Abstract
Objective
To describe the clinical evaluation and operative management of posterior semicircular canal dehiscence caused by a high jugular bulb.
Methods
Retrospective case report.
Results
The patient had clinical and audiometric findings consistent with semicircular canal dehiscence and imaging demonstrating erosion of the posterior semicircular canal by a high jugular bulb. Resurfacing of the eroded canal provided resolution of vestibular symptoms without damage to the inner ear.
Conclusions
Dehiscence of the posterior semicircular canal can cause clinical and audiometric findings similar to those of superior semicircular canal dehiscence syndrome. Resurfacing of the area of dehiscence can be performed to successfully relieve the vestibular symptoms. In the case of dehiscence of the posterior canal from a high jugular bulb, resurfacing may offer advantages over canal plugging for definitive management.
Introduction
In 1998, Minor first described superior semicircular canal dehiscence syndrome (SSCD), with clinical features of conductive hearing loss, autophony, chronic imbalance and pressure or noise induced torsional nystagmus1. In this syndrome the bone overlying the superior semicircular canal is absent leaving the temporal dura in direct contact with the membraneous labyrinth, producing a “third window” into the inner ear. Since first described, many features of this disease and methods of treatment have been more clearly defined. Surgical management for SSCD includes capping, plugging, or resurfacing.
Posterior semicircular canal dehiscence (PSCD) was first described radiographically in 1986. Bony PSCD due to a high jugular bulb has been reported by a number of authors2–6 and can present with clinical findings similar to those seen with superior canal dehiscence. In a recent case series, the majority of patients with dehiscence of the posterior semicircular canal (11/12) was due to a high riding jugular bulb4.
Surgical management of PSCD has been described only once previously by Mikulec and Poe involving transmastoid plugging of the involved canal6. We report the first case of PSCD managed operatively through decompression of the jugular bulb with resurfacing of the dehiscent canal. The retrospective review of the presentation, workup and management of a case of PSCD was performed and approved by our Institutional Review Boards. A discussion of considerations in the management of PSCD follows.
Case Report
A 20-year-old man presented to our tertiary care center with complaints of noise-induced vertigo and right-sided pulsatile tinnitus starting four months earlier after a ground-level fall where he sustained a left-sided, otic capsule-sparing temporal bone fracture isolated to the external auditory canal. A detailed neurotological examination on presentation, including fistula testing, was unremarkable aside from evidence of a healed fracture of the left external auditory canal. Audiometric evaluation revealed a symmetric, mild to moderate-severe downsloping sensorineural hearing loss with word recognition scores of 96% bilaterally. Vestibular evoked myogenic potential (VEMP) testing (100μ sec broadband click with 5 clicks/sec) revealed a lowered threshold on the right side compared to the left (67 dB NHL versus 92 dB NHL respectively) though interaural amplitude ratio was within normal limits at 25% (Fig. 1). Rotary chair testing demonstrated normal vestibulo-ocular and visual vestibulo-ocular reflexes. Infrared videonystagmography evaluation was normal aside from vertical nystagmus in the head-hanging center and seated positions in the dark. Upbeating, vertical nystagmus was recorded with application of positive pressure in the right EAC (Fig. 2). In addition, upbeating, vertical nystagmus was recorded after delivery of a 500 Hz tone at 110 dB HL to the right EAC (Fig.3) occurring in a delayed fashion after noise presentation (see Video, Supplemental Digital Content 1, which demonstrates noise-induced and pressure-induced nystagmus). High-resolution temporal bone computed tomography (CT) in oblique planes (Fig. 4) delineated a broad area of dehiscence of otic capsular bone due to a large, high-riding jugular bulb on the right side. The posterior semicircular canal was found to be widely dehiscent including the ampulla of the canal. No superior canal dehiscence was evident on either side. In addition, there was a left-sided, otic capsule-sparing temporal bone fracture isolated to the external auditory canal.
Figure 1.
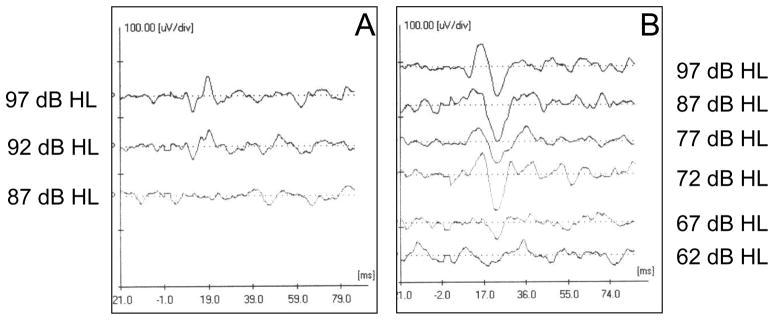
Cervical VEMP’s thresholds of 92 dB in the left (A) and 67 dB in the right (B) ear along with an increased PN amplitude on the side of the PSCD due to the high jugular bulb.
Figure 2.
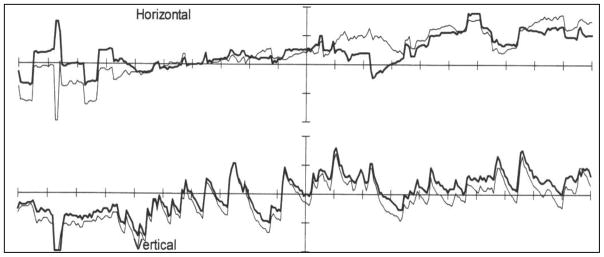
Videonystagmogram demonstrating upbeating vertical nystagmus upon application of positive pressure in right external auditory canal (Fistula test).
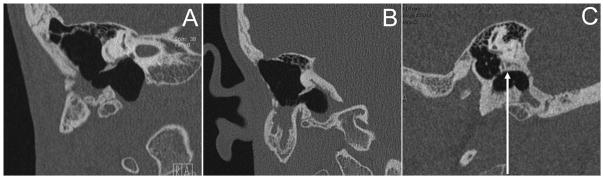
Figure 3.
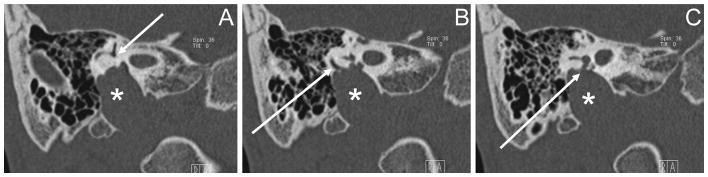
Oblique CT scan series demonstrating erosion of the otic capsule due to a high riding jugular bulb (asterisks) with a broad area of dehiscence of the PSCC. Arrows mark common crus (A) and posterior semicircular canal (B) and PSCC ampulla (C).
Figure 4.
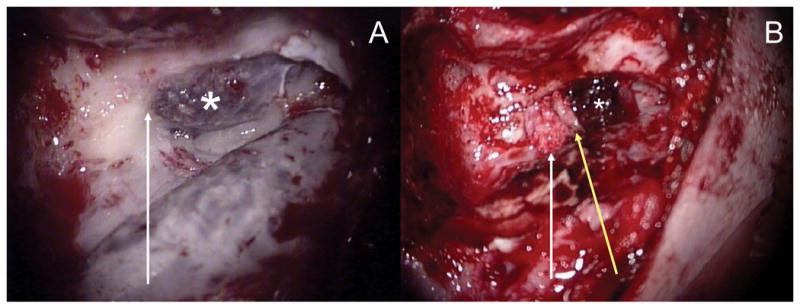
A) Intra-operative view of the high right jugular bulb (asterisk) apposed to the inferior aspect of the otic capsule (arrow) prior to repair. B) After reduction of the high jugular bulb (asterisk), composite repair was performed by plugging of the PSCD with fascia followed by placement of bone pate (arrow) and a bone graft (yellow arrow).
Due to the presence of ongoing noise-induced vertigo that interfered with the patient’s work around heavy machinery, surgical intervention was offered. A transmastoid approach was taken to allow for wide decompression of a notably high-riding jugular bulb (Figure 5). The bulb was decompressed then reduced inferiorly using bipolar cautery, surgical packing and bone wax. After decompression a temporalis fascial graft was applied into the area of dehiscence then supported by placement of a layer of bone pate. A cortical bone graft was then placed beneath the bone pate to complete the composite repair. Bleeding from the jugular bulb was controlled with topical hemostatic agents.
Figure 5.
Postoperative CT scan in oblique (A), coronal (B) and sagittal (C) views demonstrating notable reduction of the high jugular bulb inferiorly leaving an air filled infralabyrinthine space. The sagittal view (C) demonstrates successful bony resurfacing of the inferior aspect of the otic capsule (arrow) while the oblique and coronal views suggest some posterior displacement of the bone graft placed during composite repair.
The patient had an uneventful recovery from surgery and was discharged on the first postoperative day. On clinical follow-up two months after surgery the patient described resolution of his noise-induced vertigo and improvement of his pulsatile tinnitus. Audiometric evaluation revealed a new conductive hearing loss on the operated side of 20–40 decibels across all frequencies with an unchanged bone curve. Repeat VEMP testing revealed more symmetric thresholds (87 dB NHL on the right versus 97 dB NHL on the left) though the amplitude of the right-sided response was smaller than that on the left (42% interaural difference). Audiometry performed at 20 months postoperatively demonstrated normal discrimination scores, resolution of the earlier air-bone gap and pure-tone thresholds unchanged from his preoperative testing aside from a mild worsening (10–25 dB) of his pre-existing high frequency loss at 4 & 8 kHz only. The patient did complain of mild dysequilibrium at 20 months after surgery, which improved with vestibular rehabilitation therapy.
Discussion
This case report describes the successful management of a PSCD due to a high jugular bulb through bulb decompression and direct management of the area of dehiscence. The patient experienced resolution of his symptoms with this approach and no complications were encountered. In general, PSCD due to a high jugular bulb can be managed conservatively without the need for surgical intervention4,5. Our patient experienced a notable severity of symptoms, including pulsatile tinnitus, noise-induced vertigo which, given his occupation requiring work around loud machinery, caused him significant enough disability that he sought definitive therapy. We sought to directly address the broad area of PSCD in his case rather than perform a plugging maneuver of an uninvolved portion of the posterior canal, as was described in the only other report on the operative management of this condition6. Our rationale was that indirect plugging of an uninvolved portion of the canal may not preclude there from being continued interaction of the jugular bulb with the ampulla of the posterior canal, whereas resurfacing of the area of dehiscence using composite grafting might avoid this theoretic risk by establishing a solid partition between the jugular bulb and the membranous posterior canal. We were able to safely reduce the high jugular bulb inferiorly and perform a composite repair of the canal dehiscence with complete resolution of our patient’s symptoms.
Conclusion
PSCD is a rare but documented condition, in which patients present with symptoms and findings similar to those of SSCD. A high jugular bulb may be a significant contributor to PSCD. Operative management of PSCD by reduction of the jugular bulb and direct resurfacing of the area of dehiscence represents a viable approach for the temporal bone surgeon to consider when confronted with the uncommon need for definitive management of this disorder.
Supplementary Material
Infrared videonystagmography evaluation reveals upbeating, vertical nystagmus after delivery of a 3 kHz tone at 110 dB HL to the right EAC occurring in a delayed fashion after noise presentation. In addition, vertical nystagmus was recorded with application of positive pressure in the right EAC.
Acknowledgments
The project described was supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. SG receives support from NIH 1 R03 DC012432-01 and P30 HD003352.
Footnotes
Disclosure: Financial funding via salary support received from the National Institute of Health
References
- 1.Minor LB, Solomon D, et al. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal. Arch Otolaryngol. 1998;124:249–258. doi: 10.1001/archotol.124.3.249. [DOI] [PubMed] [Google Scholar]
- 2.Wadin K, Wilbrand H. The topographic relations of the high jugular fossa to the inner ear. A radioanatomic investigation. Acta Radiol Diagn. 1986;27(3):315–24. doi: 10.1177/028418518602700312. [DOI] [PubMed] [Google Scholar]
- 3.Krombach GA, DiMartino E, et al. Posterior semicircular canal dehiscence: a morphologic cause of vertigo similar to superior canal dehiscence. Eur Radiol. 2003;13:1444–50. doi: 10.1007/s00330-003-1828-5. [DOI] [PubMed] [Google Scholar]
- 4.Gopen Q, Guangwei Z, et al. Posterior semicircular dehiscence: First Reported Case Series. Otol & Neurotol. 2010;31:339–44. doi: 10.1097/MAO.0b013e3181be65a4. [DOI] [PubMed] [Google Scholar]
- 5.Friedmann DR, Le BT, et al. Clinical spectrum of patients with erosion of the inner ear by jugular bulb abnormalities. Laryngoscope. 2010;120:365–72. doi: 10.1002/lary.20699. [DOI] [PubMed] [Google Scholar]
- 6.Mikulec AA, Poe DS. Operative management of a posterior semicircular canal dehiscence. Laryngoscope. 2006;116:375–378. doi: 10.1097/01.mlg.0000200358.93385.5c. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Infrared videonystagmography evaluation reveals upbeating, vertical nystagmus after delivery of a 3 kHz tone at 110 dB HL to the right EAC occurring in a delayed fashion after noise presentation. In addition, vertical nystagmus was recorded with application of positive pressure in the right EAC.


