Summary
Objective
Based on US. Centers for Disease Control and Prevention recommendations, New York State enacted legislation in 2010 requiring healthcare providers to offer non-targeted human immunodeficiency virus (HIV) testing to all patients aged 13–64. Three New York City adult emergency departments implemented an electronic alert that required clinicians to document whether an HIV test was offered before discharging a patient. The purpose of this study was to assess the impact of the electronic alert on HIV testing rates and diagnosis of HIV positive individuals.
Methods
During the pre-intervention period (2.5–4 months), an electronic “HIV Testing” order set was available for clinicians to order a test or document a reason for not offering the test (e.g., patient is not conscious). An electronic alert was then added to enforce completion of the order set, effectively preventing ED discharge until an HIV test was offered to the patient. We analyzed data from 79,786 visits, measuring HIV testing and detection rates during the pre-intervention period and during the six months following the implementation of the alert.
Results
The percentage of visits where an HIV test was performed increased from 5.4% in the preintervention period to 8.7% (p<0.001) after the electronic alert. After the implementation of the electronic alert, there was a 61% increase in HIV tests performed per visit. However, the percentage of patients testing positive per total patients-tested was slightly lower in the post-intervention group than the pre-intervention group (0.48% vs. 0.55%), but this was not significant. The number of patients-testing positive per total-patient visit was higher in the post-intervention group (0.04% vs. 0.03%).
Conclusions
An electronic alert which enforced non-targeted screening was effective at increasing HIV testing rates but did not significantly increase the detection of persons living with HIV. The impact of this electronic alert on healthcare costs and quality of care merits further examination.
Key words: HIV testing, electronic alert, electronic order set, screening test
Introduction
The human immunodeficiency virus (HIV) epidemic continues to exact a huge toll on the United States (US) population. Despite increasingly intensive public health efforts, about 20% of HIV-positive individuals (i.e., approximately 200,000) are unaware of their HIV status, because most Americans have never been tested for HIV and are not aware that they are at-risk for the disease [1, 2]. An important approach to controlling the HIV epidemic is early identification, since late diagnosis results in increased potential for transmission and delays life-saving treatment [3]. Early diagnosis of the disease, through HIV testing, is vital to avoid increased transmission, and link patients to care, resulting in decreased morbidity and mortality [4].
The National HIV/AIDS Strategy has established a goal of increasing the awareness of HIV status in the US population from 79% to 90% by 2015 [5]. In recent years, several initiatives have sought to increase the number of persons who know their HIV status. In 2006, the U.S. Centers for Disease Control and Prevention (CDC) began recommending non-targeted HIV testing to be offered in healthcare delivery settings unless the prevalence of new HIV diagnoses is less than 0.1% [6]. In response to the CDC recommendation, New York State enacted legislation in 2010 mandating that HIV testing be offered to all persons between the ages of 13 and 64 seeking healthcare services in all settings, including primary care and specialty care practices, emergency departments (EDs), and in-patient hospital facilities [7]. Expanding HIV testing in the ED is especially important [8, 9] because those who use the ED for primary care services are most likely to be affected by HIV/AIDS [10]. Implementing non-targeted HIV screening in the ED setting, however, presents operational and financial challenges, particularly in urban environments where EDs are often overcrowded [11–17] and understaffed [18–20]. To further complicate these challenges, there is no public funding to support the New York State HIV testing legislation.
Electronic alerts are a common type of decision support for clinicians at the point of care [21]. However, the costs and benefits of such tools are coming under increased scrutiny. A recent study reported on the use of computer-facilitated HIV testing which was reported to be acceptable to ED patients but did not assess the impact of this tool on HIV testing rates and the detection of persons living with HIV [22]. In another study, a clinical informatics tool was developed to determine which ED patients are eligible for HIV screening. Findings from this study demonstrated that clinical informatics tools can be used to increase program efficiency and accelerate the integration of HIV screening into clinical practice in an ED universal HIV screening program [23]. These recent studies shed light onto the usefulness of informatics tools for improving the HIV testing process in the ED but further research is needed to understand how these tools impact the detection of persons living with HIV. The goal of this study was to measure the effectiveness of an electronic alert on HIV testing rates and diagnosis of HIV-positive individuals in the adult ED.
Methods
Study Setting
The study was conducted at three adult EDs in New York City. All three sites were part of the same hospital network and are private not-for-profit institutions. Site 1 is a community hospital associated with a major academic medical center and had an annual ED volume of 41,000 patients. Sites 1 and 2 have overlapping geographic areas served. Site 2 was a New York State-designated AIDS Center, with an annual ED volume of 79,000 patients. Designated AIDS Center (DACs) are state-certified, hospital-based programs that provide multi-disciplinary inpatient and outpatient care coordinated through hospital-based case management and there are 41 throughout New York State. The prevalence of persons living with HIV in the 5 zip codes most closely bordering sites 1 and 2 is 16.79 per 1,000 persons in 2011 [24, 25]. Sites 2 and 3 are tertiary care academic medical centers Site 2 is a level one trauma center for pediatrics. Site 3 is a level one trauma center for adult and pediatrics and was also a DAC with annual ED volume of 67,000 Adult patients [26]. This site has 4 neighboring zip codes with a total prevalence of 16.77 per 1,000 persons living with HIV in 2011 [25]. Notably the prevalence of persons living with HIV in the catchment area of site 3 is slightly lower than in the other two sites.
Intervention
In order to comply with the New York State HIV testing legislation, all three sites deployed an electronic “HIV Testing” order set and an electronic alert to ensure that an HIV test was offered to every patient discharged from the ED. Patients were offered to be given an HIV test which was billed to their medical insurance. In the case of patients who were uninsured, the hospital paid for the testing. We defined two study periods:
pre-intervention, HIV Testing order set available without an electronic alert; and
post-intervention, HIV Testing order set available and electronic alert enabled.
During the pre-intervention period, clinicians could access the HIV Testing order set (▶ Figure 1), but there was no electronic alert. The HIV Testing order set included three options:
Fig. 1.
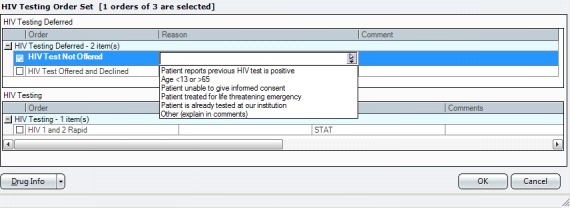
Electronic HIV Testing Order Set
order a rapid HIV test,
document that HIV testing was offered but declined by the patient, and
document that HIV testing was not offered (a reason was required if option 3 was selected – for example, “Patient is known HIV-positive”).
The time period when the HIV Testing order set was live, but no alert occurred, was defined as the pre-intervention period. At sites 1 and 2, this duration was four months; at site 3, the duration was two and a half months. The pre-intervention time period was determined by hospital and ED administration as the time that was necessary to introduce the new clinical process and documentation to the staff at each site.
During the post-intervention period, the electronic alert was implemented to enforce the HIV testing policy. An electronic alert was added to ensure that providers, including attending physicians, resident physicians, physician assistants, or nurse practitioners, offered HIV testing to patients and completed the HIV Testing order set. An electronic alert was used because it was a relatively inexpensive method for implementing a necessary clinical action for almost every patient visit in the ED. The alert appeared when a clinician electronically placed the “ED Discharge Order,” at the end of the patient visit, if the HIV Testing order set was not previously completed during the ED visit. The alert appears at the same time in all three sites. The alert prevented the clinician from continuing with the discharge order until the HIV Testing order set was completed. The post-intervention time period was six months after the introduction of the electronic alert at each site. We chose six months as a convenience sample of data which was available at the time that we analyzed our data. We chose an equal period of time for our post-intervention data across sites.
Measurements
Institutional Review Board (IRB) approval was obtained prior to conducting the study. We analyzed data from the electronic health record system used across all three EDs, (Sunrise Emergency Care, Allscripts Corporation, Chicago, IL) to understand the effect of the implementation of the HIV testing electronic alert on testing rates and detection of persons living with HIV. We obtained de-identified patient visit information for treat-and-release patients at the three EDs before and after the implementation of the electronic alert. The visit information included patient age, sex, whether blood work was ordered, and emergency severity index (ESI). ESI is categorized on 5 levels: 1-resuscitation, 2-emergent, 3-urgent, 4-less urgent, 5-non-urgent [27]. We included only treat-and-release patients, who are patients who were seen in the ED and then discharged without being admitted to the hospital. We only included treat-and-release patients in our study for three reasons:
these patients constituted the vast majority of ED visits,
patients who were admitted frequently had HIV testing performed during their inpatient stay, and
at the time of the study, the electronic alert was active only for treat-and-release patients.
Patient insurance information was not available in our data set. Race and ethnicity were not included in this study because this information was classified as “Unknown” or “Other” for more than half of the patients. We excluded patients over 64 years of age since this population was not included in the New York State HIV screening legislation. We only assessed adult EDs, since the testing process was different in the institution’s pediatric and psychiatric EDs.
Two outcome measures were used to determine the impact of the HIV testing electronic alert: overall HIV testing rate, and the detection rate of HIV-positive patients. Overall HIV testing rate was defined as the total number of HIV tests completed divided by the total number of patient visits. Detection of HIV-positive patients was determined by the number of HIV positive patients divided by the total number of patients tested.
Data Analysis
Data were managed and analyzed using IBM SPSS Statistics, release 20.0 (IBM Corp., Chicago, IL). Descriptive statistics were used to characterize patient demographics, HIV testing rates, and the percentage of persons who were diagnosed with HIV. Results are presented as frequencies with proportions. We used logistic regression to assess the effect of implementation of this electronic alert on the completion of the HIV Testing order set and testing a patient for HIV among all of the patients. We also analyzed the predictors of testing positive among the 6,279 patients who were tested for HIV to suggest further research on targeted HIV screening. Adjusted logistic regression models included the following covariates: ED site, patient age, patient sex, orders for other blood work, and ESI. Odds ratios are presented with 95% confidence intervals (CIs).
Results
A total of 79,786 patient records were examined. Mean age of patients was 39.1 years (S.D. = 12.7). Additional patient demographics are reported in ▶ Table 1. During the pre-intervention period, there were a total of 29,993 visits at the three study sites. During the six-month post-intervention period, 49,793 patient visits were analyzed. Clinicians completed the HIV Testing order set for 32.2% of patients during the pre-intervention period and for 100% of patients during the post-intervention period. In the post-intervention period, 100% of patients were offered the test because clinicians has no choice but to complete the order set if they wanted to proceed with discharging the patient. Across all three sites, patients in the post-intervention group were tested for HIV at a significantly higher rate than patients in the pre-intervention group (OR = 1.66; 95% CI, 1.57–1.77; p<0.001) (▶ Table 2). There were a total of 30 patients who tested positive for HIV during the entire study period, 9 patients in the pre-intervention group and 21 patients in the post-intervention group. Of the 30 patients who tested positive, 20 were male.
Table 1.
Patient Demographics
| Total N (%) | Site 1 | Site 2 | Site 3 | |
|---|---|---|---|---|
| Variable | 79,786 | 19,601 (24.6) | 35,916 | 24,269 |
| Gender | ||||
| Male | 34,472 (43.2) | 7,602 (38.8) | 16,140 (44.9) | 10,730 (44.2) |
| Blood Work other than the HIV test | ||||
| Yes | 29,650 (37.2) | 6,768 (34.5) | 13,484 (37.5) | 9,398 (38.7) |
| Emergency Severity Index (ESI) | ||||
| 1-resuscitation | 56 (0.1) | 4 (0.02) | 44(0.1) | 8 (0.03) |
| 2-emergent | 6,495 (8.1) | 571 (2.9) | 5,359 (14.9) | 565 (2.3) |
| 3-urgent | 46,699 (58.5) | 10,324 (52.7) | 22,813 (63.5) | 13,562 (55.9) |
| 4-less urgent | 24,064 (30.2) | 7,989 (40.8) | 7,073 (19.7) | 9,002 (37.1) |
| 5-non-urgent | 2,472 (3.1) | 713 (3.6) | 627 (1.7) | 1,132 (4.7) |
Table 2.
Number of Each HIV testing Order and Percentage of Patients Tested and HIV Positive
| Group 1 Pre-intervention (N = 29,993) |
Group 2 Post-Intervention (N= 49,786) |
||
|---|---|---|---|
| Site 1 | |||
| HIV Testing Order Set Completed | 5,709 | 11,170 | |
| • HIV Test Ordered | 470 | 788 | |
| - Positive | 2 | 1 | |
| - Negative | 468 | 787 | |
| • Total Patient Visits | 8435 | 11183 | |
| % Tested | 5.57 | 7.05 | |
| % Positive of Total Tested | 0.43 | 0.13 | |
| % Positive of Total Visits | 0.024 | 0.009 | |
| Site 2 | |||
| HIV Testing Order Set Completed | 3,699 | 21,145 | |
| • HIV Test Ordered | 1042 | 2304 | |
| - Positive | 7 | 15 | |
| - Negative | 945 | 2061 | |
| • Total Patient Visits | 14782 | 21172 | |
| % Tested | 7.05 | 10.88 | |
| % Positive of Total Tested | 0.67 | 0.65 | |
| % Positive of Total Visits | 0.047 | 0.071 | |
| Site 3 | |||
| HIV Testing Order Set Completed | 447 | 17,478 | |
| • HIV Test Ordered | 119 | 1261 | |
| - Positive | 0 | 5 | |
| - Negative | 119 | 1256 | |
| • Total Patient Visits | 6811 | 17521 | |
| % Tested | 1.75 | 7.20 | |
| % Positive of Total Tested | 0.00 | 0.40 | |
| % Positive of Total Visits | 0.00 | 0.03 | |
| All Sites | |||
| HIV Testing Order Set Completed | 9,676 | 49,786 | |
| • HIV Test Ordered | 1631 | 4353 | |
| - Positive | 9 | 21 | |
| - Negative | 1532 | 4104 | |
| % Tested | 5.43 | 8.73 | |
| % Positive of Total Tested | 0.55 | 0.48 | |
| % Positive of Total Visits | 0.030 | 0.042 | |
The percentage of patients-testing-positive per total-patients-tested was lower in the post-intervention group than the pre-intervention group (0.48% vs. 0.55%) p = 0.89. The number of patients-testing-positive per total-patient-visits was higher in the post-intervention group (0.04% than the pre-intervention group (0.03%), p = 0.50. The percentages are very similar in the pre-intervention and post-intervention groups and the differences are not significant.
Predictors of Ordering an HIV test
Clinicians were more likely to order an HIV test during the post-intervention period compared to the pre-intervention period (OR = 1.41; 95% CI, 1.33–1.49; p<0.001). Patients at site 1 (OR = 1.18; 95% CI, 1.09–1.28; p<0.001) and site 2 (OR = 1.92; 95% CI, 1.79–2.05; p<0.001) were more likely to agree to be tested for HIV than patients at site 3 (▶ Table 3). ESI was a significant covariate in our model (p<0.001), and lower-severity patients were more likely to be tested for HIV. Younger age had a small effect on testing rates (OR = 0.98; 95% CI, 0.97–0.98; p<0.001). Patients who had other blood work during their ED visit were more likely to be tested for HIV (OR = 1.45; 95% CI, 1.36–1.54; p<0.001). Patient sex was not a significant covariate in this model.
Table 3.
Odds ratios of gender, location, other blood work and severity index related to ordering an HIV test
| Variable | Odds ratio | 95% Confidence interval |
p value |
|---|---|---|---|
| Gender | |||
| Female (reference) | 1.00 | 0.06 | |
| Male | 1.06 | 1.00, 1.11 | |
| Location | |||
| Site 1 | 1.18b | 1.09, 1.28 | <0.001 |
| Site 2 | 1.92b | 1.79, 2.05 | |
| Site 3 (reference) | 1.00 | ||
| Other Blood Work | |||
| No (reference) | 1.00 | <0.001 | |
| Yes | 1.45b | 1.36, 1.54 | |
| ESI | |||
| 1-resuscitation | 0.13a | 0.02, 0.96 | <0.001 |
| 2-emergent | 0.56b | 0.46, 0.68 | |
| 3-urgent | 0.85a | 0.72, 1.00 | |
| 4-less urgent | 1.02 | 0.87, 1.20 | |
| 5-non-urgent (reference) | 1.00 | ||
aStatistically significant at 0.05 level
bStatistically significant at 0.001 level
Predictors of Detecting HIV-Positive Patients
Among patients who were tested for HIV, there was no significant difference in detection of HIV-positive patients between the pre- and post-intervention periods (p = 0.549). Site (p = 0.183), age (p = 0.716), ESI (p = 0.666) and other blood work (p = 0.202) were not significant covariates in this model. Sex was a significant covariate; of the patients who were tested, males were more likely to be HIV-positive than females (OR = 2.63; 95% CI, 1.22–5.68; p = 0.014).
Discussion
After implementing the electronic alert, we observed a significant increase in the rate of HIV tests performed (5.4% across all sites during the pre-intervention period, increasing to 8.7% during the post-intervention period). Interestingly, even the pre-intervention testing rate was much higher than rates reported in the 2009 National Hospital Ambulatory Medical Care Survey (NHAMCS) [28]. This survey demonstrated that nationwide, overall HIV testing rates in the ED for patients aged 13–64 was only 0.2%. Among patients with increased risk for HIV and other sexually transmitted diseases or pregnancy, only 2.3% were tested for HIV [28]. Since the HIV testing rates in the pre-intervention group were already higher than the national testing rates, an electronic order set without an electronic alert may be more appropriate, targeted and cost-effective than an electronic alert at detecting new cases of HIV in the ED. An interruptive hard stop alert that forces 100% completion may invite providers to complete the order set without actually offering the HIV test.
Our results suggest that there are limits to the effectiveness of an electronic alert for implementing universal non-targeted HIV screening in the ED. While the overall detection of HIV-positive persons increased with an increase in testing rates, the rate of detection of HIV-positive patients per-patient-tested decreased. The patients in the post-intervention group who were tested for HIV were not significantly more likely to be diagnosed with HIV than patients in the pre-intervention group, despite higher testing rates in this group. This finding suggests that the rate of HIV detection does not linearly increase with increased screening.
In a similar study to ours, Avery et al. implemented an electronic reminder to alert providers to the absence of an HIV test among all patients’ ages 13–64 years old in the primary care setting [29]. In that study after the implementation of HIV testing reminders, first-time HIV testing increased significantly for both men and women 18–64 years old, resulting in a significant reduction in missed opportunities. While Avery and colleagues did not assess whether there was an increase in detection of persons living with HIV, our study found similar results in the ED setting with respect to increases in testing. Additional research is warranted to understand whether use of an electronic alert for implementing non-targeted HIV screening in the ED is cost-effective, which would inform future policy decisions. In the case of this legislation, the State did not provide any financial support and so the cost burden of the increased staffing and changes to the electronic health record were assumed by the hospital system. Although previous studies have demonstrated the cost-effectiveness of performing routine non-targeted HIV screening [4, 30], further examination of our results using a cost-effectiveness analysis could provide evidence as to whether targeted screening would be more effective.
ESI and patients having other blood work were significant predictors of a patient agreeing to be tested for HIV. Lower-severity patients and patients who were already having blood work performed were more likely to be tested for HIV. This is not surprising, since additional testing fits conveniently within clinicians’ workflow and is less burdensome to patients. Site was a significant covariate in our models.
While the HIV Testing Order Set was completed more than three times as often in the post-intervention period, there were only 1.4 times as many HIV tests. One explanation for this change is that an alert at time of discharge does not fit neatly within the clinicians’ workflow. There was concern among providers that having an electronic alert earlier in the workflow may interrupt necessary and emergent care and so the hospital and ED administration decided to place the alert at the end of the visit. Because the alert now appears at the end of the patient visit , this may have reduced the likelihood that the HIV test was actually performed. Since drawing of other blood increased the chance of performing an HIV test, it is important to consider moving the alert earlier in the workflow. If an alert triggers at the time when clinicians are ordering other blood work, this may increase the likelihood of ordering an HIV test.
Patients at sites 1 and 2 were more likely to agree to be tested for HIV than at site 3. This difference may be the result of higher prevalence of HIV in the catchment area of sites 1 and 2 than site 3 [31]. Alternatively, providers may have been more persuasive in offering the HIV test at these sites because the prevalence of the disease is higher in these areas. Patient sex was a significant predictor of detecting HIV, and of those patients tested, males were more likely to be HIV-positive. Since the incidence of HIV is much higher in men than women, and men are more likely to become newly infected with HIV, these findings are consistent with the current epidemiology of the disease [32]. Gay and bisexual men remain the population most heavily affected by HIV in the US with estimates that they represent approximately 2% percent of the U.S. population, but accounted for the majority of all new HIV infections annually from 2006 to 2009— 56% in 2006 (27,000), 58% in 2007 (32,300), 56% in 2008 (26,900) and 61% in 2009 (29,300) [33].
Particular attention should be focused on the effect of non-targeted HIV screening on ED congestion and staffing [20, 34]. ED crowding is a growing national crisis and is associated with workflow challenges [13–15]. Lack of clinician time is a commonly cited barrier to implementing initiatives like HIV testing; it is likely one of the major challenges in complying with the current legislative mandate in New York State [35]. In past studies, ED physicians reported spending less than ten minutes with each patient, illustrating the complexity of implementing mandatory non-targeted HIV testing [36]. Future research should consider the effect of this legislation on patient outcomes and quality of care.
Limitations
There were limitations to our study. First, factors such as staffing level or provider type information were not available for our analysis and this may have an effect on testing rates. Second, the number of patient visits differed considerably between sites. In the multivariable model, we controlled for these differences but were not able to control for ED congestion, which could be an important co-variate. Third, the geographic setting limits the generalizability of the findings – our study was conducted in three busy urban EDs which may vary greatly from rural and less-congested environments.
Finally, our unit of analysis was the patient visit and so we may have had patients in our study sample that had repeat visits to the same ED. At the time of our study, even if a patient had been previously tested, the provider would still receive an HIV Testing electronic alert before discharging a patient. The alert has been revised since our study period to only require a provider to offer the HIV test if a patient does not have documentation of an HIV test in the past 12 months.
In conclusion, the patients in the post-intervention group who were tested for HIV were not significantly more likely to be diagnosed with HIV than patients in the pre-intervention group, despite higher testing rates in this group. This finding suggests that the rate of HIV detection does not linearly increase with increased screening. An electronic alert which enforced non-targeted screening was effective at increasing HIV testing rates but did not significantly increase the detection of persons living with HIV. The impact of this electronic alert on healthcare costs and quality of care merits further examination.
Fig. 2.
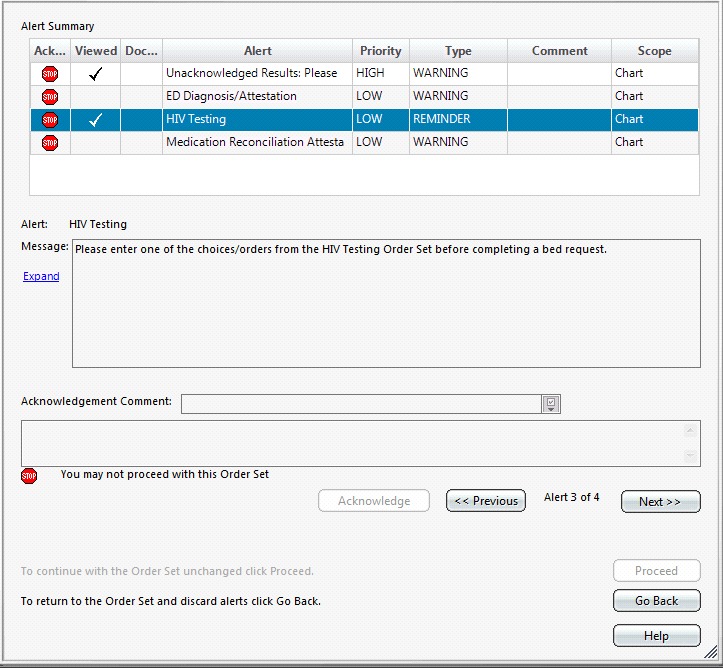
HIV Testing Alert
Acknowledgements
This work was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number KL2 TR000081, formerly the National Center for Research Resources, Grant Number KL2 RR024157. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflicts Of Interest
None of the listed authors have any financial or personal relationships with other people or organizations that may inappropriately influence or bias the objectivity of submitted content and/or its acceptance for publication in this journal.
Protection of Human Subjects and Animals in Research
The procedures used have been reviewed in compliance with ethical standards of the responsible committee on human experimentation at the home institution of the authors. All research activities are in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects.
References
- 1.CDC US HIV/AIDS Surveillance Report, 2007. Atlanta: Centers for Disease Control and Prevention, 2009 [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) HIV and AIDS in the United States 2011. Available from:http://www.cdc.gov/hiv/resources/factsheets/us.htm [Google Scholar]
- 3.Schackman BR, et al. Cost-effectiveness implications of the timing of antiretroviral therapy in HIV-infected adults. Arch Intern Med. 2002; 162(21): 2478–2486 doi: ioi10799 [pii]. PubMed PMID: 12437408 [DOI] [PubMed] [Google Scholar]
- 4.Paltiel AD, et al. Expanded screening for HIV in the United States--an analysis of cost-effectiveness. N Engl J Med 2005; 352(6): 586–595 doi: 352/6/586 [pii] 10.1056/NEJMsa042088. PubMed PMID: 15703423 [DOI] [PubMed] [Google Scholar]
- 5.The White House Office of National AIDS Policy National HIV/AIDS Strategy for the United States. 2010 [Google Scholar]
- 6.Branson BM, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep 2006; 55(RR-14): 1–17; quiz CE1–4. doi: rr5514a1 [pii]. PubMed PMID: 16988643 [PubMed] [Google Scholar]
- 7.New York State Department of Health Frequently Asked Questions regarding the HIV Testing Law Albany, NY2012. Available from:http://www.health.ny.gov/diseases/aids/testing/law/faqs.htm [Google Scholar]
- 8.Bernstein SL, Haukoos JS.Public health, prevention, and emergency medicine: a critical juxtaposition. Acad Emerg Med 2008; 15(2): 190–193 Epub 2008/02/16. doi: ACEM055 [pii] 10.1111/j.1553–2712.2008.00055.x. PubMed PMID: 18275450 [DOI] [PubMed] [Google Scholar]
- 9.Rothman RE, Lyons MS, Haukoos JS.Uncovering HIV infection in the emergency department: a broader perspective. Acad Emerg Med 2007; 14(7): 653–657 Epub 2007/06/01. doi: j.aem.2007.04.004 [pii] 10.1197/j.aem.2007.04.004. PubMed PMID: 17538079 [DOI] [PubMed] [Google Scholar]
- 10.Hall HI, et al. Estimation of HIV incidence in the United States. JAMA 2008; 300(5): 520–529 doi: 10.1001/jama.300.5.520. PubMed PMID: 18677024; PubMed Central PMCID: PMC2919237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Derlet RW, Richards JR.Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Annals of emergency medicine 2000; 35(1): 63–68 PubMed PMID: 10613941 [DOI] [PubMed] [Google Scholar]
- 12.Asplin BR, et al. A conceptual model of emergency department crowding. Annals of emergency medicine 2003; 42(2): 173–180 Epub 2003/07/29. doi: 10.1067/mem.2003.302 S019606440300444X [pii]. PubMed PMID: 12883504 [DOI] [PubMed] [Google Scholar]
- 13.Olshaker JS, Rathlev NK.Emergency Department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the Emergency Department. J Emerg Med 2006; 30(3): 351–356 Epub 2006/05/09. doi: S0736–4679(05)00442–7 [pii] 10.1016/j.jemermed.2005.05.023. PubMed PMID: 16677993 [DOI] [PubMed] [Google Scholar]
- 14.Moskop JC, et al. Emergency department crowding, part 1 - concept, causes, and moral consequences. Annals of emergency medicine 2009; 53(5): 605–611 Epub 2008/11/26. doi: S0196–0644(08)01783–6 [pii] 10.1016/j.annemergmed.2008.09.019. PubMed PMID: 19027193 [DOI] [PubMed] [Google Scholar]
- 15.Olshaker JS.Managing emergency department overcrowding. Emerg Med Clin North Am 2009; 27(4): 593–603, viii. doi: S0733–8627(09)00071–6 [pii] 10.1016/j.emc.2009.07.004. PubMed PMID: 19932394 [DOI] [PubMed] [Google Scholar]
- 16.Pines JM, et al. International perspectives on emergency department crowding. Acad Emerg Med 2011; 18(12): 1358–1370 doi: 10.1111/j.1553–2712.2011.01235.x. PubMed PMID: 22168200 [DOI] [PubMed] [Google Scholar]
- 17.Schnall R, Clark S, Olender S, Sperling JD.Providers’ Perceptions of the Factors Influencing the Implementation of the New York State Mandatory HIV Testing Law in Two Urban Academic Emergency Departments. Acad Emerg Med 2013; 20(3): 279–286 doi: 10.1111/acem.12084. PubMed PMID: 23517260; PubMed Central PMCID: PMC3608143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Office. USGA. Hospital emergency departments crowded conditions vary among hospitals and communities, report to the ranking minority member, Committee on Finance, U.S. Senate. 2003. 2003 [Google Scholar]
- 19.Derlet R, Richards J, Kravitz R.Frequent overcrowding in U.S. emergency departments. Acad Emerg Med 2001; 8(2): 151–155 PubMed PMID: 11157291 [DOI] [PubMed] [Google Scholar]
- 20.Green LV, Soares J, Giglio JF, Green RA.Using queueing theory to increase the effectiveness of emergency department provider staffing. Acad Emerg Med 2006; 13(1): 61–68 doi: j.aem.2005.07.034 [pii] 10.1197/j.aem.2005.07.034. PubMed PMID: 16365329 [DOI] [PubMed] [Google Scholar]
- 21.Schedlbauer A, et al. What evidence supports the use of computerized alerts and prompts to improve clinicians’ prescribing behavior? J Am Med Inform Assoc 2009; 16(4): 531–538 doi: 10.1197/jamia.M2910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kurth AE, Severynen A, Spielberg F.Addressing Unmet Need for HIV Testing in Emergency Care Settings: A Role for Computer-Facilitated Rapid HIV Testing? AIDS Educ Prev 2013; 25(4): 287–301 doi: 10.1521/aeap.2013.25.4.287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilbur L, Huffman G, Lofton S, Finnell JT.The use of a computer reminder system in an emergency department universal HIV screening program. Annals of emergency medicine 2011; 58(1): S71–S3.e1 [DOI] [PubMed] [Google Scholar]
- 24.New York City Department of Health and Mental Hygiene Reported HIV/AIDS Diagnoses and Deaths in 2011 2011. Available from:http://www.nyc.gov/html/doh/html/data/hivtables.shtml [Google Scholar]
- 25.United Hospital Fund United Hospital Fund Zip Codes 2013. Available from:http://www.nyc.gov/html/doh/html/data/hivtables.shtml [Google Scholar]
- 26.New York State Department of Health New York State Hospital Profile 2012. Available from:http://hospitals.nyhealth.gov/index.php?PHPSESSID=ea42335cd805a2277728fc403e9a5a1f [Google Scholar]
- 27.Singer RF, et al. The use of and satisfaction with the Emergency Severity Index. Journal of emergency nursing: JEN: official publication of the Emergency Department Nurses Association 2012; 38(2): 120–126. 10.1016/j.jen.2010.07.004. PubMed PMID 22401616. [DOI] [PubMed] [Google Scholar]
- 28.Hoover JB, Tao G, Heffelfinger JD.Monitoring HIV testing at visits to emergency departments in the United States: very-low rate of HIV testing. Journal of acquired immune deficiency syndromes 2013; 62(1): 90–94 doi: 10.1097/QAI.0b013e3182742933. PubMed PMID: 23018376 [DOI] [PubMed] [Google Scholar]
- 29.Avery A, Toro M, Einstadter D.Decreasing Missed Opportunities for HIV Testing in Primary Care through Enhanced Utilization of the Electronic Medical Record. J AIDS Clinic Res 2012; S4(006). doi: 10.4172/2155–6113.S4–006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sanders GD, et al. Cost-effectiveness of screening for HIV in the era of highly active antiretroviral therapy. N Engl J Med 2005; 352(6): 570–585 doi: 352/6/570 [pii] 10.1056/NEJMsa042657. PubMed PMID: 15703422 [DOI] [PubMed] [Google Scholar]
- 31.New York City Department of Health and Mental Hygiene Epiquery: NYC Interactive Health Data System 2012. Available from:http://nyc.gov/health/epiquery [Google Scholar]
- 32.The Kaiser Family Foundation Golbal data on HIV/AIDS, TB, Malaria & more 2010. Available from:http://www.globalhealthfacts.org/data/factsheet/factsheet.aspx?loc=221&ind=1,2,3,4,5,6,7,8,9,10,11 [Google Scholar]
- 33.Center for Disease Control. Estimates of New HIV Infections in the United States, 2006–2009 Atlanta, GA: Center for Disease Control and Prevention, 2011 [Google Scholar]
- 34.Hospital-Based Emergency Care: At the Breaking Point: The National Academies Press; 2007 [Google Scholar]
- 35.Demarco RF, et al. Recommendations and reality: Perceived patient, provider, and policy barriers to implementing routine HIV screening and proposed solutions. Nurs Outlook 2012; 60(2): 72–80 doi: S0029–6554(11)00215–6 [pii] 10.1016/j.outlook.2011.06.002. PubMed PMID: 21840554 [DOI] [PubMed] [Google Scholar]
- 36.Rothman RE.Current Centers for Disease Control and Prevention guidelines for HIV counseling, testing, and referral: critical role of and a call to action for emergency physicians. Annals of emergency medicine 2004; 44(1): 31–42 doi: 10.1016/S0196064404000678 S0196064404000678 [pii]. PubMed PMID: 15226706 [DOI] [PubMed] [Google Scholar]


