Summary
Background
Portable Data for Imaging (PDI) is regularly used as a guideline for sharing medical imaging data between hospitals and other medical institutions. When a patient is referred to another location, the patient almost always brings PDI media on a CD or DVD. However, problems often occur when trying to view images on PDI discs inserted into computer terminals, and it is more efficient to view images on the hospitals’ own picture archiving and communication system (PACS). On the request of doctors, it has become a routine practice to import PDI data to the PACS of the referred hospital.
Objective
The aim of this study was to analyze the increase in PDI image importing and investigate methods for reducing the burden caused by importing images.
Methods
We compiled representative data on image importing over time and analyzed the test modalities, number of images, volume of data, and referring hospital or medical clinic from which the data originated.
Results
The amount of PDI images imported to the PACS has risen despite no large increase in the number of patients. Currently, images imported from PDI media make up 22.8% of the total number of images stored in the PACS. The images come from a diverse array of hospitals (184 hospitals) and 82% are essential for medical care. The total annual expenditure associated with PDI data management is estimated to be 98,300 USD.
Conclusion
The spreading use of the PDI guideline has led to a dramatic increase in data image sharing in the field of healthcare. While this has great benefits for patients and doctors, it is also associated with a greater cost and an overall burden for hospitals. These results indicate the need for a system to enable many hospitals and clinics to participate in image sharing at a cheaper cost.
Key words: Portable data for imaging, PDI, PACS, cross-enterprise document sharing-imaging, XDS-I
1. Introduction
Portable Data for Imaging (PDI) is a guideline for saving medical imaging studies on CDs and other portable media to enable their sharing and viewing. The guideline defines where and how to store these imaging studies in portable media. The contents comprise where in the media and in⊠what directory the DICOM images and their directory DICOMDIR are to be located. In 2008, this guideline was adopted in Japan as the integration profile of the Integrating the Healthcare Enterprise (IHE) [1].
Sharing imaging test information from computer tomography (CT), magnetic resonance imaging (MRI), and other tests, by CD or DVD gradually increased prior to 2008, at which point a sudden switch was seen from conventional film based sharing to PDI based methods, which are now common and widespread in Japan. When referring a patient, PDI media are almost always exchanged. Numerous PDI media are now brought to hospitals from outside facilities (e.g., other hospitals, medical clinics, and imaging centers).
Many issues emerge in this process, and discussions are ongoing to consider solutions [2]. Some major problems are the difficulties in viewing images correctly due to violations of the DICOM or the PDI rules and an increased risk of virus transmission through the media [3]. Moreover, viewing images directly from a CD or DVD on a computer terminal requires installing viewer software or importing a large amount of data, both of which are very time-consuming. The IHE and various academic societies and organizations are engaging in educational activities to ensure that everyone conforms to the rules, such as complying with the PDI guideline when exporting data and limiting the total size of data exported to fit on CD or DVD. As one measure conducted by hospitals to avoid these problems that occur in outpatient clinics, the hospitals are importing the PDI data to their own picture archiving and communication systems (PACS) in advance [4, 5]. This reduces the number of problems occurring primarily in the outpatient clinics and makes it appear as though the problems associated with PDI have been eliminated.
Nevertheless, the expenditure of hospitals dealing with the ever-increasing volume of PDI continues to rise, and so has become a more serious problem. We must recognize that importing large volumes of PDI media to the PACS before patients begin their consultation requires the use of computer terminals and human resources, and that data saved on the PACS uses up a great volume of storage capacity on the hospital’s server.
Some measures are being taken to share images without using PDI [6–10]. For example, a large-scale inter-facility integrated system that includes electronic medical records is being built. However, continuing these projects, which require very large budgets or external subsidies, is an unknown economic burden.
2. Objectives
The aim of this study was to assess the conditions involving images brought to hospitals on PDI media and the increase in PDI data imported to the PACS, as well as to discuss methods for reducing the burden on hospitals due to the importing of PDI data.
We attempted to clarify the regions of the hospitals and medical clinics from which images originate and the amount of images brought, as well as how that volume has increased over the years. We also attempted to determine the ratio of images imported to the PACS versus those taken at the hospital itself.
In addition, we categorized the images based on their reason for importing by investigating the purpose for the outpatient visit, and we analyzed the extent to which those imported images were needed.
3. Methods
3.1 Study field
Yokohama, an urban city with a population of 3.7 million, has six university hospitals and 10 other hospitals with more than 500 beds within the city limits. Yokohama City University (YCU) Hospital is located in the south part of Yokohama, which is in the east part of Kanagawa Prefecture, Japan. YCU Hospital has 648 hospital beds, admits 12,635 inpatients, and receives 468,107 outpatient visits a year. It also receives 12,801 patient referrals a year, of which 68% are from medical institutions within Yokohama; the remaining referrals are from medical institutions throughout the large span of Kanagawa Prefecture.
As there are many other large-scale hospitals in the vicinity, large hospitals and smaller hospitals and medical clinics in Yokohama are not associated in a hierarchy, but rather they create a complex N-to-N network. YCU Hospital cooperates with a diverse array of medical institutions, although their relationships are unaffiliated.
▶ Figure 1 shows the two workflows from reception until doctor consultation when an outpatient brings PDI media with them [1]. If an outpatient who has come for a doctor’s visit upon referral brings his/her PDI media, then all the media are passed to the reception counter. The reception clerk issues an order for the images on the PDI media to be imported to the PACS and placed in the hospital information system (HIS), and then the media are carried over to the radiology department reception counter. The clerk at the radiology reception counter receives the HIS order, extracts the data from the media brought over, and imports the images to the PACS by using a terminal dedicated for that purpose. The examining doctor views the images imported to the PACS on the doctors’ terminal while the patient is waiting for a consultation, and then the doctor sees the patient [2]. As another type of workflow, sometimes the PDI media are not collected at reception, and the patient brings them directly to the outpatient doctor’s office. In these cases, the outpatient doctor issues an order, if necessary, for the data to be imported to the PACS by the reception clerk, as in [1]. If necessary, the doctor can choose to issue an order to the diagnostic radiologist to interpret the imported studies.
Fig. 1.
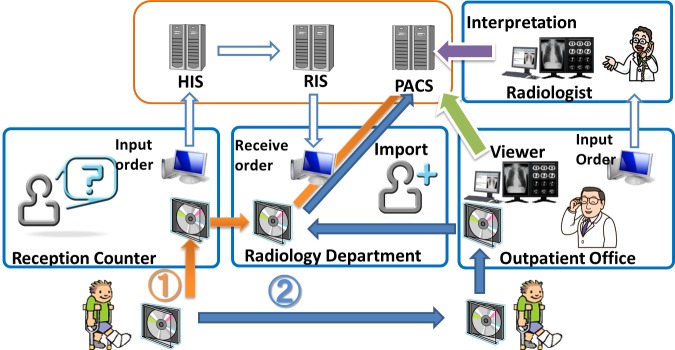
Workflow of image imported to PACS from PDI media. HIS: hospital infomation system, RIS: radiology information system , PACS: picture archiving and communication system
Until 2010, only the latter half of the practice [2] was performed. The outpatient doctor issued data import orders as needed after viewing PDI images on a stand-alone PC using the viewer application installed in the PDI media. However, not only does installing the viewer application on the computer take time, but the installation often fails and some viewers are unfamiliar with the process, possibly because they are using it for the first time. These issues can be aggravating for the doctor. As a resolution, since 2010, it has been an established practice for all PDI media to be submitted from the patient to the clerk at the reception counter and imported to the PACS.
3.2 Data collection
The number of outpatients visiting the hospital and the number of referred patients were extracted from the medical business accounting database. The number of tests stored on the PACS was compiled separately for each test modality for each year from the PACS data base (Synapse, FUJIFILM Medical, Tokyo, Japan). Imported tests are recognized with the label “DIGITIZ” on the DICOM tag.
From the information at reception, we compiled information on the hospital that referred patients. Each patient had submitted images to reception that were imported to the PACS in May 2012 (detailed information was collected for management analysis purposes). The location of the medical institution was confirmed and the number of patients from that medical institution was plotted on a map.
At the same time, we determined the conditions of the outpatient visit from the electronic medical records for all patients that had images imported to the PACS. We sorted these patients into three categories:
patients who were referred for further examination or treatment and continued receiving examinations and treatment at YCU Hospital;
patients who were referred here, but did not undergo treatment or continue receiving medical care for longer than 3 months; and
patients who had been visiting YCU Hospital for at least 1 month prior and had imported imaging data from tests taken at another medical institution.
We calculated the burden on the hospital associated with importing and saving PDI data. These calculations included the labor time and number of clerks required to import the data, the number of terminals and maintenance costs required for importing the data, and the direct cost associated with saving the data to the PACS. We also calculated the burden on the diagnostic radiologist associated with importing the data.
4. Results
4.1 Temporal changes in images imported to the PACS
The number of imaging examinations and images imported to the PACS for each test modality from 2005 to 2012, the total number of examinations and images, and the number of imaging examinations and images taken at YCU Hospital are shown in ▶ Table 1, ▶ Table 2 and ▶ Figure 2. The number of images stored on the PACS has continued to rise since the first stage of PACS operation in 2005. The number of imported images has also continued to rise, though more slowly until 2008, because only film scanning data were first imported. In 2009, importing from PDI media started. That number began increasing drastically in 2010, when in principle it became routine practice to import all PDI media data brought by patients. Most test modalities were CT scans at 42% and MR images at 35%.
Table 1.
Number of examinations stored to the PACS
| Year | Modality | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|---|---|---|---|
| Imported Examinations |
CR | NA | NA | NA | 96 | 605 | 1,396 | 2,140 | 2,858 |
| CT | NA | NA | NA | 139 | 1,102 | 2,556 | 3,211 | 4,144 | |
| MRI | NA | NA | NA | 136 | 1,094 | 2,444 | 3,234 | 4,409 | |
| PT | NA | NA | NA | 15 | 228 | 454 | 496 | 468 | |
| Rl | NA | NA | NA | 20 | 141 | 199 | 344 | 453 | |
| Others | NA | NA | NA | 4,147 | 4,125 | 2,966 | 2,796 | 2,877 | |
| Total(%) | 357 (0.3) |
2,134 (1.3) |
4,840 (2.9) |
4,553 (2.8) |
7,295 (4.9) |
10,015 (6.3) |
12,221 (7.6) |
15,209 (8.9) |
|
| Examinations Taken at YCU Hospital (%) |
135,474 (99.7) |
156,693 (98.7) |
161,914 (97.1) |
160,510 (97.2) |
141,224 (95.1) |
150,038 (93.7) |
149,515 (92.4) |
154,764 (91.1) |
|
| Total Stored Examinations | 135,831 | 158,827 | 166,754 | 165,063 | 148,519 | 160,053 | 161,736 | 169,973 | |
Table 2.
Number of images stored to the PACS
| Year | Modality | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|---|---|---|---|
| Imported Images | CR | NA | NA | NA | 246 | 1,455 | 3,361 | 5,006 | 6,601 |
| CT | NA | NA | NA | 31,216 | 270,613 | 622,350 | 879,653 | 1,157,905 | |
| MRI | NA | NA | NA | 18,018 | 209,324 | 536,880 | 708,153 | 953,512 | |
| PT | NA | NA | NA | 8,499 | 83,755 | 210,608 | 274,096 | 298,725 | |
| Rl | NA | NA | NA | 2,567 | 4,300 | 7,239 | 36,267 | 71,769 | |
| Others | NA | NA | NA | 31,411 | 81,842 | 146,571 | 194,068 | 226,193 | |
| Total (%) | 1,692 (0.0) |
13,250 (0.3) |
30,324 (0.5) |
91,957 (1.3) |
651,289 (8.2) |
1,527,009 (15.6) |
2,097,243 (19.9) |
2,714,705 (22.8) |
|
| Images Taken at YCU Hospital (%) | 4,181,056 (100.0) |
5,259,092 (99.7) |
6,186,483 (0.5) |
6,759,349 (98.7) |
7,256,081 (91.8) |
8,265,106 (84.4) |
8,436,167 (80.1) |
9,170,771 (77.2) |
|
| Total Stored lmages | 4,182,748 | 5,272,342 | 6,216,807 | 6,851,306 | 7,907,370 | 9,792,115 | 10,533,410 | 11,885,476 | |
Fig. 2.
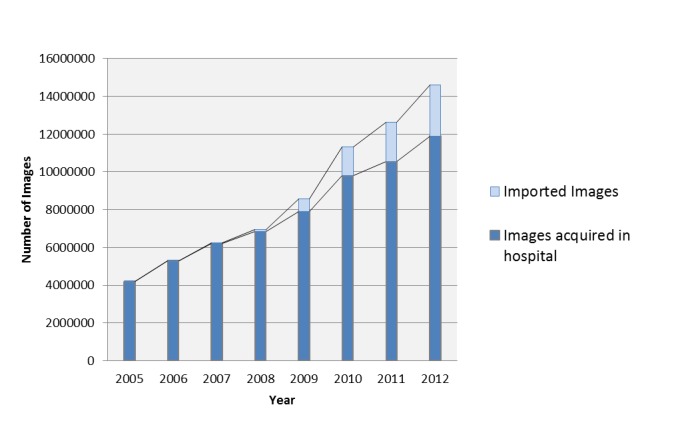
Annual stored images in PACS.
The results show that, currently in 2012, images imported from PDI media make up 22.8% of the total number of images stored to the PACS. Images make up as much as 22.8% even though the percentage of studies imported is only 8.9%. This reveals that a dominant portion of studies are CT, MRI and other modalities with a large number of images per study.
4.2 Distribution and number of tests from each referring hospital
▶ Figure 3 shows the number of patients from each referring hospital that submitted PDI media to the reception counter in May 2012 and had the data imported to the PACS. The hospital from which the most images were imported (for 31 patients in that month) was the one that was closest to YCU Hospital. This is the result of MRI requests sent to this particular hospital when the YCU Hospital reached capacity for MRIs and the results were imported back to the YCU Hospital PACS. The number from other medical institutions was less than 15 patients that month. PDI media were received from as many as 184 different medical institutions. The graph only shows the 46 medical institutions that sent PDI media for two or more patients and does not include data for the remaining 138 institutions that sent PDI media for only one patient.
Fig. 3.
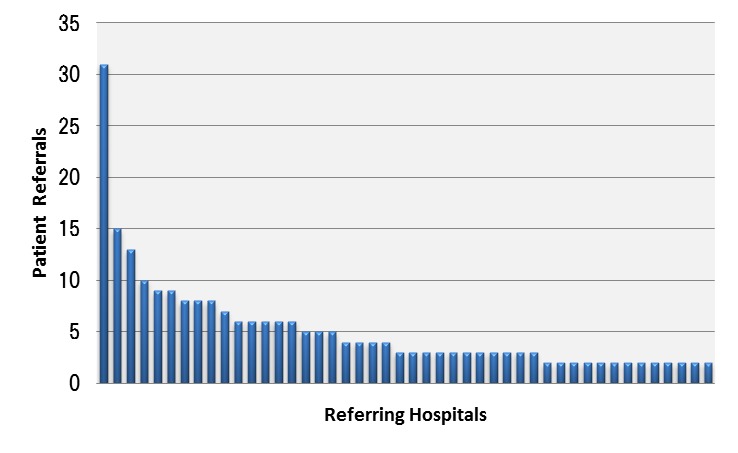
Patients from each referring hospital that imported PDI data to PACS in May 2012. The graph only shows the 46 medical institutions that sent PDI media for two or more patients and does not include data for the remaining 138 institutions that sent PDI media for only one patient.
The geographical distribution of referring hospitals is shown in ▶ Figure 4. The size of the circles represents the number of patients, and medical institutions that referred only one patient are not included. This graph reveals that the number of patients referred increases with the proximity of the medical institution to YCU Hospital, but it also shows that the range of distribution is spread throughout Kanagawa Prefecture and not limited to Yokohama.
Fig. 4.
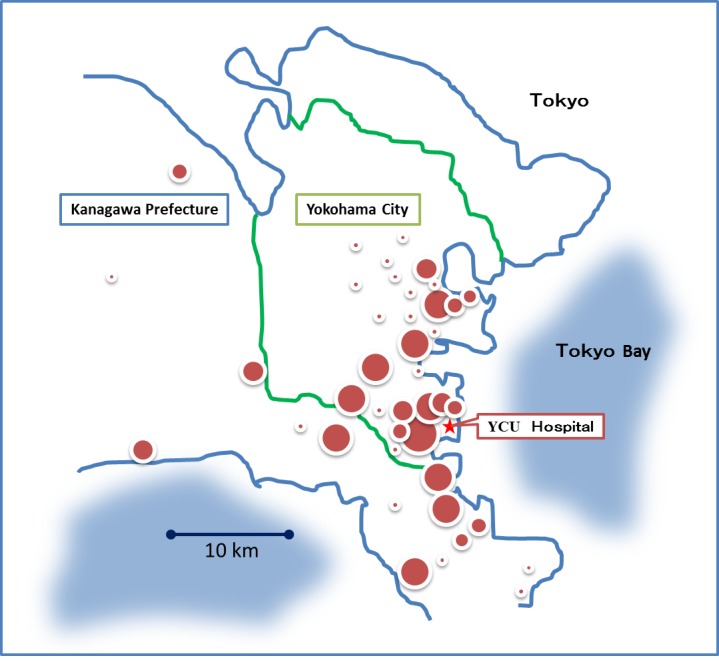
Geographical distribution of referring hospitals.
One feature of YCU Hospital as a university hospital is that it has affiliations with numerous other hospitals, and the graph shows that the distribution of the number of patients has a long tail.
4.3 Conditions of visits for patients that had PDI data imported
▶ Table 3 shows results for all patients that had images on PDI media from another medical institution and imported to the PACS during the month of May 2012. The results are divided into three categories depending on the situation before and after the images were imported. The dataset includes 589 patients, which is more patients than those stated in Section 4.2 because the dataset includes many patients who had image importing orders issued by the outpatient doctor. A total of 297 patients continued examinations and treatment, 105 patients did not undergo many examinations or much treatment and soon stopped visiting the hospital, and 187 patients had already been visiting the hospital.
Table 3.
Situation of patients that had PDI data imported in May 2012
| Situation of patient | Number of Patients | |
|---|---|---|
| 1. | Patients continued examination and treatment | 297 |
| 2. | Patients without many examinations or treatments and stopped visiting | 105 |
| 3. | Patients already visiting the hospital | 187 |
| Total Number of Patients | 589 | |
The images of the 105 patients (18%) that soon stopped visiting the hospital can be said to have gone „unused” after being imported to the PACS. Even though the images will be stored on the PACS server for a long time, they are unlikely to be used in the future.
4.4 Costs charged to the hospital associated with PDI data management
The results of calculations to determine the annual costs charged to the hospital for importing and storing PDI data are shown in ▶ Table 4. In the one-year period of 2012, a total of 15,209 imaging test examinations and 2,714,705 images of approximately 6,000 patients were imported. One reception clerk performed the task of issuing the data import orders. It was estimated that each instance of receiving the media and issuing an order took 5 minutes for one patient, and so required a total of 500 working hours for the year. At an hourly wage of 10 US dollars (USD), the total annual cost would be approximately 5,000 USD. In addition, the data is managed by two dedicated full-time employees (whose sole job is importing studies) at an annual personnel expense of 60,000 USD. Two computer terminals of portable media importer (AOC, Array Corporation, Tokyo, Japan, and PD-S, Fujifilm Medical, Tokyo, Japan) were required for importing the data, with an annual maintenance cost of 15,000 USD. The volume of data imported to the PACS was calculated to be approximately 1.4 terabytes a year, assuming an average one-image size of 0.5 Mbyte. Approximately 5,000 USD would be needed as the cost of adding hard disk space.
Table 4.
Annual costs charged to the hospital for importing and storing PDI data
| Items | Details | Annual cost (USD) |
|---|---|---|
| Reception clerk | 500 working hours/year | 5,000 |
| Radiology clerk | two full-time employees | 60,000 |
| Maintenance fee of PC terminal | two PC terminals | 15,000 |
| Adding hard disk space | 1.4 TB/year | 5,000 |
| Radiologist reporting fee | 1,330 reports | 13,300 |
| Total cost | 98,300 | |
Of the images imported, 1,330 were deemed as needed by the doctor, who then made an order for interpretation by a diagnostic radiologist. Dividing their annual salary by the annual number of studies interpreted gives an estimate of 10 USD per study.
Adding up the above costs gives a total annual expenditure of approximately 98,300 USD associated with PDI data management. There is no separate medical service payment for importing images or having them interpreted, so the hospital receives no revenue from such actions.
5. Discussion
It is certainly true that the spread of PDI has had enormous benefits for patients. With PDI, test imaging data that is essential to treatment can be brought by patients when they move to another medical institution to receive treatment. Because past information can be requested at any time, the need for unnecessary redundant testing is eliminated. As a result, diverse hospitals and medical clinics are actively adopting PDI, leading to increased convenience for patients. While the frequency of PDI use is increasing, there has also been an increase in obstacles, such as difficulties reading data and DICOM rule violations. Academic societies and healthcare-related organizations have been working to remedy these problems. However, their work is leading to smoother operation and consequently even more PDI images, in what becomes a vicious circle.
The present study revealed that less than four-fifths of the images stored in the university hospital PACS were taken within the hospital, while the remaining volume, i.e., more than one-fifth of all images, was due to images brought in from the outside as PDI media. This prompts the question of whether it is necessary to store all these images. Because patients referred to YCU Hospital for a second opinion do not necessarily continue visiting the hospital after the first visit, there is no reason to store the images on the PACS, nor is there a legal obligation to do so. However, examination of the situation of patient visits reveals that over 80% of referred patients go on to receive further examinations or treatment and continue to visit the hospital. A large portion of the images imported to the PACS from the PDI media brought by these patients is clearly indispensable for their treatment. Even if some images are not needed, it is the doctor who must determine the need. Consequently, the time burden to the doctor can also be predicted to increase. Although the decision in 2010 to begin importing all images in PDI media to the PACS meant an increase in data stored to the PACS and in hospital expenses, it also drastically reduced the burden to the doctor, who no longer needs to install PDI media on a standalone computer or to determine which images need to be stored. This change is certainly very helpful clinically.
If it is clear that the expense associated with importing data from PDI media to the PACS is unavoidable for hospitals, the next challenge is how to reduce that expense. If images can be shared without relying on PDI for offline media, but rather through a network based system, PDI media will no longer be needed. Cross-enterprise Document Sharing for Imaging (XDS-I) is a system for sharing electronic medical records, documents, and images via a network. It has the merit that only the location where the data is stored is shared, and so this system eliminates the need to copy or move actual data. Such systems are being built as a progressive approach and as useful systems for sharing information between numerous medical institutions [11, 12]. However, because a large initial investment is required to build the system and the hurdle of having numerous medical institutions join the system is quite large, such systems are not yet widespread [13].
We estimated the extent to which PDI media could be replaced by building this type of network based system. According to Figure 3, building a system with the 15 medical institutions that referred six or more patients with PDI media in one month would cover 145 patients, or only 38.6%. Building a system with the 34 medical institutions referring three or more patients in one month would cover 212 patients, which is 56.4%, or roughly half. It is clear that building a system with fewer medical institutions would not be cost-effective.
One potential solution is an online PDI system. Instead of saving data exported in accordance with the PDI guideline on media, this system would send data to the destination medical institution online in a way similar to sending a file as an e-mail attachment. Image sharing by PDI media is a common practice. All medical institutions have computer terminals for importing and exporting PDI and regularly handle PDI data. The only difference is that instead of sending data via media, it would be sent online, making it easy to adopt the system. Such a system would have great benefits, such as freeing human resources currently importing PDI data brought on media during the short time while patients are waiting for their consultation, and eliminating the risks associated with losing, returning, and disposing of the media. It is important to remember that a network based system would also have some increased risks and would require coordinating patient ID numbers. The hope would be to inexpensively build an open system that would enable participation of hospitals making referrals even only once a month. It would indeed be challenging to build a system that is less expensive than the 98,300 USD a year that was calculated in Section 4.4 as the judgment criteria for determining whether the cost is too high.
6. Limitations
Although this study used all stored imaging data, the investigations of the referring hospitals in Sections 4.2 and 4.3 are based only on data from May 2012. Nevertheless, this should not present a sampling problem, as May is a representative month of the year in terms of the number of patients.
One merit that PDI has for the referred hospital is that it receives imaging study information on the patient, eliminating the need to perform unnecessary studies. However, it is impossible to calculate how many unnecessary studies were avoided or the economic benefits of doing so. In addition to a discussion of cost-effectiveness, further discussions are needed to determine a means for reducing costs. No assessment has yet been made of online PDI or other alternative systems.
7. Conclusion
Image sharing by PDI media is becoming a widespread practice. Having all images from PDI media brought in by patients stored to the PACS has resulted in imported images making up 22.8% of all images stored on the PACS at the YCU hospital. In upcoming years, hospitals currently incurring only a small burden from the handling of PDI will likely fall into the same trap as the hospital described in this study. The expenditure related to handling PDI media cannot be avoided by hospitals. There is some debate over whether that expenditure is small or large, because it is difficult to assess the benefits of PDI media.
The YCU hospital is associated with a large number of medical institutions distributed over a wide geographic range, a situation that is similar for many university and core hospitals. To switch from a PDI media based system to a network based system, a system must be built that is both inexpensive and easy for many hospitals to join. The results of this study show that 184 hospitals are currently connected and the annual expenditure associated with PDI can be estimated to be 98,300 USD. These results may be useful criteria for evaluating the costs of building a better system.
Footnotes
Clinical Relevance Statement
The rising expenses of PDI management are a problem. Development of a more practical system than PDI to share medical imaging will reduce these costs and improve patient care and health outcomes.
Conflict Of Interest
The authors declare that they have no conflicts of interest in the research.
Human Subjects Protections
The study was approved by the Yokohama City University Hospital Review Board.
References
- 1.Portable Data for Imaging [Internet]. [Cited 2013 June 30]. Available fromhttp://wiki.ihe.net/index.php?title=Portable_Data_for_Imaging [Google Scholar]
- 2.Macura KJ, Carrino JA, Kahn CE., JrReviewing images from portable media: An ongoing challenge. Journal of the American College of Radiology 2009; 6(1: 61–64 [DOI] [PubMed] [Google Scholar]
- 3.Jung H, Kang W, Kim J, Yang K, Han D, Kim H.Interoperability validation of DICOM portable data for imaging in nuclear medicine. Med Phys 2005; 32(6): 1915 [Google Scholar]
- 4.van Ooijen PMA, Guignot J, Mevel G, Oudkerk M.Incorporating out-patient data from CD-R into the local PACS using DICOM worklist features. J Digit Imaging 2005; 18(3): 196–202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuzmak PM, Dayhoff RE, Gavrilov S, Cebelinski G, Shovestul ML, Casertano A.Streamlining importation of outside prior DICOM studies into an imaging system. J Digit Imaging 2012; 25(1): 70–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee J, Zhang J, Park R, Dagliyan G, Liu B, Huang HK.A DICOM-based 2nd generation molecular imaging data grid implementing the IHE XDS-i integration profile. Int J Comput Assist Radiol Surg 2012; 7(4): 533–545 [DOI] [PubMed] [Google Scholar]
- 7.Fernandez-Bayo J.IHE profiles applied to regional PACS. Eur J Radiol 2011; 78(2): 250–252 [DOI] [PubMed] [Google Scholar]
- 8.Koutelakis GV, Lymberopoulos DK.WADA service: An extension of DICOM WADO service. IEEE Trans Inf Technol Biomed 2009; 13(1): 121–130 [DOI] [PubMed] [Google Scholar]
- 9.Kimura M, et al. SS-MIX: A ministry project to promote standardized healthcare information exchange. Method Inform Med 2011; 50(2): 131–139 [DOI] [PubMed] [Google Scholar]
- 10.Noumeir R, Renaud B.IHE Cross-enterprise document sharing for imaging: Interoperability testing software. Source Code Biol Med 2010; 5: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mendelson DS, Bak PRG, Menschik E, Siegel E.Informatics in radiology image exchange: IHE and the evolution of image sharing. Radiographics 2008; 28(7): 1817–1833 [DOI] [PubMed] [Google Scholar]
- 12.Noumeir R.Sharing Medical Records: The XDS architecture and communication infrastructure. It Prof 2011; 13(4): 46–51 PubMed PMID: ISI:000304342900011 [Google Scholar]
- 13.Zhang JG, et al. Grid-based implementation of XDS-I as part of image-enabled EHR for regional healthcare in Shanghai. Int J Comput Ass Rad 2011; 6(2): 273–284 [DOI] [PubMed] [Google Scholar]


