Abstract
Purpose
The purpose of this pilot study was to determine the effect of varying lens diameter of two types of keratoconic lenses on lens performance and initial comfort with participants with either centered or oval cones.
Methods
Sixteen eyes of ten keratoconic participants were fitted with lenses of five diameters i.e. 8.7, 9, 9.6, 10.1 and 10.4 diameters and two commercially available lens types; “KCGP-1” and “KCGP-2”. Lensmovement, centration and initial comfort were assessed.
Results
Ten subjects (2 female and 8 male, sixteen eyes) were enrolled to participate in the pilot study, themean age was 40.4 ± 14.33 years. Six eyes were in the early centred cone group, five in the early oval cone group and five in the late oval cone group. The lenses with the 9.6 lens diameter (TD) decentered the least for all lenses (p = 0.001). When compared to cone type, the 8.7/9 were more decentered for the late oval and late centred cones (p = 0.009). The movement of the smaller KCGP-1 was greater than the KCGP-2 for the centered early cones (p = 0.001) and the movement decreased for the larger KCGP-2 lenses for all cone types but not significantly (p > 0.05). The KCGP-1 lenses were more significantly comfortable than the KCGP-2 lenses for the centered cones (p = 0.003). Only for the early oval cones, was the larger KCGP-2 lenses more comfortable (p = 0.04).
Conclusions
Lens diameter affects comfort and centration especially for the small (8.7/9) and large (10.4/10.1) diameters in this pilot study. Lens movement was not correlated with comfort.
Keywords: Keratoconus, GP lens fitting, GP lens diameter, GP lens comfort
Resumen
Objetivo
El objetivo de este estudio preliminar fue determinar el efecto de variar el diámetro total de la lente (TD) de dos tipos de lentes queratocónicas en el rendimiento de la lente y la comodidad inicial con participantes que tenían conos centrados u ovalados.
Métodos
Se adoptaron lentes de cinco diámetros (8,7, 9, 9,6, 10,1 y 10,4) y dos tipos de lentes disponibles en el mercado, KCGP-1 y KCGP-2, en dieciséis ojos de 10 participantes con queratocono. Se adoptaron el movimiento, el centrado y la comodidad inicial de las lentes.
Resultados
Se incluyó a 10 sujetos (2 mujeres y 8 hombres, 16 ojos) para participar en un estudio preliminar; la media de edad fue de 40,4 ± 14,33 años. Había seis ojos en el grupo de conos centrados incipientes, cinco en el grupo de conos ovalados avanzados y cinco en el grupo de conos centrados avanzados. Las lentes con un diámetro de 9,6 (TD) fueron las que menos se descentraron de todas (p = 0,001). Si comparamos entre tipos de cono, las de 8,7/9 se descentraron más en conos ovalados avanzados y en conos centrados avanzados (p = 0,009). El movimiento de la KCGP-1, más pequeña, fue mayor que el de la KCGP-2 para los conos incipientes centrados (p = 0,001) y el movimiento se redujo para las lentes KCGP-2, más grandes, para todos los tipos de conos, aunque no de manera significativa (p > 0,05). Las lentes KCGP-1 fueron significativamente más cómodas que las lentes KCGP-2 para los conos centrados (p = 0,003). Las lentes KCGP-2 más grandes fueron más cómodas solamente para los conos ovalados incipientes (p = 0,04).
Conclusiones
El diámetro de la lente afecta a la comodidad y el centrado, sobre todo para los diámetros pequeños (8,7/9) y grandes (10,4/10,1) de este estudio preliminar. El movimiento de la lente no se correlacionó con la comodidad.
Palabras clave: Queratocono, Ajuste de lente PG, Diámetro de lente PG, Comodidad de lente PG
Introduction
Keratoconus is a progressive, bilateral but typically asymmetric, ectasia of the cornea. The incidence of keratoconus varies greatly in the literature and ranges from 4 to 600 affected individuals per 100,000.1 The disease is highly variable in its course, beginning at about the time of puberty. Initially a patient in their teens or 20's consults an eye care practitioner with symptoms of blurry vision. As this process continues, which includes steepening and thinning of the cornea, worsening visual acuity due to irregular astigmatism and the presence of a variable degree of scarring, until the third or fourth decade of life.1 It is usually followed by a period of relative stability or a very slow increase, with occasional episodes of progression.2
This degenerative disorder is considered to be caused genetically3,4 though no clear-cut genetic pattern has been established, but a familial occurrence has been reported with a correlation to different systemic diseases.5 Recently, oxidative stress6 to stromal collagen tissue due to rigid contact lens (CL) wear, eye rubbing, atopic disease and connective tissue disorders has been postulated as a cause. CL will eventually be necessary in all cases with approximately 20 % of patients eventually needing corneal surgery, but, still requiring CL management.1
Keratoconus can be classified based on central keratometric readings, shape i.e. nipple-type (centred), oval-type and globus-type, or progression.7 One of the most important tools in managing the progression of keratoconus is computerised video-keratography (VKE) and with this information the shape, size and position of the cone can be examined, followed over time and used in order to select corneal lens parameters.8
The centred cone has been described as having a smaller diameter and its apex lies mostly centrally to slightly inferio-nasally. On the other hand, the oval cone is larger and is more prevalent in the inferio-temporal region of the cornea. The more decentred the cone, the more difficult and challenging the CL fitting.5
CL fitting in keratoconus and achieving an acceptable fit can be very difficult. The development of irregular astigmatism is a challenging problem to practitioners.9 In the early stages of keratoconus habitually both spectacles and CL can be used. There is a wide range of different varieties of lenses for keratoconus lens fitting. Each stage in the progression of the keratoconus has a special requirement for the lens fitting. As the keratoconus increases in severity, so too must the CL fit be manipulated to match the new corneal topography in order to achieve centration and comfort.8,10
Rigid gas permeable (GP) lenses have been successfully used to provide an adequate visual correction for patients with keratoconus by providing a smooth optical surface to correct irregular astigmatism. 11–13 With the advent of highly oxygen permeable materials and the availability of computer-assisted videokeratoscopes (VKE), the fitting of these patients has become more simplified with better physiological outcomes.14 With this information, lens parameters can be better selected to aid in lens centration and comfort. These lenses are typically worn during most waking hours requiring all day comfort with minimal ocular response.
Selection of lens diameter is generally based on the advancement/size of the cone.15,16 This pilot study hopes to see if any differences in lens performance and comfort can be detected with a change in contact lens diameter (TD).
The purpose of this pilot study was first, to investigate how changes in CL diameter affect the centration, movement and fit of each of two lens types for keratoconus patients with centred (early and late stage) and oval (early and late stage) cone types and second, to correlate the lens fitting characteristics with initial lens comfort.
Methods and data analysis
The study was a non-dispensing clinical trial (a fitting study) using a small sample size of 16 eyes of 10 participants who visited the University of Waterloo, School of Optometry, CL clinic. All participants were experienced CL wearers. To determine the eligibility of the participants, the initial screening examination included measurement of the best visual acuity with the patient's current CL, slit lamp examination and topography. Informed consent was obtained from all participants according to the Tenets of Helsinki and the Office of Research Ethics.
Topographic maps were taken with the Orbscan II™ Topographer (B&L Surgical, Rochester, NY) and were studied to categorise each participant into the type of keratoconus that had presented i.e. a more centrally located cone apex or one with a more displaced corneal apex. Based on the cone apex location, either within the central two millimetres or outside of that zone, the cones were labelled as “centred” or “oval,” respectively. The steepest K reading was used to define the severity of the condition. Steep K readings < 50 D (6.75 mm) were called “early” cones and > 51.25 D (6.58 mm) are referred to as “late” cones in this manuscript. In addition, the apical and overall cone diameters were measured using the 1 mm grid superimposed on the absolute scale tangential colour map. Cones were subsequently divided into two groups: centred (6 eyes) or oval (10 eyes), then further subdivided into early or late categories with equal numbers in each.
There were two lens types (i.e. of different design) manufactured with three different diameters and corresponding back optic zone diameters (BOZD), for a total of six trial lens sets used in this study. These two commercially available lens designs, one with a variable BOZD (KCGP-1) and one with a fixed BOZD (KCGP-2) were fitted on all participants regardless of cone type. The two lens types (with three lens diameters) that were used are outlined in Table 1. Some lens types have either variable (KCGP-1) or fixed BOZD's (KCGP-2). In lenses with variable BOZD's the BOZD changes with the BOZR that is, as the radius becomes steeper the BOZD becomes smaller which tend to be more stable on centred cones. In lenses with fixed BOZD's, the BOZD increases only when the lens diameter increases and are more suited for progressing oval cones.8 Lens performance and subjective comfort using analog scales (0 worst to 100 best) were assessed when the lens had settled that is, after at least five minutes.
Table 1.
Trial lens parameters
| Lens name | KCGP-1 | KCGP-2 |
|---|---|---|
| Material | BOSTON ES Std. | BOSTON EO Std. |
| Enflufocon A | Enflufocon B | |
| Custom | Custom | |
| Dk Value | 30 × 10–11 | 100 × 10–11 |
| Diameter (mm) | Custom 8.7, 9.6, 10.4 (trials) | Custom 9, 9.6, 10.1 (trials) |
| BOZR (mm) | Custom | Custom |
| Power (D) | Custom | Custom |
| Description | Posterior multicurve design with variable OZ | Posterior design divided into three principal areas for custom fit with fixed OZ |
| CT (mm) | Custom | Custom |
All three lens diameters and both lens types (i.e. six lenses) were worn by each participant in the study. Lenses with the 9.6 mm diameter (TD) were selected first and fitted according to the manufacturers’ recommendations (approximately on average K) and adjusted if necessary, until an optimal three point touch pattern was achieved for each cone type. The smaller diameter lenses were fitted 0.2 mm steeper than average K (or from the base curve of the best fit 9.6 mm lens). The larger diameter lenses were fitted 0.2 mm flatter than average K (or from the base curve of the best fit 9.6 mm lens). The fitting of the smaller and larger TDs was randomly assigned. The fluorescein patterns were rated as aligned (5 to 10 μm), slightly steep (11 to 20 μm), steep or clearly noticeable central pooling (> 20 μm), slightly flat (1 to 4 μm), flat or clearly noticeable area of touch (0 μm) for the central portion of the lens. For the peripheral portion of the lens, the clearance was graded as optimal (70 to 80 μm), slightly insufficient (40 to 69 μm), insufficient (0 to 39 μm), slightly excessive (81 to 95 μm) and excessive (96 to 120 μm). These ratings were developed by the first author's thesis work (Sorbara L, Performance of “centred” versus “upper-lid attached” rigid gas permeable lenses, University of Waterloo, 1993).
Lateral and vertical centration, and lens movement were measured using a graticule scale in the eyepiece of the Zeiss™ slit lamp biomicroscope where a positive value is nasal and superior and a negative value is temporal and inferior. Comfort, shortly after the lens settled was rated by each participant, on an analog scale from 0 (totally uncomfortable) to 100 (perfect comfort) for each of the two lens types and three diameters.
Data analyses were conducted using Statistica 7.0 (StatSoft Inc. Tulsa, USA). Data are presented in tables as mean ± standard deviation and in figures as the mean with 0.95 confidence intervals, unless otherwise indicated. Data from subjective rating scales and objective measures (continuous variables) were analysed with repeated measures ANOVAs. Kruskal-Wallis and Freidman ANOVAs were employed for non-parametric analyses (data graded on 0 to 4 scales). Where post hoc testing is reported, a Tukey HSD test was employed. Pearson correlations were used to compare data. A significance level of α = 0.05 was used for all analyses.
Results
There were 2 female and 8 male participants (total of 16 eyes) with mean age of 40.4 ± 14.33 years. Table 2 outlines the simulated topographic K readings and cone diameters for the participants.
Table 2.
Baseline participant topographic parameters
| Cone type | Steepest K | Average K | Cone diameter; apex/overall |
|---|---|---|---|
| Oval-early (n = 3) | 49.26 ± 1.71 D | 44.66 ± 1.45 D | 1.8 ± 0.76/5 ± 0.94 mm |
| Oval-Late (n = 3) | 57 ± 2.91 D | 48.39 ± 2.57 D | 1.84 ± 0.85/4.74 ± 0.49 mm |
| Centred-Early (n = 5) | 48.75 ± 0.78 D | 45.53 ± 0.13 D | 1.5 ± 0/4.75 ± 1.06 mm |
| Centred Late (n = 5) | 59.5 ± 5.5 D | 53.91 ± 5.49 D | 1.63 ± 0.75/4.5 ± 0.08 mm |
Figures 1 (centred cone) and 2 (oval cone) illustrate the cone types that were identified with the VKE images.
Figure 1.

Orbscan™ II topographic map of centred cone. Note cone apex located within the central 2 mm zone.
Figure 2.
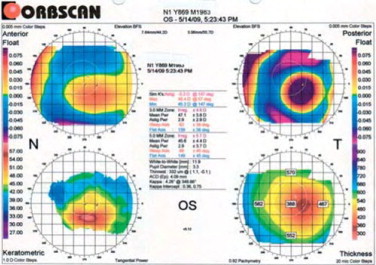
Orbscan™ II topographic map of oval cone. Note cone apex located outside the central 2 mm zone.
Regardless of the lens design and manufacture, a gentle 3-point touch was achieved in all the 9.6 mm TD cases. The parameters of the final lenses that were fitted are found in Table 3.
Table 3.
Final lens fitting parameters for each lens diameter
| ID# | Cone type | KCGP-1 BOZR (mm) |
KCGP-2 BOZR (mm) |
||||
|---|---|---|---|---|---|---|---|
| 8.7 mm | 9.6 mm | 10.4 mm | 9 mm | 9.6 mm | 10.1 mm | ||
| 3-OD | oval early | 7.3 | 7.5 | 7.7 | 7.3 | 7.5 | 7.7 |
| 6-OD | oval early | 7 | 7.2 | 7.4 | 7 | 7.2 | 7.4 |
| 9-OS | oval early | 7.5 | 7.7 | 7.9 | 7.4 | 7.6 | 7.8 |
| 10-OS | oval early | 7.5 | 7.7 | 7.9 | 7.4 | 7.6 | 7.8 |
| 11-OS | oval early | 7.4 | 7.6 | 7.8 | 7.4 | 7.6 | 7.8 |
| 2-OD | oval late | 6.1 | 6.3 | 6.5 | 6.1 | 6.3 | 6.5 |
| 2-OS | oval late | 6.9 | 7.1 | 7.3 | 6.9 | 7.1 | 7.3 |
| 8-OS | oval late | 6.6 | 6.8 | 7 | 6.7 | 6.9 | 7.1 |
| 9-OD | oval late | 6.8 | 7 | 7.2 | 6.8 | 7 | 7.2 |
| 10-OD | oval late | 7.3 | 7.5 | 7.7 | 7.3 | 7.5 | 7.7 |
| 4-OD | centred early | 7.3 | 7.5 | 7.7 | 7.3 | 7.5 | 7.7 |
| 5-OS | centred early | 7.2 | 7.4 | 7.6 | 7.2 | 7.4 | 7.6 |
| 7-OD | centred early | 6.8 | 7 | 7.2 | 6.8 | 7 | 7.2 |
| 4-OS | centred late | 5.6 | 5.8 | 6 | 5.6 | 5.8 | 6 |
| 5-OD | centred late | 6.5 | 6.7 | 6.9 | 6.5 | 6.7 | 6.9 |
| 7-OS | centred late | 5.9 | 6.1 | 6.3 | 5.9 | 6.1 | 6.3 |
Figures 3, 4 and 5 show the three point touch fluorescein patterns that correspond to a single participant with a centred cone with each of the three TD's (8.7, 9.6 and 10.4 mm, respectively) for lens type KCGP-1. In general, once the three point touch pattern was achieved for the 9.6 mm lens, the smaller and larger diameter lenses appeared slightly steep after compensation for the change in sagittal depth, but not significantly (p = 0.05).
Figure 3.

Example of fluorescein pattern of 8.7 mm KCGP-1 lens on centred cone.
Figure 4.

Example of fluorescein pattern of same participant wearing 9.6 mm KCGP-1 lens.
Figure 5.

Example of fluorescein pattern of same participant wearing 10.4 mm KCGP-1 lens.
Figures 6, 7 and 8 are illustrations of another participant having an oval cone with lens type KCGP-2 and the three lens diameters (9, 9.6 and 10.1 mm, respectively).
Figure 6.

Example of fluorescein pattern of 9 mm KCGP-2 lens on oval cone.
Figure 7.

Example of fluorescein pattern of same participant wearing 9.6 mm KCGP-2 lens.
Figure 8.

Example of fluorescein pattern of same participant wearing 10.1 mm KCGP-2 lens.
The central fluorescein patterns showed minimal apical clearance for both early cone types and slightly more apical clearance with the late cones (p = 0.005) as seen in Table 4. The edge clearance and widths were slightly reduced for both late cone types and especially for the centred cone type (p = 0.04). When comparing the two lens types and for 9.6 and 10.1/10.4 TD's, the KCGP-1 lenses had less edge clearance and width, compared to the KCGP-2 lenses (p = 0.027).
Table 4.
Central and peripheral clearance ratings (μm)
| 8.7/9 mm TD |
9.6 mm TD |
10.1/10.4 mm TD |
||||
|---|---|---|---|---|---|---|
| Central clearance | Peripheral clearance | Central clearance | Peripheral clearance | Central clearance | Peripheral clearance | |
| Oval early | 9.5 ± 10.92 | 92.5 ± 29 | 1.5 ± 2.42 | 95 ± 23.57 | 0.5 ± 1.58 | 97.5 ± 24.86 |
| Oval late | 13.5 ± 9.73 | 76.5 ± 28.7 | 5.5 ± 8.32 | 69.5 ± 49.35 | 7 ± 8.88 | 65 ± 53.8 |
| Centred early | 11.25 ± 4.79 | 87.5 ± 15 | 1.25 ± 2.5 | 97.5 ± 20.62 | 2.5 ± 5 | 57.5 ± 47.87 |
| Centred late | 17.5 ± 10.69 | 35 ± 39.64 | 9.25 ± 10.26 | 33.75 ± 47.49 | 15.63 ± 12.94 | 41.88 ± 45 |
Vertical and horizontal centrations were measured and compared. Vertical centration was found to be significantly different comparing the three lens diameters and for each lens type (p = 0.001). Post-hoc analysis indicated that 8.7/9 mm lenses centred the best on early centred cones; 9.6 mm KCGP-1 lenses centred the best on late central cones and early oval cones; 10.1/10.4 lenses centred better on early oval cones. Generally, late cones had more inferior decentration regardless of the TD (Table 5).
Table 5.
Vertical lens centration (mm)
| Vertical Centration (mm) |
||||||
|---|---|---|---|---|---|---|
| KCGP-1/8.7 | KCGP-1/9.6 | KCGP-1/10.4 | KCGP-2/9 | KCGP-2/9.6 | KCGP-2/10.1 | |
| Oval early | −0.6 ± 1.39 | +0.2 ± 0.76 | +0.3 ± 0.27 | +0.8 ± 1.15 | +1.2 ± 0.91 | +0.5 ± 0.5 |
| Oval late | −1.1 ± 0.65 | −0.9 ± 0.96 | −0.8 ± 1.04 | −1.3 ± 0.84 | −0.4 ± 0.22 | −1.2 ± 0.84 |
| Central early | −0.25 ± 0.35 | +1.5 ± 2.12 | +0.5 ± 0.71 | −0.5 ± 0 | +1.5 ± 2.12 | +1.5 ± 2.12 |
| Central late | −1.63 ± 1.25 | −0.25 ± 0.5 | −0.5 ± 1.29 | −0.87 ± 0.63 | −1.63 ± 1.11 | −0.75 ± 0.96 |
Lateral centration was not found to be significantly different comparing the lens diameters and for each lens type (p > 0.05). Lenses tended to decentre temporally on the early oval cones especially with the KCGP-2 lenses.
Movement of the lens in primary gaze with the blink was measured and we found that there was a significant difference in lens movement comparing each lens type, KCGP-1 moved more than KCGP-2 for all cone types (p = 0.018) as shown in table 6. Also, smaller lenses for either lens type moved more than the larger lenses, (p = 0.001). The movement of the smaller KCGP-1 was greater than the KCGP-2 lens for early centred cones (p = 0.001).
Table 6.
Lens movement in primary gaze (mm)
| Lens movement in primary gaze (mm) |
||||||
|---|---|---|---|---|---|---|
| KCGP-1/8.7 | KCGP-1/9.6 | KCGP-1/10.4 | KCGP-2/9 | KCGP-2/9.6 | KCGP-2/10.1 | |
| Oval early | 2.7 ± 1.3 | 2.2 ± 0.45 | 2.2 ± 1.09 | 2 ± 0.71 | 1.9 ± 0.89 | 2 ± 0.71 |
| Oval late | 2.4 ± 1.14 | 1.8 ± 0.45 | 1.6 ± 0.89 | 2 ± 0 | 1.9 ± 0.89 | 1.6 ± 0.55 |
| Central early | 3 ± 1.41 | 2.5 ± 0.71 | 1.5 ± 0.71 | 2.5 ± 0.71 | 2 ± 0 | 2 ± 1.41 |
| Central late | 1.75 ± 0.96 | 1.5 ± 0.58 | 1.25 ± 0.96 | 0.5 ± 0.58 | 1.75 ± 0.96 | 0.75 ± 0.5 |
Comfort ratings for each lens diameter versus cone type varied significantly for small KCGP-1 (centred) and large KCGP-2 (oval) (p = 0.003). For centred cones, there was better comfort with small TD (8.7 mm) KCGP-1 lens compared to KCGP-2. The comfort ratings for the 9.6 mm lenses of either type were not significantly different (p > 0.05). On the other hand for oval cones, there was improved comfort with the larger diameter KCGP-2 (10.1 mm) lens compared to KCGP-1 in this small sample (Tukey, post hoc, p = 0.04) (Figure 9).
Figure 9.

Comfort scale ratings for all cone types and TD's (KCGP-1 (TD = 8.7, 9.6, 10.4 mm) and KCGP-2 (TD = 9, 9.6, 10.1 mm). The asterisk (*) represents the significantly different ratings.
There was no relationship between comfort ratings and either the central or peripheral edge clearances, regardless of lens diameter, having Pearson correlations of 0.2 and 0.23, respectively (p > 0.05).
Discussion
Classification of cone type by measurement of the central and steepest K readings is the standard method of diagnosing keratoconus and pellucid marginal degeneration.5,9,17–21 More recently the use of video-keratoscopy and research into various indices for pattern recognition has increased the practitioners’ ability for early diagnosis of these conditions. 22–27 With the use of these tools our small sample was classified into the early and late, either centred or oval, type of keratoconus.
A three point touch fitting pattern was almost always achieved for all three lens diameters and each lens design, based on the fitting nomogram that was used requiring minimal modification (see Figures 4 to 8).28,29 Considering that the cones were not advanced to the globus stage, the fittings were uneventful for the 9.6 mm lens when starting with the average K reading for the initial base curve, as been suggested by Edrington15,30 and others.14 This method of base curve selection allowing for a gentle three point touch has been tested by others and found to least affect the biomechanical properties of the thinning cornea.10,29,31 Following the guidelines of fitting the smaller lens, 0.2 mm steeper than average K and the larger diameter, 0.2 mm flatter than average K, to compensate for the differences in sagittal depth that the BOZD and TD created31,32 did result in slightly steeper central patterns, especially for late cones and larger TD's. Some authors tend to fit these lenses with a mild amount of central clearance in any case,15,16 but with too much apical clearance, acuity may be compromised.33 Smaller lens diameters for the early centred cones were more aligned in fluorescein pattern, agreeing with other studies.14,15,34 Late cones had more apical clearance but demonstrated more movement, contrary to common belief; this may be due to short wearing times of up to one hour with each lens, in this small fitting study.
Excessive or insufficient edge clearance are both troublesome in affecting corneal physiology, comfort and lens positioning.31,35 The insufficient edge clearances that were observed here for the late cones and larger diameters, using trial lenses only, indicate the need to match the increasing eccentricity value or rate of flattening for more advanced cones with a peripheral system of a CL that has a high enough axial edge lift. Lenses can be easily modified by ordering flatter peripheral systems until an adequate amount of clearance is achieved.28
This pilot study showed that there was a significant difference in centration among the three lens diameters despite most lenses having a three point touch fluorescein pattern. There was a slight inferior decentration of the smaller lens diameters on both late cone types. These findings are in keeping with those of Rosenthal, where he found that 8.5 mm lenses tended to decentre more than larger lenses on keratoconic cornea.36 The tendency for lenses to decentre on keratoconic cornea may be due to the mismatch of the BOZD of the CL and the diameter of the cone, if it is too small the lens will be loose and decentre and on the other hand, if it is too large, the excessive pooling of tears and seal between the back surface of the CL and the cornea encourages the CL to centre over the already steep and decentred cone. 37–39 For our small sample, the 8.7 mm centred the best on the centred cones and the 9.6 mm and larger diameters showed the best centration for both cone types and especially for the late cones.
When the results for the initial comfort were analysed, there was only a significant relationship with lens diameter/lens type i.e. smaller TD were more comfortable with centred cones and larger TD were more comfortable with oval cones. There was no correlation with the central fluorescein pattern as has been suggested by Edrington et al,35 although, he did find a correlation with edge clearance, which with our small sample, we did not. Nor did we find a correlation with lens decentration, since no lenses were excessively decentred, as could be expected with more advanced cones than those in our study.
Conclusions
Only smaller KCGP-1 lenses on late centred cones were more comfortable despite having greater movement and decentration in this pilot study. Larger KCGP-2 lenses on oval cones were more comfortable despite having some decentration (early cones) and less movement. For this pilot study the 9.6 and 10.1/10.4 mm lenses had the best fitting characteristics for both the late centred and oval cones.
Conflict of interests
Authors declare that they don’t have any conflict of interests.
References
- 1.Rabinowitz Y.S. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Mannis M., Kadnik K. Contact Lens Fitting in Keratoconus. CLAO J. 1989;15:283–288. [PubMed] [Google Scholar]
- 3.Rabinowitz Y.S. The genetics of keratoconus. Ophthalmol Clin North Am. 2003;16:607–620. doi: 10.1016/s0896-1549(03)00099-3. vii. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y., Rabinowitz Y.S., Rotter J.I., Yang H. Genetic epidemiological study of keratoconus: evidence for major gene determination. Am J Med Genet. 2000;93:403–409. [PubMed] [Google Scholar]
- 5.Krachmer J.H., Feder R.S., Belin M.W. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28:293–322. doi: 10.1016/0039-6257(84)90094-8. [DOI] [PubMed] [Google Scholar]
- 6.Kenney M.C., Chwa M., Atilano S.R., Tran A., Carballo M., Saghizadeh M. Increased levels of catalase and cathepsin V/L2 but decreased TIMP-1 in keratoconus corneas: evidence that oxidative stress plays a role in this disorder. Invest Ophthalmol Vis Sci. 2005;46:823–832. doi: 10.1167/iovs.04-0549. [DOI] [PubMed] [Google Scholar]
- 7.Burger D., Zadnik K. Mosby; St. Louis, Missouri: 1997. Keratoconus: Contact Lenses for Pre- and Post-Surgery. 21–52. [Google Scholar]
- 8.Sorbara L., Dalton K. The use of video-keratoscopy in predicting contact lens parameters for keratoconic fitting. Cont Lens Anterior Eye. 2010;33:112–118. doi: 10.1016/j.clae.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 9.Lawless M., Coster D.J., Phillips A.J., Loane M. Keratoconus: diagnosis and management. Aust NZJ Ophthalmol. 1989;17:33–60. doi: 10.1111/j.1442-9071.1989.tb00487.x. [DOI] [PubMed] [Google Scholar]
- 10.Hom M.M. Another perspective on keratoconus contact lens fitting. J Am Optom Assoc. 1986;57:886–888. [PubMed] [Google Scholar]
- 11.Crews M.J., Driebe W.T., Stern G.A. The clinical management of keratoconus: a 6 year retrospective study. CLAO J. 1994;20:194–197. doi: 10.1097/00140068-199407000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Norman C.W. Keratoconus contact lens fitting: what do we really know? (… and where do we learn it?) Cont Lens Anterior Eye. 2007;30:214. doi: 10.1016/j.clae.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 13.Szczotka L.B., Thomas J. Comparison of axial and instantaneous videokeratographic data in keratoconus and utility in contact lens curvature prediction. CLAO J. 1998;24:22–28. [PubMed] [Google Scholar]
- 14.Sorbara L., Luong J. Contact lens fitting guidelines for the keratoconic patient using videokeratograhic data. Practical Optometry. 1999;10:238–243. [Google Scholar]
- 15.Edrington T.B., Barr J.T., Zadnik K., Davis L.J., Gundel R.E., Libassi D.P. Standardized rigid contact lens fitting protocol for keratoconus. Optom Vis Sci. 1996;73:369–375. doi: 10.1097/00006324-199606000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Zadnik K., Barr J.T., Steger-May K., Edrington T.B., McMahon T.T., Gordon M.O. Comparison of flat and steep rigid contact lens fitting methods in keratoconus. Optom Vis Sci. 2005;82:1014–1021. doi: 10.1097/01.opx.0000192349.11525.de. [DOI] [PubMed] [Google Scholar]
- 17.Burger D.S., Zadnik K. Mosby; St. Louis: 1997. Contact Lenses for Pre- and Post-Surgery. 21–52. [Google Scholar]
- 18.Karabatsas C.H., Cook S.D. Topographic analysis in pellucid marginal corneal degeneration and keratoglobus. Eye. 1996;10:451–455. doi: 10.1038/eye.1996.99. [DOI] [PubMed] [Google Scholar]
- 19.Lee B.W., Jurkunas U.V., Harissi-Dagher M., Poothullil A.M., Tobaigy F.M., Azar D.T. Ectatic disorders associated with a claw-shaped pattern on corneal topography. Am J Ophthalmol. 2007;144:154–156. doi: 10.1016/j.ajo.2007.02.032. [DOI] [PubMed] [Google Scholar]
- 20.Maguire L.J., Klyce S.D., McDonald M.B., Kaufman H.E. Corneal topography of pellucid marginal degeneration. Ophthalmology. 1987;94:519–524. doi: 10.1016/s0161-6420(87)33416-5. [DOI] [PubMed] [Google Scholar]
- 21.Mandell R.B. Contemporary management of keratoconus. Int Cont Lens Clin. 1997;24:43–58. [Google Scholar]
- 22.Demirbas N.H., Pflugfelder S.C. Topographic pattern and apex location of keratoconus on elevation topography maps. Cornea. 1998;17:476–484. doi: 10.1097/00003226-199809000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Rabinowitz Y.S. Videokeratographic indices to aid in screening for keratoconus. J Refract Surg. 1995;11:371–379. doi: 10.3928/1081-597X-19950901-14. [DOI] [PubMed] [Google Scholar]
- 24.Rabinowitz Y.S. Tangential vs sagittal videokeratographs in the “early” detection of keratoconus. Am J Ophthalmol. 1996;122:887–889. doi: 10.1016/s0002-9394(14)70388-5. [DOI] [PubMed] [Google Scholar]
- 25.Rabinowitz Y.S., Rasheed K. KISA % index: a quantitative videokeratography algorithm embodying minimal topographic criteria for diagnosing keratoconus. J Cataract Refract Surg. 1999;25:1327–1335. doi: 10.1016/s0886-3350(99)00195-9. [DOI] [PubMed] [Google Scholar]
- 26.Rao S.N., Raviv T., Majmudar P.A., Epstein R.J. Role of Orbscan II in screening keratoconus suspects before refractive corneal surgery. Ophthalmology. 2002;109:1642–1646. doi: 10.1016/s0161-6420(02)01121-1. [DOI] [PubMed] [Google Scholar]
- 27.Sonmez B., Doan M.P., Hamilton D.R. Identification of scanning slit-beam topographic parameters important in distinguishing normal from keratoconic corneal morphologic features. Am J Ophthalmol. 2007;143:401–408. doi: 10.1016/j.ajo.2006.11.044. [DOI] [PubMed] [Google Scholar]
- 28.Hood A. Advanced contact lens fitting: part 3 - hospital contact lens practice. Optician. 1997;214:16–22. [Google Scholar]
- 29.McMonnies C.W. Keratoconus fittings: apical clearance or apical support? Eye Contact Lens. 2004;30:147–155. doi: 10.1097/01.icl.0000138717.57592.36. [DOI] [PubMed] [Google Scholar]
- 30.Edrington T.B., Szczotka L.B., Barr J.T., Achtenberg J.F., Burger D.S., Janoff A.M. Rigid contact lens fitting relationships in keratoconus. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study Group. Optom Vis Sci. 1999;76:692–699. [PubMed] [Google Scholar]
- 31.Leung K.K. RGP fitting philosophies for keratoconus. Clin Exp Optom. 1999;82:230–235. doi: 10.1111/j.1444-0938.1999.tb06653.x. [DOI] [PubMed] [Google Scholar]
- 32.Ozkurt Y.B., Sengor T., Kurna S., Evciman T., Acikgoz S., Haboglu M., Rose K. contact lens fitting for keratoconus. Int Ophthalmol. 2008;28:395–398. doi: 10.1007/s10792-007-9156-4. [DOI] [PubMed] [Google Scholar]
- 33.Sorbara L., Chong T., Fonn D. Visual acuity, lens flexure, and residual astigmatism of keratoconic eyes as a function of back optic zone radius of rigid lenses. Cont Lens Anterior Eye. 2000;23:48–52. doi: 10.1016/s1367-0484(00)80025-9. [DOI] [PubMed] [Google Scholar]
- 34.Lembach R.G. Use of contact lenses for management of keratoconus. Ophthalmol Clin North Am. 2003;16:383–394. doi: 10.1016/s0896-1549(03)00057-9. [DOI] [PubMed] [Google Scholar]
- 35.Edrington T.B., Gundel R.E., Libassi D.P., Wagner H., Pierce G.E., Walline J.J. Variables affecting rigid contact lens comfort in the collaborative longitudinal evaluation of keratoconus (CLEK) study. Optom Vis Sci. 2004;81:182–188. doi: 10.1097/00006324-200403000-00010. [DOI] [PubMed] [Google Scholar]
- 36.Rosenthal P. The Boston lens and the management of keratoconus. Int Ophthalmol Clin. 1986;26:101–109. doi: 10.1097/00004397-198602610-00014. [DOI] [PubMed] [Google Scholar]
- 37.Betts A.M., Mitchell L.G., Zadnik K. Visual performance and comfort with the Rose K lens for keratoconus. Optom Vis Sci. 2002;79:493–501. doi: 10.1097/00006324-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 38.O’Donnel C., Codina C.M. A hyper-Dk piggyback contact lens system for keratoconus. Eye Contact Lens. 2004;30:44–48. doi: 10.1097/01.ICL.0000104596.50832.7F. [DOI] [PubMed] [Google Scholar]
- 39.Ozkurt Y., Oral Y., Karaman A., Ozgur O., Dogan O.K. A retrospective case series: use of SoftPerm contact lenses in patients with keratoconus. Eye Contact Lens. 2007;33:103–105. doi: 10.1097/01.ICL.0000258592.12598.28. [DOI] [PubMed] [Google Scholar]


