Abstract
Pyogenic liver abscesses caused by Salmonella enterica serotype Typhi, although rare, can occur especially in patients with pre-existing hepatobiliary disease, hepatocellular carcinoma, and metastatic liver tumors. We present a case of Salmonella liver abscesses complicating metastatic melanoma in a 24-year-old alcoholic male.
Introduction
Salmonella enterica serotype Typhi (S. typhi) is the causative agent of typhoid fever, an acute systemic infection that is common in developing countries, associated with low socioeconomic levels and poor sanitary conditions.1 Humans are the only natural reservoirs and can be asymptomatic carriers.2 Transmission usually occurs through the fecal–oral route by ingestion of contaminated food or water.2 In endemic areas, the majority of cases occur in children and adolescents, 3–19 years of age.2
The estimate of global burden of typhoid fever is 21,650,974 illnesses and 216,510 deaths annually.3 Regions with a high incidence of typhoid fever (> 100/100,000 cases/year) include South Central Asia and Southeast Asia.3 In Brazil, an average of 500 cases of typhoid fever have been reported each year since 2003; the majority from the Amazon region, followed by the Northeast part of the country.4
Since the advent of antibiotics, S. typhi infection and its hepatic complications have become increasingly rare.5 However, preexisting hepatobiliary diseases, including cholelithiasis,6 amebic abscess,7 echinococcal cysts,5 intrahepatic hematoma,5 and hepatocellular carcinoma8 are known risk factors.
We present a case of typhoid fever complicated by pyogenic liver abscesses (PLA) overlying hepatic metastases of melanoma. This case illustrates the importance of associated underlying diseases, such as cancer, and complications of Salmonella infection.
Case Report
A previously healthy, 24-year-old male farm worker from the rural interior of Ceará state in Northeast Brazil presented to the Hospital São José of Infectious Diseases (HSJ) in Fortaleza on April 7, 2009 with a chief complaint of severe right upper quadrant pain. Three weeks before admission, he reported mild to moderate daily fever with chills, profuse sweating, episodes of nausea, vomiting, and abdominal enlargement. Abdominal pain developed 2 weeks before admission and was accompanied by fatigue and a 4 kg weight loss. Past medical and social history were significant for alcohol dependence. Physical examination revealed no acute distress febrile (38.5°C) patient, blood pressure = 100 × 60 mmHg, pulse = 84 beats/minute, mildly pale, without peripheral lymph node enlargement. Gynecomastia and spider veins were noted on the chest, and moderate lower limb edema. Pulmonary and cardiac auscultations were normal. Abdomen was distended with enlarged palpable spleen and liver.
Laboratory tests on admission showed: hematocrit = 21.5%, hemoglobin = 7.4 g/dL, white blood cell count = 19,170 cell/mm3 (78% of neutrophil; 21% of lymphocytes; 1% of monocytes; 0% of eosinophils and basophils); platelet count was 196,000/mL. Alkaline phosphatase was 799 U/L, and lactate dehydrogenase was 1,019 U/L, but urea, creatinine, aspartate aminotransferase (AST), alanine aminotransferase (ALT), amylase, glicemia, bilirubin, and electrolytes (sodium and potassium) were normal; serology for human immunodeficiency virus (HIV) was negative. Salmonella spp. was isolated from two blood culture samples, sensitive to ampicillin, ciprofloxacin and third generation cephalosporins. Abdomen ultrasonography (USG) revealed an enlarged liver with right lobe and left lobe measuring 23.8 and 10.8 cm, respectively, showing multiple heterogeneous expansile formations of precise limits, the largest measuring 12 cm × 11.9 cm; and also an enlarged spleen measuring 17.3 cm without nodules.
Computed tomography of the abdomen showed hepatosplenomegaly, multiple nodules scattered throughout the hepatic parenchyma of heterogeneous content without ascites, but with bilateral basal pleural effusion (Figure 1). Upper gastrointestinal endoscopy showed only discrete chronic gastritis. After initiation of ceftriaxone and metronidazole, the patient showed slight improvement of his general status and was taken to Hospital Universitário Walter Cantídeo (HUWC) for further work-up.
Figure 1.
Contrast-enhanced abdominal computadorized tomography with liver abscesses caused by Salmonella typhi within a metastatic melanoma.
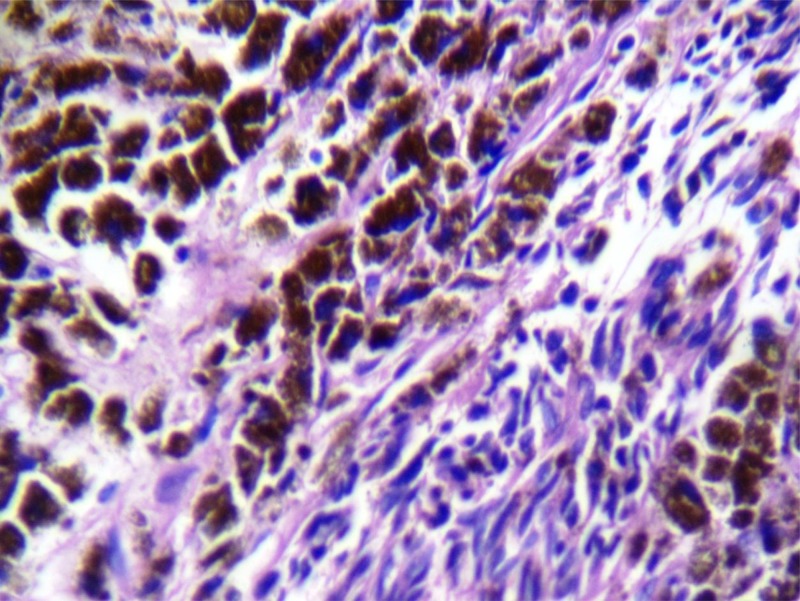
Salmonella typhi was isolated from the liver percutaneous puncture collected material and ceftriaxone and metronidazole were replaced by ciprofloxacin IV. The patient showed partial improvement of pain, no nausea or vomiting, but daily bouts of fever persisted. Subsequent USG showed an increase in volume of the liver collections (15.8 cm × 11.0 cm). A second drainage was performed and 20 mL of chocolate-like material was collected and sent for laboratory analysis. Culture samples were negative for pyogenic bacteria and microscopic examination did not show Entamoeba histolytica. Because of the persistence and increase of the nodules by USG, a liver biopsy was performed and specimens stained by hematoxylin and eosin (H&E) were diagnostic of a neoplasm, characterized by atypical spindle cells with eosinophilic cytoplasm often containing melanin and vesicular nuclei sometimes with eosinophilic macronucleoli, arranged in irregular fascicles, permeated by foci of desmoplasia. No hepatic parenchyma was seen in the samples (Figure 2). Histology was conclusive for fusiform malignant melanoma. The patient underwent chemotherapy, with no significant response, and then developed hepatic failure and was lost to follow-up.
Figure 2.
Hematoxylin and eosin (H&E) 40×. Fusiform malignant melanoma. Coarse melanin granules in hyperpigmented cells. Less pigmented somewhat spindled cells (lower half and right of the figure).
Discussion
The PLA are an uncommon clinical entity and many times difficult to diagnose and treat.9 In the majority of patients with PLA, the illness begins in an extrahepatic focus of infection, with subsequent spread to the liver by way of the portal or systemic circulation or the biliary tree.10 The PLA may also arise as a direct extension of adjacent upper abdominal suppuration or as a complication of blunt or penetrating trauma to the liver.10 Peak incidence occurs in the fifth decade, with the biliary tract as the most common starting point.9 The most frequent pathogenic agents are Gram-negatives, primarily Escherichia coli, followed by Gram-positive aerobes, with anaerobes in a lesser frequency.5 More recently, differences in the microbiological spectrum has been observed between continents.11
Since the beginning of the antibiotic era, liver abscess caused by Salmonella organisms have been very rare12 and in most cases, the species involved is S. typhi.13 Based on a report by Moralejo and others, from Spain (2002),5 of the literature review from 1995 to 2000, 14 cases of liver abscess by S. typhi have been published; of these, eight occurred associated with liver injury described as: amebic abscesses, echinococcal cysts, or intrahepatic hematomas. In a study by Ferreira and others (2007)9 from Portugal, reviewing 119 cases of PLA occurring from 1986 to 2004, they found only typhoid fever as the sole predisposing condition. In a report by Sony and others (1994)7 no associated disease, except positive amebic serology, was observed in a 47-year-old African male with multiple hypoechoic lesions in both lobes of the liver, the largest in the right lobe, which grew S. typhi in the needle aspirate.
There are several possibilities for pathogenesis of Salmonella abscesses: one is the migration of S. typhi to the liver in an asymptomatic carrier, as suggested in the report of Moralejo and others,5 and also in the report of Ciraj and others.6 The other mechanism is hematogenous migration from the focus during the intestinal phase of typhoid state.5 Through this mechanism, abscesses are most likely to be found in multiple organs, also multiple in the liver, as in the current report and in the cases described previously.7,14
Previous authors have noted that suppuration by any bacteria may complicate metastatic tumors in the liver, as reported by Trump and others (1978)10 in a patient with cloacogenic carcinoma and PLA within hepatic metastasis. Other investigators have attempted to clarify the clinical course of PLA in patients with various cancers. In a retrospective study, from January 1980 through December 1993, Yeh and others15 studied 52 cases of PLA related to preexisting or coexisting malignant disease from a total of 542 patients with PLA in Taiwan; in 32 patients, the cancers were originated from the hepatic parenchyma, biliary system, and pancreas, whereas 20 patients had cancer originating from other sites. These authors concluded that PLA can be a presentation of underlying hepatopancreatobiliary malignant disease and carries a severe prognosis.
Clinical manifestations of liver abscess caused by underlying malignant disease were fever, chills, right sided hypochondrial pain, hepatomegaly, nausea and vomiting, malaise, weight loss, and jaundice, all of which were indistinguishable from those with benign causes.15 The similarities of findings between these two entities may contribute to an almost 2-fold higher mortality rate of PLA caused by underlying malignant illness compared with PLA in the absence of malignancy.15 In many cases, tumor necrosis may be difficult to differentiate from abscess based on clinical exam and imaging alone.16 On the other hand, considering that up to a quarter of patients with liver metastases have fever and symptoms of infection, this picture can mask an underdiagnosed PLA.13
The PLA caused by S. typhi requires drainage by open or percutaneous methods, in addition to prolonged courses of antibiotics.1 Recommended therapy is intravenous ceftriaxone or fluoroquinolones for 14 –21 days.1 Alternate therapy for susceptible strains is co-trimoxazole, ampicillin, or chloramphenicol for 14 –21 days.1
In our case report, the fact that the patient came from a rural area in the state of Ceará, with little access to clean water, illustrates the association between poor sanitary conditions and S. typhi infection. In addition to the epidemiological setting, a highlight of this case was the discovery of liver metastases of a melanoma of which the primary site was undetermined. Based on the review of Moralejo and others,5 more than a half of the published cases of liver abscess by S. typhi had an underlying condition, we assume that the melanoma metastasis was the predisposing condition in this case. In our review of the literature, this is the first report of PLA caused by S. typhi in a metastatic melanoma.
In summary, we describe an unusual presentation of Salmonella typhi infection in a patient with persistent symptoms and no improvement despite treatment and emphasize the need to investigate for underlying malignant condition in cases of pyogenic liver abscess.
Footnotes
Financial support: The American Committee on Clinical Tropical Medicine and Travellers' Health (ACCTMTH) assisted with publication expenses.
Authors' addresses: Jannaina F. Jorge, Andressa B. V. Costa, Jorge L. N. Rodrigues, Evelyne S. Girão, Roberta S. Luiz, Anastácio Q. Sousa, Sean R. Moore, and Dalgimar B. Menezes, UFC, Saúde Comunitária, Fortaleza, Brazil, E-mails: jannafj@hotmail.com, andressa_brasil@hotmail.com, jorge1207@gmail.com, egirao@uol.com.br, aqsousa@gmail.com, robertaassociados@hotmail.com,mooresea@gmail.com, and dalgimar@biopse.com.br. Terezinha M. J. S. Leitão, Federal University of Ceará, Health Community Department, Rua Prof. Costa Mendes, Fortaleza, Ceará, Brazil, and Hospital São José, Fortaleza, Ceará, Brazil, E-mail: tsilva@ufc.br.
References
- 1.Huang DB, DuPont HL. Problem pathogens: extra-intestinal complications of Salmonella enterica serotype Typhi infection. Lancet Infect Dis. 2005;5:341–348. doi: 10.1016/S1473-3099(05)70138-9. [DOI] [PubMed] [Google Scholar]
- 2.WHO . Background Document: The Diagnosis, Treatment and Prevention of Typhoid Fever. Geneva: WHO/V&B/03.07; 2003. [Google Scholar]
- 3.Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World Health Organ. 2004;82:346–353. [PMC free article] [PubMed] [Google Scholar]
- 4.Ministry of Health (Brazil) Infectious and Parasitic Diseases. Eighth edition. Ministério da Saúde: Brasília, Brazil: 2010. [Google Scholar]
- 5.Moralejo ML, Montero MJ, Fuertes A, de Las Heras JA, Jimenez A. Liver abscess due to Salmonella typhi. Enferm Infecc Microbiol Clin. 2002;20:41. [PubMed] [Google Scholar]
- 6.Ciraj AM, Reetika D, Bhat GK, Pai CG, Shivananda PG. Hepatic abscess caused by Salmonella typhi. J Assoc Physicians India. 2001;49:1021–1022. [PubMed] [Google Scholar]
- 7.Soni PN, Hoosen AA, Pillay DG. Hepatic abscess caused by Salmonella typhi. A case report and review of the literature. Dig Dis Sci. 1994;39:1694–1696. doi: 10.1007/BF02087778. [DOI] [PubMed] [Google Scholar]
- 8.Cho YK, Yang SY, Chung DR, Kim EO, Kim MN, Kim YS, Woo JH, Pai CH, Ryu JS. Two cases of Salmonella typhi liver abscess after transarterial- chemoembolization. Korean J Infect Dis. 1997;29:447–451. [Google Scholar]
- 9.Ferreira S, Barros R, Santos M, Batista A, Freire E, Reis E, Correia J, Oliveira J. Abscesso Hepático Piogênico - Casuística de 19 anos. J Port Gastrenterol. 2007;14:128–133. [Google Scholar]
- 10.Trump DL, Fahnestock R, Cloutier CT, Dickman MD. Anaerobic liver abscess and intrahepatic metastases. A case report and review of the literature. Cancer. 1978;41:682–686. doi: 10.1002/1097-0142(197802)41:2<682::aid-cncr2820410237>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 11.Cerwenka H. Pyogenic liver abscess: differences in etiology and treatment in Southeast Asia and Central Europe. World J Gastroenterol. 2010;16:2458–2462. doi: 10.3748/wjg.v16.i20.2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee CC, Poon SK, Chen GH. Spontaneous gas-forming liver abscess caused by Salmonella within hepatocellular carcinoma: a case report and review of the literature. Dig Dis Sci. 2002;47:586–589. doi: 10.1023/a:1017924321058. [DOI] [PubMed] [Google Scholar]
- 13.Mòdol JM, Santaeugenia S, Tudela P, Barlueng E. Absceso hepático por Salmonella sobre metástasis de un tumor mülleriano de útero. Med Clin (Barc) 2006;127:518–519. doi: 10.1157/13093275. [DOI] [PubMed] [Google Scholar]
- 14.Kabra S, Vishal W. Hepatic abscess caused by Salmonella typhi. Indian Pediatr. 2006;43:81–82. [PubMed] [Google Scholar]
- 15.Yeh TS, Jan YY, Jeng LB, Hwang TL, Chao TC, Chien RN, Chen MF. Pyogenic liver abscesses in patients with malignant disease: a report of 52 cases treated at a single institution. Arch Surg. 1998;133:242–245. doi: 10.1001/archsurg.133.3.242. [DOI] [PubMed] [Google Scholar]
- 16.Fawcett HD, Lantieri RL, Frankel A, McDougall IR. Differentiating hepatic abscess from tumor: combined 111In white blood cell and 99mTc liver scans. AJR Am J Roentgenol. 1980;135:53–56. doi: 10.2214/ajr.135.1.53. [DOI] [PubMed] [Google Scholar]