Abstract
SUMMARY
Enteric pathogens such as Salmonella enterica cause significant morbidity and mortality. S. enterica serovars are a diverse group of pathogens that have evolved to survive in a wide range of environments and across multiple hosts. S. enterica serovars such as S. Typhi, S. Dublin, and S. Gallinarum have a restricted host range, in which they are typically associated with one or a few host species, while S. Enteritidis and S. Typhimurium have broad host ranges. This review examines how S. enterica has evolved through adaptation to different host environments, especially as related to the chicken host, and continues to be an important human pathogen. Several factors impact host range, and these include the acquisition of genes via horizontal gene transfer with plasmids, transposons, and phages, which can potentially expand host range, and the loss of genes or their function, which would reduce the range of hosts that the organism can infect. S. Gallinarum, with a limited host range, has a large number of pseudogenes in its genome compared to broader-host-range serovars. S. enterica serovars such as S. Kentucky and S. Heidelberg also often have plasmids that may help them colonize poultry more efficiently. The ability to colonize different hosts also involves interactions with the host's immune system and commensal organisms that are present. Thus, the factors that impact the ability of Salmonella to colonize a particular host species, such as chickens, are complex and multifactorial, involving the host, the pathogen, and extrinsic pressures. It is the interplay of these factors which leads to the differences in host ranges that we observe today.
INTRODUCTION
Enteric pathogens are a major source of morbidity and mortality throughout the world. It has been estimated that there are more than 3 million deaths associated with Gram-negative enteric pathogens worldwide due to diarrhea and enteric fever each year (1). Bacteria of genera such as Escherichia, Campylobacter, Vibrio, Brucella, Shigella, Yersinia, and Salmonella are responsible for causing enteric diseases. Infections by these pathogens manifest as several disease syndromes, including secretory/noninflammatory diarrhea, inflammatory diarrhea, and enteric fever (2). The differences in disease manifestations are related to the different virulence factors present in the bacteria and the altered phenotypes that these virulence factors allow the organisms to employ during disease pathogenesis.
Noninflammatory or secretory diarrhea is characterized by watery stools without the presence of white blood cells in feces. Patients generally do not develop a high fever. The diarrhea is associated with bacterial release of enterotoxin or their superficial adherence to the lumen of the proximal small intestine (3). Bacteria that are associated with secretory diarrhea include Vibrio cholerae and enterotoxigenic, enteroaggregative, or enteropathogenic pathotypes of Escherichia coli (2, 4–6). Diarrheal disease is typically associated with the interaction of the bacterial toxins with the host epithelium, leading to disruption of ion transport systems and subsequent fluid secretion that is the hallmark of diarrhea (7).
In contrast to secretory diarrhea, inflammatory diarrhea typically involves invasion of the colonic epithelium by bacterial pathogens, which may produce cytotoxins. Stool samples typically contain white blood cells, especially neutrophils, and patients often have fever associated with the illness (3). Bacteria associated with causing inflammatory diarrhea include Campylobacter jejuni, Shigella spp., nontyphoidal Salmonella enterica, and enteroinvasive E. coli (2). These organisms generally utilize mechanisms such as type III secretion systems (T3SSs) (described in detail below) to interact with the host cell's cytoskeletal system to facilitate invasion (8, 9). The cytoskeletal arrangements lead to the pathogens being internalized, where they reside predominantly in either a protected vesicle (Salmonella and Campylobacter) or the host cell cytoplasm (Shigella and enteroinvasive E. coli) (9, 10). During the attachment and internalization processes, the innate immune system can become activated through the recognition of pathogen-associated molecular patterns (PAMPs) on the surface of the pathogens (11, 12). These PAMPs include molecules such as lipopolysaccharide (LPS) and flagella that are recognized by Toll-like receptors (TLRs) on the surface of the host cells, which leads to an antibacterial response that is characterized by increased vascular permeability and the attraction of neutrophils to the site of infection (2). This response leads to the development of inflammatory diarrhea, in which the watery stool contains elevated levels of neutrophils.
Enteric fever is associated with invasive organisms that typically initially invade the distal small intestine and spread to underlying tissues and other parts of the host. Patients generally develop a high fever, and fecal samples contain white blood cells, which are predominantly monocytes and lymphocytes (3). Bacteria associated with enteric fever include typhoidal S. enterica and Brucella spp. (2). These organisms generally cause severe disease that is characterized by a disseminated infection in different parts of the body. The immune response to enteric fever is characterized by interstitial inflammation associated with mononuclear cell infiltration rather than a strong neutrophil response (3, 13). In S. enterica serovar Typhi, the presence of Salmonella pathogenicity island 7 (SPI-7) and factors encoded in its viaB locus, including the Vi capsular antigen, prevents recognition of PAMPs on the cell surface, such as LPS and flagella, by TLR4 and TLR5, respectively. Activation of these TLRs is associated with increased vascular permeability and neutrophil attraction associated with inflammatory diarrhea (14). Brucella spp. employ a distinct approach from that employed by S. Typhi to evade recognition by TLR4 and TLR5, in that Brucella spp. have modified LPS and flagellin structures that are not efficiently recognized by TLRs (15, 16). The ability to evade recognition by the innate immune system allows the organisms to establish systemic infections associated with enteric fever (2).
Of these enteric pathogens, one of the most commonly detected, in terms of both numbers of human infections and severity of disease (numbers of hospitalizations and deaths associated with infections), is Salmonella enterica (17). Salmonellosis can be manifested through different syndromes, including gastroenteritis, enteric fever (typhoid fever), and bacteremia, and as asymptomatic carriage in animals and humans (18). There are approximately 1.03 million cases of nontyphoidal Salmonella that occur each year in the United States, costing the economy approximately $3.31 billion due to premature mortality, disability, and medical and productivity costs, with an annual loss of 16,782 quality-adjusted life years (QALYs) (19). Compared to cost-of-illness figures (medical, employment, and death), the QALY losses also incorporate “psychometric scales” to quantify adverse health status due to people's discomfort and their abilities to engage in routine day-to-day activities following infection (19). Salmonella has adapted to survive in a wide range of different environments, such that a large number of human infections are associated not only with food animal sources but also with pets, reptiles, fruits, vegetable, legumes, and other humans (20–22). Among these sources, poultry and poultry-associated products are widely recognized as being among the most important vehicles for human Salmonella infections (20, 23). Therefore, S. enterica associated with chickens is likely a good model to explore bacterial host adaption and pathogenesis, which is a key focus of this review.
OVERVIEW OF SALMONELLA COLONIZATION AND PATHOGENESIS
The genus Salmonella is broken up into three different species, S. bongori, S. enterica, and S. subterranea (24, 25). Previously, the genus was broken up into many more species, with each individual serotype being considered its own species. The genus was subsequently divided into seven subgenera (I, II, IIIa, IIIb, IV, V, and VI) based on biochemical and genetic properties (24). As more advanced genetic techniques such as DNA-DNA hybridization were used to analyze the members of the genus, it was discovered that many of the serotypes shared a high degree of genetic similarity. Consequently, the genus was divided into two species, S. enterica and S. bongori, with S. bongori containing the members of subgenus V and S. enterica containing the members of the remaining six subgenera (24). S. subterranea was described as a species in 2005 (25). Serotypes in what is now S. enterica subspecies enterica (subspecies I) are the predominant pathogens associated with birds and mammals (24).
Within subspecies I, there is a diversity of Salmonella serotypes that infect different animal hosts. The ability of different Salmonella serotypes to survive and thrive in different host environments involves a number of interconnected factors, including differences in host environments (pH, temperature, and sites of attachment, etc.), the host immune system and its response to different serotypes, the commensal organisms present, and the genetics of the pathogen itself (26, 27). Many serotypes, such as those most commonly associated with human infections, including S. Enteritidis, S. Typhimurium, S. Newport, and S. Heidelberg, have a broad host range, with the ability to infect multiple host species (28). Conversely, other serotypes, such as S. Typhi, S. Paratyphi, S. Gallinarum, S. Choleraesuis, S. Abortusovis, and S. Dublin, have restricted host ranges and are associated primarily with one or a few hosts (29). S. Dublin and S. Choleraesuis are typically associated with cattle and swine, respectively; however, they also cause infections in humans (30–33). Human infections caused by these narrow-host-range serotypes tend to be fewer (with the exception of human-associated serotypes such as S. Typhi and S. Paratyphi) yet typically more severe in disease outcome. Data from the Centers for Disease Control and Prevention (CDC) FoodNet Program indicate that over 50% of human cases of S. Typhi, S. Dublin, S. Paratyphi A, and S. Choleraesuis infections are invasive rather than limited to gastroenteritis (34). Lower percentages of infections by the broader-host-range serotypes, such as S. Typhimurium (6%), S. Enteritidis (6%), and S. Heidelberg (11%), are invasive in nature (34).
Initial Colonization of the Host
The primary route of infection in humans and animals is through fecal-oral transmission of Salmonella. Salmonella pathogenesis has been studied mostly as it relates to human infections, while there is more limited information about the mechanisms of colonization and pathogenesis in food animals such as chickens. In general, when food contaminated with Salmonella is ingested, the bacteria have to pass through the alimentary system and survive the acidic environment of the stomach. Salmonella has been found to respond to the acidic environment through a complex adaptive system, called the acid tolerance response, which requires the synthesis of over 50 acid shock proteins, including the RpoS σ-factor, PhoPQ, Ada, and Fur (35, 36). Bearson et al. reported that S. Typhimurium RpoS and PhoPQ provided protection against inorganic acids, while RpoS and FurR offered protection against organic acids (35).
Those Salmonella organisms that survive the low-pH environment proceed to the lumen of gastrointestinal tract (GIT) organs, including the small intestine, colon, and cecum (in poultry). Epithelial and immune cells lining these GIT organs provide the initial protective barrier against Salmonella in the gut. Salmonella competes with the gut microflora to make the initial contact with enterocytes or M cells in order to colonize the GIT (37, 38). Adhesion to the GIT epithelium by Salmonella is facilitated by flagella and fimbriae present on the bacterial cell surface (39, 40). Studies have shown that Salmonella serovars employ both conserved and host-specific factors that facilitate colonization in the host GIT (41). Signature-tagged mutagenesis studies have reported the ability of multiple S. Typhimurium transposon mutants to colonize intestinal tracts of mice, calves (2), chickens, and pigs (42, 43). In addition to the oral-GIT route of invasion, Salmonella bacteria have been reported to invade and disseminate in swine and cattle following uptake in the tonsils and respiratory system (44, 45).
Invasion of Host Cells
Once attached to the intestinal epithelium, Salmonella bacteria typically express a T3SS, which is a multiprotein complex that facilitates endothelial uptake and invasion (28, 46). The T3SS apparatus acts as a “molecular syringe” (a conduit between the bacterial cytoplasm and the host cell membrane) to transport toxins and other effector proteins into intestinal cells and is associated with over 20 structural and regulatory proteins (47–49). Several effector proteins, such as InvJ, SpaO, PrgI/J, SipA/B/C/D, SptP, AvrA, SopA/B/D/E/E2, SlrP, and SspH1, are also secreted through the T3SS (47, 50, 51). The T3SS machinery is associated with SPI-1, which harbors virulence genes involved in Salmonella adhesion, invasion, and toxicity (see below for details on SPIs). The structural apparatus of the SPI-1 T3SS has been reported to be vital for invasion of bovine and porcine ileal mucosa by Salmonella (41).
Among the effector proteins that are translocated through the T3SS, SopB plays an important role in the activation of secretory pathways, facilitating inflammation (by attracting neutrophils to the sites of infection) and altering ion balances within cells, leading to secretion of fluids in the GIT and consequent diarrhea (52, 53) in humans (54) and cattle (55). Other translocated proteins, such as SopA, SopD, SopE2, and SipA, have been found to play a role in Salmonella gastroenteritis (53). Effector proteins such as SipA, SipC, and SopB can interact with the actin cytoskeleton, causing the host cell membrane to extend outwards, a process referred to as membrane ruffling (50). This ruffling process facilitates engulfment of the Salmonella cells by the host cell membrane and internalization in a membrane-bound compartment termed a Salmonella-containing vacuole (SCV) (56–58). As the SCV matures, it migrates from the luminal border to the basal membrane, thus avoiding destruction by the phagolysosomal processing pathways (59).
The SCVs play key roles in survival and proliferation of Salmonella in intestinal cells and macrophages (60). Once internalized into host cells, Salmonella cells express a second T3SS encoded on SPI-2 (SPI-2 T3SS) within the SCV that plays a critical role in causing systemic infections and intracellular pathogenesis (61). The SPI-2 T3SSs are responsible for secreting effector proteins in the SCV, and these proteins interact with the cytoskeleton and motor proteins, leading to the formation of Salmonella-induced filaments (SIFs), which project out of the SCV (28). Furthermore, SPI-2 T3SSs have been reported to modulate trafficking of the SCV to avoid fusion with the lysosomes (41). Several effector proteins, such as SpiC, PipB, SseF/G/I/J, SifA/B, SspH1/H2, SlrP, SopD2, and phage-located SrfA/B/C/D/E/G/I/J/K/L/M, are secreted through the SPI-2 T3SS (62). The SIF facilitates fusion of SCVs with other vesicles in the cell and may play a role in Salmonella replication (58, 61, 63); the precise role of SIFs in Salmonella infections remains unclear (28).
Survival in Macrophages and Dendritic Cells
In a small percentage of cases, Salmonella cells are able to replicate within host cells, evade immune responses, and develop invasive and systemic infections (2, 37). These severe manifestations of salmonellosis usually occur when Salmonella cells invade macrophages or dendritic (migratory phagocyte) cells. Salmonella cells have been shown to be able to multiply within macrophages (64) but do not appear to replicate within dendritic cells, even though they remain viable (60). The exact mechanisms for the differences in Salmonella responses within different immune cell types are not entirely clear, as several pathogen and host factors may play roles (65). Dendritic cells are widely distributed in the lymphoid and nonlymphoid tissues and can rapidly facilitate the spread of Salmonella cells to various organs of the host body (66). Researchers have shown that the SPI-2 T3SS in Salmonella harbors genes that can suppress antigenic presentation in dendritic cells, which limits the host immune response to infected cells (62). In general, the ability of Salmonella to cause an infection in humans or animals depends on the innate ability of the bacteria to encode and express a set (or combination) of virulence genes that can evade and neutralize host defenses. These factors are associated with pathogenicity islands, virulence plasmids, toxins, fimbriae, and flagella (28, 40, 67–69).
Salmonella Pathogenicity Islands
The ability of Salmonella to efficiently colonize the host has been attributed to gene clusters, such as SPIs, encoding virulence factors that are distributed in the Salmonella genome (28). Several major pathogenicity islands have been reported for different serovars, with SPI-1 to -5 being present in most serovars and others being less widely distributed (28, 69–71). In general, SPI-1 is required for invasion of host cells and induction of macrophage apoptosis, SPI-2 is required for systemic infection and replication within macrophages, SPI-3 is required for survival in macrophages and the ability of Salmonella to grow in low-magnesium environments, SPI-4 is required for intramacrophage survival and harbors genes for toxin secretion and apoptosis, SPI-5 has been found to cluster genes that encode multiple T3SS effector proteins, and SPI-6 has been found to transport proteins into the environment or host cells in response to external stimuli (28, 40, 41, 69, 70, 72, 73). Amavisit et al. reported genetic variations among SPI-1, -3, and -5, while SPI-2 and -4 were well conserved among 13 different Salmonella serovars isolated from warm-blooded animals (bovine, porcine, avian, and equine), the environment, and human patients in their study (73). Those authors found that, with the exception of S. Typhimurium, all isolates within the same serovar were identical with regard to the five SPIs that were tested. SPI-1 and SPI-2 have been found to play a role in Salmonella persistence and enteritis in chickens (43, 74), cattle (75–77), pigs (42), and humans (37). Fibronectin-binding proteins, encoded by SPI-3, facilitate host-specific Salmonella colonization. For example, MisL contributes to Salmonella colonization in mice, chickens, and pigs but does not play a significant role in calves (42, 43), while ShdA influenced S. Typhimurium persistence in mice but not in pigs (78, 79). SPI-4 has been reported to mediate adherence to and invasion of bovine ileal mucosa, possibly in combination with the SPI-1 T3SS, but not in chickens and pigs (41, 43, 80).
Virulence Plasmids
Strains from several Salmonella serovars have serotype-specific virulence plasmids (81). These are low-copy-number plasmids (1 to 2 copies per cell) and range from 50 to 100 kb, depending on the serovar (40). Each of the plasmids contains the Salmonella plasmid virulence (spv) locus, whose expression has been reported to be important for multiplication of Salmonella in the reticuloendothelial system, including the liver and spleen (40, 82). Other plasmids, in addition to the serotype-associated virulence plasmids, also likely contribute to the observed resistance among Salmonella bacteria. Recent studies from our laboratories have identified several different plasmids that potentially contribute to virulence in serovars such as S. Heidelberg, S. Kentucky, and S. Typhimurium (83, 84). A more in-depth exploration of plasmid-associated virulence is presented below.
Toxins
Salmonella pathogenicity has also been attributed to the production of endo- and exotoxins. Endotoxins have been found to elicit a wide range of biological responses, while exotoxins, comprising cytotoxins and enterotoxins, have the ability to kill mammalian cells (85). Ashkenazi et al. reported that Salmonella serovars Choleraesuis, Enteritidis, and Typhi produced heat-labile, trypsin-sensitive cytotoxins with various molecular masses, including 56 kDa (S. Typhi), 70 kDa (S. Typhimurium), and 78 kDa (S. Choleraesuis) (85). A Shigella dysenteriae 1-like cytotoxin has been detected in Salmonella serovars Enteritidis, Kapemba, and Thompson (86). Two other types of exotoxins, salmolysin (encoded by the slyA gene) and Salmonella enterotoxin (Stn; encoded by the stn gene), have been identified in Salmonella serovars Typhi, Typhimurium, and Enteritidis (87, 88).
Fimbriae
Fimbriae (pili) are filamentous surface structures that contribute to the colonization of the epithelium by Salmonella (89). Each of the fimbrial operons contains multiple genes (typically 8 to 11) that encode the structure and assembly of fimbrins (fimbria proteins) (90). Several fimbrial operons, ranging from 7 to 9 kb in size, have been identified in Salmonella. The sequenced strain S. Enteritidis PT4 has 13 fimbrial operons (91). Some examples of fimbrial operons include the agf and sef operons, which encode the S. Enteritidis fimbria SEF17 (92, 93); the pil operon (located in SPI-7) in S. Typhi CT18 (94); and the lpf (long polar fimbriae) and pef (plasmid-encoded fimbriae) operons in S. Typhimurium (95, 96). The SEF14 fimbriae have been found to be expressed by S. Enteritidis, S. Dublin, and poultry-associated Salmonella serovars Berta and Gallinarum, where they appear to be important for adhesion of these serovars to tissues of the reproductive tract (97, 98). Type I fimbriae contribute to Salmonella colonization of pigs (99), while 13 major fimbrial subunits of S. Enteritidis PT4 have been found to play a role in adherence and colonization of the bacteria in chicken gut (100, 101); the loci on which these subunits were detected were conserved in S. Paratyphi and S. Gallinarum. A detailed distribution of fimbrial operons among Salmonella subspecies and serovars was highlighted in a review by van Asten and van Dijk (40).
Flagella
The majority of Salmonella serovars possess up to 10 randomly positioned flagella on their cell surface, which confer motility to these bacteria (40). The ability of certain serovars to display flagellin phase variation provides a potential means for the organisms to minimize the host immune response by creating phenotypic heterogeneity of the flagellar antigens (40). The fliC gene, encoding the phase 1 flagellin protein, has been found in Salmonella serovars Gallinarum and Enteritidis (102). However, the exact role of flagella (motility and direction of rotation) in Salmonella pathogenesis and their possible role in adhesion and invasion of mammalian cells remain unclear (40).
Other Virulence Factors
Virulence factors such as surface polysaccharides may also play a role in persistence of Salmonella in the intestinal tract. Multiple mutants affecting lipopolysaccharide (LPS) biosynthesis have been identified in Salmonella strains isolated from calves and chickens (41–43, 103). For example, the virulence of the LPS rfbK, dksA, hupA, sipC, and ptsC mutants and clpB and rfaY transductants was studied in 1-day-old chicks by Turner and coworkers (103). That study showed that all but the ptsC and rfaY mutants were attenuated for virulence in chickens. Signature-tagged mutagenesis showed that LPS S. Typhimurium mutants (rfaK, rfaB, rfaG, rfbP, rfbN, rfbU, rfbH, and rfbA) were unable to colonize calf intestines, suggesting a role of surface polysaccharides and cell envelope proteins as virulence factors contributing to S. Typhimurium colonization of calves (43). LPS has been found to contribute to the ability of S. Enteritidis to survive in egg albumen (104). That study showed that a mutant strain unable to produce LPS (ΔrfbH) was not able to multiply in eggs at room temperature and did not survive in egg whites at 42°C. Those authors concluded that attenuation increased susceptibility of the ΔrfbH mutant to undefined antibacterial components of egg albumen (104).
IMPACT OF HORIZONTAL GENE TRANSFER ON GENOME EVOLUTION AND HOST RANGE
There are two major, seemingly opposite, evolutionary approaches in bacteria that impact the range of hosts which an organism can infect and in which it can survive; these approaches are gene acquisition through horizontal transfer and gene or gene function loss (105, 106). Salmonella serotypes have expanded their host ranges through the acquisition of new genes through horizontal gene transfer of plasmids and pathogenicity islands, which in turn provide genetic factors that increase the ability to infect new hosts. The addition of these pathogenicity islands to the Salmonella genome led to the ability to invade host cells and persist in causing disease. Some transfer events happened more recently, and thus, not all Salmonella serovars have acquired the clusters, while other events happened more distantly, and thus, the gene clusters are present in multiple lineages of S. enterica (73). There are five SPIs (SPI-1 to -5) that have been found to be important for the ability of Salmonella to become pathogenic relative to the commensal E. coli (107). It is estimated that 5 to 7% of the genes in the Salmonella genome play a role in virulence; interestingly, many of these genes are also present in the commensal E. coli; however, they alone are not enough to cause disease (108, 109).
It has been hypothesized that Salmonella virulence evolved in a multistep fashion, starting with the acquisition of SPI-1 by all Salmonella bacteria and acquisition of additional SPIs distinguishing S. enterica from S. bongori, followed by expansion of the host range to warm-blooded vertebrates (110). The SPIs, with the exception of a few, are highly conserved across members of the species S. enterica but are absent from closely related species such as S. bongori and E. coli (111). While most of the SPIs are not likely to retain their mobility, the ability of some Salmonella genomic islands to excise and transfer has been demonstrated. This excision is also inducible for some regions upon exposure to host conditions, such as macrophage survival and oxidative stress (112).
Integrative conjugative elements (ICEs) are also present in Salmonella. ICEs appear to be major players in the horizontal transfer of genetic material between bacterial species, as they carry genes required for their own excision and transfer to recipient bacteria (113). This is exemplified in Salmonella by SPI-7, an ICE that is present in Salmonella but also among a variety of other Enterobacteriaceae (114). SPI-7 ICEs have been found in both S. enterica and S. bongori and in other bacterial species, and they appear to be evolutionarily related, suggesting that both inter- and intraspecies ICE transfer occurs and further enhances ICE diversity (115).
Role of Plasmids in Salmonella Genome Evolution
Considerable research has focused on the plasmids that circulate among Salmonella populations of humans and animals, and there is no doubt that plasmids are indigenous to Salmonella. Evidence for this exists through a straightforward analysis of the historical ECOR and SAR reference collections, which reveal a great deal of diversity among their plasmids and an abundance of plasmids in strains of both collections (116). Indeed, a variety of plasmid types have been found among Salmonella isolates, including those of incompatibility (Inc) types IncA/C, IncF, IncH, IncI, IncL/M, IncN, IncR, and IncX (117–122). What seems to have changed over time is the accessory gene content that these plasmids carry. It can be argued that genes encoding antimicrobial resistance are omnipresent in microbial populations and that they surface under selective pressure. While this is likely true, it is difficult to argue against the notion that multidrug resistance has increased among clinical Salmonella isolates. Historical isolates generally lack phenotypic resistance patterns but still contain plasmids. In contrast, contemporary Salmonella isolates still harbor plasmids, but many seem to have evolved in the face of selective pressures to acquire resistance-associated gene arrays. The purpose of this section is not to document the hundreds to thousands of articles that have demonstrated the presence of plasmids among Salmonella but to instead present insights into the impact of their presence on genome evolution.
Salmonella virulence plasmids have been considered a defining trait of Salmonella serotypes involved in systemic disease. These plasmids range in size from approximately 50 to 100 kb and are found in numerous serovars, including S. Typhimurium, S. Enteritidis, S. Dublin, S. Choleraesuis, and S. Gallinarum (123). The Salmonella virulence plasmid harbors several key virulence factors, including the spvABCD system and its regulator spvR, which are essential for systemic virulence and are induced upon exposure to nutrient-limited conditions and host cells, particularly macrophages (124–126). These genes are also sufficient to restore systemic virulence in plasmid-cured strains (127). These genes appear to be horizontally acquired on an IncFIIA/IncFIB plasmid backbone, since they have a lower G+C content than the core plasmid (71). There are multiple lineages of the Salmonella virulence plasmid that are correlated with a respective serovar, and the virulence plasmids among these lineages have uniquely evolved (Fig. 1). The plasmids sequenced and analyzed thus far can be broadly distributed into three major lineages, and it appears that they have evolved through a combination of gene acquisition and deletion events.
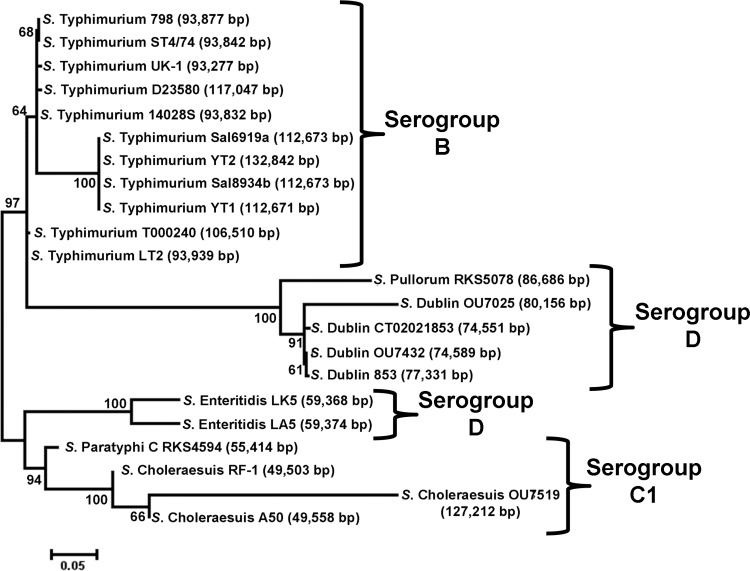
Fig 1.
Evolutionary history of Salmonella virulence plasmids inferred by using the maximum likelihood method, based on the Hasegawa-Kishino-Yano method. The bootstrap consensus tree was inferred from 100 bootstrap replicates. Analysis was based on 441 SNPs identified from the conserved sequences of 22 plasmids. Analysis was conducted with MEGA5 (403).
Several possible scenarios for the evolution of Salmonella virulence plasmids have been proposed (123, 128). It is possible that an ancestral IncFIIA spv+ plasmid present in serogroup D isolates diverged into other serogroups and acquired additional traits. A more likely scenario based upon recent work is that an ancestral plasmid type possessed an IncFIIA/IncFIB backbone containing spv, prf, and pef and separated following the divergence of serogroups and that the plasmid lineages subsequently underwent recombination events, resulting in the current virulence plasmid profiles. Interestingly, there is little evidence of extensive transfer of virulence plasmids among the Salmonella serovars, even though their transfer in vivo has been documented (129). The horizontal transfer of these plasmids is likely a neutral trait in Salmonella, and thus, transfer between serovars is not strongly selected (130, 131). In fact, not all strains of serotypes that typically contain virulence plasmids have them; this lack of virulence plasmids is likely reflective of differences in the strain's genetic background that impact the ability to utilize the plasmid for establishing systemic disease (132).
The S. Typhimurium virulence plasmid has also been shown to be capable of carrying resistance-associated integrons and transposons (133, 134). Cointegrated plasmids have surfaced in S. Dublin which include regions of the Salmonella virulence plasmid and plasmids of other incompatibility groups, such as IncX, encoding multidrug resistance (135). This could aid in the expansion of the host range of this plasmid to additional Salmonella serovars (136). Cointegrated IncFIB-IncI1 plasmids have also been identified among sequenced Salmonella genomes, and they have been found to belong to a unique clade of IncI1-type plasmids and harbor a unique subset of putative virulence genes (115). Certainly, cointegrated plasmids offer an increased potential to harbor more diverse arrays of resistance-associated genes and to expand host range and transmissibility.
In addition to virulence plasmids, Salmonella bacteria also harbor a variety of other plasmid types. It seems that the spread of such plasmids, in contrast to the Salmonella virulence plasmid, occurs primarily via horizontal gene transfer (137). Resistance-associated plasmids are found among a wide range of Salmonella serovars, in a variety of shapes and sizes (138–140). Plasmids belonging to groups such as IncI1, IncH, IncN, and IncX are not considered emergent in Salmonella, as they have been isolated from this genus for many years (118, 141). However, they appear to be actively evolving to acquire resistance genes with relevance to therapeutic antibiotics used in humans and animals. In contrast, IncA/C plasmids are not found in historical collections of Salmonella isolates but have recently emerged among Salmonella, E. coli, and Klebsiella pneumoniae isolates (142). The emergence of IncA/C plasmids among Salmonella isolates has often coincided with the emergence of dominant clonal types, such as serotype 4,[5],12:i:− in Spain (143). In some cases, IncA/C plasmids appear to have integrated into the Salmonella genome. A case in point was highlighted by a study by Shahada et al., which identified a unique 125-kb genomic island among isolates of a dominant clone of S. Typhimurium from cattle in Japan. This island, named GI-VII-6, displayed striking similarities to portions of IncA/C plasmids containing three copies of blaCMY-2 (144).
Other resistance plasmids are also emerging, with increased concern to health. IncN plasmids found in Salmonella and E. coli were recently associated with possession of genes encoding quinolone resistance (122, 145, 146). IncHI1 and IncHI2 plasmids have been linked to quinolone resistance-encoding genes, extended-spectrum beta-lactamase (ESBL) genes, heavy metal resistance genes, and carriage of typical complex class 1 integrons (119, 147–149). IncI1 plasmids are widespread among Salmonella isolates and are notorious for their carriage of blaCMY and blaTEM genes (137–139). As mentioned above, IncA/C plasmids have been identified more recently among Salmonella isolates, and they carry large numbers of resistance-associated genes, including blaCMY-2, on a conjugative transposon encoding resistance to third-generation cephalosporins; a gene module containing floR-strAB-tetAR, encoding resistance to chloramphenicol-florfenicol, streptomycin-spectinomycin, and tetracycline; and a complex class 1 integron harboring a variety of resistance genes (121, 150, 151).
Small plasmids harboring quinolone resistance genes have been identified in both Salmonella and E. coli (122, 152, 153). More importantly, it exemplifies a mechanism for plasmid gene swapping via Xer- and oriT-mediated site-specific recombination. This mechanism of recombination can occur independently of conjugative transposons or integrons and could represent an additional means of genetic recombination involving plasmids. Other mechanisms of additional recombination potential exist on the Salmonella chromosome. For example, variant regions of Salmonella genomic island 1 (SGI-1) have been identified, which include additional resistance genes driven by IS6100-mediated recombination (154). A number of variants of SGI-1 that confer resistance to a variety of classes of antimicrobial agents have been identified (155).
In addition to plasmids being mobile themselves, they harbor a variety of mobile genetic elements within them, including integrons and conjugative transposons. Class 1 integrons are the most common type among Salmonella isolates and can be localized to the bacterial chromosome or plasmids. A large number of novel gene cassette arrays have been identified among class 1 integrons harbored by Salmonella, and some appear to have been derived recently from other bacterial species (156). These accessory regions are actively evolving on plasmids, as evidenced by recent comparative genomics-based studies of closely related plasmids with a variety of resistance island variations (149).
SGI-1 is a 43-kb accessory region of the Salmonella genome that contains a class 1 integron (In104) encoding resistance toward ampicillin, chloramphenicol-florfenicol, tetracycline, sulfamethoxazole, and streptomycin-spectinomycin, also known as classical “pentaresistance.” This region is found in many Salmonella isolates and, as mentioned above, is mobilizable. This alone enables a multidrug resistance phenotype, but the carriage of additional plasmids by SGI-1-containing strains is common (157). Interestingly, some plasmids have also been shown to enhance excision and variant formation of Salmonella genomic islands, such as the enhanced excision of SGI-1 by plasmids belonging to the IncA/C type (158, 159). In addition to enhancing the excision of chromosomal islands, these plasmids may also harbor receptor sites for phage recognition. For example, plasmids such as IncN and IncX have been shown to convert phage types among Salmonella strains (160, 161), and IncX plasmids seem to harbor phage recognition sites (162). Thus, when considering the role of plasmids in genome evolution, it is important to consider not only the accessory gene repertoire that they carry but also the modulations that they confer to the Salmonella host.
Horizontal transfer of individual mobile elements between different plasmids also occurs. There are numerous examples of this, but one of recent concern involves an emergent gene known as blaNDM-1, encoding the New Delhi metallo-beta-lactamase (163). The blaNDM-1 gene was originally identified among Klebsiella pneumoniae isolates from infections originating in India. However, it was quickly realized that this gene was plasmid borne, was present on multiple plasmid types (164–167), and was rapidly spreading between bacteria (168). The first report of blaNDM in Salmonella involved a patient with a Klebsiella pneumoniae infection that was resistant to carbapenems (169). Subsequent culturing identified NDM-positive Klebsiella and Salmonella within the patient, with blaNDM apparently residing on different plasmids in each bacterial isolate. There are many additional examples of genetic transfer between Salmonella and other bacterial species. For example, heavy metal resistance operon transfer from Klebsiella spp. and environmental bacteria to Salmonella has also been hypothesized (170). Certainly, plasmid transfer and plasmid gene transposition play a major role in the evolution of Salmonella (171).
Role of Bacteriophages in Salmonella Evolution
Bacteriophages are among the most diverse and abundant forms of microbial “life” on earth and have played important roles in bacterial evolution. Phages integrate into the host chromosome as a prophage, where they can impact expression of host factors as well as facilitate the transfer of DNA among bacteria through transduction (172, 173). There are at least 170 known phages that infect Salmonella, and these generally fall into five categories based on their genetic sequences, P27-like, P2-like, P22-like, lambdoid, and T7-like, along with outliers such as ε15, KS7, and Felix O1 (174). There is a large amount of diversity that is increasingly being revealed among phage families, which reinforces the idea that recombination is occurring frequently between subgroups of phages and between unrelated groups of phages (175).
The host ranges of Salmonella bacteriophages are variable, with some being highly host specific and others being generalists. An example of a generalist is ΦX174, which has been demonstrated to lyse >99% of Salmonella isolates tested (176). Thus, the susceptibility of an organism to phage lysis (often used to describe the phage type of the organism) does not necessarily correlate with clonality in all Salmonella strains. In contrast, the host specificity of other phages to lyse a narrow range of bacteria has been utilized for subtyping of Salmonella. Phage typing has historically been a method of choice for characterizing Salmonella. The method is still used for typing of bacteria but typically in conjunction with molecular techniques. For example, single-nucleotide polymorphism (SNP) typing has been used in combination with phage typing to explore relationships between host genetics and phage susceptibility in S. Typhimurium (177). This work demonstrated that the majority of isolates of particular phage types, such as definitive type 104 (DT104), had a single evolutionary origin, while S. Typhimurium isolates belonging to other phage types, such as DT9 and DT135, seemed to have originated from multiple lineages, indicating a broader host range of the typing phages (177). Phage typing has also identified potential geographical differences among isolates; for example, in the United States, isolates of phage type 8 are the most commonly detected S. Enteritidis isolates, compared to phage type 4 in Europe (178).
Phages have played significant roles in Salmonella virulence through the regulation of expression of virulence factors and the introduction of a number of effector proteins that are implicated in pathogenesis (179). A detailed understanding of the roles that bacteriophages play in Salmonella pathogenesis has been complicated by phage diversity and Salmonella strain diversity; however, it is becoming increasingly clear that phages do indeed play major roles in terms of delivering functional effector molecules and adding to the Salmonella virulence regulatory networks. For example, SopE2 and SspH2 are effector proteins encoded adjacent to phage-like sequences in Salmonella. Others, such as SopE, GogB, SseI, SspH1, and SseK3, are found directly on various prophages of Salmonella (179). The distribution of these phage-encoded effector molecules is often serovar and even strain specific, suggesting that they are indeed incorporated via transducing phage (180). In some cases, phage-mediated acquisition of traits may confer a fitness benefit in certain niches. For example, a SopE-encoding phage was identified primarily in cattle-associated epidemic isolates, suggesting that SopE may confer a reservoir advantage in cattle (181–183). Lambdoid phages such as Gifsy-1 and Gifsy-2 have been shown to be important for modulating virulence in S. Typhimurium. The Gifsy-1 prophage carries several potential virulence-associated genes, including gipA and gogB, which may play a role in colonizing the small intestine (184, 185). The Gifsy-2 prophage also carries multiple virulence factors, including gtgE, gtgB (sseI), and sodC1, which have been shown to be important for overall Salmonella virulence (184, 186).
Plasmids have been shown to alter the susceptibility of Salmonella to bacteriophages. In S. Enteritidis, IncN plasmid acquisition resulted in conversion of the phage type from type 4 to type 24 (160). Acquisition of IncX plasmids by S. Enteritidis has been show to induce resistance to multiple bacteriophage types, thereby altering the phage type profile and facilitating phage conversion (161). Low-molecular-weight plasmids have been shown to exert similar effects on S. Enteritidis as well (187). In contrast, the acquisition of some plasmids can result in increased phage susceptibility (188). The precise mechanisms of phage conversion relative to plasmid acquisition have not been intensively investigated, but there is certainly a relationship between the two. The clustered regularly interspaced short palindromic repeats (CRISPRs) may also play an important role in the defense of Salmonella against foreign DNA from incoming plasmids and phages. A comparative analysis of 28 sequenced Salmonella genomes demonstrated that CRISPR-mediated immunity among specific strains might control short-term phenotype changes and mediate long-term sublineage evolution (189). Thus, it is evident that bacteriophages reshape the Salmonella genome not only through their direct contributions to the host bacterium but also through indirect interactions with other mobile elements and cellular regulatory networks.
IMPACT OF THE LOSS OF GENES OR THEIR FUNCTION ON GENOME EVOLUTION AND HOST RANGE
The loss of genes or gene function can also impact genome evolution and host range due to the inactivation of genes needed to infect multiple hosts (106). Host-adapted strains of Salmonella have a relatively large number of pseudogenes and chromosomal rearrangements associated with recombination of the 16S ribosomal gene (rrn) operons that impact their host range (190, 191). Host-adapted serovars often demonstrate a high degree of rrn rearrangement within their genome, which is likely the result of the adaptation to the specific host niche that the serovar occupies. This view was consistent with the finding that host-adapted and host generalist strains demonstrated similar rates of rrn rearrangement, and as such, the differences were due to adaptation rather than having a more highly mutable genotype (192). Additionally, host-adapted serovars such as S. Typhi, S. Paratyphi A, S. Dublin, S. Choleraesuis, and S. Gallinarum have a relatively high percentage of pseudogenes in their genomes, especially compared to the broad-host-range Salmonella serovars Enteritidis and Typhimurium (193). Pseudogenes are genes that have been inactivated by insertion, deletion, or nucleotide substitution, leading to a failure to express the gene product associated with the original gene. For example, the genomes of Salmonella serovars Typhi and Paratyphi, which are human-adapted serovars, have >4% of the coding sequences in their genomes as pseudogenes, while for the non-host-restricted Salmonella serovar Typhimurium, only about 0.9% of the coding sequences are pseudogenes (194). A key consideration related to host adaptation is whether the presence of pseudogenes and the corresponding loss of function led to the host restriction or whether the increased number of pseudogenes was due to the serovars adapting to their new niches. Indeed, the accumulation of pseudogenes is likely due to host adaptation and subsequent genetic drift following adaptation to the new host niche (194). Approximately one-quarter of the genomes of Salmonella serovars Typhi and Paratyphi A have a high degree of nucleotide similarity to one another, while the remaining portions are more divergent, similar to the differences between the other serovars. It is likely that the region of higher similarity is due to recombination between the two human host-adapted serovars (194). Several (22) of the pseudogenes identified between Salmonella serovar Typhi and Paratyphi A isolates were outside the recombination region and thus likely arose independently in each the two serovars. However, since the pseudogenes were present in both serotypes, they may be important for survival in the human host niche. The pseudogenes identified included safE and sefD, which are fimbrial genes, and shdA, ratB, and sivH, which are involved in intestinal colonization and persistence, pathological features not typically associated with typhoid and paratyphoid infections and, as such, not essential for Salmonella serovars Typhi and Paratyphi A (194).
Based on genome analyses, it appears that Salmonella pseudogenes are typically removed from the genome relatively early following their formation. The removal is potentially associated with the fitness costs associated with the replication of now noncoding DNA in the bacterial genome: the expression of partial, nonfunctional genes or toxicities associated with partially expressed genes (195). This selective pressure to remove the non-fully active genes is evidenced in that the host-restricted serovars have higher Ka (number of nonsynonymous substitutions per nonsynonymous site)/Ks (number of synonymous substitutions per synonymous site) ratios than broad-host-range serotypes (195, 196). The higher Ka/Ks ratio is indicative of positive evolution selective pressure for genome change (195). Other studies with S. Typhi and S. Choleraesuis have found that the majority of pseudogenes are not expressed; however, some pseudogenes appear to have undergone recoding, such that there were secondary mutations that allowed expression of a functional protein (193). In contrast to full recoding, partial expression of truncated, non-fully functional proteins can potentially bind to receptors blocking the fully functional proteins from eliciting their roles in cellular physiology, thereby harming the bacterium (195).
Other factors also likely play a role in host range variability. These factors include the genetic adaptation of organisms to particular nutrients that are abundant in the host organism but limited in other environments (106). For example, in S. Gallinarum, there are multiple pathways associated with carbon and energy metabolism that are not functional, including the catabolism of d-glucarate and long-chain maltodextrins, which may limit their ability to survive in certain environments outside the avian host (191). Loss of gene function can also be associated with an increased ability to cause disease in some instances. A good example is Shigella species, where OmpT is absent, which reduces the early immune response to infection (105). S. Typhi is also able to modulate the early immune response through the repression of fliC expression, which limits the activation of TLR5 by the flagellin FliC (197). In both examples, the loss of the immune response facilitates the intracellular spread of the organism rather than being rapidly cleared with a stronger initial immune response.
EXAMPLES OF SALMONELLA HOST RANGE IN CHICKEN-RELATED SEROVARS
Because the diversity of the Salmonella enterica species is quite expansive, this section focuses primarily on the host range adaptation of four particular serovars (S. Enteritidis, S. Heidelberg, S. Kentucky, and S. Gallinarum) that are associated very commonly with chickens and to various extents with other food animal species and human infections. According to the CDC, in the United States, S. Enteritidis was the serovar most commonly implicated in human illness, overtaking S. Typhimurium as the most common serovar (198). Likewise, when data from the National Veterinary Services Laboratory of the USDA and from other studies examining the prevalence of Salmonella serovars were compared, S. Enteritidis was associated most commonly with chickens and eggs and to a much lesser extent with other food animal species (198–202). S. Heidelberg is found in most of the major food animal species, eggs, and retail meat samples and is among the top five most common serotypes associated with human illnesses (203, 204). Conversely, Salmonella serovars Kentucky and Gallinarum rarely cause human infections in the United States (although S. Kentucky is an emerging serovar in Europe and North Africa) (205). Salmonella serovar Gallinarum is a host-adapted serovar that is presently made up of two biovars, Gallinarum and Pullorum (which were previously considered two separate serotypes) (206). This serotype was associated with severe losses to the poultry industry in the United States until it was targeted for eradication by the National Poultry Improvement Plan (NPIP) starting in 1935 (207). After implementation of the NPIP, S. Gallinarum was eradicated from commercial poultry flocks in the United States by the mid-1960s (26).
S. Kentucky is currently one of the most common serotypes isolated from broiler chickens in the United States and is detected fairly often in dairy cattle as well (198). The increase in the rate of isolation of S. Kentucky in broilers is likely related to a number of factors, including management practices, flock immunity, and genetic changes in the organism (26). When S. Kentucky was compared to other serovars with respect to virulence, it was found that the S. Kentucky isolates grew more rapidly than other serovars under moderately acidic conditions (pH 5.5) but worse under more highly acidic conditions (pH 2.5) (208). The enhanced ability to grow under these moderately acidic conditions may provide an advantage over other serotypes in environments such as the chicken cecum. This serovar exhibited greater invasiveness in in vitro assays using chicken embryo hepatocytes than serovars such as S. Enteritidis and S. Typhimurium (208). Many S. Kentucky isolates also have plasmids with factors such as those associated with antimicrobial and disinfectant resistance, iron acquisition, bacteriocin production, and complement resistance, which may enhance their abilities to survive in birds (83).
It is interesting that S. Kentucky has not become a larger public health problem for consumers in the United States, as Salmonella from poultry is predicted to be the fourth most important pathogen-food combination associated with food-borne illnesses in the United States (20). It is quite probable that S. Kentucky strains most common in poultry are not overly virulent to humans. In analyzing the data from the CDC National Salmonella Surveillance Program (http://www.cdc.gov/ncidod/dbmd/phlisdata/salmonella.htm), the states with the largest numbers of human S. Kentucky infections were generally those associated with higher rates of dairy production rather than poultry production (198, 209). Likewise, several studies have utilized pulsed-field gel electrophoresis (PFGE) for the molecular characterization of S. Kentucky isolates from various sources (chickens, dairy cattle, and human infections); the most common profiles associated with human infections were similar/visually indistinguishable from common profiles from cattle but typically distinct from those of poultry (205, 210–212). Likewise, a majority of S. Kentucky strains isolated from poultry-associated sources fall into the sequence type 152 (ST152) clonal complex, while the majority of those isolated from human patients were of ST198 (205). Therefore, a plausible explanation for S. Kentucky-associated human infections could be due to occupational exposure to cattle or due to consumption of contaminated products such as raw (unpasteurized) milk or raw-milk cheeses. S. Kentucky has been one of the most commonly detected serotypes isolated from prepasteurized milk in the United States (213), and consumption of raw milk and raw-milk cheese has been associated with multiple outbreaks of salmonellosis (214–216).
For S. Heidelberg, there does not seem to be a strong association of subtypes with a particular food animal host and subsequent human infection. When S. Heidelberg isolates from human patients were compared to those of the major food animal species, there was extensive overlap in PFGE profiles, plasmid types, and antimicrobial susceptibility profiles, indicating a lack of host restriction among S. Heidelberg genotypes (203, 217, 218). In a study examining the core genomes of the population structure of many of the prominent serovars, it was concluded that the genomes of S. Heidelberg isolates were likely shaped by a high degree of horizontal genetic transfer (219). Consequently, the S. Heidelberg strains resided in a lineage distinct from that of the avian-associated Salmonella serovars Enteritidis and Gallinarum, based on genomic comparison. Additionally, the members of S. Heidelberg fell outside the lineage containing Salmonella serovars Typhimurium and Saintpaul, yet S. Heidelberg isolates shared a relatively high proportion of sequence similarity with the lineage (219).
S. Heidelberg isolates also often contain plasmids. While they lack a serotype-specific virulence plasmid, a common feature in serovars such as S. Typhimurium, S. Enteritidis, and S. Gallinarum (81), they often contain plasmids with virulence genes (83, 84). Interestingly, a number S. Heidelberg strains isolated from poultry-associated sources were found to harbor IncFIB plasmids similar to those previously recognized as being important for extraintestinal survival in avian-pathogenic E. coli (83, 220–222). Similar plasmids have been found very commonly in S. Kentucky isolates from poultry as well. Many IncFIB plasmids contain genes for iron acquisition (aerobactin operon and Sit iron transport systems), colicin production, and serum survival, which likely play a role in increased fitness in the avian environment (83). In many cases, these IncFIB plasmids also contain genes that encode resistance to multiple antimicrobials (often including resistance to tetracycline, streptomycin, chloramphenicol, and sulfonamide). This presents the possibility for coselective pressure, with antimicrobial use selecting for enhanced virulence, or conversely, the increased ability of these bacteria to survive iron-limited environments in the host could select for resistance to one or more antimicrobials (83, 84). S. Heidelberg plasmids also contain genes encoding disinfectant and heavy metal resistance, which may provide a selective advantage for survival in the avian production environment where pathogen control strategies are employed (84, 218).
Studies have shown that Salmonella serovars Gallinarum and Enteritidis are closely related in both their gene content and their antigenic formula (191, 223–225), suggesting that these two serovars originated from a relatively recent common ancestor (226, 227). Because of their close genetic similarity, they are valuable examples to explore host adaptation. Genomic comparisons of members of these two serovars have indicated that there is a high degree of genetic similarity between the two serotypes, with average nucleotide identities among orthologous genes being 99.7% (191). The genomes of sequenced isolates shared 4,179 predicted coding sequences (CDSs). The differences in CDS content between the strains were associated primarily with bacteriophages incorporated into the respective bacterial genomes (191). The lineage of S. enterica that contains these serotypes tends to be one of the most conserved among the species, with an estimated 4% of their core genome sequences originating from recombination with genes from other Salmonella serovars (219). Both serovars share the O1, O9, and O12 antigens (223). However, even though S. Enteritidis and S. Gallinarum are relatively closely related on the genomic level, they are diverse in their numbers of pseudogenes. S. Gallinarum isolates are unable to carry out mannose-sensitive hemagglutination and do not express flagellar genes, leading to an observed lack of mobility, while the majority of S. Enteritidis strains are motile (110). This lack of motility observed for S. Gallinarum isolates is in part associated with mutations in genes associated with flagellar biosynthesis and chemotaxis, including flhA, flhB, flgI, flgK, or cheM (191). Mutations in fliC may also contribute to the lack of motility of isolates of this serovar (226).
One study found that S. Enteritidis has 21 pseudogenes, compared to 147 for S. Gallinarum, but there are only 5 pseudogenes shared between the two serovars (195). Of these five pseudogenes, three are likely ancestral in origin, and the other two were likely independently acquired. Similarly, the genetically related S. Dublin had 212 identified pseudogenes, 177 of which are active genes in S. Enteritidis. Many of these functional genes encode surface structures or are involved in the central metabolism of Salmonella; thus, their inactivation in S. Dublin likely contributes to its host restriction in cattle (91). Likewise, certain pseudogenes are common to multiple host-restricted serotypes; for example, mglA and shdA are transcribed in S. Enteritidis but are present as pseudogenes in S. Choleraesuis, S. Dublin, S. Gallinarum, S. Paratyphi A, and S. Typhi (91). MglA is a small GTP-binding protein subunit of a binding-protein-dependent galactose transport system (228, 229) that likely plays a role as a virulence regulator in intracellular pathogens such as Francisella spp. (230) and motility in Myxococcus xanthus (231). ShdA is a protein that is involved in the colonization of Peyer's patches by S. Typhimurium and the shedding of the bacteria following infection (232, 233). The presence of a larger number of functional genes in broader-host-range serovars such as S. Enteritidis likely contributed to the ability to colonize and infect a greater number of hosts (234).
There are also several differences in the numbers of the fimbrial genes between S. Gallinarum and S. Enteritidis. Several fimbrial operons, including lpf, bcf, stb, stc, std, and sth, are important for long-term carriage and shedding of Salmonella (37). The S. Enteritidis genome has 13 fimbrial operons, 12 of which are present in S. Gallinarum (191). However, several of the CDSs within these common operons were identified as pseudogenes due to mutations that potentially prevent the expression of the functional gene product, which consequently impacts the overall function of the operons. These include mutations in stiC, stfF, safC, stbC, cheM, flhB, flhA, flgK, flgI, pegC, lpfC, sefC, sefD, sthE, sthB, and sthA (191). Additionally, the virulence plasmids in the two serotypes contain fimbrial operons; however, they are unique, with the S. Enteritidis plasmids carrying the plasmid-borne fimbria (pef) operon, while the S. Gallinarum plasmids have fimbria genes similar to those of E. coli K88 (40, 81, 123, 191, 235).
The sequenced S. Gallinarum isolate also lacked some of the T3SS effectors that are present in the S. Enteritidis genome, and sopA had an early stop codon that likely prevents the expression of a functional SopA protein (191). In addition, there was a mutation in bscG of S. Gallinarum, whose gene product is predicted to be important for cellulose biosynthesis, which likely contributed to the observed deficiency in its ability to form biofilms (191). Taken together, these mutations may negatively impact the ability of S. Gallinarum to colonize mammalian hosts, thereby limiting its ability to cause illnesses in a broad range of host species.
In addition to mutations in sopA, several studies have demonstrated the influence of other T3SS effectors on the ability of Salmonella serovars to colonize different hosts (206, 236, 237). The T3SSs are multiprotein complexes composed of structural and regulatory elements that transfer functional effectors from the bacterium into host cells, thereby facilitating invasion of and survival within host cells (48, 49). The T3SSs play vital roles in the interaction of Salmonella with the host (238). Variations in the gene sequences encoding T3SS factors for both the SPI-1 and SPI-2 systems have been associated with differences in the abilities to invade different hosts. Some of the main variability associated with host specificity is with the secreted effectors and the SipD T3SS tip protein rather than other structural components of the respective T3SSs (206, 236). The SPI-1 T3SS tip protein SipD is important for cell invasion; studies showed that antibodies directed at SipD block the ability of S. Enteritidis to invade intestinal epithelial cells (239). Effectors secreted by the SPI-I T3SS may also play a role in host specificity/range; sequence variability in the genes encoding the effector proteins SipA, SopA, and SopE and the chaperones SicP and InvB showed close evolutionary similarity in S. Enteritidis and S. Gallinarum compared to other serovars not as closely associated with avian sources (206). Thus, these SPI-1-associated factors may play a role in specificity in the initial invasion of the intestinal epithelium or immune cells in birds. The inflammatory responses to infections by S. Enteritidis and S. Gallinarum are different, with S. Enteritidis eliciting a stronger inflammatory response in chickens, which may prevent a more systemic spread, while S. Gallinarum elicits a weaker initial immune response and typically leads to systemic fowl typhoid (240).
On the SPI-2 side, at least 13 SPI-2-associated genes in S. Enteritidis and S. Gallinarum show close evolutionary similarity to each other compared to other serovars (206). It was hypothesized that the sequences may have coevolved for survival in the avian host, since survival in the reticuloendothelial system has been shown to be important for host specificity in chickens (241). The SPI-2 T3SS plays an important role in survival in the SCVs of macrophages (58). Genetic variability in SPI-1 factors, such as SopE and/or SodC, along with SPI-2 factors, such as SseC, SseD, and/or SseF, may lead to differences in the abilities to survive in different host cells (236). The factors SseG and, possibly, SseF appear to impact the migration of the SCVs to the Golgi apparatus in the host cell, which may serve as a potential source of nutrition for Salmonella (242). Hence, differences in the effector proteins may impact the ability to survive in different host cells and to be transported to sites of systemic infection. In addition to changes in the gene sequences themselves, posttranslational modifications of T3SS effectors can impact the targeting of Salmonella or the SCVs to different parts of the host cells. Observed posttranslational modifications, such as lipidation, phosphorylation, and ubiquitylation, can occur following translocation into host cells (243).
THE SALMONELLA-CHICKEN HOST INTERACTION
Each of the serovars discussed above are quite proficient at colonizing chickens; this section provides a more in-depth examination of the interaction of chicken-associated serovars and the avian host environment. One issue that continues to complicate attempts to understand host responses to Salmonella infection is the potential variability in host cell interactions among the different serovars. Several studies have been undertaken to gain knowledge of these interactions. Methner et al. conducted a series of colonization inhibition studies in young chicks gavaged with Salmonella strains belonging to the same or different serovars. The results demonstrated that single strains did not prevent colonization by other serovars, but mixtures of different serovars were effective against heterologous serovars (244). He et al. compared five poultry-associated serovars (S. Typhimurium, S. Enteritidis, S. Heidelberg, S. Kentucky, and S. Senftenberg) for their impact on an MC29 virus-transformed chicken macrophage cell line, HD-11, to assess Salmonella cell invasion, intracellular survival, and modulation of phorbol myristate acetate (PMA)-stimulated oxidative burst and nitric oxide (NO) activity. Neither S. Enteritidis nor S. Typhimurium generated detectable NO production by the macrophages, while the other 3 serotypes elicited production of over 100 μm NO. All of the serotypes repressed PMA-mediated oxidative burst and were equally able to invade HD-11 chicken macrophages; however, S. Enteritidis was more resistant to intracellular killing than the other 4 serovars (245). Those researchers speculated that these findings, particularly the intracellular survival ability of S. Enteritidis, may account for its association with systemic invasion in chickens (245). However, when newly hatched chickens were challenged with each of the 5 serovars, all but S. Senftenberg exhibited high rates of organ invasion (>85%, versus 14% for S. Senftenberg), which were different than the in vitro intracellular survival outcomes (245). These findings were consistent with studies on S. Enteritidis strains classified as displaying either low- or high-invasive phenotypes in Caco-2 human colon tissue in vitro assays (246, 247). Those studies demonstrated that when mice were orally challenged, low-invasive strains were as virulent as high-invasive strains, even though not all S. Enteritidis isolates recovered from poultry are equally pathogenic. Some of the infectivity differences between S. Enteritidis and other serovars in avian model systems may be related to the seemingly high epidemiological frequency and long-term association of S. Enteritidis with egg-related salmonellosis and a potentially unique evolutionary relationship with laying hens (248–256). This relationship may be evidenced by the limited genetic diversity observed among S. Enteritidis strains based on random amplified polymorphic DNA plasmid profiling and phage typing (257). Work with laying hens suggested that because S. Enteritidis infects reproductive tissues, namely, the oviduct and ovaries, these tissues represent critical avenues for egg contamination; additionally, this serovar may also have evolved the means to survive the hostile environment of internal egg contents (252, 258–267).
More recently, attempts have been made to identify unique genetic traits which distinguish S. Enteritidis from other serovars and lead to its propensity for laying hens and eggs. Methner et al. demonstrated that S. Enteritidis strains exhibited substantial colonization inhibition of other S. Enteritidis strains but not of other serovars in young chicks, suggesting that there may be differences in colonization targets (244). However, infection studies comparing S. Enteritidis and S. Typhimurium in adult laying hens by Keller et al. indicated only minimal differences among strains from these two serovars in intestinal, hepatic, splenic, and reproductive tract colonization (261). Likewise, it appears that S. Enteritidis genes associated with intestinal colonization are similar to those observed for other Salmonella serotypes. Bohez et al. constructed a deletion mutant of the SPI-1 regulator gene hilA in S. Enteritidis and observed decreases in shedding and cecal colonization to nearly nondetectable levels after 4 weeks in young chicks. Those authors concluded that the HilA regulatory protein was required for continued cecal colonization and long-term shedding (268). Subsequent studies by these researchers demonstrated that the initial colonization by the S. Enteritidis hilA mutant was sufficient to prevent long-term fecal shedding and cecal and internal organ colonization by the respective S. Enteritidis wild-type strain (264, 269). This linkage of hilA with systemic infection is supported by the general trends of increased liver, spleen, and ovary colonization observed in adult laying hens when S. Enteritidis hilA expression levels were increased (270).
However, studies based on infection of young chicks by S. Enteritidis deletion mutants for individual SPIs (SPI-1 to -5) revealed that colonization of the liver and spleen was dependent on SPI-1 and SPI-2 but that cecal colonization was not (271). Desin et al. observed less invasion by S. Enteritidis SPI-1 mutants of polarized Caco-2 human intestinal epithelial cells and chicken cecal and small intestinal explants but no differences in cecal colonization of 1-week-old chickens, with the exception of an infection delay in livers and spleens (272). Mixed results have also been reported for other serovars and other hosts. S. Typhimurium hilA deletion mutants were recovered from infected mouse intestinal contents, intestinal tissues, and systemic tissues at a lower frequency than the parental wild-type strain, while SPI-1 deletion mutants were recovered at frequencies similar to those of the wild-type strain (273). Morgan et al. reported a similar lack of an impact on chicken cecal colonization by S. Typhimurium SPI-1 mutants, but SPI-1 was required for colonization of calf intestines (43). Dieye et al. used a mixed-infection approach by combining isogenic SPI-1 S. Typhimurium deletion mutants with their respective wild-type counterparts and administering them to 1-week-old chicks instead of younger birds. For the most part, the wild-type strain outcompeted the SPI-1 deletion mutant over the 14-day infection period. When cecal and spleen samples were recovered, the level of cecal colonization by the wild-type was substantially higher than that by the mutant by day 14 (74). More recently, Clark et al. used green fluorescent reporter gene constructs for comparison of various S. Typhimurium strains in tissue culture infection assays and discovered that only subpopulations expressed SPI-1 genes. Those researchers speculated that genetic heterogeneity of invading S. Typhimurium populations could lead to differential SPI-1 expression and heterogeneous Salmonella population behavior during infection (274).
There appear to be serovar differences in pathogenicity gene expression as well. Silva et al. constructed an S. Enteritidis transposon library and used a microarray-based negative-selection screening approach to isolate mutants deficient for liver and spleen colonization of BALB/c mice. Many of the colonization-deficient strains were identified as having mutations in SPI genes already known to be responsible for Salmonella systemic infection; however, mutants that were associated with genes and genomic islands not identified in other Salmonella serovars, including S. Typhimurium, were also isolated (275). Shah et al. also identified genes and genomic islands in S. Enteritidis that were not present in S. Typhimurium after screening S. Enteritidis mutants generated from a random Tn5 transposon library for their ability to invade Caco-2 and chicken liver (LMH) cells and for survival in chicken macrophages (HD-11) (276). Strains within individual serovars also display differences in the ability to express different genes. Shah et al. screened six S. Enteritidis isolates and were able to phenotypically differentiate them as stress sensitive (acid and oxidative stress, survival in egg albumen, and impairment in intestinal colonization and systemic infection) versus stress resistant, even though no changes in genomic content were detectable with genomic hybridization microarrays. Sequencing of the stress-regulatory gene rpoS in one of the stress-sensitive strains revealed an insertion mutation and truncated protein, leading those authors to conclude that even minor polymorphisms in certain genes would be sufficient to impact stress or virulence gene responses (277).
As more becomes known about the role of host-pathogen interactions in Salmonella pathogenesis, some of the seemingly contradictory pathogen responses may become clear. For example, Knodler et al. demonstrated that hyperreplicating Salmonella subpopulations in the cytosol of GIT epithelial cells that are distinct from the SCV populations can mediate their release back into the lumen by inducing inflammation accompanied by epithelial cell death and subsequent shedding (58). Since T3SS-based invasion gene systems are involved, it may be that pathogenicity alterations occurring with different mutants and serovars could be attributed the intracellular subpopulations that are impacted, thereby impacting the abilities to sustain long-term fecal excretion of the respective subpopulation (58, 278). This may partially explain the emergence of individual Salmonella carrier chickens within poultry flock populations as well as in other animal species.
In addition, the complexity of the indigenous GIT microflora, interaction of the immune system, and host factors such as age, stress level, and overall health status may play important roles in host-pathogen interactions (279–281). Identifying overarching themes for Salmonella pathogenesis and designing effective cross-protective control measures that can be applied across different serovars will require application of combinations of high-throughput omics analyses; animal model responses to sort out shared signals, such as common immune signatures across animal species; along with subsequent mathematical modeling (282–286). Particularly, in poultry, the potential roles of host genes that may impact infection and carrier states of Salmonella have been studied for a number of years and have been extensively discussed recently in a comprehensive review by Calenge and Beaumont (283) and will not be discussed here. The remainder of the current review focuses on Salmonella serovar responses to the poultry host.
SALMONELLA AND STRESS RESPONSES IN THE CHICKEN GIT
Prior to infecting a potential host, Salmonella encounters numerous environmental conditions that represent sufficient stress to influence the organism's ability to grow optimally and in some cases even survive. These stressors can originate as a wide range of physical and chemical challenges either in the environmental niches that Salmonella occupies or as manufactured barriers, such as those incorporated during food production and processing, such as antimicrobials, disinfectants, biocides, and preservatives. These intervention approaches have been reviewed extensively elsewhere (273, 287–291).
As noted above, when Salmonella spp. come into contact with a prospective host and gain access to its GIT, there are a number of potential barriers that the organism encounters as it travels through the GIT. Ahmer and Gunn classified these host barriers into broad categories of physical, chemical, enzymatic, and immune hurdles that must be surmounted by Salmonella spp. (292). These include, in addition to specific host-generated immune- and non-immune-based defenses, iron limitation, acidic and pH shifts, oxidative and osmolarity stresses, and limited nutrient availability that leads to starvation (35, 36, 293–301). Although these barriers are manifested either as a function of the host's defense mechanisms or as a consequence of high population densities and a metabolically active indigenous GIT microbial population, in reality, there is a substantial interaction between the two that makes it difficult to separate them experimentally. For example, the field of avian genetics has advanced sufficiently such that a range of host-innate, cell-mediated, and humoral immune responses that resist and clear pathogens such as Salmonella have been identified. The extent of the immune involvement is determined by microbial challenge severity as well as the health and nutritional status of the host (280, 283, 302). The immune system also interacts with the indigenous microflora, and the presence of this microflora is now considered essential for proper immunological development (303). Consequently, nonpathogenic bacteria can be considered active players in modulating immune recognition of pathogens (304, 305). Given the diversity of the GIT microflora, an understanding of the symbiotic relationship between the microbial consortia and the immune system is extremely complex and has been reviewed elsewhere (303, 306, 307). Here the focus is on the microbial metabolic interactions that occur in the GIT that appear to influence Salmonella and countermeasures employed by this pathogen to overcome these challenges.
Salmonella Acid Tolerance Response and Organic Acids
The compounds collectively referred to as organic acids are comprised of the saturated straight-chain monocarboxylic acids and their respective derivatives (unsaturated, hydroxylic, phenolic, and multicarboxylic organic acids) and have a long history as antifungal and antimicrobial agents in perishable animal feeds and human foods (308–310). Traditionally, organic acids have been added to elicit bacteriostatic and bactericidal impacts on undesirable organisms in potentially contaminated food products. A wide range of antimicrobial mechanisms, including osmotic stress, anion toxicity, and membrane disruption, have been proposed over the years, but inhibition is generally believed to be closely tied to pH because of its influence on the formation of undissociated organic acids, which can easily cross the cell membrane and dissociate into anions and protons in the presence of the cytoplasmic neutral pH (309–313). The acids not only result in the acidification of the cytoplasm and the accompanying difficulties for cellular constituents to perform essential metabolic functions in the cell but also lead to an energy drain due to the consumption of ATP to actively export protons (310).
Salmonella can encounter short-chain fatty organic acids (SCFAs) (primarily acetate, propionate, butyrate, and lactate) in a variety of environments, because they are used as animal feed additives and antimicrobials in food and meat processing and can be generated by certain starter cultures used for food fermentations (308, 309, 314–317). Once in the GIT, particularly in the lower regions of monogastric hosts and the foregut in ruminants, Salmonella must be able to survive the presence of variable SCFA concentrations (mM ranging from <1 to hundreds for particular organic acids) depending on the host animal and digestive tract site associated with fermentation by the indigenous microflora in the GIT (309, 311, 314, 318–321).
Traditionally, it was believed that Salmonella spp., much like other bacteria, were sensitive to organic acids and that this sensitivity was dependent on pH (322–325). However, Leyer and Johnson demonstrated that HCl acid-adapted S. Typhimurium could also resist organic acids typically found in cheeses (326). Baik et al. induced stationary- and exponential-phase acid (pH 4.4) tolerance responses in S. Typhimurium after exposure to a series of organic acids and concluded that both physiological states were protected, but the stationary-phase protection occurred with only some of the organic acids (327). The protection against organic acids did not occur if organic acids were used for the initial acid shock. When Kwon and Ricke exposed S. Typhimurium to SCFA at neutral pH for 1 h, they observed that acid tolerance was greater for cells exposed to acetate or propionate than for cells exposed to butyrate or valeric acid and was enhanced under anaerobic incubation conditions (328). Calhoun and Kwon observed substantial enhanced acid tolerance in S. Enteritidis when exposed to 100 mM propionate at neutral pH over a longer period of time (16 h) (329). The enhancement may not be surprising since Salmonella cells cultured under anaerobic growth conditions can produce fermentation acids (330, 331), suggesting that some of the resistance to SCFA may be related to protection from their own end products. It is also known that Salmonella can directly catabolize SCFA. For example, S. Typhimurium utilizes the 2-methylcitric acid cycle to convert propionate to pyruvate for reentry into the tricarboxylic acid cycle (332–334).
S. Typhimurium exposure at pH 7.0 to high (mM) levels of SCFA typical of large intestine concentrations induces not only resistance to extreme acidic conditions (pH 3.0) but also cross-protective resistance to high osmolarity (2.5 mM NaCl) and reactive oxygen (20 mM H2O2) (335). Similar cross protection against salt stress (KCl and NaCl) has been reported for acetic acid-induced acid tolerance in S. Typhimurium but not lactic acid-induced acid tolerance, which appears to be related to sensitivity to hydrogen peroxide (336, 337). Initial pH appears to be a factor, as both growth and survivability are limited when S. Typhimurium cells are exposed to propionate at pH 5.0 versus pH 7.0 (328). It appears that even more subtle fluctuations in pH can influence Salmonella growth metabolism. For example, Dunkley et al., using anaerobic continuous cultures, demonstrated that S. Typhimurium glucose- and ATP-based microbial cell yields (calculated as mg of cell protein synthesized per ATP formed or glucose consumed) were decreased when the pH in the growth vessels was shifted from near-neutral pH to levels approaching pH 6.0 (330). Other stress combinations appear to have more of an impact on SCFA inhibition of Salmonella. Milillo and coworkers demonstrated not only that the combination of heat (50°C to 60°C) and organic acids was more effective than single intervention applications when applied to S. Typhimurium but also that heated acidified solutions caused substantial membrane damage and leakage of intracellular ions (338, 339). There may also be potential serovar differences. Joerger et al. concluded that S. Kentucky was more acid sensitive (pH 2.5) than other Salmonella serovars after growth in the presence of acetic acid (340). Gene expression microarray comparisons between S. Kentucky and S. Enteritidis indicated that regulatory genes associated with acid response (rpoS, fur, and phoPQ) were similar between the two serovars, as were most global transcriptional responses, leading Joerger et al. to speculate that phenotypic differences were perhaps more a function of posttranslational or small undetectable transcriptional differences (340).
Salmonella Virulence Response and Organic Acids
While acid tolerance is considered a component of pathogenesis, the presence of SCFA may also directly impact Salmonella pathogenesis and virulence gene expression. Durant et al. conducted a series of tissue culture studies with an epidermal carcinoma cell line (HEp-2) to determine the influence of S. Typhimurium after growth in either a mixture or separate intestinal concentrations of SCFA (acetate, propionate, and butyrate at pH 6.0 or 7.0) on its subsequent ability to adhere to and invade tissue culture cells (341–343). For S. Typhimurium incubated for 4 h in the presence of SCFA, acetate at pH 6.0 and 7.0 did not alter attachment, and only slight increases in invasion occurred, while propionate and butyrate dramatically decreased attachment and invasion at pH 6.0 but not at pH 7.0. There were also indications that these S. Typhimurium responses were growth dependent, particularly in the presence of propionate and butyrate at pH 6.0, which reduced the growth rate considerably (341). However, when late-logarithmic-phase (12 h) and stationary-phase (18 h) S. Typhimurium cells were compared (342, 343), all SCFAs reduced cell attachment at pH 6.0 and 7.0 but only marginally influenced invasion for late-log-phase cultures of Salmonella. The stationary-phase Salmonella cells exhibited reduced attachment only in the presence of SCFA at pH 6.0, while actual increases in invasion occurred for lower concentrations of acetate (342, 343). Van Immerseel et al., using avian intestinal and cecal epithelial cell lines, also observed increases in invasion of S. Enteritidis exposed to acetate for 4 h and decreases with propionate and butyrate (265, 344). Gantois et al. reported that exposure of S. Enteritidis and S. Typhimurium to butyrate for 4 h resulted in the lowest percentage of invasion of HeLa cells (345).
In follow-up studies to determine the genetic elements associated with the SCFA influence on Salmonella pathogenesis, Durant et al. used S. Typhimurium strains constructed to carry chromosomal lacZY transcriptional fusions within either hilA or invF to assess the impact of pH and individual SCFAs on their expression (346). The study concluded that growth of S. Typhimurium in the presence of acetate, but not propionate and butyrate, stimulated β-galactosidase expression for both genes, even though growth was inhibited only at pH 6.0. When the S. Typhimurium hilA-lacZY fusion was incorporated into an S. Enteritidis isolate from poultry, increasing lactate concentrations along with lowering pH reduced expression levels of β-galactosidase (347). Lawhon et al. concluded that acetate provided a signal for invasion through the production of cytoplasmic acetyl-phosphate, while propionate and butyrate repressed invasion genes (348). Gantois et al. conducted comparative transcriptomic analyses of S. Enteritidis and S. Typhimurium and reported that butyrate downregulated SPI-1 genes, including the regulatory genes hilD and infV, while Huang et al. identified formate as a diffusible signal to induce SPI-1 genes and invasion (345, 349). Virulence gene responses to organic acids may vary in different serovars as well. Using quantitative reverse transcriptase real-time PCR, Gonzalez-Gil et al. reported that expression of the virulence gene regulator hilA was both serovar and strain dependent when isolates were exposed to either mild acetic or HCl acid stress. Responses were dependent on the type of acid used and were time dependent, with hilA being upregulated after a 2-h exposure to the respective acid (350). When Milillo et al. compared S. Typhimurium transcriptome responses to sodium acetate and sodium propionate exposure after 1 min (55°C at pH 4.0), the respective gene expression patterns were similar, with no increases in expression levels of rpoS, phoPQ, or virulence factors despite their established roles in organic and inorganic acid stress (35, 327, 328, 338). Conversely, genes related to attachment and/or motility functions were induced, which has been observed previously for S. Typhimurium attachment genes after exposure to 42°C (351). There was also a repression of several heat shock response genes, which, in conjunction with cell membrane damage, indicates that membrane integrity is an important component for Salmonella cells to accurately assess their extracellular environmental conditions and respond accordingly (351). Clearly, more in-depth genetic analysis is needed to sort out the interactions that occur among different stresses in Salmonella versus its collective virulence response capabilities as well as how these may shift over time after initial encounters with the cell's surrounding environment. Serovar and strain differences will also need to be examined to determine whether some of the serovar dissemination patterns are due to the ability of some serovars, but not others, to effectively counter external stresses in their environments.
Salmonella Virulence Response and Competition with GIT Microflora
The GIT systems in most hosts, including food animals and humans, harbor highly complex and metabolically interactive microbial consortia. Particularly in the lower GIT of monogastric animals (colon or cecum) and the foregut (rumen) of ruminants, microbial populations consist of large numbers of mostly saccharolytic anaerobic microorganisms along with methanogenic archaea, which together result in a highly reduced ecosystem with minimal oxygen (318, 320, 352–359). Given the complexity of diets in general and the recalcitrant nature of some of the fiber-containing components (particularly those consumed by herbivores), the GIT microbial consortia are characterized not only by their anaerobic physiology but also by their ability to hydrolyze fiber polymers into soluble carbohydrates that are readily fermentable (360–364). Since energy generation for ATP formation is anaerobic and, therefore, much more limited per carbon source, GIT saccharolytic microorganisms must extract maximum ATP through a multitude of limited-substrate-level and anaerobic respiration phosphorylation pathways (318, 365–368). Given the complexity of the GIT microflora and the limited energy generation capabilities for microbial growth, each species must catabolize similar carbon sources, necessitating a hierarchy for substrate preferences and competition among microorganisms based on maximum growth, energy efficiency, and substrate affinity (369, 370). If these capabilities are combined with the constant GIT turnover that occurs due to the passage rate of digesta, GIT microbial ecosystems are characterized by their exceptional ability to metabolically scavenge and extract maximum nutritional value from incoming dietary sources.
Consequently, pathogens entering the GIT, in addition to combating the hostile environment derived from fermentation activities of the indigenous microflora and the host barriers, must also directly compete with the GIT microflora for scarce nutrients (298, 371). Pathogen metabolism and virulence are often interconnected to the point that it becomes difficult to distinguish which functions are occurring simultaneously. Rohmer et al. suggested that not only do pathogens acquire virulence factors to access new niches, they may also require new metabolic pathways to sequester available nutrient sources, as evidenced by the presence of metabolic functions encoded on pathogenicity islands (371, 372). In the GIT, pathogens entering the lumen during times of nutritional stress could conceivably employ this strategy by either inducing virulence to escape the GIT altogether or manipulating the GIT environment to outcompete indigenous microflora.
Starvation, malnutrition, or abrupt changes in diet can alter the composition of indigenous GIT microflora and potentially impact the host's immune system and the host's general physiology and well being (373–375). Changes in nutritional status and dietary alteration have also been known for some time to alter the relationship between the GIT and pathogens, such as attachment to the epithelial lining (376). Emptying of the GIT content represents one of the more drastic alterations that occurs either naturally or as part of a prescribed treatment in humans or a management option in animals. Increased populations of Salmonella have been consistently observed in a variety of animals undergoing emptying of the GIT due to feed removal, including chickens (377–381), mice (382), and ruminants (383–385). Although the indigenous GIT microflora were not characterized in these early studies, it was speculated that feed removal/GIT emptying potentially influenced the microbial populations or activities, and susceptibility to Salmonella colonization was presumed to be related to decreases in levels of antimicrobial organic acids generated during fermentation (250).
One of the most extensively studied host-pathogen systems, which represented a nutritional management strategy linked with Salmonella dissemination, was the use of dietary restrictions to induce artificial molting in laying hens. In the U.S. egg industry, laying hens can be induced to molt in order to cease egg production and allow the reproductive tract to undergo a rest phase to allow flock rejuvenation, feather renewal, and a second, higher-production egg-laying cycle (386). Historically, this was accomplished by complete removal of diet for anywhere from 5 to 14 days until cessation of egg production was completed (386, 387). However, S. Enteritidis was closely linked with egg contamination, and research conducted during the 1990s with laying hens as the infection model suggested that management practices such as feed removal-induced molts might be partially responsible for the contamination (388, 389). In the following decade, more detailed studies on S. Enteritidis infection in susceptible laying hens concluded that complete removal of feed created a GIT environment in laying hens that not only was easily colonized by S. Enteritidis but also led to systemic infection of internal organs, including the ovaries (250, 331, 390). Increased expression levels of the S. Enteritidis lacZY-hilA fusion gene in cells incubated in crop contents from birds that had undergone feed removal demonstrated that enhanced systemic invasiveness could be linked with increased expression levels of hilA (391). These findings were later replicated and confirmed in vivo by quantitative PCR (392). This increase in S. Enteritidis colonization and invasiveness also coincided with diminished numbers of lactic acid bacteria in the crop and reduced organic acids in the crop (391) and cecum (270, 393) and led to major shifts in fecal and cecal bacteria compared to fully fed birds (270, 394, 395). Ricke hypothesized that the key to limiting S. Enteritidis during molt was to develop low-nutrient dietary strategies, such as formulations with high fiber content, that would still induce molt due to low energy density but were sufficiently fermentable to support an active GIT microflora that would serve as a barrier to pathogen establishment (255). Several molt diets with fermentable substrate combinations have been screened in vitro and shown to support optimal avian cecal fermentation (396–398) and retain similar cecal microbial molecular profiles (397). In vivo application of some of these diets was shown to retain fermentation and GIT populations during molt while limiting the ability of S. Enteritidis to colonize the GIT and become invasive (255, 270, 392, 399, 400). The overall results of the studies demonstrate that there is a complex and important relationship between the microflora of the avian GIT and Salmonella, which is key to limiting the pathogen.
CONCLUDING REMARKS
Salmonella serovars display a range of abilities to colonize different animal hosts and cause illnesses in humans. Many of the serovars most commonly implicated in food-borne human infections have a broad range of animal hosts that they can colonize, while others, especially some that cause severe human infections, have much narrower host ranges. Some serovars, such as S. Typhi and S. Paratyphi A, are human-restricted serovars and can cause severe disease manifestations such as enteric fever. The factors that impact Salmonella pathogenesis and host range are complex and are associated with differences in variables such as the genetics of the bacterium and expression of these genetic factors, the host immune status and specific pathogen responses, the host environment, and interactions with intestinal microflora.
A great deal of work has been undertaken to understand the genetics of Salmonella and explore the factors that contribute to the evolution of pathogenesis. Based on genome sequencing results and pangenome analyses of Salmonella serovars, it is evident that two distinct, yet potentially complementary, evolutionary approaches that impact host range and virulence are occurring. These approaches include gene acquisition through horizontal transfer (associated with SPIs, transposable elements, phages, and plasmids) and the loss of genes or a loss of their function, which impacts host range (105, 106). As the species S. enterica evolved, its members' genomes acquired the multiple SPIs that allowed the organism to become pathogenic. Several serovars also acquired specific virulence plasmids that harbor the spv operon, which increases virulence (126). Other serovars, while not having serovar-specific virulence plasmids, have other plasmids that may encode factors that are important for survival in a potential host niche. Plasmids have played a significant role in the evolution of host specificity in some Salmonella serovars. A key example includes some of the plasmids of S. Kentucky and some S. Heidelberg isolates that contain genes associated with extraintestinal survival in poultry, which may provide a selective advantage in poultry (83). Many of these plasmids also contain genes for antimicrobial resistance, which is concerning because of the possibility that antimicrobial use could select for enhanced virulence or conversely that the selective advantage to survive in one environment/host may select for resistance to one or more antimicrobials (83, 84). While our knowledge of the genetic composition of these plasmids has greatly increased with the advent of next-generation sequencing, our understanding of the evolution and dissemination of these plasmids and their interactions with one another remains limited. There is not a clear correlation between carriage of the plasmid and the establishment of systemic disease in humans, further suggesting that it may be a requirement of some strains but not others (401).
On the other side of the spectrum of factors that impact virulence and host range is gene loss or the loss of gene function due to mutation, insertion, or deletion in the gene or regulatory element. Many of the host-restricted serovars have a large number of pseudogenes, which inactivate genes that are often involved in aspects of virulence, nutrient utilization, and metabolism (91). The impact of pseudogenes on host restriction seems fairly clear; however, it is less clear whether gene inactivation leads to the host-restricted phenotypes or whether the organisms settled in the niche and those genes not essential for survival are undergoing the process of genome reduction. Interestingly, Salmonella serovar Typhi demonstrates aspects of functional gene loss (a high percentage of pseudogenes) (193) and the impact of horizontal gene transfer on pathogenicity (14). S. Typhi isolates have mutations in several of the fimbrial genes that are associated with intestinal attachment, which is important for gastroenteritis but not enteric fever (194). Members of the serovar also acquired SPI-7, which harbors genes for the Vi capsule, which prevents recognition of PAMPs on the surface of S. Typhi, thereby limiting the initial immune response following infection (2).
Despite the wealth of knowledge associated with Salmonella pathogenesis mechanisms in host animals, several key questions remain on the exact roles and extent of involvement of the respective virulence genes and genomic islands of particular serovars and their characteristic pathogenic phenotypes expressed in animal models. Not only do in vitro models, such as tissue culture adhesion and invasion assays, sometimes differ from in vivo results, there may also be differences in responses depending on the type of cell line used (402). It is also becoming apparent, as more sophisticated genetic analyses are being applied to animal infection studies, that Salmonella serovars vary in their virulence gene capacities, and given the tremendous number of serovars identified and the wide range of corresponding strains isolated for some serovars, there is the potential for almost endless nuances of perhaps subtle but different serovar- and even strain-specific genetic strategies for overcoming host barriers.
An in-depth understanding of the mechanisms of Salmonella pathogenesis is important for developing intervention strategies to limit their prevalence and spread and aid in the development of newer drugs and vaccines which could result in better treatment and/or prevention of salmonellosis in animals and humans. The continued use of whole-genome sequencing, gene expression, and bioinformatics analyses of Salmonella serovars from host-restricted and host-specific serovars should continue to provide insights into the specific genetic traits that could contribute to symbiotic and/or disease-causing potential in humans and animals and lead to an overall reduction in disease burden associated with Salmonella.
ACKNOWLEDGMENTS
We thank Jing Han, Huizhong Chen, and Carl Cerniglia for their insightful reviews of the manuscript.
The views presented in this article do not necessarily reflect those of the U.S. Food and Drug Administration.
Biographies

Steven L. Foley is a Research Microbiologist with the U.S. Food and Drug Administration's National Center for Toxicological Research. Dr. Foley earned his Ph.D. in Cellular and Molecular Biology from North Dakota State University and completed a postdoctoral fellowship with FDA's Center for Veterinary Medicine. His research program focuses on understanding the role of plasmids in Salmonella virulence and antimicrobial resistance and factors that contribute to their spread. He also has an interest in the development and evaluation of molecular subtyping methods for enteric pathogens.

Timothy J. Johnson received his Ph.D. in 2004 from North Dakota State University in Fargo, ND, and his postdoctoral work was performed at the College of Veterinary Medicine at Iowa State University. From 2007 to 2013, he worked as an Assistant Professor of Microbiology within the Department of Veterinary and Biomedical Sciences, College of Veterinary Medicine, University of Minnesota, and is currently an Associate Professor in the same department. Dr. Johnson's research interests involve genomics-based approaches towards understanding the evolution of virulence and antimicrobial resistance in enteric bacteria of production animals and humans and the impact of microbial community succession on animal gut health.

Steven C. Ricke received his B.S. from the University of Illinois and his Ph.D. from the University of Wisconsin and was a USDA-ARS postdoctoral fellow at North Carolina State University. He was a professor at Texas A&M until 2005, when he became the Wray Endowed Chair and Director of the Center for Food Safety at the University of Arkansas. He has received the Poultry Science Association Research Award and American Egg Board Award, was named a Texas Agricultural Experiment Station Faculty Fellow, and received the Division of Agriculture, University of Arkansas, John White Outstanding Research Award. He is a member and served as cofounder and former President of the Arkansas Association of Food Protection. Dr. Ricke's research program is focused primarily on virulence and pathogenic characteristics of food-borne Salmonella spp., with emphasis on the growth, survival, and pathogenesis of the organism under conditions encountered during food animal production and processing.

Rajesh Nayak is a Research Scientist with the U.S. Food and Drug Administration and an Adjunct Professor with the Universities of Arkansas and West Virginia. Dr. Nayak earned his Ph.D. at West Virginia University and postdoctoral fellowship at the National Center for Toxicological Research. His research interests are in (i) molecular epidemiology, surveillance, and microbial source tracking of food animal-infectious pathogens through the food production environment using genotyping methods; (ii) threat assessment of emerging pathogens and their genetic characteristics using microarray, whole-genome sequencing, and bioinformatics platforms; (iii) investigating the mechanisms of antimicrobial resistance and pathogenesis in bacterial pathogens isolated from food, feed, environment, human, and veterinary sources; and (iv) developing molecular tools for detection of bacterial pathogens and their genetic traits. Dr. Nayak serves on the editorial board and is an ad hoc reviewer for several national and international journals.
Jessica Danzeisen received her M.S. in Microbiology in 2008 from North Dakota State University in Fargo, ND. She is currently a Research Scientist in the laboratory of Dr. Timothy J. Johnson within the Department of Veterinary and Biomedical Sciences, College of Veterinary Medicine, University of Minnesota. Ms. Danzeisen's research interests include antimicrobial resistance in production animals and the gut microbiome related to production animal health.
REFERENCES
- 1.Donnenberg MS. 2000. Pathogenic strategies of enteric bacteria. Nature 406:768–774 [DOI] [PubMed] [Google Scholar]
- 2.Tsolis RM, Young GM, Solnick JV, Baumler AJ. 2008. From bench to bedside: stealth of enteroinvasive pathogens. Nat. Rev. Microbiol. 6:883–892 [DOI] [PubMed] [Google Scholar]
- 3.Guerrant RL, Steiner TS. 2005. Principles and syndromes of enteric infections, p 1215–1230 In Mandell GL, Bennett JE, Dolin R. (ed), Principles and practice of infectious diseases, 6th ed, vol 1 Elsevier Churchill Livingstone, Philadelphia, PA [Google Scholar]
- 4.Herrington DA, Hall RH, Losonsky G, Mekalanos JJ, Taylor RK, Levine MM. 1988. Toxin, toxin-coregulated pili, and the toxR regulon are essential for Vibrio cholerae pathogenesis in humans. J. Exp. Med. 168:1487–1492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nataro JP, Kaper JB. 1998. Diarrheagenic Escherichia coli. Clin. Microbiol. Rev. 11:142–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu H, Magoun L, Luperchio S, Schauer DB, Leong JM. 1999. The Tir-binding region of enterohaemorrhagic Escherichia coli intimin is sufficient to trigger actin condensation after bacterial-induced host cell signalling. Mol. Microbiol. 34:67–81 [DOI] [PubMed] [Google Scholar]
- 7.Stephen J. 2001. Pathogenesis of infectious diarrhea. Can. J. Gastroenterol. 15:669–683 [DOI] [PubMed] [Google Scholar]
- 8.Bhavsar AP, Guttman JA, Finlay BB. 2007. Manipulation of host-cell pathways by bacterial pathogens. Nature 449:827–834 [DOI] [PubMed] [Google Scholar]
- 9.Cossart P, Sansonetti PJ. 2004. Bacterial invasion: the paradigms of enteroinvasive pathogens. Science 304:242–248 [DOI] [PubMed] [Google Scholar]
- 10.Watson RO, Galan JE. 2008. Campylobacter jejuni survives within epithelial cells by avoiding delivery to lysosomes. PLoS Pathog. 4:e14. 10.1371/journal.ppat.0040014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoebe K, Janssen E, Beutler B. 2004. The interface between innate and adaptive immunity. Nat. Immunol. 5:971–974 [DOI] [PubMed] [Google Scholar]
- 12.Tang D, Kang R, Coyne CB, Zeh HJ, Lotze MT. 2012. PAMPs and DAMPs: signal 0s that spur autophagy and immunity. Immunol. Rev. 249:158–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nguyen QC, Everest P, Tran TK, House D, Murch S, Parry C, Connerton P, Phan VB, To SD, Mastroeni P, White NJ, Tran TH, Vo VH, Dougan G, Farrar JJ, Wain J. 2004. A clinical, microbiological, and pathological study of intestinal perforation associated with typhoid fever. Clin. Infect. Dis. 39:61–67 [DOI] [PubMed] [Google Scholar]
- 14.Sharma A, Qadri A. 2004. Vi polysaccharide of Salmonella Typhi targets the prohibitin family of molecules in intestinal epithelial cells and suppresses early inflammatory responses. Proc. Natl. Acad. Sci. U. S. A. 101:17492–17497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andersen-Nissen E, Smith KD, Strobe KL, Barrett SL, Cookson BT, Logan SM, Aderem A. 2005. Evasion of Toll-like receptor 5 by flagellated bacteria. Proc. Natl. Acad. Sci. U. S. A. 102:9247–9252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lapaque N, Takeuchi O, Corrales F, Akira S, Moriyon I, Howard JC, Gorvel JP. 2006. Differential inductions of TNF-alpha and IGTP, IIGP by structurally diverse classic and non-classic lipopolysaccharides. Cell. Microbiol. 8:401–413 [DOI] [PubMed] [Google Scholar]
- 17.Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, Jones JL, Griffin PM. 2011. Foodborne illness acquired in the United States—major pathogens. Emerg. Infect. Dis. 17:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andrews-Polymenis HL, Baumler AJ, McCormick BA, Fang FC. 2010. Taming the elephant: Salmonella biology, pathogenesis, and prevention. Infect. Immun. 78:2356–2369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoffmann S, Batz MB, Morris JG., Jr 2012. Annual cost of illness and quality-adjusted life year losses in the United States due to 14 foodborne pathogens. J. Food Prot. 75:1292–1302 [DOI] [PubMed] [Google Scholar]
- 20.Batz MB, Hoffman S, Morris JG., Jr 2011. Ranking the risks: the 10 pathogen-food combinations with the greatest burden on public health. University of Florida, Gainesville, FL [Google Scholar]
- 21.Batz MB, Doyle MP, Morris G, Jr, Painter J, Singh R, Tauxe RV, Taylor MR, Lo Fo Wong DM, Food Attribution Working Group 2005. Attributing illness to food. Emerg. Infect. Dis. 11:993–999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention 1997. Salmonella serotype Montevideo infections associated with chicks—Idaho, Washington, and Oregon, spring 1995 and 1996. MMWR Morb. Mortal. Wkly. Rep. 46:237–239 [PubMed] [Google Scholar]
- 23.Batz MB, Hoffmann S, Morris JG., Jr 2012. Ranking the disease burden of 14 pathogens in food sources in the United States using attribution data from outbreak investigations and expert elicitation. J. Food Prot. 75:1278–1291 [DOI] [PubMed] [Google Scholar]
- 24.Brenner FW. 1998. Modified Kauffmann-White scheme. Centers for Disease Control and Prevention, Atlanta, GA [Google Scholar]
- 25.Su LH, Chiu CH. 2007. Salmonella: clinical importance and evolution of nomenclature. Chang Gung Med. J. 30:210–219 [PubMed] [Google Scholar]
- 26.Foley SL, Nayak R, Hanning IB, Johnson TJ, Han J, Ricke SC. 2011. Population dynamics of Salmonella enterica serotypes in commercial egg and poultry production. Appl. Environ. Microbiol. 77:4273–4279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goto Y, Kiyono H. 2011. Epithelial cell microRNAs in gut immunity. Nat. Immunol. 12:195–197 [DOI] [PubMed] [Google Scholar]
- 28.Foley SL, Lynne AM, Nayak R. 2008. Salmonella challenges: prevalence in swine and poultry and potential pathogenicity of such isolates. J. Anim. Sci. 86:E149–E162. 10.2527/jas.2007-0464 [DOI] [PubMed] [Google Scholar]
- 29.Uzzau S, Brown DJ, Wallis T, Rubino S, Leori G, Bernard S, Casadesus J, Platt DJ, Olsen JE. 2000. Host adapted serotypes of Salmonella enterica. Epidemiol. Infect. 125:229–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McDonough PL, Fogelman D, Shin SJ, Brunner MA, Lein DH. 1999. Salmonella enterica serotype Dublin infection: an emerging infectious disease for the northeastern United States. J. Clin. Microbiol. 37:2418–2427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chiu CH, Su LH, Chu C. 2004. Salmonella enterica serotype Choleraesuis: epidemiology, pathogenesis, clinical disease, and treatment. Clin. Microbiol. Rev. 17:311–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chiu CH, Wu TL, Su LH, Chu C, Chia JH, Kuo AJ, Chien MS, Lin TY. 2002. The emergence in Taiwan of fluoroquinolone resistance in Salmonella enterica serotype Choleraesuis. N. Engl. J. Med. 346:413–419 [DOI] [PubMed] [Google Scholar]
- 33.Lynne AM, Dorsey LL, David DE, Foley SL. 2009. Characterisation of antibiotic resistance in host-adapted Salmonella enterica. Int. J. Antimicrob. Agents 34:169–172 [DOI] [PubMed] [Google Scholar]
- 34.Vugia DJ, Samuel M, Farley MM, Marcus R, Shiferaw B, Shallow S, Smith K, Angulo FJ. 2004. Invasive Salmonella infections in the United States, FoodNet, 1996-1999: incidence, serotype distribution, and outcome. Clin. Infect. Dis. 38(Suppl 3):S149–S156. 10.1086/381581 [DOI] [PubMed] [Google Scholar]
- 35.Bearson BL, Wilson L, Foster JW. 1998. A low pH-inducible, PhoPQ-dependent acid tolerance response protects Salmonella typhimurium against inorganic acid stress. J. Bacteriol. 180:2409–2417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bearson SM, Bearson BL, Rasmussen MA. 2006. Identification of Salmonella enterica serovar Typhimurium genes important for survival in the swine gastric environment. Appl. Environ. Microbiol. 72:2829–2836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ruby T, McLaughlin L, Gopinath S, Monack D. 2012. Salmonella's long-term relationship with its host. FEMS Microbiol. Rev. 36:600–615 [DOI] [PubMed] [Google Scholar]
- 38.Velge P, Wiedemann A, Rosselin M, Abed N, Boumart Z, Chausse AM, Grepinet O, Namdari F, Roche SM, Rossignol A, Virlogeux-Payant I. 2012. Multiplicity of Salmonella entry mechanisms, a new paradigm for Salmonella pathogenesis. Open Microbiol. 1:243–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Darwin KH, Miller VL. 1999. Molecular basis of the interaction of Salmonella with the intestinal mucosa. Clin. Microbiol. Rev. 12:405–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Asten AJ, van Dijk JE. 2005. Distribution of “classic” virulence factors among Salmonella spp. FEMS Immunol. Med. Microbiol. 44:251–259 [DOI] [PubMed] [Google Scholar]
- 41.Stevens MP, Humphrey TJ, Maskell DJ. 2009. Molecular insights into farm animal and zoonotic Salmonella infections. Philos. Trans. R. Soc. Lond. B Biol. Sci. 364:2709–2723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carnell SC, Bowen A, Morgan E, Maskell DJ, Wallis TS, Stevens MP. 2007. Role in virulence and protective efficacy in pigs of Salmonella enterica serovar Typhimurium secreted components identified by signature-tagged mutagenesis. Microbiology 153:1940–1952 [DOI] [PubMed] [Google Scholar]
- 43.Morgan E, Campbell JD, Rowe SC, Bispham J, Stevens MP, Bowen AJ, Barrow PA, Maskell DJ, Wallis TS. 2004. Identification of host-specific colonization factors of Salmonella enterica serovar Typhimurium. Mol. Microbiol. 54:994–1010 [DOI] [PubMed] [Google Scholar]
- 44.de Jong H, Ekdahl MO. 1965. Salmonellosis in calves—the effect of dose rate and other factors on transmission. N. Z. Vet. J. 13:59–64 [DOI] [PubMed] [Google Scholar]
- 45.Fedorka-Cray PJ, Kelley LC, Stabel TJ, Gray JT, Laufer JA. 1995. Alternate routes of invasion may affect pathogenesis of Salmonella typhimurium in swine. Infect. Immun. 63:2658–2664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Winnen B, Schlumberger MC, Sturm A, Schupbach K, Siebenmann S, Jenny P, Hardt WD. 2008. Hierarchical effector protein transport by the Salmonella Typhimurium SPI-1 type III secretion system. PLoS One 3:e2178. 10.1371/journal.pone.0002178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schlumberger MC, Hardt WD. 2006. Salmonella type III secretion effectors: pulling the host cell's strings. Curr. Opin. Microbiol. 9:46–54 [DOI] [PubMed] [Google Scholar]
- 48.Galan JE, Wolf-Watz H. 2006. Protein delivery into eukaryotic cells by type III secretion machines. Nature 444:567–573 [DOI] [PubMed] [Google Scholar]
- 49.Marlovits TC, Kubori T, Sukhan A, Thomas DR, Galan JE, Unger VM. 2004. Structural insights into the assembly of the type III secretion needle complex. Science 306:1040–1042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lostroh CP, Lee CA. 2001. The Salmonella pathogenicity island-1 type III secretion system. Microbes Infect. 3:1281–1291 [DOI] [PubMed] [Google Scholar]
- 51.Galan JE. 2001. Salmonella interactions with host cells: type III secretion at work. Annu. Rev. Cell Dev. Biol. 17:53–86 [DOI] [PubMed] [Google Scholar]
- 52.Norris FA, Wilson MP, Wallis TS, Galyov EE, Majerus PW. 1998. SopB, a protein required for virulence of Salmonella dublin, is an inositol phosphate phosphatase. Proc. Natl. Acad. Sci. U. S. A. 95:14057–14059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wallis TS, Galyov EE. 2000. Molecular basis of Salmonella-induced enteritis. Mol. Microbiol. 36:997–1005 [DOI] [PubMed] [Google Scholar]
- 54.Hopkins KL, Threlfall EJ. 2004. Frequency and polymorphism of sopE in isolates of Salmonella enterica belonging to the ten most prevalent serotypes in England and Wales. J. Med. Microbiol. 53:539–543 [DOI] [PubMed] [Google Scholar]
- 55.Mirold S, Rabsch W, Rohde M, Stender S, Tschape H, Russmann H, Igwe E, Hardt WD. 1999. Isolation of a temperate bacteriophage encoding the type III effector protein SopE from an epidemic Salmonella typhimurium strain. Proc. Natl. Acad. Sci. U. S. A. 96:9845–9850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Frost AJ, Bland AP, Wallis TS. 1997. The early dynamic response of the calf ileal epithelium to Salmonella typhimurium. Vet. Pathol. 34:369–386 [DOI] [PubMed] [Google Scholar]
- 57.Goosney DL, Knoechel DG, Finlay BB. 1999. Enteropathogenic E. coli, Salmonella, and Shigella: masters of host cell cytoskeletal exploitation. Emerg. Infect. Dis. 5:216–223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Knodler LA, Vallance BA, Celli J, Winfree S, Hansen B, Montero M, Steele-Mortimer O. 2010. Dissemination of invasive Salmonella via bacterial-induced extrusion of mucosal epithelia. Proc. Natl. Acad. Sci. U. S. A. 107:17733–17738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Holden DW. 2002. Trafficking of the Salmonella vacuole in macrophages. Traffic 3:161–169 [DOI] [PubMed] [Google Scholar]
- 60.Tierrez A, Garcia-del Portillo F. 2005. New concepts in Salmonella virulence: the importance of reducing the intracellular growth rate in the host. Cell. Microbiol. 7:901–909 [DOI] [PubMed] [Google Scholar]
- 61.Hensel M. 2000. Salmonella pathogenicity island 2. Mol. Microbiol. 36:1015–1023 [DOI] [PubMed] [Google Scholar]
- 62.Waterman SR, Holden DW. 2003. Functions and effectors of the Salmonella pathogenicity island 2 type III secretion system. Cell. Microbiol. 5:501–511 [DOI] [PubMed] [Google Scholar]
- 63.Abrahams GL, Hensel M. 2006. Manipulating cellular transport and immune responses: dynamic interactions between intracellular Salmonella enterica and its host cells. Cell. Microbiol. 8:728–737 [DOI] [PubMed] [Google Scholar]
- 64.Hensel M, Shea JE, Waterman SR, Mundy R, Nikolaus T, Banks G, Vazquez-Torres A, Gleeson C, Fang FC, Holden DW. 1998. Genes encoding putative effector proteins of the type III secretion system of Salmonella pathogenicity island 2 are required for bacterial virulence and proliferation in macrophages. Mol. Microbiol. 30:163–174 [DOI] [PubMed] [Google Scholar]
- 65.Bueno SM, Riquelme S, Riedel CA, Kalergis AM. 2012. Mechanisms used by virulent Salmonella to impair dendritic cell function and evade adaptive immunity. Immunology 137:28–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sundquist M, Rydstrom A, Wick MJ. 2004. Immunity to Salmonella from a dendritic point of view. Cell. Microbiol. 6:1–11 [DOI] [PubMed] [Google Scholar]
- 67.Garai P, Gnanadhas DP, Chakravortty D. 2012. Salmonella enterica serovars Typhimurium and Typhi as model organisms: revealing paradigm of host-pathogen interactions. Virulence 3:377–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lahiri A, Iyer N, Das P, Chakravortty D. 2010. Visiting the cell biology of Salmonella infection. Microbes Infect. 12:809–818 [DOI] [PubMed] [Google Scholar]
- 69.Foley SL, Lynne AM. 2008. Food animal-associated Salmonella challenges: pathogenicity and antimicrobial resistance. J. Anim. Sci. 86:E173–E187. 10.2527/jas.2007-0447 [DOI] [PubMed] [Google Scholar]
- 70.Leung KY, Siame BA, Snowball H, Mok YK. 2011. Type VI secretion regulation: crosstalk and intracellular communication. Curr. Opin. Microbiol. 14:9–15 [DOI] [PubMed] [Google Scholar]
- 71.Marcus SL, Brumell JH, Pfeifer CG, Finlay BB. 2000. Salmonella pathogenicity islands: big virulence in small packages. Microbes Infect. 2:145–156 [DOI] [PubMed] [Google Scholar]
- 72.Bingle LE, Bailey CM, Pallen MJ. 2008. Type VI secretion: a beginner's guide. Curr. Opin. Microbiol. 11:3–8 [DOI] [PubMed] [Google Scholar]
- 73.Amavisit P, Lightfoot D, Browning GF, Markham PF. 2003. Variation between pathogenic serovars within Salmonella pathogenicity islands. J. Bacteriol. 185:3624–3635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dieye Y, Ameiss K, Mellata M, Curtiss R., III 2009. The Salmonella pathogenicity island (SPI) 1 contributes more than SPI2 to the colonization of the chicken by Salmonella enterica serovar Typhimurium. BMC Microbiol. 9:3. 10.1186/1471-2180-9-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhang S, Kingsley RA, Santos RL, Andrews-Polymenis H, Raffatellu M, Figueiredo J, Nunes J, Tsolis RM, Adams LG, Baumler AJ. 2003. Molecular pathogenesis of Salmonella enterica serotype Typhimurium-induced diarrhea. Infect. Immun. 71:1–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhang S, Santos RL, Tsolis RM, Stender S, Hardt WD, Baumler AJ, Adams LG. 2002. The Salmonella enterica serotype Typhimurium effector proteins SipA, SopA, SopB, SopD, and SopE2 act in concert to induce diarrhea in calves. Infect. Immun. 70:3843–3855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Coombes BK, Coburn BA, Potter AA, Gomis S, Mirakhur K, Li Y, Finlay BB. 2005. Analysis of the contribution of Salmonella pathogenicity islands 1 and 2 to enteric disease progression using a novel bovine ileal loop model and a murine model of infectious enterocolitis. Infect. Immun. 73:7161–7169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Boyen F, Pasmans F, Donne E, Van Immerseel F, Morgan E, Adriaensen C, Hernalsteens JP, Wallis TS, Ducatelle R, Haesebrouck F. 2006. The fibronectin binding protein ShdA is not a prerequisite for long term faecal shedding of Salmonella Typhimurium in pigs. Vet. Microbiol. 115:284–290 [DOI] [PubMed] [Google Scholar]
- 79.Kingsley RA, Santos RL, Keestra AM, Adams LG, Baumler AJ. 2002. Salmonella enterica serotype Typhimurium ShdA is an outer membrane fibronectin-binding protein that is expressed in the intestine. Mol. Microbiol. 43:895–905 [DOI] [PubMed] [Google Scholar]
- 80.Gerlach RG, Claudio N, Rohde M, Jackel D, Wagner C, Hensel M. 2008. Cooperation of Salmonella pathogenicity islands 1 and 4 is required to breach epithelial barriers. Cell. Microbiol. 10:2364–2376 [DOI] [PubMed] [Google Scholar]
- 81.Rotger R, Casadesus J. 1999. The virulence plasmids of Salmonella. Int. Microbiol. 2:177–184 [PubMed] [Google Scholar]
- 82.Ahmer BM, Tran M, Heffron F. 1999. The virulence plasmid of Salmonella typhimurium is self-transmissible. J. Bacteriol. 181:1364–1368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Han J, Lynne AM, David DE, Tang H, Xu J, Nayak R, Kaldhone P, Logue CM, Foley SL. 2012. DNA sequence analysis of plasmids from multidrug resistant Salmonella enterica serotype Heidelberg isolates. PLoS One 7:e51160. 10.1371/journal.pone.0051160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Johnson TJ, Thorsness JL, Anderson CP, Lynne AM, Foley SL, Han J, Fricke WF, McDermott PF, White DG, Khatri M, Stell AL, Flores C, Singer RS. 2010. Horizontal gene transfer of a ColV plasmid has resulted in a dominant avian clonal type of Salmonella enterica serovar Kentucky. PLoS One 5:e15524. 10.1371/journal.pone.0015524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ashkenazi S, Cleary TG, Murray BE, Wanger A, Pickering LK. 1988. Quantitative analysis and partial characterization of cytotoxin production by Salmonella strains. Infect. Immun. 56:3089–3094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ketyi I, Pacsa S, Emody L, Vertenyi A, Kocsis B, Kuch B. 1979. Shigella dysenteriae 1-like cytotoxic enterotoxins produced by Salmonella strains. Acta Microbiol. Acad. Sci. Hung. 26:217–223 [PubMed] [Google Scholar]
- 87.Prager R, Fruth A, Tschape H. 1995. Salmonella enterotoxin (stn) gene is prevalent among strains of Salmonella enterica, but not among Salmonella bongori and other Enterobacteriaceae. FEMS Immunol. Med. Microbiol. 12:47–50 [DOI] [PubMed] [Google Scholar]
- 88.Libby SJ, Goebel W, Ludwig A, Buchmeier N, Bowe F, Fang FC, Guiney DG, Songer JG, Heffron F. 1994. A cytolysin encoded by Salmonella is required for survival within macrophages. Proc. Natl. Acad. Sci. U. S. A. 91:489–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Collinson SK, Liu SL, Clouthier SC, Banser PA, Doran JL, Sanderson KE, Kay WW. 1996. The location of four fimbrin-encoding genes, agfA, fimA, sefA and sefD, on the Salmonella enteritidis and/or S. typhimurium XbaI-BlnI genomic restriction maps. Gene 169:75–80 [DOI] [PubMed] [Google Scholar]
- 90.Clouthier SC, Collinson SK, Kay WW. 1994. Unique fimbriae-like structures encoded by sefD of the SEF14 fimbrial gene cluster of Salmonella enteritidis. Mol. Microbiol. 12:893–901 [DOI] [PubMed] [Google Scholar]
- 91.Betancor L, Yim L, Martinez A, Fookes M, Sasias S, Schelotto F, Thomson N, Maskell D, Chabalgoity JA. 2012. Genomic comparison of the closely related Salmonella enterica serovars Enteritidis and Dublin. Open Microbiol. J. 6:5–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.White AP, Gibson DL, Collinson SK, Banser PA, Kay WW. 2003. Extracellular polysaccharides associated with thin aggregative fimbriae of Salmonella enterica serovar Enteritidis. J. Bacteriol. 185:5398–5407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Thorns CJ, Turcotte C, Gemmell CG, Woodward MJ. 1996. Studies into the role of the SEF14 fimbrial antigen in the pathogenesis of Salmonella enteritidis. Microb. Pathog. 20:235–246 [DOI] [PubMed] [Google Scholar]
- 94.Zhang XL, Tsui IS, Yip CM, Fung AW, Wong DK, Dai X, Yang Y, Hackett J, Morris C. 2000. Salmonella enterica serovar Typhi uses type IVB pili to enter human intestinal epithelial cells. Infect. Immun. 68:3067–3073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Baumler AJ, Heffron F. 1995. Identification and sequence analysis of lpfABCDE, a putative fimbrial operon of Salmonella typhimurium. J. Bacteriol. 177:2087–2097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Friedrich MJ, Kinsey NE, Vila J, Kadner RJ. 1993. Nucleotide sequence of a 13.9 kb segment of the 90 kb virulence plasmid of Salmonella typhimurium: the presence of fimbrial biosynthetic genes. Mol. Microbiol. 8:543–558 [DOI] [PubMed] [Google Scholar]
- 97.Turcotte C, Woodward MJ. 1993. Cloning, DNA nucleotide sequence and distribution of the gene encoding the SEF14 fimbrial antigen of Salmonella enteritidis. J. Gen. Microbiol. 139:1477–1485 [DOI] [PubMed] [Google Scholar]
- 98.Doran JL, Collinson SK, Clouthier SC, Cebula TA, Koch WH, Burian J, Banser PA, Todd EC, Kay WW. 1996. Diagnostic potential of sefA DNA probes to Salmonella enteritidis and certain other O-serogroup D1 Salmonella serovars. Mol. Cell. Probes 10:233–246 [DOI] [PubMed] [Google Scholar]
- 99.Althouse C, Patterson S, Fedorka-Cray P, Isaacson RE. 2003. Type 1 fimbriae of Salmonella enterica serovar Typhimurium bind to enterocytes and contribute to colonization of swine in vivo. Infect. Immun. 71:6446–6452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.De Buck J, Van Immerseel F, Haesebrouck F, Ducatelle R. 2005. Protection of laying hens against Salmonella Enteritidis by immunization with type 1 fimbriae. Vet. Microbiol. 105:93–101 [DOI] [PubMed] [Google Scholar]
- 101.Clayton DJ, Bowen AJ, Hulme SD, Buckley AM, Deacon VL, Thomson NR, Barrow PA, Morgan E, Jones MA, Watson M, Stevens MP. 2008. Analysis of the role of 13 major fimbrial subunits in colonisation of the chicken intestines by Salmonella enterica serovar Enteritidis reveals a role for a novel locus. BMC Microbiol. 8:228. 10.1186/1471-2180-8-228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dauga C, Zabrovskaia A, Grimont PA. 1998. Restriction fragment length polymorphism analysis of some flagellin genes of Salmonella enterica. J. Clin. Microbiol. 36:2835–2843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Turner AK, Lovell MA, Hulme SD, Zhang-Barber L, Barrow PA. 1998. Identification of Salmonella typhimurium genes required for colonization of the chicken alimentary tract and for virulence in newly hatched chicks. Infect. Immun. 66:2099–2106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gantois I, Ducatelle R, Pasmans F, Haesebrouck F, Hautefort I, Thompson A, Hinton JC, Van Immerseel F. 2006. Butyrate specifically down-regulates Salmonella pathogenicity island 1 gene expression. Appl. Environ. Microbiol. 72:946–949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ochman H, Moran NA. 2001. Genes lost and genes found: evolution of bacterial pathogenesis and symbiosis. Science 292:1096–1099 [DOI] [PubMed] [Google Scholar]
- 106.Maurelli AT. 2007. Black holes, antivirulence genes, and gene inactivation in the evolution of bacterial pathogens. FEMS Microbiol. Lett. 267:1–8 [DOI] [PubMed] [Google Scholar]
- 107.Groisman EA, Ochman H. 1997. How Salmonella became a pathogen. Trends Microbiol. 5:343–349 [DOI] [PubMed] [Google Scholar]
- 108.Bowe F, Lipps CJ, Tsolis RM, Groisman E, Heffron F, Kusters JG. 1998. At least four percent of the Salmonella typhimurium genome is required for fatal infection of mice. Infect. Immun. 66:3372–3377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jarvik T, Smillie C, Groisman EA, Ochman H. 2010. Short-term signatures of evolutionary change in the Salmonella enterica serovar Typhimurium 14028 genome. J. Bacteriol. 192:560–567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Baumler AJ, Tsolis RM, Ficht TA, Adams LG. 1998. Evolution of host adaptation in Salmonella enterica. Infect. Immun. 66:4579–4587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jacobsen A, Hendriksen RS, Aaresturp FM, Ussery DW, Friis C. 2011. The Salmonella enterica pan-genome. Microb. Ecol. 62:487–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Quiroz TS, Nieto PA, Tobar HE, Salazar-Echegarai FJ, Lizana RJ, Quezada CP, Santiviago CA, Araya DV, Riedel CA, Kalergis AM, Bueno SM. 2011. Excision of an unstable pathogenicity island in Salmonella enterica serovar Enteritidis is induced during infection of phagocytic cells. PLoS One 6:e26031. 10.1371/journal.pone.0026031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wozniak RA, Fouts DE, Spagnoletti M, Colombo MM, Ceccarelli D, Garriss G, Dery C, Burrus V, Waldor MK. 2009. Comparative ICE genomics: insights into the evolution of the SXT/R391 family of ICEs. PLoS Genet. 5:e1000786. 10.1371/journal.pgen.1000786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Seth-Smith HM, Fookes MC, Okoro CK, Baker S, Harris SR, Scott P, Pickard D, Quail MA, Churcher C, Sanders M, Harmse J, Dougan G, Parkhill J, Thomson NR. 2012. Structure, diversity, and mobility of the Salmonella pathogenicity island 7 family of integrative and conjugative elements within Enterobacteriaceae. J. Bacteriol. 194:1494–1504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Moreno Switt AI, den Bakker HC, Cummings CA, Rodriguez-Rivera LD, Govoni G, Raneiri ML, Degoricija L, Brown S, Hoelzer K, Peters JE, Bolchacova E, Furtado MR, Wiedmann M. 2012. Identification and characterization of novel Salmonella mobile elements involved in the dissemination of genes linked to virulence and transmission. PLoS One 7:e41247. 10.1371/journal.pone.0041247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Williams LE, Wireman J, Hilliard VC, Summers AO. 2013. Large plasmids of Escherichia coli and Salmonella encode highly diverse arrays of accessory genes on common replicon families. Plasmid 69:36–48 [DOI] [PubMed] [Google Scholar]
- 117.Bielak E, Bergenholtz RD, Jorgensen MS, Sorensen SJ, Hansen LH, Hasman H. 2011. Investigation of diversity of plasmids carrying the blaTEM-52 gene. J. Antimicrob. Chemother. 66:2465–2474 [DOI] [PubMed] [Google Scholar]
- 118.Jones C, Stanley J. 1992. Salmonella plasmids of the pre-antibiotic era. J. Gen. Microbiol. 138:189–197 [DOI] [PubMed] [Google Scholar]
- 119.Gilmour MW, Thomson NR, Sanders M, Parkhill J, Taylor DE. 2004. The complete nucleotide sequence of the resistance plasmid R478: defining the backbone components of incompatibility group H conjugative plasmids through comparative genomics. Plasmid 52:182–202 [DOI] [PubMed] [Google Scholar]
- 120.Tosini F, Visca P, Luzzi I, Dionisi AM, Pezzella C, Petrucca A, Carattoli A. 1998. Class 1 integron-borne multiple-antibiotic resistance carried by IncFI and IncL/M plasmids in Salmonella enterica serotype Typhimurium. Antimicrob. Agents Chemother. 42:3053–3058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Welch TJ, Fricke WF, McDermott PF, White DG, Rosso ML, Rasko DA, Mammel MK, Eppinger M, Rosovitz MJ, Wagner D, Rahalison L, Leclerc JE, Hinshaw JM, Lindler LE, Cebula TA, Carniel E, Ravel J. 2007. Multiple antimicrobial resistance in plague: an emerging public health risk. PLoS One 2:e309. 10.1371/journal.pone.0000309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Garcia-Quintanilla M, Ramos-Morales F, Casadesus J. 2008. Conjugal transfer of the Salmonella enterica virulence plasmid in the mouse intestine. J. Bacteriol. 190:1922–1927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Rychlik I, Karasova D, Sebkova A, Volf J, Sisak F, Havlickova H, Kummer V, Imre A, Szmolka A, Nagy B. 2009. Virulence potential of five major pathogenicity islands (SPI-1 to SPI-5) of Salmonella enterica serovar Enteritidis for chickens. BMC Microbiol. 9:268. 10.1186/1471-2180-9-268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Guiney DG, Fang FC, Krause M, Libby S. 1994. Plasmid-mediated virulence genes in non-typhoid Salmonella serovars. FEMS Microbiol. Lett. 124:1–9 [DOI] [PubMed] [Google Scholar]
- 125.Wilson JA, Gulig PA. 1998. Regulation of the spvR gene of the Salmonella typhimurium virulence plasmid during exponential-phase growth in intracellular salts medium and at stationary phase in L broth. Microbiology 144:1823–1833 [DOI] [PubMed] [Google Scholar]
- 126.Gulig PA, Doyle TJ, Hughes JA, Matsui H. 1998. Analysis of host cells associated with the Spv-mediated increased intracellular growth rate of Salmonella typhimurium in mice. Infect. Immun. 66:2471–2485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gulig PA, Danbara H, Guiney DG, Lax AJ, Norel F, Rhen M. 1993. Molecular analysis of spv virulence genes of the Salmonella virulence plasmids. Mol. Microbiol. 7:825–830 [DOI] [PubMed] [Google Scholar]
- 128.Chu C, Feng Y, Chien AC, Hu S, Chu CH, Chiu CH. 2008. Evolution of genes on the Salmonella virulence plasmid phylogeny revealed from sequencing of the virulence plasmids of S. enterica serotype Dublin and comparative analysis. Genomics 92:339–343 [DOI] [PubMed] [Google Scholar]
- 129.Garcia P, Guerra B, Bances M, Mendoza MC, Rodicio MR. 2011. IncA/C plasmids mediate antimicrobial resistance linked to virulence genes in the Spanish clone of the emerging Salmonella enterica serotype 4,[5],12:i. J. Antimicrob. Chemother. 66:543–549 [DOI] [PubMed] [Google Scholar]
- 130.Garcia Fernandez A, Cloeckaert A, Bertini A, Praud K, Doublet B, Weill FX, Carattoli A. 2007. Comparative analysis of IncHI2 plasmids carrying blaCTX-M-2 or blaCTX-M-9 from Escherichia coli and Salmonella enterica strains isolated from poultry and humans. Antimicrob. Agents Chemother. 51:4177–4180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yu H, Wang J, Ye J, Tang P, Chu C, Hu S, Chiu CH. 2006. Complete nucleotide sequence of pSCV50, the virulence plasmid of Salmonella enterica serovar Choleraesuis SC-B67. Plasmid 55:145–151 [DOI] [PubMed] [Google Scholar]
- 132.Olsen JE, Brown DJ, Thomsen LE, Platt DJ, Chadfield MS. 2004. Differences in the carriage and the ability to utilize the serotype associated virulence plasmid in strains of Salmonella enterica serotype Typhimurium investigated by use of a self-transferable virulence plasmid, pOG669. Microb. Pathog. 36:337–347 [DOI] [PubMed] [Google Scholar]
- 133.Villa L, Carattoli A. 2005. Integrons and transposons on the Salmonella enterica serovar Typhimurium virulence plasmid. Antimicrob. Agents Chemother. 49:1194–1197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Herrero A, Mendoza MC, Rodicio R, Rodicio MR. 2008. Characterization of pUO-StVR2, a virulence-resistance plasmid evolved from the pSLT virulence plasmid of Salmonella enterica serovar Typhimurium. Antimicrob. Agents Chemother. 52:4514–4517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Rodriguez I, Rodicio MR, Guerra B, Hopkins KL. 2012. Potential international spread of multidrug-resistant invasive Salmonella enterica serovar Enteritidis. Emerg. Infect. Dis. 18:1173–1176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Fluit AC. 2005. Towards more virulent and antibiotic-resistant Salmonella? FEMS Immunol. Med. Microbiol. 43:1–11 [DOI] [PubMed] [Google Scholar]
- 137.Folster JP, Pecic G, McCullough A, Rickert R, Whichard JM. 2011. Characterization of bla(CMY)-encoding plasmids among Salmonella isolated in the United States in 2007. Foodborne Pathog. Dis. 8:1289–1294 [DOI] [PubMed] [Google Scholar]
- 138.Folster JP, Pecic G, Singh A, Duval B, Rickert R, Ayers S, Abbott J, McGlinchey B, Bauer-Turpin J, Haro J, Hise K, Zhao S, Fedorka-Cray PJ, Whichard J, McDermott PF. 2012. Characterization of extended-spectrum cephalosporin-resistant Salmonella enterica serovar Heidelberg isolated from food animals, retail meat, and humans in the United States 2009. Foodborne Pathog. Dis. 9:638–645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Johnson TJ, Siek KE, Johnson SJ, Nolan LK. 2005. DNA sequence and comparative genomics of pAPEC-O2-R, an avian pathogenic Escherichia coli transmissible R plasmid. Antimicrob. Agents Chemother. 49:4681–4688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Garcia-Quintanilla M, Casadesus J. 2011. Virulence plasmid interchange between strains ATCC 14028, LT2, and SL1344 of Salmonella enterica serovar Typhimurium. Plasmid 65:169–175 [DOI] [PubMed] [Google Scholar]
- 141.Sampei G, Furuya N, Tachibana K, Saitou Y, Suzuki T, Mizobuchi K, Komano T. 2010. Complete genome sequence of the incompatibility group I1 plasmid R64. Plasmid 64:92–103 [DOI] [PubMed] [Google Scholar]
- 142.Johnson TJ, Shepard SM, Rivet B, Danzeisen JL, Carattoli A. 2011. Comparative genomics and phylogeny of the IncI1 plasmids: a common plasmid type among porcine enterotoxigenic Escherichia coli. Plasmid 66:144–151 [DOI] [PubMed] [Google Scholar]
- 143.Garcia-Fernandez A, Fortini D, Veldman K, Mevius D, Carattoli A. 2009. Characterization of plasmids harbouring qnrS1, qnrB2 and qnrB19 genes in Salmonella. J. Antimicrob. Chemother. 63:274–281 [DOI] [PubMed] [Google Scholar]
- 144.Shahada F, Sekizuka T, Kuroda M, Kusumoto M, Ohishi D, Matsumoto A, Okazaki H, Tanaka K, Uchida I, Izumiya H, Watanabe H, Tamamura Y, Iwata T, Akiba M. 2011. Characterization of Salmonella enterica serovar Typhimurium isolates harboring a chromosomally encoded CMY-2 beta-lactamase gene located on a multidrug resistance genomic island. Antimicrob. Agents Chemother. 55:4114–4121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Antunes P, Mourao J, Machado J, Peixe L. 2011. First description of qnrS1-IncN plasmid in a ST11 Salmonella Enteritidis clinical isolate from Portugal. Diagn. Microbiol. Infect. Dis. 69:463–465 [DOI] [PubMed] [Google Scholar]
- 146.Szmolka A, Fortini D, Villa L, Carattoli A, Anjum MF, Nagy B. 2011. First report on IncN plasmid-mediated quinolone resistance gene qnrS1 in porcine Escherichia coli in Europe. Microb. Drug Resist. 17:567–573 [DOI] [PubMed] [Google Scholar]
- 147.Gutierrez B, Herrera-Leon S, Escudero JA, Hidalgo L, Gonzalez-Sanz R, Arroyo M, San Millan A, Echeita MA, Gonzalez-Zorn B. 2009. Novel genetic environment of qnrB2 associated with TEM-1 and SHV-12 on pB1004, an IncHI2 plasmid, in Salmonella Bredeney BB1047 from Spain. J. Antimicrob. Chemother. 64:1334–1336 [DOI] [PubMed] [Google Scholar]
- 148.Garcia-Fernandez A, Chiaretto G, Bertini A, Villa L, Fortini D, Ricci A, Carattoli A. 2008. Multilocus sequence typing of IncI1 plasmids carrying extended-spectrum beta-lactamases in Escherichia coli and Salmonella of human and animal origin. J. Antimicrob. Chemother. 61:1229–1233 [DOI] [PubMed] [Google Scholar]
- 149.Cain AK, Hall RM. 2012. Evolution of a multiple antibiotic resistance region in IncHI1 plasmids: reshaping resistance regions in situ. J. Antimicrob. Chemother. 67:2848–2853 [DOI] [PubMed] [Google Scholar]
- 150.Fernandez-Alarcon C, Singer RS, Johnson TJ. 2011. Comparative genomics of multidrug resistance-encoding IncA/C plasmids from commensal and pathogenic Escherichia coli from multiple animal sources. PLoS One 6:e23415. 10.1371/journal.pone.0023415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Fricke WF, Welch TJ, McDermott PF, Mammel MK, LeClerc JE, White DG, Cebula TA, Ravel J. 2009. Comparative genomics of the IncA/C multidrug resistance plasmid family. J. Bacteriol. 191:4750–4757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Tran T, Andres P, Petroni A, Soler-Bistue A, Albornoz E, Zorreguieta A, Reyes-Lamothe R, Sherratt DJ, Corso A, Tolmasky ME. 2012. Small plasmids harboring qnrB19: a model for plasmid evolution mediated by site-specific recombination at oriT and Xer sites. Antimicrob. Agents Chemother. 56:1821–1827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Hammerl JA, Beutlich J, Hertwig S, Mevius D, Threlfall EJ, Helmuth R, Guerra B. 2010. pSGI15, a small ColE-like qnrB19 plasmid of a Salmonella enterica serovar Typhimurium strain carrying Salmonella genomic island 1 (SGI1). J. Antimicrob. Chemother. 65:173–175 [DOI] [PubMed] [Google Scholar]
- 154.Targant H, Doublet B, Aarestrup FM, Cloeckaert A, Madec JY. 2010. IS6100-mediated genetic rearrangement within the complex class 1 integron In104 of the Salmonella genomic island 1. J. Antimicrob. Chemother. 65:1543–1545 [DOI] [PubMed] [Google Scholar]
- 155.Siebor E, Neuwirth C. 2011. The new variant of Salmonella genomic island 1 (SGI1-V) from a Proteus mirabilis French clinical isolate harbours blaVEB-6 and qnrA1 in the multiple antibiotic resistance region. J. Antimicrob. Chemother. 66:2513–2520 [DOI] [PubMed] [Google Scholar]
- 156.Krauland M, Harrison L, Paterson D, Marsh J. 2010. Novel integron gene cassette arrays identified in a global collection of multi-drug resistant non-typhoidal Salmonella enterica. Curr. Microbiol. 60:217–223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Beutlich J, Jahn S, Malorny B, Hauser E, Huhn S, Schroeter A, Rodicio MR, Appel B, Threlfall J, Mevius D, Helmuth R, Guerra B. 2011. Antimicrobial resistance and virulence determinants in European Salmonella genomic island 1-positive Salmonella enterica isolates from different origins. Appl. Environ. Microbiol. 77:5655–5664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kiss J, Nagy B, Olasz F. 2012. Stability, entrapment and variant formation of Salmonella genomic island 1. PLoS One 7:e32497. 10.1371/journal.pone.0032497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Douard G, Praud K, Cloeckaert A, Doublet B. 2010. The Salmonella genomic island 1 is specifically mobilized in trans by the IncA/C multidrug resistance plasmid family. PLoS One 5:e15302. 10.1371/journal.pone.0015302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Frost JA, Ward LR, Rowe B. 1989. Acquisition of a drug resistance plasmid converts Salmonella enteritidis phage type 4 to phage type 24. Epidemiol. Infect. 103:243–248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Brown DJ, Baggesen DL, Platt DJ, Olsen JE. 1999. Phage type conversion in Salmonella enterica serotype Enteritidis caused by the introduction of a resistance plasmid of incompatibility group X (IncX). Epidemiol. Infect. 122:19–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Coetzee JN, Bradley DE, du Toit L, Hedges RW. 1988. Bacteriophage X-2: a filamentous phage lysing IncX-plasmid-harbouring bacterial strains. J. Gen. Microbiol. 134:2535–2541 [DOI] [PubMed] [Google Scholar]
- 163.Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, Walsh TR. 2009. Characterization of a new metallo-beta-lactamase gene, bla(NDM-1), and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob. Agents Chemother. 53:5046–5054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Ho PL, Lo WU, Yeung MK, Lin CH, Chow KH, Ang I, Tong AH, Bao JY, Lok S, Lo JY. 2011. Complete sequencing of pNDM-HK encoding NDM-1 carbapenemase from a multidrug-resistant Escherichia coli strain isolated in Hong Kong. PLoS One 6:e17989. 10.1371/journal.pone.0017989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Poirel L, Bonnin RA, Nordmann P. 2011. Analysis of the resistome of a multidrug-resistant NDM-1-producing Escherichia coli strain by high-throughput genome sequencing. Antimicrob. Agents Chemother. 55:4224–4229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Poirel L, Dortet L, Bernabeu S, Nordmann P. 2011. Genetic features of blaNDM-1-positive Enterobacteriaceae. Antimicrob. Agents Chemother. 55:5403–5407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Carattoli A, Villa L, Poirel L, Bonnin RA, Nordmann P. 2012. Evolution of IncA/C blaCMY-2-carrying plasmids by acquisition of the blaNDM-1 carbapenemase gene. Antimicrob. Agents Chemother. 56:783–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Chen Y, Zhou Z, Jiang Y, Yu Y. 2011. Emergence of NDM-1-producing Acinetobacter baumannii in China. J. Antimicrob. Chemother. 66:1255–1259 [DOI] [PubMed] [Google Scholar]
- 169.Savard P, Gopinath R, Zhu W, Kitchel B, Rasheed JK, Tekle T, Roberts A, Ross T, Razeq J, Landrum BM, Wilson LE, Limbago B, Perl TM, Carroll KC. 2011. First NDM-positive Salmonella sp. strain identified in the United States. Antimicrob. Agents Chemother. 55:5957–5958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Reva O, Bezuidt O. 2012. Distribution of horizontally transferred heavy metal resistance operons in recent outbreak bacteria. Mob. Genet. Elements 2:96–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Brilli M, Mengoni A, Fondi M, Bazzicalupo M, Lio P, Fani R. 2008. Analysis of plasmid genes by phylogenetic profiling and visualization of homology relationships using Blast2Network. BMC Bioinformatics 9:551. 10.1186/1471-2105-9-551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Figueroa-Bossi N, Bossi L. 1999. Inducible prophages contribute to Salmonella virulence in mice. Mol. Microbiol. 33:167–176 [DOI] [PubMed] [Google Scholar]
- 173.Lemire S, Figueroa-Bossi N, Bossi L. 2011. Bacteriophage crosstalk: coordination of prophage induction by trans-acting antirepressors. PLoS Genet. 7:e1002149. 10.1371/journal.pgen.1002149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Kropinski AM, Sulakvelidze A, Konczy P, Poppe C. 2007. Salmonella phages and prophages—genomics and practical aspects. Methods Mol. Biol. 394:133–175 [DOI] [PubMed] [Google Scholar]
- 175.Casjens SR, Thuman-Commike PA. 2011. Evolution of mosaically related tailed bacteriophage genomes seen through the lens of phage P22 virion assembly. Virology 411:393–415 [DOI] [PubMed] [Google Scholar]
- 176.Poppe C. 1999. Epidemiology of Salmonella enterica serovar Enteritidis, p 3–18 In Saeed AM, Gast RK, Potter ME, Wall PG. (ed), Salmonella enterica serovar Enteritidis in humans and animals—epidemiology, pathogenesis, and control. Iowa State University Press, Ames, IA [Google Scholar]
- 177.Pang S, Octavia S, Reeves PR, Wang Q, Gilbert GL, Sintchenko V, Lan R. 2012. Genetic relationships of phage types and single nucleotide polymorphism typing of Salmonella enterica serovar Typhimurium. J. Clin. Microbiol. 50:727–734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Altekruse S, Koehler J, Hickman-Brenner F, Tauxe RV, Ferris K. 1993. A comparison of Salmonella enteritidis phage types from egg-associated outbreaks and implicated laying flocks. Epidemiol. Infect. 110:17–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Boyd EF. 2012. Bacteriophage-encoded bacterial virulence factors and phage-pathogenicity island interactions. Adv. Virus Res. 82:91–118 [DOI] [PubMed] [Google Scholar]
- 180.Brown NF, Coombes BK, Bishop JL, Wickham ME, Lowden MJ, Gal-Mor O, Goode DL, Boyle EC, Sanderson KL, Finlay BB. 2011. Salmonella phage ST64B encodes a member of the SseK/NleB effector family. PLoS One 6:e17824. 10.1371/journal.pone.0017824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Wray C, Beedell YE, McLaren IM. 1991. A survey of antimicrobial resistance in salmonellae isolated from animals in England and Wales during 1984-1987. Br. Vet. J. 147:356–369 [DOI] [PubMed] [Google Scholar]
- 182.Threlfall EJ, Ward LR, Rowe B. 1978. Spread of multiresistant strains of Salmonella typhimurium phage types 204 and 193 in Britain. Br. Med. J. 2:997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Kuhn H, Rabsch W, Tschape H, Tietze E. 1982. Characterization and epidemiology of a Salmonella typhimurium epidemic strain. Z. Arztl. Fortbild. (Jena) 76:607–610 [PubMed] [Google Scholar]
- 184.Slominski B, Calkiewicz J, Golec P, Wegrzyn G, Wrobel B. 2007. Plasmids derived from Gifsy-1/Gifsy-2, lambdoid prophages contributing to the virulence of Salmonella enterica serovar Typhimurium: implications for the evolution of replication initiation proteins of lambdoid phages and enterobacteria. Microbiology 153:1884–1896 [DOI] [PubMed] [Google Scholar]
- 185.Figueroa-Bossi N, Uzzau S, Maloriol D, Bossi L. 2001. Variable assortment of prophages provides a transferable repertoire of pathogenic determinants in Salmonella. Mol. Microbiol. 39:260–271 [DOI] [PubMed] [Google Scholar]
- 186.Ho TD, Figueroa-Bossi N, Wang M, Uzzau S, Bossi L, Slauch JM. 2002. Identification of GtgE, a novel virulence factor encoded on the Gifsy-2 bacteriophage of Salmonella enterica serovar Typhimurium. J. Bacteriol. 184:5234–5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Rychlik I, Sebkova A, Gregorova D, Karpiskova R. 2001. Low-molecular-weight plasmid of Salmonella enterica serovar Enteritidis codes for retron reverse transcriptase and influences phage resistance. J. Bacteriol. 183:2852–2858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Smarda J, Doroszkiewicz W, Lachowicz TM. 1990. Sensitivity of Shigella flexneri and Escherichia coli bacteria to bacteriophages and to colicins, lost or established by the acquisition of R plasmids. Acta Microbiol. Pol. 39:23–35 [PubMed] [Google Scholar]
- 189.Fricke WF, Mammel MK, McDermott PF, Tartera C, White DG, Leclerc JE, Ravel J, Cebula TA. 2011. Comparative genomics of 28 Salmonella enterica isolates: evidence for CRISPR-mediated adaptive sublineage evolution. J. Bacteriol. 193:3556–3568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Matthews TD, Edwards R, Maloy S. 2010. Chromosomal rearrangements formed by rrn recombination do not improve replichore balance in host-specific Salmonella enterica serovars. PLoS One 5:e13503. 10.1371/journal.pone.0013503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Thomson NR, Clayton DJ, Windhorst D, Vernikos G, Davidson S, Churcher C, Quail MA, Stevens M, Jones MA, Watson M, Barron A, Layton A, Pickard D, Kingsley RA, Bignell A, Clark L, Harris B, Ormond D, Abdellah Z, Brooks K, Cherevach I, Chillingworth T, Woodward J, Norberczak H, Lord A, Arrowsmith C, Jagels K, Moule S, Mungall K, Sanders M, Whitehead S, Chabalgoity JA, Maskell D, Humphrey T, Roberts M, Barrow PA, Dougan G, Parkhill J. 2008. Comparative genome analysis of Salmonella Enteritidis PT4 and Salmonella Gallinarum 287/91 provides insights into evolutionary and host adaptation pathways. Genome Res. 18:1624–1637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Helm RA, Lee AG, Christman HD, Maloy S. 2003. Genomic rearrangements at rrn operons in Salmonella. Genetics 165:951–959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Feng Y, Chien KY, Chen HL, Chiu CH. 2012. Pseudogene recoding revealed from proteomic analysis of Salmonella serovars. J. Proteome Res. 11:1715–1719 [DOI] [PubMed] [Google Scholar]
- 194.Holt KE, Thomson NR, Wain J, Langridge GC, Hasan R, Bhutta ZA, Quail MA, Norbertczak H, Walker D, Simmonds M, White B, Bason N, Mungall K, Dougan G, Parkhill J. 2009. Pseudogene accumulation in the evolutionary histories of Salmonella enterica serovars Paratyphi A and Typhi. BMC Genomics 10:36. 10.1186/1471-2164-10-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Kuo CH, Ochman H. 2010. The extinction dynamics of bacterial pseudogenes. PLoS Genet. 6:e1001050. 10.1371/journal.pgen.1001050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Hurst LD. 2002. The Ka/Ks ratio: diagnosing the form of sequence evolution. Trends Genet. 18:486. [DOI] [PubMed] [Google Scholar]
- 197.Winter SE, Raffatellu M, Wilson RP, Russmann H, Baumler AJ. 2008. The Salmonella enterica serotype Typhi regulator TviA reduces interleukin-8 production in intestinal epithelial cells by repressing flagellin secretion. Cell. Microbiol. 10:247–261 [DOI] [PubMed] [Google Scholar]
- 198.Centers for Disease Control and Prevention 2011. Salmonella surveillance: annual summary, 2009. Centers for Disease Control and Prevention, Atlanta, GA [Google Scholar]
- 199.Elson R, Little CL, Mitchell RT. 2005. Salmonella and raw shell eggs: results of a cross-sectional study of contamination rates and egg safety practices in the United Kingdom catering sector in 2003. J. Food Prot. 68:256–264 [DOI] [PubMed] [Google Scholar]
- 200.Hennessy TW, Cheng LH, Kassenborg H, Ahuja SD, Mohle-Boetani J, Marcus R, Shiferaw B, Angulo FJ. 2004. Egg consumption is the principal risk factor for sporadic Salmonella serotype Heidelberg infections: a case-control study in FoodNet sites. Clin. Infect. Dis. 38:S237–S243. 10.1086/381593 [DOI] [PubMed] [Google Scholar]
- 201.Kuehn BM. 2010. Salmonella cases traced to egg producers: findings trigger recall of more than 500 million eggs. JAMA 304:1316. 10.1001/jama.2010.1330 [DOI] [PubMed] [Google Scholar]
- 202.Roy P, Dhillon AS, Lauerman LH, Schaberg DM, Bandli D, Johnson S. 2002. Results of Salmonella isolation from poultry products, poultry, poultry environment, and other characteristics. Avian Dis. 46:17–24 [DOI] [PubMed] [Google Scholar]
- 203.Han J, David DE, Deck J, Lynne AM, Kaldhone P, Nayak R, Stefanova R, Foley SL. 2011. Comparison of Salmonella enterica serovar Heidelberg isolated from human patients with those from animal and food sources. J. Clin. Microbiol. 49:1130–1133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Hennessy TW, Hedberg CW, Slutsker L, White KE, Besser-Wiek JM, Moen ME, Feldman J, Coleman WW, Edmonson LM, MacDonald KL, Osterholm MT. 1996. A national outbreak of Salmonella enteritidis infections from ice cream. The Investigation Team. N. Engl. J. Med. 334:1281–1286 [DOI] [PubMed] [Google Scholar]
- 205.Le Hello S, Hendriksen RS, Doublet B, Fisher I, Nielsen EM, Whichard JM, Bouchrif B, Fashae K, Granier SA, Jourdan-Da Silva N, Cloeckaert A, Threlfall EJ, Angulo FJ, Aarestrup FM, Wain J, Weill FX. 2011. International spread of an epidemic population of Salmonella enterica serotype Kentucky ST198 resistant to ciprofloxacin. J. Infect. Dis. 204:675–684 [DOI] [PubMed] [Google Scholar]
- 206.Eswarappa SM, Janice J, Nagarajan AG, Balasundaram SV, Karnam G, Dixit NM, Chakravortty D. 2008. Differentially evolved genes of Salmonella pathogenicity islands: insights into the mechanism of host specificity in Salmonella. PLoS One 3:e3829. 10.1371/journal.pone.0003829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.US Department of Agriculture 2010. Overview of the United States dairy industry. US Department of Agriculture, National Agricultural Statistics Service, Washington, DC [Google Scholar]
- 208.Joerger RD, Sartori CA, Kniel KE. 2009. Comparison of genetic and physiological properties of Salmonella enterica isolates from chickens reveals one major difference between serovar Kentucky and other serovars: response to acid. Foodborne Pathog. Dis. 6:503–512 [DOI] [PubMed] [Google Scholar]
- 209.Johnson TJ, Johnson SJ, Nolan LK. 2006. Complete DNA sequence of a ColBM plasmid from avian pathogenic Escherichia coli suggests that it evolved from closely related ColV virulence plasmids. J. Bacteriol. 188:5975–5983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.US Department of Agriculture 1997. The national poultry improvement plan and auxiliary provisions. US Department of Agriculture, Animal and Plant Health Inspection Service, Washington, DC [Google Scholar]
- 211.Marrero-Ortiz R, Han J, Lynne AM, David DE, Stemper ME, Farmer D, Burkhardt W, III, Nayak R, Foley SL. 2012. Genetic characterization of antimicrobial resistance in Salmonella enterica serovars isolated from dairy cattle in Wisconsin. Food Res. Int. 45:962–967 [Google Scholar]
- 212.Melendez SN, Hanning I, Han J, Nayak R, Clement AR, Wooming A, Hererra P, Jones FT, Foley SL, Ricke SC. 2010. Salmonella enterica isolates from pasture-raised poultry exhibit antimicrobial resistance and class I integrons. J. Appl. Microbiol. 109:1957–1966 [DOI] [PubMed] [Google Scholar]
- 213.Van Kessel JA, Karns JS, Wolfgang DR, Hovingh E, Schukken YH. 2012. Dynamics of Salmonella serotype shifts in an endemically infected dairy herd. Foodborne Pathog. Dis. 9:319–324 [DOI] [PubMed] [Google Scholar]
- 214.Van Kessel JA, Karns JS, Lombard JE, Kopral CA. 2011. Prevalence of Salmonella enterica, Listeria monocytogenes, and Escherichia coli virulence factors in bulk tank milk and in-line filters from U.S. dairies. J. Food Prot. 74:759–768 [DOI] [PubMed] [Google Scholar]
- 215.Dominguez M, Jourdan-Da Silva N, Vaillant V, Pihier N, Kermin C, Weill FX, Delmas G, Kerouanton A, Brisabois A, de Valk H. 2009. Outbreak of Salmonella enterica serotype Montevideo infections in France linked to consumption of cheese made from raw milk. Foodborne Pathog. Dis. 6:121–128 [DOI] [PubMed] [Google Scholar]
- 216.Centers for Disease Control and Prevention 2007. Salmonella Typhimurium infection associated with raw milk and cheese consumption—Pennsylvania, 2007. MMWR Morb. Mortal. Wkly. Rep. 56:1161–1164 [PubMed] [Google Scholar]
- 217.Mazurek J, Salehi E, Propes D, Holt J, Bannerman T, Nicholson LM, Bundesen M, Duffy R, Moolenaar RL. 2004. A multistate outbreak of Salmonella enterica serotype Typhimurium infection linked to raw milk consumption—Ohio, 2003. J. Food Prot. 67:2165–2170 [DOI] [PubMed] [Google Scholar]
- 218.Kaldhone P, Nayak R, Lynne AM, David DE, McDermott PF, Logue CM, Foley SL. 2008. Characterization of Salmonella enterica serovar Heidelberg from turkey-associated sources. Appl. Environ. Microbiol. 74:5038–5046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Lynne AM, Kaldhone P, David D, White DG, Foley SL. 2009. Characterization of antimicrobial resistance in Salmonella enterica serotype Heidelberg isolated from food animals. Foodborne Pathog. Dis. 6:207–215 [DOI] [PubMed] [Google Scholar]
- 220.Didelot X, Bowden R, Street T, Golubchik T, Spencer C, McVean G, Sangal V, Anjum MF, Achtman M, Falush D, Donnelly P. 2011. Recombination and population structure in Salmonella enterica. PLoS Genet. 7:e1002191. 10.1371/journal.pgen.1002191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Johnson TJ, Siek KE, Johnson SJ, Nolan LK. 2006. DNA sequence of a ColV plasmid and prevalence of selected plasmid-encoded virulence genes among avian Escherichia coli strains. J. Bacteriol. 188:745–758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Johnson TJ, Lang KL. 2012. IncA/C plasmids: an emerging threat to human and animal health? Mob. Genet. Elements 2:55–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Brenner FW, Villar RG, Angulo FJ, Tauxe R, Swaminathan B. 2000. Salmonella nomenclature. J. Clin. Microbiol. 38:2465–2467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Porwollik S, Boyd EF, Choy C, Cheng P, Florea L, Proctor E, McClelland M. 2004. Characterization of Salmonella enterica subspecies I genovars by use of microarrays. J. Bacteriol. 186:5883–5898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Porwollik S, Santiviago CA, Cheng P, Florea L, Jackson S, McClelland M. 2005. Differences in gene content between Salmonella enterica serovar Enteritidis isolates and comparison to closely related serovars Gallinarum and Dublin. J. Bacteriol. 187:6545–6555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Li J, Smith NH, Nelson K, Crichton PB, Old DC, Whittam TS, Selander RK. 1993. Evolutionary origin and radiation of the avian-adapted non-motile salmonellae. J. Med. Microbiol. 38:129–139 [DOI] [PubMed] [Google Scholar]
- 227.Olsen JE, Skov MN, Christensen JP, Bisgaard M. 1996. Genomic lineage of Salmonella enterica serotype Gallinarum. J. Med. Microbiol. 45:413–418 [DOI] [PubMed] [Google Scholar]
- 228.Richarme G, el Yaagoubi A, Kohiyama M. 1993. The MglA component of the binding protein-dependent galactose transport system of Salmonella typhimurium is a galactose-stimulated ATPase. J. Biol. Chem. 268:9473–9477 [PubMed] [Google Scholar]
- 229.Zhang Y, Franco M, Ducret A, Mignot T. 2010. A bacterial Ras-like small GTP-binding protein and its cognate GAP establish a dynamic spatial polarity axis to control directed motility. PLoS Biol. 8:e1000430. 10.1371/journal.pbio.1000430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Nano FE, Schmerk C. 2007. The Francisella pathogenicity island. Ann. N. Y. Acad. Sci. 1105:122–137 [DOI] [PubMed] [Google Scholar]
- 231.Mauriello EM, Mouhamar F, Nan B, Ducret A, Dai D, Zusman DR, Mignot T. 2010. Bacterial motility complexes require the actin-like protein, MreB and the Ras homologue, MglA. EMBO J. 29:315–326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Kingsley RA, van Amsterdam K, Kramer N, Baumler AJ. 2000. The shdA gene is restricted to serotypes of Salmonella enterica subspecies I and contributes to efficient and prolonged fecal shedding. Infect. Immun. 68:2720–2727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Kingsley RA, Abi Ghanem D, Puebla-Osorio N, Keestra AM, Berghman L, Baumler AJ. 2004. Fibronectin binding to the Salmonella enterica serotype Typhimurium ShdA autotransporter protein is inhibited by a monoclonal antibody recognizing the A3 repeat. J. Bacteriol. 186:4931–4939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Wain J, House D, Parkhill J, Parry C, Dougan G. 2002. Unlocking the genome of the human typhoid bacillus. Lancet Infect. Dis. 2:163–170 [DOI] [PubMed] [Google Scholar]
- 235.Edwards RA, Olsen GJ, Maloy SR. 2002. Comparative genomics of closely related salmonellae. Trends Microbiol. 10:94–99 [DOI] [PubMed] [Google Scholar]
- 236.Eswarappa SM, Janice J, Balasundaram SV, Dixit NM, Chakravortty D. 2009. Host-specificity of Salmonella enterica serovar Gallinarum: insights from comparative genomics. Infect. Genet. Evol. 9:468–473 [DOI] [PubMed] [Google Scholar]
- 237.Araya DV, Quiroz TS, Tobar HE, Lizana RJ, Quezada CP, Santiviago CA, Riedel CA, Kalergis AM, Bueno SM. 2010. Deletion of a prophage-like element causes attenuation of Salmonella enterica serovar Enteritidis and promotes protective immunity. Vaccine 28:5458–5466 [DOI] [PubMed] [Google Scholar]
- 238.Schleker S, Sun J, Raghavan B, Srnec M, Muller N, Koepfinger M, Murthy L, Zhao Z, Klein-Seetharaman J. 2012. The current Salmonella-host interactome. Proteomics Clin. Appl. 6:117–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Desin TS, Mickael CS, Lam PK, Potter AA, Koster W. 2010. Protection of epithelial cells from Salmonella enterica serovar Enteritidis invasion by antibodies against the SPI-1 type III secretion system. Can. J. Microbiol. 56:522–526 [DOI] [PubMed] [Google Scholar]
- 240.Kaiser P. 2010. Advances in avian immunology—prospects for disease control: a review. Avian Pathol. 39:309–324 [DOI] [PubMed] [Google Scholar]
- 241.Barrow PA, Huggins MB, Lovell MA. 1994. Host specificity of Salmonella infection in chickens and mice is expressed in vivo primarily at the level of the reticuloendothelial system. Infect. Immun. 62:4602–4610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Salcedo SP, Holden DW. 2005. Bacterial interactions with the eukaryotic secretory pathway. Curr. Opin. Microbiol. 8:92–98 [DOI] [PubMed] [Google Scholar]
- 243.van der Heijden J, Finlay BB. 2012. Type III effector-mediated processes in Salmonella infection. Future Microbiol. 7:685–703 [DOI] [PubMed] [Google Scholar]
- 244.Methner U, Haase A, Berndt A, Martin G, Nagy B, Barrow PA. 2011. Exploitation of intestinal colonization-inhibition between Salmonella organisms for live vaccines in poultry: potential and limitations. Zoonoses Public Health 58:540–548 [DOI] [PubMed] [Google Scholar]
- 245.He H, Genovese KJ, Swaggerty CL, Nisbet DJ, Kogut MH. 2012. A comparative study on invasion, survival, modulation of oxidative burst, and nitric oxide responses of macrophages (HD11), and systemic infection in chickens by prevalent poultry Salmonella serovars. Foodborne Pathog. Dis. 9:1104–1110 [DOI] [PubMed] [Google Scholar]
- 246.Shah DH, Zhou X, Addwebi T, Davis MA, Orfe L, Call DR, Guard J, Besser TE. 2011. Cell invasion of poultry-associated Salmonella enterica serovar Enteritidis isolates is associated with pathogenicity, motility and proteins secreted by the type III secretion system. Microbiology 157:1428–1445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Shah DH, Zhou X, Addwebi T, Davis MA, Call DR. 2011. In vitro and in vivo pathogenicity of Salmonella Enteritidis clinical strains isolated from North America. Arch. Microbiol. 193:811–821 [DOI] [PubMed] [Google Scholar]
- 248.St Louis ME, Morse DL, Potter ME, DeMelfi TM, Guzewich JJ, Tauxe RV, Blake PA. 1988. The emergence of grade A eggs as a major source of Salmonella enteritidis infections. New implications for the control of salmonellosis. JAMA 259:2103–2107 [PubMed] [Google Scholar]
- 249.Guard J, Gast RK, Guraya R. 2010. Colonization of avian reproductive-tract tissues by variant subpopulations of Salmonella Enteritidis. Avian Dis. 54:857–861 [DOI] [PubMed] [Google Scholar]
- 250.Ricke SC, Jones DR, Gast RK. Eggs and egg products. In Doores S, Tortorello ML. (ed), Compendium of methods for the microbiological examinations of foods, 5th ed, in press American Public Health Association, Washington, DC [Google Scholar]
- 251.Golden NJ, Marks HH, Coleman ME, Schroeder CM, Bauer NE, Jr, Schlosser WD. 2008. Review of induced molting by feed removal and contamination of eggs with Salmonella enterica serovar Enteritidis. Vet. Microbiol. 131:215–228 [DOI] [PubMed] [Google Scholar]
- 252.Gantois I, Ducatelle R, Pasmans F, Haesebrouck F, Van Immerseel F. 2009. The Salmonella Enteritidis lipopolysaccharide biosynthesis gene rfbH is required for survival in egg albumen. Zoonoses Public Health 56:145–149 [DOI] [PubMed] [Google Scholar]
- 253.Howard ZR, O'Bryan CA, Crandall PG, Ricke SC. 2012. Salmonella Enteritidis in shell eggs: current issues and prospects for control. Food Res. Int. 45:755–764 [Google Scholar]
- 254.Barrow PA, Jones MA, Smith AL, Wigley P. 2013. The long view: Salmonella—the last forty years. Avian Pathol. 41:413–420 [DOI] [PubMed] [Google Scholar]
- 255.Ricke SC. 2003. The gastrointestinal tract ecology of Salmonella Enteritidis colonization in molting hens. Poult. Sci. 82:1003–1007 [DOI] [PubMed] [Google Scholar]
- 256.Ricke SC, Dunkley CS, Durant JA. 2013. A review on development of novel strategies for controlling Salmonella Enteritidis colonization in laying hens: fiber-based molt diets. Poult. Sci. 92:502–525 [DOI] [PubMed] [Google Scholar]
- 257.Botteldoorn N, Van Coillie E, Goris J, Werbrouck H, Piessens V, Godard C, Scheldeman P, Herman L, Heyndrickx M. 2010. Limited genetic diversity and gene expression differences between egg- and non-egg-related Salmonella Enteritidis strains. Zoonoses Public Health 57:345–357 [DOI] [PubMed] [Google Scholar]
- 258.Gast RK, Beard CW. 1990. Isolation of Salmonella enteritidis from internal organs of experimentally infected hens. Avian Dis. 34:991–993 [PubMed] [Google Scholar]
- 259.De Buck J, Van Immerseel F, Meulemans G, Haesebrouck F, Ducatelle R. 2003. Adhesion of Salmonella enterica serotype Enteritidis isolates to chicken isthmal glandular secretions. Vet. Microbiol. 93:223–233 [DOI] [PubMed] [Google Scholar]
- 260.Keller LH, Benson CE, Krotec K, Eckroade RJ. 1995. Salmonella enteritidis colonization of the reproductive tract and forming and freshly laid eggs of chickens. Infect. Immun. 63:2443–2449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Keller LH, Schifferli DM, Benson CE, Aslam S, Eckroade RJ. 1997. Invasion of chicken reproductive tissues and forming eggs is not unique to Salmonella enteritidis. Avian Dis. 41:535–539 [PubMed] [Google Scholar]
- 262.Gantois I, Ducatelle R, Pasmans F, Haesebrouck F, Gast R, Humphrey TJ, Van Immerseel F. 2009. Mechanisms of egg contamination by Salmonella Enteritidis. FEMS Microbiol. Rev. 33:718–738 [DOI] [PubMed] [Google Scholar]
- 263.Guard-Petter J. 2001. The chicken, the egg and Salmonella enteritidis. Environ. Microbiol. 3:421–430 [DOI] [PubMed] [Google Scholar]
- 264.Bohez L, Dewulf J, Ducatelle R, Pasmans F, Haesebrouck F, Van Immerseel F. 2008. The effect of oral administration of a homologous hilA mutant strain on the long-term colonization and transmission of Salmonella Enteritidis in broiler chickens. Vaccine 26:372–378 [DOI] [PubMed] [Google Scholar]
- 265.Van Immerseel F, De Buck J, Pasmans F, Velge P, Bottreau E, Fievez V, Haesebrouck F, Ducatelle R. 2003. Invasion of Salmonella enteritidis in avian intestinal epithelial cells in vitro is influenced by short-chain fatty acids. Int. J. Food Microbiol. 85:237–248 [DOI] [PubMed] [Google Scholar]
- 266.Raspoet R, Gantois I, Devloo R, Martel A, Haesebrouck F, Pasmans F, Ducatelle R, Van Immerseel F. 2011. Salmonella Enteritidis universal stress protein (usp) gene expression is stimulated by egg white and supports oviduct colonization and egg contamination in laying hens. Vet. Microbiol. 153:186–190 [DOI] [PubMed] [Google Scholar]
- 267.De Vylder J, Raspoet R, Dewulf J, Haesebrouck F, Ducatelle R, Van Immerseel F. 2013. Salmonella Enteritidis is superior in egg white survival compared with other Salmonella serotypes. Poult. Sci. 92:842–845 [DOI] [PubMed] [Google Scholar]
- 268.Bohez L, Ducatelle R, Pasmans F, Botteldoorn N, Haesebrouck F, Van Immerseel F. 2006. Salmonella enterica serovar Enteritidis colonization of the chicken caecum requires the HilA regulatory protein. Vet. Microbiol. 116:202–210 [DOI] [PubMed] [Google Scholar]
- 269.Bohez L, Ducatelle R, Pasmans F, Haesebrouck F, Van Immerseel F. 2007. Long-term colonisation-inhibition studies to protect broilers against colonisation with Salmonella Enteritidis, using Salmonella pathogenicity island 1 and 2 mutants. Vaccine 25:4235–4243 [DOI] [PubMed] [Google Scholar]
- 270.Dunkley KD, McReynolds JL, Hume ME, Dunkley CS, Callaway TR, Kubena LF, Nisbet DJ, Ricke SC. 2007. Molting in Salmonella Enteritidis-challenged laying hens fed alfalfa crumble. II. Fermentation and microbial ecology response. Poult. Sci. 86:2101–2109 [DOI] [PubMed] [Google Scholar]
- 271.Rychlik I, Gregorova D, Hradecka H. 2006. Distribution and function of plasmids in Salmonella enterica. Vet. Microbiol. 112:1–10 [DOI] [PubMed] [Google Scholar]
- 272.Desin TS, Lam PK, Koch B, Mickael C, Berberov E, Wisner AL, Townsend HG, Potter AA, Koster W. 2009. Salmonella enterica serovar Enteritidis pathogenicity island 1 is not essential for but facilitates rapid systemic spread in chickens. Infect. Immun. 77:2866–2875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Murray RA, Lee CA. 2000. Invasion genes are not required for Salmonella enterica serovar Typhimurium to breach the intestinal epithelium: evidence that Salmonella pathogenicity island 1 has alternative functions during infection. Infect. Immun. 68:5050–5055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Clark L, Perrett CA, Malt L, Harward C, Humphrey S, Jepson KA, Martinez-Argudo I, Carney LJ, La Ragione RM, Humphrey TJ, Jepson MA. 2011. Differences in Salmonella enterica serovar Typhimurium strain invasiveness are associated with heterogeneity in SPI-1 gene expression. Microbiology 157:2072–2083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Silva CA, Blondel CJ, Quezada CP, Porwollik S, Andrews-Polymenis HL, Toro CS, Zaldivar M, Contreras I, McClelland M, Santiviago CA. 2012. Infection of mice by Salmonella enterica serovar Enteritidis involves additional genes that are absent in the genome of serovar Typhimurium. Infect. Immun. 80:839–849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Shah DH, Zhou X, Kim HY, Call DR, Guard J. 2012. Transposon mutagenesis of Salmonella enterica serovar Enteritidis identifies genes that contribute to invasiveness in human and chicken cells and survival in egg albumen. Infect. Immun. 80:4203–4215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Shah DH, Casavant C, Hawley Q, Addwebi T, Call DR, Guard J. 2012. Salmonella Enteritidis strains from poultry exhibit differential responses to acid stress, oxidative stress, and survival in the egg albumen. Foodborne Pathog. Dis. 9:258–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Knodler LA, Steele-Mortimer O. 2003. Taking possession: biogenesis of the Salmonella-containing vacuole. Traffic 4:587–599 [DOI] [PubMed] [Google Scholar]
- 279.Beal RK, Wigley P, Powers C, Hulme SD, Barrow PA, Smith AL. 2004. Age at primary infection with Salmonella enterica serovar Typhimurium in the chicken influences persistence of infection and subsequent immunity to re-challenge. Vet. Immunol. Immunopathol. 100:151–164 [DOI] [PubMed] [Google Scholar]
- 280.Kaiser P, Rothwell L, Galyov EE, Barrow PA, Burnside J, Wigley P. 2000. Differential cytokine expression in avian cells in response to invasion by Salmonella typhimurium, Salmonella enteritidis and Salmonella gallinarum. Microbiology 146:3217–3226 [DOI] [PubMed] [Google Scholar]
- 281.Tsolis RM, Xavier MN, Santos RL, Baumler AJ. 2011. How to become a top model: impact of animal experimentation on human Salmonella disease research. Infect. Immun. 79:1806–1814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.De Keersmaecker SC, Thijs IM, Vanderleyden J, Marchal K. 2006. Integration of omics data: how well does it work for bacteria? Mol. Microbiol. 62:1239–1250 [DOI] [PubMed] [Google Scholar]
- 283.Calenge F, Beaumont C. 2012. Toward integrative genomics study of genetic resistance to Salmonella and Campylobacter intestinal colonization in fowl. Front. Genet. 3:261. 10.3389/fgene.2012.00261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Lee SJ, Liang L, Juarez S, Nanton MR, Gondwe EN, Msefula CL, Kayala MA, Necchi F, Heath JN, Hart P, Tsolis RM, Heyderman RS, MacLennan CA, Felgner PL, Davies DH, McSorley SJ. 2012. Identification of a common immune signature in murine and human systemic salmonellosis. Proc. Natl. Acad. Sci. U. S. A. 109:4998–5003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Thiele I, Hyduke DR, Steeb B, Fankam G, Allen DK, Bazzani S, Charusanti P, Chen FC, Fleming RM, Hsiung CA, De Keersmaecker SC, Liao YC, Marchal K, Mo ML, Ozdemir E, Raghunathan A, Reed JL, Shin SI, Sigurbjornsdottir S, Steinmann J, Sudarsan S, Swainston N, Thijs IM, Zengler K, Palsson BO, Adkins JN, Bumann D. 2011. A community effort towards a knowledge-base and mathematical model of the human pathogen Salmonella Typhimurium LT2. BMC Syst. Biol. 5:8. 10.1186/1752-0509-5-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Gast RK, Guraya R, Guard-Bouldin J, Holt PS, Moore RW. 2007. Colonization of specific regions of the reproductive tract and deposition at different locations inside eggs laid by hens infected with Salmonella enteritidis or Salmonella heidelberg. Avian Dis. 51:40–44 [DOI] [PubMed] [Google Scholar]
- 287.Jones FT. 2011. A review of practical Salmonella control measures in animal feed. J. Appl. Poult. Res. 20:102–113 [Google Scholar]
- 288.Park SY, Woodward CL, Kubena LF, Nisbet DJ, Birkhold SG, Ricke SC. 2008. Environmental dissemination of foodborne Salmonella in preharvest poultry production: reservoirs, critical factors and research strategies. Crit. Rev. Environ. Sci. Technol. 38:73–111 [Google Scholar]
- 289.Sirsat SA, Muthaiyan A, Ricke SC. 2009. Antimicrobials for pathogen reduction in organic and natural poultry production. J. Appl. Poult. Res. 18:379–388 [Google Scholar]
- 290.Hur J, Jawale C, Lee JW. 2013. Antimicrobial resistance of Salmonella isolated from food animals: a review. Food Res. Int. 45:819–830 [Google Scholar]
- 291.Moretrø T, Heir E, Nesse LL, Vestby LK, Langsrud S. 2012. Control of Salmonella in food related environments by chemical disinfection. Food Res. Int. 45:532–544 [Google Scholar]
- 292.Ahmer BM, Gunn JS. 2011. Interaction of Salmonella spp. with the intestinal microbiota. Front. Microbiol. 2:101. 10.3389/fmicb.2011.00101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Farr SB, Kogoma T. 1991. Oxidative stress responses in Escherichia coli and Salmonella typhimurium. Microbiol. Rev. 55:561–585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Evans MR, Fink RC, Vazquez-Torres A, Porwollik S, Jones-Carson J, McClelland M, Hassan HM. 2011. Analysis of the ArcA regulon in anaerobically grown Salmonella enterica sv. Typhimurium. BMC Microbiol. 11:58. 10.1186/1471-2180-11-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Troxell B, Fink RC, Porwollik S, McClelland M, Hassan HM. 2011. The Fur regulon in anaerobically grown Salmonella enterica sv. Typhimurium: identification of new Fur targets. BMC Microbiol. 11:236. 10.1186/1471-2180-11-236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Foster JW, Spector MP. 1995. How Salmonella survive against the odds. Annu. Rev. Microbiol. 49:145–174 [DOI] [PubMed] [Google Scholar]
- 297.Wooldridge KG, Williams PH. 1993. Iron uptake mechanisms of pathogenic bacteria. FEMS Microbiol. Rev. 12:325–348 [DOI] [PubMed] [Google Scholar]
- 298.Foster JW. 1991. Salmonella acid shock proteins are required for the adaptive acid tolerance response. J. Bacteriol. 173:6896–6902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Spector MP. 1998. The starvation-stress response (SSR) of Salmonella. Adv. Microb. Physiol. 40:233–279 [DOI] [PubMed] [Google Scholar]
- 300.Smith JL. 2003. The role of gastric acid in preventing foodborne disease and how bacteria overcome acid conditions. J. Food Prot. 66:1292–1303 [DOI] [PubMed] [Google Scholar]
- 301.Bearson SMD, Bearson BL. 2010. Traversing the swine gastrointestinal tract: Salmonella survival and pathogenesis, p 35–48 In Ricke SC, Jones FT. (ed), Perspectives on food-safety issues of animal-derived foods. University of Arkansas Press, Fayetteville, AR [Google Scholar]
- 302.Korver DR. 2006. Overview of the immune dynamics of the digestive system. J. Appl. Poult. Res. 15:123–135 [Google Scholar]
- 303.Kosiewicz MM, Zirnheld AL, Alard P. 2011. Gut microbiota, immunity, and disease: a complex relationship. Front. Microbiol. 2:180. 10.3389/fmicb.2011.00180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Kelly D, Conway S, Aminov R. 2005. Commensal gut bacteria: mechanisms of immune modulation. Trends Immunol. 26:326–333 [DOI] [PubMed] [Google Scholar]
- 305.Kelly D, Mulder IE. 2012. Microbiome and immunological interactions. Nutr. Rev. 70:S18–S30. 10.1111/j.1753-4887.2012.00498.x [DOI] [PubMed] [Google Scholar]
- 306.Hallstrom K, McCormick BA. 2011. Salmonella interaction with and passage through the intestinal mucosa: through the lens of the organism. Front. Microbiol. 2:88. 10.3389/fmicb.2011.00088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Reading NC, Kasper DL. 2011. The starting lineup: key microbial players in intestinal immunity and homeostasis. Front. Microbiol. 2:148. 10.3389/fmicb.2011.00148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Cherrington CA, Hinton M, Mead GC, Chopra I. 1991. Organic acids: chemistry, antibacterial activity and practical applications. Adv. Microb. Physiol. 32:87–108 [DOI] [PubMed] [Google Scholar]
- 309.Ricke SC, Koo OK, Keeton JT. 2013. Fermented meat, poultry, and fish products, p 857–880 In Doyle MP, Buchanan RL. (ed), Food microbiology: fundamentals and frontiers, 4th ed. ASM Press, Washington, DC [Google Scholar]
- 310.Davidson PM, Taylor TM, Schmidt SE. 2013. Chemical preservatives and natural antimicrobial compounds, p 765–801 In Doyle MP, Buchanan RL. (ed), Food microbiology: fundamentals and frontiers, 4th ed. ASM Press, Washington, DC [Google Scholar]
- 311.Russell JB, Diez-Gonzalez F. 1998. The effects of fermentation acids on bacterial growth. Adv. Microb. Physiol. 39:205–234 [DOI] [PubMed] [Google Scholar]
- 312.Hirshfield IN, Terzulli S, O'Byrne C. 2003. Weak organic acids: a panoply of effects on bacteria. Sci. Prog. 86:245–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Van Immerseel F, Russell JB, Flythe MD, Gantois I, Timbermont L, Pasmans F, Haesebrouck F, Ducatelle R. 2006. The use of organic acids to combat Salmonella in poultry: a mechanistic explanation of the efficacy. Avian Pathol. 35:182–188 [DOI] [PubMed] [Google Scholar]
- 314.Russell JB. 1992. Another explanation for the toxicity of fermentation acids at low pH—anion accumulation versus uncoupling. J. Appl. Bacteriol. 73:363–370 [Google Scholar]
- 315.Ricke SC. 2003. Perspectives on the use of organic acids and short chain fatty acids as antimicrobials. Poult. Sci. 82:632–639 [DOI] [PubMed] [Google Scholar]
- 316.Maciorowski KG, Jones FT, Pillai SD, Ricke SC. 2004. Incidence and control of food-borne Salmonella spp. in poultry feeds—a review. Worlds Poult. Sci. J. 60:446–457 [Google Scholar]
- 317.Jones FT, Ricke SC. 2003. Observations on the history of the development of antimicrobials and their use in poultry feeds. Poult. Sci. 82:613–617 [DOI] [PubMed] [Google Scholar]
- 318.Hungate RE. 1966. The rumen and its microbes. Academic Press, Inc, New York, NY [Google Scholar]
- 319.Annison EF, Hill KJ, Kenworthy R. 1968. Volatile fatty acids in the digestive tract of the fowl. Br. J. Nutr. 22:207–216 [DOI] [PubMed] [Google Scholar]
- 320.Cummings JH, Macfarlane GT. 1991. The control and consequences of bacterial fermentation in the human colon. J. Appl. Bacteriol. 70:443–459 [DOI] [PubMed] [Google Scholar]
- 321.Cummings JH, Pomare EW, Branch WJ, Naylor CP, Macfarlane GT. 1987. Short chain fatty acids in human large intestine, portal, hepatic and venous blood. Gut 28:1221–1227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Goepfert JM, Hicks R. 1969. Effect of volatile fatty acids on Salmonella typhimurium. J. Bacteriol. 97:956–958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Khan M, Katamay M. 1969. Antagonistic effect of fatty acids against Salmonella in meat and bone meal. Appl. Microbiol. 17:402–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Eklund T. 1983. The antimicrobial effect of dissociated and undissociated sorbic acid at different pH levels. J. Appl. Bacteriol. 54:383–389 [DOI] [PubMed] [Google Scholar]
- 325.McHan F, Shotts EB. 1993. Effect of short-chain fatty acids on the growth of Salmonella typhimurium in an in vitro system. Avian Dis. 37:396–398 [PubMed] [Google Scholar]
- 326.Leyer GJ, Johnson EA. 1992. Acid adaptation promotes survival of Salmonella spp. in cheese. Appl. Environ. Microbiol. 58:2075–2080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Baik HS, Bearson S, Dunbar S, Foster JW. 1996. The acid tolerance response of Salmonella typhimurium provides protection against organic acids. Microbiology 142:3195–3200 [DOI] [PubMed] [Google Scholar]
- 328.Kwon YM, Ricke SC. 1998. Induction of acid resistance of Salmonella typhimurium by exposure to short-chain fatty acids. Appl. Environ. Microbiol. 64:3458–3463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Calhoun LN, Kwon YM. 2010. The effect of long-term propionate adaptation on the stress resistance of Salmonella Enteritidis. J. Appl. Microbiol. 109:1294–1300 [DOI] [PubMed] [Google Scholar]
- 330.Dunkley KD, Callaway TR, O'Bryan C, Kundinger MM, Dunkley CS, Anderson RC, Nisbet DJ, Crandall PG, Ricke SC. 2009. Cell yields and fermentation responses of a Salmonella Typhimurium poultry isolate at different dilution rates in an anaerobic steady state continuous culture. Antonie Van Leeuwenhoek 96:537–544 [DOI] [PubMed] [Google Scholar]
- 331.Dunkley KD, Callaway TR, Chalova VI, Anderson RC, Kundinger MM, Dunkley CS, Nisbet DJ, Ricke SC. 2008. Glucose yields and genetic responses in a poultry isolate of Salmonella Typhimurium in an anaerobic continuous culture during shifts in pH. Anaerobe 14:35–42 [DOI] [PubMed] [Google Scholar]
- 332.Horswill AR, Escalante-Semerena JC. 1999. Salmonella typhimurium LT2 catabolizes propionate via the 2-methylcitric acid cycle. J. Bacteriol. 181:5615–5623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Horswill AR, Dudding AR, Escalante-Semerena JC. 2001. Studies of propionate toxicity in Salmonella enterica identify 2-methylcitrate as a potent inhibitor of cell growth. J. Biol. Chem. 276:19094–19101 [DOI] [PubMed] [Google Scholar]
- 334.Rocco CJ, Escalante-Semerena JC. 2010. In Salmonella enterica, 2-methylcitrate blocks gluconeogenesis. J. Bacteriol. 192:771–778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Kwon YM, Park SY, Birkhold SG, Ricke SC. 2000. Induction of resistance of Salmonella typhimurium to environmental stresses by exposure to short-chain fatty acids. J. Food Sci. 65:1037–1040 [Google Scholar]
- 336.Greenacre EJ, Brocklehurst TF. 2006. The acetic acid tolerance response induces cross-protection to salt stress in Salmonella typhimurium. Int. J. Food Microbiol. 112:62–65 [DOI] [PubMed] [Google Scholar]
- 337.Greenacre EJ, Lucchini S, Hinton JC, Brocklehurst TF. 2006. The lactic acid-induced acid tolerance response in Salmonella enterica serovar Typhimurium induces sensitivity to hydrogen peroxide. Appl. Environ. Microbiol. 72:5623–5625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Milillo SR, Martin E, Muthaiyan A, Ricke SC. 2011. Immediate reduction of Salmonella enterica serotype Typhimurium viability via membrane destabilization following exposure to multiple-hurdle treatments with heated, acidified organic acid salt solutions. Appl. Environ. Microbiol. 77:3765–3772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Milillo SR, Ricke SC. 2010. Synergistic reduction of Salmonella in a model raw chicken media using a combined thermal and acidified organic acid salt intervention treatment. J. Food Sci. 75:M121–M125. 10.1111/j.1750-3841.2009.01510.x [DOI] [PubMed] [Google Scholar]
- 340.Joerger RD, Sartori C, Frye JG, Turpin JB, Schmidt C, McClelland M, Porwollik S. 2012. Gene expression analysis of Salmonella enterica Enteritidis Nal(R) and Salmonella enterica Kentucky 3795 exposed to HCl and acetic acid in rich medium. Foodborne Pathog. Dis. 9:331–337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Durant JA, Lowry VK, Nisbet DJ, Stanker LH, Corrier DE, Ricke SC. 1999. Short-chain fatty acids affect cell-association and invasion of HEp-2 cells by Salmonella typhimurium. J. Environ. Sci. Health B 34:1083–1099 [DOI] [PubMed] [Google Scholar]
- 342.Durant JA, Lowry VK, Nisbet DJ, Stanker LH, Corrier DE, Ricke SC. 2000. Late logarithmic Salmonella typhimurium HEp-2 cell-association and invasion response to short chain volatile fatty acid addition. J. Food Saf. 20:1–11 [Google Scholar]
- 343.Durant JA, Lowry VK, Nisbet DJ, Stanker LH, Corrier DE, Ricke SC. 2000. Short-chain fatty acids alter HEp-2 cell association and invasion by stationary growth phase Salmonella typhimurium. J. Food Sci. 65:1206–1209 [DOI] [PubMed] [Google Scholar]
- 344.Van Immerseel F, De Buck J, De Smet I, Pasmans F, Haesebrouck F, Ducatelle R. 2004. Interactions of butyric acid- and acetic acid-treated Salmonella with chicken primary cecal epithelial cells in vitro. Avian Dis. 48:384–391 [DOI] [PubMed] [Google Scholar]
- 345.Gantois I, Ducatelle R, Pasmans F, Haesebrouck F, Van Immerseel F. 2008. Salmonella enterica serovar Enteritidis genes induced during oviduct colonization and egg contamination in laying hens. Appl. Environ. Microbiol. 74:6616–6622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Durant JA, Corrier DE, Ricke SC. 2000. Short-chain volatile fatty acids modulate the expression of the hilA and invF genes of Salmonella typhimurium. J. Food Prot. 63:573–578 [DOI] [PubMed] [Google Scholar]
- 347.Durant JA, Corrier DE, Stanker LH, Ricke SC. 2000. Expression of the hilA Salmonella typhimurium gene in a poultry Salm. enteritidis isolate in response to lactate and nutrients. J. Appl. Microbiol. 89:63–69 [DOI] [PubMed] [Google Scholar]
- 348.Lawhon SD, Maurer R, Suyemoto M, Altier C. 2002. Intestinal short-chain fatty acids alter Salmonella typhimurium invasion gene expression and virulence through BarA/SirA. Mol. Microbiol. 46:1451–1464 [DOI] [PubMed] [Google Scholar]
- 349.Huang Y, Suyemoto M, Garner CD, Cicconi KM, Altier C. 2008. Formate acts as a diffusible signal to induce Salmonella invasion. J. Bacteriol. 190:4233–4241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Gonzalez-Gil F, Le Bolloch A, Pendleton S, Zhang N, Wallis A, Hanning I. 2012. Expression of hilA in response to mild acid stress in Salmonella enterica is serovar and strain dependent. J. Food Sci. 77:M292–M297. 10.1111/j.1750-3841.2012.02684.x [DOI] [PubMed] [Google Scholar]
- 351.Sirsat SA, Burkholder KM, Muthaiyan A, Dowd SE, Bhunia AK, Ricke SC. 2011. Effect of sublethal heat stress on Salmonella Typhimurium virulence. J. Appl. Microbiol. 110:813–822 [DOI] [PubMed] [Google Scholar]
- 352.Hungate RE. 1975. The rumen microbial ecosystem. Annu. Rev. Ecol. Syst. 6:39–66 [Google Scholar]
- 353.Macfarlane GT, Macfarlane S. 1997. Human colonic microbiota: ecology, physiology and metabolic potential of intestinal bacteria. Scand. J. Gastroenterol. Suppl. 222:3–9 [DOI] [PubMed] [Google Scholar]
- 354.Jósefiak D, Rutowski A, Martin SA. 2004. Carbohydrate fermentation in the avian ceca: a review. Anim. Feed Sci. Technol. 113:1–15 [Google Scholar]
- 355.Burr G, Ricke S, Gatlin D. 2005. Microbial ecology of the gastrointestinal tract of fish and the potential application of prebiotics and probiotics in finfish. J. World Aquacult. Soc. 36:425–436 [Google Scholar]
- 356.Muegge BD, Kuczynski J, Knights D, Clemente JC, Gonzalez A, Fontana L, Henrissat B, Knight R, Gordon JI. 2011. Diet drives convergence in gut microbiome functions across mammalian phylogeny and within humans. Science 332:970–974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Saengkerdsub S, Ricke SC. Ecology and characteristics of methanogenic archaea in animals and humans. Crit. Rev. Microbiol., in press [DOI] [PubMed] [Google Scholar]
- 358.Mead GC. 1989. Microbes of the avian cecum: types present and substrates utilized. J. Exp. Zool. Suppl. 3:48–54 [DOI] [PubMed] [Google Scholar]
- 359.Cahill MM. 1990. Bacterial flora of fishes: a review. Microb. Ecol. 19:21–41 [DOI] [PubMed] [Google Scholar]
- 360.Wolin MJ, Miller TL. 1983. Interactions of microbial populations in cellulose fermentation. Fed. Proc. 42:109–113 [PubMed] [Google Scholar]
- 361.Ricke SC, Martin SA, Nisbet DJ. 1996. Ecology, metabolism, and genetics of ruminal selenomonads. Crit. Rev. Microbiol. 22:27–56 [DOI] [PubMed] [Google Scholar]
- 362.Mackie RI. 2002. Mutualistic fermentative digestion in the gastrointestinal tract: diversity and evolution. Integr. Comp. Biol. 42:319–326 [DOI] [PubMed] [Google Scholar]
- 363.Weimer PJ, Russell JB, Muck RE. 2009. Lessons from the cow: what the ruminant animal can teach us about consolidated bioprocessing of cellulosic biomass. Bioresour. Technol. 100:5323–5331 [DOI] [PubMed] [Google Scholar]
- 364.Weimer PJ. 2002. Cellulose degradation by ruminal microorganisms. Crit. Rev. Biotechnol. 12:189–223 [Google Scholar]
- 365.Hespell RB, Bryant MP. 1979. Efficiency of rumen microbial growth: influence of some theoretical and experimental factors of YATP. J. Anim. Sci. 49:1640–1659 [DOI] [PubMed] [Google Scholar]
- 366.Hespell RB. 1979. Efficiency of growth by ruminal bacteria. Fed. Proc. 38:2707–2712 [PubMed] [Google Scholar]
- 367.Russell JB. 1984. Factors influencing competition and composition of the rumen bacterial flora, p 313–345 In Gilchrist FMC, Mackie RI. (ed), Herbivore nutrition in the subtropics and tropics. The Science Press, Craighall, South Africa [Google Scholar]
- 368.Demeyer D, Van Nevel C. 1986. Influence of substrate and microbial interaction on efficiency of rumen microbial growth. Reprod. Nutr. Dev. 26:161–179 [DOI] [PubMed] [Google Scholar]
- 369.Russell JB, Hespell RB. 1981. Microbial rumen fermentation. J. Dairy Sci. 64:1153–1169 [DOI] [PubMed] [Google Scholar]
- 370.Coleman ME, Dreesen DW, Wiegert RG. 1996. A simulation of microbial competition in the human colonic ecosystem. Appl. Environ. Microbiol. 62:3632–3639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Rohmer L, Hocquet D, Miller SI. 2011. Are pathogenic bacteria just looking for food? Metabolism and microbial pathogenesis. Trends Microbiol. 19:341–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Schmidt H, Hensel M. 2004. Pathogenicity islands in bacterial pathogenesis. Clin. Microbiol. Rev. 17:14–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Tannock GW. 1984. Effect of dietary and environmental stress on the gastrointestinal microbiota, p 517–539 In Hentges DJ. (ed), Human intestinal microflora and disease. Academic Press, Inc, New York, NY [Google Scholar]
- 374.Hashimoto T, Perlot T, Rehman A, Trichereau J, Ishiguro H, Paolino M, Sigl V, Hanada T, Hanada R, Lipinski S, Wild B, Camargo SM, Singer D, Richter A, Kuba K, Fukamizu A, Schreiber S, Clevers H, Verrey F, Rosenstiel P, Penninger JM. 2012. ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature 487:477–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Smith MI, Yatsunenko T, Manary MJ, Trehan I, Mkakosya R, Cheng J, Kau AL, Rich SS, Concannon P, Mychaleckyj JC, Liu J, Houpt E, Li JV, Holmes E, Nicholson J, Knights D, Ursell LK, Knight R, Gordon JI. 2013. Gut microbiomes of Malawian twin pairs discordant for kwashiorkor. Science 339:548–554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Alverdy J, Stern E. 1998. Effect of immunonutrition on virulence strategies in bacteria. Nutrition 14:580–584 [DOI] [PubMed] [Google Scholar]
- 377.Moran ET, Jr, Bilgili SF. 1990. Influence of feeding and fasting broilers prior to marketing on cecal access of orally administered Salmonella. J. Food Prot. 53:205–207 [DOI] [PubMed] [Google Scholar]
- 378.Humphrey TJ, Baskerville A, Whitehead A, Rowe B, Henley A. 1993. Influence of feeding patterns on the artificial infection of laying hens with Salmonella enteritidis phage type 4. Vet. Rec. 132:407–409 [DOI] [PubMed] [Google Scholar]
- 379.Ramirez GA, Sarlin LL, Caldwell DJ, Yezak CR, Jr, Hume ME, Corrier DE, Deloach JR, Hargis BM. 1997. Effect of feed withdrawal on the incidence of Salmonella in the crops and ceca of market age broiler chickens. Poult. Sci. 76:654–656 [DOI] [PubMed] [Google Scholar]
- 380.Corrier DE, Byrd JA, Hargis BM, Hume ME, Bailey RH, Stanker LH. 1999. Survival of Salmonella in the crop contents of market-age broilers during feed withdrawal. Avian Dis. 43:453–460 [PubMed] [Google Scholar]
- 381.Corrier DE, Byrd JA, Hargis BM, Hume ME, Bailey RH, Stanker LH. 1999. Presence of Salmonella in the crop and ceca of broiler chickens before and after preslaughter feed withdrawal. Poult. Sci. 78:45–49 [DOI] [PubMed] [Google Scholar]
- 382.Miller CP, Bohnhoff M. 1962. A study of experimental Salmonella infection in the mouse. J. Infect. Dis. 111:107–116 [DOI] [PubMed] [Google Scholar]
- 383.Brownlie LE, Grau FH. 1967. Effect of food intake on growth and survival of salmonellas and Escherichia coli in the bovine rumen. J. Gen. Microbiol. 46:125–134 [DOI] [PubMed] [Google Scholar]
- 384.Grau FH, Brownlie LE, Roberts EA. 1968. Effect of some preslaughter treatments on the Salmonella population in the bovine rumen and faeces. J. Appl. Bacteriol. 31:157–163 [DOI] [PubMed] [Google Scholar]
- 385.Grau FH, Brownlie LE, Smith MG. 1969. Effects of food intake on numbers of salmonellae and Escherichia coli in rumen and faeces of sheep. J. Appl. Bacteriol. 32:112–117 [DOI] [PubMed] [Google Scholar]
- 386.Bell DD. 2003. Historical and current molting practices in the U.S. table egg industry. Poult. Sci. 82:965–970 [DOI] [PubMed] [Google Scholar]
- 387.Park SY, Kim WK, Birkhold SG, Kubena LF, Nisbet DJ, Ricke SC. 2004. Induced moulting issues and alternative dietary strategies for the egg industry in the United States. Worlds Poultry Sci. J. 60:196–209 [Google Scholar]
- 388.Holt PS. 1999. Impact of induced molting on immunity and Salmonella enterica serovar Enteritidis infection in laying hens, p 367–375 In Saeed AM, Gast RK, Potter ME, Wall PG. (ed), Salmonella enterica serovar Enteritidis in humans and animals—epidemiology, pathogenesis, and control. Iowa State University Press, Ames, IA [Google Scholar]
- 389.Poppe C, McFadden KA, Demczuk WH. 1996. Drug resistance, plasmids, biotypes and susceptibility to bacteriophages of Salmonella isolated from poultry in Canada. Int. J. Food Microbiol. 30:325–344 [DOI] [PubMed] [Google Scholar]
- 390.Holt PS. 2003. Molting and Salmonella enterica serovar Enteritidis infection: the problem and some solutions. Poult. Sci. 82:1008–1010 [DOI] [PubMed] [Google Scholar]
- 391.Durant JA, Corrier DE, Byrd JA, Stanker LH, Ricke SC. 1999. Feed deprivation affects crop environment and modulates Salmonella enteritidis colonization and invasion of leghorn hens. Appl. Environ. Microbiol. 65:1919–1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Dunkley KD, McReynolds JL, Hume ME, Dunkley CS, Callaway TR, Kubena LF, Nisbet DJ, Ricke SC. 2007. Molting in Salmonella Enteritidis-challenged laying hens fed alfalfa crumbles. I. Salmonella Enteritidis colonization and virulence gene hilA response. Poult. Sci. 86:1633–1639 [DOI] [PubMed] [Google Scholar]
- 393.Corrier DE, Nisbet DJ, Hargis BM, Holt PS, DeLoach JR. 1997. Provision of lactose to molting hens enhances resistance to Salmonella enteritidis colonization. J. Food Prot. 60:10–15 [DOI] [PubMed] [Google Scholar]
- 394.Hume ME, Kubena LF, Edrington TS, Donskey CJ, Moore RW, Ricke SC, Nisbet DJ. 2003. Poultry digestive microflora biodiversity as indicated by denaturing gradient gel electrophoresis. Poult. Sci. 82:1100–1107 [DOI] [PubMed] [Google Scholar]
- 395.Ricke SC, Hume ME, Park SY, Moore RW, Birkhold SG, Kubena LF, Nisbet DJ. 2004. Denaturing gradient gel electrophoresis (DGGE) as a rapid method for assessing gastrointestinal tract microflora responses in laying hens fed similar zinc molt induction diets. J. Rapid Methods Autom. Microbiol. 12:69–81 [Google Scholar]
- 396.Saengkerdsub S, Kim WK, Andersen RC, Woodward CL, Nisbet DJ, Ricke SC. 2006. Effects of nitrocompounds and feedstuffs on in vitro methane production in chicken cecal contents and rumen fluid. Anaerobe 12:85–92 [DOI] [PubMed] [Google Scholar]
- 397.Dunkley KD, Dunkley CS, Njongmeta NL, Callaway TR, Hume ME, Kubena LF, Nisbet DJ, Ricke SC. 2007. Comparison of in vitro fermentation and molecular microbial profiles of high-fiber feed substrates incubated with chicken cecal inocula. Poult. Sci. 86:801–810 [DOI] [PubMed] [Google Scholar]
- 398.Donalson LM, Kim WK, Chalova VI, Herrera P, McReynolds JL, Gotcheva VG, Vidanovic D, Woodward CL, Kubena LF, Nisbet DJ, Ricke SC. 2008. In vitro fermentation response of laying hen cecal bacteria to combinations of fructooligosaccharide prebiotics with alfalfa or a layer ration. Poult. Sci. 87:1263–1275 [DOI] [PubMed] [Google Scholar]
- 399.Woodward CL, Kwon YM, Kubena LF, Byrd JA, Moore RW, Nisbet DJ, Ricke SC. 2005. Reduction of Salmonella enterica serovar Enteritidis colonization and invasion by an alfalfa diet during molt in Leghorn hens. Poult. Sci. 84:185–193 [DOI] [PubMed] [Google Scholar]
- 400.Seo KH, Holt PS, Gast RK. 2001. Comparison of Salmonella Enteritidis infection in hens molted via long-term feed withdrawal versus full-fed wheat middling. J. Food Prot. 64:1917–1921 [DOI] [PubMed] [Google Scholar]
- 401.Chiu CH, Chu C, Ou JT. 2000. Lack of evidence of an association between the carriage of virulence plasmid and the bacteremia of Salmonella typhimurium in humans. Microbiol. Immunol. 44:741–748 [DOI] [PubMed] [Google Scholar]
- 402.Hurley BP, McCormick BA. 2003. Translating tissue culture results into animal models: the case of Salmonella typhimurium. Trends Microbiol. 11:562–569 [DOI] [PubMed] [Google Scholar]
- 403.Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. 2011. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol. Biol. Evol. 28:2731–2739 [DOI] [PMC free article] [PubMed] [Google Scholar]