Summary
Background
The term filariasis comprises a group of parasitic infections caused by helminths belonging to different genera in the superfamily Filaroidea. The human parasites occur mainly in tropical and subtropical regions, but filariae are also found in temperate climates, where they can infect wild and domestic animals. Humans are rarely infected by these zoonotic parasites.
Patients and Methods
A 55-year-old patient presented with a new-onset, subcutaneous, non-tender palpable mass in the right axilla. Ultrasonography showed a 1.3-cm, solid, singular encapsulated node. Sonography of the breast on both sides, axilla and lymphatic drainage on the left side, lymphatic drainage on the right side, and mammography on both sides were without pathological findings. The node was excised under local anesthesia as the patient refused minimal invasive biopsy.
Results
On histopathological examination, the tail of a parasite of the group of filariae was found. The patient revealed that she had stayed in Africa and Malaysia for professional reasons. 6 months before the time of diagnosis, she had also suffered from a fever and poor general condition after a trip abroad. The patient was referred for further treatment to the Institute for Tropical Medicine at the University of Dusseldorf, where a treatment with ivermectin was conducted on the basis of positive staining with antibodies against filariae.
Conclusion
Our case demonstrates the importance of interdisciplinary collaboration between breast center, pathology, and other specialties such as microbiology and tropical medicine.
Keywords: Filariasis, Breast, Axilla
Zusammenfassung
Hintergrund
Der Begriff Filariose umfasst eine Gruppe von parasitären Infektionen, die von Helminthen verschiedener Gattungen der Überfamilie der Filaroidea verursacht werden. Die Humanparasiten kommen hauptsächlich in tropischen und subtropischen Regionen vor. Filarien werden jedoch auch in gemäßigten Klimazonen gefunden, wo sie sowohl Wild- als auch Haustiere infizieren. Menschen werden selten von diesen zoonotischen Parasiten befallen.
Patientin und Methoden
Eine 55-jährige Patientin stellte sich mit dem Verdacht einer neu aufgetretenen axillären Lymphknotenschwellung rechts vor. Die Sonographie der rechten Axilla zeigte einen singulären, 1,3 cm großen, soliden Befund. Sonographie der Mamma beidseits, Axilla und Lymphabflusswege links sowie Lymphabflusswege rechts und Mammographie beidseits waren unauffällig. Der Knoten wurde exzidiert, da die Patientin eine Jet-Biopsie ablehnte.
Ergebnisse
In der Histologie fand sich das Hinterende eines Parasiten aus der Gruppe der Filarien. Die Patientin gab an, beruflich in Afrika und Malaysia gewesen zu sein. Außerdem hatte sie 6 Monate zuvor nach einer Auslandsreise an Fieber und reduziertem Allgemeinzustand gelitten. Die Patientin wurde zur weiteren Behandlung an die Tropenmedizin der Universität Düsseldorf überwiesen, wo aufgrund des positiven Befundes mit Antikörpern gegen Filarien eine Therapie mit Ivermectin durchgeführt wurde.
Schlussfolgerung
Dieser Fall zeigt, wie wichtig die interdisziplinäre Zusammenarbeit zwischen Brustzentrum, Pathologie und weiteren Spezialgebieten wie Mikrobiologie und Tropenmedizin ist.
Introduction
The term filariasis comprises a group of parasitic infections caused by helminths belonging to different genera in the superfamily Filaroidea. The human parasites occur mainly in tropical and subtropical regions, but filariae are also found in temperate climates, where they can infect wild and domestic animals. Humans are rarely infected by these zoonotic parasites.
Case Report
A 55-year-old patient with a family history positive for breast cancer presented with a new-onset, subcutaneous, non-tender palpable mass in the right axilla. High-end ultrasonography showed a 1.3-cm, solid, singular encapsulated node (a B IV). Sonography of the breast on both sides, axilla and lymphatic drainage on the left side, lymphatic drainage on the right side, and mammography on both sides were without pathological findings (American College of Radiology, classification of breast density (ACR) II, B I) (figs. 1 and 2). The node was excised under local anesthesia as the patient refused minimal invasive biopsy. On histopathological examination, a severe granulomatous inflammation with massive eosinophilic infiltrates was found surrounding the tail of a parasite (figs. 3 and 4). A precise diagnosis of the filarial species was not possible because the parasite showed an advanced degree of disintegration. In addition, the cross-section of the worm at the level of the tail did not show morpho-logical criteria sufficient to allow a species diagnosis, but permitted the diagnosis of the genus Dirofilaria. The laboratory results included a serological test. The serology was strongly positive using Dirofilaria immitis antigen, our normal test agent for all kinds of filariae. In addition, low titers were detected against Ascaris lumbricoides and Strongyloides spp. antigen. These are most likely to be interpreted as cross-reactions. The serological tests for Schistosoma spp. and Gnathostoma spinigerum were negative. In the peripheral blood, the count for eosinophilic leukocytes was only minimally raised (6%, normal < 4%). Fecal examinations using microscopy, Baermann technique, and culture were negative. Microfiltration of the blood at noon revealed no microfilariae in the peripheral blood. In an extended medical history, the patient revealed that she had stayed in Africa and Malaysia 6 months before the time of diagnosis. She had also suffered from fever and poor general condition 6 months earlier, after a trip abroad. The clinical examination conducted at that time, including blood samples and serology tests, had been without pathological findings.
Fig. 1.

Macroscopic view prior to excision.
Fig. 2.
Ultrasonography of the right axilla at first presentation, pre-surgical.
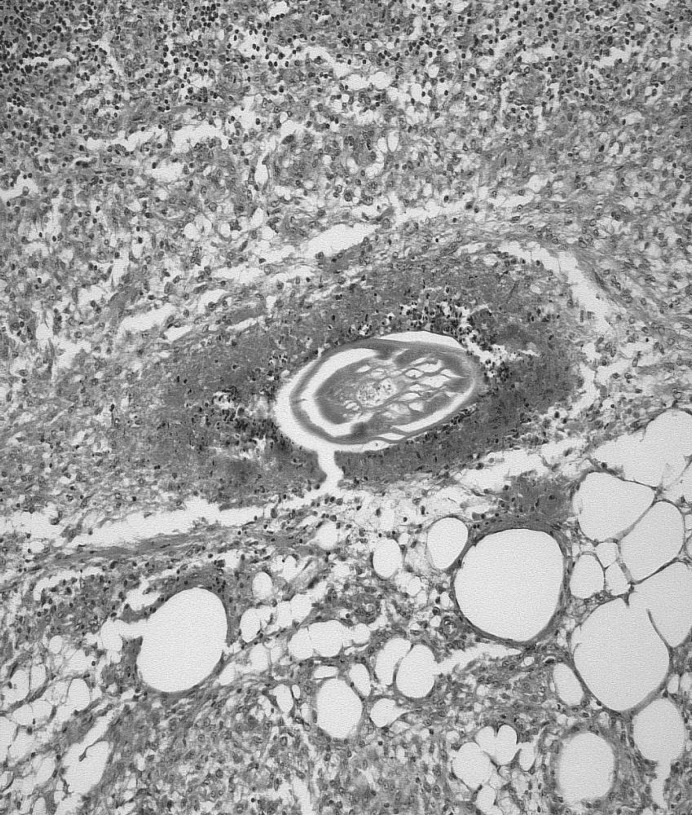
Fig. 3.
Histology of the removed tissue. An oblique cross-cut of the worm, showing a cuticula with at least 2 layers and disintegrated musculature. The surrounding granuloma is packed with degranulated leukocytes.
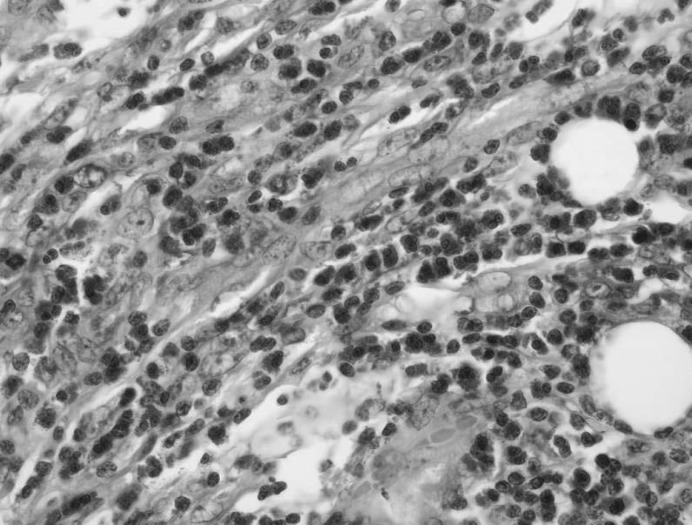
Fig. 4.
Histology of the inflammation at some distance from the parasite: pronounced eosinophilic infiltration.
The patient was referred for further treatment to the Unit for Tropical Medicine at the University of Dusseldorf, where a treatment with ivermectin was conducted on the basis of positive antibodies against filariae, although the test for immunoglobulin G4 (IgG4) was negative, most likely because of the disintegration of the worm. In a follow-up examination 3 months later, the patient showed no further signs of filarial infection; in a follow-up exam 1.5 years later, all serology tests for filariae were negative.
Discussion
While filarial infections in general affect up to 120 million people worldwide [1], diagnoses of infections are very rare in Caucasians in Germany and are mostly due to a temporary stay in tropical countries. Rarely, cases of zoonotic filariasis may originate even in temperate climates. The breast, including the axillary lymph nodes, is an uncommon site for filarial infection (except for Wuchereria bancrofti); only 25 cases have been reported worldwide [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11] (table 1). This case is the first to be reported from Germany.
Table 1.
Cases of filariae in breast and axilla reported worldwide
| Publication | Number of cases, location | Country | Diagnosis and therapy |
|---|---|---|---|
| Bastarrika et al., 2001 [1] | 4, breast | Spain | calcifications in mammography; follow-up mammography, no further treatment |
| Mondal et al., 2010 [2] | 2, breast | India | palpable mass, fine-needle aspiration; follow-up, no further treatment |
| Alkadhi et al., 2005 [3] | 1, breast | Switzerland | palpable masses, mammography; no therapy described |
| Muholkar et al., 2011 [4] | 1, breast | India | palpable mass, fine-needle aspiration; diethyl carbamazepine |
| Parida et al., 2008 [5] | 1, breast | India | palpable mass, fine-needle aspiration; drug treatment for filariae (no specific drug reported) |
| Miller et al., 1965 [6] | 1, breast | Canada | palpable mass, excision; no therapy reported |
| Singh et al., 2009 [7] | 1, breast | India | palpable mass, fine-needle aspiration; no therapy reported |
| Yenkeshwar et al., 2006 [8] | 3, breast | India | palpable mass, fine-needle aspiration; no therapy reported |
| Rukmangadha et al., 2006 [9] | 1, breast | India | palpable mass, fine-needle aspiration; no therapy reported |
| Kapila et al., 1996 [10] | 9, breast and axilla | India | palpable mass, fine-needle aspiration; no therapy reported |
| Kurtycz et al., 1983 [11] | 1, axilla | USA | palpable mass, biopsy; excision |
When a patient is infected by filariae for the first time, usually a poor general condition ensues, as also exhibited by our patient. This is normally not the case in Dirofilaria infections, which are of zoonotic origin. Infection occurs by blood-sucking insects that tranfer the infective stage of the parasite (L 3). In the new host, the larva develops further, but in zoonotic infections (where the parasites are not adapted to humans) this development is usually arrested before the parasite reaches the stage of reproduction. Dead and decaying parasites can cause subcutaneous swelling and local eosinophilia, as seen in our patient [2]. Calcified filariae seen in mammography have also been reported [1, 3]. Interestingly, mammography on both sides of our patient showed no signs of calcification.
Our case shows the importance of interdisciplinary collaboration between breast center, pathology, and other specialties such as microbiology and tropical medicine in case of rare pathological findings in breast and axillary lymph node biopsies. It also emphasizes the need to obtain an exact medical history, including a history of recent travels.
Disclosure Statement
All authors declare that there were no conflicts of interest concerning this work.
References
- 1.Bastarrika G, Pina L, Vivas I, Elorz M, San Julian M, Alberro JA. Calcified filariasis of the breast: report of four cases. Eur Radiol. 2001;11:1195–1197. doi: 10.1007/s003300000711. [DOI] [PubMed] [Google Scholar]
- 2.Mondal SK. Incidental detection of filaria in fine-needle aspirates: A cytologic study of 14 clinically unsuspected cases at different sites. Diagn Cytopathol. 2012;40:292–296. doi: 10.1002/dc.21557. [DOI] [PubMed] [Google Scholar]
- 3.Alkadhi H, Garzoli E. Images in clinical medicine. Calcified filariasis of the breasts. N Engl J Med. 2005;352:e2. doi: 10.1056/ENEJMicm040651. [DOI] [PubMed] [Google Scholar]
- 4.Mudholkar V, Muley P, Suvernkar S, Deshpande S. Filariasis of breast in young female: A case diagnosed on fine needle aspiration cytology. Diagn Cytopathol. 2012;40:466–467. doi: 10.1002/dc.21685. [DOI] [PubMed] [Google Scholar]
- 5.Parida G, Rout N, Samantaray S, Devi P, Pattanayak L, Kakkar S. Filariasis of breast-simulating carcinoma. Breast J. 2008;14:598–599. doi: 10.1111/j.1524-4741.2008.00658.x. [DOI] [PubMed] [Google Scholar]
- 6.Miller MJ, Moore S. Nodular breast lesion caused by Bancroft's filariasis. Can Med Assoc J. 1965;93:711–714. [PMC free article] [PubMed] [Google Scholar]
- 7.Singh NG, Chatterjee L. Filariasis of the breast, diagnosed by fine needle aspiration cytology. Ann Saudi Med. 2009;29:414–415. doi: 10.4103/0256-4947.55178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yenkeshwar PN, Kumbhalkar DT, Bobhate SK. Microfilariae in fine needle aspirates: a report of 22 cases. Indian J Pathol Microbiol. 2006;49:365–369. [PubMed] [Google Scholar]
- 9.Rukmangadha N, Shanthi V, Kiran CM, Kumari NP, Bai SJ. Breast filariasis diagnosed by fine needle aspiration cytology – a case report. Indian J Pathol Microbiol. 2006;49:243–244. [PubMed] [Google Scholar]
- 10.Kapila K, Verma K. Diagnosis of parasites in fine needle breast aspirates. Acta Cytol. 1996;40:653–656. doi: 10.1159/000333934. [DOI] [PubMed] [Google Scholar]
- 11.Kurtycz DF, Alt B, Mack E. Incidental coenurosis: larval cestode presenting as an axillary mass. Am J Clin Pathol. 1983;80:735–738. doi: 10.1093/ajcp/80.5.735. [DOI] [PubMed] [Google Scholar]