Abstract
Objectives
To determine the extent to which the impact of obesity on disability and physical function is mediated by bodily pain.
Design
Cross-sectional analysis
Setting
Population-based sample of residents in the Greater Boson area
Participants
736 community-dwelling adults, aged 70 years and older
Measurements
Weight status, obtained from measured height and weight, was categorized: normal weight – BMI 19–25 kg/m2, overweight – BMI 25–29.9 kg/m2, obese – BMI ≥30 kg/m.2 Main outcome measures were the Physical Component Score of the SF12 (PCS), activities of daily living (ADL) disability and Short Physical Performance Battery score (SPPB). Chronic pain was assessed as the number of weight-bearing joint pain sites (hips, knees, feet and pain all over).
Results
Older, obese adults had greater ADL disability and lower SPPB and PCS scores compared with their non-obese counterparts. However in sex-stratified adjusted analyses, obesity was adversely associated with outcomes only in women. Obesity was associated with greater number of pain sites; and lower body pain was associated with greater odds of disability. Mediation analysis suggests that pain is a significant mediator (22% to 44%) of the adverse impact of obesity on disability and physical function in women.
Conclusion
Bodily pain may be an important, treatable mediator of the adverse impact of obesity on disability and physical function in women.
Keywords: Obesity, physical function, pain, disability
INTRODUCTION
It is estimated that 37% of men and 34% of women aged 60 years and older are obese.1 The high prevalence of obesity in older adults is concerning as obesity is associated with a number of adverse health outcomes, including physical disability.2–5 Physical disability is a substantial public health issue for the older adult population. Disability is associated with increased mortality, lower quality of life, lower family resources, loss of independence and increased health care costs.6,7 The hazard of physical disability is particularly relevant in older populations as the risk of functional problems increases with advancing age.
Several prior studies have demonstrated an association of obesity with increased future risk of physical disability.5,8–10 However, the pathways linking obesity with increased disability are not entirely understood. Obesity is associated with increased risk of several medical conditions, such as diabetes, cardiovascular disease and lower extremity osteoarthritis, which could be contributing factors in the development of physical disability associated with obesity. Obesity may also induce biomechanical stresses that lead to mobility difficulties.11–13 Another factor that could partially mediate the adverse impact of obesity on physical function is bodily pain. Previous work has suggested that obese persons could be disproportionately affected by pain, both pain related to osteoarthritis as well as and non-arthritic pain.14,15 The extent to which pain may contribute to obesity-related physical disability is not known. If pain is a significant mediator of obesity-related disability and poorer physical function in older adults, then pain management might be an effective target to mitigate this problem.
The intersection of the aging of the U.S population with the currently high prevalence of obesity means that research elucidating mechanisms linking obesity and disability and that helps to identify populations at highest risk for obesity-related disability, will be critically important for the development of effective public health and clinical management strategies to reduce disability in older adults. The objectives of our study were to understand how pain may mediate the association of obesity with physical disability, performance and function. We hypothesized that pain would partially mediate any observed relationship between obesity and poorer physical function and disability.
METHODS
Study population
We used data from the MOBILIZE Boston Study (MBS), a population-based study of older persons residing in the Boston area. MBS is a National Institute of Aging funded study with the primary aim of identifying novel risk factors for falls in the elderly.16 Eligible participants were 70 years and older, living within a five mile radius of the study’s coordinating center, the Institute for Aging Research, Hebrew SeniorLife, Boston, Massachusetts. Spouses or companions aged 64 or older of participants were also eligible to join the study. The study was initiated in 2005 with 765 people enrolled at baseline. Participants underwent baseline assessments both, at their own home and also at a clinical research center located at the Institute for Aging Research. Together, these baseline assessments collected information related to a number of domains including demographics, health measures, and measured and self assessed physical and mental functioning. For this cross-sectional analysis, we used the baseline assessment data. Participants eligible for our study had weight and height data available at baseline. (n=744) We excluded 8 participants with very low BMI (<19), because these seniors were thought more likely to have complex health problems that might complicate our observation of the relationships of interest; therefore our analytic sample included 736 participants.
Disability and Physical Performance
We used three outcome measures of disability and physical function. Activities of daily living (ADL), are considered basic self care activities.17 ADLs measured in MBS were bathing, dressing, transferring, using the toilet, and eating. Participants were asked to identify their level of difficulty performing each ADL by responding with one of the following options: no difficulty, a little difficulty, a lot of difficulty or inability to perform. In our analysis, participants who reported any difficulty or inability to perform any of the five ADLs were classified as having ADL disability and all others were classified as not having ADL disability (dichotomous variable).
The Short Physical Performance Battery (SPPB) is a commonly used instrument to measure lower extremity mobility performance.18 The SPPB includes tests of standing balance, 4-meter usual-paced walking speed, and ability and time to rise from a chair 5 times. Participant performance on each of these three maneuvers is graded categorically on a scale of 1 to 4; inability to perform any of the maneuvers results in a score of 0. Thus, summary scores for the SPPB range from 0 to 12; SPPB was analyzed as a continuous variable.
The third functional outcome was the Physical Component Score (PCS), of the Short Form -12 (SF-12).19 The SF-12 is a well validated, multipurpose short form survey with 12 questions that measure eight domains of health. The PCS measures physical health, including physical functioning and evaluation of the ability to perform physical activity. PCS is derived from all eight health domains measures in the SF-12; scores are calibrated such that 50 is the average score or norm and the standard deviation is 10. This measure was included in our analyses as a continuous measure.
Weight status
Weight was measured without shoes using a calibrated balance beam scale; height was measured without shoes using a stadiometer. Body mass index (BMI) was calculated as weight in kilograms divided by height in squared meters. BMI was then analyzed in three categories in accordance with the classification schema proposed by the NIH20: normal weight – BMI 19–24.9 kg/m2, overweight – BMI 25–29.9 kg/m2, obese - BMI ≥30 kg/m.2
Pain
Pain was assessed using the joint pain questionnaire from the Women’s Health and Aging Study, assessing presence of chronic pain in musculoskeletal sites.21 For the purposes of the present analysis, we were interested in pain in weight-bearing joints (hips, knees, feet) and widespread pain, as we felt that pain symptoms in these areas would be more likely to be related to obesity and contribute to disability. Participants were asked whether they had pain in their hips, knees, feet or all-over on most days for at least 3 months of the previous year. They were also asked whether they had bodily pain (any location) within the past month. We combined the responses to these questions to categorize pain. If a participant responded that they had pain in a given bodily location on most days in the past three months and also had bodily pain within the past month, they were classified as having chronic pain in that location. We then counted the number of weight-bearing sites a participant noted having pain. For example, if a participant had pain in their hips and knees, they had two pain sites. If a participant reported pain in all three bodily locations or had all-over pain, they had three or more pain sites. Number of pain sites was used in our main analysis. In secondary analyses, we separately analyzed the effect of pain intensity using the 4-item Brief Pain Inventory (BPI) which has been validated for use in musculoskeletal pain.22
Statistical analysis
We used descriptive statistics to characterize participant’s demographic and clinical characteristics at baseline. Descriptive statistics were also used to examine the unadjusted relationship between weight status and both disability and physical function, as well as with pain prevalence.
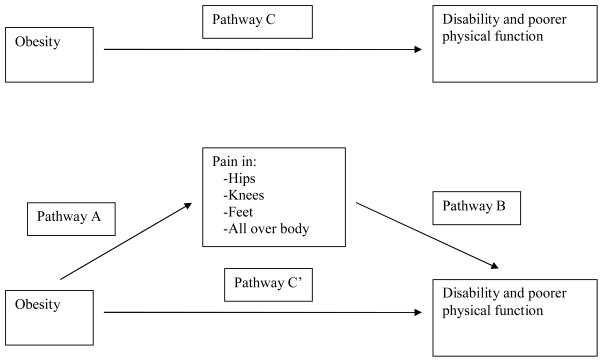
We then conducted a mediation analysis to understand how much of the measured effect of the independent variable (obesity) on the dependent variables (physical performance/function/disability) is attributable to a potential mediator variable (pain). In this model (Figure 1), the observed effect of the independent variable on the dependent variable is called the total effect (pathway C). The total effects are comprised of a direct effect pathway (pathway C’) of the independent variable on the dependent variable, and a total indirect pathway (mediated: pathway A + B) of the independent variable on the dependent variable through the mediator. We approached this mediation analysis using two methods. The Baron and Kenny proposed a four step approach in which several regression analyses are conducted and the relevant coefficients are examined at each step.23 Using the Baron and Kenny method, mediation can be said to be present when the following conditions hold in sequential regression analyses: 1) The independent variable (obesity) is associated with the dependent variable (physical performance/function/disability) in the absence of the putative mediator variable (pain);.2) The independent variable (obesity) is associated with the mediator variable (pain); 3) The mediator (number of pain sites) is associated with the dependent variable (physical performance/function/disability); 4) the observed effect of the independent variable on the outcome shrinks when the mediator is added to the model. Full mediation occurs if inclusion of the mediation variable shrinks the observed relationship between the independent variable and dependent variable to zero. However, full mediation rarely occurs. Partial mediation occurs when the observed relationship between the independent and dependent variable is weaker with the inclusion of the mediation effect. The multivariable regression models used for these analyses were logistic regression for dichotomous outcomes (i.e. ADL disability) and linear regression for continuous outcomes (SPPB, PCS scores).
Figure 1.
Model of the Potential Mediating Effect of Pain on the Relationship between Obesity and Disability and Poorer Physical Function
We also used statistically based methods to asses for statistical significance of the mediation pathway.24 We used a series of regression modeling to estimate the coefficient for the indirect effect by calculating the product of the standardized regression coefficient (path A) of the independent variable on the mediator with the regression coefficient (path B) of the mediator variable on the dependent variable (A * B). Thus, the regression coefficient for the indirect effect represents the change in the dependent variable for every unit change in the independent variable that is mediated by the mediator. Bootstrapping methods were used to calculate the 95% confidence intervals for the coefficients for the total, indirect, and direct effect.21 Coefficients were considered statistically significant if the confidence intervals did not cross zero.
We conducted analyses stratified by sex, as prior research suggests that the effects of obesity on disability and physical function may vary with sex. Final models controlled for covariates that could confound the relationship between obesity and disability including age, sex, race (black, white), education level (less than high school, high school completion, more than high school), smoking status (never, former, current), physical activity (Physical Activity Scale for the Elderly, continuous) and self-reported physician diagnosis of chronic medical conditions, including diabetes, heart disease, congestive heart failure, hypertension and stroke (yes/no).
All analyses were conducted using Stata v12.
RESULTS
Forty percent of our sample was overweight and 29% were obese. Obese participants were more likely to be female, Black and with less education. (Table 1) Overweight and obese participants were also more likely to have medical morbidities such as diabetes, hypertension and stroke. The number of lower body joint pain sites increased across weight categories with obese persons reporting more sites of pain.
Table 1.
Baseline Characteristics According to Body-Mass Index Categories
| All N=736 |
Normal weight N=231 |
Overweight N=291 |
Obese N=214 |
P value | |
|---|---|---|---|---|---|
|
Demographic/clinical characteristics
| |||||
| Age – mean (sd) | 78.1 (5.4) | 78.6 (5.7) | 78.1 (5.6) | 77.5 (4.9) | 0.105 |
| Female (%) | 64 | 64 | 56.7 | 72.9 | <0.005 |
| Race | |||||
| White (%) | 77 | 83 | 78 | 70 | 0.011 |
| Black (%) | 17 | 11 | 16 | 23 | |
| Other (%) | 6 | 6 | 6 | 7 | |
| Education level | |||||
| Less than HS (%) | 11 | 9 | 12 | 13 | 0.100 |
| HS (%) | 23 | 23 | 19 | 28 | |
| More than HS (%) | 66 | 68 | 69 | 60 | |
| Smoking status | |||||
| Never (%) | 44 | 44 | 45 | 44 | 0.122 |
| Former (%) | 51 | 48 | 52. | 53 | |
| Current (%) | 5 | 8 | 3 | 4 | |
| Physical Activity (SD) | 107 (70) | 112 (72) | 112 (76) | 96 (58) | <0.005 |
| Self report of: | |||||
| Hypertension (%) | 62 | 53 | 63 | 70 | <0.005 |
| Diabetes (%) | 19 | 12 | 19 | 26 | <0.005 |
| Heart disease (%) | 26 | 24 | 28 | 26 | 0.651 |
| CHF (%)* | 5 | 4 | 5 | 6 | 0.565 |
| Stroke (%) | 10 | 7 | 8 | 15 | 0.003 |
|
| |||||
|
Disability/Physical performance measures
| |||||
| ADL Disability (%) | 20 | 18 | 20 | 29 | <0.005 |
| PCS [mean (sd)] | 46.4 (10.1) | 47.9 (10.2) | 47.2 (9.7) | 43.7 (10.0) | <0.005 |
| SPPB [ mean (sd)] | 9.3 (2.5) | 9.7 (2.3) | 9.4 (2.4) | 8.9 (2.7) | <0.005 |
|
| |||||
|
Pain prevalence by number of sites
| |||||
| No pain | 55 | 65 | 55 | 45 | <0.005 |
| One site of pain | 29 | 25 | 30 | 33 | |
| Two sites of pain | 12 | 8 | 11 | 17 | |
| Three or more sites of pain | 4 | 2 | 4 | 5 | |
Congestive Heart Failure
Activities of Daily Living - bathing, dressing, transferring, using the toilet, and eating
Physical Component Score (Short form-12) – mean score 50, standard deviation 10
Short Physical Performance Battery – scores from 0 to 12 (12 is the best)
We first used the Baron and Kenny method of sequential regression modeling to assess for the mediating effect of pain. We found that obesity was associated with each of the three measures of disability/physical performance. Unadjusted results suggested that overweight and obesity were associated with lower PCS and SPPB scores, and higher likelihood of ADL disability compared to the normal weight participants. (Table 1) In adjusted analyses including both men and women, obesity but not overweight, was significantly adversely associated with two of the measures of physical performance, SPPB and PCS. (Table 2) For example, older adults with obesity had mean PCS and SPPB scores that were significantly lower (3 points and 0.6 points respectively) than their normal weight counterparts. However, sex stratified analyses suggest substantial differences according to sex. In both unadjusted and adjusted analyses in men, overweight and obesity had null effect on physical outcomes. For women, obesity, but not overweight, was significantly associated with disability and poor physical function, as measured by all three outcomes in adjusted analyses. (Table 2)
Table 2.
Sequential Multivariable Adjusted† Models of Disability Measures by Weight Status and Sex
| Activities of Daily Living Disability Adjusted odds ratio (95%CI) |
Short Physical Performance Battery Adjusted β coefficient (95%CI) |
Physical Component Score Adjusted β coefficient (95%CI) |
||||
|---|---|---|---|---|---|---|
|
| ||||||
| Men and Women | Without number of pain sites in the model | With number of pain sites in model | Without number of pain sites in the model | With number of pain sites in model | Without number of pain sites in the model | With number of pain sites in model |
| Weight Status | ||||||
| Normal weight | Referent | Referent | Referent | Referent | Referent | Referent |
| Overweight | 0.95 (0.59, 1.55) | 0.78 (0.46, 1.33) | −0.30 (−0.67, 0.06) | −0.22 (0.−58, 0.14) | −0.83 (−2.44, 0.79) | −0.14 (−1.62, 1.34) |
| Obese | 1.54 (0.94, 2.54) | 1.11 (0.63, 1.94) | −0.59 (−0.99, −0.19)* | −0.44 (−0.84, −0.04)* | −2.90(−4.70, −1.10)* | −1.30 (−2.97, 0.38) |
| Number of Pain sites | ||||||
| No pain | - | Referent | - | Referent | - | Referent |
| One site of pain | - | 2.11 (1.29, 3.46)* | - | −0.44 (−0.78, −0.09)* | - | −4.40 (−5.82, −2.98)* |
| Two sites of pain | - | 3.18 (1.71, 5.91)* | - | −0.69 (−1.18, −0.20)* | - | −6.05 (−8.10, −4.00)* |
| Three or more sites of pain | - | 6.46 (2.46, 16.96)* | - | −1.80 (−2.62, −0.98)* | - | −12.48 (−15.99, −8.97)* |
|
| ||||||
| Men | Without number of pain sites in the model | With number of pain sites in model | Without number of pain sites in the model | With number of pain sites in model | Without number of pain sites in the model | With number of pain sites in model |
|
| ||||||
| Weight Status | ||||||
| Normal weight | Referent | Referent | Referent | Referent | Referent | Referent |
| Overweight | 0.72 (0.34, 1.54) | 0.56 (0.24, 1.32) | −0.27 (−0.84, 0.29) | −.013 (−0.68, 0.41) | 1.15 (−1.26, 3.55) | 1.68 (−0.59, 3.96) |
| Obese | 0.74 (0.29, 1.86) | 0.65 (0.24, 1.81) | −0.41 (−1.10, 0.27) | −0.44 (−1.10, 0.22) | 0.57 (−2.71, 3.24) | 0.36 (−2.42, 3.14) |
| Number of Pain sites | ||||||
| No pain | - | Referent | - | Referent | - | Referent |
| One site of pain | - | 2.51 (1.08, 5.82)* | - | −0.31 (−0.84, 0.23) | - | −4.03 (−6.71, −2.11)* |
| Two sites of pain | - | 4.89 (1.48, 16.19)* | - | −0.84 (−1.72, 0.05) | - | −4.92 (−8.58, −1.25)* |
| Three or more sites of pain | - | 8.75 (1.53, 49.99)* | - | −1.83 (−3.15, −0.52) | - | −10.81 (−16.74, −4.89)* |
|
| ||||||
| Women | Without number of pain sites in the model | With number of pain sites in model | Without number of pain sites in the model | With number of pain sites in model | Without number of pain sites in the model | With number of pain sites in model |
|
| ||||||
| Weight Status | ||||||
| Normal weight | Referent | Referent | Referent | Referent | Referent | Referent |
| Overweight | 1.10 (0.57, 2.13) | 0.95 (0.46, 1.94) | −0.34 (−0.88, 0.11) | −0.27 (−0.76, 0.21) | −2.04 (−4.22, 0.14) | −1.40 (−3.37, 0.58) |
| Obese | 2.38 (1.27, 4.48)* | 1.69 (0.83, 3.45) | −0.71 (−1.22, −0.20)* | −0.47 (−0.99, −0.06) | −4.49 (−6.78, −2.19)* | −2.25 (−4.39, −0.10)* |
| Number of Pain sites | ||||||
| No pain | - | Referent | - | Referent | - | Referent |
| One site of pain | - | 2.01 (1.06, 3.81)* | - | −0.51 (−0.94, −0.05)* | - | −4.62 (−6.48, −2.77)* |
| Two sites of pain | - | 2.76 (1.27, 5.99)* | - | −0.68 (−1.30, −0.06)* | - | −6.83 (−9.39, −4.27)* |
| Three or more sites of pain | - | 5.13 (1.47, 17.92)* | - | −1.73 (−2.80, −0.65) | - | −12.94 (−17.38, −8.50)* |
Models adjusted for age, sex, race, education, smoking status, physical activity and chronic medical conditions
p<0.05
In the unadjusted analyses, we found that obesity is significantly associated with number of pain sites – greater number of pain sites was associated with greater disability and worse physical functioning. (Table 1) Adjusted analysis for both men and women showed that bodily pain is significantly associated with disability, performance and physical function (Table 2). These associations were similar across sex. The adjusted analyses with models including both weight status and pain, suggest that there is an independent effect of pain on our physical outcomes. (Table 2)
Given that our initial analyses found that obesity was not associated with disability or physical function in men, (Table 2) the first condition of Baron and Kenny mediation was not met in this group. However, for women obesity was significantly associated with disability and poorer function, as measured by all three outcomes, in analyses adjusted for covariates other than pain. When pain is included in these models, the observed impact of obesity on disability and functional outcomes in women shrinks substantially. These data suggest partial mediation of the observed adverse impact of obesity on disability and function in women by bodily pain.
We also used modeling techniques to estimate the coefficient for the indirect effect using the product of standardized coefficients and to estimate how much of the total effect of obesity is mediated by bodily pain in women only. We found that for each of our measures of disability and physical functioning, the estimate of the coefficient for the indirect effect was statistically significant. (Table 3) Our analyses suggest that bodily pain mediates approximately 22 to 44% of the total observed adverse effect of obesity on disability and physical function in women.
Table 3.
Coefficients and Confidence Intervals for Mediation Analysis in Women† (n=462)
| Outcome Measure |
Total Effect Direct Effect + Indirect Effect |
Direct effect Path C’ |
Indirect effect Path A + Path B |
Percentage of total effect of obesity mediated by pain |
|---|---|---|---|---|
| Activities of Daily Living | 0.17 (0.01, 0.33)* | 0.14 (−0.02, 0.29) | 0.04 (0.01, 0.07)* | 22% |
| Short Physical Performance Battery | −0.08 (−0.17, 0.02) | −0.06 (−0.15, 0.03) | −0.03 (−0.05, −0.01)* | 31% |
| Physical Component Score | −0.12 (−0.21, −0.03)* | −0.07 (−0.15, 0.01) | −0.05 (−0.10, −0.02)* | 44% |
Models adjusted for age, sex, race, education, smoking status, physical activity and chronic medical conditions
p<0.05
In secondary analyses, we examined the potential impact of pain severity (BPI). While pain severity was associated with increased ADL disability and lower PCS scores in women (not men), obesity was not associated with pain severity (data not shown). Thus, in mediation analyses pain severity did not mediate the effect of obesity on any of our outcomes (data not shown). Additionally, we conducted sensitivity analyses employing BMI as a continuous (rather than categorical) measure. While some of the point estimates of effect were modestly different than the estimates from models using BMI in categories, this did not change the interpretation of our results.
DISCUSSION
Physical disability is increasingly recognized as an important adverse outcome of obesity in older adults. Our analysis of a population-based sample of community-dwelling older adults finds that obesity is associated with increased ADL disability and worse physical functioning. We also found that obesity is associated with increased distribution of pain sites. Additionally, pain was found to be independently associated with poorer physical function. Finally, our data suggests that number of pain sites appears to be an important mediator of the association between obesity and poorer physical function in obese, older women, but not obese, older men. Intensity of pain was not associated with weight category and did not mediate the relationship between obesity and physical function or disability.
Only a relatively small number of studies examine factors that may mediate the association of obesity with disability in older adults. The main objective of our study was to understand how pain may mediate the increased risk of disability associated with obesity. Both obesity and disability are complex conditions and thus, the pathogenesis of obesity-related disability is likely to be complex and multifactorial. Obesity leads to chronic medical conditions such as diabetes and coronary artery disease;18–21 these conditions may be mediators of obesity-related disability. Obesity may also cause gait and balance disturbances that lead to mobility difficulties.23,24 Additionally, there is emerging evidence that inflammation associated with the excess adipose tissue of the obese state may lead to muscle and bone loss, thus contributing to functional decline.25,26
We postulated that pain could be an important, under-recognized mechanism by which obesity leads to disability. Examination of prior research supports the framework for our hypothesis. Previous work has demonstrated an association of higher BMI with increased bodily pain, both arthritic and non-arthritic. 22 In one study of middle-aged male military veterans, both overweight and obesity were associated with a significantly higher prevalence of bodily pain.25 Another study of older men and women found that moderate obesity was associated with twice the odds of chronic pain compared to normal weight peers; severely obese subjects had more than four times the odds of having chronic pain.26 Our work also confirms this association between obesity and greater likelihood and distribution of pain. Pain has also been found to be associated with increased risk of developing physical disability in seniors.27,28 A study of community dwelling older adults found that musculoskeletal pain in one or two body areas was associated with a 30% increased risk of mobility limitations; pain in three or more areas was associated with an 80% greater risk of mobility limitations.27 Similarly, another study found that the adjusted risk of developing ADL disability increased significantly by about by 20% for each area of bodily pain reported.29 We observed that up to 44% of the obesity-disability/function relationship could be related to chronic pain in older women. Thus, while the magnitude of the mediating effect of pain on the negative physical outcomes associated with obesity in older women appears substantial, further work is needed to understand the optimal management approach to reduce functional decline in this vulnerable population.
Our work has extended the scientific understanding of the association between obesity and disability by establishing that bodily pain could be an important mediator of this relationship in older women. We are not aware of prior work that estimates how much of the adverse impact of obesity on disability might be mediated by pain. However, one prior study using national data of adults of all ages found that pain and medical comorbidities were mediators of the adverse impact of obesity on health-related quality of life.30 Further research is warranted to determine whether effective treatment of bodily pain may be a useful strategy to reduce the negative impact of obesity on physical function in women.
Results from our study confirmed the previously observed association between obesity and disability. Additionally, we found that the impact of obesity on physical function depends on gender. Obese, older women have poorer physical function than their normal weight counterparts; whereas for older men, obesity did not increase the likelihood of disability or poorer function. Others have observed the differential impact of obesity by sex, however the reasons for this difference are not clear. A study by LaCroix et al. found that women with higher BMI had greater risk of mobility problems, but this was not true in men.31 Another study by Friedmann et al. observed that women in the highest quintile of BMI had higher prevalence of disability in activities of daily living or instrumental activities of daily living; whereas this was not true in men.32 Some have suggested that women are more sensitive to somatic symptoms and also may be more likely than men to report physical difficulties.27 Further, the higher skeletal muscle mass in men may allow for better strategies to compensate for the excess body weight compared to obese women.30 These data suggest that weight-loss related interventions to prevent functional decline may be best targeted towards women.
Our study has several strengths including analysis of a multiethnic, population-based sample. We also analyzed several measures of disability and physical functioning, including both performance-based and self-reported function. We also utilized measures of pain at multiple sites. However, some limitations of our study have to be considered. The cross-sectional design does not allow us to establish temporality of our factors of interest. We postulate that obesity develops initially, which subsequently leads to more pain and disability. However, in this study we cannot definitively establish causal inference between the association of obesity and disability. We cannot rule out the possibility that seniors initially develop pain and disability, and then develop and obesity secondarily. Additionally, we did not have measures of body composition which may have enhanced the interpretation of our findings.
In conclusion, as the increasing prevalence and severity of obesity intersects with the aging of the population in the coming years, it is feared that these combined trends may produce severe strain on the medical infrastructure and health care funding related to disability. It is important to understand which populations are at particular risk of developing obesity-related disability and which factors might mediate this association in order to better target interventions that might mitigate this problem. Women seem to be more vulnerable to functional problems associated with obesity; therefore, interventions to prevent obesity-related disability should target obese women. Further, bodily pain may be an important mediator of the disability associated with obesity in women. Bodily pain is potentially treatable and could represent an effective target of interventions designed to reduce the morbidity of obesity in seniors.
Acknowledgments
FUNDING
Dr. Fowler-Brown was supported by the National Institute on Aging funded HRC/Harvard Research Nursing Home Program Project Award (AG004390) and the Harvard Older Americans Independence Center (AG287171). Dr Marcantonio is the recipient of a Mid-Career Investigator Award from the National Institute of Aging (K24). Dr. Wee is also supported by a Mid-Career Investigator Award from the National Institute of Health (K24).
Sponsor’s Role: None.
Footnotes
Conflict of Interest: The authors have no financial or personal conflicts of interest related to this paper.
Author Contributions: Study concept and design (AFB, SL), acquisition of subjects (SL), data analysis (AFB, LN), interpretation of data (AFB, CW, LN, EM, SL), and preparation of manuscript (AFB, CW, EM, LN, SL).
References
- 1.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Jensen GL. Obesity and functional decline: Epidemiology and geriatric consequences. Clin Geriatr Med. 2005;21:677–87. doi: 10.1016/j.cger.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Jensen GL, Silver HJ, Roy MA, et al. Obesity is a risk factor for reporting homebound status among community-dwelling older persons. Obesity (Silver Spring) 2006;14:509–517. doi: 10.1038/oby.2006.66. [DOI] [PubMed] [Google Scholar]
- 4.Lee JS, Kritchevsky SB, Tylavsky F, et al. Weight change, weight change intention, and the incidence of mobility limitation in well-functioning community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2005;60:1007–1012. doi: 10.1093/gerona/60.8.1007. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharya J, Choudhry K, Lakdawalla D. Chronic disease and severe disability among working-age populations. Med Care. 2008;46:92–100. doi: 10.1097/MLR.0b013e3181484335. [DOI] [PubMed] [Google Scholar]
- 6.Ferraro KF, Su YP, Gretebeck RJ, et al. Body mass index and disability in adulthood: A 20-year panel study. Am J Public Health. 2002;92:834–840. doi: 10.2105/ajph.92.5.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schoeni RF, Martin LG, Andreski PM, et al. Persistent and growing socioeconomic disparities in disability among the elderly: 1982–2002. Am J Public Health. 2005;95:2065–2070. doi: 10.2105/AJPH.2004.048744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dunlop DD, Song J, Manheim LM, et al. Racial/ethnic differences in the development of disability among older adults. Am J Public Health. 2007;97:2209–2215. doi: 10.2105/AJPH.2006.106047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang J, Bennett JM, Shaw BA, et al. Gender differences in functional status in middle and older age: Are there any age variations? J Gerontol B Psychol Sci Soc Sci. 2008;63:S282–S292. doi: 10.1093/geronb/63.5.s282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buchner DM, Beresford SAA, Larson EB, et al. Effects of physical activity on health status in older adults II: Intervention Studies. Annu Rev Public Health. 1992;13:469–488. doi: 10.1146/annurev.pu.13.050192.002345. [DOI] [PubMed] [Google Scholar]
- 11.Leveille SG, Kiel DP, Jones RN, et al. The MOBILIZE Boston Study: design and methods of a prospective cohort study of novel risk factors for falls in an older population. BMC Geriatr. 2008;8:16. doi: 10.1186/1471-2318-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Wiener JM, Hanley RJ, Clark R, et al. Measuring the activities of daily living: Comparisons across national surveys. J Gerontol. 1990;45:S229–S237. doi: 10.1093/geronj/45.6.s229. [DOI] [PubMed] [Google Scholar]
- 14.Guralnik JM, Seeman TE, Tinetti ME, et al. Validation and use of performance measures of functioning in a non-disabled older population: MacArthur studies of successful aging. Aging (Milano) 1994;6:410–419. doi: 10.1007/BF03324272. [DOI] [PubMed] [Google Scholar]
- 15.U.S. National Institutes of Health. Clinical Guidelines for the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Bethesda, MD: National Institutes of Health; 1998. [Google Scholar]
- 16.Washburn RA, Smith KW, Jette AM, et al. The Physical Activity Scale For The Elderly (PASE): Development and evaluation. J Clin Epidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 17.Washburn RA, McAuley E, Katula J, et al. The Physical Activity Scale for the Elderly (PASE): Evidence for validity. J Clin Epidemiol. 1999;52:643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 18.Hu G, Tuomilehto J, Silventoinen K, et al. Body mass index, waist circumference, and waist-hip ratio on the risk of total and type-specific stroke. Arch Intern Med. 2007;167:1420–1427. doi: 10.1001/archinte.167.13.1420. [DOI] [PubMed] [Google Scholar]
- 19.Gregg EW, Cheng YJ, Cadwell BL, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293:1868–1874. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 20.Gregg EW, Cheng YJ, Narayan KM, et al. The relative contributions of different levels of overweight and obesity to the increased prevalence of diabetes in the United States: 1976–2004. Prev Med. 2007;45:348–352. doi: 10.1016/j.ypmed.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 21.Hu FB, Manson JE, Stampfer MJ, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001;345:790–797. doi: 10.1056/NEJMoa010492. [DOI] [PubMed] [Google Scholar]
- 22.Leveille SG, Ling S, Hochberg MC, et al. Widespread musculoskeletal pain and the progression of disability in older disabled women. Ann Intern Med. 2001;135:1038–1046. doi: 10.7326/0003-4819-135-12-200112180-00007. [DOI] [PubMed] [Google Scholar]
- 23.Handrigan G, Hue O, Simoneau M, et al. Weight loss and muscular strength affect static balance control. Int J Obes (Lond) 2010;34:936–942. doi: 10.1038/ijo.2009.300. [DOI] [PubMed] [Google Scholar]
- 24.Teasdale N, Hue O, Marcotte J, et al. Reducing weight increases postural stability in obese and morbid obese men. Int J Obes (Lond) 2007;31:153–160. doi: 10.1038/sj.ijo.0803360. [DOI] [PubMed] [Google Scholar]
- 25.Visser M, Pahor M, Taaffe DR, et al. Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: The Health ABC Study. J Gerontol A Biol Sci Med Sci. 2002;57:M326–M332. doi: 10.1093/gerona/57.5.m326. [DOI] [PubMed] [Google Scholar]
- 26.Stenholm S, Rantanen T, Heliovaara M, et al. The mediating role of C-reactive protein and handgrip strength between obesity and walking limitation. J Am Geriatr Soc. 2008;56:462–469. doi: 10.1111/j.1532-5415.2007.01567.x. [DOI] [PubMed] [Google Scholar]
- 27.Gijsbers van Wijk CM, Kolk AM. Sex differences in physical symptoms: The Contribution of Symptom Perception Theory. Soc Sci Med. 1997;45:231–246. doi: 10.1016/s0277-9536(96)00340-1. [DOI] [PubMed] [Google Scholar]
- 28.Orfila F, Ferrer M, Lamarca R, et al. Gender differences in health-related quality of life among the elderly: The role of objective functional capacity and chronic conditions. Soc Sci Med. 2006;63:2367–2380. doi: 10.1016/j.socscimed.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 29.Merrill SS, Seeman TE, Kasl SV, et al. Gender differences in the comparison of self-reported disability and performance measures. J Gerontol A Biol Sci Med Sci. 1997;52:M19–M26. doi: 10.1093/gerona/52a.1.m19. [DOI] [PubMed] [Google Scholar]
- 30.Broadwin J, Goodman-Gruen D, Slymen D. Ability of fat and fat-free mass percentages to predict functional disability in older men and women. J Am Geriatr Soc. 2001;49:1641–1645. doi: 10.1046/j.1532-5415.2001.t01-1-49273.x. [DOI] [PubMed] [Google Scholar]
- 31.LaCroix AZ, Guralnik JM, Berkman LF, et al. Maintaining mobility in late life. II. Smoking, alcohol consumption, physical activity, and body mass index. Am J Epidemiol. 1993;137:858–869. doi: 10.1093/oxfordjournals.aje.a116747. [DOI] [PubMed] [Google Scholar]
- 32.Friedmann JM, Elasy T, Jensen GL. The relationship between body mass index and self-reported functional limitation among older adults: A gender difference. J Am Geriatr Soc. 2001;49:398–403. doi: 10.1046/j.1532-5415.2001.49082.x. [DOI] [PubMed] [Google Scholar]
- 33.Weinstein AR, Sesso HD, Lee IM, et al. The joint effects of physical activity and body mass index on coronary heart disease risk in women. Arch Intern Med. 2008;168:884–890. doi: 10.1001/archinte.168.8.884. [DOI] [PubMed] [Google Scholar]
- 34.Koster A, Penninx BWJH, Newman AB, et al. Lifestyle factors and incident mobility limitation in obese and non-obese older adults] Obesity. 2007;15:3122–3132. doi: 10.1038/oby.2007.372. [DOI] [PubMed] [Google Scholar]
- 35.Koster A, Patel KV, Visser M, et al. Joint effects of adiposity and physical activity on incident mobility limitation in older adults. J Am Geriatr Soc. 2008;56:636–643. doi: 10.1111/j.1532-5415.2007.01632.x. [DOI] [PubMed] [Google Scholar]