Abstract
Background
Acute stroke patients require immediate medical attention. Therefore, American Stroke Association guidelines recommend that for suspected stroke cases, emergency medical services (EMS) personnel spend less than 15 minutes (min) on-scene at least 90% of the time. However, not all EMS providers include specific scene time limits in their stroke patient care protocols.
Objective
We sought to determine whether having a protocol with a specific scene time limit was associated with less time EMS spent on scene.
Methods
Stroke protocols from the 100 EMS systems in North Carolina (NC) were collected and abstracted for scene time instructions. Suspected stroke events occurring in 2009 were analyzed using data from the NC Prehospital Medical Information System. Scene time was defined as the time from EMS arrival at the scene to departure with the patient. Quantile regression was used to estimate how the 90th percentile of the scene time distribution varied by systems with protocol instructions limiting scene time, adjusting for system patient volume and metropolitan status.
Results
In 2009, 23 EMS systems in NC had no instructions regarding scene time; 73 had general instructions to minimize scene time; and 4 had a specific limit for scene time (i.e. 10 or 15 min). Among 9,723 eligible suspected stroke events, mean scene time was 15.9 min (standard deviation 6.9 min) and median scene time was 15.0 min (90th percentile 24.3 min). In adjusted quantile regression models, the estimated reduction in the 90th percentile scene time, comparing protocols with a specific time limit to no instructions, was 2.2 min (95% confidence interval 1.3, 3.1 min). The difference in 90th percentile scene time between general and absent instructions was not statistically different (0.7 min (95% confidence interval -0.1, 1.4 min)).
Conclusion
Protocols with specific scene time limits were associated with EMS crews spending less time at the scene while general instructions were not. These findings suggest EMS systems can modestly improve scene times for stroke by specifying a time limit in their protocols.
Keywords: emergency medical services, stroke, protocol, ambulances, transportation of patients
INTRODUCTION
An acute stroke requires immediate medical attention. For every minute an ischemic stroke goes untreated, the typical patient loses an estimated 1.9 million brain cells.1 Current acute stroke therapy with intravenous tissue plasminogen activator can prevent further tissue death and potentially rescue damaged tissue when administered to eligible patients within 3 to 4.5 hours of symptom onset.2 Appropriate prehospital care of stroke patients by emergency medical services (EMS) personnel ensures timely identification, evaluation, and transport.3 Moreover, EMS use by stroke patients has been associated with shorter times to initial physician evaluation, brain imaging, and intravenous thrombolysis.4-9
Given the time urgency of current stroke treatment, EMS systems are recommended to capture and continually review specific time parameters that measure the timeliness of their prehospital stroke care.3 According to American Stroke Association (ASA) guidelines, the on-scene time, or amount of time EMS personnel spend with the patient before transport, should be less than 15 minutes (min) for stroke, excluding extenuating circumstances.3,10 Systems are encouraged to monitor and improve the 90th percentile of all response times since this metric best describes performance for the majority of patients.
In a 2008 survey in 9 states, 81% of EMS agencies reported having a specific scene time benchmark for responding to stroke,11 though the presence of a time benchmark was not objectively assessed. EMS protocols provide written instructions for evidence-based prehospital care of patients with a particular condition and often vary by the type and amount of information provided. Therefore, we assessed 2009 stroke protocols from North Carolina (NC) EMS systems for the presence of scene time instructions. Furthermore, we sought to determine whether having a stroke protocol with a specific scene time limit was associated with less time EMS spent on scene with stroke patients.
METHODS
Study Setting and Data Collection
In 2003, NC’s 100 local EMS systems were established to organize the state’s more than 35,000 EMS personnel and more than 540 EMS agencies on a county basis.12 All protocols, medical direction, and quality assurance activities occur at the system rather than the agency level. We retrospectively collected existing 2009 EMS stroke protocols from all NC systems. Two reviewers (MDP and CM) independently assessed stroke protocols for instructions regarding the minimization of on-scene time and whether a specific time limit was provided. Disagreements were adjudicated by a third reviewer (JHB). Systems with a specific limit for time spent on scene on their protocol were classified as “Specific time limit “ while those with only general instructions were classified as “General instructions “ and those with no stroke protocol or no scene time instructions were classified as “None”. The EMS system’s annual patient volume was estimated by using the number of total EMS patient encounters occurring in the past year, as recorded in the NC Credentialing Information System,13 and then categorized into 3 groups: <5,000, 5,000-20,000, and >20,000 patients per year. EMS systems were classified as metropolitan based on the county population.14
We analyzed EMS responses occurring in 2009 with data from the NC Prehospital Medical Information System (PreMIS), a statewide electronic healthcare record used for evaluation of EMS patient care and system performance.15 The PreMIS database collects more than 200 data elements defined in the National EMS Information System dataset.16 Each patient encounter by EMS in NC is submitted to PreMIS, amounting to over 1 million records per year. This database includes detailed data on the patient condition and care provided by EMS across the entire state. We defined a suspected stroke event as any 9-1-1 response in which the EMS personnel’s impression of the patient’s condition was stroke or the EMS personnel documented use of a stroke protocol. The outcome of interest was the time EMS personnel spent with the patient before transport, or “scene time,” which was defined as the time from EMS arrival at the scene to departure with the patient.17 For the final eligible sample, events were excluded if missing either EMS arrival or departure time, having an invalid computed scene time (i.e. ≤0 minutes), or scene time exceeded 2 hours. This study was approved by the University of North Carolina at Chapel Hill Public Health-Nursing Institutional Review Board.
Statistical Analysis
Descriptive statistics for scene times in suspected stroke events were calculated overall and by system-level protocol instructions and other system-level factors of interest (i.e. annual patient volume and metropolitan status). Quantile regression18 was used to estimate how the 10th to 90th percentiles of the scene time distribution in 10-percentile intervals varied by stroke protocol classification: specific time limit, general instructions, or no instructions (referent). The main association of interest was the difference in the 90th percentile of scene time by stroke protocol instructions because the recommended benchmark for EMS scene time is less than 15 min for at least 90% percent of suspected stroke patients. Since large, urban EMS systems tend to be more sophisticated and advanced, regression models were adjusted for annual patient volume and metropolitan status to account for potential confounding of the protocol-scene time association. Event counts among low volume and nonmetropolitan systems were insufficient to test for statistical interaction of the association between presence of protocol instructions and scene time. To further investigate the role of patient volume and metropolitan status, we fit models in the subgroup of high volume (i.e. >20,000 patients annually) and metropolitan EMS systems. Quantile regression parameters were estimated using the interior point algorithm,19 and 95% confidence intervals (CI) were constructed with bootstrap standard errors. Corresponding estimates from ordinary least squares models are presented for comparison. Statistical models were fit in SAS version 9.2 (Cary, NC).
Sensitivity Analysis
Thirty-two percent of records in the PreMIS database were missing data on both EMS personnel’s impression and protocol(s) used, whereas only 11% of records were missing the complaint determined by 9-1-1 dispatch. In an attempt to capture any events missed by the primary case definition, we included events for which dispatch reported stroke to the responding EMS unit and then repeated analyses to investigate the sensitivity of results to differences in case definition. We also conducted analyses only among events with documented use of a stroke protocol, presumably restricting to just those in which EMS personnel used the protocol to direct patient care.
RESULTS
Descriptive Characteristics
Of the 100 NC EMS systems, 2 provided basic life support only whereas the remaining provided all or some advanced life support. Annual patient volume widely varied by system (median 8,004; interquartile range 3,754-17,848), and 40 of 100 EMS systems served metropolitan counties. In 2009, NC EMS systems varied in their stroke protocols: 23 were classified as having no instructions regarding scene time; 73 classified as having general instructions to minimize scene time; and 4 classified as having a specific limit for scene time (3 used 10 min and 1 used 15 min). Of the systems that had a stroke protocol with a specific time limit, all used only paid EMS personnel and first responders to arrive before EMS. Most (3 systems) had at least 5,000 patient encounters per year and served metropolitan areas. Overall, systems with protocols with a specific time limit, compared to general only or no instructions, were more likely to have larger patient volumes, serve metropolitan areas, and use paid EMS personnel and first responders.
In the PreMIS database, we identified 96,688 records for a 9-1-1 response within a NC EMS system occurring in 2009 in which the patient had a possible neurological condition (Figure 1). Of these, 10,155 events had a documented impression of stroke or a stroke protocol used. Three hundred ninety-nine (4%) events were excluded if either the date and time of EMS unit arriving on scene or unit left scene with patient was missing, and 33 (0.3%) were excluded for invalid or extreme scene times, resulting in 9,723 eligible suspected stroke events for the main analysis.
Figure 1.
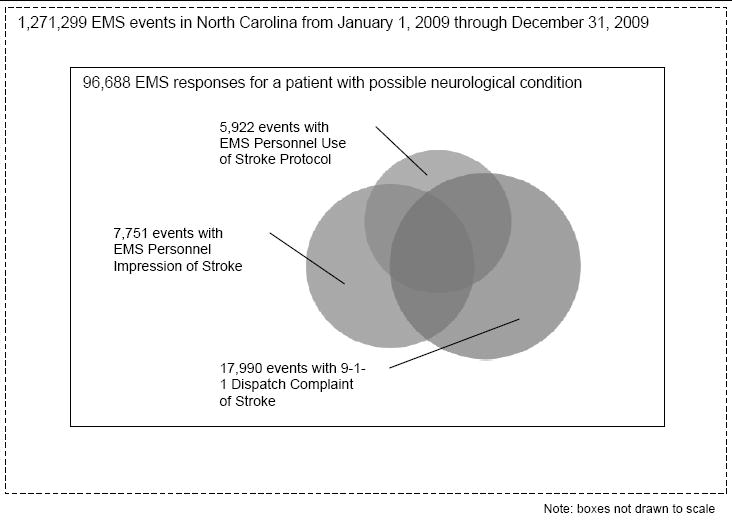
Diagram of suspected stroke events in the Prehospital Medical Information System, North Carolina, 2009. There were a total of 22,789 events having a stroke 9-1-1 dispatch complaint, EMS personnel impression, or protocol use, of which 10,155 had stroke impression or protocol use.
There were 86 EMS systems represented in this analysis (Table 1). No eligible suspected stroke events were identified from the other 14 NC EMS systems either due to no occurrences within the time period or incomplete data in PreMIS. Only 4 systems were found to have a specific limit for scene time provided in the stroke protocol although these 4 systems accounted for 18% of the eligible suspected stroke events for this study. The mean scene time was 15.9 min (standard deviation 6.9 min), and median scene time was 15.0 min (interquartile range 11.0-19.5 min). The 90th percentile was 24.3 min and well exceeded the 15-min benchmark. The median and 90% percentile scene times for systems with stroke protocols with a specific time limit were about 2-3 minutes shorter when compared to both general only and no instructions. General and no instructions had roughly equivalent scene time distributions. While there were minimal differences by system patient volume, metropolitan systems had about 2-min shorter scene times.
Table 1.
Distribution of Scene Times by Stroke Protocol Instructions and Other Covariates (N=9,723 stroke events), Prehospital Medical Information System, North Carolina, 2009
| Number of EMS Systems | Number of Stroke Events | Scene Time (in minutes) | ||
|---|---|---|---|---|
| Mean (Standard Deviation) | Median (90th Percentile) | |||
| Protocol Instructions on Scene Time | ||||
| Specific Time Limit | 4 | 1,728 | 14.3 (5.9) | 13.6 (22.0) |
| General Instructions | 63 | 5,146 | 16.2 (7.2) | 15.0 (25.0) |
| None | 19 | 2,849 | 16.2 (6.8) | 15.3 (24.6) |
| Annual Patient Volume | ||||
| >20,000 | 18 | 4,987 | 15.8 (6.9) | 15.0 (24.0) |
| 5,000-20,000 | 40 | 3,608 | 15.8 (6.9) | 15.0 (25.0) |
| <5,000 | 28 | 1,128 | 16.4 (7.7) | 16.0 (25.0) |
| Metropolitan Status | ||||
| Yes | 34 | 6,518 | 15.4 (6.6) | 14.4 (23.7) |
| No | 52 | 3,205 | 16.8 (7.5) | 16.0 (26.0) |
Adjusted Associations
After adjusting for annual patient volume and metropolitan status, systems having stroke protocols with a specific time limit (versus no instructions) remained associated with shorter scene times across the range of percentiles estimated (Table 2, Figure 2). The most pronounced quantile regression estimate was at the 90th percentile (-2.2 min, 95% CI -3.1 to - 1.3 min), meaning the greatest scene time for 90% of stroke patients was 2-min less if there was a specific time limit provided as opposed to no instructions. Quantile regression estimates comparing general to no instructions remained close to the null value. Ordinary least squares regression estimates were similar to the 50th percentile estimates.
Table 2.
Adjusted* Associations of Stroke Protocol Instructions and Scene Times (N=9,723)
| Protocol Instructions on Scene Time | Quantile Regression Estimates (95% CI)
|
OLS Estimates (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|
| 10th Percentile | 50th Percentile | 90th Percentile | ||||||
| Specific Time Limit | -1.3 | (-1.6, -0.9) | -1.5 | (-2.1, -1.0) | -2.2 | (-3.1, -1.3) | -1.9 | (-2.9, -0.8) |
| General Instructions | -0.1 | (-0.4, 0.2) | 0.0 | (-0.4, 0.3) | 0.7 | (-0.2, 1.5) | 0.0 | (-1.2, 1.2) |
| None (referent) | 0 | --- | 0 | --- | 0 | --- | 0 | --- |
Models adjusted for system-level annual patient volume and metropolitan status
CI = confidence interval; OLS = ordinary least squares
Figure 2.
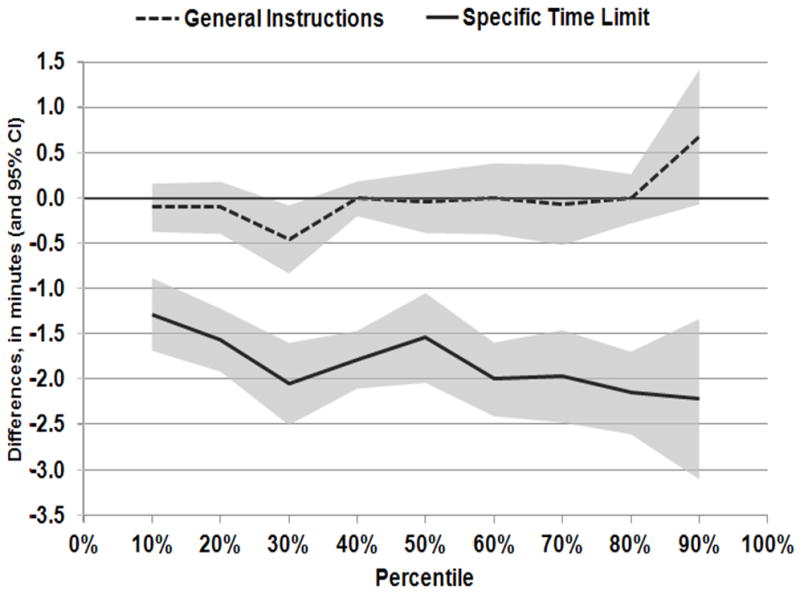
Adjusted differences in scene time for suspected stroke by protocol instructions, Prehospital Medical Information System, North Carolina, 2009. Quantile regression estimates (in minutes) across 10th to 90th percentiles were adjusted for system annual patient volume and metropolitan status. Solid line: point estimates of specific time limit versus none. Dotted line: point estimates of general instructions versus none. Shaded areas: 95% confidence intervals. Reference line: null values.
In the subgroup analysis within high patient volume and metropolitan EMS systems, we observed a similar magnitude for the 90th percentile comparison of specific time limit and no instructions (-2.5 min, 95% CI -3.5 to -1.4 min) while the comparison of general to no instructions was substantially greater than the null (2.0 min, 95% CI 0.9 to 3.1 min), suggesting that having general instructions as opposed to none in the protocol has longer scene times for stroke patients in this subpopulation.
Sensitivity Analysis
Our primary case definition resulted in 9,723 eligible suspected stroke events (Table 3). The inclusion of dispatch complaints of stroke resulted in 20,750 total eligible events. Among this larger group, the association of specific time limit to no instructions was still negative though attenuated (-1.7 min, 95% CI -2.5 to -1.0). In addition, when we restricted to only those eligible events in which a stroke protocol was used (N=5,740), the specific time limit association was very similar (-2.1 min, 95% CI -3.1 to -1.0 min); however, general instruction (versus none) was now associated with shorter scene time, though weakly (-1.0 min, 95% CI -2.1 to 0.1 min). Overall, the sensitivity of these results to differences in case definition appears minimal.
Table 3.
Adjusted Differences in 90th Percentile Scene Time by Case Definitions of Suspected Stroke Events in the Prehospital Medical Information System, North Carolina, 2009
| Case Definition | Eligible Events (N) | Regression Estimate (95% Confidence Interval) | |
|---|---|---|---|
| Protocol Instructions on Scene Time | |||
| 1) Stroke Impression or Protocol | 9,723 | ||
| Specific Time Limit | -2.2 | (-3.1, -1.3) | |
| General Instructions | 0.7 | (-0.2, 1.5) | |
| None (referent) | 0 | --- | |
| 2) Stroke Impression, Protocol, or Dispatch Complaint | 20,750 | ||
| Specific Time Limit | -1.7 | (-2.5, -1.0) | |
| General Instructions | 0.0 | (-0.6, 0.6) | |
| None (referent) | 0 | --- | |
| 3) Stroke Protocol | 5,740 | ||
| Specific Time Limit | -2.1 | (-3.1, -1.0) | |
| General Instructions | -1.0 | (-2.1, 0.1) | |
| None (referent) | 0 | --- | |
DISCUSSION
In this study of suspected stroke events, we found a 2.2-min reduction in 90th percentile scene times for stroke patients in EMS systems having stroke protocols with a specific time limit compared to protocols with no instructions on scene time. No significant difference in scene time was detected in EMS systems with general protocol instructions compared to none. While a 2.2-min reduction in the 90th percentile scene time makes up only 9% of the 24.6-min scene time among no protocol instructions, the percentage of the modifiable scene time would be greater because there is always a minimum amount of time needed to, for example, access and load the patient.20 Moreover, we believe lower scene time represents a heightened sense of urgency in EMS personnel, which could have a cascading effect on the transport time and perhaps even emergency department processing times. In fact, previous research on EMS responses for trauma showed a strong correlation between scene time and transport time.21 Additionally, a study of acute myocardial infarction patients found achieving benchmarks for EMS response, scene, and transport times was associated with reduced time to reperfusion.22 Similar studies of prehospital time intervals and stroke treatment would be informative.
Our findings highlight the importance of detailed protocols for the prehospital care and management of stroke patients. Since use of EMS protocols provide some assurance of best medical practices and appropriate delivery of care, additional studies are needed to provide information to guide their development and implementation. To our knowledge, no previous studies have estimated the effect of stroke protocols on reducing scene time. There have been limited studies on the impact of interventions to minimize EMS scene times for patients with stroke. The Houston Paramedic and Emergency Stroke Outcomes (HoPSTO) study, an educational intervention to improve EMS and hospital stroke care, found mean scene times for suspected stroke patients unexpectedly increased from 16.7 to 18.2 min after training in prehospital stroke identification.23 Frendl, et al. trained EMS personnel on prehospital stroke screening and observed a moderate decrease in mean scene time (19 versus 17 min).24 These studies simply compared mean scene times and, thus, may have missed important differences that are detectable using quantile regression methods.25,26
The average scene time in our study is comparable to previous reports from the US, which range from 13 to 20 min.23,24,27-32 Notably, only 50% of suspected stroke events had a scene time of 15 min or less, whereas the benchmark is at least 90% of stroke patients. Starting in 2010, the NC regulatory office of EMS mandated the use of standardized protocols throughout the state, of which the stroke protocol (available at http://www.ncems.org/pdf/Pro33-SuspectedStroke.pdf) specifically instructs responders to limit scene time to 10 minutes. However, we found only 4% of NC EMS systems in 2009 provided specific time limits in their stroke protocols. According to a 2008 survey of EMS agencies in 9 states, 81% of respondents reported their agencies had an on-scene time limit for responding to stroke patients,11 though this study did not objectively assess protocols. Nonetheless, there still remain opportunities to improve EMS scene times for stroke, perhaps through protocol development and implementation at the agency or state level.
Since a statewide shift to standardized protocols took place at the beginning of 2010, we were concerned that some systems classified as having general only or no instructions, based on protocols at the start of 2009, may have switched to the state protocol at some point in the year. Since protocol misclassification was more likely at the near the end of 2009, we repeated analyses stratified by calendar year quarter (e.g. first quarter represents events occurring in January through March). Associations among stroke events occurring in the first quarter of 2009 were similar to overall associations, whereas the weakest association between a specific time limit and no instruction was observed during the last quarter. This attenuation suggests systems could have adopted the new protocol during the time range of this study.
A major strength of this study was the use of existing data from a geographic region with both urban and rural areas. While we evaluated a single state, most previous studies of EMS scene times for stroke have focused solely on local, mostly metropolitan regions.23,30,31 We were able to adjust for volume and population density of the EMS system, though our sample size was limited by the presence of only 4 systems with specific scene time limits on their protocols, in which most suspected stroke events were from high volume and metropolitan systems. Within this subpopulation, the association of specific time limits on minimizing scene time remained similar to the overall association.
Unlike previous studies using patients with a final hospital diagnosis of stroke, our study population was composed of patients with a prehospital impression of stroke. Although a number of these would not have had a stroke diagnosis, they are relevant to the study of prehospital stroke care since they should be managed like a stroke by EMS personnel, if only to be later ruled out. Although ASA guidelines emphasize EMS rapid response for the early management of ischemic stroke patients,3 EMS time benchmarks for stroke systems of care do not specify stroke subtype(s),10 as the accurate identification of stroke subtype requires brain imaging. To our knowledge, this is the largest study to date of EMS scene times for stroke, which was made possible by the availability of electronic records on EMS events across NC. We previously noted missing data in PreMIS as a major limitation. For key elements (i.e. personnel’s impression and protocols used) needed to identify suspected stroke events, data were missing for almost one-third of records. In sensitivity analyses, we varied the case definition to include more events, and while the magnitude of estimates changed, the major findings remained the same. Another limitation of identifying suspected stroke is the variability in how EMS personnel arrived to an impression of stroke or decided to use a stroke protocol. The usage and results for prehospital stroke assessment tools are not well-documented in these data, and differences in knowledge and practices between EMS systems may influence estimates. Completeness and quality of scene time data were less of a concern. We had to exclude only 4% of events due to missing or invalid times, which was better than a previous study of electronic EMS records, in which only 70% of suspected stroke events could had sufficient information to calculate scene time.32 In addition to state and system efforts to ensure that electronic EMS records are collected accurately and completely, we recommend further research on the implications of data completeness and quality.
We used 2 independent reviewers and an expert adjudicator to classify systems by their stroke protocol instructions regarding scene time, if any, at a given time. However, we were not able to assess changes in protocols prior to this time or during the study period. The main association of shorter scene times for systems with protocols specifying time limits compared to those systems with no protocol instructions could be explained by the influence of extraneous factors on EMS system protocols and personnel response times. Upon further adjustment of models with patient (i.e. age, sex, race) and event (i.e. time of day, day of week, response with lights and sirens, location) characteristics, associations were slightly attenuated yet remained significant. Data on other potentially influential individual-level factors, like patient status and procedures performed by EMS, were not sufficiently recorded in the database to allow for inclusion in multivariable models. Lastly, we did not control for other potentially confounding system-level factors, such as the role of emergency medical dispatch and medical direction,11,30 but given the amount standardization across NC, we suspect these influences to be minor.
CONCLUSION
In this statewide analysis, EMS personnel spent at most 24 min with 90% of suspected stroke patients before commencing transport to the hospital. We estimated a roughly 2-min reduction among EMS systems that stated a specific time limit on the suspected stroke patient care protocol, even compared to systems with general instructions to minimize scene time. Our findings suggest that systems can modestly improve scene times by specifying a limit in their patient care protocols. Moreover, these improvements may be markers of a greater sense of urgency among EMS personnel when responding to stroke. Additional studies, ideally experimental, are needed to study the effect of system protocols on EMS response times. Furthermore, evidence of EMS impact on stroke patient outcomes is needed to determine the clinical relevance of EMS stroke care performance.
Acknowledgments
This research received no specific funding support. The NC Office of EMS and the NC EMS Data System support state, regional and local EMS and healthcare related service delivery from a patient care, resource allocation, and regulatory perspective. This manuscript was not prepared in collaboration with investigators of the NC EMS Data System and does not necessarily reflect the opinions or views of the NC Office of EMS, EMS Performance Improvement Center or the study sites participating in the NC EMS Data System.
Footnotes
DECLARATION OF INTEREST
The authors have no conflicts of interest to disclose.
References
- 1.Saver JL. Time is brain—quantified. Stroke. 2006;37(1):263–266. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]
- 2.Saver JL. The 2012 Feinberg lecture treatment swift and treatment sure. Stroke. 2013;44(1):270–277. doi: 10.1161/STROKEAHA.112.671354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jauch EC, Saver JL, Adams HP, Bruno A, Connors JJ, Demaerschalk BM, Khatri P, McMullan PW, Qureshi AI, Rosenfield K, Scott PA, Summers DR, Wang DZ, Wintermark M, Yonas H. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 4.Kothari R, Jauch E, Broderick J, Brott T, Sauerbeck L, Khoury J, Liu T. Acute stroke: Delays to presentation and emergency department evaluation. Ann Emerg Med. 1999;33:3–8. doi: 10.1016/s0196-0644(99)70431-2. [DOI] [PubMed] [Google Scholar]
- 5.Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S. Prehospital and emergency department delays after acute stroke: The Genentech stroke presentation survey. Stroke. 2000;31(11):2585–2590. doi: 10.1161/01.str.31.11.2585. [DOI] [PubMed] [Google Scholar]
- 6.Lacy CR, Suh DC, Bueno M, Kostis JB. Delay in presentation and evaluation for acute stroke stroke time registry for outcomes knowledge and epidemiology (STROKE) Stroke. 2001;32(1):63–69. doi: 10.1161/01.str.32.1.63. [DOI] [PubMed] [Google Scholar]
- 7.Katzan IL, Graber TM, Furlan AJ, Sundararajan S, Sila CA, Houser G, Landis DM. Cuyahoga county operation stroke speed of emergency department evaluation and compliance with National Institutes of Neurological Disorders and Stroke time targets. Stroke. 2003;34(4):994–998. doi: 10.1161/01.STR.0000060870.55480.61. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Prehospital and hospital delays after stroke onset--United States, 2005-2006. MMWR Morb Mortal Wkly Rep. 2007;56(19):474–478. [PubMed] [Google Scholar]
- 9.Rose KM, Rosamond WD, Huston SL, Murphy CV, Tegeler CH. Predictors of time from hospital arrival to initial brain imaging among suspected stroke patients the North Carolina Collaborative Stroke Registry. Stroke. 2008;39(12):3262–3267. doi: 10.1161/STROKEAHA.108.524686. [DOI] [PubMed] [Google Scholar]
- 10.Acker JE, III, Pancioli AM, Crocco TJ, et al. Implementation strategies for emergency medical services within stroke systems of care: A policy statement from the American Heart Association/American Stroke Association expert panel on emergency medical services systems and the stroke council. Stroke. 2007;38(11):3097–3115. doi: 10.1161/STROKEAHA.107.186094. [DOI] [PubMed] [Google Scholar]
- 11.Greer S, Williams I, Valderrama AL, Bolton P, Patterson DG, Zhang Z. EMS medical direction and prehospital practices for acute cardiovascular events. Prehosp Emerg Care. 2012 doi: 10.3109/10903127.2012.710718. [DOI] [PubMed] [Google Scholar]
- 12.Mears GD, Pratt D, Glickman SW, et al. The north carolina EMS data system: A comprehensive integrated emergency medical services quality improvement program. Prehosp Emerg Care. 2010;14(1):85–94. doi: 10.3109/10903120903349846. [DOI] [PubMed] [Google Scholar]
- 13.Credentialing Information System (CIS) Chapel Hill (NC): EMS Performance Improvement Center, North Carolina Office of EMS; [March 15, 2012]. https://www.emspic.org/applications/cis. [Google Scholar]
- 14.US Office of Management and Budget. Update of Statistical Area Definitions and Guidance on Their Uses. Washington (DC): Executive Office of the President; 2009. [August 4, 2012]. http://www.whitehouse.gov/sites/default/files/omb/assets/bulletins/b10-02.pdf. [Google Scholar]
- 15.Prehospital Medical Information (PreMIS) Chapel Hill (NC): EMS Performance Improvement Center, North Carolina Office of EMS; [September 6, 2011]. https://www.emspic.org/applications/premis. [Google Scholar]
- 16.National EMS Information System (NEMSIS) [April 15, 2013]; http://www.nemsis.org.
- 17.Williams I, Mears G, Wilson J, Raisor C. An emergency medical services toolkit for improving systems of care for stroke in North Carolina. Prev Chron Dis. 2009;6(2) [PMC free article] [PubMed] [Google Scholar]
- 18.Koenker R, Bassett G., Jr Regression quantiles. Econometrica: journal of the Econometric Society. 1978:33–50. [Google Scholar]
- 19.Karmarkar N. A new polynomial-time algorithm for linear programming. Proceedings of the sixteenth annual ACM symposium on Theory of computing; 1984. pp. 302–311. [Google Scholar]
- 20.Honigman B, Rehweder K, Moore EE, Lowenstein SR, Pons PT. Prehospital advanced trauma life support for penetrating cardiac wounds. Ann Emerg Med. 1990;19(2):145–150. doi: 10.1016/s0196-0644(05)81799-8. [DOI] [PubMed] [Google Scholar]
- 21.Hedges JR, Feero S, Moore B, Shultz B, Haver DW. Factors contributing to paramedic onscene time during evaluation and management of blunt trauma. Am J Emerg Med. 1988;6(5):443–448. doi: 10.1016/0735-6757(88)90242-2. [DOI] [PubMed] [Google Scholar]
- 22.Studnek JR, Garvey L, Blackwell T, Vandeventer S, Ward SR. Association between prehospital time intervals and ST-elevation myocardial infarction system performance. Circulation. 2010;122(15):1464–1469. doi: 10.1161/CIRCULATIONAHA.109.931154. [DOI] [PubMed] [Google Scholar]
- 23.Wojner-Alexandrov AW, Alexandrov AV, Rodriguez D, Persse D, Grotta JC. Houston paramedic and emergency stroke treatment and outcomes study (HoPSTO) Stroke. 2005;36(7):1512–1518. doi: 10.1161/01.STR.0000170700.45340.39. [DOI] [PubMed] [Google Scholar]
- 24.Frendl DM, Strauss DG, Underhill BK, Goldstein LB. Lack of impact of paramedic training and use of the cincinnati prehospital stroke scale on stroke patient identification and onscene time. Stroke. 2009;40(3):754–756. doi: 10.1161/STROKEAHA.108.531285. [DOI] [PubMed] [Google Scholar]
- 25.Austin PC, Schull MJ. Quantile regression: A statistical tool for out-of-hospital research. Acad Emerg Med. 2003;10(7):789–797. doi: 10.1111/j.1553-2712.2003.tb00075.x. [DOI] [PubMed] [Google Scholar]
- 26.Do YK, Foo K, Ng YY, Ong MEH. A quantile regression analysis of ambulance response time. Prehosp Emerg Care. 2012;17(2):170–6. doi: 10.3109/10903127.2012.729127. [DOI] [PubMed] [Google Scholar]
- 27.Evenson KR, Schroeder EB, Legare TB, Brice JH, Rosamond WD, Morris DL. A comparison of emergency medical services times for stroke and myocardial infarction. Prehosp Emerg Care. 2001;5(4):335–339. doi: 10.1080/10903120190939463. [DOI] [PubMed] [Google Scholar]
- 28.Wojner AW, Morgenstern L, Alexandrov AV, Rodriguez D, Persse D, Grotta JC. Paramedic and emergency department care of stroke: Baseline data from a citywide performance improvement study. Am J Crit Care. 2003;12(5):411–417. [PubMed] [Google Scholar]
- 29.Rosamond WD, Evenson KR, Schroeder EB, Morris DL, Johnson AM, Brice JH. Calling emergency medical services for acute stroke: A study of 9-1-1 tapes. Prehosp Emerg Care. 2005;9(1):19–23. doi: 10.1080/10903120590891985. [DOI] [PubMed] [Google Scholar]
- 30.Kleindorfer DO, Lindsell CJ, Broderick JP, et al. Community socioeconomic status and prehospital times in acute stroke and transient ischemic attack: Do poorer patients have longer delays from 911 call to the emergency department? Stroke. 2006;37(6):1508–1513. doi: 10.1161/01.STR.0000222933.94460.dd. [DOI] [PubMed] [Google Scholar]
- 31.Ramanujam P, Castillo E, Patel E, Vilke G, Wilson MP, Dunford JV. Prehospital transport time intervals for acute stroke patients. J Emerg Med. 2009;37(1):40–45. doi: 10.1016/j.jemermed.2007.11.092. [DOI] [PubMed] [Google Scholar]
- 32.Shaeffer Z, Gohdes D, Legler J, Taillac P, Larsen B. Monitoring prehospital stroke care in utah to assess the feasibility of using EMS data for surveillance. Prev Chronic Dis. 2009;6(4):A137. [PMC free article] [PubMed] [Google Scholar]


