Abstract
Background and objectives
Elderly patients require tunneled central vein dialysis catheters more often than younger patients. Little is known about the risk of catheter-related bloodstream infection in this population.
Design, setting, participants, & measurements
This study identified 464 patients on hemodialysis with tunneled central vein dialysis catheters between 2005 and 2007 and excluded patients who accrued <21 catheter-days during this period. Outpatient and inpatient catheter-related bloodstream infection data were collected. A Cox proportional hazards regression analysis adjusting for sex, ancestry, comorbidites, dialysis vintage, dialysis unit, immunosuppression, initial catheter site, and first antimicrobial catheter lock solution was performed for risk of catheter-related bloodstream infection between nonelderly (18–74 years) and elderly (≥75 years) patients.
Results
In total, 374 nonelderly and 90 elderly patients with mean (SD) ages of 54.8 (12.3) and 81.3 (4.9) years and dialysis vintages of 1.8 (3.3) and 1.5 (2.9) years (P=0.47), respectively, were identified. Mean at-risk catheter-days were 272 (243) in nonelderly and 318 (240) in elderly patients. Between age groups, there were no significant differences in initial catheter site, type of catheter lock solution, or microbiology results. A total of 208 catheter-related bloodstream infection events occurred (190 events in nonelderly and 18 events in elderly patients), with a catheter-related bloodstream infection incidence per 1000 catheter-days of 1.97 (4.6) in nonelderly and 0.55 (1.6) in elderly patients (P<0.001). Relative to nonelderly patients, the hazard ratio for catheter-related bloodstream infection in the elderly was 0.33 (95% confidence interval, 0.20 to 0.55; P<0.001) after multivariate analysis.
Conclusion
Elderly patients on hemodialysis using tunneled central vein dialysis catheters are at lower risk of catheter-related bloodstream infection than their younger counterparts. For some elderly patients, tunneled central vein dialysis catheters may represent a suitable dialysis access option in the setting of nonmaturing arteriovenous fistulae or poorly functioning synthetic grafts.
Introduction
Caring for elderly individuals with advanced CKD or end stage kidney disease (ESKD) encompasses complex medical decisions, including the choice of optimal hemodialysis (HD) vascular access (1,2). Although avoidance of tunneled central venous dialysis catheters (TCVCs) is a major goal in all HD patients, arteriovenous fistulae (AVFs) often fail to develop and/or are not used in the elderly (3,4). Dialysis catheters are associated with systemic inflammation and catheter-related bloodstream infections (CRBSIs), which are linked to shortened dialysis survival (5–7). Nevertheless, elderly patients on dialysis represent a unique subgroup, and consideration of all potential access options should be given when presented with nonmaturing AVF or poorly functioning grafts. Knowledge of age-specific risk of CRBSIs could aid the decision-making process regarding choice of dialysis vascular access, balancing likelihood of prolonged access function with complications. In this retrospective study, the incidence of CRBSIs between elderly (age≥75 years) and young, middle-aged, and old (ages 18–74 years) patients receiving HD by means of TCVCs was compared.
Material and Methods
Study Participants
We accessed the central database of all prevalent and incident patients on HD ages≥18 years dialyzed through TCVCs at nine Wake Forest Outpatient Dialysis (WFOPD) units between January 1, 2005 and December 31, 2007. Patients with <21 catheter-days (single catheter observation or total time accrued from multiple catheters) by the end of study period were excluded. No distinction was made between acute and chronic dialysis. The computerized database provides information regarding dialysis access type in each patient and is updated whenever a new access is placed, an access is used for the first time, or catheters are removed. Age at dialysis initiation and study entry, sex, ancestry, catheter-days during the observation period, and initial allocation of the TCVC and first catheter lock solution (CLS) used at study entry were recorded. Etiology of ESKD and comorbidities (diabetes, coronary artery disease [CAD], congestive heart failure [CHF], hypertension, and peripheral vascular disease [PVD]) were abstracted from the Center for Medicare and Medicaid Services 2728 Form. All episodes of CRBSI occurring during the study period for each individual were analyzed, including outpatient infections treated at the dialysis unit and infections requiring hospitalization or diagnosed during an unrelated hospital admission. For each subject with CRBSI, we reviewed inpatient and outpatient records to assess (1) occurrence of complications related to CRBSI, such as sepsis, endocarditis, osteomyelitis, septic arthritis, or diskitis; (2) prescription of immunosuppressant drugs (e.g., prednisone, cyclosporine, tacrolimus, sirolimus, mycophenolate mofetil, azathioprine, or methotrexate); and (3) prescription of chemotherapy during the study. Place of residence for elderly patients during the study period (home, assisted living facility, or nursing home) was extracted from medical records. The initial CLS used during the study was heparin (1000 U/ml), gentamicin (GM) citrate (solution of 320 μg/ml GM in 4% sodium citrate), or normal saline (10 ml per catheter branch). At WFOPD facilities, patients receive GM citrate CLS either (1) temporarily (as treatment for CRBSI in conjunction with systemic antibiotics) or (2) on a regular basis when facing limited vascular access options or to prevent CRBSI. For this study, GM citrate was recorded as the patient’s CLS only when used in the latter fashion. Medical records for all hospitalizations were reviewed by a single investigator (K.M.J.) to consistently ascertain causes of hospitalization. Patients were censored when they reached the end of the study while dialyzing with a TCVC, when switched to an alternative access (AVF or arteriovenous graft [AVG]), at transplant, or at death with a functioning TCVC. The study was approved by the Wake Forest School of Medicine Institutional Review Board.
Measurements and Outcomes
Laboratory measurements (dialysis adequacy measured as single pool Kt/V, urea reduction ratio, serum albumin, hemoglobin, and ferritin) were extracted from routine monthly dialysis laboratory measurements predating within 30 days of the first episode of CRBSI (Meridian Laboratory Corporation, Charlotte, NC). Patients received protocol-standardized exit site care for the TCVC. Blood cultures were obtained at the outpatient dialysis unit and/or while hospitalized. Catheter-days were calculated from the date of study entry (in those patients with a TCVC placed before January 1, 2005) or the date of catheter placement (in those patients with a TCVC placed during the study period) to the date of catheter removal or censoring. In case of multiple periods of TCVC use per individual, catheter-days were summated, and the observation for CRBSI events overlapped the respective catheter-days. Based on existing WFOPD clinical practice, CRBSI was diagnosed if (1) positive blood cultures were obtained through the TCVC in the absence of an alternative source of bacteremia, (2) the patient was hospitalized for TCVC infection with bacteremia, or (3) the patient developed a fever or chills in the absence of an alternative source of infection followed by administration of intravenous antibiotics for presumed infected TCVC, with subsequent resolution of infection.
Statistical Analyses
Results are expressed as numerical values and percentages for categorical variables and mean (SD) for continuous variables. Comparisons for baseline characteristics between age groups were based on the chi-squared test for categorical data and the t test for continuous data. Age at study entry was stratified into two categories: elderly (≥75 years) and nonelderly (18–74 years). Because the catheter position and CLS varied during the observation period, we used initial catheter location and initial CLS for statistical analysis. The primary end point was age group-specific incidence of CRBSI per 1000 catheter-days. Using a multivariate Cox proportional hazards regression model and stepwise removal of other variables (sex, ancestry, comorbidities, dialysis vintage, immunosuppression, dialysis unit, initial catheter site, and initial CLS), we assessed the hazard ratio (HR) of CRBSIs for elderly compared with nonelderly (young, middle-aged, and older) patients. These variables were also analyzed separately in multivariate Cox proportional hazards regression models. Using logistic regression to fit a log-linear model using PROC GENMOD (version 9.3; SAS, Cary, NC), estimates were calculated for the HR of developing an infection for age as a continuous measure and five age groups (18–35, 36–45, 46–55, 56–65, and 66–74 years), with ≥75 years serving as the referent group. The GENMOD procedure accounted for patients who had multiple periods of catheter use. The analyses accounted for the number of infections and at-risk days observed for each participant, with P<0.05 (two-sided) denoting statistical significance. To assess the sensitivity of results, we repeated the analysis, with the outcome being documented positive blood cultures, and calculated the adjusted HR using Cox regression and the same set of variables in a multivariate model.
Results
Patients Characteristics
In total, 464 patients received HD through a TCVC at WFOPD centers between 2005 and 2007. Participants’ baseline characteristics are shown in Table 1 and comparable with those characteristics reported in the US Renal Data System (USRDS) (8). The mean (SD) age of the cohort was 59.9 (15.7) years, with dialysis vintage of 1.7 (3.2) years. There were 218 (47.0%) African Americans, 260 (56.0%) patients with diabetes, and 90 (19.4%) elderly (age≥75 years) patients; 73.3% of the elderly patients were European American, whereas only 43.8% of the nonelderly (age=18–74 years) patients were European American (Table 1) (P<0.001). GN was more commonly listed as a cause of ESKD in nonelderly patients; CAD and CHF were more prevalent in the elderly patients.
Table 1.
Baseline characteristics
| Characteristic | All | Elderly (≥75 yr) | Nonelderly (18–74 yr) | P Value |
|---|---|---|---|---|
| N (%) | 464 | 90 (19) | 374 (81) | |
| Age (yr), mean (SD) | 59.9 (15.7) | 81.3 (4.9) | 54.8 (12.3) | |
| Men, n (%) | 237 (51.0) | 44 (48.8) | 193 (51.6) | 0.64 |
| Ancestry, n (%) | ||||
| European American | 230 (49.6) | 66 (73.3) | 164 (43.8) | <0.001 |
| African American | 218 (47.0) | 24 (26.7) | 194 (51.9) | |
| Hispanic | 16 (3.4) | 0 | 16 (4.3) | |
| HD vintage (d) | ||||
| Mean (SD) | 629 (1180) | 547 (1063) | 649 (1207) | 0.47 |
| Median (25th, 75th percentiles) | 21 (21, 777) | 21 (21, 812) | 21 (21, 774) | |
| Cause of end stage kidney disease, n (%) | ||||
| Diabetes | 167 (36.0) | 32 (35.6) | 135 (36.1) | 0.92 |
| GN | 65 (14.0) | 4 (4.4) | 61 (16.3) | 0.004 |
| Hypertension-attributed | 70 (15.1) | 15 (16.7) | 55 (14.7) | 0.64 |
| AKI | 30 (6.5) | 9 (10) | 21 (5.6) | 0.13 |
| Autosomal dominant polycystic kidney disease | 8 (1.7) | 0 | 8 (2.1) | 0.16 |
| Paraproteinemia | 13 (2.8) | 1 (1.1) | 12 (3.2) | 0.28 |
| Comorbidities, n (%) | ||||
| Coronary artery disease | 147 (31.7) | 46 (51.1) | 101 (27.0) | <0.001 |
| Diabetes mellitus | 260 (56.0) | 52 (57.8) | 208 (55.6) | 0.71 |
| Congestive heart failure | 143 (30.8) | 44 (48.9) | 99 (26.5) | <0.001 |
| Hypertension | 434 (93.5) | 85 (94.4) | 349 (93.3) | 0.69 |
| Peripheral vascular disease | 73 (15.7) | 18 (20.0) | 55 (14.7) | 0.22 |
| Medications, n (%) | ||||
| Immunosuppressant | 26 (5.6) | 1 (1.1) | 25 (6.6) | 0.05 |
Age is expressed in years at study entry. Immunosuppressant medications included prednisone, cyclosporine, tacrolimus, sirolimus, mycophenolate mofetil, azathioprine, methotrexate, or chemotherapy.
Of 90 elderly patients, 51 (57%) patients lived at home (mean [SD] age=80.8 [4.2] years), 5 (6%) patients lived at an assisted living facility (81.6 [5.5] years), 31 (35%) patients lived at a nursing home during the entire study period (82.1 [6.0] years), and 2 (2%) patients lived in a nursing home temporarily. During the observation period, 26 (5.6% of total patients and 13% of patients with CRBSI) patients were on immunosuppressant medications for GN (14 patients), kidney transplant (6 patients), and malignancy (6 patients). Of these patients, only one patient was elderly (78.6 years; taking thalidomide and prednisone for amyloidosis). Remaining participants had mean (SD) age of 44.8 (17.8) years.
Follow-up was censored at (1) study close in 128 (27.5%) patients (19 [21.1%] elderly and 109 [29.1%] nonelderly patients), (2) conversion from TCVC to AVF or AVG in 291 (63.9%) patients (52 [57.7%] elderly and 239 [63.9%] nonelderly patients), (3) kidney transplantation in 3 (0 elderly patients) patients, and (4) death in 42 (9.0%) patients (19 [21.1%] elderly and 23 [6.1%] nonelderly patients).
Catheter Characteristics
Mean (SD) at-risk total catheter-days were 318 (240) in elderly and 272 (243) in nonelderly patients. The most frequent TCVC insertion site was upper body (internal jugular [IJ] or subclavian [SCL] vein) in 442(95.2%) patients followed by transitions between upper body and femoral catheters in 19 (4.0%) patients (Table 2). Of these sites, the insertion site was limited to the IJ vein in 412 (88.7%), SCL vein in 16 (3.4%), switched between IJ and SCL in 14 (3.0%), transitioned between femoral and IJ in 12 (1.9%), and transitioned between femoral and SCL in 7 (1.0%) patients. Femoral TCVCs alone were used in only two patients, and one patient (age=46 years) had a translumbar catheter. The type of CLS varied during the study period and in each individual. Heparin alone throughout the study period was the most frequently prescribed CLS in 369 (79.5%) patients (87.7% elderly and 77.5% nonelderly patients). GM citrate only was used in 20 (4.3%) patients (3.3% elderly and 4.6% nonelderly patients), and saline alone was used in 7 (1.5%) patients (1.1% elderly and 1.6% nonelderly patients). A subset of 68 (14.6%) patients received heparin followed by GM citrate (7.7% elderly and 16.3% nonelderly patients). Overall, there was no significant difference in the type of CLS used between elderly and nonelderly patients (heparin versus GM citrate versus saline; P=0.15).
Table 2.
Tunneled central venous catheter access characteristics
| Catheter Characteristic | All | Elderly (≥75 yr) | Nonelderly (18–74 yr) | P Value |
|---|---|---|---|---|
| Initial catheter site, n (%) | 0.42 | |||
| Internal jugular or subclavian | 442 (95.2) | 87 (96.6) | 355 (94.9) | |
| Femoral | 2 (0.4) | 1 (1.1) | 1 (0.3) | |
| Internal jugular/subclavian or femoral | 19 (4.0) | 3 (3.3) | 16 (4.2) | |
| Translumbar | 1 (0.2) | 0 | 1 (0.3) | |
| Initial catheter lock solution, n (%) | 0.15 | |||
| Heparin | 369 (79.5) | 79 (87.8) | 290 (77.5) | |
| Saline | 7 (1.5) | 1 (1.1) | 6 (1.6) | |
| Gentamicin citrate | 20 (4.3) | 3 (3.3) | 17 (4.6) | |
| Heparin or gentamicin citrate | 68 (14.7) | 7 (7.8) | 61 (16.3) | |
| Catheter-related bloodstream infection events (total) | 208 | 18 | 190 | |
| Catheter-da | 188 (104, 386) | 252 (130, 446) | 183 (99, 372) | |
| Catheter-related bloodstream infection events per 1000 catheter-da | 1.70 (4.2) | 0.55 (1.6) | 1.97 (4.6) | <0.001 |
Data expressed in median (25th, 75th percentiles).
Age-Related Risk of CRBSI
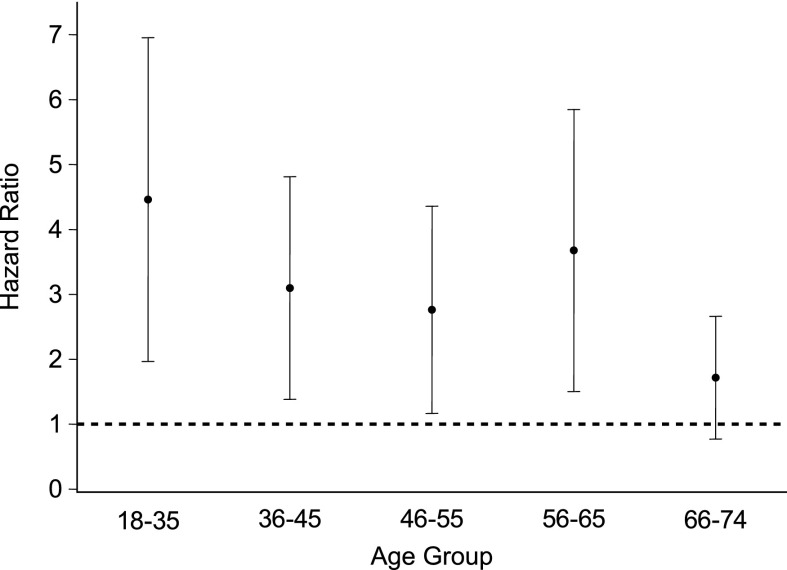
There were 190 episodes of CRBSI in nonelderly and 18 episodes of CRBSI in elderly patients, with a CRBSI rate of 0.55 events per 1000 catheter-days in elderly and 1.97 events per 1000 catheter-days in nonelderly patients (P<0.001) (Table 2). In univariate analysis, the risk of CRBSI was significantly lower in elderly compared with adult patients: HR, 0.34; 95% confidence interval (95% CI), 0.21 to 0.55; P<0.001 (Table 3). Sex, ancestry (African American versus European American/Hispanic), diabetes, and dialysis vintage were not associated with risk of CRBSI. There was a trend to an association between immunosuppressive medications and risk of CRBSI in univariate analysis (HR, 1.61; 95% CI, 0.95 to 2.72) that diminished in multivariate analysis (HR, 1.44; 95% CI, 0.83 to 2.48). Adjusting for sex, ancestry, dialysis vintage, diabetes, CAD, CHF, immunosuppression, dialysis unit, first CLS, and initial catheter location, the association between age and risk of CRBSI did not change; relative to young, middle-aged, and old patients, elderly patients had an HR for CRBSI of 0.33 (95% CI, 0.20 to 0.55; P<0.001). The risk of CRBSI decreased by 10% for each 5-year increase in patient age (HR, 0.89; 95% CI, 0.85 to 0.93; P<0.001). Interage group comparisons relative to the ≥75-year-old patients age group produced a range of HRs between 2.8 and 4.5 (95% CI, 1.2 to 7.0; P<0.001) for ages 18–65 years. Statistical significance was lost for the 66- to 74-year-old patients age group (HR, 1.7; 95% CI, 0.9 to 2.5; P=0.07) compared with elderly patients, likely because of reduced power (Figure 1).
Table 3.
Unadjusted and adjusted rates of catheter-related bloodstream infection
| Variable Association with CRBSI | Hazard Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| Univariate analysis | |||
| Age (≥75 versus 18–74 yr) | 0.34 | 0.21 to 0.55 | <0.001 |
| Sex (women versus men) | 1.17 | 0.89 to 1.54 | 0.26 |
| Ancestry (African American versus European American/Hispanic) | 1.25 | 0.95 to 1.65 | 0.12 |
| Vintage (1-yr increments) | 1.02 | 0.98 to 1.06 | 0.29 |
| Diabetes mellitus (no versus yes) | 0.89 | 0.68 to 1.18 | 0.42 |
| Tunneled central venous catheter site (internal jugular/subclavian versus femoral) | 0.51 | 0.36 to 0.73 | <0.001 |
| Catheter lock solution (gentamicin/citrate versus heparin/saline) | 1.07 | 0.75 to 1.52 | 0.72 |
| Immunosuppression (yes versus no) | 1.61 | 0.95 to 2.72 | 0.09 |
| Multivariate analysis | |||
| Age (≥75 versus 18–74 yr) | 0.33 | 0.20 to 0.55 | <0.001 |
| Sex (women versus men) | 1.07 | 0.80 to 1.42 | 0.66 |
| Ancestry (African American versus European American/Hispanic) | 1.30 | 0.92 to 1.84 | 0.13 |
| Vintage (1-yr increments) | 1.01 | 0.97 to 1.05 | 0.66 |
| Diabetes mellitus (no versus yes) | 0.88 | 0.66 to 1.19 | 0.41 |
| Tunneled central venous catheter site (internal jugular/subclavian versus femoral) | 0.50 | 0.33 to 0.79 | 0.002 |
| Catheter lock solution (gentamicin/citrate versus heparin/saline) | 0.85 | 0.57 to 1.25 | 0.40 |
| Immunosuppression (yes versus no) | 1.40 | 0.81 to 2.43 | 0.25 |
Multivariate analysis adjusted for sex, ancestry, dialysis vintage, diabetes mellitus, coronary artery disease, congestive heart failure, dialysis unit, initial tunneled central venous catheter site, first catheter lock solution, and immunosuppression. CRBSI, catheter-related bloodstream infection.
Figure 1.
Hazard ratios for catheter-related bloodstream infections across the range of ages. Hazard ratio (HRs) with 95% confidence intervals (95% CIs) by age group relative to elderly subjects≥75 years are shown. A dashed reference line for lack of significant association is drawn at HR, 1. Age group: 18–35 years: HR, 4.5; 95% CI, 2.0 to 7.0; P<0.001; 36–45 years: HR, 3.1; 95% CI, 1.3 to 4.9; P<0.001; 46–55 years: HR, 2.8; 95% CI, 1.2 to 4.4; P<0.001; 56–65 years: HR, 3.7; 95% CI, 1.6 to 5.8; P<0.001; 66–74 years: HR, 1.7; 95% CI, 0.9 to 2.5; P=0.07.
For sensitivity analysis, we included only 177 cases with positive blood culture-documented CRBSI. The primary results were not substantially changed in univariate analysis (HR for CRBSI in the elderly relative to nonelderly patients, 0.38; 95% CI, 0.22 to 0.62) or when adjusted for sex, ancestry, diabetes, CAD, CHF, dialysis vintage, dialysis unit, immunosuppression medication, CLS, and catheter site (HR, 0.39; 95% CI, 0.23 to 0.66) (Table 4).
Table 4.
Rates of catheter-related bloodstream infection for participants with positive blood cultures
| Variable Association with CRBSI | Hazard Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| Univariate analysis | |||
| Age (≥75 versus 18–74 yr) | 0.38 | 0.22 to 0.62 | <0.001 |
| Multivariate analysis | |||
| Age (≥75 versus 18–74 yr) | 0.39 | 0.23 to 0.66 | <0.001 |
| Sex (women versus men) | 1.06 | 0.77 to 1.44 | 0.73 |
| Ancestry (African American versus European American/Hispanic) | 1.33 | 0.91 to 1.94 | 0.13 |
| Vintage (1-yr increments) | 1.01 | 0.97 to 1.06 | 0.58 |
| Diabetes mellitus (no versus yes) | 0.96 | 0.70 to 1.32 | 0.81 |
| Tunneled central venous catheter site (internal jugular/subclavian versus femoral) | 0.52 | 0.33 to 0.83 | 0.01 |
| Catheter lock solution (gentamicin/citrate versus heparin/saline) | 0.77 | 0.49 to 1.20 | 0.22 |
| Immunosuppression (yes versus no) | 1.48 | 0.82 to 2.68 | 0.22 |
Multivariate analysis adjusted for sex, ancestry, dialysis vintage, diabetes mellitus, coronary artery disease, congestive heart failure, dialysis unit, initial tunneled central venous catheter site, first catheter lock solution, and immunosuppression.
Catheter Insertion Site and Risk of CRBSI
There was no significant difference in the site of TCVC insertion and CLS between the two age groups, including presence of temporary or permanent femoral TCVC and use of GM citrate lock (Table 2). In this analysis, upper body TCVC location (IJ or SCL) was associated with lower risk of CRBSI than femoral TCVC (HR, 0.51; 95% CI, 0.36 to 0.73; P=0.001). The association between catheter site and CRBSI remained significant in multivariate analysis (HR, 0.50; 95% CI, 0.33 to 0.79; P=0.002 for IJ and SCL versus femoral catheters) (Table 3).
Microbiology, Laboratory Parameters, and CRBSI-Related Complications
Positive blood cultures with speciation were obtained from 177 (85.0%) episodes of CRBSI. Of these episodes, 74% of episodes were caused by gram-positive cocci (GPCs), 21.4% of episodes were caused by gram-negative rods, 4.5% of episodes were polymicrobial, and 1 episode was caused by Candida albicans fungemia. Staphylococcus aureus accounted for 44.4% of GPC infections in elderly patients and 34.4% of GPC infections in nonelderly patients (Table 5). There was no significant difference in serum albumin, hemoglobin, ferritin, or dialysis clearance (single pool Kt/V and urea reduction ratio) obtained within 1 month before the first episode of CRBSI between elderly and young, middle-aged, and older patients (Table 5).
Table 5.
Laboratory parameters and microorganisms recovered
| Laboratory Parameters | All | Elderly (>75 yr) | Nonelderly (18–74 yr) | P Value |
|---|---|---|---|---|
| n | 208 | 18 | 190 | |
| spKt/V | 1.49 (0.4) | 1.52 (0.70) | 1.50 (0.42) | 0.57 |
| URR (%) | 71.0 (10.3) | 69.2 (15.7) | 71.2 (9.9) | 0.47 |
| Serum albumin (g/L) | 3.7 (0.5) | 3.6 (0.5) | 3.7 (0.5) | 0.56 |
| Hemoglobin (g/dl) | 11.2 (1.4) | 11.7 (1.6) | 11.2 (1.4) | 0.37 |
| Serum ferritin (ng/ml) | 639.4 (505.1) | 465 (379) | 656 (516) | 0.12 |
| Microorganisms, n (%) | 177 (85) | 13 (72) | 164 (86) | |
| Gram-positive cocci | 131 (74) | 9 (75) | 122 (74) | |
| Staphylococcus aureus | 46 (35) | 4 (44) | 42 (34) | |
| Gram-negative rods | 38 (21) | 3 (25) | 35 (21) | |
| Fungal | 2 (0.5) | 0 (0) | 2 (0.6) |
Laboratory parameters obtained within 30 days of the first catheter-related bloodstream infection event and microorganisms recovered throughout the entire study period. Data expressed in mean (SD). spKt/V, single pool Kt/V; URR, urea reduction ratio.
In total, 20 complications related to CRBSI were recorded: 4 episodes of endocarditis (mean [SD] age=56.89 [9.06] years), 2 episodes of osteomyelitis (1 episode was further complicated by diskitis; ages 43 and 75.42 years), 3 episodes of sepsis (mean [SD] age=54.55 [8.83] years), and 11 episodes of septic shock (mean [SD] age=67.52 [8.98] years). Of 11 cases of septic shock, 8 cases were complicated by death (mean [SD] age=67.88 [10.08] years). Across all complications, three events occurred in elderly patients (one event of osteomyelitis with diskitis at age 75.42 years and two events of septic shock and death at ages 79.75 and 83.5 years).
Discussion
To our knowledge, this study is the first study to analyze age-specific incidence of CRBSI. This retrospective study shows that, in a large dialysis practice, elderly patients were diagnosed with and treated for CRBSI significantly less often than their nonelderly counterparts.
Initiating dialysis in elderly patients is increasingly common. In 2010, one quarter of all United States dialysis patients were ≥75 years of age, a 12.2% increase over the prior decade (9). Despite age nondiscriminative fistula first efforts, more than two thirds of incident octogenarians rely on TCVCs (10). Advanced age is a risk factor for failure of primary AVF and shortened patency duration caused by atherosclerotic or calcified arteries, and many elderly patients end up not using their AVF. A meta-analysis of 13 studies showed that the risk of primary AVF failure is 80% higher in patients≥65 years old (4). In those patients having AVF surgery predialysis, only one of six AVFs placed in patients older than 75 years is ultimately used for dialysis access (11,12).
Physicians face a major decision as to what vascular access to plan for elderly patients with advanced CKD. This study complements our knowledge about the use of TCVCs in elderly patients. Our results showed that patients ages 75 years and older on HD have an approximately 60% lower incidence of CRBSI. Remarkably, incidence of CRBSI decreased by 10% per 5-year age increment, with the highest risk of CRBSI present in the age group 18–35 years (HR, 4.5; 95% CI, 2.0 to 7.0; P<0.001). Among other variables, sex, ancestry, dialysis vintage, and diabetes were not associated with CRBSI. Although CRBSI risk was impacted by catheter site, the incidence of CRBSI per 1000 catheter-days remained lower among elderly compared with younger patients independent of this variable (Table 3). It is noteworthy that CRBSI-related complications did not differ by age group in our data.
Existing literature has been equivocal with respect to age and risk of bacteremia in patients on dialysis. Age was not associated with higher risk for bacteremia in some studies (13–16), whereas other studies reported higher risk of hospitalized septicemia in older patients (17). Although we assessed age as a binary predictor with a cutoff≥75 years, previous studies used lower age cutoffs of ≥57 (15), ≥60 (14), or ≥65 years (17). Some studies included bacteremia or septicemia of any etiology in the outcome as opposed to solely CRBSI (13,15,17). Indeed, general medicine studies revealed that elderly patients not on dialysis have higher incidence of bacteremia and sepsis secondary to underlying infections (e.g., pneumonia) because of atypical symptoms and delayed diagnosis (18). This finding could explain the higher risk of hospitalized bacteremia and septicemia of any etiology in older ESKD patients on HD and peritoneal dialysis reported in the work by Powe et al. (17)
Causes of lower rates of CRBSI in elderly patients on HD are unknown. Decreased bacterial colonization in nares and skin is a potential explanation. Jean et al. (19) reported that dialysis patients without nasal carriage of S. aureus are of nominally significant older age (68 [12] years) than carriers (58.6 [15] years; P<0.001). Skin infections are significantly less common in patients ages≥75 compared with 65–74 years, and they continue to decrease among octogenarians (20,21). Aging is also associated with diminished response of the sweat glands to thermal stimuli, structural alteration in the eccrine glands, and reduced sweat output (22). Lower functional status with older age may pose less external mechanical stress on the catheter (e.g., catheter disruption associated with bathing or physical exercise), which in turn, may maintain the integrity of the subcutaneous tunnel and reduce entrance of skin bacteria and catheter biofilm formation.
This study has limitations. Retrospective in nature, it cannot eliminate the presence of additional variables that might confound results. Our data did not evaluate the timing of catheter site location for those patients who switched catheters, and it did not evaluate the timing of change in CLS for those patients who had more than one type of CLS during the study period. To compensate, statistical analyses were adjusted for first catheter site location and first CLS used during the study (catheter-days before the study period were not collected). Younger dialysis patients could have exhausted AVF or AVGs as forms of dialysis access, becoming dependent on TCVCs and having accrued more catheter-days and previous bacteremia episodes. Both of these factors associate with higher risk of CRBSIs (23). Nonetheless, a snapshot of CRBSI rates in elderly compared with younger dialysis patients is informative, because it might suggest the need to recalibrate dialysis access practices based on age. Our CRBSI inclusion criteria did not exactly match Centers for Disease Control and Prevention definitions (24). However, our criteria reflect widespread clinical practice in the nephrology community. Future studies with larger sample sizes need to be performed to validate these results.
The predicament of optimizing dialysis vascular access in elderly patients grew based on recent data showing near-equivalent survival on dialysis for elderly patients with TCVCs relative to AVFs or AVGs. In the Choices for Healthy Outcomes in Caring study, survival did not differ by access type in those patients≥65 years after comprehensive multivariable adjustments (7). In a recent USRDS-based study including solely incident HD patients≥67 years old, fistula first planning carried similar mortality outcomes as graft first planning, but 50% of those patients who had AVF placed and 25% of those patients who had AVG placed were, in fact, dialyzed through TCVCs, suggesting that TCVCs per se might not negatively impact survival in elderly patients (25). In a cohort of 33 dialysis-dependent octogenarians, of which 78% of patients were using TCVCs, 19 deaths occurred within 18 months of study, but 0 deaths were related to CRBSIs (10). Furthermore, DeSilva et al. (8) showed that dialysis mortality rates were similar between AVG and TCVC as first vascular access in patients 81–90 years old with prior malignancy or PVD; additionally, DeSilva et al. (8) showed similar mortality rates between AVF, AVG, and TCVC in patients>90 years old with prior malignancy, PVD, or diabetes. A randomized trial of AVF versus AVG versus watchful waiting with TCVC placement in elderly patients with advanced CKD would address whether dialysis catheters impact survival. This type of study is important, because it would assess the balance between the lower risk of CRBSI in the elderly and their higher comorbidity-driven competing risk for mortality.
We conclude that elderly patients≥75 years of age on HD with TCVCs have a much lower risk of CRBSIs than their younger counterparts. This finding may explain why older patients with multiple comorbidities on dialysis do not face higher mortality when using TCVCs versus AVFs or AVGs. Dialysis access guidelines may benefit from customization for patient age to more efficiently allocate medical resources. Comprehensive geriatric assessments are recommended to determine the optimal dialysis vascular access in elderly patients; use of TCVCs for HD could be a suitable approach in some geriatric patients.
Disclosures
None.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Recalibrating Vascular Access for Elderly Patients,” on pages 645–647.
References
- 1.Schmidt RJ: Informing our elders about dialysis: Is an age-attuned approach warranted? Clin J Am Soc Nephrol 7: 185–191, 2012 [DOI] [PubMed] [Google Scholar]
- 2.Steinman TI: The older patient with end-stage renal disease: Is chronic dialysis the best option? Semin Dial 25: 602–605, 2012 [DOI] [PubMed] [Google Scholar]
- 3.Ponce P: Vascular access for dialysis in the elderly. Int Urol Nephrol 33: 571–573, 2001 [DOI] [PubMed] [Google Scholar]
- 4.Lazarides MK, Georgiadis GS, Antoniou GA, Staramos DN: A meta-analysis of dialysis access outcome in elderly patients. J Vasc Surg 45: 420–426, 2007 [DOI] [PubMed] [Google Scholar]
- 5.Pastan S, Soucie JM, McClellan WM: Vascular access and increased risk of death among hemodialysis patients. Kidney Int 62: 620–626, 2002 [DOI] [PubMed] [Google Scholar]
- 6.Ishani A, Collins AJ, Herzog CA, Foley RN: Septicemia, access and cardiovascular disease in dialysis patients: The USRDS Wave 2 study. Kidney Int 68: 311–318, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J, CHOICE Study : Type of vascular access and survival among incident hemodialysis patients: The Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol 16: 1449–1455, 2005 [DOI] [PubMed] [Google Scholar]
- 8.DeSilva RN, Sandhu GS, Garg J, Goldfarb-Rumyantzev AS: Association between initial type of hemodialysis access used in the elderly and mortality. Hemodial Int 16: 233–241, 2012 [DOI] [PubMed] [Google Scholar]
- 9.US Renal Data System : USRDS 2012 Annual Data Report, Vol 1: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2012 [Google Scholar]
- 10.Vachharajani TJ, Moossavi S, Jordan JR, Vachharajani V, Freedman BI, Burkart JM: Re-evaluating the Fistula First Initiative in octogenarians on hemodialysis. Clin J Am Soc Nephrol 6: 1663–1667, 2011 [DOI] [PubMed] [Google Scholar]
- 11.Hemmelgarn BR, Zhang J, Manns BJ, Tonelli M, Larsen E, Ghali WA, Southern DA, McLaughlin K, Mortis G, Culleton BF: Progression of kidney dysfunction in the community-dwelling elderly. Kidney Int 69: 2155–2161, 2006 [DOI] [PubMed] [Google Scholar]
- 12.O’Hare AM, Allon M, Kaufman JS: Whether and when to refer patients for predialysis AV fistula creation: Complex decision making in the face of uncertainty. Semin Dial 23: 452–455, 2010 [DOI] [PubMed] [Google Scholar]
- 13.Hoen B, Paul-Dauphin A, Hestin D, Kessler M: EPIBACDIAL: A multicenter prospective study of risk factors for bacteremia in chronic hemodialysis patients. J Am Soc Nephrol 9: 869–876, 1998 [DOI] [PubMed] [Google Scholar]
- 14.Tokars JI, Light P, Anderson J, Miller ER, Parrish J, Armistead N, Jarvis WR, Gehr T: A prospective study of vascular access infections at seven outpatient hemodialysis centers. Am J Kidney Dis 37: 1232–1240, 2001 [DOI] [PubMed] [Google Scholar]
- 15.Taylor G, Gravel D, Johnston L, Embil J, Holton D, Paton S, Canadian Nosocomial Infection Surveillance Program. Canadian Hospital Epidemiology Committee : Incidence of bloodstream infection in multicenter inception cohorts of hemodialysis patients. Am J Infect Control 32: 155–160, 2004 [DOI] [PubMed] [Google Scholar]
- 16.Sedlacek M, Gemery JM, Cheung AL, Bayer AS, Remillard BD: Aspirin treatment is associated with a significantly decreased risk of Staphylococcus aureus bacteremia in hemodialysis patients with tunneled catheters. Am J Kidney Dis 49: 401–408, 2007 [DOI] [PubMed] [Google Scholar]
- 17.Powe NR, Jaar B, Furth SL, Hermann J, Briggs W: Septicemia in dialysis patients: Incidence, risk factors, and prognosis. Kidney Int 55: 1081–1090, 1999 [DOI] [PubMed] [Google Scholar]
- 18.Girard TD, Ely EW: Bacteremia and sepsis in older adults. Clin Geriatr Med 23: 633–647, 2007 [DOI] [PubMed] [Google Scholar]
- 19.Jean G, Charra B, Chazot C, Vanel T, Terrat JC, Hurot JM, Laurent G: Risk factor analysis for long-term tunneled dialysis catheter-related bacteremias. Nephron 91: 399–405, 2002 [DOI] [PubMed] [Google Scholar]
- 20.Bilgili SG, Karadag AS, Ozkol HU, Calka O, Akdeniz N: The prevalence of skin diseases among the geriatric patients in Eastern Turkey. J Pak Med Assoc 62: 535–539, 2012 [PubMed] [Google Scholar]
- 21.Yalçin B, Tamer E, Toy GG, Oztaş P, Hayran M, Alli N: The prevalence of skin diseases in the elderly: Analysis of 4099 geriatric patients. Int J Dermatol 45: 672–676, 2006 [DOI] [PubMed] [Google Scholar]
- 22.Dufour A, Candas V: Ageing and thermal responses during passive heat exposure: Sweating and sensory aspects. Eur J Appl Physiol 100: 19–26, 2007 [DOI] [PubMed] [Google Scholar]
- 23.Lemaire X, Morena M, Leray-Moragués H, Henriet-Viprey D, Chenine L, Defez-Fougeron C, Canaud B: Analysis of risk factors for catheter-related bacteremia in 2000 permanent dual catheters for hemodialysis. Blood Purif 28: 21–28, 2009 [DOI] [PubMed] [Google Scholar]
- 24.Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, Raad II, Rijnders BJ, Sherertz RJ, Warren DK: Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 49: 1–45, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DeSilva RN, Patibandla BK, Vin Y, Narra A, Chawla V, Brown RS, Goldfarb-Rumyantzev AS: Fistula first is not always the best strategy for the elderly. J Am Soc Nephrol 24: 1297–1304, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]