Abstract
Purpose
Alcohol use disorders, substance use disorders, and antisocial personality disorder share a common externalizing liability, which may also include attention-deficit hyperactivity disorder (ADHD). However, few studies have compared formal quantitative models of externalizing liability, with the aim of delineating the categorical and/or continuous nature of this liability in the community. This study compares categorical, continuous, and hybrid models of externalizing liability.
Method
Data were derived from the 2004–2005 National Epidemiologic Survey on Alcohol and Related Conditions (N = 34,653). Seven disorders were modeled: childhood ADHD and lifetime diagnoses of antisocial personality disorder (ASPD), nicotine dependence, alcohol dependence, marijuana dependence, cocaine dependence, and other substance dependence.
Results
The continuous latent trait model provided the best fit to the data. Measurement invariance analyses supported the fit of the model across genders, with females displaying a significantly lower probability of experiencing externalizing disorders. Cocaine dependence, marijuana dependence, other substance dependence, alcohol dependence, ASPD, nicotine dependence, and ADHD provided the greatest information, respectively, about the underlying externalizing continuum.
Conclusions
Liability to externalizing disorders is continuous and dimensional in severity. The findings have important implications for the organizational structure of externalizing psychopathology in psychiatric nomenclatures.
Keywords: Externalizing, Comorbidity, ADHD, Classification, DSM-5
Introduction
Common mental disorders co-occur more often than expected by chance [1, 2] and some disorders exhibit greater comorbidity among themselves than with other disorders, such as antisocial behavior disorders, alcohol use disorders, and drug use disorders [3]. Krueger and colleagues [4, 5] suggest that patterns of co-occurrence among these disorders indicate a coherent underlying externalizing spectrum. The externalizing spectrum conceptualization has been robustly supported [6–8] and its phenotypic coherence is undergirded by genetic correlations among its constituent disorders [9]. Recent commentators in the literature have suggested that the externalizing spectrum may also include a broader range of psychopathology than has been shown to date [10]. This may include attention-deficit hyperactivity disorder (ADHD), which shares common etiological influences, including similar genetic factors [11] and neural underpinnings [12], with other externalizing disorders and an elevated risk of experiencing nicotine dependence, alcohol, and other substance use disorders [13, 14]. A small number of studies have formally tested the fit of ADHD in the externalizing spectrum [15–20]. However, these studies were largely based on a priori assumptions about underlying latent structure; i.e., they assumed an underlying latent trait [15–18] or a combination of latent traits and latent classes [19]. This is a significant limitation in the literature. To adequately characterize the structure of externalizing syndromes it is necessary to compare the relative fit of continuous (i.e., latent trait), categorical (i.e., latent class), and hybrid (i.e., factor mixture) models. Only one study has compared alternative latent variable models of externalizing liability including ADHD [20]. The present study adds to the scant international literature incorporating ADHD into the externalizing spectrum and directly compares alternative quantitative models of externalizing liability. We also examined gender invariance using nationally representative data from the largest psychiatric epidemiologic survey conducted to date in the US. Evidence of invariance suggests that any observed gender differences in prevalence rates arise from differences in means on latent externalizing liability.
Method
Sample
Data were drawn from the 2004–2005 Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a follow-up of the Wave 1 NESARC which was conducted in 2001–2002. In brief, the NESARC Wave 1 was a nationally representative, face-to-face survey of the civilian, non-institutionalized US population aged 18 years and over. Interviews were conducted with 43,093 respondents, with oversampling of African-Americans, Hispanics, and young adults aged 18–24 years. The response rate was 81 %.
In NESARC Wave 2, efforts were made to conduct interviews with all respondents in Wave 1. Interviews were completed with 34,653 individuals. The NESARC Wave 2 data were carefully weighted to reflect design characteristics, adjustments for non-response, and attrition between Wave 1 and Wave 2. In particular, adjustment for non-response across sociodemographic characteristics and the presence of any lifetime Wave 1 substance use disorder or psychiatric disorder was performed at the household and person levels to ensure that the sample approximates the target population. This took into account the original sample minus attrition between the two waves due to death, institutionalization or incapacitation, as well as deportation or permanent departure from the US, and being in the military for the full length of the Wave 2 interviewing period. The cumulative response rate of Wave 2 as a national sample was 70.2 %, incorporating non-response in both Waves 1 and 2.
Comparison of Wave 2 respondents with the target population that comprised Wave 2 respondents plus eligible non-respondents in terms of baseline (Wave 1) sociodemographic and diagnostic measures indicated no significant differences between Wave 2 respondents and the target population with respect to age, race-ethnicity, sex, socioeconomic status, or the presence of any lifetime substance use, mood, anxiety, or personality disorder (each examined separately). Subsequently, the weighted Wave 2 data were adjusted to be representative of the US population on socioeconomic variables including region, age, race-ethnicity and sex, based on the 2000 Decennial Census [21]. In summary, attrition and/or non-response is likely to have minimal impact on the current findings with regard to externalizing diagnosis prevalence or latent structure.
The research protocol, including informed consent procedures, received full ethical review and approval from the US Census Bureau and the US Office of Management and Budget. Further details regarding the survey methodology [22] and Wave II demographic characteristics are reported elsewhere [7]. The mean age of respondents was 49.06 years.
Assessment
The NIAAA’s Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV) was used to generate diagnoses. This is a structured interview designed for use by non-clinician interviewers. The reliability of AUDADIS diagnoses has been extensively documented elsewhere [22–25]. Seven disorders were included in the present analyses: ADHD, antisocial personality disorder, nicotine dependence, alcohol dependence, marijuana dependence, cocaine dependence, and other substance dependence. Other substance dependence included heroin, amphetamines, sedatives, tranquilizers, opioids, hallucinogens, inhalants or solvents, or other substances not specified a priori. Respondents were considered to meet criteria for other substance dependence if they met full dependence criteria for at least one of these substances.
Analyses were conducted on lifetime diagnoses, comprising lifetime diagnostic assessments from Wave 1 and ‘since last interview’ diagnostic assessments from Wave 2. In other words, if a respondent met lifetime diagnostic criteria for a given disorder at Wave 1 or in the interval between Waves 1 and 2, they were considered to have a lifetime diagnosis at Wave 2. Exceptions included ADHD, which was assessed only at Wave 2. An extensive list of questions queried ADHD symptom onset before age 18 and subsequent course across the lifespan. We examined cases of ADHD with childhood onset.
The weighted lifetime prevalence estimates of the disorders were as follows: ADHD = 2.5 % (S.E. 0.06), antisocial personality disorder = 3.8 % (SE 0.07), nicotine dependence = 23.1 % (SE 0.14), alcohol dependence = 15.2 % (SE 0.15), marijuana dependence = 1.7 % (SE 0.03), cocaine dependence = 1.2 % (SE 0.04), and other substance dependence = 1.5 % (SE 0.05).
Statistical analyses
Analyses were conducted in Mplus version 6 using maximum likelihood estimation with robust standard errors (MLR). To accommodate the complex design features of the NESARC, all analyses were conducted using the Wave 2 stratification, clustering, and sampling weight variables. Model fit was evaluated using the Bayesian Information Criterion (BIC) [26], Akaike Information Criterion (AIC) [27], and the sample size adjusted BIC (SSABIC) [28]. These information-based criteria aim to strike a compromise between model fit and parsimony by imposing a penalty on overparameterized models or small sample sizes. Smaller values suggest better model fit.
Greater emphasis was placed herein on the BIC, which is a reliable index and has been used as a sole index of model fit in similar structural analyses of this kind [6, 8, 29–31]. Moreover, contrary to what is sometimes assumed in the literature, the BIC does not assume that the true model is among those being compared: as sample size increases, it will tend to choose the model that is closest to the true model (in a relative entropy sense) [32–34]. Finally, BIC has also been shown to perform well in choosing between different latent variable models of the sort examined in this paper [35]. A difference of more than 10 in BIC values between two models indicates support for the model with the lower BIC value [36]. For completeness, the number of free parameters and log likelihood values associated with each model are presented, though these criteria cannot be used solely to test differences in model fit. The smaller the number of freely estimated parameters, the less complex and more parsimonious the model.
Latent trait models
Latent trait models account for patterns of co-occurrence among disorders with reference to an underlying dimension(s) (i.e., individuals are arrayed along a continuum ranging from very low pathology, mild, moderate, and severe pathology). According to this continuous perspective, diagnostic comorbidity is accounted for by population variation in the latent trait.
Response functions and information functions are useful for graphically depicting the latent trait model. Response functions are s-shaped curves representing the probability of disorder as a function of underlying liability. Similarly, information functions express the relative amount of statistical information each disorder provides about underlying liability. Generally, the maximum height of a given response or information function is relative to the slope parameter for the disorder. A steeper slope indicates a stronger relationship between underlying liability and the observed disorder, and suggests that the disorder provides greater information about liability. The location of a response or information function reflects the severity of a disorder, and shifts from left to right along the x-axis as the disorder increases in severity.
Latent class models
In latent class models, patterns of comorbidity are explained by a finite number of mutually exclusive classes. We fitted a series of latent class models ranging from two to seven classes (given that there were seven observed disorders, it was not possible to fit latent class models having more than seven classes). If a latent class model provided the best fit to the data it would suggest that there are distinct groups of individuals differing in liability for externalizing syndromes. Groups may differ qualitatively (i.e., differences in patterns of liability based on those externalizing disorders endorsed) or quantitatively (i.e., differences in the extent of externalizing liability). This categorical approach assumes that there is no diagnostic covariance amongst individuals in the same latent class.
Factor mixture models
We also estimated models that reflect a conceptual midpoint between categorical and continuous models. These hybrid models are considered categorical insofar as they group individuals into categories and considered dimensional because once individuals have been assigned to liability classes, differences in severity between classes are modeled through the use of continuous latent variables. These hybrid models facilitate meaningful distinctions between homogeneous groups whilst also allowing for different levels of severity within a given class.
Following guidelines in the literature [37], we estimated factor mixture models in which the factor means were the only parameters allowed to vary across classes. Item thresholds and factor loadings were held invariant across the latent classes, and the factor covariance matrix was fixed to zero. Similar to latent class models, we fitted a series of factor mixture models, ranging from two to seven latent values. Class membership is based on each individual’s location on the factor (i.e., arrayed along a dimension), as represented by the varying factor means. If one of these models provided the best fit to the data it would suggest that groups of individuals in the population differ according to the amount (or severity) of the disorders they experience.
Invariance analyses
In addition to analyses comparing the relative fit of categorical, dimensional and hybrid models, we conducted invariance analyses to determine whether parameter estimates of the best-fitting model were similar across males and females. Models in which parameter estimates were constrained to be equal across gender were compared with models in which parameter estimates were allowed to vary across gender.
Results
Evaluation of model fit in the entire NESARC sample
In the full sample, we tested latent trait, latent class, and factor mixture models. We regard to the latent trait models, the number of latent dimensions specified was guided by the extant literature [5, 6] and examined using exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). The EFA specified up to two latent dimensions. The statistical fit indices indicated minimal difference in model fit between the one-factor EFA model (AIC = 93,497.118; BIC = 93,615.462; SSABIC = 93,570.970) and the two-factor model EFA model (AIC = 93,442.352; BIC = 93,611.415; SSABIC = 93,547.855). The difference in BIC values was less than 10 indicating support for the one-factor model. In the two-factor model, high factor correlations (r = 0.80) were observed indicating multi-collinearity and casting doubt on the discriminant validity of two factors [38].
In summary, the high factor correlation and minimal improvement in fit based on the BIC suggested that the one-factor model provided a more parsimonious fit to the data. Accordingly, a one-factor model was selected and specified in a CFA framework (AIC = 93,499.783; BIC = 93,618.127; SSABIC = 93,573.635).
Overall, the continuous latent trait provided the best fit to the data (see Table 1). This model had the lowest BIC value (BIC = 93,618.127), suggesting that it provided the optimal account of comorbidity patterns among the seven externalizing disorders. These findings were robust even when nicotine dependence, cocaine dependence, marijuana dependence, alcohol dependence, and other drug dependence were combined into a composite substance use dependence syndrome (for further details please contact the corresponding author). Thereafter, the 3-, 4-, 5-, and 6-value factor mixture models exhibited superior fit compared to the majority of the latent class models. Among the latent class models, the 3-class model provided the best fit to the data. This general pattern of results was consistent across males and females (see Table 1). In particular, among females the best-fitting model was the latent trait model, followed by the 3-, 4-, and 5-value factor mixture models, followed by the 3-class model. Among males, the latent trait model provided the best fit to the data, followed by the 3-, 4-, 5-, 6-, and 7-value factor mixture models, followed by the 3-class model.
Table 1.
Fit indices for latent class, latent trait, and factor mixture models of externalizing liability in the 2004–2005 National Epidemiologic Survey on Alcohol and Related Conditions
| Model | k | LL | BIC | AIC | SSABIC |
|---|---|---|---|---|---|
| Entire sample (n = 34,653) | |||||
| Latent class models | |||||
| 2 classes | 15 | −47,019.464 | 94,195.726 | 94,068.929 | 94,148.056 |
| 3 classes | 23 | −46,732.210 | 93,704.843 | 93,510.421 | 93,631.749 |
| 4 classes | 31 | −46,703.143 | 93,730.333 | 93,468.286 | 93,631.815 |
| 5 classes | 39 | −46,679.846 | 93,767.365 | 93,437.693 | 93,643.424 |
| 6 classes | 47 | −46,667.835 | 93,826.967 | 93,429.669 | 93,677.601 |
| 7 classes | 55 | −46,662.786 | 93,900.495 | 93,435.573 | 93,725.706 |
| Latent trait model | 14 | −46,735.891 | 93,618.127 | 93,499.783 | 93,573.635 |
| Factor mixture models | |||||
| 2 values | 16 | −47,019.464 | 94,206.179 | 94,070.929 | 94,155.331 |
| 3 values | 17 | −46,736.789 | 93,651.282 | 93,507.578 | 93,597.256 |
| 4 values | 19 | −46,723.873 | 93,646.355 | 93,485.745 | 93,585.973 |
| 5 values | 21 | −46,723.916 | 93,667.348 | 93,489.832 | 93,600.610 |
| 6 values | 23 | −46,723.873 | 93,688.167 | 93,493.745 | 93,615.074 |
| 7 values | 25 | −46,723.889 | 93,709.106 | 93,497.778 | 93,629.657 |
| Females (n = 20,089) | |||||
| Latent class models | |||||
| 2 classes | 15 | −22,146.548 | 44,441.716 | 44,323.097 | 44,394.047 |
| 3 classes | 23 | −22,008.251 | 44,244.385 | 44,062.503 | 44,171.292 |
| 4 classes | 31 | −21,990.597 | 44,288.340 | 44,043.194 | 44,189.823 |
| 5 classes | 39 | −21,979.948 | 44,346.306 | 44,037.897 | 44,222.366 |
| 6 classes | 47 | −21,971.395 | 44,408.462 | 44,036.790 | 44,259.098 |
| 7 classes | 55 | −21,965.394 | 44,475.724 | 44,040.788 | 44,300.936 |
| Latent trait model | 14 | −22,022.086 | 44,182.883 | 44,072.172 | 44,138.931 |
| Factor mixture models | |||||
| 2 values | 16 | −22,146.548 | 44,451.624 | 44,325.097 | 44,400.776 |
| 3 values | 17 | −22,013.607 | 44,195.648 | 44,061.213 | 44,141.623 |
| 4 values | 19 | −22,011.636 | 44,211.523 | 44,061.272 | 44,151.142 |
| 5 values | 21 | −22,011.655 | 44,231.376 | 44,065.310 | 44,164.639 |
| 6 values | 23 | −22,011.672 | 44,251.227 | 44,069.344 | 44,178.134 |
| 7 values | 25 | −22,011.627 | 44,270.952 | 44,073.254 | 44,191.503 |
| Males (n = 14,564) | |||||
| Latent class models | |||||
| 2 classes | 15 | −23,284.280 | 46,712.354 | 46,598.559 | 46,664.685 |
| 3 classes | 23 | −23,140.588 | 46,501.661 | 46,327.176 | 46,428.569 |
| 4 classes | 31 | −23,121.160 | 46,539.495 | 46,304.319 | 46,440.979 |
| 5 classes | 39 | −23,102.310 | 46,578.486 | 46,282.619 | 46,454.547 |
| 6 classes | 47 | −23,090.158 | 46,630.872 | 46,274.316 | 46,481.510 |
| 7 classes | 55 | −23,086.152 | 46,699.552 | 46,282.305 | 46,524.766 |
| Latent trait model | 14 | −23,134.157 | 46,402.522 | 46,296.313 | 46,358.031 |
| Factor mixture models | |||||
| 2 values | 16 | −23,284.280 | 46,721.940 | 46,600.559 | 46,671.094 |
| 3 values | 17 | −23,143.396 | 46,449.760 | 46,320.793 | 46,395. 735 |
| 4 values | 19 | −23,128.782 | 46,439.705 | 46,295.565 | 46,379.324 |
| 5 values | 21 | −23,128.782 | 46,458.877 | 46,299.565 | 46,392.141 |
| 6 values | 23 | −23,128.785 | 46,478.054 | 46,303.569 | 46,404.962 |
| 7 values | 25 | −23,128.788 | 46,497.234 | 46,307.577 | 46,417.786 |
Criterion. Bold type indicates the best-fitting model
k number of estimated parameters, LL Log likelihood, BIC Bayesian information, AIC Akaike information criterion, SSABIC sample size adjusted BIC
Evaluation of model fit by gender
Multiple-group CFA tested whether the latent trait model was equivalent across genders (see Table 2).
Table 2.
Measurement invariance tests of the externalizing spectrum across gender: summary of fit indices
| Model | Test | CFI | TLI | RMSEA | Δχ2 |
|---|---|---|---|---|---|
| Model 1 (unconstrained model) | 0.997 | 0.995 | 0.008 | – | |
| Model 2 (constrained model) | 2–1 | 0.994 | 0.992 | 0.010 | 27.791** |
CFI comparative fit index, TLI Tucker–Lewis index, RMSEA root mean square error of approximation
p < 0.0001
Following recommendations in the literature [39], we fitted a model in which thresholds and factor loadings were freed across both genders; scale factors were fixed at one in both genders; and factor means were fixed at zero in both genders (unconstrained model; Model 1). This was compared to a second model in which thresholds and factor loadings were held equal across genders; scale factors were fixed at one in men and freed in women; factor means were fixed at zero in men and freed to vary in women (constrained model; Model 2). Model 2 represents the gender invariant model. Model fit was evaluated using the root mean square error of approximation (RMSEA) [40], the Comparative fit index (CFI) [41], and the Tucker–Lewis index (TLI) [42]. Recommendations in the literature suggest that RMSEA values less than 0.05 indicate close model fit; values up to 0.08 suggest a reasonable error of approximation in the population, and values exceeding 0.10 indicate poor fit [43]. CFI and the TLI values ≥0.90 indicate acceptable fit and values ≥0.95 imply very good fit [44].
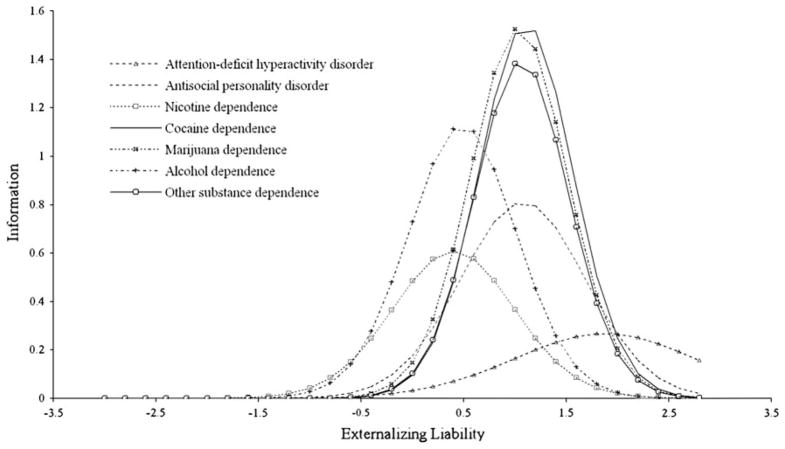
The CFI (0.994), TLI (0.992), and RMSEA (0.010) values associated with the constrained model (Model 2) demonstrated excellent fit and nearly identical fit to the unconstrained model (Model 1), suggesting that the latent trait model was invariant between males and females. The difference in CFI values did not exceed 0.01 [45], indicating that invariance is supported and lending further support for the constrained model. Comparison of latent mean differences indicated that, compared to males, females had a significantly lower probability of experiencing externalizing disorders (−0.574, i.e., roughly half of a standard deviation lower, p < 0.001). The constrained model is presented in Fig. 1.
Fig. 1.
The constrained latent trait model in women and men (Model 2). Values presented on the structural paths from externalizing to the disorders are standardized factor loadings; values presented in boxes are thresholds (all significant p < 0.001). Values before the slash and in bold relate to women; values after the slash relate to men. ASPD antisocial personality disorder, Nic nicotine dependence, Alc alcohol dependence, Marij marijuana dependence, Coc cocaine dependence, Sub other substance dependence, ADHD attention-deficit hyperactiv-ity disorder. Arrows without numbers indicate unique variances, including error
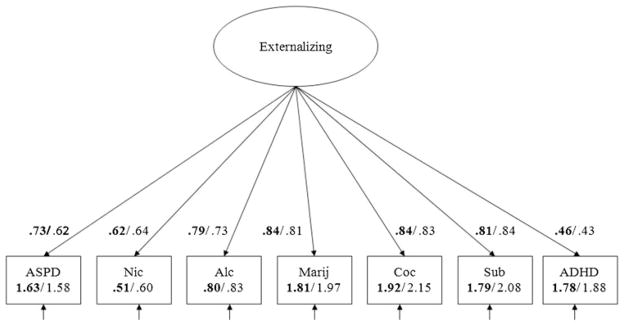
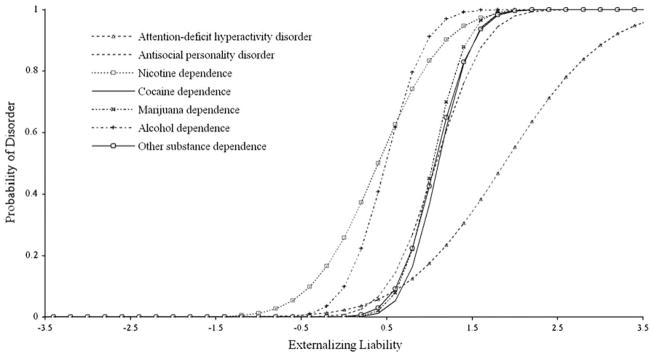
Parameter estimates under the invariant latent trait model (Model 2) provide important details about the relative information and severity of the seven disorders arrayed along the externalizing continuum. The response and information functions are presented in Figs. 2 and 3, respectively. In general, cocaine dependence, marijuana dependence, and other substance dependence provided the greatest information about the underlying externalizing continuum relative to the other disorders; ADHD provided the least information. The response functions for ADHD and cocaine dependence were placed on the extreme end of the liability continuum, suggesting that across males and females these disorders tapped the more severe end of the externalizing continuum, compared to alcohol dependence and nicotine dependence.
Fig. 2.
Response functions of externalizing disorders under a latent trait liability model (Model 2: constrained model)
Fig. 3.
Information functions of externalizing disorders under a latent trait liability model (Model 2: constrained model)
Across genders, the response and information functions for alcohol dependence and nicotine dependence were located at the negative end of the liability continuum, suggesting that these disorders provided information about less severe forms of externalizing pathology (see Figs. 2 and 3). Across males and females, the response and information functions for ADHD and cocaine dependence were placed on the extreme end of the liability continuum, suggesting that these disorders provided more information about more severe forms of externalizing pathology.
Discussion
Externalizing structure
This study compared the relative fit of continuous, categorical, and hybrid models of externalizing liability, including ADHD. In the entire sample, as well as males and females separately, the continuous latent trait model provided the best fit to the data. In the entire sample as well as the gender-stratified groups, the next best-fitting models were the factor mixture models, providing further evidence that continuous conceptualizations of externalizing liability provide superior fit over categorical conceptualizations of liability, as represented by latent class models. Measurement invariance analyses highlighted that the latent trait model was invariant across genders, with females displaying a significantly lower probability of experiencing externalizing disorders compared to males.
This study extends earlier work by Markon and Krueger [6] who modeled the externalizing spectrum using comorbidity data on six DSM-IV syndromes (past-year and lifetime diagnoses) from Wave I of the NESARC. This paper extended this work in two important ways: firstly, this paper expanded the empirically based externalizing spectrum by including ADHD, which was not assessed at Wave 1, but was assessed at Wave 2 of the NESARC. Using this follow-up wave, we modeled the same six externalizing disorders as Markon and Krueger [6] in addition to ADHD; secondly, Markon and Krueger [6] limited analyses to only testing categorical and continuous models. Clarifying the exact nature of externalizing liability has important clinical, theoretical, and practical implications. Accordingly, we extended previous structural analyses of the externalizing spectrum (including ADHD) by modeling categorical, continuous, and hybrid models of liability. To our knowledge, this is only the second study of this kind to do so.
The present study is congruent with previous findings by Markon and Krueger [6] and Krueger [46] suggesting that externalizing liability is best conceptualized as a continuum rather than a set of discrete risk groups. The seven disorders were arrayed along a continuum of graded severity, with nicotine dependence and alcohol dependence less severe than ADHD and cocaine dependence. Marijuana dependence, cocaine dependence, and other substance dependence provided the greatest information regarding externalizing liability. Only one previous study examined alternative categorical, continuous, and hybrid latent variable conceptualizations of externalizing liability, including ADHD. The authors [20] found that a continuous, two-factor model provided the best fit to the data. Divergence between these findings and the current study may relate to the inclusion of different externalizing syndromes. Witkiewitz et al. [20] did not include nicotine or cocaine dependence, hallmarks of externalizing liability [6], and we did not include conduct disorder and oppositional defiant disorder in the present analyses. Due to practical constraints involved in conducting a national survey, the NESARC could not include all DSM-IV disorders; oppositional defiant disorder was one such disorder that was omitted. We excluded conduct disorder because it was assessed at Wave 1 only. We limited the disorders analyzed to only those assessed at Wave 2 to avoid any potential bias due to the wave at which the disorder was assessed. However, as an exploratory step (and in response to a reviewer’s request), we re-ran the latent trait models to incorporate Wave I conduct disorder. The findings indicated minimal improvement in fit based on the BIC, providing convergent support for a one-factor model. Finally, a further noteworthy difference between the study by Witkiewitz et al. [20] and the present analyses relates to the examination of gender differences in this paper.
Implications
By drawing on data from a large-scale epidemiological survey and by investigating a wider panoply of competing measurement models than hitherto, this paper informs the literature on the empirical structure of externalizing psychopathology. These findings should ultimately inform the organizational structure of future editions of the DSM and other nomenclatures. Indeed, acknowledging the utility of the internalizing–externalizing framework in explaining “much of the systematic comorbidities seen in both clinical and community samples” [3], the recently released DSM-5 places internalizing disorders adjacent to one another and externalizing disorders next to one another. This new organizational structure marks efforts to develop a more valid foundation for classifying mental disorders [47] and to provide a bridge to new diagnostic approaches [3].
It should be noted that though ADHD loaded significantly on the externalizing factor in the present study, relatively speaking it was the weakest indicator of the seven syndromes examined. This suggests that ADHD may crossload onto another liability. As part of the DSM-5 revision process, ADHD has been speculated to load onto neurodevelopmental liability [48]. Future structural research should investigate whether ADHD loads onto other latent factors in addition to externalizing liability.
This paper found evidence for a continuous model of externalizing liability. Continuous models resolve inherent problems with the extant psychiatric classification system, such as extensive comorbidity and within-category heterogeneity, and offer flexibility to identify cut-off points to facilitate research and clinical decision-making [49]. From a research perspective, representing disorders as quantitative scores increases reliability, yields greater statistical power, and provides more comprehensive clinical information [50]. From a clinical perspective, some authors have found that dimensional models predict better clinical course, treatment needs, social and occupational functioning than their categorical counterparts [51–53]. In addition, a dimensional perspective provides a meaningful framework for informing our understanding of the specificity of biomarkers, putative endophenotypes, and genetic factors linked to liability.
The identification of a unitary continuum underlying externalizing liability, however, does not preclude the identification of thresholds [47]. Even if externalizing liability varies continuously in the general population, beyond a particular level, externalizing behaviors become problematic for the individual and/or those around them. It is unlikely that a uniform diagnostic threshold exists; as Widiger and Mullins-Sweatt [54] point out, a continuous model offers the flexibility to identify different thresholds to suit different social and clinical decisions. Indeed, a similar situation is evident in clinical medicine where, for instance, blood pressure is continuous yet a threshold signaling hypertension (i.e., systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg) is used to aid clinical decision-making [55]. Future research could be directed towards identifying meaningful thresholds of externalizing liability according to external validators, such as measures of social and occupational impairment, and functional disability. These cut-offs could then be used to ensure individual treatments match the level of externalizing liability.
Although we did not find evidence that a hybrid model provided the best fit to the data, this paper adds to the sparse literature comparing the fit of hybrid models to traditional categorical and continuous models of psychopathology. Hybrid models capitalize on the merits of continuous and categorical approaches. Clinically speaking, this model supports the interpretation that a subgroup in the population has an elevated risk for experiencing externalizing syndromes and that, within this subgroup, symptoms are graded in severity.
Limitations
The present findings should be tempered by a number of caveats. First, structured interviews were conducted by non-clinicians who were unable to access independent sources of information or probe respondents for further information. Moreover, information was gathered through retrospective self-report. These survey design features, though common in psychiatric epidemiology and indeed clinical evaluation, have particular relevance for the assessment of childhood ADHD. Respondents were asked an extensive list of items enquiring about ADHD symptom onset before age 18; however, because significant others from childhood/adolescence and objective measures like report cards were not available to corroborate reports, the only source of information about symptoms and behaviors was the respondent. Recall bias therefore cannot be ruled out. Empirical research on the validity of retrospectively reported ADHD is mixed [56]. Relatedly, whilst it would be preferable to include a diagnosis of ADHD capturing childhood and adult symptom manifestations, the NESARC data set only comprises a childhood diagnosis which necessarily limits the focus of the present study. Nevertheless, ADHD functioned as a reliable indicator of overall externalizing level in the present study and demonstrated reliability in psychometric tests of the AUDADIS [22].
Second, analyses were based on lifetime diagnoses (with the exception of childhood ADHD). Analyses of past-year diagnoses herein were precluded due to low prevalence estimates of some disorders (e.g., cocaine dependence and other substance dependence). Third, the study was limited to data collected at a single point in time. Longitudinal data facilitates insights about stability and changes in externalizing symptomatology and behaviors over time, and has demonstrated utility in refining our understanding of liability to other forms of psychopathology [57]. In the context of a population genetic framework, longitudinal data holds promise of informing our understanding of whether the externalizing liability continuum is activated early in the developmental process to set in motion a chain reaction of disorders, or is present relatively constant throughout development as a predisposition towards externalizing disorders. Although the NESARC is a longitudinal design, since ADHD was only assessed at Wave 2 it was not possible to conduct longitudinal analyses to ascertain which of these accounts of the externalizing spectrum is most accurate.
Closing remarks
In closing, this study highlighted that liability to externalizing spectrum disorders is continuous in nature and dimensional in severity. Moreover, this study adds to a small body of research demonstrating that externalizing liability encompasses childhood ADHD. Congruent with longitudinal and genetic findings highlighted earlier, this observation suggests a degree of developmental continuity such that a childhood diagnosis of ADHD predicts the later development of other externalizing disorders in adulthood. Accurate identification, intervention, and treatment of childhood ADHD are therefore crucial.
Acknowledgments
This work was funded by NIH grants U01AA018111 and K05AA014223 and the New York State Psychiatric Institute (Dr. Hasin).
Footnotes
Conflict of interest None declared.
Contributor Information
Natacha Carragher, Email: n.carragher@unsw.edu.au, National Drug and Alcohol Research Centre, University of New South Wales, Sydney, NSW 2052, Australia.
Robert F. Krueger, Department of Psychology, University of Minnesota, 75 East River Road, Minneapolis, MN 55455-0344, USA
Nicholas R. Eaton, Department of Psychology, Stony Brook University, Stony Brook, NY 11794-2500, USA
Kristian E. Markon, Department of Psychology, University of Iowa, Iowa City, IA 52242, USA
Katherine M. Keyes, Department of Epidemiology, Mailman School of Public Health, Columbia University, 1051 Riverside Drive 123, New York, NY 10032, USA
Carlos Blanco, New York State Psychiatric Institute, Columbia University College of Physicians and Surgeons, 1051 Riverside Drive, Unit 69, New York, NY 10032, USA.
Tulshi D. Saha, Laboratory of Epidemiology and Biometry, Division of Intramural Clinical and Biological Research, National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health, 5635 Fishers Lane, Bethesda, USA
Deborah S. Hasin, Department of Psychiatry, College of Physicians and Surgeons, Columbia University, 1051 Riverside Drive No. 123, New York, NY 10032, USA
References
- 1.Beesdo-Baum K, Höfler M, Gloster AT, Klotsche J, Lieb R, Beauducel A, et al. The structure of common mental disorders: a replication study in a community sample of adolescents and young adults. Int J Methods Psychiatr Res. 2009;18:204–220. doi: 10.1002/mpr.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychol Med. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. American Psychiatric Association; Washington, DC: 2013. (DSM-5) [Google Scholar]
- 4.Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: an integrative quantitative model of the adult externalizing spectrum. J Abnorm Psychol. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krueger RF, Markon KE, Patrick CJ, Iacono WG. Externalizing psychopathology in adulthood: a dimensional-spectrum conceptualization and its implications for DSM-V. J Abnorm Psychol. 2005;114:537–550. doi: 10.1037/0021-843X.114.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Markon K, Krueger RF. Categorical and continuous models of liability to externalizing disorders: A direct comparison in NESARC. Arch Gen Psychiatry. 2005;62:1352–1359. doi: 10.1001/archpsyc.62.12.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, Hasin DS. Borderline personality disorder co-morbidity: relationship to the internalizing-externalizing structure of common mental disorders. Psychol Med. 2011;41:1041–1050. doi: 10.1017/S0033291710001662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eaton NR, Krueger RF, Markon KE, Keyes KM, Skodol AE, Wall M, Hasin DS, Grant BF. The structure and predictive validity of the internalizing disorders. J Abnorm Psychol. 2013;122:86–92. doi: 10.1037/a0029598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 10.Hasin D, Kilcoyne B. Comorbidity of psychiatric and substance use disorders in the United States: current issues and findings from the NESARC. Curr Opin Psychiatry. 2012;25:165–171. doi: 10.1097/YCO.0b013e3283523dcc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arcos-Burgos M, Vélez JI, Solomon BD, Muenke M. A common genetic network underlies substance use disorders and disruptive or externalizing disorders. Human Genet. 2012;131:917–929. doi: 10.1007/s00439-012-1164-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frodl T. Comorbidity of ADHD and substance use disorder (SUD): a neuroimaging perspective. J Atten Disord. 2010;14:109–120. doi: 10.1177/1087054710365054. [DOI] [PubMed] [Google Scholar]
- 13.Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin Psychol Rev. 2011;31:328–341. doi: 10.1016/j.cpr.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charach A, Yeung E, Climans T, Lillie E. Childhood attention-deficit/hyperactivity disorder and future substance use disorders: comparative meta-analyses. J Am Acad Child Adolesc Psychiatry. 2011;50:9–21. doi: 10.1016/j.jaac.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 15.Cosgrove VE, Rhee SH, Gelhorn HL, Boeldt D, Corley RC, Ehringer MA, et al. Structure and etiology of co-occurring internalizing and externalizing disorders in adolescents. J Abnorm Child Psychol. 2011;39:109–123. doi: 10.1007/s10802-010-9444-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Farmer RF, Seeley JR, Kosty DB, Lewinsohn PM. Refinements in the hierarchical structure of externalizing psychiatric disorders: patterns of lifetime liability from mid-adolescence through early adulthood. J Abnorm Psychol. 2009;118:699–710. doi: 10.1037/a0017205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forbush KT, Watson D. The structure of common and uncommon mental disorders. Psychol Med. 2013;43:97–108. doi: 10.1017/S0033291712001092. [DOI] [PubMed] [Google Scholar]
- 18.Lahey BB, Rathouz PJ, Van Hulle C, Urbano RC, Krueger RF, Applegate B, et al. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. J Abnorm Child Psychol. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- 19.Almansa J, Vermunt JK, Forero CG, Vilagut G, De Graaf R, De Girolamo G, et al. Measurement and description of underlying dimensions of comorbid mental disorders using factor mixture models: results of the ESEMeD project. Int J Methods Psychiatr Res. 2011;20:116–133. doi: 10.1002/mpr.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Witkiewitz K, King K, McMahon RJ, Wu J, Luk J, Bierman KL, et al. Evidence for a multidimensional latent structural model of externalizing disorders. J Abnorm Child Psychol. 2013;41:233–237. doi: 10.1007/s10802-012-9674-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stinson FS, Dawson DA, Goldstein RB, Chou SP, Huang B, Smith SM, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV narcissistic personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69:1033–1045. doi: 10.4088/jcp.v69n0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, et al. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Canino G, Bravo M, Ramírez R, Febo VE, Rubio-Stipec M, Fernández RL, et al. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. J Stud Alcohol. 1999;60:790–799. doi: 10.15288/jsa.1999.60.790. [DOI] [PubMed] [Google Scholar]
- 24.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 25.Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend. 1997;44:133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- 26.Schwartz G. Estimating the dimension of a model. Ann Stat. 1978;6:461–464. [Google Scholar]
- 27.Akaike H. A new look at the statistical model identification. IEEE Trans Autom Control. 1974;19:716–723. [Google Scholar]
- 28.Sclove SL. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- 29.Conway C, Hammen C, Brennan P. A comparison of latent class, latent trait, and factor mixture models of DSM-IV borderline personality disorder criteria in a community setting: implications for DSM-5. J Pers Disord. 2012;26:793–803. doi: 10.1521/pedi.2012.26.5.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walton KE, Ormel J, Krueger RF. The dimensional nature of externalizing behaviors in adolescence: evidence from a direct comparison of categorical, dimensional, and hybrid models. J Abnorm Child Psychol. 2011;39:553–561. doi: 10.1007/s10802-010-9478-y. [DOI] [PubMed] [Google Scholar]
- 31.Wright AG, Krueger RF, Hobbs MJ, Markon KE, Eaton NR, Slade T. The structure of psychopathology: toward an expanded quantitative empirical model. J Abnorm Psychol. 2013;122:281–294. doi: 10.1037/a0030133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barron AR, Cover TM. Minimum complexity density estimation. IEEE Trans Inf Theory. 1991;37:1034–1054. [Google Scholar]
- 33.Grunwald PD. The minimum description length principle. MIT Press; Cambridge: 2007. [Google Scholar]
- 34.Rissanen J. Information and complexity in statistical modelling. Springer; New York: 2007. [Google Scholar]
- 35.Markon KE, Krueger RF. Information-theoretic latent distribution modelling: distinguishing between discrete and continuous latent variable models. Psychol Methods. 2006;11:228–243. doi: 10.1037/1082-989X.11.3.228. [DOI] [PubMed] [Google Scholar]
- 36.Raftery AE. Bayesian model selection in social research. Sociol Methodol. 1995;25:111–163. [Google Scholar]
- 37.Clark SL, Muthén BO, Kaprio J, D’Onofrio BM, Viken R, Rose RJ, et al. Models and strategies for factor mixture analysis: two examples concerning the structure of underlying psychological disorders. 2009 doi: 10.1080/10705511.2013.824786. http://www.statmodel.com/download/FMA%20Paper_v142.pdf. [DOI] [PMC free article] [PubMed]
- 38.Kline RB. Principles and practice of structural equation modeling. Guilford Press; New York: 1998. [Google Scholar]
- 39.Millsap RE, Yun-Tein J. Assessing factorial invariance in ordered-categorical measures. Multivar Behav Res. 2004;39:479–515. [Google Scholar]
- 40.Steiger JH. Structural model evaluation and modification: an internal estimation approach. Multivar Behav Res. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- 41.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 42.Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- 43.Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociol Method Res. 1993;21:230–258. [Google Scholar]
- 44.Hu L, Bentler PM. Fit indices in covariance structure modeling: sensitivity to under parameterized model misspecification. Psychol Methods. 1998;3:424–453. [Google Scholar]
- 45.Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model. 2002;9:233–255. [Google Scholar]
- 46.Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 47.Regier DA, Kuhl EA, Kupfer DJ. The DSM-5: classification and criteria changes. World Psychiatry. 2013;12:92–98. doi: 10.1002/wps.20050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Andrews G, Pine DS, Hobbs MJ, Anderson TM, Sunderland M. Neurodevelopmental disorders: cluster 2 of the proposed meta-structure for DSM-V and ICD-11. Psychol Med. 2009;39:2013–2023. doi: 10.1017/S0033291709990274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Widiger TA. The DSM-III-R categorical personality disorder diagnoses: a critique and an alternative. Psychol Inq. 1993;4:75–90. [Google Scholar]
- 50.Helzer JE, Bucholz KK, Gossop M. A dimensional option for the diagnosis of substance dependence in DSM-V. Int J Methods Psychiatr Res. 2007;16:S24–S33. doi: 10.1002/mpr.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Peralta V, Cuesta MJ, Giraldo C, Cardenas A, Gonzalez F. Classifying psychotic disorders: issues regarding categorical vs. dimensional approaches and time frame to assess symptoms. Eur Arch Psychiatry Clin Neurosci. 2002;252:12–18. doi: 10.1007/s004060200002. [DOI] [PubMed] [Google Scholar]
- 52.Rosenman S, Korten A, Medway J, Evans M. Dimensional vs. categorical diagnosis in psychosis. Acta Psychiatr Scand. 2003;107:378–384. doi: 10.1034/j.1600-0447.2003.00059.x. [DOI] [PubMed] [Google Scholar]
- 53.van Os J, Gilvarry C, Bale R, Van Horn E, Tattan T, White I, et al. A comparison of the utility of dimensional and categorical representations of psychosis. Psychol Med. 1999;29:595–606. doi: 10.1017/s0033291798008162. [DOI] [PubMed] [Google Scholar]
- 54.Widiger TA, Mullins-Sweatt SN. Clinical utility of a dimensional model of personality disorder. Prof Psychol Res Pr. 2010;41:488–494. [Google Scholar]
- 55.Kessler RC. The categorical versus dimensional assessment controversy in the sociology of mental illness. J Health Soc Behav. 2002;43:171–188. [PubMed] [Google Scholar]
- 56.Miller CJ, Newcorn JH, Halperin JM. Fading memories: retrospective recall inaccuracies in ADHD. J Atten Disord. 2010;14:7–14. doi: 10.1177/1087054709347189. [DOI] [PubMed] [Google Scholar]
- 57.Mesman J, Koot HM. Early preschool predictors of pre-adolescent internalizing and externalizing DSM-IV diagnoses. J Am Acad Child Adolesc Psychiatry. 2001;40:1029–1036. doi: 10.1097/00004583-200109000-00011. [DOI] [PubMed] [Google Scholar]