Abstract
Purpose
This study was performed to evaluate the position of impacted mandibular third molars in different skeletal facial types among a group of Iranian patients.
Materials and Methods
A total of 400 mandibular third molars in 200 subjects with different types of facial growth were radiographically investigated for their positions according to their types of facial growth on the basis of the β angle. The subjects were divided into three groups (class I, II, and III) according to ANB angle, representing the anteroposterior relationship of the maxilla to the mandible. Meanwhile, the subjects were also divided into three groups (long, normal, and short face) according to the angle between the stella-nasion and mandibular plane (SNGoGn angle). ANOVA was used for statistical analysis.
Results
The mean β angle showed no significant difference among class I, II, and III malocclusions (df=2, F=0.669, p=0.513). The same results were also found in short, normal, and long faces (df=1.842, F=2, p=0.160). The mesioangular position was the most frequent one in almost all of the facial growth patterns. Distoangular and horizontal positions of impaction were not found in the subjects with class III and normal faces. In the long facial growth pattern, the frequency of vertical and distoangular positions were not different.
Conclusion
In almost all of the skeletal facial types, the mesioangular impaction of the mandibular third molar was the most prevalent position, followed by the horizontal position. In addition, β angle showed no significant difference in different types of facial growth.
Keywords: Mandible; Molar, Third; Tooth, Impacted; Malocclusion
Introduction
The third molar (M3) varies more than the other molars in terms of shape, size, timing of eruption, and even tendency toward impaction. In modern societies, M3s get impacted far more than any other teeth, and impaction of mandibular M3 is more common than its maxillary counterpart.1 According to several studies, there is no sex predilection in the impaction of M3.1,2,3 However, Hugoson and Kugelberg showed a higher frequency in females than males.4
It has been noted that M3 crypt formation starts at the age of 3 to 4, and calcification begins at 7 to 10 years of age. However, the time of eruption varies from 14 to 24 years in different populations.1,5 Several factors are involved in impaction of mandibular M3. First, the shortage of space between the anterior border of the ascending ramus and the distal area of the mandibular second molar (M2) has been identified as a major factor in M3 impaction.1 Björk demonstrated reduction of the alveolar arch space behind the mandibular M2 in 90% of patients with M3 impaction.6 Second, a short mandibular length is thought to be another etiologic factor in M3 impaction.2 However, Kaplan did not find any significant difference in mandibular length between subjects with erupted and impacted molars.7 Third, the size of mandibular M3 has a possible role in this regard as well.1 Hattab and Alhaija showed that impacted M3s were larger in size than erupted ones.8
Finally, impaction of mandibular M3 has also been associated with the pattern of facial growth.9 In contrast, Legović et al showed no significant difference between the position of mandibular M3 and the type of facial growth.10 Due to these controversies, further studies should be done to clarify the factors associated with M3 impaction.
Therefore, the aim of this study was to evaluate the impacted mandibular M3 positions in different skeletal facial types. To best of our knowledge, this is the first study on the topic in a group of Iranian patients.
Materials and Methods
A list of patients referred to the Orthodontics Department of Hamadan Dental School, Iran in 2012 and 2013 was identified (1,650 cases: 921 women and 629 men). The inclusion criteria for this study were as follows: 1) adequate data records and complete history of surgical and orthodontic treatments, 2) panoramic radiographs showing complete dentition dating back to pre-orthodontic treatment, 3) lateral cephalometric image pertaining to pre-orthodontic treatment, 4) presence of mandibular M3s with at least two-thirds of root formation being complete, 5) no missing or extracted permanent teeth or any previous orthodontic procedures, 6) presence of bilateral impaction in both left and right sides of the mandible for comparison, and 7) no history of medical problems with a potential effect on facial growth. Patients with pathological conditions related to mandibular M2 and M3 such as extensive caries or cystic lesions were excluded.
In this study, 265 out of 1,650 cases had one or two impacted mandibular M3. However, only 200 cases (66 males and 134 females) met the inclusion criteria. The age of the patients included in this study ranged between 19 and 32 years, and the average age was 22.5±2.03.
The ANB angle representing the relative position of the maxilla and mandible anteroposteriorly, and the SNGoGn angle representing the angle between the stella-nasion and mandibular plane, were used to detect different skeletal facial types. The patients were divided into three subgroups on the basis of their ANB angle as follows: skeletal class I (ANB: 1-5 degrees), skeletal class II (ANB more than 5 degrees), and skeletal class III (ANB less than 1 degree).
At the same time, the patients were divided into three subgroups according to their SNGoGn angle as follows: short face (low angle: SNGoGn less than 27 degrees), normal (SNGoGn between 27 and 37 degrees), and long face (long angle: SNGoGn more than 37 degrees).11
The type of mandibular M3 impaction was determined according to Winter's classification by using β angle as follows: distoangular position (angle from -11 to -79 degrees), vertical position (angle from -10 to 10 degrees), mesioangular position (angle from 11 to 79 degrees), and horizontal position (angle from 80 to 100 degrees). The β angle was formed between the intersecting long axes of the M2 and M3 and drawn through the midpoint of the occlusal surface and midpoint of the root bifurcation.12 We did not consider the buccal/lingual obliquity (transverse) because we needed an occlusal radiograph to confirm this position.
Lateral cephalometric radiographs were taken for each patient in centric occlusion with the lips in repose and the Frankfort plane horizontal, according to the natural head position, using a Cranex D X-ray unit (Sordex, Helsinki, Finland) at 66 to 70 kVp, 10 mA, and 14.2 s exposure. Lateral cephalometric radiographs were used to allocate the subjects to their groups according to the ANB angle and SNGoGn angle to identify the type of facial growth. Panoramic radiographs were also taken for each patient with the upper and lower incisors in an edge-to-edge relationship using the Cranex D X-ray unit (Soredex, Helsinki, Finland) at 66 to 70 kVp, 10 mA, and 17.6 s.
All of the images were displayed on a 17-inch Samsung monitor (Syncmaster 740N, Seoul, Korea) with the screen resolution set at 1,280×1,024 pixels and color set to 32-bit depth. Finally, tracing was done using Scanora software (Soredex, Helsinki, Finland) by two investigators for measurement of the ANB, SNGoGn, and β angles. The reliability and degree of agreement between investigators were also determined by the mean of Cohen's kappa analysis so that intra- and inter-examiner reliability was above 0.70 and 0.88, respectively. The data were statistically analyzed by the analysis of variance (ANOVA) and t-test using SPSS software (ver. 15.0, SPSS Inc, Chicago, USA). A p value less than 0.05 was considered to indicate statistical significance.
Results
The incidence of mandibular M3 impaction was 16.06% (265 out of 1650 cases). The incidence of bilateral impaction of the mandibular M3 was 12.12% (200 out of 1650 cases).
The means of the β angle in class I, II, and III were 29.63±16.29, 30.15±17.69, and 33.27±12.17, respectively. Meanwhile, it was found to be 31.21±16.53, 30.69±14.66, and 27.57±16.53 in different skeletal facial types of short face, normal face, and long face, respectively. The mean of the β angle in females (30.66±17.24) and males (29.04±15.12) did not show a significant difference (p=0.657).
According to ANOVA, the mean of the β angle did not differ significantly among class I, II, and III patients (df=2, F=0.669, p=0.513). The same results were also found among the short, normal, and long face groups (df=1.842, F=2, p=0.160).
In addition, according to ANOVA, the mean of the β angle in both sides (the left and right sides of the mandible) was higher in class III than class I and II. However, the β angle showed no significant difference between the left and right sides in class I, II, and III (right side: F=0.239, df=2.197, p=0.788; left side: F=0.491, df=2.197, p=0.613) (Table 1). Although the β angle showed no significant difference between the left and right sides in the short, normal, and long faces (right side: F=0.128, df=2.197, p=0.880; left side: F=0.491, df=2.197, p=0.613), in short faces, the mean of the β angle in the right side was almost equal to the left side.
Table 1.
Distribution of β angle (mean±SD) in the right and left sides of the mandible according to different skeletal facial types
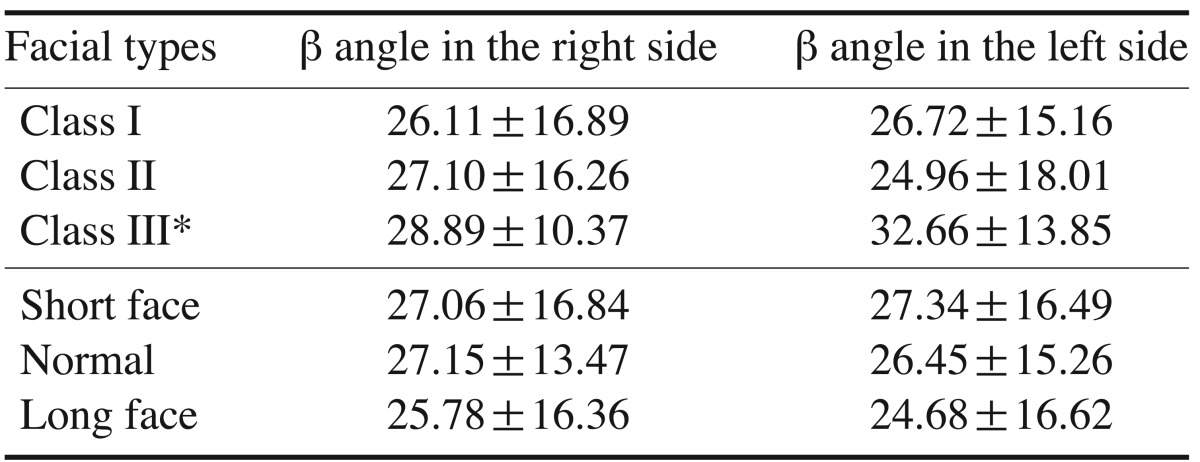
*: significantly different from Class I and II
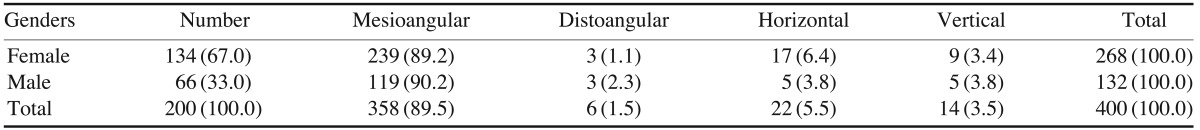
In both genders, mesioangular and distoangular positions were found to be the most and the least prevalent types of mandibular M3 impaction, respectively. In addition, the frequency of vertical and horizontal types of mandibular M3 impaction was equal in the men in our study (Table 2).
Table 2.
Distribution (number and percentage) of different positions of mandibular M3 impaction according to the genders
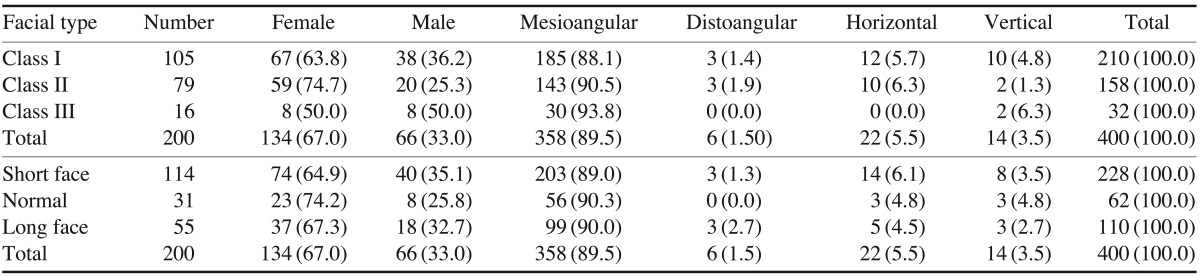
In all of facial growth patterns, the mesioangular position was found to be the most common type of mandibular M3 impaction (Table 3). In almost all facial growth patterns, except for class III, a horizontal position of the impacted mandibular M3 was the second most common one after the mesioangular position, followed by the vertical and distoangular positions (Table 3).
Table 3.
Distribution (Number and percentage) of different positions of mandibular M3 impaction according to different skeletal facial types
Discussion
The results of this study demonstrated an overall rate of mandibular M3 impaction of 16.06%. According to Andreasen et al, impaction of mandibular M3 varies from 18% to 32% in different populations.13 This rate was also estimated by Dachi and Howell as 17.5% and 21.9% for mandibular and maxillary M3s, respectively.14 In addition, in a recent study, Breik and Grubor showed a rate of 58.76% for mandibular M3 impaction in Melbourne, Australia.2
Vilela and Vitol reported that the most frequently impacted teeth are M3s (90%) with a higher prevalence in the mandible than the maxilla (60% vs. 30%), followed by the upper canine teeth (5%), lower bicuspids, and supernumerary teeth (5%).15
The mean age of our study sample was 22.5±3.02 years, which was similar to the study by Abu Alhaija et al (20.80±2.03 years).1
According to Vilela and Vitoi,15 the crown formation of M3s begins around 9 to 10 years of age, which might be seen in panoramic radiographs at 11 years of age in about 90% of cases. They more frequently erupt between 18 and 20 years of age.
In the present report, generally, a mesioangular position of the impacted mandibular M3 was the most prevalent position (89.5%), followed by horizontal, vertical, and distoangular positions. In accordance to our findings, Breik and Grubor showed that over 80% of the mandibular M3 impactions in all facial types were in the mesioangular position.2 Vilela and Vitoi15 found that the vertical position was most prevalent, followed by mesioangular position. In contrast, Quek et al,16 Sandhu and Kaur,17 and Venta et al18 noted the mesioangular position to be the most prevalent one.
According to our results, in both genders, the mesioangular position was the most common position, followed by the horizontal, vertical, and distoangular positions. However, the number of females with impacted mandibular M3s was higher than that of males. Many researchers such as Abu Alhaija et al,1 Breik and Grubor,2 Hattab et al,3 and Brown et al19 reported no sex predilection in mandibular M3 impaction. In contrast, Hugoson and Kugelberg4 and Murtomaa et al20 found a higher frequency in women than men.
Generally, the number of women was more than men in our study, possibly because women are more willing to receive orthodontic treatment for esthetic reasons. That is why the number of recorded impacted M3s in women was greater than men in our study.
In the subjects in class I group as well as those of the short face group, the mesioangular position was the most frequent position, followed by horizontal, vertical, and distoangular positions (mesioangular>horizontal>vertical>distoangular).
In the patients in class II occlusion, the mesioangular position had the highest prevalence, followed by horizontal, distoangular, and vertical positions (mesioangular>horizontal>distoangular>vertical).
In the subjects with class III occlusion, the mesioangular position was the most frequent position, followed by the vertical position. In this type of facial growth, we did not find distoangular and horizontal positions of impaction, perhaps due to small number of class III cases (16 cases).
In patients with a normal growth pattern of the face, the mesioangular position was the most prevalent position, and the frequency of horizontal and vertical positions were equal. Also, distoangular position was not found in this type of growth pattern (mesioangular>horizontal=vertical).
In the long facial growth pattern, the mesioangular position had the highest prevalence, followed by the horizontal position. In addition, the frequency of the vertical and distoangular positions were equal in this growth pattern.
According to Breik, mesioangular impaction of the mandibular M3 was most common in mesofacial subjects, followed by brachyfacials and dolichofacials. On the other hand, Breik showed that horizontal impaction was mostly common in dolichofacials followed by brachyfacials and mesofacials.2
In our study, there was no significant difference in the β angles of different types of skeletal facial growth. This finding was in agreement with the results of Abu Alhaija et al1 and Behbehani et al.21 Behbehani et al demonstrated that a higher mesial angulation of the M3 bud increased the risk of impaction.21 Furthermore, Uthman suggested that the β angle showed a marked increase in the marginal eruption group compared to the full eruption group.22 According to Farzanegan and Goya, the largest β angle was measured in the normal group, followed by deep bite and open bite groups.23
It was noted that an impacted mandibular M3 at the normal time of eruption might erupt later in life.2 Although rarely leading to clinical eruption, Richardson pointed out that between the age 18 and 21, many unerupted M3s changed their position appreciably.24 Hattab reported that by the age of 19, some impacted molars erupt into functional occlusion.25
According to Kruger et al,26 impacted M3s at age 19 could be fully erupted by age 26. Hesby et al27 observed that during the growth period, the mandibular inter-molar width increased by 2.05 mm, and the mandibular crossarch width at the level of the alveolar crest increased by 1.60 mm (left buccal surface to right buccal surface) and 1.02 mm (left lingual surface to right lingual surface). Furthermore, the basal bone of the mandible increased in width by 14.54.
In conclusion, in almost all skeletal facial types, the mesioangular position of the impacted mandibular M3 was the most prevalent position, followed by the horizontal position. Moreover, various types of facial growth did not show a significant difference in terms of the β angle.
References
- 1.Abu Alhaija ES, AlBhairan HM, AlKhateeb SN. Mandibular third molar space in different antero-posterior skeletal patterns. Eur J Orthod. 2011;33:570–576. doi: 10.1093/ejo/cjq125. [DOI] [PubMed] [Google Scholar]
- 2.Breik O, Grubor D. The incidence of mandibular third molar impactions in different skeletal face types. Aust Dent J. 2008;53:320–324. doi: 10.1111/j.1834-7819.2008.00073.x. [DOI] [PubMed] [Google Scholar]
- 3.Hattab FN, Rawashdeh MA, Fahmy MS. Impaction status of third molars in Jordanian students. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:24–29. doi: 10.1016/s1079-2104(05)80068-x. [DOI] [PubMed] [Google Scholar]
- 4.Hugoson A, Kugelberg CF. The prevalence of third molars in a Swedish population. An epidemiological study. Community Dent Health. 1988;5:121–138. [PubMed] [Google Scholar]
- 5.Mady Maricić B, Legović M, Slaj M, Lapter Varga M, Zuvić Butorac M, Kapović M. Presence of third molar germs in orthodontic patients with class II/2 and class III malocclusions. Coll Antropol. 2009;33:1171–1175. [PubMed] [Google Scholar]
- 6.Björk A, Jensen E, Palling M. Mandibular growth and third molar impaction. Acta Odontol Scand. 1956;14:231–272. [Google Scholar]
- 7.Kaplan RG. Some factors related to mandibular third molar impaction. Angle Orthod. 1975;45:153–158. doi: 10.1043/0003-3219(1975)045<0153:SFRTMT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Hattab FN, Alhaija ES. Radiographic evaluation of mandibular third molar eruption space. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:285–291. doi: 10.1016/s1079-2104(99)70029-6. [DOI] [PubMed] [Google Scholar]
- 9.Richardson ME. The etiology and prediction of mandibular third molar impaction. Angle Orthod. 1977;47:165–172. doi: 10.1043/0003-3219(1977)047<0165:TEAPOM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Legović M, Legović I, Brumini G, Vandura I, Cabov T, Ovesnik M, et al. Correlation between the pattern of facial growth and the position of the mandibular third molar. J Oral Maxillofac Surg. 2008;66:1218–1224. doi: 10.1016/j.joms.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 11.Tecco S, Caputi S, Tete S, Orsini G, Festa F. Electromyographic activity of masticatory, neck and trunk muscles of subjects with different mandibular divergence. A cross-sectional evaluation. Angle Orthod. 2007;77:260–265. doi: 10.2319/0003-3219(2007)077[0260:EAOMNA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Winter GB. Impacted mandibular third molars. St. Louis: American Medical Book; 1926. pp. 241–279. [Google Scholar]
- 13.Andreasen JO, Petersen JK, Laskin DM. Textbook and color atlas of tooth impactions: diagnosis, treatment, prevention. Copenhagen: Munksgaard; 1997. pp. 222–223. [Google Scholar]
- 14.Dachi SF, Howell FV. A survey of 3,874 routine full-mouth radiographs. I. A study of retained roots and teeth. Oral Surg Oral Med Oral Pathol. 1961;14:916–924. doi: 10.1016/0030-4220(61)90003-2. [DOI] [PubMed] [Google Scholar]
- 15.Vilela EM, Vitoi PA. Study of position and eruption of lower third molars in adolescents. South Braz Dent J. 2011;8:390–397. [Google Scholar]
- 16.Quek SL, Tay CK, Tay KH, Toh SL, Lim KC. Pattern of third molar impaction in a Singapore Chinese population: a retrospective radiographic survey. Int J Oral Maxillofac Surg. 2003;32:548–552. [PubMed] [Google Scholar]
- 17.Sandhu S, Kaur T. Radiographic evaluation of the status of third molars in the Asian-Indian students. J Oral Maxillofac Surg. 2005;63:640–645. doi: 10.1016/j.joms.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 18.Ventä I, Turtola L, Ylipaavalniemi P. Radiographic follow-up of impacted third molars from age 20 to 32 years. Int J Oral Maxillofac Surg. 2001;30:54–57. doi: 10.1054/ijom.2000.0002. [DOI] [PubMed] [Google Scholar]
- 19.Brown LH, Berkman S, Cohen D, Kaplan AL, Rosenberg M. A radiological study of the frequency and distribution of impacted teeth. J Dent Assoc S Afr. 1982;37:627–630. [PubMed] [Google Scholar]
- 20.Murtomaa H, Turtola L, Ylipaavalniemi P, Rytömaa I. Status of the third molars in the 20- to 21-year-old Finnish university population. J Am Coll Health. 1985;34:127–129. doi: 10.1080/07448481.1985.9939622. [DOI] [PubMed] [Google Scholar]
- 21.Behbehani F, Artun J, Thalib L. Prediction of mandibular third-molar impaction in adolescent orthodontic patients. Am J Orthod Dentofacial Orthop. 2006;130:47–55. doi: 10.1016/j.ajodo.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 22.Uthman AT. Retromolar space analysis in relation to selected linear and angular measurements for an Iraqi sample. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e76–e82. doi: 10.1016/j.tripleo.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 23.Farzanegan F, Goya A. Evaluation of mandibular third molar positions in various vertical skeletal malocclusions. J Dent Mater Tech. 2012;1:58–62. [Google Scholar]
- 24.Richardson M. Changes in lower third molar position in the young adult. Am J Orthod Dentofacial Orthop. 1992;102:320–327. doi: 10.1016/0889-5406(92)70047-E. [DOI] [PubMed] [Google Scholar]
- 25.Hattab FN. Positional changes and eruption of impacted mandibular third molars in young adults. A radiographic 4-year follow-up study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:604–608. doi: 10.1016/s1079-2104(97)90359-0. [DOI] [PubMed] [Google Scholar]
- 26.Kruger E, Thomson WM, Konthasinghe P. Third molar outcomes from age 18 to 26: findings from a population-based New Zealand longitudinal study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:150–155. doi: 10.1067/moe.2001.115461. [DOI] [PubMed] [Google Scholar]
- 27.Hesby RM, Marshall SD, Dawson DV, Southard KA, Casko JS, Franciscus RG, et al. Transverse skeletal and dentoalveolar changes during growth. Am J Orthod Dentofacial Orthop. 2006;130:721–731. doi: 10.1016/j.ajodo.2005.03.026. [DOI] [PubMed] [Google Scholar]


