Abstract
Objective
To compare the phenomenology and course of bereavement-related depression to depression that occurred later in the course of bereavement and to depression in non-bereaved youth.
Method
This sample is drawn from a cohort of parentally bereaved youth and non-bereaved controls followed for approximately 5 years. Three groups of depressed youth were compared with respect to symptoms, severity, duration, risk for recurrence, and correlates and risk factors: (1) a group with bereavement-related depression (BRD, n = 42), with the onset of a depressive episode within the first 2 months after parental loss; a group with later bereavement depression (LBD, n = 30), with onset at least 12 months after parental loss; and a non-bereaved control group with depression (CD, n = 30).
Results
BRD episodes were similar to LBD and CD with respect to number of symptoms, severity, functional impairment, duration, risk for recurrence, and most risk factors and correlates. BRD, compared with both CD and LBD, were younger, exposed to fewer life events, and less likely to have experienced feelings of worthlessness. Also, caregivers of BRD showed higher rates of depression and post-traumatic stress disorder at the time of the depression compared with each of the other two groups.
Conclusion
BRD is similar to both LBD and CD in phenomenology, course, and risk factors, supporting a diagnostic and therapeutic approach to BRD similar to that for non–bereavement-related depressions. In the bereaved child who presents with depression shortly after parental death, the clinician should also be alert to caregiver depression and post-traumatic stress disorder.
Keywords: bereavement, depression, nosology
Sadness in response to loss and separation has been consistently served as a model for depression in both humans and in animals.1 However, in recognition of the wide variation of the effects of loss, clinicians since antiquity and certainly since the time of Freud have tried to differentiate between the expectable sadness associated with bereavement and true clinical depression that requires treatment.2,3 The attempt to differentiate between an expectable response to bereavement and major depression is reflected in current DSM-IV criteria, which require a 2-month duration, or “marked functional impairment, morbid preoccupation with worthlessness, suicidal ideation, psychotic symptoms, or psychomotor retardation, to make a diagnosis of depression in the post-bereavement period.”4 This additional requirement for the diagnosis of major depression after the loss of a loved one has engendered a wide range of views, ranging from concerns that diagnosing depression in bereaved individuals inappropriately “medicalizes sadness” to advocacy for dropping this exclusionary criterion completely, because it unnecessarily increases the diagnostic and therapeutic threshold for bereaved people with significant depressive symptomatology.5–7 Although there are some data on bereavement-related depression in adults,5,8–13 there are virtually none to inform diagnostic practices in bereaved adolescents.
If depression that immediately follows bereavement is different from depression that occurs at other times, then there should be some differences in phenomenology, risk factors, or course of bereavement-related depression compared with non–bereavement related depression. Studies in adults have found that the risk factors, phenomenology, and course of bereavement-related depression are virtually the same as in non–bereavement-related depression, or, for that matter, in depression related to any other stressful event.5,8–13 Given that major depression appears to be a common sequela of bereavement, it is important to properly classify and refer those bereaved individuals who require mental health care.14,15 To our knowledge, only two studies have examined the correlates, phenomenology, and course of bereavement-related depression in adolescents. In youth who lost a friend to suicide, bereavement-related depression was found to have similar phenomenology, severity, risk factors, and course, compared with depression in the bereaved group that began before exposure.16,17 However, that study relied on recall of depressive episodes that may have begun long before the death, and had very few non-bereaved participants with depression for purposes of comparison. In addition, Weller et al. found that a family history of depression was associated with depression in parentally bereaved children, which also confers a risk for depression in non-bereaved youth.18
In a previous paper, we reported on the incidence and prevalence of the psychiatric sequelae among youth who lost a parent to suicide, accident, or sudden natural death, compared with non-bereaved comparison youth at 9 and 21 months after the death. At 9 months, the bereaved sample showed higher rates of incident depression and post-traumatic stress disorder (PTSD) than non-bereaved controls.19 At 21 months after the death, although the prevalence of depression was still elevated in the bereaved group, the rates of incident depression between 9 and 21 months were similar in the bereaved and non-bereaved groups.14 However, the duration of depressive episodes was longer in the bereaved group.
To address the question of whether the phenomenology of bereavement-related depression is similar to non–bereavement-related depression, we examined the correlates, phenomenology, and course of depression in this cohort over time, of three sub-groups from this sample, characterized by the following: bereavement-related depression (BRD), defined as new-onset depression that began within 2 months of the death; later bereavement depression (LBD) that began at least 12 months after the loss; and (3) non-bereaved control group with depression (CD). We hypothesized that the baseline correlates, clinical phenomenology, and course would be similar among the three groups, thus supporting a common diagnostic and therapeutic approach to depression, regardless of bereavement.
METHOD
Study Sample
The three groups of depressed youth were drawn from a sample of 423 bereaved and non-bereaved offspring. The deceased parents (probands) were between the ages of 30 and 60 years and had died within 24 hours of the precipitating event from suicide, an accident, or sudden natural death. Families in which there were multiple deaths or injuries were excluded. The most common methods of accidental and sudden death were traffic accident and myocardial infarction, respectively. Control families had to have both biological parents alive, and the child living with at least one of them, with no loss of a first or second-degree relative of the child within the past 2 years.
Participant Recruitment
As described previously, bereaved families were recruited through coroner’s records (49.7%) and by newspaper advertisement (50.3%).14,19 Among eligible bereaved families approached for the study, 71% accepted. Those families who accepted were similar to those who did not with respect to age, race, sex, and method of suicide or accident.14,19 Because sudden natural death cases do not necessarily come to the coroner, it is not possible to ascertain the representativeness of these cases. Control families were recruited using random-digit dialing and by advertisement. Controls were frequency matched with the bereaved families on the age, race, sex, and neighborhood of the proband. Of potential controls that were eligible, 55% agreed to participate. The University of Pittsburgh Institutional Review Board approved this study. After a complete description of the study, research interviewers obtained caregivers’ consent for their participation, and either assent or consent for their offspring.
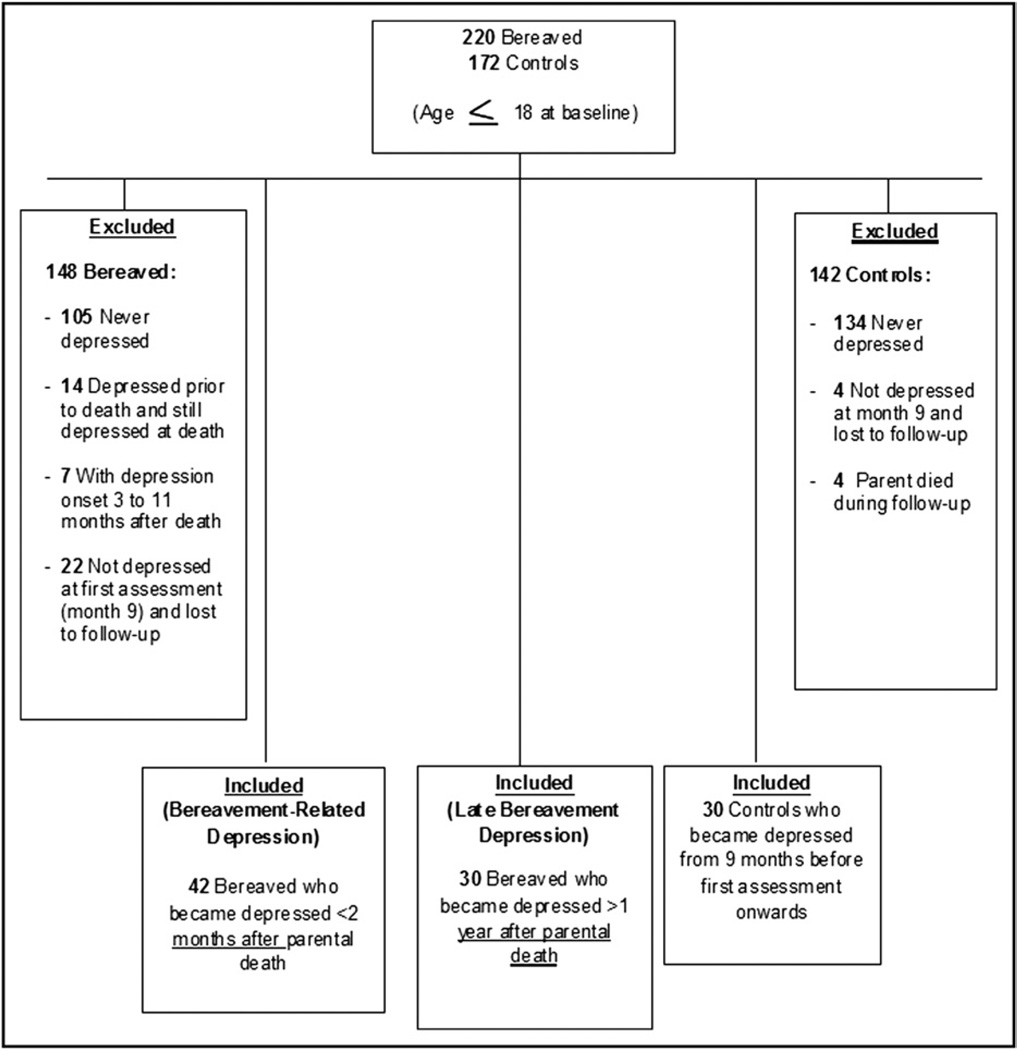
Figure 1 illustrates how the sub-sample for study was selected. It consists of the following: 42 bereaved participants whose depression began within 2 months of the parental death (bereavement-related depression [BRD]); 30 bereaved participants who had not developed BRD but developed a depression at least 12 months after the death (later bereavement depression [LBD]); and 30 non-bereaved individuals who experienced depression (control depression [CD]). Bereaved participants who were depressed before the death and whose depression continued after the death were excluded (n = 14), as were those whose onset of depression occurred 3 to 11 months after the death (n = 7). There were no non-bereaved cases whose depressive onset began before 9 months before the first assessment and continued beyond it. No participant could be in more than one depression group. Of those with BRD, 97.6% had an onset immediately after the death of the parent (median time of onset, 1 month), whereas those with LBD had a median onset 26 months after death (range, 12–82 months), and CD had wide range of onsets (from 8 months before the first assessment to 54 months after it).
FIGURE 1.
Study inclusion flow chart.
Participant Assessment
Participants were interviewed at four points in time, at baseline, and at three follow-up points. In this subsample, the assessments were as follows: mean = 8.0 months after the death, standard deviation (SD) = 3.5; mean = 20.7 months, SD = 3.7; mean = 32.9 months, SD = 3.8; and mean = 65.9, SD = 10.2 months after the death, with parallel timing for the non-bereaved controls. Retention for the study was 89.5%, 73.9%, and 73.1% for the three follow-up points. Participants lost to follow-up were more likely to be bereaved (76.3% versus 53.4%, χ21 = 7.31, p = .007), and caregiving adults of participants lost to follow-up were more functionally impaired (mean 71.06; SD = 13.8 versus mean = 77.9, SD = 11.4), t = 3.30, df = 367, p = .001).
The School Age Schedule for Schizophrenia and Affective Disorders, Present and Lifetime Version (K-SADS-PL)20 was used to assess offspring younger than 18 years old, and the Structured Interview for DSM-IV Axis I Disorders (SCID-I) was used for adult offspring and caregivers.21 The presence of clinically significant symptoms of depression was also assessed using these interviews. The onset, offset, and duration of disorders were recorded on the Adolescent Longitudinal Interval Follow-Up Evaluation (A-LIFE)— Psychiatric Status Ratings (PSR)22 score sheet for offspring younger than 18 years old, and on the Psychiatric Rating Scale (PSR) of the Longitudinal Interval Follow-up Evaluation (LIFE) for older offspring and caregivers.22 The extent of the subject’s recovery from previous episodes of DSM-IV disorders as well as the occurrence and degree of severity of any new disorders was recorded using a four-point rating over monthly intervals on the PSR score sheet (1 = fully recovered; 4 = met criteria for disorder). Psychiatric assessment of the proband was conducted using a psychological autopsy procedure.23 Functional status was determined using the Children’s Global Assessment Scale (CGAS) or the Global Assessment Scale (GAS) for adults.24,25 In both of these scales, a lower score is associated with greater impairment. Inter-rater reliability on the K-SAD-PL and the SCID-I were high (κ values 0.83–100% agreement), as were those for the CGAS, and GAS (intra-class correlations [ICCs] 0.85–0.90).
A battery of self-report instruments was administered to assess the severity of symptomatology, social support, coping, and history of family adversity. Self-reported depression, anxiety, and suicidal ideation were assessed in offspring younger than 18 years using the Mood and Feelings Questionnaire,26 the Screen for Child Anxiety Related Emotional Disorders (SCARED),27 and the Suicide Ideation Questionnaire—Jr. (SIQ-Jr), respectively.28 For adult offspring, the Beck Depression and Anxiety Inventories29,30 and the Adult Suicidal Ideation Questionnaire31 were used. The severity of DSM-IV PTSD symptoms was assessed using the Child PTSD Symptom Scale32 for children, and the parallel PTSD Symptom Scale33 interview for adults.
Intercurrent life events were assessed using the Life Events Checklist in offspring younger than 18 years34 and the Social Readjustment Rating Scale35 in offspring 18 years or older. In this study, life events that were counted occurred either from the time of death to the first assessment or during the inter-assessment period for subsequent interviews. Social support and coping style were evaluated using the Survey of Children’s Social Support36 and the Kidcope37 respectively, in offspring younger than 18 years. The Multidimensional Scale of Perceived Social Support38 and the Ways of Coping Questionnaire39 were used in adult offspring. The Abuse Dimensions Inventory40 was used to obtain abuse history, including physical and sexual abuse. When different measures were used for offspring who were under or over age 18, scores from these measures were standardized.
Data Analysis
We compared the baseline demographic, clinical, and psychological characteristics, assessed at baseline and at the time closest to the depressive episode, among the BRD, LBD, and CD groups using standard parametric and nonparametric univariate statistics (χ2, Fisher’s exact test, analysis of variance (ANOVA), Kruskal–Wallis). In addition, we examined other variables related to depression, namely, symptoms, age of onset, previous history, course, and rates of recurrence. We set the overall α value at 0.05, which is conservative, because the main aim of the study was to test support for the null hypothesis. Accordingly, we set the α value for post-hoc pairwise comparisons at 0.05/3 = 0.017, and at this α value, we had 80% power to detect effect sizes of d = 0.72.41 All tests were two tailed. We then identified the most parsimonious set of variables that discriminated among the groups using multinomial logistic regression. Because of missing data, to conduct these multivariate analyses, we constructed an imputed dataset. We applied Multiple Imputation by Chained Equations (MICE) technique42,43 using the ice command in STATA 11.2.44 This approach is based on each conditional density of a variable, given all other variables, and does not require that the multivariate joint normal distribution assumption be met. MICE allows for the conjoint imputation of variables based on a set of predictor variables by an appropriate regression model (e.g., ordinary least square, logit). We used the multiple imputation approach with an inclusive strategy as recommended by Collins et al.,45 which makes use of auxiliary variables that are correlates of missingness and/or correlates of the variable of interest, to improve the missing data procedure. Multiple imputed datasets were created and combined using the “mim” command for regression analysis. Convergence was observed after five imputations. Similar results were obtained using the imputed and the original datasets. We report here the results from the imputed dataset. We also compared the three groups on time to recurrence of a depressive episode using Kaplan–Meier survival analysis and the Wilcoxon and log-rank tests.
RESULTS
Demographic Characteristics
The three groups differed with respect to age, socio-economic status after the death, and duration of follow-up (Table 1). Post hoc, the BRD group was significantly younger compared with both LBD (mean = 13.3, SD = 3.0 versus mean = 16.5, SD = 3.3, years; p < .001) and CD (mean = 16.5, SD = 3.5 years, p < .001). In fact, almost all of the BRD youth were less than 18 years of age at the time of their depression (90.4%) versus only half of the LBD (53.3%) and of the CD (50%; χ22 = 17.08, p = .0002; pairwise contrasts both significant at p < .0009). Pairwise contrasts showed that the BRD group had a lower socioeconomic status compared with the CD group (mean = 35.7, SD = 13.7 versus mean = 44.8, SD = 9.4; p = .002) and that BRD youth had a shorter period of follow-up than the LBD group (mean = 52.1, SD = 23.6 vs. mean = 66.1, SD = 13.5, months, p = .004).
TABLE 1.
Offspring Demographic and Statistically Significant Clinical and Psychological Characteristics of Youth, by Depression Group
| BRD (n = 42) | LBD (n = 30) | CD (n = 30) | Test | df | p | |
|---|---|---|---|---|---|---|
| Age (years at relevant timepoint) | 13.3 ± 3.0a | 16.5 ± 3.3b | 16.5 ± 3.5b | F = 11.94 | 2, 97 | <.001 |
| Socioeconomic status after death | 35.7 ± 13.7a | 41.1 ± 10.2ab | 44.8 ± 9.4b | F = 5.13 | 2, 92 | .008 |
| Duration of follow-up (mo) | 52.1 ± 23.6a | 66.1 ± 13.5b | 54.2 ± 19.8ab | F = 4.67 | 2, 99 | .01 |
| Sex, n (% female) | 21 (50.0) | 17 (56.7) | 22 (73.3) | χ2 = 4.01 | 2 | .13 |
| Race/ethnicity, n (% white) | 32 (76.2) | 25 (83.3) | 26 (86.7) | χ2 = 1.38 | 2 | .50 |
| PTSD (self-report) | 8.0 ± 8.5ab | 9.8 ± 8.9a | 3.0 ± 3.1b | KW: χ2 = 6.87 | 2 | .03 |
| Life events | 0.5 ± 1.5a | 6.2 ± 3.3b | 4.2 ± 4.1b | KW: χ2 = 40.54 | 2 | <.001 |
Note: Data are mean ± SD unless otherwise indicated. Items with different superscripts are significantly different at α = 0.017.
BRD = bereavement-related depression (within 2 months of loss); CD = depression in controls; LBD = later depression in the bereaved; KW = Kruskal–Wallis test; PTSD = posttraumatic stress disorder.
Clinical Characteristics of Offspring
The groups were similar with respect to self-reported depression, anxiety, suicidal ideation, and aggression (all p > .56), but differed with respect to current PTSD symptomatology (Kruskal-Wallis χ22 = 6.87, p = .03), with significant pairwise differences between CD (mean = 3.0, SD = 3.1) and LBD (mean = 9.8, SD = 8.9) (p = .007) (Table 1). There was a significant difference among the groups with respect to life events experienced since the previous assessment (p < .001), with significant pairwise contrasts between the BRD group and both the LBD (mean = 0.5, SD = 1.5 versus mean = 6.2, SD = 3.3; p < .001) and the CD groups (mean = 4.2, SD = 4.1, p < .001). The offspring groups were similar with respect to self-esteem, coping, social support, family adaptability and cohesion, and frequency of a history of physical and sexual abuse (all p > .15).
Phenomenology of Depression
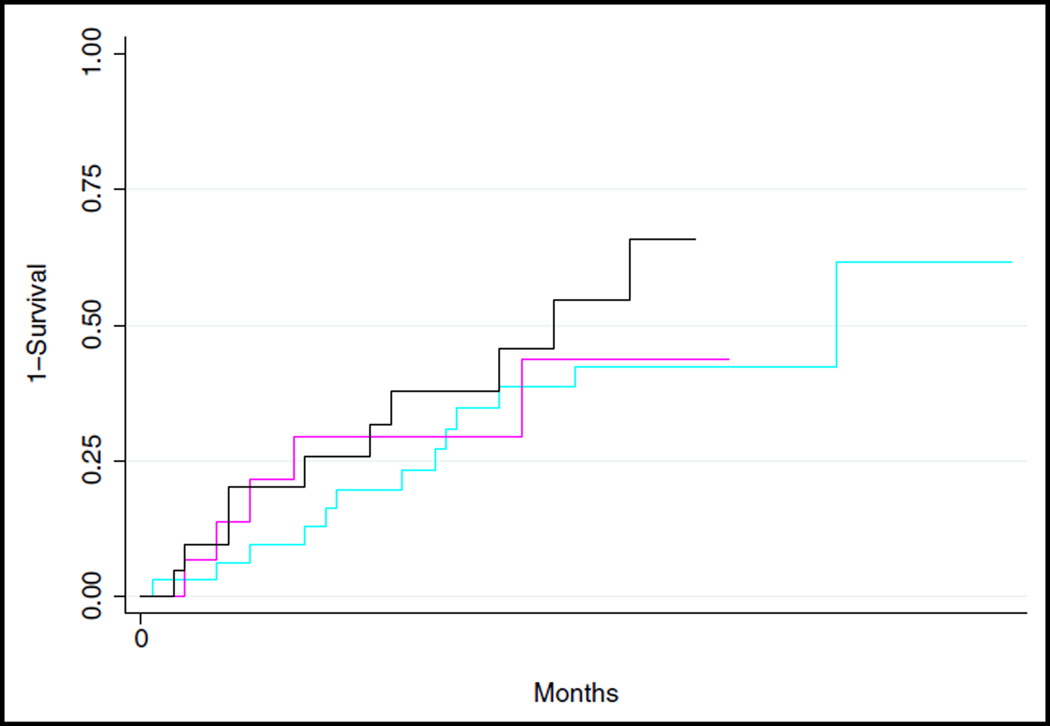
There was an overall difference in the duration of depressive episodes, as determined by the A-LIFE (p = .009), with no differences between BRD and either of the other two groups, but a pairwise difference showing a higher episode length in LBD versus CD (p = .001) (Table 2). There were no group differences with respect to risk for a depressive recurrence (Wilcoxon test: χ22 = 1.29, p = .52; log-rank test: χ22 = 1.56, p = .46) (Figure 2). There were no group differences with respect to the frequencies of a lifetime previous history of depression with onset before death (FET: p = .12). The rates of mental health treatment (at least one professional contact) were similar across groups. In addition, there were no group differences in the total number of symptoms, as determined by the K-SADS-PL and SCID-I (p = .13), but there were group differences with respect to the presence of clinically significant anhedonia, fatigue, feelings of worthlessness, and inappropriate feelings of guilt (p < .01) (Table 2). Post-hoc pairwise comparisons showed that BRD had a lower prevalence of clinically significant fatigue compared with LBD (p = .003), and lower prevalence of anhedonia (p = .004), fatigue (p = .007), feelings of worthlessness (p = .009), and feelings of guilt (p = .003) compared with CD.
TABLE 2.
Phenomenology of Depression Among the Depression Groups
| BRD (n = 42) | LBD (n = 30) | CD (n = 30) | Test | df | p | |
|---|---|---|---|---|---|---|
| History of depression before death, n (%) | 8 (19.0) | 2 (6.7) | 8 (26.7) | χ2 = 4.23 | 2 | .12 |
| Duration of MDD episode (mo)a (M ± SD) | 12.9 ± 13.9de | 17.6 ± 13.8d | 9.8 ± 13.3e | KW: χ2 = 9.46 | 2 | .009 |
| Mental health treatment, n (%) | 31 (73.8) | 22 (73.3) | 20 (66.7) | χ2 = 0.50 | 2 | .78 |
| Depression Symptoms (n, %) | ||||||
| No. of symptoms (mean ± SD)b | 4.3 ± 1.7 | 4.6 ±1.7 | 5.2 ± 1.9 | F = 2.12 | 2, 85 | .13 |
| Anhedoniaa | 17 (42.5)d | 13 (48.1)de | 21 (77.8)e | χ2 = 8.65 | 2 | .01 |
| Fatigue | 13 (33.3)d | 18 (72.0)e | 17 (68.0)e | χ2 = 11.94 | 2 | .003 |
| Feelings of worthlessness | 11 (27.5)d | 13 (56.5)de | 14 (60.9)e | χ2 = 8.53 | 2 | .01 |
| Inappropriate feelings of guilt | 4 (10.3)d | 3 (14.3)de | 10 (43.5)e | FET | — | .008 |
| Depressed mood | 37 (88.1) | 20 (71.4) | 25 (89.3) | FET | — | .15 |
| Irritability and anger | 24 (60.0) | 16 (72.7) | 12 (52.2) | χ2 = 2.04 | 2 | .36 |
| Suicidality/thoughts of death | 8 (19.5) | 6 (30.0) | 8 (32.0) | χ2 = 1.54 | 2 | .46 |
| Lack of reactivityc | 7 (22.6) | 5 (29.4) | 2 (14.3) | FET | — | .62 |
| Sleep difficulties | 25 (64.1) | 14 (63.6) | 20 (71.4) | χ2 = 0.48 | 2 | .79 |
| Concentration | 18 (42.9) | 15 (60.0) | 12 (46.2) | χ2 = 1.92 | 2 | .38 |
| Appetite | 17 (44.7) | 9 (40.9) | 10 (43.5) | χ2 = 0.08 | 2 | .96 |
Note: Items with different superscripts (d, e) are significantly different at α = .017.
BRD = bereavement-related depression (within 2 months of loss) group; CD = depression in controls; FET = Fisher’s exact test; KW = Kruskal–Wallis test; LBD = later depression in the bereaved (≥ 1 year after loss).
Determined by the Longitudinal Follow-up Interview, Adolescent and Adult versions (A-LIFE and LIFE).22
Determined by symptoms counts from the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL) and Structured Clinical Interview for DSM Disorders (SCID-I).20,21
Lack of reactivity of depressed or irritable mood to positive stimuli: short duration and small degree of temporary improvement in mood is associated with positive environmental events.
FIGURE 2.
Kaplan–Meier plots comparing the risk of recurrence of depression among groups. Note: Cyan line represents the bereavement-related depression (BRD) (within 2 months of loss) group. Magenta line represents the later bereavement depression (LBD) group. Black line indicates the controls with depression (CD) group. Wilcoxon test: χ22 = 1.29, p = .52. Log-rank test: χ22 = 1.56, p = .46.
Probands and Adult Caregivers
The probands of the three groups were similar except for rates of antisocial personality disorder (χ22 = 9.30, p = .01); in post-hoc comparisons, CD probands showed lower rates of antisocial personality disorder than BRD probands (0.0% versus 26.2%, p = .002) and LBD probands (0.0% versus 24.1%, p = .005) (Table 3). For adult caregivers, there were no differences among the three groups with respect to rates of previous (history up to and including the time of death) psychiatric disorders. There were group differences with respect to the clinical status of caregivers at the same interview point as the depression in offspring with respect to current caregiver depression (p = .001), PTSD (p < .001), and functional status (p = .001). In post-hoc comparisons, the caregivers of BRD showed higher rates of current depression compared with LBD (57.1% versus 20.7%, χ21 = 9.34, p = .002) and compared with CD (57.1% vs. 11.5%, χ21 = 13.95, p < .001), higher rates of PTSD compared with LBD (45.2% versus 10.3%, χ21 = 9.77, p = .002) and CD (45.2% versus 7.7%, χ21 = 10.61, p = .001), and showed greater functional impairment compared with CD (mean = 69.2, SD = 12.9 versus mean = 81.3, SD = 9.0; p < .001).
TABLE 3.
Statistically Significant Differences Among Depression Groups in Probands and Adult Caregivers
| BRD (n = 42) | LBD (n = 30) | CD (n = 30) | Test | df | p | |
|---|---|---|---|---|---|---|
| Proband | ||||||
| Antisocial personality, n (%) | 11 (26.2)a | 7 (24.1)a | 0 (0.0)b | χ2 = 9.30 | 2 | .01 |
| Adult Caregiver | ||||||
| Depression (current), n (%) | 24 (57.1)a | 6 (20.7)b | 3 (11.5)b | χ2 = 18.15 | 2 | .001 |
| PTSD (current), n (%) | 19 (45.2)a | 3 (10.3)b | 2 (7.7)b | χ2 = 16.76 | 2 | <.001 |
| Functional impairment, (M ± SD) | 69.2 ± 12.9a | 74.6 ± 14.3ab | 81.3 ± 9.0b | F = 7.58 | 2, 93 | .001 |
Note: Items with different superscript letters are significantly different at α = 0.017.
BRD = bereavement-related depression (within 2 months of loss); CD = depression in controls; LBD = later depression in the bereaved group (≥ 1 year after loss); PTSD = post-traumatic stress disorder.
Multinomial Logistic Regression
The risk factors and correlates of BRD relative to CD and to LBD were assessed using multinomial logistic regression. The most parsimonious set of predictors and correlates of BRD compared with CD were younger age (risk rate ratio [RRR] = 0.76, 95% CI = 0.59–0.98, p = .03), fewer number of life events (RRR = 0.51, 95% CI = 0.31–0.83, p = .009), lower socio-economic status (RRR = 0.92, 95% CI = 0.86–0.98, p = .01) and absence of feelings of worthlessness (RRR = 0.12, 95% CI = 0.02–0.69, p = .02). Similarly, BRD, relative to LBD, were younger (RRR = 0.77, 95% CI = 0.60–0.99, p = .04), had experienced fewer life events (RRR = 0.44, 95% CI = 0.28–0.70, p < .001), and were less likely to have had feelings of worthlessness (RRR = 0.09, 95% CI = 0.01–0.55, p = .01).
DISCUSSION
The aim of this report was to examine whether the phenomenology of bereavement-related depression is similar to depression that occurred later in the course of bereavement, or to non–bereavement-related depression. We found that bereaved youth who became depressed shortly after the death of their parent had depressive episodes that were similar in length, severity, and number of symptoms compared with both bereaved youth whose depression occurred at least 12 months after the loss and non-bereaved youth who experienced a depression. The likelihood of recurrence of depression was also similar among the three groups. BRD was distinguished from both CD and LBD by being younger, and having been exposed to fewer life events, and were less likely than either of the other two groups to have clinically significant feelings of worthlessness. Although not significant in the multivariate model, the caregiving parents of BRD were more likely to be depressed and to have PTSD compared with the other two groups.
These results should be considered in the context of the strengths and limitations of this study. It is one of the only prospective, controlled community studies of parental bereavement to be conducted, with relatively good sample retention over a 5-year period of time and with periodic assessments across a broad range of salient domains. However, because of our sample size, we are powered to detect only medium to large effect sizes that might discriminate among these three groups. Also, youth were assessed at 8 months after the parent’s death, so that brief depressive episodes of questionable clinical significance that occurred shortly after the death might have been less likely to be reported. Finally, this study focuses on bereavement-related depression in adolescents, which may or may not be similar to bereavement-related depression in older individuals. For example, youth who are bereaved by sudden parental death are at higher risk for depression, not only because of the experience of bereavement but because conditions that predispose parents to die young also place their children at increased risk for a mood disorder.19
Our most important finding in this study was that the phenomenology of bereavement-related depression, with respect to range and severity of depressive symptoms, episode duration, treatment history, and risk of recurrence was similar in bereavement-related depression compared with those depressive episodes that occurred at least 12 months after the loss in the bereaved sample, or at any point in time in the non-bereaved control group. These findings are consistent with previous studies that compare bereavement-related and non–bereavement-related depression in adolescents16,17 and in adults.5,8,9,11,13
Although the preponderance of evidence supports similar phenomenology and course of depression in BRD versus the other two groups, we did find lower frequencies of clinically significant worthlessness in BRD. Since the symptom count, severity, duration, and risk for recurrence among the BRD is similar to CD despite having a slightly different symptom profile, this suggests that the presence or absence of worthlessness as a symptom is not of a great prognostic significance.
Other than a lower prevalence of feelings of worthlessness, the most robust variables that discriminated BRD from the other two groups were younger age and lower number of stressful life events. Although, at first, the finding of lower numbers of life events in the BRD group seems counterintuitive, this finding may be attributable to a widely accepted view that parental bereavement is a qualitatively different and more severe stressor than almost any other life event, and consequently, in these youth, no additional life events were necessary to precipitate a depression. This is consistent with our previous finding that bereavement per se is associated with a threefold increased risk of incident depression even after controlling for antecedent individual and familial risk factors (including previous personal and family history of psychiatric disorders).19 In contrast, in those who either were not bereaved or whose depression developed much later after the death, an accumulation of other types of stressors may have been required to increase the risk of a depressive occurrence.
The association of caregiver depression and PTSD with BRD is consistent with previously reported path analyses showing that parental caregiver functioning partially mediated the effects of parental bereavement on youth depression.14 Identification and treatment of depression, as well as other psychopathology in the parents of these youth, is important; as the treatment of depression in mothers results in improved treatment outcome in their children.46,47 As almost all of the BRD, but only half of the other two groups, were less than 18 years of age, this suggests that younger children are more vulnerable to the immediate effects of bereavement when the surviving parent is depressed.
Our findings are consonant with the view the depression that follows immediately after bereavement has a similar phenomenology and course to depression that is not related to bereavement, and support the removal of the bereavement exclusion. However, other researchers who have looked at bereavement-related depression within 2 months of the loss have drawn divergent conclusions.
For example, in a large community study of adults, Mojtabai et al.48 compared bereaved and non-bereaved individuals whose episodes of depression were less than 2 months in duration, and found that the bereaved and non-bereaved individuals differed with respect to severity, comorbidity, and likelihood of recurrence, causing the authors to conclude that the exclusion criteria for depression should be retained in DSM-V. Although our sample of bereavement-related depression did begin within 2 months of parental death, the average duration was much more than 2 months, meaning that brief-duration bereavement-related depression was rare in our sample.
In summary, these findings support the view that the phenomenology, risk factors, and course of bereavement-related depression are similar to those of depression that occurs later in the course of bereavement or in non-bereaved individuals. Therefore, we recommend a common approach to the diagnosis and treatment of depression in adolescents, regardless of bereavement status. However, because bereaved youth whose depressive episodes began shortly after the death of the parent were younger and had caregivers who were more likely to have depression and PTSD, the treatment of bereavement-related depression needs to be considered in the context of the youth’s surviving family.
Acknowledgments
This study work was supported by R01grant MH65368 (DAB), K01 grant MH77930 (N.M.M.), a young investigator award from the American Foundation for Suicide Prevention (N.M.M.), and a Fulbright Scholarship from the Council for International Exchange of Scholars—a Division of the Institute of International Education (S.H.).
Footnotes
Disclosure: Dr. Brent has received research support from the National Institute of Health. He receives royalties from Guilford Press. He servers as editor for UpToDate Psychiatry. Drs. Hamdan and Melhem, and Ms. Porta and Ms. Walker Payne report no biomedical financial interests or potential conflicts of interest.
Contributor Information
Sami Hamdan, University of Pittsburgh School of Medicine and Tel Aviv Jaffa College..
Nadine M. Melhem, University of Pittsburgh School of Medicine..
Giovanna Porta, Western Psychiatric Institute and Clinic.
Monica Walker Payne, Western Psychiatric Institute and Clinic.
David A. Brent, University of Pittsburgh School of Medicine and Western Psychiatric Institute and Clinic.
References
- 1.Gilmer WS, McKinney WT. Early experience and depressive disorders: human and non-human primate studies. J Affect Disord. 2003;75:97–113. doi: 10.1016/s0165-0327(03)00046-6. [DOI] [PubMed] [Google Scholar]
- 2.Jackson DN, MacLennan RN, Erdle SW, Holden RR, Lalonde RN, Thompson GR. Clinical judgments of depression. J Clin Psychol. 1986;42:136–145. doi: 10.1002/1097-4679(198601)42:1<136::aid-jclp2270420123>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 3.Freud S. 14th ed. London: Vintage; 1917. Mourning and Melancholia. [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 5.Zisook S, Shear K, Kendler KS. Validity of the bereavement exclusion criterion for the diagnosis of major depressive episode. World Psychiatry. 2007;6:102–107. [PMC free article] [PubMed] [Google Scholar]
- 6.Horwitz AV, Wakefield JC, Spitzer RL. The Loss of Sadness: How Psychiatry Transformed Normal Sorrow into Depressive Disorder. New York: Oxford University Press; 2007. [DOI] [PubMed] [Google Scholar]
- 7.Wakefield JC, Baer JC, Schmitz MF. Differential diagnosis of depressive illness versus intense normal sadness: how significant is the ‘clinical significance criterion’ for major depression? Expert Rev Neurother. 2010;10:1015–1018. doi: 10.1586/ern.10.67. [DOI] [PubMed] [Google Scholar]
- 8.Karam EG, Tabet CC, Alam D, et al. Bereavement related and non-bereavement related depressions: a comparative field study. J Affect Disord. 2009;112:102–110. doi: 10.1016/j.jad.2008.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kessing LV, Bukh JD, Bock C, Vinberg M, Gether U. Does bereavement-related first episode depression differ from other kinds of first depressions? Soc Psychiatry Psychiatr Epidemiol. 2010;45:801–808. doi: 10.1007/s00127-009-0121-6. [DOI] [PubMed] [Google Scholar]
- 10.Bruce ML, Kim K, Leaf PJ, Jacobs S. Depressive episodes and dysphoria resulting from conjugal bereavement in a prospective community sample. Am J Psychiatry. 1990;147:608–611. doi: 10.1176/ajp.147.5.608. [DOI] [PubMed] [Google Scholar]
- 11.Kendler KS, Myers J, Zisook S. Does bereavement-related major depression differ from major depression associated with other stressful life events? Am J Psychiatry. 2008;165:1449–1455. doi: 10.1176/appi.ajp.2008.07111757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lamb K, Pies R, Zisook S. The bereavement exclusion for the diagnosis of major depression: to be, or not to be. Psychiatry (Edgmont) 2010;7:19–25. [PMC free article] [PubMed] [Google Scholar]
- 13.Corruble E, Chouinard VA, Letierce A, Gorwood PA, Chouinard G. Is DSM-IV bereavement exclusion for major depressive episode relevant to severity and pattern of symptoms? A case-control, cross-sectional study. J Clin Psychiatry. 2009;70:1091–1097. doi: 10.4088/JCP.08m04475. [DOI] [PubMed] [Google Scholar]
- 14.Brent D, Melhem N, Donohoe MB, Walker M. The incidence and course of depression in bereaved youth 21 months after the loss of a parent to suicide, accident, or sudden natural death. Am J Psychiatry. 2009;166:786–794. doi: 10.1176/appi.ajp.2009.08081244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaplow JB, Saunders J, Angold A, Costello EJ. Psychiatric symptoms in bereaved versus nonbereaved youth and young adults: a longitudinal epidemiological study. J Am Acad Child Adolesc Psychiatry. 2010;49:1145–1154. doi: 10.1016/j.jaac.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brent DA, Perper J, Moritz G, et al. Bereavement or depression? The impact of the loss of a friend to suicide. J Am Acad Child Adolesc Psychiatry. 1993;32:1189–1197. doi: 10.1097/00004583-199311000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Brent DA, Perper JA, Moritz G, Liotus L, Schweers J, Canobbio R. Major depression or uncomplicated bereavement? A follow-up of youth exposed to suicide. J Am Acad Child Adolesc Psychiatry. 1994;2:231–239. doi: 10.1097/00004583-199402000-00012. 33. [DOI] [PubMed] [Google Scholar]
- 18.Weller RA, Weller EB, Fristad MA, Bowes JM. Depression in recently bereaved prepubertal children. Am J Psychiatry. 1991;148:1536–1540. doi: 10.1176/ajp.148.11.1536. [DOI] [PubMed] [Google Scholar]
- 19.Melhem NM, Walker M, Moritz G, Brent DA. Antecedents and sequelae of sudden parental death in offspring and surviving caregivers. Arch Pediatr Adolesc Med. 2008;162:403–410. doi: 10.1001/archpedi.162.5.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 21.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) (Version 2.0) Washington DC: American Psychiatric Press; 1996. [Google Scholar]
- 22.Keller MB, Lavori PW, Friedman B, et al. The Longitudinal Interval Follow-Up Evaluation: a comprehensive method for outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 23.Hawton K, Appleby L, Platt S, et al. The psychological autopsy approach to studying suicide: a review of methodological issues. J Affect Disord. 1998;50:269–276. doi: 10.1016/s0165-0327(98)00033-0. [DOI] [PubMed] [Google Scholar]
- 24.Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H. A Children’s Global Assessment Scale (C-GAS) Arch Gen Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 25.Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- 26.Angold A, Costello EJ, Messer SC, Pickles A, WInder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatr Res. 1995;5:237–249. [Google Scholar]
- 27.Birmaher B, Khetarpal S, Brent D, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- 28.Reynolds WM. Suicidal ideation and depression in adolescents: assessment and research. In: Lovibond P, Wilson P, editors. Clinical and Abnormal Psychology. Amsterdam: Elsevier; 1989. pp. 125–135. [Google Scholar]
- 29.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 30.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 31.Reynolds WM. Suicidal Ideation Questionnaire: Professional Manual. Odessa, FL: Psychological Assessment Resources; 1988. [Google Scholar]
- 32.Foa EB, Johnson KM, Feeny N, Treadwell KR. The Child PTSD Symptom Scale: a preliminary examination of its psychometric properties. J Clin Child Psychology. 2001;30:376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- 33.Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress. 1993;6:459–473. [Google Scholar]
- 34.Brand AH, Johnson JH. Note on reliability of the Life Events Checklist. Psychol Rep. 1982;50:1274. [Google Scholar]
- 35.Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res. 1967;11:213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 36.Dubow EF, Ullman DG. Assessing social support in elementary school children: the survey of children’s social support. J Clin Child Psychology. 1989;18:52–64. [Google Scholar]
- 37.Spirito A, Stark LJ, Williams C. Development of a brief coping checklist for use with pediatric populations. J Pediatr Psychol. 1988;13:555–574. doi: 10.1093/jpepsy/13.4.555. [DOI] [PubMed] [Google Scholar]
- 38.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52:30–41. [Google Scholar]
- 39.Lazarus RS. Coping theory and research: past, present, and future. Psychosom Med. 1993;55:234–247. doi: 10.1097/00006842-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Chaffin M, Wherry JN, Newlin C, Crutchfield A, Dykman R. The Abuse Dimensions Inventory: initial data on a research measure of abuse severity. J Interpers Viol. 1997:569–589. [Google Scholar]
- 41.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 1st ed. New York: Academic Press, Inc.; 1977. [Google Scholar]
- 42.Royston P. Multiple imputation of missing values: further update of ice, with an emphasis on categorical variables. Stata J. 2009;9:466–477. [Google Scholar]
- 43.Van Buuren S, Oudshoorn CGM. Flexible multivariate imputation by MICE. Leiden: Netherlands: TNO Institute of Prevention and Health; 1999. [Google Scholar]
- 44.ICE: Stata module for multiple imputation of missing values. [Accesssed November 9, 2011];2011 Available at: http://ideas repec org/c/boc/bocode/s446602 html. [Google Scholar]
- 45.Collins L, Schafer JL, Kam CM. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychol Methods. 2001;6:330–351. [PubMed] [Google Scholar]
- 46.Swartz HA, Frank E, Zuckoff A, et al. Brief interpersonal psychotherapy for depressed mothers whose children are receiving psychiatric treatment. Am J Psychiatry. 2008;165:1155–1162. doi: 10.1176/appi.ajp.2008.07081339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pilowsky DJ, Wickramaratne P, Talati A, et al. Children of depressed mothers 1 year after the initiation of maternal treatment: findings from the STAR*D-Child study. Am J Psychiatry. 2008;165:1136–1147. doi: 10.1176/appi.ajp.2008.07081286. [DOI] [PubMed] [Google Scholar]
- 48.Mojtabai R. Bereavement-related depressive episodes: characteristics, 3-year course, and implications for the DSM-5. Arch Gen Psychiatry. 2011;68:920–928. doi: 10.1001/archgenpsychiatry.2011.95. [DOI] [PubMed] [Google Scholar]