Abstract
Acquired resistance toward apoptosis represents one of the hallmarks of human cancer and a major cause of the inefficacy of most anticancer treatment regimens. Based on its ability to inhibit apoptosis, the B-cell lymphoma/leukemia 2 (Bcl-2) protein family has garnered the most attention as a promising therapeutic target in cancer. Accordingly, efforts have lately been focused on the development of drugs targeting Bcl-2 proteins with considerable therapeutic success, particularly in hematologic malignancies. Here, we review the previous studies and highlight the pivotal role of the Bcl-2 protein family in the homeostasis of hematologic tissue compartment. This knowledge provides more insight into why some cancers are more sensitive to Bcl-2 targeting than others and will foster the clinical evaluation of Bcl-2-targeting strategies in cancer by avoiding severe on-target side effects in the development of healthy tissues.
Keywords: apoptosis, BH3 mimetics, Bcl-2 targeting
Facts
Inefficient mitochondrial apoptosis is a key determinant in therapeutic success of a number of anticancer regimens.
Mitochondrial apoptosis is tightly controlled by the Bcl-2 protein family.
Bcl-2 proteins have a crucial role in the development and the homeostasis of cells of hematopoietic origin.
Imbalanced expression of Bcl-2-family members has been readily associated with the development of hematologic malignancies such as lymphoma, leukemia or myeloma.
Several small-molecule inhibitors of Bcl-2 proteins have been developed and are currently under clinical evaluation with a marked susceptibility to hematologic malignancies.
Open Questions
What is the impact of Bcl-2-targeting anticancer therapy in solid tumors?
How can hematologic side effects be avoided upon Bcl-2-targeting anticancer therapy?
How and in combination with which additional chemotherapeutics provoke Bcl-2-antagonizing protocols for a potent anticancer effect?
Compelling studies conducted over the last 20 years established the concept that apoptosis serves as a natural barrier to cancer development, which is triggered autonomously during the process of malignant transformation or as a result of anticancer treatment.1 Accordingly, acquired resistance toward apoptosis is a hallmark of most types of human cancer and a major cause of the inefficacy of most anticancer treatment regimens.2 Mitochondria represents a central regulatory node in the apoptotic machinery and the decisive event thereby is the process of mitochondrial outer membrane permeabilization (MOMP). Upon MOMP, multiple pro-apoptotic molecules are released from the mitochondrial intermembrane space to coordinate most of the hallmarks of apoptosis, like nuclear condensation and caspase activation. Inefficient MOMP has been considered to be one of the key determinants of therapeutic success of a number of anticancer regimens. Accordingly, reactivation of the mitochondrial apoptotic machinery by restoration of MOMP has been viewed as a promising strategy to combat human cancer.1
Bcl-2 Protein Family, the Gatekeepers of Mitochondrial Outer Membrane
MOMP is tightly controlled by the Bcl-2 (B-cell lymphoma/leukemia 2) protein family via protein–protein interaction (Figure 1). Bcl-2-family members have been grouped into three classes (Figure 1) The antiapoptotic Bcl-2-family members including Bcl-2, Bcl-xl and Mcl-1 inhibit apoptosis, whereas a second class including Bax and Bak promotes apoptosis. A third divergent class of BH3-only proteins including Bad, Bik, Bid, Bim, Bmf, Noxa and Puma have a conserved BH3 domain that can bind and regulate the activity of Bcl-2 proteins. Recent evidence suggests that BH3-only proteins derepress and liberate Bax and Bak by direct binding and inhibition of anti-apoptotic family members including Bcl-2. By contrast, an opposing model postulates direct activation of Bax and Bak by BH3-only proteins including Bim, tBid and Puma (Figure 1).1
Figure 1.
Bcl-2 protein family in apoptosis and hematologic malignancies. Mitochondria represent a cellular regulatory node in apoptosis induced by death cues (e.g. DNA damage) or by the deprivation of survival signals (e.g. emitted by antigen receptor). The pro-apoptotic activity of mitochondria involves the mitochondrial outer membrane permeabilization (MOMP), which is tightly regulated by anti- and pro-apoptotic Bcl-2 protein family members. This is in turn is controlled by BH3-only proteins that initiate MOMP by either direct binding to the pro-apoptotic Bcl-2 members or by antagonizing their anti-apoptotic counterparts. Upon MOMP cytochrome c is released from the mitochondrial intermembrane space and initiates proteolytic activation of caspases, culminating in apoptotic cell death. Imbalanced expression of Bcl-2-family members has been readily associated with the development of hematologic malignancies such as lymphoma, leukemia or myeloma as summarized. PCL, plasma cell leukemia. Astrisks indicate the association of the Bcl-2 protein family members (gain- or loss-of-function) in chemosusceptibility (green) and/or malignant transformation of lymphoid malignancies (red or blue)
Apoptosis Represents a Fundamental Regulatory System During Hematopoiesis
Hematopoiesis gives rise to blood cells of different lineages throughout normal life. Abnormalities in this developmental program lead to blood cell diseases including leukemia and lymphoma.3 During hematopoiesis, a complex interacting network of cytokines and adhesion molecules tightly regulates the survival of progenitor cells, both positively and negatively. Following deprivation of these survival cues apoptotic death of progenitor cells actively safeguards hematologic homeostasis and prevents malignant transformation.4 Accordingly, almost 90% of pre-T- and B-cells undergo apoptosis during maturation in the thymus or bone marrow, respectively. Furthermore, after antigen exposure T- and B-cells undergo clonal expansion, giving rise to the generation of a large number of active effector lymphocytes. Apoptosis triggers the shutdown of the immune response when an infection has been overcome.5 Importantly, key elements of the basic apoptotic signaling machinery have been first discovered in the hematopoietic system associated with diseases when aberrantly expressed (Bcl-2 and lymphoma) or mutated (CD95 and ALPS),6 underscoring the intimate association of the apoptotic machinery, in particular, Bcl-2 proteins with the homeostasis of the hematopoietic system (Figure 1).
Bcl-2 Proteins – Their Physiologic Role in Cells of Hematopoietic System and Hematologic Cancer
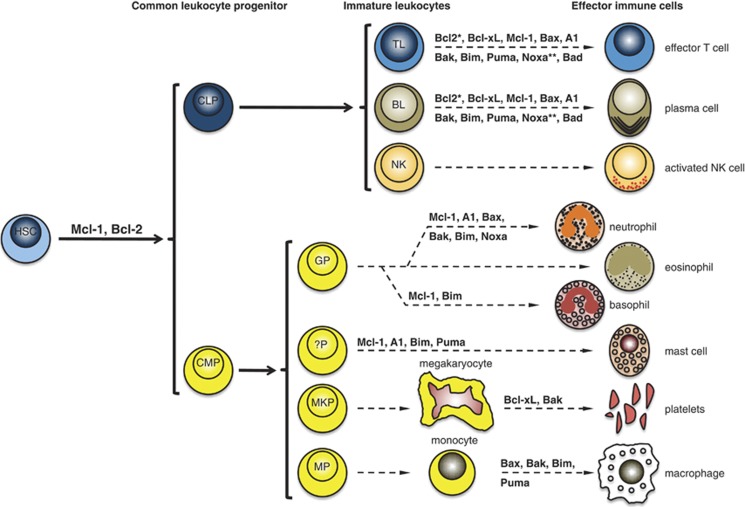
Imbalanced expression of Bcl-2-family members has been readily associated with the development of hematologic malignancies such as human lymphoma, leukemia or myeloma. Besides the extensive biochemical characterization, gene-targeting experiments in mice repeatedly showed that Bcl-2 proteins are essential for the development and homeostasis of the hematopoietic system. In the following we will summarize the data obtained in the previous years demonstrating the pivotal role of Bcl-2 proteins in hematologic compartment homeostasis (Figure 2), which may account for the observed association of hematologic malignancies with imbalanced Bcl-2 expression (Figure 1) and the marked susceptibility of hematologic malignancies toward Bcl-2-targeting strategies (Figure 3 and Table 1).
Figure 2.
The Bcl-2 protein family in the development and homeostasis of the hematologic system. A summary of the current knowledge about the physiological role of Bcl-2 protein family in hematopoiesis based on the results obtained in mice. common lymphoid progenitor (CLP), common myeloid progenitor (CMP), T lymphocyte (TL), BL (B lymphocyte), NK (natural killer cells), GP (granulocyte progenitor), ?P (unknown progenitor), MKP (megakaryocyte progenitor), MP (monocyte progenitor). *Bcl-2 ablation reduces the number and the lifespan of leukocytes but presumably does not impact on lymphoid development. **Noxa impacts on the lymphocyte function upon infection but is not involved in lymphoid development
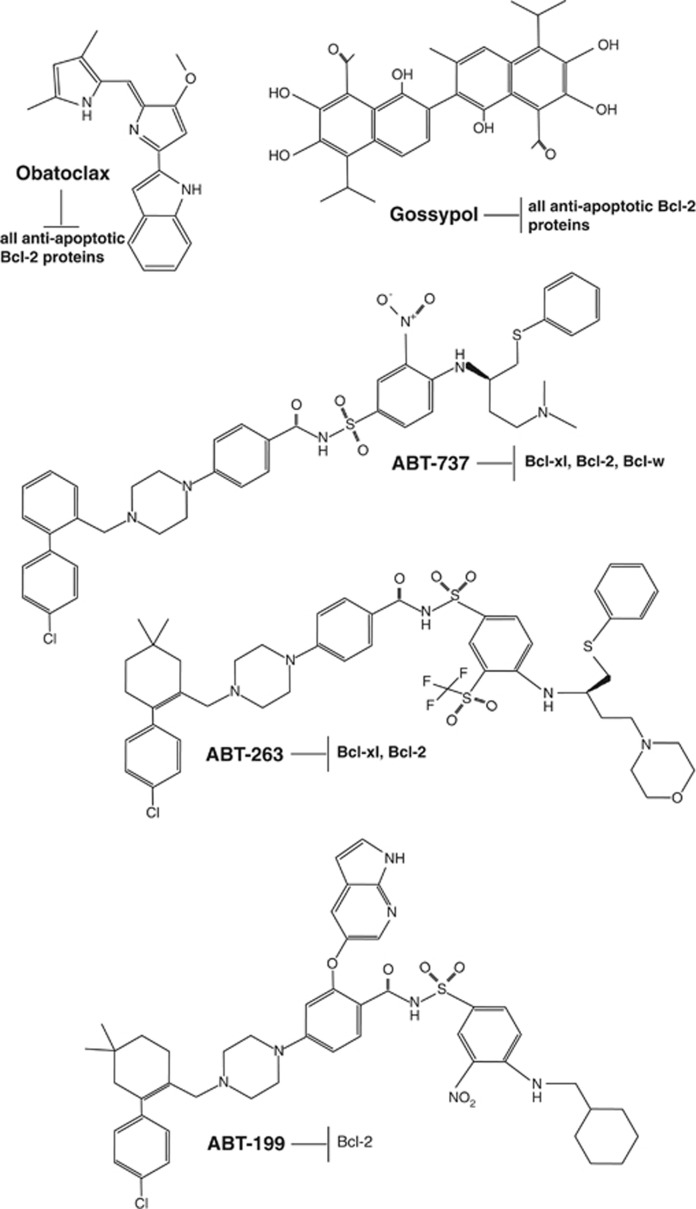
Figure 3.
Structural view of BH3 mimetics. Obatoclax (GX15-070) is a Bcl-2 homology domain-3 (BH3) mimetic. It occupies a hydrophobic cleft within the BH3-binding groove of Bcl-2, antagonizing Bcl-2 and thus inducing apoptosis. Gossypol is a natural phenol derived from the cotton plant (genus: Gossypium). The phenolic aldehyde permeates cells and acts as an inhibitor for several dehydrogenase enzymes and in particular in its (R)-configuration (known as AT-101) it acts as a pan-Bcl-2-family inhibitor, capable to bind and inhibit most antiapoptotic Bcl-2-family members. Abt-737 is a small-molecule BH3 mimetic developed by Abbott that binds to the hydrophobic BH3-binding groove of antiapoptotic Bcl-2-family members. ABT-737 binds with high affinity (Ki ≤1 nM) to Bcl-xl, Bcl-2 and Bcl-w, but not to the less-homologous proteins Bcl-b, Mcl-1 and A1. Abt-263 (Navitoclax, Abbott Laboratories) is structurally related to Abt-737. It represents an orallybioavailable small-molecule Bad-like BH3 mimetic which efficiently antagonizes antiapoptotic Bcl-2-family members (Ki's of <1 nM for Bcl-2, Bcl-xl and Bcl-w). Abt-199, generated by Abbott is a high-affinity Bcl-2-selective small-molecule BH3 mimetic. It is not interacting with Bcl-xl and thus not interfering with platelet homeostasis
Table 1. Published phase II/III clinical trials of drugs targeting the Bcl-2 family.
| Study description | Tumor entity | Study summary | Reference |
|---|---|---|---|
| Phase II trial of oblimersen as a single treatment | advanced CLL | 2/26 patients achieved PR; 7/17 patients showed ≥50% reduction in splenomegaly; 2/7 patients showed complete disappearance of hepatomegaly; 7/22 patients showed ≥ 50% reduction of lymphadenopathy; 11/22 patients showed ≥50% reduction in circulating lymphocyte count | O'Brien et al.99 |
| Phase III trial of fludarabine plus cyclophosphamide with (group 1) or without (group 2) oblimersen | Relapsed or refractory CLL | 17 % CR in group 1 versus 7% CR in group 2. Among patients with CR, response duration was significantly longer in group 1 versus group 2 (>36 months versus 22 months); 40% of patients with CR or PR of group 1 showed a significant 5-year survival benefit | O'Brien et al.128 |
| Phase II trial of oblimersen in combination with rituximab | Recurrent B-cell non-Hodgkin lymphoma | CR in 23 % patients, a PR in 19 % patients and 28 % patients showed a minimal response or stable disease | Pro et al.101 |
| Phase II trial of oblimersen in combination with gemtuzumab ozogamicin | AML | 12/48 patients (25%) achieved a major response with 5 CR and 7 CR without platelet recovery. Ten of the 12 patients who achieved a major response survived >6 months compared with six of 36 nonresponders | Moore et al.102 |
| Phase II trial of oblimersen in combination with dexamethasone and thalidomide | Relapsed MM | 55% of patients achieved objective responses, including CR in 2/33 patients, 4/33 near CRs, PR in 12/33 patients and 6/33 patients had minimal responses | Badros et al.103 |
| Phase III trial of dexamethasone with (group 1) or without oblimersen (group 2) | Advanced MM | No significant differences between the two groups in time to tumor progression or objective-response rates | Chanan-Khan et al.105 |
| Phase II trial oblimersen in combination with dacarbazine | Advanced melanoma | The addition of oblimersen to dacarbazine yielded a trend toward improved survival at 24-month minimum follow-up (median, 9.0 versus 7.8 months; P=077) and significant increases in progression-free survival (median, 2.6 versus 1.6 months; P<001), overall response (13.5 versus 7.5% P=007), complete response (2.8 versus 0.8%), and durable response (7.3 versus 3.6% P=03) | Bedikian et al.104 |
| Phase II trial of docetaxel in combination with oblimersen | Castration-resistant prostate cancer | No statistical difference in overall survival | Sternberg et al.106 |
| Phase I/II trial of gossypol in combination with topotecan | Relapsed and refractory SCLC | No convincing clinical activity | Heist et al.115 |
| Phase II trial of gossypol in combination with docetaxel | NSCLC | No convincing clinical activity | Ready et al.117 |
| Phase II trial of gossypol | Chemotherapy-sensitive recurrent extensive-stage SCLC | No observed clinical activity | Baggstrom et al.118 |
| Phase II trial of docetaxel plus prednisone in combination with gossypol | Metastatic castration-resistant prostate cancer | No statistical difference in overall survival | Sonpavde et al.119 |
| Phase II trial of obatoclax mesylate | Myelofibrosis | No convincing clinical activity | Parikh et al.132 |
| Phase II trial of Abt-263 | Relapsed SCLC | PR in 2.6% and stable disease in 23% patients. The most common toxicity associated with navitoclax was thrombocytopenia, which reached grade III–IV in 41% of patients. |
Abbreviations: AML, acute myeloid leukemia; CLL, chronic lymphocytic leukemia; CR, complete remission; MM, multiple myeloma; NSCLC, non-small cell lung cancer; PR, partial remission; SCLC, small cell lung cancer
Antiapoptotic Bcl-2 Proteins
The discovery of Bcl-2 family of proteins is intimately linked to many B-cell malignancies.
The bcl-2 gene was initially discovered at the t(14;18) chromosome translocation breakpoint in B-cell follicular lymphomas, where its transcription becomes excessively driven by the immunoglobulin heavy chain gene promoter and enhancer on chromosome 14.7 In line with the data obtained in human tumor samples, mice lacking bcl-2 have severe defects in the development of lymphoid progenitor cells from hematopoietic stem cells (HSC) and display reduced lifespan of lymphoid and myeloid cells.8, 9, 10 Conversely, early studies reported that Bcl-2 overexpression enhanced the survival of T-11 and B-cells.12 More strikingly, ectopic expression of Bcl-2 was capable of rescuing lymphopoiesis in SCID mice.13 The oncogenic potential of Bcl-2 was explored by showing that its overexpression facilitates the c-myc-driven proliferation of B-cell precursors and tumorigenesis.14
Myeloid cell leukemia sequence 1 (Mcl-1) was identified as an immediate-early gene induced by TPA-mediated differentiation of a human myeloid leukemia cell line (ML-1).15 mcl-1 is one of the most highly amplified genes in a variety of human cancers. Specifically, elevated Mcl-1 was shown in acute myeloid leukaemia (AML),16 mantle cell lymphoma (MCL),17 diffuse large B-cell lymphoma (DLBL),18 non-Hodgkin's lymphoma19 and multiple myeloma (MM).20 In line with these observations, removal of Mcl-1 caused cell death of transformed AML and rescued AML-afflicted mice from disease development.21 Mcl-1 is unique among the antiapoptotic Bcl-2 members in being essential for early embryonic development. Deletion of mcl-1 results in lethality at embryonic day 3.5,22 whereas tissue-specific ablation of mcl-1 in mice demonstrated that Mcl-1 is essential for the survival and the development of B- and T-lymphocytes,23 germinal center formation and B-cell memory,24 plasma cells,25 neutrophils,26 basophil and mast cells,27 and has an obligate role for the survival of HSCs.28 Remarkably, inducible Cre-mediated deletion of even a single Mcl-1 allele substantially impaired the growth of c-myc-driven mouse lymphomas.29 In line with these observations, overexpression of Mcl-1 results in the development of lymphomas30 identifying Mcl-1 as a critical regulator of hematopoiesis and hematologic malignancies.
Initial studies using low stringency hybridization assays in chicken lymphoid cells identified bcl-x, a bcl-2-related gene that can function as a Bcl-2-independent regulator of apoptosis. Alternative splicing results in two distinct bcl-x mRNAs. The protein product of the larger mRNA, Bcl-xl, was similar in size and predicted structure to Bcl-2.31 Similar to Bcl-2 and Mcl-1, elevated Bcl-xl expression has been frequently observed in hematologic malignancies and is implicated to have a role in disease progression.32 bcl-x−/− mice died at embryonic day 13 and displayed massive cell death of immature hematopoietic cells and thus severe defects in the development of the hematopoietic system,33 underlining the essential role of Bcl-x for the survival and development of lymphoid cells. In line with these observations, an independent approach showed that genetic ablation or pharmacological inactivation of Bcl-xl reduces platelet half-life and causes thrombocytopenia in mice.34 The central role of Bcl-xl in malignant transformation of hematopoietic cells was further strengthened with the fact that transgenic mice overexpressing Bcl-xl developed lymphomas.35
In contrast to Bcl-2 and Mcl-1 the described roles for A1 are more restricted. A1 is a hematopoietic tissue-specific gene that is expressed in several hematopoietic cell lineages, including T-helper lymphocytes, macrophages and neutrophils.36 High expression of a1 mRNA was reported in acute lymphoblastic leukemia (ALL) and chronic lymphocytic leukemia (CLL), MCL and multiple types of DLBL,37, 38, 39 especially the OxPhos subgroup of DLBL.40 Mouse a1 mRNA is induced during myeloid differentiation,36 mast cell activation upon an allergic reaction,41 lymphocyte development42 and lymphocyte and macrophage activation,36 emphasizing the importance of A1 in the hematopoietic system. Genetic deletions of a1 in mice are challenging owing to the existence of multiple genetic copies of the a1 gene in mice with a highly cell type-specific expression pattern. However, mice lacking only one a1 gene, a1-a, show hematologic defects including reduced number of neutrophils43 and mast cells owing to enhanced apoptosis.41 A1 knockdown mice harboring a tg-driven short-hairpin RNA (shRNA) targeting A1-a, A1-b and A1-d mRNA did not show a severe phenotype. However, gene silencing appeared to be highly restricted and a significant knockdown of A1 abundance could only be achieved in thymocytes, while it was not efficient in mature lymphocytes.44 Remarkably, a tg shA1 mouse expressing a micro-RNA30-based precursor harboring a shRNA able to efficiently target all A1 isoforms revealed multiple roles of A1 in lymphocyte development. Specifically, knockdown of A1 impaired early stages of T-cell differentiation, B-cell homeostasis and sensitized transitional as well as follicular B-cells to apoptosis induced by ligation of the B-cell receptor. As a consequence, B-cell proliferation in response to mitogens was severely impaired, whereas T-cell survival was not affected. Moreover, granulocytes showed increased spontaneous death in culture or failed to accumulate in significant numbers in vivo.45 Enforced expression of A1-a in T-cells was found to accelerate T-cell survival in a1-a tg mice.46 Overexpression of A1 in B- and T-cell lineages in Eμ-a1-a tg mice extended the lifespan of thymocytes and early B-cells.47
Pro-apoptotic Bcl-2 Proteins
Bax was initially identified as a Bcl-2-interacting factor capable to antagonize the pro-survival activity of Bcl-2.48 Based on a sequence homology, Bak (Bcl-2-homologous antagonist/killer) was identified and characterized as another pro-apoptotic member of the Bcl-2 protein family.49, 50 The mitochondrial apoptotic pathway converges on these two pro-apoptotic Bcl-2 proteins either of which is sufficient to drive MOMP in the majority of cells. Bax and Bak are highly redundant and this redundancy has been expected to limit their roles as tumor suppressors.51 However, different human malignancies including hematologic tumors exhibit mutated bax52 or bak53 and reduced expression levels of these pro-apoptotic Bcl-2-family members have been associated with a great number of hematologic malignancies including CLL, follicular lymphoma, MCL and marginal zone B-cell lymphoma.54 In line with these observations, genomic ablation of bax impaired myc-driven apoptosis and circumvents the selection of p53 mutations during myc-mediated lymphomagenesis.55 Despite having an outwardly normal phenotype, bax−/− or bak−/− single knockout mice display a mild hematologic phenotype with only a mild lymphoid hyperplasia, probably owing to the functional redundancy of the two proteins.56, 57 Double-knockout bak−/−bax−/− animals display an increase (three- to 10-fold) in both myeloid and lymphoid cells compared with either single bak−/− or bax−/− knockouts or wild-type mice. Progressive accumulation of mature B- and T-cells led to massive enlargement of the spleen and lymph nodes and infiltration of parenchymal organs.57 Furthermore, bak−/−bax−/− mice display severe defects in the T-cell development and homeostasis after infection.58 Independently, inactivation of bak restored thrombocytopenia caused by bcl-xl deletion, suggesting a crucial role of Bak in platelet lifespan.34
BH3-only Proteins
An expression screen for proteins that bind to Bcl-2 yielded a small novel protein, denoted as Bim, whose only similarity to any known protein was the short (9-amino-acid) BH3 motif shared by most Bcl-2 homologs.59 Sequence analysis of murine cDNAs revealed the presence of three major isoforms (BimEL-196aa, BimL-140aa and BimS-110aa), produced by alternative splicing.59 Independently, the same gene was discovered in an ovarian cDNA library, using Mcl-1 as bait, that they initially termed Bod (Bcl-2-related ovarian death agonist). Bim has a critical role during hematopoiesis (Figure 1) and the in vivo function of this protein has received the most attention among the pro-apoptotic Bcl-2 members. Blocking Bim expression by gene deletion or epigenetic silencing has a central role in the pathogenesis or the response to anticancer therapeutics in a number of human hematologic malignancies including Burkitt's lymphoma (BL), MCL and various B-cell non-Hodgkin's lymphomas.60, 61, 62 Consistent with these observations, gene-targeting experiments of the bim locus in mice demonstrated a crucial role of Bim in the homeostasis of most immune cells. In particular, bim−/− mice have abnormal high numbers of T- and B-cells, macrophages and granulocytes owing to improved apoptosis resistance to several stimuli, including cytokine deprivation, abnormal calcium flux or irradiation.63, 64 They also show defects in the immune response shutdown as indicated by increased numbers of antibody-secreting plasma cells and the extended survival of activated cytotoxic T-cells after infection.65, 66 Furthermore, Bim seems to be essential for the apoptosis of autoreactive B- and T-cells (negative selection) resulting in systemic lupus erythematosus-like autoimmune disease in bim−/− animals.67, 68 Moreover, loss of Bim accelerates lymphomagenesis in Eμ-myc transgenic mice.69
Puma (p53 upregulated modulator of apoptosis) is one of the most potent killers among the BH3-only proteins, which was initially identified as an antagonist of Bcl-2, induced by p53.70, 71, 72 In view of the fact that more than half of human tumors comprise p53 mutations, Puma represents an important factor in human cancer as the induction of Puma expression in response to genotoxic anticancer therapeutics is efficiently abrogated in p53-deficient tumors.73 Furthermore, ∼40% of primary human BL fail to express detectable levels of Puma and in some tumors this is based on the epigenetic silencing of puma.74 puma−/− mice show no abnormalities in hematologic tissue development, whereas lymphocytes, myeloid cells and certain other cell types show resistance to apoptosis induced by growth factor withdrawal or DNA damage.75, 76, 77 Suppression of Puma by shRNAs or its genetic ablation in bim−/− mice enhanced myc-driven B-cell lymphomagenesis.77, 78, 79 In cooperation with Bim, Puma was additionally shown to be involved in homeostasis of mast cells and macrophages.77, 80 Furthermore, the combined deletion of bim and puma, but not in either single knockout, impaired the elimination of autoreactive T-cells and led to autoimmune reactions in various organs.81
After its initial description as a novel phorbol-12-myristate-13-acetate-responsive gene in adult T-cell leukemia, Noxa was rediscovered in a differential display approach using mRNA from γ-irradiated wild-type and IRF-1/p53 double-deficient mouse embryonic fibroblasts.82 Like Puma, Noxa was initially identified as a primary p53-response gene. Noxa has been described as an important determinant of cell death in response to chemotherapy in lymphoid malignancies including CLL, HL, MM and MCL cells.83, 84, 85, 86 Furthermore, array-based comparative genomic hybridization and gene-expression microarray analysis showed that Noxa is mutated and preferentially silenced in DLBL.60 Gene-targeting experiments of noxa in mice displayed defects in T-and B-cell activation and the immune response against viral infection.87, 88 Furthermore, Noxa was shown to be centrally involved in neutrophils apoptosis.89
By utilizing Bcl-2 protein to screen cDNA libraries the Bcl-xl/Bcl-2-associated death promoter homolog (Bad) was identified.90 Bad was the first BH3-only protein to be connected to proximal signal transduction through its differential phosphorylation in response to extracellular survival factors.91 In particular, phosphatidylinositol-3-kinase/Akt signaling, a survival pathway frequently hyper-activated in many lymphocytic malignancies, negatively regulates Bad's function.92 In line with these observations, bad−/− mice develop DLBL of the germinal center or post-germinal center, B220+CD19+ B-cells expressing the zinc finger transcription factor Bcl-6 (latency >15 months).93 Although DLBLs were the most frequent tumor entity observed (>40%), bad−/− mice additionally suffered a broad range of different hematologic malignancies.93 This is particularly intriguing, as the inactivation of Bad's pro-apoptotic function by phosphorylation appears to have a prominent role in the survival of these lymphocyte populations.92
Together, the data obtained by analyzing human tumor samples and in particular the use of transgenic mouse models conclusively support the notion that the Bcl-2 protein family represents a central regulatory node in the development of hematopoietic system.
Bcl-2 Targeting as a Therapeutic Option in Hematologic Malignancies
Owing to their imbalance expression levels in tumor cells and their capability to regulate MOMP, Bcl-2 proteins have been viewed as promising therapeutic targets in cancer and research efforts have lately been focusing on the development of drugs targeting Bcl-2 proteins. Accordingly, several small-molecule inhibitors of Bcl-2 proteins have been developed and are currently under clinical evaluation (Figure 3 and Table 1). The following paragraphs summarize the results obtained by surveying these small molecules as a therapeutic option with special emphasis on their activity in hematologic malignancies.
Bcl-2 Antisense Oligodeoxynucleotide G3139/Oblimersen
G3139 (INN, trade name Genasense; also known as Augmerosen or Oblimersen) is an antisense oligodeoxyribonucleotide, specifically targeting bcl-2 mRNA. Initial in vitro studies using an 18-base phosphorothioate oligonucleotide complementary to the first six codons of the bcl-2 mRNA (G3139)94 showed that this molecule selectively and specifically inhibits Bcl-2 expression in the SU-DHL-4 t(14;18)-containing lymphoma cell lines.94, 95 By performing rigorous efficacy, pharmacokinetic and toxicity studies using a number of different lymphoma mouse models95, 96, 97 the preclinical evaluation of G3139 was completed and further studies were extended into a phase I study for lymphoma patients with high Bcl-2 expression.98 Overall the human phase I studies with G3139 demonstrated good efficacy with low toxicity. In particular, tumor regression, improvement in the laboratory parameters, and symptom improvement together with downregulation of the target protein expression were achieved. Based on these promising results several phase II/III clinical trials were initiated (Table 1). A phase II trial of oblimersen sodium as a single agent showed only modest clinical activity in heavily pre-treated patients with advanced CLL.99 However, a separate phase III study of fludarabine plus cyclophosphamide with or without oblimersen showed a 5-year survival benefit in a post hoc analysis of patients with CLL who achieved complete (CR) or partial remission (PR).100 Oblimersen in combination with rituximab was tested in a phase II trial in non-Hodgkin lymphoma. This study revealed a CR in 23% patients, a PR in 19% patients and 28% of patients showed a minimal response or a stable disease (SD).101 Another phase II trial was conducted for the treatment of AML with a combination of oblimersen and gemtuzumab ozogamicin with 10% patients achieved a CR and 15% patients achieved a PR.102 Oblimersen was also tested in combination with dexamethasone and thalidomide in a phase II trial for the treatment of relapsed MM patients. Fifty five percent of patients had objective responses, including 2/36 CRs, 4/36 near CRs, and 12/36 PR and 6/36 patients had minimal responses.103 However, a randomised phase III trial of oblimersen in combination with other drugs in advanced MM, melanoma or prostate cancer did not show a statistical difference in overall survival.104, 105, 106 Based on these results oblimersen was not approved as a therapeutic option by the FDA.107 Though, oblimersen efficiently downregulated Bcl-2 in cell culture and thereby effectively reduced lymphoma cell survival the lack of efficiency in primary tumors might be a result of insufficient drug delivery in patients.108 Furthermore, those studies demonstrated a long-term benefit for some patients after completing the study and encouraged a renewal of the drug approval, which is still ongoing.
Gossypol
Gossypol, a natural phenol derived from the cotton plant, was characterized as a specific antagonist of Bcl-xl.109 Further studies showed that gossypol acts as a pan-Bcl-2-family inhibitor, capable of binding and inhibiting most antiapoptotic Bcl-2-family members.110 Preclinical evaluation of gossypol revealed a potent anti-tumor activity by activating the mitochondrial apoptotic pathway in DLBL,111 CML (chronic myeloid leukemia),112 CLL,113 and non-Hodgkin lymphoma.114 Based on these analyses an orally-bioavailable enantiomer of gossypol, AT-101, was evaluated in phase II clinical trials for the treatment of prostate and lung cancer as single agent or in combination with conventional chemotherapeutics (Table 1). However, these efforts did not show convincing clinical activity.115, 116, 117, 118, 119 Notably, the most common toxicity was observed in hematologic compartment, suggesting a more potent toxic effect on hematologic malignancies.115 Phase II trials for the treatment of hematological malignancies are still in progress.120
Obatoclax (GX15-070)
Obatoclax, a pan-Bcl-2-family inhibitor, was developed from a natural lead compound that potently disrupted the interaction of members of the Bcl-2-family in a functional screen.121 As a single agent, obatoclax possesses pronounced anticancer activity in cell lines or primary cells derived from patients suffering from different hematologic malignancies including AML,122 mast cell leukemia,123 ALL124 CLL,125 MM,126 and HL (Hodgkin Lymphoma).127 Albeit promising results were obtained in vitro and in vivo mouse models, phase I clinical trials for the treatment of AML, CLL, ALL, lymphoma and solid tumors as well as phase II clinical trials for the treatment of HL and myelofibrosis revealed a clinical activity as single agent only in a minority of patients (Table 1).128, 129, 130, 131, 132 However, further phase I trials for the combined treatment show very promising clinical activity of obatoclax in specific treatment protocols, such as the combination with bortezomib in MCL133 and MM134 with 3/12 and 4/10 patients showing a clinical response, respectively.
ABT-737/ABT-263 (Navitoclax)/ABT-199 (GDC-0199)
A high-throughput NMR-based method was used to screen a chemical library to identify small molecules that bind to the hydrophobic BH3-binding groove of Bcl-xl. The resultant compound ABT-737, developed by Abbott Laboratories (North Chicago, IL, USA), bound with high affinity (Ki ≤1 nM) to Bcl-xl, Bcl-2 and Bcl-w, but not to the less-homologous proteins Bcl-b, Mcl-1 and A1.135 Further evaluation of its anti-tumor activity showed that ABT-737 displayed potent single-agent activity against a subset of cell lines representing lymphoid malignancies.135 In combination with conventional chemotherapeutics, ABT-737 was shown to potently induce apoptosis in HL,136 MM,137 AMC,138 and CLL 139 and also solid tumors such as non-small cell lung cancer (NSCLC).135 In addition to established human tumor cell lines, ABT-737 effectively induced apoptosis in primary patient-derived lymphoma and CLL cells ex vivo.135
However, the prospects for ABT-737 as a therapeutic agent have been hampered by its poor physiochemical and pharmaceutical properties. This compound is not orally bioavailable and its low aqueous solubility makes formulation for i.v. delivery challenging. However, the impressive biological activity of ABT-737 encouraged research to develop an orally-bioavailable compound. On the basis of various pharmacokinetic/pharmacodynamic models and animal studies ABT-263 (Navitoclax; Figure 3), an orraly-bioavailable Bad-like BH3 mimetic (Kis of <1 nM for Bcl-2, Bcl-xl, and Bcl-w) was generated. ABT-263 disrupts Bcl-2/Bcl-xl interactions with pro-death proteins (e.g. Bim), leading to the initiation of apoptosis within 2 h post treatment.140 Initial analyses showed that the oral administration of ABT-263 alone induces complete tumor regressions in xenograft models of small cell lung cancer (SCLC) and ALL. In xenograft models of aggressive B-cell lymphoma and MM ABT-263 promoted significant efficacy of clinically relevant chemotherapeutic regimens.140 A detailed activity screen revealed that ABT-263 enhances the response of multiple chemotherapeutic regimens, for example, rituximab, rapamycine, rituximab–cyclophosphamide-adriamycin-vincristine-prednisone, and bortezomib, in several models of hematologic malignancies.141 However, owing to the crucial role of Bcl-xl in platelet homeostasis34 the therapeutic use of ABT-263 was associated with transient thrombocytopenia in preclinical trials.142
Based on the results obtained by ABT-737 and ABT-263, Abbott Laboratories has recently developed a high-affinity Bcl-2-selective BH3 mimetic, ABT-199 (GDC-0199), which spared human platelets in vitro and dog platelets in vivo.143 Tumor regression was achieved for xenografts of human lymphoma cell lines. ABT-199 was as effective as ABT-737 in prolonging survival of immuno-competent mice bearing aggressive progenitor cell lymphomas (derived from bitransgenic myc/bcl-2 mice) without causing thrombocytopenia.144 Furthermore, ABT-199 was identified as a promising therapeutic option for the treatment of t(11;14) MM145 and AML.146 More strikingly, the first clinical trial using a single dose of ABT-199 in three patients with refractory CLL resulted in a rapid tumor lysis within 24 h in 3 of 3 patients.143
Together the data obtained by using different pharmacological inhibitors of Bcl-2 indicated a marked susceptibility of hematologic malignancies towards the Bcl-2-targeting protocols (Table 1).
Perspectives and Restrictions
There are not many anticancer therapeutics that are as exclusively characterized as Bcl-2-targeting strategies concerning their specificity toward the designated target and the mode of their interference with cellular actions and cell death. This is indeed based on our increasing knowledge about Bcl-2 protein family in the last 20 years, which finally has entered the translational stage in the last couple of years. One major aspect about Bcl-2 proteins is their crucial role in the development and the homeostasis of cells of hematopoietic origin. Previous data showed that an imbalanced Bcl-2 protein level causally determines hematologic malignant progression and accordingly targeting the Bcl-2 protein family has been proven to be successful, in particular, in hematologic malignancies. However, manipulations in their function or abundance in the healthy hematologic system may result in fatal changes in this tissue compartment.147 Accordingly, this may indicate that in non-hematologic malignancies Bcl-2-targeting strategies should be used with specific caution concerning the functionality and homeostasis of the hematologic system. Alternatively, given the cell type-specific role of some Bcl-2-family members and a more abundant role of other members a highly selective targeting strategy is necessary to avoid severe on-target side effects in the development of other tissues. However, agents targeting the Bcl-2 protein family have been generally shown to be a potent killer of tumor cells derived from hematologic malignancies and accumulating evidence supports the idea that the treatment of other cancer entities may strongly benefit from the Bcl-2-antagonizing protocols in combination with other chemotherapy regimens. The knowledge of how and in combination with which additional chemotherapeutics Bcl-2-antagonizing protocols provoke a potent anticancer effect will strongly foster the clinical evaluation of Bcl-2-targeting strategies.
Acknowledgments
This work was supported by a grant from the Deutsche Forschungsgemeinschaft (DFG), KFO 286-RP3, SFB 832-A9 and Köln Fortune Program/Faculty of Medicine, University of Cologne.
Glossary
- AML
acute myeloid leukemia
- ALL
acute lymphoblastic leukemia
- BL
Burkitt's lymphoma
- CGH
comparative genomic hybridization
- CLL
chronic lymphocytic leukemia
- CML
chronic myeloid leukemia
- CR
complete remission
- DLBL
diffuse large B-cell lymphoma
- FDA
Food and Drug Administration
- HL
Hodgkin's lymphoma
- HSC
hematopoietic stem cells
- IMS
mitochondrial intermembrane space
- MCL
mantle cell lymphoma
- MM
multiple myeloma
- MOMP
mitochondrial outer membrane permeabilization
- PR
partial remission
- SCLC
small cell lung cancer
- SD
stable disease
- SLE
systemic lupus erythematosus
The authors declare no conflict of interest.
Footnotes
Edited by H-U Simon
References
- Adams JM, Cory S. The Bcl-2 apoptotic switch in cancer development and therapy. Oncogene. 2007;26:1324–1337. doi: 10.1038/sj.onc.1210220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- Sachs L. The control of hematopoiesis and leukemia: from basic biology to the clinic. Proc Natl Acad Sci USA. 1996;93:4742–4749. doi: 10.1073/pnas.93.10.4742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickremasinghe RG, Hoffbrand AV. Biochemical and genetic control of apoptosis: relevance to normal hematopoiesis and hematological malignancies. Blood. 1999;93:3587–3600. [PubMed] [Google Scholar]
- Renault TT, Chipuk JE. Getting away with murder: how does the BCL-2 family of proteins kill with immunity. Ann N Y Acad Sci. 2013;1285:59–79. doi: 10.1111/nyas.12045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debatin KM. Role of apoptosis in congenital hematologic disorders and bone marrow failure. Rev Clin Exp Hematol. 2003;7:57–71. [PubMed] [Google Scholar]
- Tsujimoto Y, Finger LR, Yunis J, Nowell PC, Croce CM. Cloning of the chromosome breakpoint of neoplastic B cells with the t(14;18) chromosome translocation. Science. 1984;226:1097–1099. doi: 10.1126/science.6093263. [DOI] [PubMed] [Google Scholar]
- Nakayama K, Nakayama K, Negishi I, Kuida K, Shinkai Y, Louie MC, et al. Disappearance of the lymphoid system in Bcl-2 homozygous mutant chimeric mice. Science. 1993;261:1584–1588. doi: 10.1126/science.8372353. [DOI] [PubMed] [Google Scholar]
- Veis DJ, Sorenson CM, Shutter JR, Korsmeyer SJ. Bcl-2-deficient mice demonstrate fulminant lymphoid apoptosis, polycystic kidneys, and hypopigmented hair. Cell. 1993;75:229–240. doi: 10.1016/0092-8674(93)80065-m. [DOI] [PubMed] [Google Scholar]
- Matsuzaki Y, Nakayama K, Nakayama K, Tomita T, Isoda M, Loh DY, et al. Role of bcl-2 in the development of lymphoid cells from the hematopoietic stem cell. Blood. 1997;89:853–862. [PubMed] [Google Scholar]
- Strasser A, Harris AW, Cory S. bcl-2 transgene inhibits T cell death and perturbs thymic self-censorship. Cell. 1991;67:889–899. doi: 10.1016/0092-8674(91)90362-3. [DOI] [PubMed] [Google Scholar]
- Strasser A, Whittingham S, Vaux DL, Bath ML, Adams JM, Cory S, et al. Enforced BCL2 expression in B-lymphoid cells prolongs antibody responses and elicits autoimmune disease. Proc Natl Acad Sci USA. 1991;88:8661–8665. doi: 10.1073/pnas.88.19.8661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strasser A, Harris AW, Corcoran LM, Cory S. Bcl-2 expression promotes B- but not T-lymphoid development in scid mice. Nature. 1994;368:457–460. doi: 10.1038/368457a0. [DOI] [PubMed] [Google Scholar]
- Vaux DL, Cory S, Adams JM. Bcl-2 gene promotes haemopoietic cell survival and cooperates with c-myc to immortalize pre-B cells. Nature. 1988;335:440–442. doi: 10.1038/335440a0. [DOI] [PubMed] [Google Scholar]
- Kozopas KM, Yang T, Buchan HL, Zhou P, Craig RW. MCL1 a gene expressed in programmed myeloid cell differentiation, has sequence similarity to BCL2. Proc Natl Acad Sci USA. 1993;90:3516–3520. doi: 10.1073/pnas.90.8.3516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okita H, Umezawa A, Fukuma M, Ando T, Urano F, Sano M, et al. Acute myeloid leukemia possessing jumping translocation is related to highly elevated levels of EAT/mcl-1, a Bcl-2 related gene with anti-apoptotic functions. Leuk Res. 2000;24:73–77. doi: 10.1016/s0145-2126(99)00137-x. [DOI] [PubMed] [Google Scholar]
- Khoury JD, Medeiros LJ, Rassidakis GZ, McDonnell TJ, Abruzzo LV, Lai R. Expression of Mcl-1 in mantle cell lymphoma is associated with high-grade morphology, a high proliferative state, and p53 overexpression. J Pathol. 2003;199:90–97. doi: 10.1002/path.1254. [DOI] [PubMed] [Google Scholar]
- Wenzel SS, Grau M, Mavis C, Hailfinger S, Wolf A, Madle H, et al. MCL1 is deregulated in subgroups of diffuse large B-cell lymphoma. Leukemia. 2012;27:1381–1390. doi: 10.1038/leu.2012.367. [DOI] [PubMed] [Google Scholar]
- Kuramoto K, Sakai A, Shigemasa K, Takimoto Y, Asaoku H, Tsujimoto T, et al. High expression of MCL1 gene related to vascular endothelial growth factor is associated with poor outcome in non-Hodgkin's lymphoma. Br J Haematol. 2002;116:158–161. doi: 10.1046/j.1365-2141.2002.03253.x. [DOI] [PubMed] [Google Scholar]
- Zhang B, Gojo I, Fenton RG. Myeloid cell factor-1 is a critical survival factor for multiple myeloma. Blood. 2002;99:1885–1893. doi: 10.1182/blood.v99.6.1885. [DOI] [PubMed] [Google Scholar]
- Glaser SP, Lee EF, Trounson E, Bouillet P, Wei A, Fairlie WD, et al. Anti-apoptotic Mcl-1 is essential for the development and sustained growth of acute myeloid leukemia. Genes Dev. 2012;26:120–125. doi: 10.1101/gad.182980.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinkenberger JL, Horning S, Klocke B, Roth K, Korsmeyer SJ. Mcl-1 deficiency results in peri-implantation embryonic lethality. Genes Dev. 2000;14:23–27. [PMC free article] [PubMed] [Google Scholar]
- Opferman JT, Letai A, Beard C, Sorcinelli MD, Ong CC, Korsmeyer SJ. Development and maintenance of B and T lymphocytes requires antiapoptotic MCL-1. Nature. 2003;426:671–676. doi: 10.1038/nature02067. [DOI] [PubMed] [Google Scholar]
- Vikstrom I, Carotta S, Luthje K, Peperzak V, Jost PJ, Glaser S, et al. Mcl-1 is essential for germinal center formation and B cell memory. Science. 2010;330:1095–1099. doi: 10.1126/science.1191793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peperzak V, Vikstrom I, Walker J, Glaser SP, LePage M, Coquery CM, et al. Mcl-1 is essential for the survival of plasma cells. Nat Immunol. 2013;14:290–297. doi: 10.1038/ni.2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzhagalov I, St, John A, He YW. The antiapoptotic protein Mcl-1 is essential for the survival of neutrophils but not macrophages. Blood. 2007;109:1620–1626. doi: 10.1182/blood-2006-03-013771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilla JN, Chen CC, Mukai K, BenBarak MJ, Franco CB, Kalesnikoff J, et al. Reduced mast cell and basophil numbers and function in Cpa3-Cre; Mcl-1fl/fl mice. Blood. 2011;118:6930–6938. doi: 10.1182/blood-2011-03-343962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opferman JT, Iwasaki H, Ong CC, Suh H, Mizuno S, Akashi K, et al. Obligate role of anti-apoptotic MCL-1 in the survival of hematopoietic stem cells. Science. 2005;307:1101–1104. doi: 10.1126/science.1106114. [DOI] [PubMed] [Google Scholar]
- Kelly GL, Grabow S, Glaser SP, Fitzsimmons L, Aubrey BJ, Okamoto T, et al. Targeting of MCL-1 kills MYC-driven mouse and human lymphomas even when they bear mutations in p53. Genes Dev. 2014;28:58–70. doi: 10.1101/gad.232009.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou P, Levy NB, Xie H, Qian L, Lee CY, Gascoyne RD, et al. MCL1 transgenic mice exhibit a high incidence of B-cell lymphoma manifested as a spectrum of histologic subtypes. Blood. 2001;97:3902–3909. doi: 10.1182/blood.v97.12.3902. [DOI] [PubMed] [Google Scholar]
- Boise LH, Gonzalez-Garcia M, Postema CE, Ding L, Lindsten T, Turka LA, et al. bcl-x, a bcl-2-related gene that functions as a dominant regulator of apoptotic cell death. Cell. 1993;74:597–608. doi: 10.1016/0092-8674(93)90508-n. [DOI] [PubMed] [Google Scholar]
- Horita M, Andreu EJ, Benito A, Arbona C, Sanz C, Benet I, et al. Blockade of the Bcr-Abl kinase activity induces apoptosis of chronic myelogenous leukemia cells by suppressing signal transducer and activator of transcription 5-dependent expression of Bcl-xL. J Exp Med. 2000;191:977–984. doi: 10.1084/jem.191.6.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motoyama N, Wang F, Roth KA, Sawa H, Nakayama K, Nakayama K, et al. Massive cell death of immature hematopoietic cells and neurons in Bcl-x-deficient mice. Science. 1995;267:1506–1510. doi: 10.1126/science.7878471. [DOI] [PubMed] [Google Scholar]
- Mason KD, Carpinelli MR, Fletcher JI, Collinge JE, Hilton AA, Ellis S, et al. Programmed anuclear cell death delimits platelet life span. Cell. 2007;128:1173–1186. doi: 10.1016/j.cell.2007.01.037. [DOI] [PubMed] [Google Scholar]
- Kelly PN, Grabow S, Delbridge AR, Strasser A, Adams JM. Endogenous Bcl-xL is essential for Myc-driven lymphomagenesis in mice. Blood. 2011;118:6380–6386. doi: 10.1182/blood-2011-07-367672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin EY, Orlofsky A, Berger MS, Prystowsky MB. Characterization of A1, a novel hemopoietic-specific early-response gene with sequence similarity to bcl-2. J Immunol. 1993;151:1979–1988. [PubMed] [Google Scholar]
- Nagy B, Lundan T, Larramendy ML, Aalto Y, Zhu Y, Niini T, et al. Abnormal expression of apoptosis-related genes in haematological malignancies: overexpression of MYC is poor prognostic sign in mantle cell lymphoma. Br J Haematol. 2003;120:434–441. doi: 10.1046/j.1365-2141.2003.04121.x. [DOI] [PubMed] [Google Scholar]
- Mahadevan D, Spier C, Della Croce K, Miller S, George B, Riley C, et al. Transcript profiling in peripheral T-cell lymphoma, not otherwise specified, and diffuse large B-cell lymphoma identifies distinct tumor profile signatures. Mol Cancer Ther. 2005;4:1867–1879. doi: 10.1158/1535-7163.MCT-05-0146. [DOI] [PubMed] [Google Scholar]
- Piva R, Pellegrino E, Mattioli M, Agnelli L, Lombardi L, Boccalatte F, et al. Functional validation of the anaplastic lymphoma kinase signature identifies CEBPB and BCL2A1 as critical target genes. J Clin Invest. 2006;116:3171–3182. doi: 10.1172/JCI29401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti S, Savage KJ, Kutok JL, Feuerhake F, Kurtin P, Mihm M, et al. Molecular profiling of diffuse large B-cell lymphoma identifies robust subtypes including one characterized by host inflammatory response. Blood. 2005;105:1851–1861. doi: 10.1182/blood-2004-07-2947. [DOI] [PubMed] [Google Scholar]
- Xiang Z, Ahmed AA, Moller C, Nakayama K, Hatakeyama S, Nilsson G. Essential role of the prosurvival bcl-2 homologue A1 in mast cell survival after allergic activation. J Exp Med. 2001;194:1561–1569. doi: 10.1084/jem.194.11.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomayko MM, Cancro MP. Long-lived B cells are distinguished by elevated expression of A1. J Immunol. 1998;160:107–111. [PubMed] [Google Scholar]
- Hamasaki A, Sendo F, Nakayama K, Ishida N, Negishi I, Nakayama K, et al. Accelerated neutrophil apoptosis in mice lacking A1-a, a subtype of the bcl-2-related A1 gene. J Exp Med. 1998;188:1985–1992. doi: 10.1084/jem.188.11.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberdoerffer P, Kanellopoulou C, Heissmeyer V, Paeper C, Borowski C, Aifantis I, et al. Efficiency of RNA interference in the mouse hematopoietic system varies between cell types and developmental stages. Mol Cell Biol. 2005;25:3896–3905. doi: 10.1128/MCB.25.10.3896-3905.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottina E, Grespi F, Tischner D, Soratroi C, Geley S, Ploner A, et al. Targeting antiapoptotic A1/Bfl-1 by in vivo RNAi reveals multiple roles in leukocyte development in mice. Blood. 2012;119:6032–6042. doi: 10.1182/blood-2011-12-399089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verschelde C, Michonneau D, Trescol-Biemont MC, Berberich I, Schimpl A, Bonnefoy-Berard N. Overexpression of the antiapoptotic protein A1 promotes the survival of double positive thymocytes awaiting positive selection. Cell Death Differ. 2006;13:1213–1221. doi: 10.1038/sj.cdd.4401814. [DOI] [PubMed] [Google Scholar]
- Chuang PI, Morefield S, Liu CY, Chen S, Harlan JM, Willerford DM. Perturbation of B-cell development in mice overexpressing the Bcl-2 homolog A1. Blood. 2002;99:3350–3359. doi: 10.1182/blood.v99.9.3350. [DOI] [PubMed] [Google Scholar]
- Oltvai ZN, Milliman CL, Korsmeyer SJ. Bcl-2 heterodimerizes in vivo with a conserved homolog, Bax, that accelerates programmed cell death. Cell. 1993;74:609–619. doi: 10.1016/0092-8674(93)90509-o. [DOI] [PubMed] [Google Scholar]
- Chittenden T, Harrington EA, O'Connor R, Flemington C, Lutz RJ, Evan GI, et al. Induction of apoptosis by the Bcl-2 homologue Bak. Nature. 1995;374:733–736. doi: 10.1038/374733a0. [DOI] [PubMed] [Google Scholar]
- Kiefer MC, Brauer MJ, Powers VC, Wu JJ, Umansky SR, Tomei LD, et al. Modulation of apoptosis by the widely distributed Bcl-2 homologue Bak. Nature. 1995;374:736–739. doi: 10.1038/374736a0. [DOI] [PubMed] [Google Scholar]
- Adams JM, Cory S. Bcl-2-regulated apoptosis: mechanism and therapeutic potential. Curr Opin Immunol. 2007;19:488–496. doi: 10.1016/j.coi.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijerink JP, Mensink EJ, Wang K, Sedlak TW, Sloetjes AW, de Witte T, et al. Hematopoietic malignancies demonstrate loss-of-function mutations of BAX. Blood. 1998;91:2991–2997. [PubMed] [Google Scholar]
- Kondo S, Shinomura Y, Miyazaki Y, Kiyohara T, Tsutsui S, Kitamura S, et al. Mutations of the bak gene in human gastric and colorectal cancers. Cancer Res. 2000;60:4328–4330. [PubMed] [Google Scholar]
- Agarwal B, Naresh KN. Bcl-2 family of proteins in indolent B-cell non-Hodgkin's lymphoma: study of 116 cases. Am J Hematol. 2002;70:278–282. doi: 10.1002/ajh.10139. [DOI] [PubMed] [Google Scholar]
- Eischen CM, Roussel MF, Korsmeyer SJ, Cleveland JL. Bax loss impairs Myc-induced apoptosis and circumvents the selection of p53 mutations during Myc-mediated lymphomagenesis. Mol Cell Biol. 2001;21:7653–7662. doi: 10.1128/MCB.21.22.7653-7662.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudson CM, Tung KS, Tourtellotte WG, Brown GA, Korsmeyer SJ. Bax-deficient mice with lymphoid hyperplasia and male germ cell death. Science. 1995;270:96–99. doi: 10.1126/science.270.5233.96. [DOI] [PubMed] [Google Scholar]
- Lindsten T, Ross AJ, King A, Zong WX, Rathmell JC, Shiels HA, et al. The combined functions of proapoptotic Bcl-2 family members bak and bax are essential for normal development of multiple tissues. Mol Cell. 2000;6:1389–1399. doi: 10.1016/s1097-2765(00)00136-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathmell JC, Lindsten T, Zong WX, Cinalli RM, Thompson CB. Deficiency in Bak and Bax perturbs thymic selection and lymphoid homeostasis. Nat Immunol. 2002;3:932–939. doi: 10.1038/ni834. [DOI] [PubMed] [Google Scholar]
- O'Connor L, Strasser A, O'Reilly LA, Hausmann G, Adams JM, Cory S, et al. Bim: a novel member of the Bcl-2 family that promotes apoptosis. EMBO J. 1998;17:384–395. doi: 10.1093/emboj/17.2.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mestre-Escorihuela C, Rubio-Moscardo F, Richter JA, Siebert R, Climent J, Fresquet V, et al. Homozygous deletions localize novel tumor suppressor genes in B-cell lymphomas. Blood. 2007;109:271–280. doi: 10.1182/blood-2006-06-026500. [DOI] [PubMed] [Google Scholar]
- Pinon JD, Labi V, Egle A, Villunger A. Bim and Bmf in tissue homeostasis and malignant disease. Oncogene. 2008;27 (Suppl 1:S41–S52. doi: 10.1038/onc.2009.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tagawa H, Suguro M, Tsuzuki S, Matsuo K, Karnan S, Ohshima K, et al. Comparison of genome profiles for identification of distinct subgroups of diffuse large B-cell lymphoma. Blood. 2005;106:1770–1777. doi: 10.1182/blood-2005-02-0542. [DOI] [PubMed] [Google Scholar]
- Bouillet P, Metcalf D, Huang DC, Tarlinton DM, Kay TW, Kontgen F, et al. Proapoptotic Bcl-2 relative Bim required for certain apoptotic responses, leukocyte homeostasis, and to preclude autoimmunity. Science. 1999;286:1735–1738. doi: 10.1126/science.286.5445.1735. [DOI] [PubMed] [Google Scholar]
- Villunger A, Scott C, Bouillet P, Strasser A. Essential role for the BH3-only protein Bim but redundant roles for Bax, Bcl-2, and Bcl-w in the control of granulocyte survival. Blood. 2003;101:2393–2400. doi: 10.1182/blood-2002-07-2132. [DOI] [PubMed] [Google Scholar]
- Hildeman DA, Zhu Y, Mitchell TC, Bouillet P, Strasser A, Kappler J, et al. Activated T cell death in vivo mediated by proapoptotic bcl-2 family member bim. Immunity. 2002;16:759–767. doi: 10.1016/s1074-7613(02)00322-9. [DOI] [PubMed] [Google Scholar]
- Pellegrini M, Belz G, Bouillet P, Strasser A. Shutdown of an acute T cell immune response to viral infection is mediated by the proapoptotic Bcl-2 homology 3-only protein Bim. Proc Natl Acad Sci USA. 2003;100:14175–14180. doi: 10.1073/pnas.2336198100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouillet P, Purton JF, Godfrey DI, Zhang LC, Coultas L, Puthalakath H, et al. BH3-only Bcl-2 family member Bim is required for apoptosis of autoreactive thymocytes. Nature. 2002;415:922–926. doi: 10.1038/415922a. [DOI] [PubMed] [Google Scholar]
- Villunger A, Marsden VS, Zhan Y, Erlacher M, Lew AM, Bouillet P, et al. Negative selection of semimature CD4(+)8(-)HSA+ thymocytes requires the BH3-only protein Bim but is independent of death receptor signaling. Proc Natl Acad Sci USA. 2004;101:7052–7057. doi: 10.1073/pnas.0305757101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egle A, Harris AW, Bouillet P, Cory S. Bim is a suppressor of Myc-induced mouse B cell leukemia. Proc Natl Acad Sci USA. 2004;101:6164–6169. doi: 10.1073/pnas.0401471101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakano K, Vousden KH. PUMA a novel proapoptotic gene, is induced by p53. Mol Cell. 2001;7:683–694. doi: 10.1016/s1097-2765(01)00214-3. [DOI] [PubMed] [Google Scholar]
- Yu J, Zhang L, Hwang PM, Kinzler KW, Vogelstein B. PUMA induces the rapid apoptosis of colorectal cancer cells. Mol Cell. 2001;7:673–682. doi: 10.1016/s1097-2765(01)00213-1. [DOI] [PubMed] [Google Scholar]
- Han J, Flemington C, Houghton AB, Gu Z, Zambetti GP, Lutz RJ, et al. Expression of bbc3, a pro-apoptotic BH3-only gene, is regulated by diverse cell death and survival signals. Proc Natl Acad Sci USA. 2001;98:11318–11323. doi: 10.1073/pnas.201208798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J, Zhang L. The transcriptional targets of p53 in apoptosis control. Biochem Biophys Res Commun. 2005;331:851–858. doi: 10.1016/j.bbrc.2005.03.189. [DOI] [PubMed] [Google Scholar]
- Garrison SP, Jeffers JR, Yang C, Nilsson JA, Hall MA, Rehg JE, et al. Selection against PUMA gene expression in Myc-driven B-cell lymphomagenesis. Mol Cell Biol. 2008;28:5391–5402. doi: 10.1128/MCB.00907-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villunger A, Michalak EM, Coultas L, Mullauer F, Bock G, Ausserlechner MJ, et al. p53- and drug-induced apoptotic responses mediated by BH3-only proteins puma and noxa. Science. 2003;302:1036–1038. doi: 10.1126/science.1090072. [DOI] [PubMed] [Google Scholar]
- Jeffers JR, Parganas E, Lee Y, Yang C, Wang J, Brennan J, et al. Puma is an essential mediator of p53-dependent and -independent apoptotic pathways. Cancer Cell. 2003;4:321–328. doi: 10.1016/s1535-6108(03)00244-7. [DOI] [PubMed] [Google Scholar]
- Erlacher M, Labi V, Manzl C, Bock G, Tzankov A, Hacker G, et al. Puma cooperates with Bim, the rate-limiting BH3-only protein in cell death during lymphocyte development, in apoptosis induction. J Exp Med. 2006;203:2939–2951. doi: 10.1084/jem.20061552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemann MT, Zilfou JT, Zhao Z, Burgess DJ, Hannon GJ, Lowe SW. Suppression of tumorigenesis by the p53 target PUMA. Proc Natl Acad Sci USA. 2004;101:9333–9338. doi: 10.1073/pnas.0403286101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalak EM, Jansen ES, Happo L, Cragg MS, Tai L, Smyth GK, et al. Puma and to a lesser extent Noxa are suppressors of Myc-induced lymphomagenesis. Cell Death Differ. 2009;16:684–696. doi: 10.1038/cdd.2008.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrison SP, Phillips DC, Jeffers JR, Chipuk JE, Parsons MJ, Rehg JE, et al. Genetically defining the mechanism of Puma- and Bim-induced apoptosis. Cell Death Differ. 2012;19:642–649. doi: 10.1038/cdd.2011.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray DH, Kupresanin F, Berzins SP, Herold MJ, O'Reilly LA, Bouillet P, et al. The BH3-only proteins Bim and Puma cooperate to impose deletional tolerance of organ-specific antigens. Immunity. 2012;37:451–462. doi: 10.1016/j.immuni.2012.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oda E, Ohki R, Murasawa H, Nemoto J, Shibue T, Yamashita T, et al. Noxa, a BH3-only member of the Bcl-2 family and candidate mediator of p53-induced apoptosis. Science. 2000;288:1053–1058. doi: 10.1126/science.288.5468.1053. [DOI] [PubMed] [Google Scholar]
- Gomez-Bougie P, Wuilleme-Toumi S, Menoret E, Trichet V, Robillard N, Philippe M, et al. Noxa up-regulation and Mcl-1 cleavage are associated to apoptosis induction by bortezomib in multiple myeloma. Cancer Res. 2007;67:5418–5424. doi: 10.1158/0008-5472.CAN-06-4322. [DOI] [PubMed] [Google Scholar]
- Perez-Galan P, Roue G, Villamor N, Montserrat E, Campo E, Colomer D. The proteasome inhibitor bortezomib induces apoptosis in mantle-cell lymphoma through generation of ROS and Noxa activation independent of p53 status. Blood. 2006;107:257–264. doi: 10.1182/blood-2005-05-2091. [DOI] [PubMed] [Google Scholar]
- Qin JZ, Ziffra J, Stennett L, Bodner B, Bonish BK, Chaturvedi V, et al. Proteasome inhibitors trigger NOXA-mediated apoptosis in melanoma and myeloma cells. Cancer Res. 2005;65:6282–6293. doi: 10.1158/0008-5472.CAN-05-0676. [DOI] [PubMed] [Google Scholar]
- Brinkmann K, Zigrino P, Witt A, Schell M, Ackermann L, Broxtermann P, et al. Ubiquitin C-terminal hydrolase-L1 potentiates cancer chemosensitivity by stabilizing NOXA. Cell Rep. 2013;3:881–891. doi: 10.1016/j.celrep.2013.02.014. [DOI] [PubMed] [Google Scholar]
- Wensveen FM, Derks IA, van Gisbergen KP, de Bruin AM, Meijers JC, Yigittop H, et al. BH3-only protein Noxa regulates apoptosis in activated B cells and controls high-affinity antibody formation. Blood. 2012;119:1440–1449. doi: 10.1182/blood-2011-09-378877. [DOI] [PubMed] [Google Scholar]
- Wensveen FM, Klarenbeek PL, van Gisbergen KP, Pascutti MF, Derks IA, van Schaik BD, et al. Pro-apoptotic protein Noxa regulates memory T cell population size and protects against lethal immunopathology. J Immunol. 2013;190:1180–1191. doi: 10.4049/jimmunol.1202304. [DOI] [PubMed] [Google Scholar]
- Kirschnek S, Vier J, Gautam S, Frankenberg T, Rangelova S, Eitz-Ferrer P, et al. Molecular analysis of neutrophil spontaneous apoptosis reveals a strong role for the pro-apoptotic BH3-only protein Noxa. Cell Death Differ. 2011;18:1805–1814. doi: 10.1038/cdd.2011.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang E, Zha J, Jockel J, Boise LH, Thompson CB, Korsmeyer SJ. Bad a heterodimeric partner for Bcl-XL and Bcl-2, displaces Bax and promotes cell death. Cell. 1995;80:285–291. doi: 10.1016/0092-8674(95)90411-5. [DOI] [PubMed] [Google Scholar]
- Zha J, Harada H, Yang E, Jockel J, Korsmeyer SJ. Serine phosphorylation of death agonist BAD in response to survival factor results in binding to 14-3-3 not BCL-X(L) Cell. 1996;87:619–628. doi: 10.1016/s0092-8674(00)81382-3. [DOI] [PubMed] [Google Scholar]
- Datta SR, Dudek H, Tao X, Masters S, Fu H, Gotoh Y, et al. Akt phosphorylation of BAD couples survival signals to the cell-intrinsic death machinery. Cell. 1997;91:231–241. doi: 10.1016/s0092-8674(00)80405-5. [DOI] [PubMed] [Google Scholar]
- Ranger AM, Zha J, Harada H, Datta SR, Danial NN, Gilmore AP, et al. Bad-deficient mice develop diffuse large B cell lymphoma. Proc Natl Acad Sci USA. 2003;100:9324–9329. doi: 10.1073/pnas.1533446100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitada S, Miyashita T, Tanaka S, Reed JC. Investigations of antisense oligonucleotides targeted against bcl-2 RNAs. Antisense Res Dev. 1993;3:157–169. doi: 10.1089/ard.1993.3.157. [DOI] [PubMed] [Google Scholar]
- Cotter FE, Johnson P, Hall P, Pocock C, al Mahdi N, Cowell JK, et al. Antisense oligonucleotides suppress B-cell lymphoma growth in a SCID-hu mouse model. Oncogene. 1994;9:3049–3055. [PubMed] [Google Scholar]
- Devereux S, Cotter FE. Anti-sense and gene therapy approaches to the treatment of lymphomas. Baillieres Clin Haematol. 1996;9:819–834. doi: 10.1016/s0950-3536(96)80055-2. [DOI] [PubMed] [Google Scholar]
- Pocock CF, Malone M, Booth M, Evans M, Morgan G, Greil J, et al. BCL-2 expression by leukaemic blasts in a SCID mouse model of biphenotypic leukaemia associated with the t(4;11)(q21;q23) translocation. Br J Haematol. 1995;90:855–867. doi: 10.1111/j.1365-2141.1995.tb05207.x. [DOI] [PubMed] [Google Scholar]
- Cotter FE, Waters J, Cunningham D. Human Bcl-2 antisense therapy for lymphomas. Biochim Biophys Acta. 1999;1489:97–106. doi: 10.1016/s0167-4781(99)00139-6. [DOI] [PubMed] [Google Scholar]
- O'Brien SM, Cunningham CC, Golenkov AK, Turkina AG, Novick SC, Rai KR. Phase I to II multicenter study of oblimersen sodium, a Bcl-2 antisense oligonucleotide, in patients with advanced chronic lymphocytic leukemia. J Clin Oncol. 2005;23:7697–7702. doi: 10.1200/JCO.2005.02.4364. [DOI] [PubMed] [Google Scholar]
- O'Brien S, Moore JO, Boyd TE, Larratt LM, Skotnicki AB, Koziner B, et al. 5-year survival in patients with relapsed or refractory chronic lymphocytic leukemia in a randomized, phase III trial of fludarabine plus cyclophosphamide with or without oblimersen. J Clin Oncol. 2009;27:5208–5212. doi: 10.1200/JCO.2009.22.5748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pro B, Leber B, Smith M, Fayad L, Romaguera J, Hagemeister F, et al. Phase II multicenter study of oblimersen sodium, a Bcl-2 antisense oligonucleotide, in combination with rituximab in patients with recurrent B-cell non-Hodgkin lymphoma. Br J Haematol. 2008;143:355–360. doi: 10.1111/j.1365-2141.2008.07353.x. [DOI] [PubMed] [Google Scholar]
- Moore J, Seiter K, Kolitz J, Stock W, Giles F, Kalaycio M, et al. A Phase II study of Bcl-2 antisense (oblimersen sodium) combined with gemtuzumab ozogamicin in older patients with acute myeloid leukemia in first relapse. Leuk Res. 2006;30:777–783. doi: 10.1016/j.leukres.2005.10.025. [DOI] [PubMed] [Google Scholar]
- Badros AZ, Goloubeva O, Rapoport AP, Ratterree B, Gahres N, Meisenberg B, et al. Phase II study of G3139, a Bcl-2 antisense oligonucleotide, in combination with dexamethasone and thalidomide in relapsed multiple myeloma patients. J Clin Oncol. 2005;23:4089–4099. doi: 10.1200/JCO.2005.14.381. [DOI] [PubMed] [Google Scholar]
- Bedikian AY, Millward M, Pehamberger H, Conry R, Gore M, Trefzer U, et al. Bcl-2 antisense (oblimersen sodium) plus dacarbazine in patients with advanced melanoma: the Oblimersen Melanoma Study Group. J Clin Oncol. 2006;24:4738–4745. doi: 10.1200/JCO.2006.06.0483. [DOI] [PubMed] [Google Scholar]
- Chanan-Khan AA, Niesvizky R, Hohl RJ, Zimmerman TM, Christiansen NP, Schiller GJ, et al. Phase III randomised study of dexamethasone with or without oblimersen sodium for patients with advanced multiple myeloma. Leuk Lymphoma. 2009;50:559–565. doi: 10.1080/10428190902748971. [DOI] [PubMed] [Google Scholar]
- Sternberg CN, Dumez H, Van Poppel H, Skoneczna I, Sella A, Daugaard G, et al. Docetaxel plus oblimersen sodium (Bcl-2 antisense oligonucleotide): an EORTC multicenter, randomized phase II study in patients with castration-resistant prostate cancer. Ann Oncol. 2009;20:1264–1269. doi: 10.1093/annonc/mdn784. [DOI] [PubMed] [Google Scholar]
- Advani PP, Paulus A, Masood A, Sher T, Chanan-Khan A. Pharmacokinetic evaluation of oblimersen sodium for the treatment of chronic lymphocytic leukemia. Expert Opin Drug Metab Toxicol. 2011;7:765–774. doi: 10.1517/17425255.2011.579105. [DOI] [PubMed] [Google Scholar]
- Davids MS, Letai A. Targeting the B-cell lymphoma/leukemia 2 family in cancer. J Clin Oncol. 2012;30:3127–3135. doi: 10.1200/JCO.2011.37.0981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitada S, Leone M, Sareth S, Zhai D, Reed JC, Pellecchia M. Discovery, characterization, and structure-activity relationships studies of proapoptotic polyphenols targeting B-cell lymphocyte/leukemia-2 proteins. J Med Chem. 2003;46:4259–4264. doi: 10.1021/jm030190z. [DOI] [PubMed] [Google Scholar]
- Zhai D, Jin C, Satterthwait AC, Reed JC. Comparison of chemical inhibitors of antiapoptotic Bcl-2-family proteins. Cell Death Differ. 2006;13:1419–1421. doi: 10.1038/sj.cdd.4401937. [DOI] [PubMed] [Google Scholar]
- Mohammad RM, Wang S, Aboukameel A, Chen B, Wu X, Chen J, et al. Preclinical studies of a nonpeptidic small-molecule inhibitor of Bcl-2 and Bcl-X(L) [(-)-gossypol] against diffuse large cell lymphoma. Mol Cancer Ther. 2005;4:13–21. [PubMed] [Google Scholar]
- Meng Y, Li Y, Li J, Li H, Fu J, Liu Y, et al. (-)Gossypol and its combination with imatinib induce apoptosis in human chronic myeloid leukemic cells. Leuk Lymphoma. 2007;48:2204–2212. doi: 10.1080/10428190701583991. [DOI] [PubMed] [Google Scholar]
- Balakrishnan K, Burger JA, Wierda WG, Gandhi V. AT-101 induces apoptosis in CLL B cells and overcomes stromal cell-mediated Mcl-1 induction and drug resistance. Blood. 2009;113:149–153. doi: 10.1182/blood-2008-02-138560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li ZM, Jiang WQ, Zhu ZY, Zhu XF, Zhou JM, Liu ZC, et al. Synergistic cytotoxicity of Bcl-xL inhibitor, gossypol and chemotherapeutic agents in non-Hodgkin's lymphoma cells. Cancer Biol Ther. 2008;7:51–60. doi: 10.4161/cbt.7.1.5128. [DOI] [PubMed] [Google Scholar]
- Heist RS, Fain J, Chinnasami B, Khan W, Molina JR, Sequist LV, et al. Phase I/II study of AT-101 with topotecan in relapsed and refractory small cell lung cancer. J Thorac Oncol. 2010;5:1637–1643. doi: 10.1097/JTO.0b013e3181e8f4dc. [DOI] [PubMed] [Google Scholar]
- Liu G, Kelly WK, Wilding G, Leopold L, Brill K, Somer B. An open-label, multicenter, phase I/II study of single-agent AT-101 in men with castrate-resistant prostate cancer. Clin Cancer Res. 2009;15:3172–3176. doi: 10.1158/1078-0432.CCR-08-2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ready N, Karaseva NA, Orlov SV, Luft AV, Popovych O, Holmlund JT, et al. Double-blind, placebo-controlled, randomized phase 2 study of the proapoptotic agent AT-101 plus docetaxel, in second-line non-small cell lung cancer. J Thorac Oncol. 2011;6:781–785. doi: 10.1097/JTO.0b013e31820a0ea6. [DOI] [PubMed] [Google Scholar]
- Baggstrom MQ, Qi Y, Koczywas M, Argiris A, Johnson EA, Millward MJ, et al. A phase II study of AT-101 (Gossypol) in chemotherapy-sensitive recurrent extensive-stage small cell lung cancer. J Thorac Oncol. 2011;6:1757–1760. doi: 10.1097/JTO.0b013e31822e2941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonpavde G, Matveev V, Burke JM, Caton JR, Fleming MT, Hutson TE, et al. Randomized phase II trial of docetaxel plus prednisone in combination with placebo or AT-101, an oral small molecule Bcl-2 family antagonist, as first-line therapy for metastatic castration-resistant prostate cancer. Ann Oncol. 2012;23:1803–1808. doi: 10.1093/annonc/mdr555. [DOI] [PubMed] [Google Scholar]
- Clinic MA. Phase I/II Clinical Trial of Lenalidomide in Combination With AT-101 for the Treatment of Relapsed B-cell Chronic Lymphocytic Leukemia (B-CLL) ClinicalTrials.gov. 2009.
- Shore GC, Viallet J. Modulating the bcl-2 family of apoptosis suppressors for potential therapeutic benefit in cancer. Hematology Am Soc Hematol Educ Program. 2005;2005:226–230. doi: 10.1182/asheducation-2005.1.226. [DOI] [PubMed] [Google Scholar]
- Konopleva M, Watt J, Contractor R, Tsao T, Harris D, Estrov Z, et al. Mechanisms of antileukemic activity of the novel Bcl-2 homology domain-3 mimetic GX15-070 (obatoclax) Cancer Res. 2008;68:3413–3420. doi: 10.1158/0008-5472.CAN-07-1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buet D, Gallais I, Lauret E, Denis N, Lombard B, Guillonneau F, et al. Cotargeting signaling pathways driving survival and cell cycle circumvents resistance to Kit inhibitors in leukemia. Blood. 2012;119:4228–4241. doi: 10.1182/blood-2011-07-368316. [DOI] [PubMed] [Google Scholar]
- Bonapace L, Bornhauser BC, Schmitz M, Cario G, Ziegler U, Niggli FK, et al. Induction of autophagy-dependent necroptosis is required for childhood acute lymphoblastic leukemia cells to overcome glucocorticoid resistance. J Clin Invest. 2010;120:1310–1323. doi: 10.1172/JCI39987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campas C, Cosialls AM, Barragan M, Iglesias-Serret D, Santidrian AF, Coll-Mulet L, et al. Bcl-2 inhibitors induce apoptosis in chronic lymphocytic leukemia cells. Exp Hematol. 2006;34:1663–1669. doi: 10.1016/j.exphem.2006.07.008. [DOI] [PubMed] [Google Scholar]
- Trudel S, Li ZH, Rauw J, Tiedemann RE, Wen XY, Stewart AK. Preclinical studies of the pan-Bcl inhibitor obatoclax (GX015-070) in multiple myeloma. Blood. 2007;109:5430–5438. doi: 10.1182/blood-2006-10-047951. [DOI] [PubMed] [Google Scholar]
- Jona A, Khaskhely N, Buglio D, Shafer JA, Derenzini E, Bollard CM, et al. The histone deacetylase inhibitor entinostat (SNDX-275) induces apoptosis in Hodgkin lymphoma cells and synergizes with Bcl-2 family inhibitors. Exp Hematol. 2011;39:1007–1017 e1001. doi: 10.1016/j.exphem.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien SM, Claxton DF, Crump M, Faderl S, Kipps T, Keating MJ, et al. Phase I study of obatoclax mesylate (GX15-070), a small molecule pan-Bcl-2 family antagonist, in patients with advanced chronic lymphocytic leukemia. Blood. 2009;113:299–305. doi: 10.1182/blood-2008-02-137943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schimmer AD, O'Brien S, Kantarjian H, Brandwein J, Cheson BD, Minden MD, et al. A phase I study of the pan bcl-2 family inhibitor obatoclax mesylate in patients with advanced hematologic malignancies. Clin Cancer Res. 2008;14:8295–8301. doi: 10.1158/1078-0432.CCR-08-0999. [DOI] [PubMed] [Google Scholar]
- Hwang JJ, Kuruvilla J, Mendelson D, Pishvaian MJ, Deeken JF, Siu LL, et al. Phase I dose finding studies of obatoclax (GX15-070), a small molecule pan-BCL-2 family antagonist, in patients with advanced solid tumors or lymphoma. Clin Cancer Res. 2010;16:4038–4045. doi: 10.1158/1078-0432.CCR-10-0822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oki Y, Copeland A, Hagemeister F, Fayad LE, Fanale M, Romaguera J, et al. Experience with obatoclax mesylate (GX15-070), a small molecule pan-Bcl-2 family antagonist in patients with relapsed or refractory classical Hodgkin lymphoma. Blood. 2012;119:2171–2172. doi: 10.1182/blood-2011-11-391037. [DOI] [PubMed] [Google Scholar]
- Parikh SA, Kantarjian H, Schimmer A, Walsh W, Asatiani E, El-Shami K, et al. Phase II study of obatoclax mesylate (GX15-070), a small-molecule BCL-2 family antagonist, for patients with myelofibrosis. Clin Lymphoma Myeloma Leuk. 2010;10:285–289. doi: 10.3816/CLML.2010.n.059. [DOI] [PubMed] [Google Scholar]
- Goard CA, Schimmer AD. An evidence-based review of obatoclax mesylate in the treatment of hematological malignancies. Core Evid. 2013;8:15–26. doi: 10.2147/CE.S42568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart AK. Novel therapeutics in multiple myeloma. Hematology. 2012;17 (Suppl 1:S105–S108. doi: 10.1179/102453312X13336169156131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oltersdorf T, Elmore SW, Shoemaker AR, Armstrong RC, Augeri DJ, Belli BA, et al. An inhibitor of Bcl-2 family proteins induces regression of solid tumours. Nature. 2005;435:677–681. doi: 10.1038/nature03579. [DOI] [PubMed] [Google Scholar]
- Brinkmann K, Hombach A, Michael Seeger J, Wagner-Stippich D, Klubertz D, Kronke M, et al. SMAC mimetic potentiates tumor susceptibility towards natural killer cell-mediated killing. Leuk Lymphoma. 2014;55:645–651. doi: 10.3109/10428194.2013.807925. [DOI] [PubMed] [Google Scholar]
- Chauhan D, Velankar M, Brahmandam M, Hideshima T, Podar K, Richardson P, et al. A novel Bcl-2/Bcl-X(L)/Bcl-w inhibitor ABT-737 as therapy in multiple myeloma. Oncogene. 2007;26:2374–2380. doi: 10.1038/sj.onc.1210028. [DOI] [PubMed] [Google Scholar]
- Konopleva M, Contractor R, Tsao T, Samudio I, Ruvolo PP, Kitada S, et al. Mechanisms of apoptosis sensitivity and resistance to the BH3 mimetic ABT-737 in acute myeloid leukemia. Cancer Cell. 2006;10:375–388. doi: 10.1016/j.ccr.2006.10.006. [DOI] [PubMed] [Google Scholar]
- Kuroda J, Puthalakath H, Cragg MS, Kelly PN, Bouillet P, Huang DC, et al. Bim and Bad mediate imatinib-induced killing of Bcr/Abl+ leukemic cells, and resistance due to their loss is overcome by a BH3 mimetic. Proc Natl Acad Sci USA. 2006;103:14907–14912. doi: 10.1073/pnas.0606176103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tse C, Shoemaker AR, Adickes J, Anderson MG, Chen J, Jin S, et al. ABT-263: a potent and orally bioavailable Bcl-2 family inhibitor. Cancer Res. 2008;68:3421–3428. doi: 10.1158/0008-5472.CAN-07-5836. [DOI] [PubMed] [Google Scholar]
- Ackler S, Mitten MJ, Foster K, Oleksijew A, Refici M, Tahir SK, et al. The Bcl-2 inhibitor ABT-263 enhances the response of multiple chemotherapeutic regimens in hematologic tumors in vivo. Cancer Chemother Pharmacol. 2010;66:869–880. doi: 10.1007/s00280-009-1232-1. [DOI] [PubMed] [Google Scholar]
- Wilson WH, O'Connor OA, Czuczman MS, LaCasce AS, Gerecitano JF, Leonard JP, et al. Navitoclax, a targeted high-affinity inhibitor of BCL-2, in lymphoid malignancies: a phase 1 dose-escalation study of safety, pharmacokinetics, pharmacodynamics, and antitumour activity. Lancet Oncol. 2010;11:1149–1159. doi: 10.1016/S1470-2045(10)70261-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souers AJ, Leverson JD, Boghaert ER, Ackler SL, Catron ND, Chen J, et al. ABT-199, a potent and selective BCL-2 inhibitor, achieves antitumor activity while sparing platelets. Nat Med. 2013;19:202–208. doi: 10.1038/nm.3048. [DOI] [PubMed] [Google Scholar]
- Vandenberg CJ, S Cory. ABT-199, a new Bcl-2-specific BH3 mimetic, has in vivo efficacy against aggressive Myc-driven mouse lymphomas without provoking thrombocytopenia. Blood. 2013;121:2285–2288. doi: 10.1182/blood-2013-01-475855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touzeau C, Dousset C, Le Gouill S, Sampath D, Leverson JD, Souers AJ, et al. The Bcl-2 specific BH3 mimetic ABT-199: a promising targeted therapy for t(11;14) multiple myeloma. Leukemia. 2014;28:210–212. doi: 10.1038/leu.2013.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan R, Hogdal LJ, Benito JM, Bucci D, Han L, Borthakur G, et al. Selective BCL-2 inhibition by ABT-199 causes on target cell death in acute myeloid leukemia Cancer Discov 2014. e-pub ahead of print 13 February 2014; doi: 10.1158/2159-8290.CD-13-0609 [DOI] [PMC free article] [PubMed]
- Khaw SL, Merino D, Anderson MA, Glaser SP, Bouillet P, Roberts AW, et al. Both leukaemic and normal peripheral B lymphoid cells are highly sensitive to the selective pharmacological inhibition of pro-survival Bcl-2 with ABT-199 Leukemia 2014. e-pub ahead of print 9 January 2014; doi: 10.1038/leu.2014.1 [DOI] [PubMed]