Abstract
Purpose. The aim of this study was to investigate whether single nucleotide polymorphisms (SNPs) in genes of the stress hormone signaling pathway, specifically FKBP5, NR3C1, and CRHR1, are associated with depressive symptoms during and after pregnancy. Methods. The Franconian Maternal Health Evaluation Study (FRAMES) recruited healthy pregnant women prospectively for the assessment of maternal and fetal health including the assessment of depressiveness. The German version of the 10-item Edinburgh Postnatal Depression Scale (EPDS) was completed at three time points in this prospective cohort study. Visit 1 was at study entry in the third trimester of the pregnancy, visit 2 was shortly after birth, and visit 3 was 6–8 months after birth. Germline DNA was collected from 361 pregnant women. Nine SNPs in the above mentioned genes were genotyped. After construction of haplotypes for each gene, a multifactorial linear mixed model was performed to analyse the depression values over time. Results. EPDS values were within expected ranges and comparable to previously published studies. Neither did the depression scores differ for comparisons among haplotypes at fixed time points nor did the change over time differ among haplotypes for the examined genes. No haplotype showed significant associations with depressive symptoms severity during pregnancy or the postpartum period. Conclusion. The analysed candidate haplotypes in FKBP5, NR3C1, and CRHR1 did not show an association with depression scores as assessed by EPDS in this cohort of healthy unselected pregnant women.
1. Introduction
During pregnancy the overall prevalence of depressive episodes is about 10–20% [1, 2] and about 6–15% in childbed [3, 4]. A total of about 70,000–90,000 women in Germany suffer from this disorder every year, with 5-6% developing major depression [2, 4, 5]. The prevalence compares to that of non-pregnancy-associated depression; however, new depression occurs more often during pregnancy and in the postpartum period [6].
There is a correlation of pregnancy-associated depression with poorer obstetric outcome measures, with fetal and neonatal complications [7, 8], with the length of the mother's hospital stay at the time of delivery [9], and with a negative impact on the child's development [10–13]. Information about the pathogenesis for pregnancy-associated depression may therefore be helpful for planning early interventions and understanding the pathogenesis of this disease, as it is not a part of the early intervention program in Germany yet [14]. In the general population, it is thought that between 33% and 77% of major depression can be attributed to genetic susceptibility [15, 16]. Several genome-wide association studies have been conducted [17–24] with some evidence for genetic susceptibility variants. Some studies described an association between perinatal depression and a family history of depression or perinatal depression [25–27]; however, only few studies have investigated specific genetic risk factors for perinatal depression.
One signalling pathway that is of specific interest in this context is the stress hormone system [28]. This signalling system is thought to be the key regulator of the response to environmental stressors. Its dysregulation is found consistently in stress related psychiatric disorders like major depression or posttraumatic stress disorder [29–31] and might play a relevant role in pregnant women [32]. With regard to pregnancy-associated depression, stress appeared to be one of the most stable factors in multivariate models for the prediction of depression during pregnancy [33], making this topic interesting for further research concerning this phenotype. Furthermore in utero exposure to stress and its subsequent exposure to glucocorticoids are discussed to have an influence on the development of behavioural stress response in the offspring [34, 35].
This study focuses on three genes, for which it is has been shown that genetic variants are associated with depressive symptomatology, especially in the context of stressful or adverse life events: the genes encoding the corticotropin releasing factor receptor 1 (CRHR1), the glucocorticoid receptor (NR3C1), and FK506 binding protein 51 (FKBP5).
CRHR1 function has been reported to be specifically associated with increased fear, alertness, depression, and anxiety [36–39]. Genetic variants in CRHR1 have been associated with anxiety disorders, major depression, and alcoholism, especially in the context of early life adverse events [28, 40].
NR3C1 encodes the glucocorticoid receptor (GR). GR signalling has been reported to be disrupted in both depression and anxiety disorders [30, 41]. Several genetic variants have been described to result in functional changes of the GR [42, 43].
FKBP5 is known to bind to and alter the function of steroid hormone receptors, including the GR [44] and is a negative feedback regulator of GR function [31, 45]. Functional genetic variants in FKBP5 have been described to alter stress hormone response regulation as well as the risk to suffer from depression and other psychiatry disorders when exposed to childhood trauma [28, 46].
The aim of the present study was to test whether genetic variants in FKBP5, GR (NR3C1), and CRHR1, previously described to increase the risk for depression, are associated with longitudinal measures of depressive symptoms in a cohort of pregnant women assessed in the third trimester of pregnancy, 2-3 days and 6 months after delivery.
2. Patients and Methods
2.1. Patient Selection and Biomaterial Retrieval
The Franconian Maternal Health Evaluation Study (FRAMES) is a prospective study, which recruited pregnant women from 2005 to 2007. Aim was the investigation of risk factors for pregnancy-associated depression [4, 47–49]. Previously we presented the influence of variants in TPH2 on depression measurement scores during the pregnancy [47] and that of variants in the serotonin transporter 5-HTTLPR on different depression levels after childbirth with regard to lifetime and current psychological stressors [50].
Inclusion criteria were age of 18 years or older with an intact pregnancy and at a gestational age of at least 31 weeks. They were invited to participate when they presented to register for the upcoming birth. A total of 1100 women were prospectively included. Assessment of genetic risk factors for postpartum depression was included as a study aim after the recruitment of women was completed in 2008. Blood samples for genetic analysis were therefore not taken prospectively, and the women had to be recalled for this purpose. This took place between January 2008 and July 2008. The patients were contacted by phone and invited to undergo blood sampling and take part in the genetic association study. From the primary study population (n = 1100) current phone numbers could be determined from 780 patients and 705 could be reached. 130 women declined to take part; the rest was appointed for a blood draw. Women, who did not show up, were contacted again and offered another appointment. A total of 431 women presented for blood sampling (final study population). DNA extraction was successful in 423 cases. DNA was considered unsuitable for the study if the DNA concentration was below 30 ng/μL according to the PicoGreen DNA concentration measurements. In addition, 62 women had to be excluded from the analysis because the depression measurement was lacking for at least one time point in the study, resulting in a final sample size for this study of 361 patients. The study was approved by the Ethics Committee of the Medical Faculty of Friedrich-Alexander University of Erlangen-Nuremberg and all of the patients provided written informed consent.
2.2. Questionnaire
The participants were interviewed using standardised 10-item Edinburgh Postnatal Depression Scale (EPDS) questionnaires, in the German version [51], at three time points: prepartal, from the 31st week of pregnancy onwards (Q1); 48–72 hours postpartum (Q2) to capture the initial phase of the maternity blues; and 6–8 months after birth (Q3). Additionally a structured questionnaire was used to document common epidemiological parameters and medical history that was not documented in the patients' files. This questionnaire included the question about preexisting psychiatric disorders, which was an exclusion criteria for this study. The first two questionnaires (Q1, Q2) were structured as personal interviews using standardised manuals, which were conducted by trained and medically qualified staff. The third questionnaire (Q3) was carried out by phone interview. The reliability of phone questionnaires in this setting can be regarded as confirmed [52].
2.3. SNP Selection
SNPs in the genes FKBP5, NR3C1, and CRHR1 have been selected for genotyping based on published positive association studies with depression or depressive symptoms for the respective SNPs and haplotypes (see Section 1). The SNPs with the strongest gene environment interaction effects, which mean depressive symptoms, were selected (CRHR1 SNPs: rs7209436 and rs110402 [28, 40]; NR3C1 SNPs: rs41423247, rs6195, and rs10482605 [42, 43]; FKBP5 SNPs: rs1360780, rs9296158, rs3800373, and rs9470080 [28, 46]). SNP IDs and their minor allele frequency (MAF) are reported in Table 1.
Table 1.
Genotype and allele distribution for each single nucleotide polymorphism (SNP). Absolute frequencies and percentages (in brackets) are shown.
| SNP | Chrom.1 | Position | Alleles2 | MAF3 (%) | Homozygous, common4 | Heterozygous4 | Homozygous rare4 |
|---|---|---|---|---|---|---|---|
| rs1360780 (FKBP5) | 6 | 35607571 | C/T | 32.0 | 168 (46.5) | 155 (43.2) | 38 (10.5) |
| rs9296158 (FKBP5) | 6 | 35567082 | G/A | 32.0 | 166 (46.1) | 156 (43.3) | 37 (10.2) |
| rs3800373 (FKBP5) | 6 | 35542476 | T/G | 28.4 | 185 (51.8) | 147 (40.7) | 29 (8.0) |
| rs9470080 (FKBP5) | 6 | 35646435 | C/T | 34.7 | 155 (42.9) | 160 (44.6) | 45 (12.5) |
| rs41423247 (NR3C1) | 5 | 142778575 | G/C | 34.7 | 156 (43.3) | 158 (43.9) | 46 (12.7) |
| rs6195 (NR3C1) | 5 | 142779317 | A/G | 4.7 | 327 (91.6) | 34 (9.4) | 0 (0.0) |
| rs10482605 (NR3C1) | 5 | 142783521 | T/C | 18.3 | 242 (67.0) | 99 (27.6) | 16 (4.4) |
| rs110402 (CRHR1) | 17 | 43880047 | C/T | 45.3 | 110 (30.6) | 175 (48.6) | 76 (21.1) |
| rs7209436 (CRHR1) | 17 | 43870142 | C/T | 44.0 | 115 (32.2) | 174 (48.2) | 72 (19.9) |
1Chromosome; 2major/minor allele, based on the forward strand and minor allele frequency; 3minor allele frequency; 4frequency, percentage in brackets.
2.4. DNA Preparation and Genotyping
DNA was extracted from 10 mL of ethylenediaminetetraacetic acid (EDTA) blood using the Puregene whole-blood DNA extraction kit (Gentra Systems, Minneapolis, MN, USA). FKBP5, NR3C1, and CRHR1 SNPs were analysed on a Sequenom platform using the iPlex technology (Sequenom, San Diego, CA, USA) in a multiplex assay using 10 ng of DNA. For quality control, duplicate DNAs as well as negative controls were included in the genotyping plates. Genotype calls were made using the ArrayTyper 3.4 software (Sequenom, San Diego, CA, USA).
2.5. Statistical Considerations
Genotypes were analysed as haplotypes. The reconstruction of haplotypes was carried out with an expectation-maximisation (EM) algorithm [53]. For the haplotype reconstruction, all SNPs were grouped by gene. Genotype distributions were tested for Hardy-Weinberg Equilibrium. Haplotypes were examined rather than single SNPs because haplotypes may provide more genetic information. Associations between SNPs and outcome measure are expected to be reflected in associations between haplotypes and outcome measure, but not necessarily vice versa.
The EPDS value was regarded as continuous measurement with a range from 0 to 26. Depression values from the three different time points Q1, Q2, and Q3 were compared. For each haplotype, a categorical variable with levels according to the frequency of 0, 1, or 2 copies per patient was generated. Small groups with fewer than five carriers of two copies of a haplotype were joined with the carriers of one copy. Extremely rare haplotypes with an overall haplotype frequency of fewer than 10 occurrences were excluded from the analysis. Consideration of the haplotypes as ordinal variables was rejected due to nonlinear coherence with EPDS.
The association between haplotypes and the course of depression was analysed using linear mixed models with EPDS as target variable. For each haplotype block, a linear mixed model was fitted with patient as random effect and haplotypes, time (Q1, Q2, Q3), and the interactions of haplotypes by time as fixed effects. These linear models were each compared with a basic linear mixed model with patient as random effect and time as the only fixed effect, using the likelihood ratio test. A significant test result means that the haplotypes are associated with EPDS. In that case the linear model was further analysed using F-tests of fixed effects. The P values of the likelihood ratio tests were adjusted for multiple testing according to the method of Bonferroni-Holm.
The model requirements (e.g., normal distribution of the standardised residuals) were tested graphically. No replacement of missing data took place. The random effect “patient” takes into account the fact that each patient had repeated EPDS measures. The models were fitted by maximum likelihood (ML) instead of restricted maximum likelihood (REML) in order to apply likelihood ratio tests to models with different fixed effects. A sensitivity analyses showed that both estimation methods gave almost identical results.
All of the tests were two-sided, and a P value of <0.05 was regarded as statistically significant. The statistical analyses were carried out using the R system for statistical computing (version 2.13.1; R Development Core Team, Vienna, Austria, 2011) and the SAS software package (version 9.2, SAS Institute, Inc., Cary, NC, USA).
3. Results
The genotype frequency and allele distributions are shown in Table 1. The genotype distribution for all SNPs was consistent with the Hardy-Weinberg equilibrium (P = 0.16 for rs10482605; P between 0.56 and 1.00 for the other SNPs). The distributions and frequencies for each haplotype block are presented in Table 2. For the most frequent haplotype of each gene the mean EPDS values of Q1, Q2, and Q3 are shown in Figures 1, 2, and 3 for carriers of 0, 1, or 2 copies of the respective haplotypes.
Table 2.
Reconstructed haplotypes for each gene and absolute frequencies and percentages (in brackets).
| No | Gene | SNP | Haplotype | Haplotype frequency | ||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | ||||
| 1 | FKBP5 | 1–4 | CGTC | 46 (12.74%) | 163 (45.15%) | 152 (42.11%) |
| 2 | CGTT | 341 (94.46%) | 19 (5.26%) | 1 (0.28%) | ||
| 3 | CATC | 360 (99.72%) | 1 (0.28%) | 0 (0.00%) | ||
| 4 | CATT | 360 (99.72%) | 1 (0.28%) | 0 (0.00%) | ||
| 5 | CAGC | 360 (99.72%) | 1 (0.28%) | 0 (0.00%) | ||
| 6 | TGTT | 358 (99.17%) | 3 (0.38%) | 0 (0.00%) | ||
| 7 | TATC | 359 (99.45%) | 2 (0.55%) | 0 (0.00%) | ||
| 8 | TATT | 339 (93.91%) | 22 (6.09%) | 0 (0.00%) | ||
| 9 | TAGC | 360 (99.72%) | 1 (0.28%) | 0 (0.00%) | ||
| 10 | TAGT | 187 (51.80%) | 145 (40.17%) | 29 (8.03%) | ||
|
| ||||||
| 11 | GR-NR3C1 | 5–7 | GAT | 118 (32.69%) | 178 (49.31%) | 65 (18.01%) |
| 12 | GAC | 247 (68.42%) | 99 (27.42%) | 15 (4.16%) | ||
| 13 | GGT | 327 (90.58%) | 33 (9.14%) | 1 (0.28%) | ||
| 14 | CAT | 158 (43.77%) | 158 (43.77%) | 45 (12.47%) | ||
| 15 | CAC | 359 (99.45%) | 2 (0.55%) | 0 (0.00%) | ||
|
| ||||||
| 16 | CRHR1 | 8+9 | CC | 76 (21.05%) | 175 (48.48%) | 110 (30.47%) |
| 17 | TC | 352 (97.51%) | 9 (2.49%) | 0 (0.00%) | ||
| 18 | TT | 115 (31.86%) | 174 (48.20%) | 72 (19.94%) | ||
Figure 1.
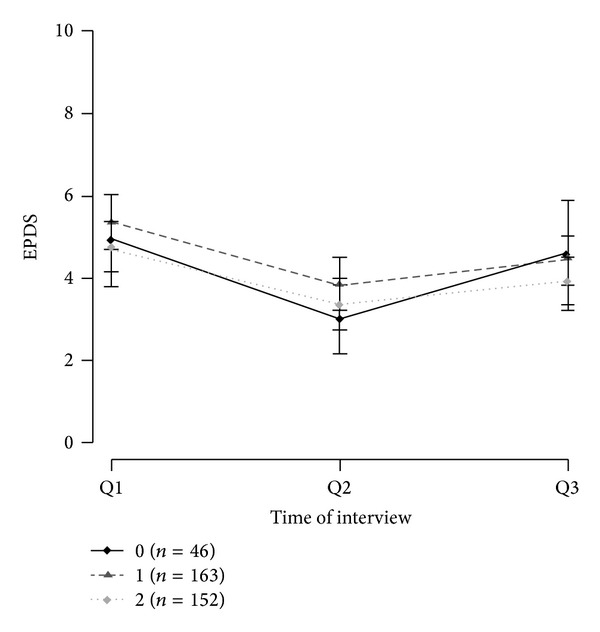
Mean EPDS values of FKBP5 haplotype CGTC with 95% confidence intervals.
Figure 2.
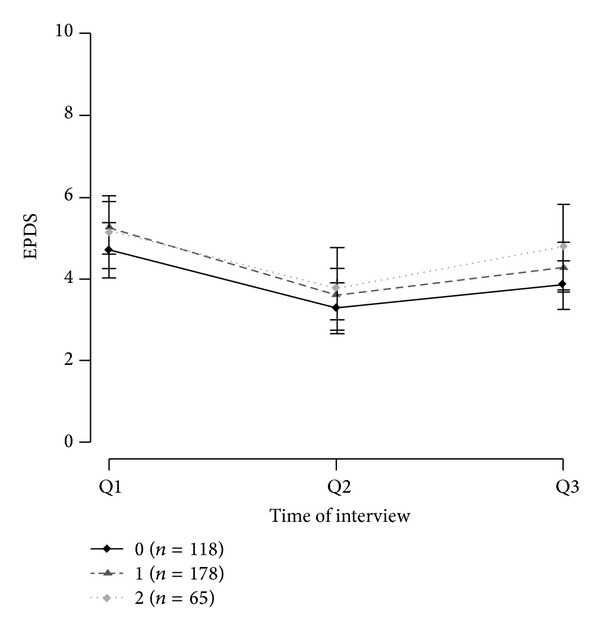
Mean EPDS values of GRNR3C1 haplotype GAT with 95% confidence intervals.
Figure 3.
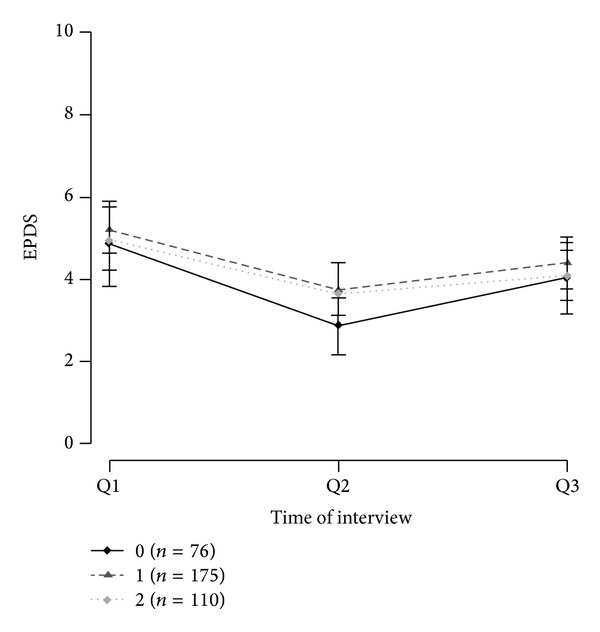
Mean EPDS values of CRHR1 haplotype CC with 95% confidence intervals.
The SNPs within gene FKBP5 formed ten haplotypes, but only four of them, CGTC, CGTT, TATT, and TAGT, occurred with a frequency usable for analysis. For haplotype CGTT the group of carriers of two copies (0.28%) was joined with the carriers of one copy (5.26%).
Haplotype reconstruction with the NR3C1 SNPs resulted in five haplotypes. The most common haplotype was GAT, with 49.31% of patients carrying two copies and 32.69% carrying one copy. For haplotype GGT the group of carriers of two copies (0.28%) was joined with the carriers of one copy (9.14%). The haplotype CAC had to be discarded because of only two occurrences.
The haplotype reconstruction within gene CRHR1 resulted in three haplotypes where haplotype CC was the most common with 30.47% carrying two copies and 48.48% carrying one copy.
None of the haplotypes showed a significant result for the likelihood ratio test (unadjusted P values: FKBP5, P = 0.45; NR3C1, P = 0.78; CRHR1, P = 0.61). Therefore no further analysis was performed, as differences between genotype groups at one time point or over different time points cannot be assumed.
4. Discussion
With our association study in a cohort of pregnant women without further risk factors for depressive or anxiety disorders, we could not show that candidate single nucleotide polymorphisms within the genes FKBP5, NR3C1, and CRHR1 are associated with EPDS values during or after pregnancy.
The candidate genes were selected because of their role within stress hormone signalling system which is one of the possible mediators between environmental stressors and the development of a depressive reaction. Several genetic factors have been discovered that explain individual responses to stressful events [28, 29, 54–56].
However, with our study design and the examined genetic variants, no effect on EPDS values could be seen, neither between haplotypes at specific time points, nor in comparing the changes of EPDS over time according to haplotypes. Several factors specific to this study will be discussed below.
As we were studying a cohort of women with an uncomplicated pregnancy and no prior history of psychiatric disease, there might be a different genotype distribution in our cohort than in cohorts of women without the inclusion criterion of pregnancy. It was reported that variants in NR3C1 may have an influence on gonadotropin levels in women with anovulatory polycystic ovary syndrome (PCOS) [57]. Another study reported variants in NR3C1 to be associated with recurrent miscarriages [58]. There is further preclinical evidence that exposure to glucocorticoids leads to the apoptosis of fetal ovary germline cells, having possible impact on fertility [59]. Preselecting of women with an uncomplicated pregnancy could therefore result in a population with slightly different genotype distribution.
Furthermore during pregnancy many signalling pathways adapt with regard to ensuring the function of the pregnancy, with one of them being the hypothalamic-pituitary-adrenal axis or stress hormone system [60]. Therefore genetic associations that are observed in women without a pregnancy might not be found in a population of pregnant women. In particular during the third trimester progressively increasing circulating levels of placental CRH are seen [61] as well as gradually decreasing levels of CRH binding protein [62]. Maternal distress during pregnancy increases plasma levels of cortisol and CRH in addition to the already physiologically increased levels [63]. After delivery a central suppression of hypothalamic CRH secretion might explain a generally increased vulnerability to the affective disorders observed during this period [64]. For these reasons associations between genotypes and phenotypes might be different in pregnant and nonpregnant populations.
Several limitations of this study have to be taken into consideration. One might be the use of the EPDS questionnaire a few days after childbirth. The EPDS reflects the experience and mood state of women during the week before completing the questionnaire, intentionally skipping somatic symptoms that are associated with depression but appear quite often after delivery in healthy women, such as sleep disturbances or fatigue, and it has been validated for administration during pregnancy and a few weeks into the postpartum period [65–69]. The rating within the first days after delivery might thus also reflect the mood during the last days of pregnancy. Another limitation might be that patients were recontacted for blood sampling for DNA extraction after the end of the study. However, there were no differences with regard to prepartum or postpartum EPDS scores in women participating or not participating in the genetic substudy (data not shown). Women were screened for preexisting psychiatric disorders only by a questionnaire. This self-reported depression is not as accurate as the assessment by a formal psychiatric diagnostic interview. However, in contrast to other studies, a classic case/control design was not used for the analysis, and the prevalence of clinical depression was rather low in this cohort (6% as measured with the EPDS). Continuous EPDS values were therefore selected as the outcome variable in order to maximize the power of the study. Finally, due to the limited sample size our study might not show smaller effect of the examined genetic variants.
In conclusion we could not show an association between depression measurements as assessed by EPDS values during or after pregnancy and candidate haplotypes in the genes FKBP5, NR3C1, and CRHR1. As other studies have shown some association between genetic variants in these genes and depressive symptomatology, our null results could be explained by a small sample size or a generally different role of genetic variants in genes of the stress hormone signalling pathway in pregnant women.
Acknowledgments
The authors acknowledge the support by Deutsche Forschungsgemeinschaft and Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) within the funding programme Open Access Publishing.
Conflict of Interests
The authors have no conflict of interests to report.
References
- 1.Gawlik S, Reck C, Kuelkens S, et al. Prenatal depression and anxiety what is important for the obstetrician? Geburtsh Frauenheilk. 2010;70(5):361–368. [Google Scholar]
- 2.Gaynes BN, Gavin N, Meltzer-Brody S, et al. Perinatal depression: prevalence, screening accuracy, and screening outcomes. Evidence Report/Technology Assessment (Summary) 2005;(119):1–8. doi: 10.1037/e439372005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perfetti J, Clark R, Fillmore C-M. Postpartum depression: identification, screening, and treatment. Wisconsin Medical Journal. 2004;103(6):56–63. [PubMed] [Google Scholar]
- 4.Reulbach U, Bleich S, Knörr J, et al. Pre-, peri- and postpartal depression first cognition from FRAMES (Franconian Maternal Health Evaluation Studies) Fortschritte der Neurologie Psychiatrie. 2009;77(12):708–713. doi: 10.1055/s-0028-1109822. [DOI] [PubMed] [Google Scholar]
- 5.Voigt M, Schild RL, Mewitz M, et al. Maternal weight gain during pregnancy and somatic classification of neonates according to birth weight and duration of pregnancy taking account of maternal body weight and height. Geburtsh Frauenheilk. 2013;73(4):318–323. doi: 10.1055/s-0032-1328436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstetrics and Gynecology. 2005;106(5):1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 7.Alder J, Fink N, Bitzer J, Hösli I, Holzgreve W. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. Journal of Maternal-Fetal and Neonatal Medicine. 2007;20(3):189–209. doi: 10.1080/14767050701209560. [DOI] [PubMed] [Google Scholar]
- 8.Bansil P, Kuklina EV, Meikle SF, et al. Maternal and fetal outcomes among women with depression. Journal of Women’s Health. 2010;19(2):329–334. doi: 10.1089/jwh.2009.1387. [DOI] [PubMed] [Google Scholar]
- 9.Lancaster CA, Flynn HA, Johnson TRB, Marcus SM, Davis MM. Peripartum length of stay for women with depressive symptoms during pregnancy. Journal of Women’s Health. 2010;19(1):31–37. doi: 10.1089/jwh.2009.1383. [DOI] [PubMed] [Google Scholar]
- 10.Agnafors S, Sydsjö G, deKeyser L, Svedin CG. Symptoms of depression postpartum and 12 years later-associations to child mental health at 12 years of age. Maternal and Child Health Journal. 2013;17(3):405–414. doi: 10.1007/s10995-012-0985-z. [DOI] [PubMed] [Google Scholar]
- 11.Deave T, Heron J, Evans J, Emond A. The impact of maternal depression in pregnancy on early child development. BJOG: An International Journal of Obstetrics and Gynaecology. 2008;115(8):1043–1051. doi: 10.1111/j.1471-0528.2008.01752.x. [DOI] [PubMed] [Google Scholar]
- 12.Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clinical Child and Family Psychology Review. 2011;14(1):1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- 13.Besier T, Pillhofer M, Botzenhart S, et al. Child abuse and neglect: screening for risks during the perinatal period. Geburtsh Frauenheilk. 2012;72(5):397–402. doi: 10.1055/s-0031-1298442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yazdi B, Abele H, Grischke EM, et al. Obstetrics. Prenatal care in reconstruction: from head to toe? Geburtsh Frauenheilk. 2013;73(4):295–298. [Google Scholar]
- 15.Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. The lifetime history of major depression in women: reliability of diagnosis and heritability. Archives of General Psychiatry. 1993;50(11):863–870. doi: 10.1001/archpsyc.1993.01820230054003. [DOI] [PubMed] [Google Scholar]
- 16.McGuffin P, Katz R, Watkins S, Rutherford J. A hospital-based twin register of the heritability of DSM-IV unipolar depression. Archives of General Psychiatry. 1996;53(2):129–136. doi: 10.1001/archpsyc.1996.01830020047006. [DOI] [PubMed] [Google Scholar]
- 17.Kohli MA, Lucae S, Saemann PG, et al. The neuronal transporter gene slc6a15 confers risk to major depression. Neuron. 2011;70(2):252–265. doi: 10.1016/j.neuron.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewis RA, Shahi SK, Laing E, et al. Genome-wide transcriptomic analysis of the response to nitrogen limitation in Streptomyces coelicolor A3(2) BMC Research Notes. 2011;4, article 78 doi: 10.1186/1756-0500-4-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muglia P, Tozzi F, Galwey NW, et al. Genome-wide association study of recurrent major depressive disorder in two European case-control cohorts. Molecular Psychiatry. 2010;15(6):589–601. doi: 10.1038/mp.2008.131. [DOI] [PubMed] [Google Scholar]
- 20.Rietschel M, Mattheisen M, Frank J, et al. Genome-wide association-, replication-, and neuroimaging study implicates homer1 in the etiology of major depression. Biological Psychiatry. 2010;68(6):578–585. doi: 10.1016/j.biopsych.2010.05.038. [DOI] [PubMed] [Google Scholar]
- 21.Shi J, Potash JB, Knowles JA, et al. Genome-wide association study of recurrent early-onset major depressive disorder. Molecular Psychiatry. 2011;16(2):193–201. doi: 10.1038/mp.2009.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shyn SI, Shi J, Kraft JB, et al. Novel loci for major depression identified by genome-wide association study of sequenced treatment alternatives to relieve depression and meta-analysis of three studies. Molecular Psychiatry. 2011;16(2):202–215. doi: 10.1038/mp.2009.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sullivan PF, De Geus EJC, Willemsen G, et al. Genome-wide association for major depressive disorder: a possible role for the presynaptic protein piccolo. Molecular Psychiatry. 2009;14(4):359–375. doi: 10.1038/mp.2008.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wray NR, Pergadia ML, Blackwood DHR, et al. Genome-wide association study of major depressive disorder: new results, meta-analysis, and lessons learned. Molecular Psychiatry. 2012;17(1):36–48. doi: 10.1038/mp.2010.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Forty L, Jones L, Macgregor S, et al. Familiality of postpartum depression in unipolar disorder: results of a family study. American Journal of Psychiatry. 2006;163(9):1549–1553. doi: 10.1176/ajp.2006.163.9.1549. [DOI] [PubMed] [Google Scholar]
- 26.Murphy-Eberenz K, Zandi PP, March D, et al. Is perinatal depression familial? Journal of Affective Disorders. 2006;90(1):49–55. doi: 10.1016/j.jad.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 27.Payne JL, Mackinnon DF, Mondimore FM, et al. Familial aggregation of postpartum mood symptoms in bipolar disorder pedigrees. Bipolar Disorders. 2008;10(1):38–44. doi: 10.1111/j.1399-5618.2008.00455.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Binder EB, Nemeroff CB. The CRF system, stress, depression and anxietyinsights from human genetic studies. Molecular Psychiatry. 2010;15(6):574–588. doi: 10.1038/mp.2009.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Menke A, Klengel T, Rubel J, et al. Genetic variation in FKBP5 associated with the extent of stress hormone dysregulation in major depression. Genes, Brain and Behavior. 2013;12(3):289–296. doi: 10.1111/gbb.12026. [DOI] [PubMed] [Google Scholar]
- 30.De Kloet ER, Joëls M, Holsboer F. Stress and the brain: from adaptation to disease. Nature Reviews Neuroscience. 2005;6(6):463–475. doi: 10.1038/nrn1683. [DOI] [PubMed] [Google Scholar]
- 31.Binder EB. The role of FKBP5, a co-chaperone of the glucocorticoid receptor in the pathogenesis and therapy of affective and anxiety disorders. Psychoneuroendocrinology. 2009;34(1):S186–S195. doi: 10.1016/j.psyneuen.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 32.Schwab W, Marth C, Bergant AM. Post-traumatic stress disorder post partum: the impact of birth on the prevalence of post-traumatic stress disorder (PTSD) in multiparous women. Geburtsh Frauenheilk. 2012;72(1):56–63. doi: 10.1055/s-0031-1280408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. American Journal of Obstetrics and Gynecology. 2010;202(1):5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davis EP, Waffarn F, Sandman CA. Prenatal treatment with glucocorticoids sensitizes the hpa axis response to stress among full-term infants. Developmental Psychobiology. 2011;53(2):175–183. doi: 10.1002/dev.20510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davis EP, Sandman CA, Buss C, et al. Fetal glucocorticoid exposure is associated with preadolescent brain development. Biological Psychiatry. 2013;74(9):647–655. doi: 10.1016/j.biopsych.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heinrichs SC, Lapsansky J, Lovenberg TW, De Souza EB, Chalmers DT. Corticotropin-releasing factor CRF1, but not CRF2, receptors mediate anxiogenic-like behavior. Regulatory Peptides. 1997;71(1):15–21. doi: 10.1016/s0167-0115(97)01005-7. [DOI] [PubMed] [Google Scholar]
- 37.Arborelius L, Owens MJ, Plotsky PM, Nemeroff CB. The role of corticotropin-releasing factor in depression and anxiety disorders. Journal of Endocrinology. 1999;160(1):1–12. doi: 10.1677/joe.0.1600001. [DOI] [PubMed] [Google Scholar]
- 38.Reul JMHM, Holsboer F. On the role of corticotropin-releasing hormone receptors in anxiety and depression. Dialogues in Clinical Neuroscience. 2002;4(1):31–46. doi: 10.31887/DCNS.2002.4.1/jreul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nemeroff CB. The corticotropin-releasing factor (CRF) hypothesis of depression: new findings and new directions. Molecular Psychiatry. 1996;1(4):336–342. [PubMed] [Google Scholar]
- 40.Bradley RG, Binder EB, Epstein MP, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Archives of General Psychiatry. 2008;65(2):190–200. doi: 10.1001/archgenpsychiatry.2007.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology. 2000;23(5):477–501. doi: 10.1016/S0893-133X(00)00159-7. [DOI] [PubMed] [Google Scholar]
- 42.Russcher H, Van Rossum EFC, De Jong FH, Brinkmann AO, Lamberts SWJ, Koper JW. Increased expression of the glucocorticoid receptor-A translational isoform as a result of the ER22/23EK polymorphism. Molecular Endocrinology. 2005;19(7):1687–1696. doi: 10.1210/me.2004-0467. [DOI] [PubMed] [Google Scholar]
- 43.Huizenga NATM, Koper JW, De Lange P, et al. A polymorphism in the glucocorticoid receptor gene may be associated with an increased sensitivity to glucocorticoids in vivo. Journal of Clinical Endocrinology and Metabolism. 1998;83(1):144–151. doi: 10.1210/jcem.83.1.4490. [DOI] [PubMed] [Google Scholar]
- 44.Sanchez ER. Hsp56: a novel heat shock protein associated with untransformed steroid receptor complexes. Journal of Biological Chemistry. 1990;265(36):22067–22070. [PubMed] [Google Scholar]
- 45.Jääskeläinen T, Makkonen H, Palvimo JJ. Steroid up-regulation of FKBP51 and its role in hormone signaling. Current Opinion in Pharmacology. 2011;11(4):326–331. doi: 10.1016/j.coph.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 46.Zannas AS, Binder EB. Gene-environment interactions at the FKBP5 locus: sensitive periods, mechanisms and pleiotropism. Genes, Brain and Behavior. 2014;13(1):25–37. doi: 10.1111/gbb.12104. [DOI] [PubMed] [Google Scholar]
- 47.Fasching PA, Faschingbauer F, Goecke TW, et al. Genetic variants in the tryptophan hydroxylase 2 gene (TPH2) and depression during and after pregnancy. Journal of Psychiatric Research. 2012;46(9):1109–1117. doi: 10.1016/j.jpsychires.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 48.Hein A, Rauh C, Engel A, et al. Socioeconomic status and depression during and after pregnancy in the Franconian Maternal Health Evaluation Studies (FRAMES) Archives of Gynecology and Obstetrics. 2013 doi: 10.1007/s00404-013-3046-y. [DOI] [PubMed] [Google Scholar]
- 49.Rauh C, Beetz A, Burger P, et al. Delivery mode and the course of pre- and postpartum depression. Archives of Gynecology and Obstetrics. 2012;286(6):1407–1412. doi: 10.1007/s00404-012-2470-8. [DOI] [PubMed] [Google Scholar]
- 50.Mehta D, Quast C, Fasching PA, et al. The 5-HTTLPR polymorphism modulates the influence on environmental stressors on peripartum depression symptoms. Journal of Affective Disorders. 2012;136(3):1192–1197. doi: 10.1016/j.jad.2011.11.042. [DOI] [PubMed] [Google Scholar]
- 51.Bergant AM, Nguyen T, Heim K, Ulmer H, Dapunt O. German version and validation of the Edinburgh depression scale (EPDS) Deutsche Medizinische Wochenschrift. 1998;123(3):35–40. doi: 10.1055/s-2007-1023895. [DOI] [PubMed] [Google Scholar]
- 52.Mitchell AM, Mittelstaedt ME, Schott-Baer D. Postpartum depression: the reliability of telephone screening. MCN The American Journal of Maternal/Child Nursing. 2006;31(6):382–387. doi: 10.1097/00005721-200611000-00010. [DOI] [PubMed] [Google Scholar]
- 53.Schaid DJ, Rowland CM, Tines DE, Jacobson RM, Poland GA. Score tests for association between traits and haplotypes when linkage phase is ambiguous. American Journal of Human Genetics. 2002;70(2):425–434. doi: 10.1086/338688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Minelli A, Maffioletti E, Cloninger CR, et al. Role of allelic variants of FK506-binding protein 51 (fkbp5) gene in the development of anxiety disorders. Depression and Anxiety. 2013;30(12):1170–1176. doi: 10.1002/da.22158. [DOI] [PubMed] [Google Scholar]
- 55.Velders FP, Dieleman G, Cents RA, et al. Variation in the glucocorticoid receptor gene at rs41423247 moderates the effect of prenatal maternal psychological symptoms on child cortisol reactivity and behavior. Neuropsychopharmacology. 2012;37(11):2541–2549. doi: 10.1038/npp.2012.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu Z, Zhu F, Wang G, et al. Association of corticotropin-releasing hormone receptor1 gene SNP and haplotype with major depression. Neuroscience Letters. 2006;404(3):358–362. doi: 10.1016/j.neulet.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 57.Valkenburg O, Uitterlinden AG, Themmen AP, et al. Genetic polymorphisms of the glucocorticoid receptor may affect the phenotype of women with anovulatory polycystic ovary syndrome. Human Reproduction. 2011;26(10):2902–2911. doi: 10.1093/humrep/der222. [DOI] [PubMed] [Google Scholar]
- 58.Hanna CW, Bretherick KL, Liu C-C, Stephenson MD, Robinson WP. Genetic variation within the hypothalamus-pituitary-ovarian axis in women with recurrent miscarriage. Human Reproduction. 2010;25(10):2664–2671. doi: 10.1093/humrep/deq211. [DOI] [PubMed] [Google Scholar]
- 59.Poulain M, Frydman N, Duquenne C, et al. Dexamethasone induces germ cell apoptosis in the human fetal ovary. The Journal of Clinical Endocrinology and Metabolism. 2012;97(10):E1890–E1897. doi: 10.1210/jc.2012-1681. [DOI] [PubMed] [Google Scholar]
- 60.Magiakou M-A, Mastorakos G, Rabin D, et al. The maternal hypothalamic-pituitary-adrenal axis in the third trimester of human pregnancy. Clinical Endocrinology. 1996;44(4):419–428. doi: 10.1046/j.1365-2265.1996.683505.x. [DOI] [PubMed] [Google Scholar]
- 61.Goland RS, Jozak S, Conwell I. Placental corticotropin-releasing hormone and the hypercortisolism of pregnancy. American Journal of Obstetrics and Gynecology. 1994;171(5):1287–1291. doi: 10.1016/0002-9378(94)90149-x. [DOI] [PubMed] [Google Scholar]
- 62.Linton EA, Perkins AV, Woods RJ, et al. Corticotropin releasing hormone-binding protein (CRH-BP): plasma levels decrease during the third trimester of normal human pregnancy. Journal of Clinical Endocrinology and Metabolism. 1993;76(1):260–262. doi: 10.1210/jcem.76.1.8421097. [DOI] [PubMed] [Google Scholar]
- 63.Oppo A, Mauri M, Ramacciotti D, et al. Risk factors for postpartum depression: the role of the Postpartum Depression Predictors Inventory-Revised (PDPI-R) : Rlts from the Perinatal Depression-Research Sc&reening Unit (PNDReScU) study. Archives of Women’s Mental Health. 2009;12(4):239–249. doi: 10.1007/s00737-009-0071-8. [DOI] [PubMed] [Google Scholar]
- 64.Magiakou M-A, Mastorakos G, Rabin D, Dubbert B, Gold PW, Chrousos GP. Hypothalamic corticotropin-releasing hormone suppression during the postpartum period: implications for the increase in psychiatric manifestations at this time. Journal of Clinical Endocrinology and Metabolism. 1996;81(5):1912–1917. doi: 10.1210/jcem.81.5.8626857. [DOI] [PubMed] [Google Scholar]
- 65.Sit DKY, Wisner KL. Identification of postpartum depression. Clinical Obstetrics and Gynecology. 2009;52(3):456–468. doi: 10.1097/GRF.0b013e3181b5a57c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Navarro P, Ascaso C, Garcia-Esteve L, Aguado J, Torres A, Martín-Santos R. Postnatal psychiatric morbidity: a validation study of the GHQ-12 and the EPDS as screening tools. General Hospital Psychiatry. 2007;29(1):1–7. doi: 10.1016/j.genhosppsych.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 67.Murray L, Carothers AD. The validation of the Edinburgh Post-natal Depression Scale on a community sample. British Journal of Psychiatry. 1990;157:288–290. doi: 10.1192/bjp.157.2.288. [DOI] [PubMed] [Google Scholar]
- 68.Harris B, Huckle P, Thomas R, Johns S, Fung H. The use of rating scales to identify post-natal depression. British Journal of Psychiatry. 1989;154:813–817. doi: 10.1192/bjp.154.6.813. [DOI] [PubMed] [Google Scholar]
- 69.Eberhard-Gran M, Eskild A, Tambs K, Opjordsmoen S, Samuelsen SO. Review of validation studies of the Edinburgh postnatal depression scale. Acta Psychiatrica Scandinavica. 2001;104(4):243–249. doi: 10.1034/j.1600-0447.2001.00187.x. [DOI] [PubMed] [Google Scholar]


