke, such as returning to work [2].
Both policy [6] and clinical guidelines [7] state that stroke survivors should have access to vocational rehabilitation (VR) services, enabling them to participate in paid, supported or voluntary employment. VR is defined as a process ‘whereby those disadvantaged by illness or disability can be enabled to access, maintain, or return to employment, or other useful occupation’ [8]. It is concerned with finding ways to ‘match’ the stroke survivor’s abilities and their limitations to the demands of the job and the work environment. It also involves working with the stroke survivor and their family to manage the physical, cognitive and emotional consequences of stroke as well as liaising with employers to facilitate RTW.
However, not everybody has access to this type of support and only 37% of primary care trusts provide rehabilitation that addresses stroke survivors’ work needs [8]. Where it is provided, it is rarely organised in a way that helps prevent job loss by ensuring the stroke survivor's opportunities to retain work with an existing employer are maximised [9]. Stroke survivors are frequently discharged from hospital without any support or advice about returning to work and can be prematurely ‘written off’ by health care professionals who make assumptions about the individual’s work capability based on the nature of stroke deficits and the job they were doing before their stroke [10,11].
Evidence in the form of national policy [12,13] and clinical guidelines [14] recommend VR services for individuals with neurological conditions should provide early intervention with information and support to prevent breakdown of relations with existing employers, flexibility to allow people to re-access services when required and services that are sufficiently individualised to meet people’s differing and changing needs. They also call for partnerships between health and social services, statutory and voluntary services to identify gaps in local provision, and to develop ‘specialist skills training’ for all those providing VR [15].
There are many factors which affect a person’s ability to RTW following stroke, including mobility, cognitive impairment and hand function [2,16,17]. However, there has been little attention paid to the organisational factors within the stroke rehabilitation pathway which influence the degree to which a stroke survivor is supported in their RTW. Factors such as staffing and skill mix, competing priorities for health resources, the structure of an organisation and the delivery of services, access to these services and the beliefs and attitudes of service providers and commissioners are key to achieving the required health outcomes [9].
It is important that stroke-specific vocational rehabilitation (SSVR) services are developed in line with national policy and clinical guidelines. To achieve this, it is necessary to identify current service provision, how the needs of stroke survivors wishing to RTW are met and where service gaps exist.
The aims of this study were to
Clarify existing service provision by identifying facilitators to RTW after stroke and exploring local contextual factors which limit service success.
Identify where service gaps exist and explore stakeholder perceptions of how these could be addressed.
Explore issues relating to the uptake of new approaches to care and to clarify the relevant policy, organizational and professional factors likely to affect the way SSVR can be delivered.
Methods
We sought to identify service gaps and barriers to work return, so that a SSVR intervention could be developed and the feasibility of delivering and measuring its effects tested in a separate feasibility trial.
This study involved the identification of key stakeholders for interview and observation and mapping services which purported to advise or support stroke survivors in RTW. We also gathered service data and public facing information, which described or defined the services.
Ethical clearance was granted in April 2010 by the Leicestershire, Northamptonshire and Rutland Research Ethics Committee (reference number: 10/H0406/21) and mapping took place between April 2010 and April 2011.
Systems methodology
To determine what happens to stroke survivors in one English county, we used soft systems methodology (SSM) [18]. In SSM, services are seen as complex human activity systems which can be understood in terms of the relationships between their structure, process and outcomes. The aim of SSM is to describe these relationships and use them to generate an operational definition of how the service operates. This is known as its “root definition” [18].
The seven stages of the SSM model [18] were followed; these are listed in Table 1.
Table 1.
The seven stages of SSM [17]: Identifying the problematic situation.
| 1. Identifying the problematic situation |
| 2. Researching the situation and building a “rich picture” |
| 3. Building “root definitions” using CATWOE |
| 4. Developing a conceptual model of the change system |
| 5. Comparing the model with the real-world situation |
| 6. Defining the changes to be implemented |
| 7. Taking action* |
*The last phase is beyond the scope of this current investigation.
Sampling
In order to identify those suitable for interview or observation, a database was developed of experts in the field of stroke or VR. These “key” stakeholders were initially identified by the diffusion fellow (a clinician and part of the research team responsible for bridging the gap between the project and clinical practice), and then further identified through snowball sampling.
In order to understand the “worldview” of stakeholders with an interest in returning stroke survivors to work, we sought to represent views from different perspectives including those from stroke survivors, service providers and commissioners and attempted to obtain these from different provider sectors including acute and community NHS services, social services, the Department for Work and Pensions (DWP) as well as voluntary and independent services.
Procedure
Phase 1: Identifying the problematic situation (mapping current service provision)
Mapping commenced by holding a focus group with six service providers from secondary health care, social care and community services who had been identified through the clinical knowledge of the diffusion fellow and networks developed by the research team. The aim was to build on a rudimentary map of VR provision generated by the clinical therapist and to identify key stakeholders for interview. Formal data concerning the number of stroke survivors seen per annum, who were working at the time of stroke, and who were offered support with RTW issues, were requested by email.
Phase 2: Researching the situation and building a rich picture (qualitative investigation into gaps in service provision)
A mixed-methodology approach was adopted whereby observation and documentary analysis were utilised alongside stakeholder interviews, focus groups and an “engagement event”. This triangulation served to deepen understanding of service provision and enabled validation of data.
Formal interviews conducted by three researchers (M.G., J.T. and K.S.) were recorded and transcribed verbatim; written informed consent was obtained from all participants. Interviews were semi-structured and open-ended questions were developed using the “CATWOE” mnemonic (see Table 2 for example questions), a structured framework used in SSM to explore the perspectives or “worldview” of interviewees. Themes evolving from the interviews were explored throughout the data collection process and informed future questions iteratively.
Table 2.
SSM CATWOE mnemonic with example questions; adapted from Checkland and Scholes [18].
| Label | Descriptor | Example question |
|---|---|---|
| Customers | Who are the beneficiaries of this system? | Where and how do stroke survivors enter the pathway? |
| Actors | Who facilitates the transformation? | Which people deliver VR? Who else within the service is involved in return to work issues? |
| Transformation | Changes occurring because of this service | What methods of communication exist within this service or between these related services? |
| Worldview | The context in which such transformations are deemed to be desirable | How are the services you provide marketed, researched and evaluated? |
| Ownership | To whom the service is answerable | Who commissions the service? |
| Environmental | Contextual factors relating to the service | Does/do the environment(s) present any problem/barrier to the organisation and delivery of the service or services which form part of this VR pathway? |
Informal interviews and observations of relevant services were also conducted by one researcher (M.G.), often simultaneously. Verbal informed consent was obtained. Detailed notes were taken and analysed retrospectively. Documentary analysis was conducted on all relevant public facing information such as patient information leaflets, online service descriptions and published material.
Finally, an “engagement event” was held in order to validate our findings; delegates were presented with initial findings and were asked to ratify these, to correct misinterpretations and to clarify our understanding. Invitations were sent to 60 key stakeholders identified throughout the course of the project. A total of 49 stakeholders attended the event including service providers, service users, researchers and commissioners, representing organisations such as the NHS, Social Care, the DWP, voluntary and independent sectors.
Figure 1 summarises the stages of the procedure.
Figure 1.
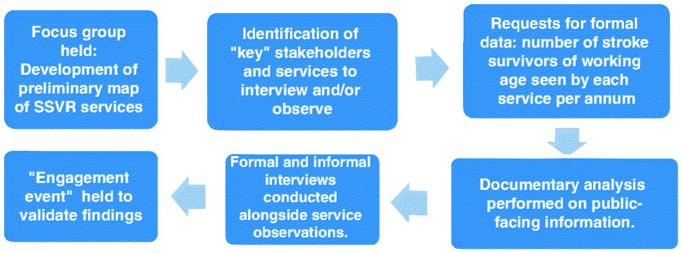
Flow chart of mapping and qualitative procedure.
Analysis
The data were analysed in line with the SSM CATWOE mnemonic, which is described in Table 2. Themes were defined and modified in light of the incoming data and were organised using a software package (NVivo; QSR International Pty Ltd, Cheshire, UK).
All interview transcripts were coded by one researcher (E.S.) and read separately by members of the team to ensure impartiality (K.R., M.G. and J.T.). The developing themes were validated by other members of the team and independently verified.
Results
Phase 1: Identifying the problem situation (mapping current service provision)
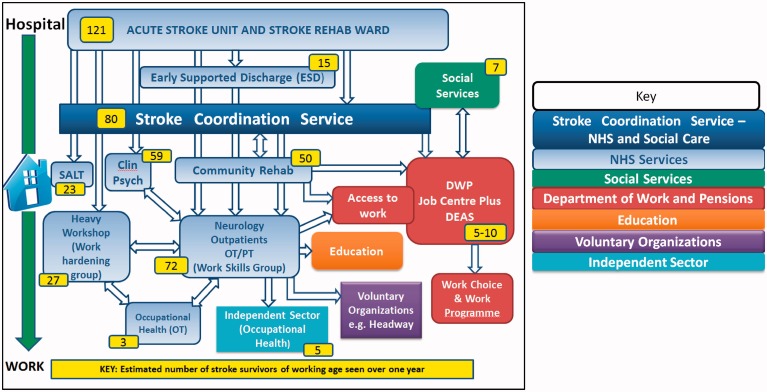
A “rich picture” [18] was developed which reflected the myriad of services which stroke survivors may encounter on the journey between hospital and work (see Figure 2).
Figure 2.
Map of services offering vocational advice or support to stroke survivors showing numbers of stroke survivors seen each year in one English county.
Multiple service providers in health, the DWP, social care, education, the independent and voluntary sectors purported to offer support to stroke survivors in returning to work. However, this was often limited to advice and few actually delivered vocational interventions.
Most VR was delivered by outpatient services in the acute trust including neurological services, occupational therapy and physiotherapy, speech and language therapy and clinical psychology.
Except for within the health sector, most referrals made (represented by the white arrows in Figure 2) were unidirectional which suggests tenuous cross-sector working as well as little opportunity to re-engage health services if stroke survivors encountered problems in the workplace. Service gaps included provision for individuals who were out of work and unable to return to existing jobs as well as support to broker work placements.
Phase 2: Researching the situation and building a rich picture (qualitative study)
The qualitative findings are organised under three themes. The first is the “lack of a sanctioned stroke VR pathway” which addresses the absence of a coherent RTW pathway for stroke survivors. The second, entitled “timeliness” refers to the complexities of getting the timing of VR right for stroke survivors. Finally “barriers to service development” explores the gaps identified in the available service provision. These themes and their sub-themes are presented in Table 3.
Table 3.
Themes.
| Lack of sanctioned VR pathway | Informal mechanisms of communication |
| Unmet need for young and/or mild stroke survivors | |
| Timeliness | Early, late and responsive care |
| Length of intervention | |
| Barriers to service development | Insufficient evidence |
| Knowledge gaps | |
| VR is not the core business of health |
Lack of sanctioned VR pathway
Informal mechanisms of communication
The lack of a dedicated VR pathway for stroke was identified by interviewees, irrespective of their position or background. It was also suggested this caused piecemeal provision of VR as many different services only offered individual VR components. The resulting service provision was described by commissioners and service providers as, “patchy”, “disjointed”, “inequitable”, “fragmented”, “ad-hoc” and “disorganised”.
Without formal collaboration, service providers relied on informal mechanisms of communication to navigate the pathway. The extent to which stroke survivors received co-ordinated VR depended on brokered provision and the individual service providers’ knowledge of the system and available services, including VR. As a consequence, referrals to other VR services were frequently low:
“Well I suppose [an outpatient OT] has been referring me the odd one or two … Because she’s on my corridor and I think that’s how she knows about me … We’ve done some informal … you know you bump into people at lunchtime, which is quite useful”. [Neuropsychologist: SI-D-101].
Dependence on informal mechanisms of communication was further compounded in health services by the absence of clear service level agreements to delineate where responsibility for SSVR delivery lies. Consequently, services did not perceive VR to be within their remit, resulting in ad-hoc and non-formalised provision, where clinicians relied upon their clinical judgement in order to respond to stroke survivors’ unmet needs:
“So I’ve actually said to [stroke co-ordinators] and [a voluntary organisation], can you meet and can you get written criteria and what each other’s roles are … it’s hard to partnership if we’re not completely clear on what on their role is.” [Community OT: SI-D-104].
“Interviewer: Do you link with the NHS?
Respondent: Not if I can help it! … I'd leave it to them to deal with their therapy … it would be really, really difficult for [the patient’s therapists] to get hold of us” [Occupational Health Advisor: SI-D-115]
Another area of concern was communication between service providers from all sectors (particularly non-health services) and the stroke survivors’ GP. Despite service providers’ promotional activities, GP’s lacked awareness that support existed:
“I don’t think GPs understand the role of occupational health I don’t. I mean there’s always been this sort of barrier and it could be utilized better, you know, we’ve tried in the past to get involved or introduce ourselves to the GPs … they never refer to occupational health. Irrespective” [Occupational Health Advisor: SI-D-115].
“GPs? No, never. And we have leaflets and GP because I saw a leaflet at my GP surgery, but never had a referral from a GP.” [Life Skills Advisor, Social Services: SI-D-105].
Conversely, all four service providers interviewed who provided outpatient and community rehabilitation; (two OTs, one speech and language therapist, and one neuropsychologist) stressed that they were hesitant to advertise their services to GPs due to over-saturation, which exacerbated the poor awareness of available services on the part of GPs. The resultant infrequent referrals from GPs to VR services aggravated the problem of re-accessing the stroke pathway, particularly as GPs were the primary gatekeeper of referrals for late rehabilitation:
“We don’t need to market ourselves any more at the minute, because we wouldn’t have the capacity” [Community OT: SI-D-104].
Falling through the net
The unmet need of mild stroke patients was acknowledged amongst interviewees. They were frequently identified as people who “fell through the gap” [stroke coordinator: SI-D-108] and received little or no support post-discharge. Acute NHS service providers described pressure to discharge patients as soon as they were functionally able. Milder stroke survivors might spend as little as a day on the stroke unit. Consequently, acute staff routinely relied on community and out-patient support to meet rehabilitation needs:
“I think what we can do is refer on but we can't really delve … I'd say for home, just the nature of this ward is that you know, you've got to get them … out really and referred on.” [Acute Stroke OT: SI-D-109].
However, mild stroke survivors often failed to meet inclusion criteria for over-saturated community and out-patient rehabilitation services which prioritised people with more severe and often visible (physical) difficulties. One community OT stated that the inclusion criterion for their service was two or more rehabilitation needs. This system resulted in those with mild, invisible difficulties receiving little, if any, support after discharge from acute services:
“One of the things we identified for example was that to a certain extent if people had a severe stroke they had reasonable services to be fair, we all rose to the occasion as it were. The areas that were less good were those people, well we begin to call them the walking wounded as a cohort, people who on the face of it could be discharged from hospital quite quickly and probably little or no obvious support” [Commissioner: SI-D-123].
“They’re sent home because they're, you know, walking about and they can feed and they can dress themselves. They are independent from that point of view but actually they've got a lot of high cognitive deficits so when they try and go back to work you know they haven't got the concentration, their memory is not so good … ” [Stroke Consultant: SI-D-116].
There was a sense of abandonment from stroke survivors who felt that rehabilitation had not met their needs; many said they were simply “left to get on with it” [stroke survivor: SI-D-111]. The following quotations highlight their frustration:
“Well about six or seven weeks ago I tried to hang myself … because I was depressed with the stroke … I tried to get a job and no one wanted to know” [SI-D-127].
“I think I felt abandoned when I came out of hospital and it would have been nice to have had some follow up, really. There was nothing” [SI-D-103].
Timeliness
“Early”
A common consensus amongst service providers and commissioners was that early VR intervention is critical; partly because it reduces the risk of stroke survivors falling through the net:
“I've seen it time and time again that they, you know, they've, they fall between the cracks and they don't get the support they should do” [Occupational Health OT: SI-D-115].
Furthermore, service providers indicated that if intervention was delayed, stroke survivors risk losing their job. Returning someone to work (in an existing role) with a former employer was believed to be more successful than re-training the stroke survivor for a new role; capitalising on well-established relationships and employers who are willing to make allowances:
“In a way it’s a bit too late, and if you can catch people before they get to that process, it’s easier to keep your job than to find a new job sometimes I think” [Life skills advisor: S-D-105].
“I think you know it’s always easier if you’ve a) got somebody who’s already got a job and the employer is supportive, they’re well-liked by the firm or by the company and you know if the employer is oh yeah, we really need so and so back at work, they’re usually very, very good. It’s a bit more challenging when you’ve got somebody who needs to completely retrain” [Community OT: SI-D-107].
“Late”
Even though early input was considered crucial by health service providers, it was not always desired by the stroke survivor or considered appropriate by providers in other sectors:
“But [the stroke co-coordinator] doesn’t want them to fall through the net, so that’s why she refers early. [Her] referrals tend to be very soon after discharge, which sometimes is not the right time” [Life skills advisor: SI-D-105].
“I also think as well that perhaps, I mean people who are coming out of hospital maybe on the whole aren’t quite ready for a return to work service … That’s another thing is about getting information and intervention to people at the right time, it’s not always appropriate to do that two weeks post-stroke, it might be appropriate to do it five months after when it really is having an impact when someone’s made adjustments. And again that doesn’t reflect well on the fact that maybe five months down the line there’s nobody there to ask” [Third Sector Commissioner: SI-EM-02].
Both service providers and users suggested being able to access support later in recovery may be beneficial and described the consequences a RTW may have on the stroke survivors’ self-esteem and confidence if it is too early:
“I felt really guilty being off … I went back far too soon … I went back after five months … I wasn’t, like, emotionally, psychologically ready, no … I got no confidence at all, totally stripped, and just struggled with everything really. And also [stroke survivor’s manager] was asking me to do things that I wasn’t really able to do, but I didn’t like to say I couldn’t” [Stroke survivor: SI-D-103].
Another issue affecting the timing of support was that some stroke survivors were unable to contemplate work in the immediate aftermath of stroke and refused support. Others with severe stroke are overwhelmed with their medical issues and general rehabilitation:
“Because the first two years were just very … she was just in a crisis situation, she wasn’t able to think about [returning to work]” [Life Skills Advisor SI-D-105].
“People don’t want to talk about work when they’ve just had a stroke. They want to talk about recovery and then suddenly they get home and I think it’s at that it hits … but then they feel an obligation to get back to work because of money” [Stroke co-ordinator: SI-D-108].
“Responsive”
Stakeholders emphasised the need for a more flexible rehabilitation pathway where patients can “dip in and dip out” [DEA: SI-D-131]. At present, successful entry or re-entry into the rehabilitation pathway relies upon persistence and resourcefulness on the part of the patient with little or no support from rehabilitation services:
“You don’t know what you can have if you get back into the system. You know if you barge your way, sharpen your elbows up” [Stroke survivor: SI-D-111]
Barriers to service development
Insufficient evidence
There was a dearth of evidence to support the efficacy and cost effectiveness of VR interventions following stroke and a lack of local audit data to demonstrate benefits to patient outcomes. Available evidence was often not in a format that was easily accessible to commissioners who stressed the need for clear-cut business cases which demonstrate the economic benefits before commissioning could be considered:
“I mean we’ve put outcomes in, we ask for feedback … and to be fair it is very hard to get realistic info fed back to us. And I don’t quite understand why really” [Commissioner: SI-D-123].
“I would really like to see some financial case study about okay so someone did return to work, so what has that meant? So they’ve claimed x less in benefit, they’ve paid x in tax and then you can really see” [Third Sector Commissioner: SI-EM-02].
This problem was exacerbated by poor data and a distinct lack of information relating to vocational activities, which meant it was almost impossible to determine how many working age stroke survivors a service had seen or whether their work needs were addressed. This problem was greater in non-health services, where ‘stroke’ was rarely identified as a separate condition and therefore service providers could only speculate about numbers of stroke survivors treated annually:
“It is not something we have been recording really about how many people wish to return to work. I can’t imagine where, from my perspective you would get these statistics from.” [Commissioner: SI-EM-01]
“Knowledge gaps”
A lack of stroke-specific knowledge was apparent in non-health service providers who felt overwhelmed or poorly equipped dealing with a condition for which they lacked sufficient knowledge:
“To be honest if we get a referral and it says somebody’s had a stroke and they want them to return back to work our hearts sink … Yeah. It’s quite a tough call really; we find it quite difficult really being honest” [Life skills advisor: SI-D-105]
The lack of stroke-specific knowledge amongst (non-NHS) service providers and commissioners was accompanied by perceptions that stroke was a condition of the elderly and therefore work was irrelevant, or that stroke is an acute episode rather than a long-term condition. Interviewees failed to fully appreciate the debilitating, and often “invisible” effects of stroke. There was a distinct lack of clinical training or stroke-specific knowledge amongst these service providers, despite their role in supporting work return in people with specific health needs:
“We’ve had a few dealings with [an independent occupational health service] with a few patients and their knowledge base isn’t good on neuro, I don’t think” [Neuropsychologist: SI-D-101].
“People don’t understand the underlying difficulties, people at the job centre may see a patient walk in and appear perfectly healthy, but they don’t find out if they have any underlying difficulties which aren’t obvious” [Stroke support worker at a voluntary organisation: SI-D-133]
Conversely, formal VR training amongst NHS service providers was almost non-existent and many were required to devise their own “common sense” approach to addressing RTW issues. For example, one commissioner said service providers were required to draw upon “ancient knowledge” in order to address vocational needs of patients as she didn’t think “there’s much in the way of training around vocational rehab” [Commissioner: SI-D-123].
Service providers were frustrated as they wanted to address work issues but felt they lacked the necessary knowledge and skills. The lack of VR training amongst NHS services meant service providers were reluctant to contact stroke survivors’ employers because they lacked confidence or did not see employer liaison as part of their remit:
“Some staff are unsure as to whether they have permission to visit other places with patients including work places. These visits are time costly and carry risks including legal risks about identifying disabilities to employers that may result in the loss of someone’s job” [Senior Community Speech and Language Therapist: SI-D-134]
The indispensable role of highly skilled and knowledgeable “champions” within the stroke pathway was frequently highlighted. However, this created an inherent vulnerability in the system as specialist roles were under constant threat of not having contracts renewed. Thus VR expertise, tacit knowledge of the system and well-established inter-service communication could be lost:
“Well I term [VR service provision] as a patchwork, because historically services have been developed in localities where people have had a good idea or a champion” [Commissioner: SI-D-125]
“We’ve lost over a hundred staff in commissioning … we’ve lost an awful lot of knowledge, skills and experience, because a lot of the staff that have gone have been the longer serving staff, and then things are being re-shuffled if you like. So I do think it’s quite a risk” [Commissioner: SI-D-123]
“VR is not the core business of health”
Here we highlight the opinion that VR is not a “core business of health”, frequently expressed by those responsible for commissioning VR services. Often it was the case that “big burning projects that impact upon the majority of our patients” which had a “clear national evidence base” [Commissioner: SI-EM-01] were cited as commissioning priorities, over and above less crucial rehabilitative services. This was exacerbated by the austere economic climate for health service funding, which means that only “essential” care (such as thrombolysis) are funded, resulting in rehabilitation falling behind acute care. Many acknowledged that provision for existing stroke rehabilitation was insufficient and VR even less so:
“What I know is there’s not much really in terms of stroke rehab, or not as much as there should be, what there is, is essentially the bare minimum that we can get away with to be frank… I don’t think I could say hand on heart that we have a very comprehensive service for rehab, stroke rehab.”[Commissioner: SI-D-124]
“At the moment we have been working very much, as people have nationally, on hyper acute stroke care … [Longer term rehab goals] aren’t the immediate priorities” [Commissioner: SI-EM-01].
“Because we’re not seen as an essential service in some ways … So I’m seen as a bit of a luxury.” [Life skills advisor: SI-D-105].
The majority of commissioners failed to see VR within the remit of health and felt other sectors such as DWP should be the main provider because “investment in the rehab would make savings somewhere else, not in the health service so it’s not prioritised” [Commissioner: SI-D-124]. Consequently, government emphasis on the need for health interventions to reduce health risks and state dependency were not replicated in commissioning priorities:
“I haven’t had an engagement with that sort of complexity of funding before … I think that is some of the issue with people fast stream down a health condition and some of the other health conditions; it is like whose responsibility? Where does the funding priority sit?” [Commissioner: SI-EM-01].
“I think [VR] is a harder one to sell, to build a business case on … because (a) you can’t, it’s quite hard to pin down okay (a) the size of the service you’d want, and (b) the kind of realistic model”. [Commissioner: SI-D-123].
Nevertheless, shifting the responsibility away from health was not a universal opinion. One commissioner with a background in social work and health care rehabilitation argued:
“Poor employment outcomes lead to poor health outcomes … The NHS has to quantify the risks of not supporting people into work. If there is an evidence base that not doing this will lead to more NHS presentations, whether in primary or secondary care, which will cost the NHS more money, then NHS investment in return to work may well be worthwhile” [SI-D-132].
Those from voluntary organisations also viewed VR from a broader health and social care perspective:
“The knock on effects that [stroke] has for health and social care are incredible financially, if people are going to deteriorate in the community, physically and mentally, as a result of isolation and no intervention and so forth is only going to build a greater burden of need. And going back to work is good for your mental health, so much to be done I think, I just find it staggering really that people are left after a couple of months and that’s you, you’ve had everything that’s available to you.” [Third Sector Commissioner: SI-EM-02].
However, there was very little support for a stroke-specific VR programme amongst commissioners. Saturated services and limited resources were cited as reasons for not commissioning new condition-specific services. A generic RTW service for all individuals with disabilities was considered a more viable option. However, some commissioners believed this should be the responsibility of commissioning strands that were not specific to stroke, such as physical disability or generic vocational services without a health or disability focus:
“Because [returning stroke survivors to work] is no different to some of the services that are looking for young people, to get young people into work” [Commissioner: SI-EM-01].
“Vocational rehab to me could have other client groups, a more cost effective way might be to diversify and say and say well we would offer it to other client groups as well” [Commissioner: SI-D-123].
Discussion
We aimed to investigate VR service provision for stroke survivors and identify barriers and enablers to its delivery from a wide range of perspectives. Best practice guidelines and recommendations state that stroke survivors should routinely receive VR, however to date, there has been no comprehensive appraisal of the barriers inherent in stroke rehabilitation services which prevent the implementation of these recommendations. Therefore, this study is an important step towards understanding the service gaps in supporting stroke survivors back to work.
The lack of a sanctioned VR pathway resulted in miscommunication and poor cross-service collaboration. The NSF for long term neurological conditions [6] stresses the need for specialist services for individuals with complex needs and recommends that “rehabilitation services are planned and delivered through co-ordinated networks, wherein specialist neuro-rehabilitation services work both in hospital and the community to support local rehabilitation and care support teams” [15]. Our findings suggest close collaboration between acute and community services is crucial to prevent stroke survivors ‘falling through the net’ in the transition from acute to community care. Similarly, a multi-disciplinary approach is vital as supporting stroke survivors back to work is a complex rehabilitation intervention, and often requires input from less traditional sources. For example Playford et al. [9] argue a core VR team should consist of occupational therapy and psychology with access to JobCentrePlus, others studies have stressed the need for input from Disability Employment Advisers, social services [19] occupational health and GPs [20].
The stilted nature of the VR pathway had implications for the timing of SSVR. Previous literature stressed the need for early intervention [20,21] to prevent job loss. However, not all stroke survivors are willing, or able, to consider a RTW early in their recovery. Consequently, a more flexible and responsive pathway is needed, where patients can “dip-in-and-out” and receive support later in their recovery.
This view is supported by findings from a prospective study by Saeki et al. [22] identifying two time clusters in which stroke survivors returned to work: early (0–180 days post stroke) and late (12–18 months post stroke). Although the authors did not investigate the causes of “early” or “late” return, they suggested that late return coincides with the withdrawal of sickness benefits and argued “unless stroke patients returned to work during the earlier period, they preferred to receive longer sickness benefits, and such benefits may delay them from returning to work”. Further investigation into factors influencing the timing of a RTW is warranted to ensure that rehabilitation services can meet the needs of stroke survivors at a time when they are ready for support.
One key finding was the inadequacy of training and VR knowledge in most sectors. Health staff lacked VR training and most non-health staff had limited understanding of stroke. The necessity for specialist and well-trained staff has been identified [23] yet we found service providers lacking in skills necessary to support a stroke survivor back to work. There was a general lack of awareness of policy [3,12,13,20] or guidelines [7,14,24] necessary to support VR delivery. Furthermore, staff from generic services were overwhelmed with clinical guidance and found it difficult to implement recommendations for the varied conditions they dealt with. Efforts are needed to ensure the gaps between knowledge and practice are closed, and guidance for condition-specific care is in a format easily accessible to service providers.
Our findings have implications for health service commissioning. A shift towards targeted service provision and the introduction of Commissioning for Quality and Innovation (CQUIN) targets means portions of services’ budgets are now dependent on meeting quality goals. However, the failure on the part of commissioners to set CQUIN targets around work return, and on the part of service providers to measure work outcomes, threatens the likelihood SSVR will be commissioned in future [25]. Moreover, the move towards community based GP-led clinical commissioning groups raises concern; in this study, GPs were identified as lacking knowledge and awareness of VR services and were rarely identified as having a role in supporting stroke survivors in RTW. Services must routinely collect work-based outcomes and raise awareness of VR amongst commissioners, particularly those new in post.
We found commissioners reluctant to discuss the commissioning of SSVR. Many did not see ‘work’ as a health problem, and believed the financial benefits of a VR service would be felt elsewhere, despite evidence to the contrary [2,3]. The lack of clear funding priorities and limited evidence meant commissioners were hesitant to agree its value. The prospect of commissioning a service involving complex cross-sector collaboration (e.g. social services, DWP, healthcare, etc.) was a deterrent. Similar obstacles to commissioning VR are highlighted by the BSRM [19] including the highly specialist, complex nature of a service perceived as “low volume, high-cost”. However, this concern is disputed by findings from a pilot study comparing the work outcomes of people with traumatic brain injury, who received a specialist VR intervention to those who received routine care in Nottinghamshire. At one year post injury, 27% more people who received VR were in work and the mean cost difference from a health and social care perspective was only £75 (95% CI -£1200.00, £1350.00) per person – about the cost of one therapy session [26]. Further work is necessary to provide rigorous evidence to commissioners which supports the need for SSVR and demonstrates its cost-effectiveness.
These findings should be interpreted in light of the strengths and limitations of the study. The services mapped were specific to one English county. Geographical variations in service provision mean the results may not generalise. However, our findings resonate with literature investigating barriers and enablers of SSVR elsewhere [9,10,17,27].
Another limitation is the potential for interviewing bias as the interviewees mostly had health backgrounds and most were OTs. Whilst efforts were made to represent the views of different stakeholders, stroke survivors and non-health service providers were under-represented.
Nevertheless, the methods employed in this study ensured findings were embedded in the context of the service and ratified by service providers. SSM provided the opportunity to gather data from a number of different sources enabling cross-verification. Validation was also facilitated iteratively during the engagement event and frequent contact with stakeholders, allowed us to check our interpretations were accurate.
Future research should build upon the findings of this project and address the implementation of policy guidelines and recommendations which acknowledge the importance of SSVR. Whilst little is known about the true economic impact of stroke resulting directly from loss of work or reduced productivity at a societal and personal level [28], if patterns similar to those witnessed in people with TBI are followed, the impact, resulting from spiralling unemployment, a decline in monthly earnings, (resulting from a shift to lower paid work) and an increase in public assistance is likely to be substantial and on-going [29]. Consequently, SSVR could potentially mediate the escalation of health and social costs resulting from reduced or lost vocational status following stroke.
Conclusion
Our study supports the findings and recommendations from previous work and best practice guidelines for VR, a summary of recommendations from this study can be found in Table 4. Successful RTW after stroke requires the right support at the right time, however, not all stroke survivors benefit from timely support and many are missed. Despite pockets of excellent stroke-specific expertise and VR knowledge, these skills are rarely combined. A flexible, integrated approach, rigorous data collection, work-related outcome measurement and better training of service providers is required to meet the complex needs of working age stroke survivors.
Table 4.
Recommendations.
| 1. SSVR should be delivered by an integrated cross-sector multi-disciplinary team with significantly improved cross-service collaboration. The introduction of a SSVR case manager who can to bridge gaps between different services and sectors would ensure delivery. |
| 2. Routine collection of work-related outcomes from stroke survivors is needed to inform business case development and local commissioning. |
| 3. Joint or integrated commissioning between health and other sectors, e.g. DWP with CQUIN targets set to ensure work outcomes are recognised locally by health services. |
| 4. Service providers should receive adequate VR and/or stroke specific training and guidance to meet the work needs of stroke survivors. Awareness of policy and best practice guidelines needs to be raised in all sectors. |
Acknowledgements
This paper was written by the authors on behalf of the “Return to Work after Stroke” team which consists of Kate Radford, Mary Grant, Jane Terry, Karen Stainer, Carol Coole and Emma Sinclair. We would like to thank all participants who have contributed to the study. We would also like to acknowledge the contributions of Lou Watkins, who provided service data, Simon Bailey and Karen Stainer who completed a number of interviews on behalf of the team and Niki Chouliara who assisted with the development of the final manuscript.
Declaration of interest
This research was funded by the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care for Nottinghamshire, Derbyshire and Lincolnshire (NIHR CLAHRC NDL). The views expressed in this article are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
References
- 1.National Audit Office London: The Stationary Office; 2005. Reducing brain damage: faster access to better stroke care. [Google Scholar]
- 2.Daniel K, Wolfe CDA, Busch MA, McKevitt C. What are the social consequences of stroke for working-aged adults? a systematic review. Stroke. 2009;40:e431–40. doi: 10.1161/STROKEAHA.108.534487. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health. The NHS outcomes framework 2011/12. London: DH; 2010. [Google Scholar]
- 4.Waddell G, Burton A. Is work good for your health and well-being. Department of Work and Pensions. London: The Stationary Office; 2006. [Google Scholar]
- 5.Saka O, McGuire A, Wolfe C. Cost of stroke in the United Kingdom. Age Ageing. 2009;38:27–32. doi: 10.1093/ageing/afn281. [DOI] [PubMed] [Google Scholar]
- 6.Department of Health. The national service framework for long term conditions. London: DH; 2005. [Google Scholar]
- 7.Tyerman A, Meehan MJ. Vocational assessment and rehabilitation after acquired brain injury: inter-agency guidelines. London: British Society of Rehabilitation Medicine/Royal College of Physicians; 2004. [Google Scholar]
- 8.Care Quality Commission London, UK: The Care Quality Commission (CQC); 2011. Supporting life after stroke: a review of service for people who have had a stroke and their carers. [Google Scholar]
- 9.Playford E, Radford K, Burton C, et al. London, UK: Department of Health; 2011. Mapping vocational rehabilitation services for people with long term neurological conditions: summary report. [Google Scholar]
- 10.Lock S, Jordan L, Bryan K, Maxim J. Work after stroke: focusing on barriers and enablers. Disabil Soc. 2005;20:33–47. [Google Scholar]
- 11.Barker G. London: The Stroke Association and Different Strokes; 2006. Getting back to work after stroke. [Google Scholar]
- 12.Department of Health. National stroke strategy. London, UK: The Department of Health; 2007. [Google Scholar]
- 13.Black C, Frost D. Health at work; an independent review of sickness absence. London: The Stationary Office; 2011. [Google Scholar]
- 14.Department of Health. Equity and excellence: liberating the NHS. London: The Stationary Office; 2010. [Google Scholar]
- 15.British Society of Rehabilitation Medicine. BSRM standards for rehabilitation services, mapped onto the national service framework for long-term conditions. London: The British Society of Rehabilitation Medicine (BSRM): 2009. [Google Scholar]
- 16.Saeki S, Toyonaga T. Determinants of early return to work after first stroke in Japan. J Rehabil Med. 2010;42:254–8. doi: 10.2340/16501977-0503. [DOI] [PubMed] [Google Scholar]
- 17.Vestling M, Tufvesson B, Iwarsson S. Indicators for return to work after stroke and the importance of work for subjective well-being and life satisfaction. J Rehabil Med. 2003;35:127–31. doi: 10.1080/16501970310010475. [DOI] [PubMed] [Google Scholar]
- 18.Checkland P, Scholes J. Soft systems methodology in action. Chichester: John Wiley; 1999. [Google Scholar]
- 19.British Society of Rehabilitation Medicine. Neurological rehabilitation: a briefing paper for commissioners of clinical neurosciences. London: The British Society of Rehabilitation Medicine (BSRM); 2008. [Google Scholar]
- 20.Black C. Working for a healthier tomorrow; Dame Carol Black's review of the health of Britain's working age population. London: The Stationary Office; 2008. [Google Scholar]
- 21.Scottish Intercollegiate Guidelines Network. Management of patients with stroke; rehabilitation, prevention and management of complications and discharge planning. Edinburgh: NHS Quality Improvement Scotland; 2010. [Google Scholar]
- 22.Saeki S, Ogata H, Okubo T, et al. Return to work after stroke -- a follow-up-study. Stroke. 1995;26:399–401. doi: 10.1161/01.str.26.3.399. [DOI] [PubMed] [Google Scholar]
- 23.Bedekar Y. Vocational rehabilitation: a model for stroke, Glasgow. Int J Stroke. 2009;4:1–45. [Google Scholar]
- 24.Intercollegiate Stroke Working Party. National clinical guidelines for stroke. 3rd. London: Royal College of Physicians; 2008. [Google Scholar]
- 25.Radford KA, Crompton A, Stainer K. Commissioning vocational rehabilitation (VR) after stroke: can the Cinderella service get to the ball? A qualitative study. Health Serv Res J. in press. [DOI] [PubMed]
- 26.Radford KA, Phillips J, Drummond A, et al. Employment rates and health costs one year after traumatic brain injury (TBI) A cohort comparison. Brain Inj. 2012;26:600–1. [Google Scholar]
- 27.Turner-Stokes L, Williams H, Abraham R. Clinical standards for specialist community rehabilitation services in the UK. Clin Rehabil. 2001;15:611–23. doi: 10.1191/0269215501cr455oa. [DOI] [PubMed] [Google Scholar]
- 28.van Eeden M, van Heugten CM, Evers SMAA. The economic impact of stroke in The Netherlands: the €-restore4stroke study. BMC Public Health. 2012;12:122. doi: 10.1186/1471-2458-12-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnstone B, Mount D, Schopp LH. Financial and vocational outcomes 1 year after traumatic brain injury. Arch Phys Med Rehabil. 2003;84:238–41. doi: 10.1053/apmr.2003.50097. [DOI] [PubMed] [Google Scholar]