Abstract
Objective
We investigate trends in contraceptive behaviors in France and how they may have contributed to fluctuations in unintended pregnancy rates over time and across subgroups of the population between 2000 and 2010.
Study design
Data are drawn from 3 national surveys in France, comprising 4714 women ages 15 to 49 in 2000, 8613 in 2005 and 5260 in 2010. We used multinomial and simple logistic regression models to explore trends in contraceptive behaviors over time. We estimated trends in unintended pregnancy rates in relation to population shifts in contraceptive behaviors between 2000 and 2010.
Results
A third of women were not using contraception at the time of the surveys. However, only 2.4% in 2000, 3.2% in 2005 and 2.4% in 2010 had an unmet need for contraception (p=0.002). Among contraceptive users, user-dependent hormonal methods decreased from 59% in 2000 to 52% in 2010 (p<0.0001), while long acting reversible methods increased from 22% to 24% (p=0.04). Changes in contraceptive behaviors resulted in fluctuations in unintended pregnancy rates estimated to have risen from 3.16% to 3.49% between 2000 and 2005, and to have decreased to 3.26% in 2010. Small changes in unmet need for contraception exerted the largest effects.
Conclusion
This study indicates that changes in contraceptive behaviors over the past decade in France have potentially resulted in significant fluctuations in unintended pregnancy rates. Our results also demonstrate that a simple algorithm combining contraceptive behaviors and typical use failure rates may be an acceptable proxy for monitoring trends in unintended pregnancies.
Keywords: contraception behavior, unintended pregnancy, contraceptive failure rates, population based survey, France
INTRODUCTION
After experiencing a large-scale increase in use of very effective methods of contraception (hormonal contraception and the Intra uterine device (IUD), as sterilization is marginal in France) from the 1970s to the mid 1990s, the gain in very effective contraceptive coverage in France seems to have stalled to a high of 82% of women in need of contraception (women who have been sexually active in the past year, non sterile, not pregnant or trying to conceive) while 15% were using barrier or natural methods (condoms, withdrawal or fertility awareness methods) and less than 3% had an unmet need for contraception (women in need of contraception who are not using a method) (1). This stabilization was confirmed in the 2005 French Barometer survey (2). Annual abortion rates have increased from 13.6 to 14.8 per 1000 women ages 15 to 49 between 1999 and 2006 and stabilized since at 14.7 per 1000 in 2010 (3). These fluctuations are more pronounced in women under the age of 25 years with a 12% increase in abortion rates between 1999 and 2006 (from 18.99 per 1000 to 21.53 per 1000) followed by a subsequent 3% drop in the next 3 years, leveling out at 20.9 per 1000 in 2010 (3). Abortion rates, however, result from a complex series of conditional decisions involving sexual activity, contraceptive practices and decisions to terminate an unintended pregnancy (pregnancies that are either mistimed or unwanted) (4). Therefore, in order to improve our understanding of recent trends in reproductive behaviors and outcomes in France, we explore how patterns of contraceptive behaviors may contribute to fluctuations in unintended pregnancies rates over time.
MATERIALS AND METHODS
Study population
In this study we use data from the 2000 and 2005 waves of the National Health Barometer Survey, a periodic national French study assessing knowledge, attitudes and behaviors of the general population with respect t o health. We also use data from the FECOND study, the most recent national survey on sexual and reproductive health in France conducted in 2010.
The two waves of the Health Barometer survey shared the same study protocol. Sampling design and data collection have been published in detail elsewhere (5). A two stage probability sampling procedure was used to identify 13,685 male and female respondents between the ages of 12 and 75 years in 2000, and 30,514 respondents of the same ages in 2005. An initial sample of households was drawn from the telephone directory, from which one eligible respondent per household was then randomly selected to participate. The present analysis includes 4,775 women aged 15–49 years in 2000 and 8,776 in 2005.
The FECOND study followed the same methodology for selecting a national probably sample of 7,340 male and female respondents’ ages 15 to 49 who had a landline. The survey also included a subsample of 1,193 individuals who were cell phone only users to represent the growing population who does not own a landline (14% of the 15 to 49 age group in France in 2009). One eligible individual per telephone number was randomly selected for participation. Both samples were merged as a unique population as individuals responded to the same questionnaire. The overall refusal rate was 20% among eligible participants. All 3 studies received approval from the relevant French government oversight agency (CNIL, the Commission Nationale de l’Informatique et des Libertés).
Socio-demographic and reproductive health histories
In all 3 surveys, data were collected via anonymous telephone interviews, after participants had given oral consent. Questionnaires included a set of social and demographic questions as well as indicators of women’s sexual and reproductive histories. We retained factors that were comparable across the 3 surveys, including age, level of education, professional situation, marital and cohabitation status, number of children in the household, lifetime sexual experience, sexual activity in the last year, history of abortion and sexually transmitted disease. While questions were identical in the 2000 and 2005 Health Barometer surveys, some formulations differed slightly in the 2010 FECOND survey. In particular, all women were asked about a current partner at the beginning of the survey in the FECOND survey, while current partner status resulted as a combination of living with a partner or having a boyfriend/girlfriend in the Health Barometer surveys. Women were asked about their own children, adopted children and children currently living in the household in the FECOND survey while they were only asked if they had children and if so, if the children were living in the household in the Health Barometer surveys. Finally, the FECOND study provided a detailed description of all pregnancy outcomes, whereas the Health Barometer Surveys collected lifetime history of abortions with a single question “In the course of your life, have you ever had an elective abortion, by taking the RU pill or having a surgical intervention”.
Current contraceptive practices
All 3 surveys collected the same information on current contraceptive behaviors and reasons for non-use. A hierarchical algorithm was used to identify the most effective method based on typical use failure rates (6,7) if women reported more than one method. We were considered not to be at risk of an unintended pregnancy if they were: 1) sterile or their partner was sterile; 2) pregnant or trying to conceive 3) had no heterosexual activity in the last 12 months 4) had just given birth or were breastfeeding The later criteria was based on women’s reasons for not using contraception, rather than an objective assessment of pregnancy risk, in the absence of data on the date of last birth and partial breastfeeding. Only 17 women fitted these criteria. We considered they were unlikely to be at risk as most women stop breastfeeding in the first month and all women are counseled about the risk of pregnancy during the postpartum period. Women who fitted the above criteria were considered in the category “not at risk” regardless of their use of contraception. Information on current contraceptive use was missing in 61 women (1.2%) in 2000, 163 women (1.8%) in 2005 and 12 women (0.2%) in 2010. The final sample included 4714 women ages 15–49 years in 2000, 8613 women in 2005 and 5260 women in 2010.
Analysis
We used descriptive statistics to compare women’s socio-demographic characteristics and examine contraceptive behaviors by survey year, for all women and across subgroups. We used multinomial logistic regression models (defining contraceptive behaviors in 5 categories: male or female sterilization/ long acting reversible contraception (LARC) (including IUD, implant)/ hormonal user dependent methods (pill, patch, vaginal ring, Depo-Provera)/ barrier or natural methods (withdrawal, fertility awareness, spermicides) / no contraception) to explore differences in contraceptive use among women in need of contraception by survey year, controlling for other factors. We tested for differences in the effects of age, socio-economic status and reproductive characteristics (parity and history of abortion) on differences in contraceptive behaviors from survey year to survey year and over the 3 time points. Because differences of effects only related to the use of LARC methods over time, we present the results of separate multivariate analysis by method type and report on different trends in long acting methods by women’s age and by parity. The use of sterilization almost exclusively pertained to women with children and over the age of 30 years (1 nulliparous woman over the age of 30 had tubal ligation).
In the second part of the analysis, we assessed the potential consequences of population shifts in contraceptive practices on unintended pregnancies rates based on French estimates of first year method-specific typical use failure rates provided in the literature (6). Around 85% of women would be expected to become pregnant within a year if they were not using contraception and seeking to become pregnant (8). However, a significant proportion of women with an unmet need is not trying to conceive and therefore may lower levels of exposure to pregnancy (due to age and sexual activity). This is made evident in the national epidemiological observatory of fertility study in France (the Obseff cohort), which estimated the first year probability of a pregnancy among non-contraceptive users at potential risk to be 71% (9). In that study, women were considered at risk if they had sexual intercourse in the last 3 months, while in our study population, women at risk were defined as having had sexual intercourse in the last 12 months. Therefore, we expect first year pregnancy rates among women with an unmet need in our population to be lower than in the Obseff study. We set this probability at 60%. We performed a sensitivity analysis to assess the robustness of our conclusions on overall differences in expected unintended pregnancy rates by considering different probabilities of pregnancy among among women with an unmet need (set at 45%, 60% or 85%) and by using the US contraceptive typical use failure rates that are substantially higher than the French failure rates (7).
All analyses are weighted to account for the complex survey designs of each survey. Women were assigned a sampling weight inversely proportional to the probability of being selected in the sample. Post-stratification adjustments (age, marital status, professional activity, level of education) were also applied to reflect the characteristics of women in the general population based on census data. These adjustments account for sampling distortion due to non-response. Analyses were performed using Stata software version11SE to account for the complex sampling design.
RESULTS
Women’s socio-demographic and reproductive characteristics by year are presented in Table 1. Mean age of respondents was 32.7 years [32.4–33.0] in 2000, 32.8 years [32.6–33.1] in 2005, and 32.6 years [32.2–32.9] in 2010. Women were less likely to be married and to be living with children in 2010. Women’s level of education and professional situation also evolved over time (p<0.001), with an increasing proportion of students between 2000 and 2005, and a slight increase in women with higher education (p<0.001). The proportion of obese women increased from 5% to 7% between 2005 and 2010 (p<0.001) as well as the proportion of current smokers which rose from 33% to 36% (p=0.001) after an initial decline from 40% in 2000 to 33% in 2005 (p=0.001). Women were equally sexually experienced and sexually active in the last 12 months across the 3 time points. The proportion of women reporting a history of abortion was greater in the 2000 and 2005 Health Barometer surveys than in the FECOND study of 2010 (p=0.001), likely due to differences in survey instruments.
Table 1.
Women’s sociodemographic and sexual and reproductive characteristics by year
| 2000 | 2005 | 2010 | ||
|---|---|---|---|---|
| N=4714 | N=8613 | N=5260 | ||
| Age | 15–19 | 13% | 13% | 15% |
| 20–24 | 12% | 12% | 11% | |
| 25–29 | 14% | 13% | 14% | |
| 30–34 | 16% | 17% | 14% | |
| 35–39 | 16% | 15% | 15% | |
| 40–44 | 15% | 16% | 16% | |
| 45–49 | 15% | 15% | 15% | |
| Cohabitating with partner | yes | 64% | 64% | 61% |
| Marital status | single | 44% | 47% | 53% |
| Married or in civil union | 49% | 46% | 40% | |
| divorced/widowed | 7% | 7% | 7% | |
| children | 62% | 61% | 56% | |
| Abortion history | 19% | 17% | 13% | |
| level of education | <high school | 50% | 43% | 46% |
| high school | 20% | 21% | 22% | |
| > high school | 29% | 35% | 33% | |
| professional situation | Works/ on leave from work | 60% | 58% | 64% |
| student | 19% | 20% | 19% | |
| unemployment | 8% | 10% | 9% | |
| other | 13% | 12% | 8% | |
| sexually experienced | 91% | 90% | 90% | |
| has had sexual intercourse in the last 12 months | 85% | 84% | 84% | |
| Number of partners in the last year | no partner | 16% | 16% | |
| 1 partner | 78% | 73% | ||
| 2 partners | 4% | 7% | ||
| >2 partners | 2% | 3% | ||
| STI in the past 10/5 y | 4% | 3% | 3% | |
| Current smoker | 40% | 33% | 36% | |
| Obese | BMI=>30 | 5% | 5% | 7% |
A third of women were not using any form of contraception at the time of the surveys. However, less than 3% (2.4% in 2000, 3.2% in 2005 and 2.4% in 2010, p=0.002) had an unmet need for contraception (Table 2). Among contraceptive users, 59% of women in 2000 and 2005 relied on user-dependent hormonal methods (in almost all cases the pill), with this proportion declining to 52% in 2010 (p<0.0001). The decline in user-dependent hormonal methods was only partially compensated by an increase in LARC methods, which rose from 22% of method mix in 2000 to 25% in 2005 and 24% in 2010 (p=0.04). There was also a significant increase in the use of permanent contraception (tubal ligation) from 1% in 2000 to 2% in 2005 and 4% in 2010 (p<0.001). After a drop of 4 percentage points in the first five years of the decade (from 18% to 14% in 2005), the use of barrier and natural methods (condoms, withdrawal, fertility based methods or spermicides) rose by 6% percentage points in the last five years, representing 20% of contraceptive users in 2010. Among these women, the proportion relying on condoms decreased from 81% in 2005 to 64% in 2010, while those using withdrawal and fertility awareness methods increased. Differences in overall contraceptive behaviors were significant in all comparisons (2000 vs 2005, 2005 vs 2010 and 2000 vs 2010).
Table 2.
Contraceptive practices and estimated unintended pregnancies in the last 10 years in France
| First year contraceptive failure rates |
% Contraceptive use | Expected number of unintended pregnancies |
|||||
|---|---|---|---|---|---|---|---|
| 2000 | 2005 | 2010 | 2000 | 2005 | 2010 | ||
| not at risk* | 0 | 32.1% | 29.9% | 30.5% | 0 | 0 | 0 |
| Sterilization | 0.5% | 0.7% | 1.3% | 2.4% | 520 | 950 | 1700 |
| Implant | 0.5% | 0.0% | 0.8% | 1.8% | 0 | 544 | 1306 |
| Intra Uterine Device | 1% | 14.7% | 16.2% | 14.3% | 21210 | 23505 | 20477 |
| Patch/ring | 2.4% | 0.0% | 0.1% | 1.0% | 0 | 452 | 3478 |
| Pill | 2.4% | 38.3% | 39.1% | 34.1% | 132948 | 136211 | 117474 |
| Condom | 3.5% | 8.2% | 7.6% | 8.7% | 41669 | 38723 | 43545 |
| Other Barrier/natural methods (withdrawal, fertility awareness, spermicides) | 10% | 3.5% | 1.8% | 4.8% | 50858 | 25376 | 69309 |
| No contraception (unmet need) | 60% | 2.4% | 3.2% | 2.4% | 208923 | 280149 | 210082 |
| Estimated total annual number of unintended pregnancies | 456128 | 505910 | 467372 | ||||
| Estimated annual number of unintended pregnancies/100 women 15–49 years** | 3.16 | 3.49 | 3.26 | ||||
women were not at risk of an unintended pregnancy if they were sterile or their partner was sterile; if they were pregnant or trying to conceive, if they had just given birth or were breastfeeding or if they had no heterosexual activity in the last 12 months
Estimated annual unintended pregnancies rates are calculated among all women 15–49 years, regardless of their risk of pregnancy.
Results from the multinomial logistic regression models confirm the significant changes in contraceptive behaviors among women in need of contraception across the 3 survey years as well as from year to year (Table 3). We found no significant differences in contraceptive behavior changes overall from survey year to survey year or over the 3 time points according to women’s socio-demographic and reproductive history (all test of interactions p>0.05). However, these trends were significantly different by age and by parity specifically in the case of LARC use, with a greater increase in use among younger and nulliparous women after controlling for other factors. The odds of LARC use were 4 times as high in 2010 as in 2000 (OR=4.1 [2.0–8.5]) among nulliparous women but only 25% higher (OR=1.25 [1.1–1.4]) among women with children during the same period. Likewise, the odds of LARC use increased significantly more between 2000 and 2010 among women less than 25 years (OR=3.9 [1.6–10.0]) than among older women (OR=1.3 [1.1–1.6]).
Table 3.
Odds of method use by survey year among women at potential risk of an unintended pregnancy*: results from multinomial logistic regression model and method specific logistic regression
| 2005 vs 2000 | 2010 vs 2000 | 2010 vs 2005 | |
|---|---|---|---|
| Adjusted OR 95% CI |
Adjusted OR 95% CI |
Adjusted OR 95% CI |
|
| Multinomial regression model | |||
| No contraception (unmet need) | 1 | 1 | 1 |
| Natural and Barrier methods | 0.6* [0.4–0.8] | 1.1 [0.8–1.6] | 2.0* [1.5–2.6] |
| User dependent Hormonal methods | 0.7* [0.6–1.0] | 0.9 [0.6–1.2] | 1.2 [0.9–1.5] |
| Long acting reversible methods | 0.9 [0.6–1.1] | 1.2 [0.9–1.7] | 1.4* [1.1–1.8] |
| Sterilization | 1.4 [0.8–2.5] | 3.9* [2.2–6.9] | 2.8* [1.9–4.1] |
| Separate Logistic regression models | |||
| No contraception (unmet need) versus other | 1.3* [1.0–1.7] | 1.0 [0.7–1.3] | 0.7* [0.6–0.9] |
| Natural and barrier methods versus other | 0.7* [0.6–0.8] | 1.2* [1.0–1.3] | 1.6* [1.4–1.8] |
| User dependent Hormonal methods versus other | 1.0 [0.9–1.1] | 0.7* [0.6–0.8] | 0.7* [0.6–0.8] |
| Long acting reversible methods versus other | 1.2* [1.1–1.4] | 1.3* [1.1–1.5] | 1.0 [0.9–1.1] |
| Sterilization versus other | 2.0* [1.3–3.2] | 4.0* [2.5–6.5] | 2.1* [1.5–2.8] |
women were not at risk of an unintended pregnancy if they were sterile or their partner was sterile; if they were pregnant or trying to conceive, if they had just given birth or were breastfeeding or if they had no heterosexual activity in the last 12 months
Results are adjusted for age, parity, cohabitation status, level of education, professional situation, abortion history, smoking status, and obesity
p<0.05
Based on the distribution of contraceptive behaviors from 2000 to 2010 among all women, we estimated trends in number of unintended pregnancies by applying first year method-specific failure rates in France to the number of women using each form of contraception by year of survey (Table 2). Trends in annual unintended pregnancy rates rose from 3.16% to 3.49% between 2000 and 2005, declining to 3.26% in 2010. When excluding cell phone users from the 2010 sample (cell phone users were not included in the 2000 and 2005 surveys), results also showed a decline in unintended pregnancy rates in 2010 (3.14% unintended pregnancy rate among landline users). In all 3 years, the minority of women with an unmet need for contraception contributed for the largest proportion of estimated unintended pregnancies: 46% in 2000; 55% in 2005 and 45% in 2010. Hormonal methods contributed more than a quarter of estimated unintended pregnancies in 2000 (29%), with a slight decline over time (27% in 2005 and 26% in 2010). Conversely, after a 7% point reduction in the proportion of unintended pregnancies resulting from barrier or natural method failures between 2000 and 2005 (from 20% to 13%), the contribution of barrier and natural method failures to estimated unintended pregnancy rates rose by 11% points in the last 5 years to 24% in 2010.
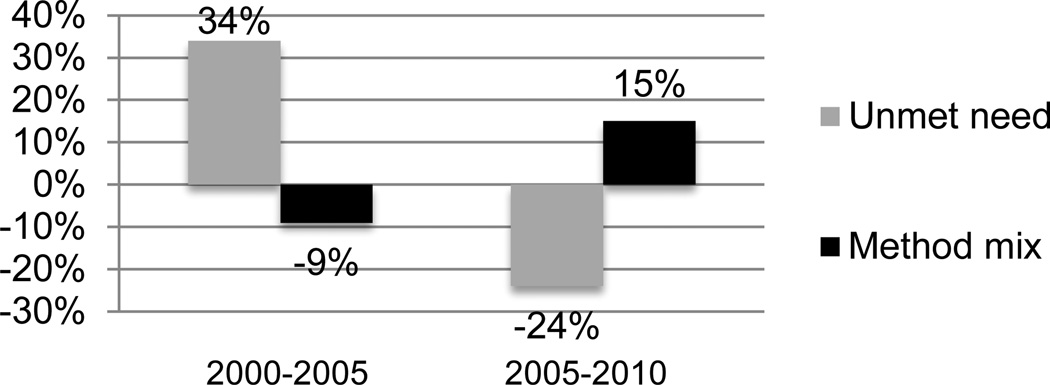
Altogether, the small changes in unmet need for contraception exerted the largest effects on unintended pregnancy rates while changes in method mix had smaller yet opposite effects in both time periods (Figure 1).
Figure 1.
Contribution of changes in unmet need for contraception and changes in method mix to overall changes in annual unintended pregnancy rates between 2000 and 2010
Because the French failure rates are underestimated (6) (due to underreporting of 50% of abortions in the 2000 national survey from which typical use failure rates were derived (10)), we examined the robustness of our conclusions using US typical use failure rates, which correct for underreporting of US abortions (also found to be 50% in US surveys (11)) (Table 4). The US failure rates however are an overestimation of typical use failure rates in France. First uncorrected failure rates in the US are substantially higher than uncorrected failure rates in France. In addition, using the US failure rates, the number of estimated pregnancies resulting from failures would equal the total number of pregnancies (intended and unintended) reported in France (based on birth and abortion registries). Results show that overall trends in unintended pregnancy rates would be similar when substituting the French with the US failure rates (Table 4). Because the largest effect on unintended pregnancy rates was due to unmet need for contraception rather than method mix, we examined the robustness of our conclusions when considering different pregnancy rates among women with an unmet need (set at 45%, 60% or 85%). Again, our conclusions remained unchanged when using French typical use failure rates. In fact, failure rates among women with an unmet need would need to have been as low as 30% to reverse our conclusions on the decline in unintended pregnancy rates between 2005 and 2010 and as low as 15% to change our conclusions on the increase in unintended pregnancy rates between 2000 and 2005. The same exercise using US typical use failure rates shows failure rates among women with an unmet need would need to have been as low as 50% to reverse our conclusions on the decline in unintended pregnancy rates between 2005 and 2010 and as low as 42% to change our conclusions regarding the increase in unintended pregnancy rates between 2000 and 2005.
Table 4.
Sensitivity Analysis of estimated a nnual unintended pregnancy rates
| Expected annual number of unintended pregnancies/ 100 women 15–49 |
Expected changes in unintended pregnancies /100 women 15–49 |
|||||
|---|---|---|---|---|---|---|
| French failure rates | 2000 | 2005 | 2010 | 2000 to 2005 | 2005 to 2010 | |
| 60% first year pregnancy rate among non-users | 3.16 | 3.49 | 3.26 | 0.33 | −0.23 | |
| 85% first year pregnancy rate among non-users | 3.76 | 4.29 | 3.87 | 0.53 | −0.42 | |
| 45% first year pregnancy rate among non-users | 2.80 | 3.01 | 2.89 | 0.20 | −0.12 | |
| US failure rates | ||||||
| 60% first year pregnancy rate among non-users | 7.03 | 7.18 | 7.10 | 0.15 | −0.08 | |
| 85% first year pregnancy rate among non-users | 7.63 | 7.99 | 7.71 | 0.36 | −0.28 | |
| 45% first year pregnancy rate among non-users | 6.67 | 6.70 | 6.74 | 0.03 | 0.04 | |
DISCUSSION
This study indicates that changes in contraceptive behaviors in the last 10 years, contribute to significant fluctuations in unintended pregnancy rates, which seemed to have peaked in 2005. We believe these findings are significant in several ways.
First, our results highlight the relative importance of overall contraceptive coverage versus method mix in changes in unintended pregnancy rates. Marginal changes in the small proportion of women with an unmet need for contraception contribute the most to changes in unintended pregnancy rates. Since most non-users have used contraception in the past, these results draw attention to the role of contraceptive gaps that are frequent, yet under studied and poorly acknowledged in clinical practice.
While contraceptive gaps carry the greatest impact, changes in method mix also prove effective, as evidenced by the decline in unintended pregnancy rates due to an increase in use of more effective methods between 2000 and 2005. With only 6% of LARC users among women under the age of 30 years (12) and 3% among nulliparous women in need of contraception in 2010 (13), there is room for improvement in contraceptive care, especially as a growing proportion of women seemed to have switched from hormonal to less effective methods in the last 5 years. Results from the CHOICE project in Saint Louis, which resulted in 67% women (including nulliparous and teenagers) choosing LARC methods over other options when starting a new method (14), should inspire healthcare professionals in France to expand eligibility criteria for LARC methods and provide all women with evidenced based information so they can make informed choices. Likewise, since the 2001 law allowing the use of sterilization for contraceptive purposes in France, there has been small, yet significant increases in the use of tubal sterilization. However, barriers to use permanent methods, rarely offered by healthcare professionals due to misperceptions about the methods and lack of professional training, are still prevalent in France.
Beyond implications for family planning programs in France, this study also provides a rationale for using data on contraceptive behaviors as a proxy to monitor trends in unintended pregnancy rates, when data on pregnancy intentions are lacking and abortion data are incomplete. Indeed our estimates of trends in unintended pregnancy rates mirror National abortion rates, both peaking in 2005–2006. The concordance of these indicators adds some external validity to our study, although we acknowledge that abortion rates not only reflect contraceptive effectiveness but also attitudes towards pregnancy termination (4). However, changes in social norms are likely to be limited over short periods of time. Thus, replication of this study could prove valuable in monitoring trends in unintended pregnancy rates in many European countries, which have no reliable data on unintended pregnancies and abortions (15). Likewise, our simple algorithm could be used to compare estimates of unintended pregnancy rates across (European) countries, although the assumed consistency in typical use failure rates over time is less likely to be true across populations (as evidenced by the differences in contraceptive failure rates between France and the US (6,7)). Further investigation of differences in contraceptive patterns of use and typical use failure rates are needed to validate such a cross-national comparison.
Our study also reveals the velocity of changes in contraceptive behaviors, prompting a reflection on research strategies, such as continuous data collection, to better monitor national and international reproductive health behaviors and outcomes. Such a transition from repeated to continuous data collection was implemented in 2006 in the United States (16), allowing for a better understanding of the impact of evolving socio-economic circumstances on reproductive health indicators, while at the same time improving cost/effectiveness and quality of data collection (17). The implementation of such a monitoring system in the European region would allow a better assessment of local and regional trends in reproductive health and the impact of family planning policies or media coverage such as the recurrent episodes of pill scares (currently ongoing in France) on women’s contraceptive practices and associated health outcomes.
This study has several limitations that will now be discussed. The comparison of the 3 surveys shows a number of socio-demographic differences, mostly due to a greater proportion of adolescents in the 2010 survey (who were slightly over-represented in the 2010 sample). We adjusted all multivariate analysis on the socio-demographic characteristics of women to account for these differences across surveys. In addition, unlike the 2000 and 2005 Health Barometer surveys, the 2010 FECOND study included a subsample of cell phone users with no landlines, which represent a growing proportion of the population. Our conclusions, however, were unchanged when excluding the cell phone users from the analysis. Also, while we acknowledge a potential effect of differential selection bias, the concordance of our trend estimates with the national trends in abortion rates, adds some external validity to our results (18). During the same period, birth rates declined from 5.42 per 100 women aged 15 to 49 years in 2000 to 5.39 per 100 women 15–49 years in 2005 and increased to 5.63 per 100 women 15–49 years in 2010 (national statistics INSEE). The national birth certificate does not provide information on pregnancy intentions rendering the estimate of unintended births from these data impossible. In this study, we used French first year failure rates, which are underestimated due to the underreporting of abortion (6). However, our conclusions are unchanged when using US failure rates, which are over-estimated in the French context. In addition, when using first year failure rates, we overestimate failures because typical use failure rates decline over time (the probability of failure is reduced as duration of use increases (6)). In light of these limitations, our results do not represent a true estimation of annual unintended pregnancy rates but rather indices of unintended pregnancies allowing for trend analyses of unintended pregnancy rates (as the same biases apply to all annual estimates). Future models should consider a more dynamic approach using agent based modeling (19), to integrate failure rates and switching patterns over time, as well as patterns of contraceptive behaviors by women’s characteristics to provide a better estimate of the absolute number of unintended pregnancies. The absence of population-based estimates of pregnancy rates among women with an unmet need for contraception may also affect the validity of our results. While our study shows the importance of this parameter on overall pregnancy rates, our sensitivity analysis also indicates pregnancy rates among non-users would need to be quite low to overturn our conclusions. Therefore, we believe the imprecision in pregnancy rates among women with an unmet need is likely to affect the magnitude but not the direction of changes in unintended pregnancy rates over time. Finally, in this study, we assume that typical failure rates are constant from year to year, which has been shown to be the case in the US context (7). Further investigation is warranted to confirm this assumption in France.
Despite these limitations, we believe this study contributes to our current understanding of trends in unintended pregnancy rates in relation to changing patterns of contraceptive behaviors over time. It also offers a framework towards improving monitoring systems to provide better estimates of national trends in unintended pregnancies even when data on abortion and unintended pregnancies are not available. Results, based on this simple model show that even in the context of high contraceptive coverage, gaps of use undermine efforts to improve contraceptive effectiveness, as small fluctuations in unmet need for contraception contribute significantly to trends in unintended pregnancy rates.
IMPLICATIONS.
This study offers a framework towards assessing trends in unintended pregnancies, when data on abortions and unintended births are not available. In the context of high contraceptive coverage, gaps of use undermine efforts to improve contraceptive effectiveness, as small fluctuations in unmet need contribute significantly to trends in unintended pregnancy rates.
ACKNOWELDGEMENT
We thank all women who participated in the 3 French National surveys.
Study funding:
The FECOND study was supported by a grant from the French Ministry of Health, a grant from the French National Agency of Research (#ANR-08-BLAN-0286-01), and funding from National Institute of Health and Medical Research (INSERM) and the National Institute for Demographic Research (INED).
This work was supported, in part, by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant for Infrastructure for Population Research at Princeton University (Grant No. R24HD047879) (J. Trussell)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflict of interest.
REFERENCES
- 1.Bajos N, Leridon H, Goulard H, Oustry P, Job-Spira N, COCON Group Contraception: from accessibility to efficiency. Hum Reprod. 2003 May;18(5):994–999. doi: 10.1093/humrep/deg215. [DOI] [PubMed] [Google Scholar]
- 2.Moreau C, Lydie N, Warzwaski J, Bajos N. Activité sexuelle, infections sexuellement transmissibles, contraception. In: INPES, editor. baromètre Santé 2005. 2008. [Google Scholar]
- 3.Vilain A. Les interruptions volontaires de grossesses en 2010. [accessed, Feb 20th, 2013];Etudes et résultats. 2012 804 http://www.drees.sante.gouv.fr/IMG/pdf/er804.pdf. [Google Scholar]
- 4.Bajos N, Guillaume A, Kontula O. Reproducitve Health behaviour of young Europeans. Population studies, n°42, Council of Europe Publishing. 2003 [Google Scholar]
- 5.Guibert P, Baudier F, Gautier A, Goubert AC, Arwidson P, Janvrin MP. Baromètre Santé. Méthode. Vanves INPES. 2001 [Google Scholar]
- 6.Moreau C, Trussell J, Rodriguez G, Bajos N, Bouyer J. Contraceptive failure rates in France: results from a population-based survey. Hum Reprod. 2007;22(9):2422–2427. doi: 10.1093/humrep/dem184. [DOI] [PubMed] [Google Scholar]
- 7.Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77:10–21. doi: 10.1016/j.contraception.2007.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trussell J. Contraceptive failure in the United States. Contraception. 2004;70:89–96. doi: 10.1016/j.contraception.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 9.Slama R, Hansen OK, Ducot B, Bohet A, Sorensen D, Giorgis Allemand L, Eijkemans MJ, Rosetta L, Thalabard JC, Keiding N, Bouyer J. Estimation of the frequency of involuntary infertility on a nation-wide basis. Hum Reprod. 2012;27:1489–1498. doi: 10.1093/humrep/des070. [DOI] [PubMed] [Google Scholar]
- 10.Moreau C, Bajos N, Bouyer J. Question comprehension and recall: the reporting of induced abortions in quantitative surveys on the general population. Population. 2004;(3–4):439–454. [Google Scholar]
- 11.Jones RK, Kost K. Underreporting of induced and spontaneous abortion in the United States: an analysis of the 2002 National Survey of Family Growth. Stud Fam Plann. 2007;38:187–197. doi: 10.1111/j.1728-4465.2007.00130.x. [DOI] [PubMed] [Google Scholar]
- 12.Moreau C, Bohet A, Hassoun D, Teboul M, Bajos N the FECOND working group. Trends and determinants of use of long acting reversible contraception utilization among young women in France; results from 3 national surveys conducted between 2000 and 2010. Fertility and Sterility. 2013;100:451–458. doi: 10.1016/j.fertnstert.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Bajos N, Bohet A, Le Guen M, Moreau C. Contraception in France en 2010: new context, new practices ? Population and Societies. 2012;492 http://www.ined.fr/fichier/t_publication/1606/publi_pdf2_492.pdf. [Google Scholar]
- 14.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203:115.e1–115.e7. doi: 10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gissler M, Fronteira I, Jahn A, Karro H, Moreau C, Oliveira da Silva M, Olsen J, Savona-Ventura C, Temmerman M, Hemminki E REPROSTAT group. Terminations of pregnancy in the European Union. BJOG. 2012;119:324–332. doi: 10.1111/j.1471-0528.2011.03189.x. [DOI] [PubMed] [Google Scholar]
- 16.Groves RM, Mosher WD, Lepkowski JM, Kirgis NG. Planning and development of the continuous National Survey of Family Growth. Vital Health Stat 1. 2009;48:1–64. [PubMed] [Google Scholar]
- 17.Lepkowski JM, Mosher WD, Davis KE, Groves RM, Van Hoewyk J. The 2006–2010 National Survey of Family Growth: sample design and analysis of a continuous survey. Vital Health Stat 2. 2010;150:1–36. [PubMed] [Google Scholar]
- 18.Rossier C, Toulemon L, Prioux F. Abortion Trends in France, 1990–2005. Population-E – English edition. 2009;64(3):495–530. [Google Scholar]
- 19.Bonabeau E. Agent-based modeling: Methods and techniques for simulating human systems. Proceedings of the National Academy of Science of the United States of America. 2002;99(Suppl 3):7280–7287. doi: 10.1073/pnas.082080899. [DOI] [PMC free article] [PubMed] [Google Scholar]