Abstract
Soil-transmitted helminth (STH) infections, and schistosomiasis and other trematodiases often have a high prevalence in developing countries. Here, we present updated information on the prevalence of these parasites in the Lao People's Democratic Republic (Lao PDR) in 2012, arising from the annual national helminthiasis survey. Fecal specimens were collected from 8,610 inhabitants of 12 provinces and one municipality (Bokeo, Houaphan, Luang Namtha, Luang Prabang, Oudomxay, and Phongsaly Provinces from northern Lao PDR; Bolikhamxay and Xieng Khouang Provinces and Vientiane Municipality from the central part of the country; and Attapeu, Champasak, Saravan, and Sekong Provinces from southern Lao PDR). The overall prevalence of three major STHs, Ascaris lumbricoides, Trichuris trichiura, and hookworms (Necator americanus and Ancylostoma duodenale) were 11.6%, 8.5%, and 25.0%, respectively. Prevalence of Schistosoma mekongi infection was 0.1%, and of miscellaneous trematodiases (including opisthorchiasis) was 14.0%. Clearly, the nationwide parasite control project is still necessary to reduce morbidity caused by helminthic diseases.
Three major soil-transmitted helminths (STHs), i.e., roundworms (Ascaris lumbricoides), whipworms (Trichuris trichiura), and hookworms (Necator americanus and Ancylostoma duodenale) are important public health problems, mostly impacting the health of children in several countries of the Americas, sub-Saharan Africa, China, and East and Southeast Asia, including Lao People's Democratic Republic (Lao PDR).1–3 Ascaris lumbricoides is estimated to infect 1.221 billion people globally, T. trichiura 795 million, and hookworms, 740 million globally.1 The blood fluke, Schistosoma mekongi, occurs in communities along the Mekong River in Cambodia and Lao PDR,4 causing intestinal and hepatosplenic disease.5,6 Many other trematode species can also infect people in Lao PDR. These include the highly pathogenic liver fluke, Opisthorchis viverrini, heterophyids such as Haplorchis taichui, and lecithodendriids such as Phaneropsolus bonnei, and Prosthodendrium molenkampi.7 To help planning for improvement of control strategies and evaluation of existing control activities, there was a need to update information on the prevalence and distributions of STHs and schistosomiasis and other trematodes. The information is presented here.
During parasitological surveys in 2012, fecal specimens were collected from 8,610 inhabitants located in 12 provinces and one municipality (Bokeo [N = 537], Houaphan [N = 780], Luang Namtha [N = 440], Luang Prabang [N = 157], Oudomxay N = 969], and Phongsaly Provinces [N = 688] from northern Lao PDR; Bolikhamxay [N = 611]and Xieng Khouang [N = 1,143] Provinces and Vientiane Municipality [N = 243] from the central part of the country and Attapeu [N = 645], Champasak [N = 1,076], Saravan [N = 624], and Sekong Provinces [N = 697] from southern Lao PDR) (Figure 1). Sample size calculation was performed by using simple random sampling based on estimated preliminary prevalence data for STHs (Laymanivong and others, unpublished data). A total of 58 villages from 29 districts were randomly selected (2 or 3 districts per province and 2–3 villages per district). Approximately 300 inhabitants, with equal sex ratio, were randomly selected per village. The study was approved by the Ministry of Public Health, Lao PDR. Oral informed consent was obtained from all human adult participants and from parents or legal guardians of minors.
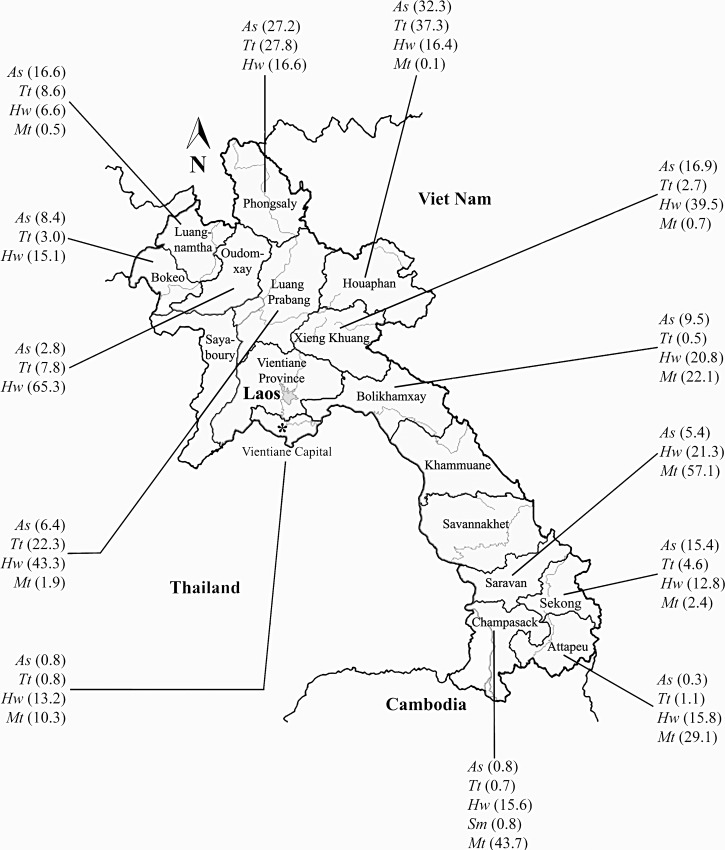
Figure 1.
Percentage prevalence of Ascaris lumbricoides (As), Trichuris trichiura (Tt), hookworm (Hw), Schistosoma mekongi (Sm), and miscellaneous trematodes (including Opisthorchis viverrini) (Mt) in Lao People's Democratic Republic (PDR) in year 2012.
Fecal specimens were examined twice for helminth eggs using the Kato-Katz thick smear technique. Parasitic infections were recorded; numbers of eggs for each helminth species were counted, and intensity of infection was calculated and expressed as eggs per gram of feces (epg). The overall prevalence of A. lumbricoides, T. trichiura, and hookworms were 11.6%, 8.5%, and 25.0%, respectively. The proportion of individuals infected with S. mekongi was 0.1%. Because it is difficult to differentiate eggs of the other trematode species from each other using the Kato-Katz thick smear technique,7 such eggs were recorded as miscellaneous trematode eggs. The overall prevalence of flukes producing such eggs was 14.0%. The individual prevalence of parasites in 12 provinces and one municipality are shown in Figure 1. Infections were categorized as light, moderate, or heavy, following previous criteria8 and are presented in Table 1. Prevalence and intensity according to age and sex distributions (except Luang Prabang province and Vientiane Municipality) are shown in the Supplemental Table. The majority of infections were light. Before the implementation of a 5-year project9 supported by Loa PDR-Korea and the World Health Organization (WHO) Regional Office for the Western Pacific on the control of intestinal parasitic diseases for primary school in Lao PDR was commenced in 2000, the baseline data on the high prevalence of intestinal parasitic infections in Lao PDR were 34.9% for A. lumbricoides, 19.1% for hookworm, and 25.8% for T. trichiura.9 This study revealed that the prevalence of A. lumbricoides and T. trichiura infections decreased about 70% and parasite loads are also low. This reason could be a result of the good effective approach of a nationwide parasite control project.9
Table 1.
Prevalences and intensities of Ascaris lumbricoides, Trichuris trichiura, hook worm, Schistosoma mekongi, and miscellaneous trematode infections in LAO PDR in year 2012
| Area parts | Provinces | % Prevalence (% intensity; light: moderate: heavy)* | ||||
|---|---|---|---|---|---|---|
| As | Tt | Hw | Sm | Mt | ||
| North | Bokeo | 8.4 (80: 20: 0) | 3.0 (100: 0: 0) | 15.1 (100: 0: 0) | NF | NF |
| Houaphan | 32.3 (98.8: 1.2: 0) | 37.3 (100: 0: 0) | 16.4 (94.5: 5.5: 0) | NF | 0.1 (100: 0: 0) | |
| Luang Namtha | 16.6 (87.7: 11: 1.3) | 8.6 (97.4: 2.6: 0) | 6.6 (93.1: 6.9: 0) | NF | 0.5 (100: 0: 0) | |
| Luang Prabang | 6.4 (ND) | 22.3 (ND) | 43.3 (ND) | NF | 1.9 (ND) | |
| Oudomxay | 2.8 (100: 0: 0) | 7.8 (100: 0: 0) | 65.3 (100: 0: 0) | NF | NF | |
| Phongsaly | 27.2 (92: 8: 0) | 27.8 (100: 0: 0) | 16.6 (100: 0: 0) | NF | NF | |
| Central | Bolikhamxay | 9.5 (100: 0: 0) | 0.5 (100: 0: 0) | 20.8 (100: 0: 0) | NF | 22.1 (87.4: 11.1: 1.5) |
| Xieng Khouang | 16.9 (100: 0: 0) | 2.7 (100: 0: 0) | 39.5 (96.9: 2: 1.1) | NF | 0.7 (100: 0: 0) | |
| Vientiane | 0.8 (ND) | 0.8 (ND) | 13.2 (ND) | NF | 10.3 (ND) | |
| South | Attapeu | 0.3 (100: 0: 0) | 1.1 (85.7: 14.3: 0) | 15.8 (100: 0: 0) | NF | 29.1 (98.9: 1.1: 0) |
| Champasak | 0.8 (66.7: 22.2: 11.1) | 0.7 (100: 0: 0) | 15.6 (98.2: 1.8: 0) | 0.8 (55.6: 33.3:11.1) | 43.7 (91.5: 8.3: 0.2) | |
| Saravan | 5.4 (100: 0: 0) | NF | 21.3 (99.2: 0: 0.8) | NF | 57.1 (91.3: 8.7: 0) | |
| Sekong | 15.4 (100: 0: 0) | 4.6 (100: 0: 0) | 12.8 (100: 0: 0) | NF | 2.4 (100: 0: 0) | |
Intensity of egg per gram of feces (EPG) was divided to light (1–4,999), moderate (5,000–49,999), heavy infections (> 50,000) for As (Ascaris lumbricoides), to light (1–999), moderate (1,000–9,999), heavy infections (> 10,000) for Tt (Trichuris trichiura), to light (1–1,999), moderate (2,000–3,999), heavy infections (> 4,000) for Hw (hookworm), to light (1–99), moderate (100–399), heavy infections (> 400) for Sm (Schistosoma mekongi) and to light (1–999), moderate (1,000–9,999), heavy infections (10,000–99,000) for Mt (miscellaneous trematode eggs including Opisthorchis viverrini).
ND = not determined; NF = not found.
Lao PDR has one of the highest prevalence of STHs in Southeast Asia and polyparasitism is common.9,10 The high prevalence of Schistosoma mekongi infection still occurs in a number of small foci, with new infections continuing to occur in the endemic population and travelers.4 We found a high prevalence of STHs and other parasites all over Lao PDR, despite a mass drug administration program providing a high coverage of mebendazole treatment in school-age children since 2006.11 Several factors may explain the continuing high prevalence of STH infections in this region, including poor sanitation and the low socio-economic status in the rural areas, which facilitate high parasite transmission and frequent reinfections. In addition, new S. mekongi cases still occur in Champasak Province, southern Lao PDR, indicating that infected snails (Neotricula aperta) remain prevalent in this setting. Interestingly, a high prevalence of miscellaneous trematode eggs in fecal specimens were found in Bolikhamxay Province and Vientiane Municipality in central Lao PDR, and in Attapeu, Champasak, Saravan, and Sekong Provinces in the southern part of the country. It will be very important to confirm whether O. viverrini is common there, requiring use of the formalin-ether-concentration technique to differentiate between eggs of O. viverrini and those of other flukes.
Our results indicate that a nationwide parasite control program is still necessary to reduce possible morbidity caused by parasitic diseases in Lao PDR. Armed with this new information, it is now possible to plan future public health research and control programs, thus increasing human health and welfare, and supporting socio-economic growth and development in this country.2
Supplementary Material
ACKNOWLEDGMENTS
We acknowledge the support of the Khon Kaen University Publication Clinic, Research and Technology Transfer Affairs, Khon Kaen University, for their assistance.
Footnotes
Financial support: This research was funded by a grant from the Ministry of Public Health, Lao PDR to SL, BH, BK, MP, and BP. OS, WM, and PMI, were supported by a TRF Senior Research Scholar Grant, Thailand Research Fund grant no. RTA5580004, the Higher Education Research Promotion and National Research University Project of Thailand, the Office of the Higher Education Commission through the Health Cluster (SHeP-GMS), and Khon Kaen University.
Authors' addresses: Sakhone Laymanivong, Bouasy Hangvanthong, Boualy Keokhamphavanh, Manisak Phommasansak, and Baunphone Phinmaland, Laboratory Unit, Centre of Malariology, Parasitology and Entomology, Ministry of Health, Lao PDR, E-mails: sakhone07@gmail.com, cmpelao@gmail.com, b.keokhamphavanh@gmail.com, manisak.pham@gmail.com, and baunphone.phin@gmail.com. Oranuch Sanpool, Wanchai Maleewong, and Pewpan M. Intapan, Department of Parasitology and Research and Diagnostic Center for Infectious Disease, Faculty of Medicine, Khon Kaen University, Thailand, E-mails: sanpoolor@yahoo.com, wanch_ma@kku.ac.th, and pewpan@kku.ac.th.
References
- 1.de Silva NR, Brooker S, Hotez PJ, Montresor A, Engels D, Savioli L. Soil-transmitted helminth infections: updating the global picture. Trends Parasitol. 2003;19:547–551. doi: 10.1016/j.pt.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Jex AR, Lim YA, Bethony JM, Hotez PJ, Young ND, Gasser RB. Soil-transmitted helminths of humans in Southeast Asia–towards integrated control. Adv Parasitol. 2011;74:231–265. doi: 10.1016/B978-0-12-385897-9.00004-5. [DOI] [PubMed] [Google Scholar]
- 3.Saboyá MI, Catalá L, Nicholls RS, Ault SK. Update on the mapping of prevalence and intensity of infection for soil-transmitted helminth infections in Latin America and the Caribbean: a call for action. PLoS Negl Trop Dis. 2013;7:e2419. doi: 10.1371/journal.pntd.0002419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muth S, Sayasone S, Odermatt-Biays S, Phompida S, Duong S, Odermatt P. Schistosoma mekongi in Cambodia and Lao People's Democratic Republic. Adv Parasitol. 2010;72:179–203. doi: 10.1016/S0065-308X(10)72007-8. [DOI] [PubMed] [Google Scholar]
- 5.Hatz CF. The use of ultrasound in schistosomiasis. Adv Parasitol. 2001;48:225–284. doi: 10.1016/s0065-308x(01)48007-9. [DOI] [PubMed] [Google Scholar]
- 6.Sinuon M, Tsuyuoka R, Socheat D, Odermatt P, Ohmae H, Matsuda H, Montresor A, Palmer K. Control of Schistosoma mekongi in Cambodia: results of eight years of control activities in the two endemic provinces. Trans R Soc Trop Med Hyg. 2007;101:34–39. doi: 10.1016/j.trstmh.2006.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chai JY, Han ET, Guk SM, Shin EH, Sohn WM, Yong TS, Eom KS, Lee KH, Jeong HG, Ryang YS, Hoang EH, Phommasack B, Insisiengmay B, Lee SH, Rim HJ. High prevalence of liver and intestinal fluke infections among residents of Savannakhet Province in Laos. Korean J Parasitol. 2007;45:213–218. doi: 10.3347/kjp.2007.45.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montresor A, Crompton DWT, Hall A, Bundy DAP, Savioli L. Guidelines for the Evaluation of Soil-Transmitted Helminthiasis and Schistosomiasis at Community Level. 1998. http://www.who.int/iris/handle/10665/63821#sthash WHO/CDS/SIP/98. Available at.
- 9.Rim HJ, Chai JY, Min DY, Cho SY, Eom KS, Hong SJ, Sohn WM, Yong TS, Deodato G, Standgaard H, Phommasack B, Yun CH, Hoang EH. Prevalence of intestinal parasite infections on a national scale among primary schoolchildren in Laos. Parasitol Res. 2003;91:267–272. doi: 10.1007/s00436-003-0963-x. [DOI] [PubMed] [Google Scholar]
- 10.Conlan JV, Khamlome B, Vongxay K, Elliot A, Pallant L, Sripa B, Blacksell SD, Fenwick S, Thompson RC. Soil-transmitted helminthiasis in Laos: a community-wide cross-sectional study of humans and dogs in a mass drug administration environment. Am J Trop Med Hyg. 2012;86:624–634. doi: 10.4269/ajtmh.2012.11-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization . First Mekong-Plus Programme Managers Workshop on Lymphatic Filariasis and Other Helminthiasis. 2009. MVP/WPRO March 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.