Abstract
The transforming JAK2V617F kinase is frequently associated with myeloproliferative neoplasms (MPNs) and thought to be instrumental for the overproduction of myeloid lineage cells. Several small molecule drugs targeting JAK2 are currently in clinical development for treatment in these diseases. We performed a high-throughput in vitro screen to identify point mutations in JAK2V617F that would be predicted to have potential clinical relevance and associated with drug resistance to the JAK2 inhibitor ruxolitinib (INCB018424). Seven libraries of mutagenized JAK2V617F cDNA were screened to specifically identify mutations in the predicted drug-binding region that would confer resistance to ruxolitinib, using a BaF3 cell-based assay. We identified 5 different non-synonymous point mutations that conferred drug resistance. Cells containing mutations had a 9 to 33-fold higher EC50 for ruxolitinib compared to native JAK2V617F. Our results further indicated that these mutations also conferred cross-resistance to all JAK2 kinase inhibitors tested, including AZD1480, TG101348, lestaurtinib (CEP-701) and CYT-387. Surprisingly, introduction of the ‘gatekeeper’ mutation (M929I) in JAK2V617F affected only ruxolitinib sensitivity (4-fold increase in EC50). These results suggest that JAK2 inhibitors currently in clinical trials may be prone to resistance as a result of point mutations and caution should be exercised when administering these drugs.
Keywords: Myeloid neoplasia, JAK2, drug resistance
Introduction
Myeloproliferative neoplasms (MPNs) are frequently associated with a mutation in the non-receptor tyrosine kinase JAK2 at codon 617 that changes valine (V) to phenylalanine (F). This activating JAK2V617F mutation is not only found in the majority of patients with myeloproliferative neoplasms, including polycythemia vera, essential thrombocythemia, idiopathic myelofibrosis, but can also be present at lower frequency in other myeloid malignancies, including acute myeloid leukemia and myelodysplastic syndromes 1. JAK2V617F is thought to be instrumental for the overproduction of myeloid lineage cells and in mice it is sufficient by itself to cause a myeloproliferative disease 2. Even though the crystal structure of the JAK2 kinase domain has been solved 3, 4, it is not known how exactly the V617F mutation in the pseudokinase domain leads to constitutive activation. The JAK2V617F mutation seems insufficient for its kinase activation and association with a cytokine receptor, such as the erythropoietin receptor (EpoR) appears to be required 5. Lack of a functional FERM domain in JAK2V617F, which mediates interaction with cytokine receptors, results in a loss of its transforming activity 6. It is likely that inhibitory constraints, normally overcome by ligand binding, are targeted by the JAK2V617F mutation, therefore leading to hyperresponsiveness or factor-independent growth.
One of the first JAK2 inhibitors entering clinical trials for the treatment of myelofibrosis was ruxolitinib (INCB018424). This drug has shown significant efficacy and dose-limiting toxicity is thrombocytopenia 7. Nevertheless, it is expected that there are additional activities that may lead to specific toxic effects, such as dose-limiting hyperamylasaemia with TG101348 and other effects with related drugs 8, 9. Like other JAK2 inhibitors, including TG101348, AZD1480 and CYT-387, ruxolitinib displays activity against the related JAK1 10-14. In contrast, the JAK2 inhibitor lestaurtinib (CEP-701) is structurally related to the pan protein kinase inhibitor staurosporine and also shows activity against FLT3, RET and Trk family members 15-18. All inhibitors tested for myelofibrosis demonstrated efficacy with a reduction of splenomegaly, including ruxolitinib, lestaurtinib, CYT-387, SB1518 and TG101348 9. There are additional JAK2 inhibitors at various stages in clinical trials for the treatment of MPNs and their toxicity and efficacy is currently under investigation 9.
Most, if not all, tyrosine kinase inhibitors that are currently used to target transforming tyrosine kinase oncogenes in various cancers are susceptible to resistance, as a result of point mutations in the corresponding kinase domain 19-23. We sought to investigate whether mutations in the JAK2 JH1 domain would confer resistance and compare the sensitivity of different inhibitors that are currently in clinical trials towards these mutations. Using the JAK2 inhibitor ruxolitinib in our primary screen, we identified five different non-synonymous point mutations in JAK2V617F that conferred drug resistance. We also observed cross-resistance between all mutations and five different JAK2 inhibitors tested. In addition, an analysis of the ruxolitinib-docked JAK2 structure was performed to identify potential sites of drug-target interaction. Interestingly, introduction of the M929I ‘gatekeeper’ mutation in JAK2V617F lead to ruxolitinib resistance only. Point mutations in the JAK2 kinase domain may provide a significant obstacle and it would be predicted that drugs currently in clinical development may not be sufficient to overcome resistance. It will now be interesting to determine whether these mutations occur in patients that fail to respond to JAK2 inhibitors in clinical trials.
Materials And Methods
Cells
The murine pre-B BaF3 cell line expressing the erythropoietin receptor (EpoR) was maintained in RPMI 1640 (Mediatech, Manassas, VA) containing 10% fetal bovine serum (FBS; Lonza, Walkersville, MD), supplemented with WEHI-3B conditioned medium under a 5% CO2 atmosphere. In some experiments, cells were treated with kinase inhibitors, including ruxolitinib (INCB018424), TG101348 (both Active Biochemicals, Hong Kong, China), CYT-387 (ChemieTek, Indianapolis, IN), AZD1480 (Selleck, Houston, TX) and lestaurtinib (CEP701, Tocris Bioscience Ellisville, MO). Cell growth in response to various drug concentrations was measured by trypan blue (Sigma) exclusion or with the CellTiter 96® AQueous One Solution Cell Proliferation Assay reagent (Promega, Madison, WI). The CalcuSyn (Biosoft, Great Shelford, United Kingdom) analysis program was used to estimate drug concentrations resulting in 50% inhibition (EC50), compared to control treated cells.
Random mutagenesis of JAK2V617F
Random mutations were introduced into the pMSCV.JAK2V617F.IRES.GFP construct using the mutT (unable to hydrolyze 8-oxodGTP), mutS (error-prone mismatch repair) and mutD (deficient in 3′- to 5′-exonuclease of DNA polymerase III) deficient XL1-Red E.coli strain, according to the manufacturer's protocol (Agilent, Santa Clara, CA). A total of seven different libraries of mutagenized JAK2V617F were generated.
Identification of cells resistant to ruxolitinib
Mutagenized JAK2V617F libraries were used to prepare retroviral supernatants 6 to infect BaF3 cells expressing the erythropoietin receptor (BaF3.EpoR). Cells were expanded for at least three days and pretreated with 1.44 μM ruxolitinib (12 times the EC50 in parental cells) for two days before sorting of single GFP-expressing cells into 96-well plates. Resistant colonies were isolated in the presence of 1.44 μM ruxolitinib.
Detection of mutations in the JAKV617F kinase domain
Genomic DNA was isolated (QIAmp DNA Blood kit, Qiagen, Germantown, MD) from drug resistant colonies and the putative drug binding region in the kinase domain amplified by PCR (AccuPrime Pfx, Invitrogen, Carlsbad, CA) using standard methods and specific primers (forward: 5′-ATGAGCCAGATTTCAGGCCTGCTT-3′; reverse 5′-AGAAAGTTGGGCATCACGCAGCTA-3′) on a MJ Research PTC-200 Peltier Thermal Cycler (St. Bruno, Canada). DNA sequencing was performed at the DFCI Molecular Biology Core Facility (forward PCR primer or 5′-ACATGAGAATAGGTGCCCTAGG-3′) and ambiguous results were confirmed by sequencing of the reverse strand (not shown). Identified mutations were reintroduced into JAK2V617F by site-directed mutagenesis using the QuikChange II XL Mutagenesis Kit (Agilent) and specific mutagenesis primers, according to the manufacturer's protocol. The entire cDNA sequence of the mutagenized product was verified by DNA sequencing (not shown).
Characterization of cell lines expressing mutated JAK2V617F
BaF3.EpoR cell lines expressing potential drug resistant mutant JAK2V617F were generated by retroviral infection, as described previously 6. Stable transfectants were sorted for GFP+ cells and the presence of the mutation confirmed by DNA sequencing of the putative drug-binding site, as described above. Polyclonal populations of these cells were used to determine changes in growth in response to various JAK2 inhibitors.
Docking of ruxolitinib to JAK2 and structure analysis
The three-dimensional structure of INCB018424 (PubChem: CID 25126798) was docked onto the monomer three-dimensional structure of JAK2 extracted from the CMP6-bound JAK2 crystal structure (PDB ID: 2B7A) 3. Docking calculations were carried out using DockingServer 24. Gasteiger partial charges were added to the ligand atoms. Non-polar hydrogen atoms were merged, and rotatable bonds were defined. Essential hydrogen atoms, Kollman united atom type charges, and solvation parameters were added with the aid of AutoDock tools 25. To limit the docking simulations to the inhibitor-binding pocket, determined from the CMP6-JAK2 structure, the affinity grid was set to fit the inhibitor-binding pocket. AutoDock parameter set- and distance-dependent dielectric functions were used in the calculation of the van der Waals and the electrostatic terms, respectively. Docking simulations were performed using the Lamarckian genetic algorithm (LGA) and the Solis & Wets local search method as applied in the DockingServer 24. Initial position, orientation, and torsions of the ligand molecules were set randomly. All rotatable torsions were released during docking. Each docking experiment was derived from 2 different runs that were set to terminate after a maximum of 250,000 energy evaluations. The population size was set to 150. During the search, a translational step of 0.2 Å, and quaternion and torsion steps of 5 were applied. The best scoring docking pose of ruxolitinib-JAK2 was used for the drug-target interface analysis in PyMOL (http://www.pymol.org) and structure figures were rendered using PyMOL.
Immunoblotting
Immunoblotting was performed using a standard chemiluminescence technique, as described previously 26. Rabbit polyclonal antibodies against STAT5 (Santa Cruz Biotechnology, Santa Cruz, CA), phospho-STAT5 (Y694 - Cell Signaling, Danvers, MA) or a mouse monoclonal antibody against β-actin (AC-15; Sigma) were used.
Results
Identification of novel mutations in JAK2V617F that cause ruxolitinib resistance
In this study, we performed a screen for ruxolitinib resistant JAK2V617F mutations using a mutagenesis strategy with a repair deficient E. coli strain, similar to previously described approaches 27, 28. Seven independent libraries of mutated JAK2V617F expression vector were generated and expressed in BaF3.EpoR cells. Our approach was specifically designed to look for mutations in the predicted drug binding region of JAK2. In preliminary experiments, resistant clones were initially selected at 3-, 6- and 12-times the EC50 of ruxolitinib (0.36 μM, 0.72 μM and 1.44 μM, respectively). Only the highest ruxolitinib (1.44 μM) concentration was sufficient to allow for the identification of resistant mutations at a frequency >10% of total. We isolated 128 independent resistant clones, but the majority of clones did not contain a mutation in the sequenced region and the mechanism of resistance was not further investigated. Overall, we identified five different point mutations, including Y931C (Tyr931Cys), G935R (Gly935Arg), R938L (Arg938Leu), I960V (Ile960Val) and E985K (Glu985Lys).
Structural analysis of JAK2V617F kinase domain mutations
The crystal structure for JAK2-bound ruxolitinib is not available and we therefore performed docking simulations of this drug onto the monomer JAK2 structure, extracted from the crystal structure of the JAK2-CMP6 complex. Published structures of JAK2 bound to CMP6 3 and CP690,550 4 provide important clues on the mode of binding and interactions between the related JAK2 inhibitors and the protein. Both CMP6 and CP690,550 bind in the ATP-binding pocket of JAK2. With this in mind, we set the parameters to preferentially simulate ruxolitinib docking positions in the CMP6 and CP690,550 binding pocket on JAK2. The best scoring docking pose, with least estimated free energy of binding (-9.05 kCal/mol), best estimated inhibition constant (KI of 231.83nM) and highest interaction interface area (567.6 Å2), was used for the inhibitor-JAK2 interface analysis. Ruxolitinib snugly fits into the ATP-binding pocket of JAK2 similar to CMP6 and CP690,550, with the cyclopentyl and pyrazol rings tightly fitting in the deep hydrophobic groove (Figure 1A). JAK2-ruxolitinib interaction interface buries most of the surface area of the inhibitor. The inhibitor is held in the pocket by polar contacts between cyclopentyl ring and mainchain atoms in the hinge region (between Y931 and L932), and also pyrrolopyrimidine moiety with N981 sidechain. Ruxolitinib may also form hydrogen bonds with water molecules in the pocket. Ruxolitinib makes extensive hydrophobic interactions with several residues that line the binding pocket, similar to what was observed for CMP6 and CP690,550. A880, L855, V863 and M929 hold the inhibitor tight from the top and L932 from the hinge region holds it from the side. Further, V911 and L983 provide hydrophobic interactions from the bottom (Figure 1B, left panel). The pyrazol ring of ruxolitinib is in a distance to have π–π interaction with the Y931 ring. Most mutations that were identified in our screen are either interacting residues with ruxolitinib or in proximity of the binding pocket (Figure 1B, right panels) and hence are likely to alter the inhibitor binding. Y931 seems to be a critical residue for inhibitor-protein interaction as its side chain and mainchain atoms have interactions with the inhibitor. The Y931C mutation might disrupt the π–π interaction between tyrosine ring and the inhibitor ring structure, thus weakening the inhibitor binding and resulting in easy expulsion from the pocket. The G935R mutation pushes a large charged sidechain towards the mouth of the hydrophobic cavity (Figure 1B, right), which results in a strong positive charge at the corner of the binding pocket, compared to the native protein (Figure 1C). The exact mechanism by which the R938L (Figure 1B, right) and I960V mutations may effect the inhibitor binding cannot easily be explained based on our computational analysis of the structure, but these two residues lie near the binding pocket (R938L at the end of the hinge region and I960V in close proximity of the binding pocket). The E985K mutation could bring the sidechain very close to the inhibitor-binding site and result in charge repulsion of the inhibitor.
Figure 1. Structural analysis of JAK2V617F kinase domain mutations.
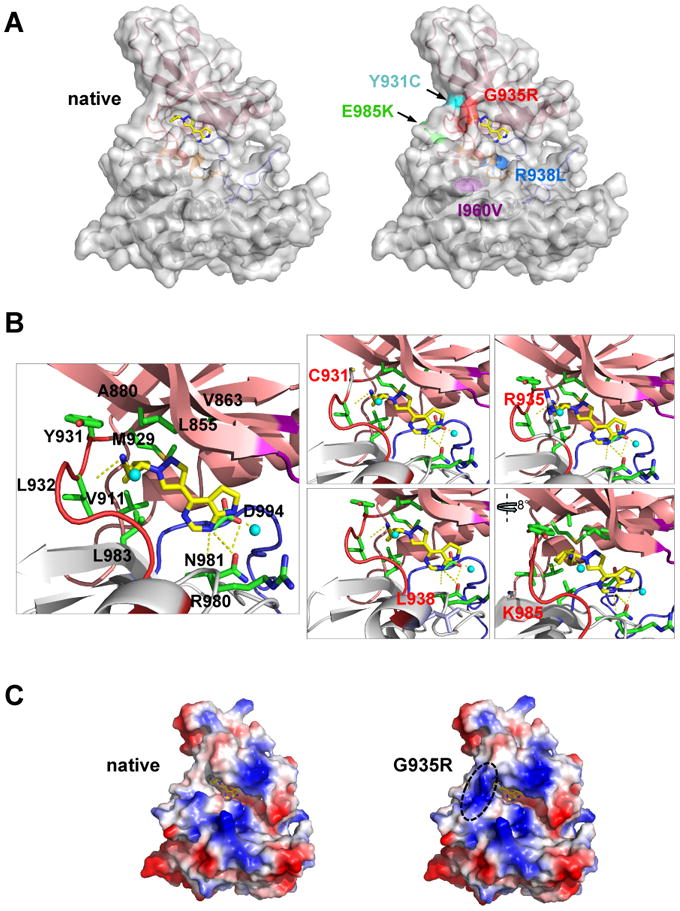
A, cartoon and transparent surface representation of ruxolitinib-docked JAK2 kinase domain (A and B) (left) and JAK2 with location of point mutations that lead to drug resistance (right). N-terminal lobe (salmon), C-terminal lobe (grey), glycine loop (purple), activation loop (blue) and hinge region (red) form the boundaries for the binding site of ruxolitinib (stick representation in yellow (carbon) and blue (nitrogen)). The I960V sidechain (purple) is buried within the protein interior. B, enlarged ruxolitinib binding pocket with secondary structure elements (cartoon) and the interactions of the sidechains (labeled sticks) with the inhibitor. Hydrogen-bonds between the inhibitor and the protein are indicated as dotted yellow lines (one hydrogen-bond between backbone of Y931 and L932; and two hydrogen-bonds with R980 and N981 and pyrrolopyrimidine ring of the inhibitor; additional hydrogen bonds are with water molecules (cyan spheres)). Mutated amino acids are labeled red (right panels). C, surface electrostatic potential representation of the native (left) and G935R (right) containing JAK2 JH1 domain with ruxolitinib. Charged surfaces are displayed in shades of blue (positive), red (negative) and white (non-polar).
Ruxolitinib-resistant mutations display cross-resistance to other JAK2 tyrosine kinase inhibitors
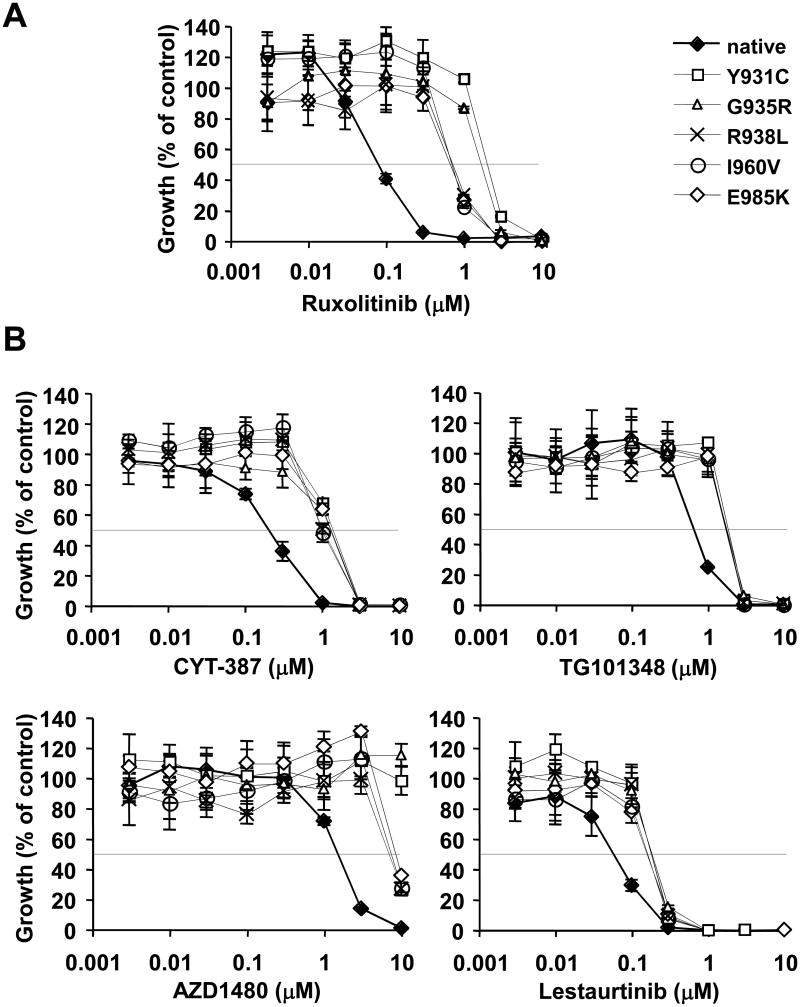
In order to confirm that the mutants identified in our screen truly conferred drug resistance, they were reintroduced into JAK2V617F and expressed in BaF3.EpoR cells. All cell lines generated, spontaneously converted into growth factor independence (not shown). Consistent with our structural analysis, we found that both the Y931C as well as the G935R mutation resulted in the largest increase (33.3-fold and 19.5-fold, respectively) in EC50 values, compared to native JAK2V617F (Figure 2A). The increase in EC50 values of ruxolitinib for the R938L (12.7-fold), I960V (11.5-fold) and the E985K (9.0-fold) mutation containing cells was somewhat lower. These data are also consistent with our screening approach, allowing survival and outgrowth of resistant colonies at 1.44 μM ruxolitinib. We next asked whether these mutations would also affect the sensitivity of other JAK2 tyrosine kinase inhibitors (Figure 2B). In contrast to ruxolitinib, there was a comparable increase in drug resistance for all mutations in response to CYT-387 (5.1 to 7.4-fold increase in EC50), TG101348 (2.2 to 2.8-fold increase in EC50) and Lestaurtinib (2.6 to 3.3-fold increase in EC50). The changes in EC50 in response to AZD1480 were qualitatively similar to ruxolitinib. Both, the Y931C and G935R mutations had the highest EC50 values (>10μM), corresponding to a >7-fold increase in EC50. Also, like ruxolitinib, lower EC50 values for AZD1480 were found with R938L, I960V and E985K (5.6 to 6.5-fold increase) mutation containing cells.
Figure 2. Mutations in the JAK2V617F kinase domain confer resistance to JAK2 tyrosine kinase inhibitors.
Growth of BaF3.EpoR cells expressing JAK2V617F (◆) and the additional Y931C (□), G935R (△)), R938L (×), I960V (○) or E985K (◊) mutations was determined in response to ruxolitinib (A) or CYT-387, TG101348, AZD1480 and lestaurtinib (B) at various concentrations, as indicated (n=4). Changes in growth in response to JAK2 inhibitors were calculated relative to cells that were treated with the solvent DMSO.
Ruxolitinib resistance confers a growth advantage during JAK2 inhibition
In order to further confirm the growth advantage of resistant mutations in the presence of ruxolitinib, we cocultured JAK2V617F expressing cells with a defined amount of cells containing the E985K or Y931C mutation (1% of total). These mutants were chosen due to their likely different mode of interaction with JAK2 inhibitors. Under these conditions, neither mutation could be detected by sequencing of the genomic DNA at the beginning of the assay (Figure 3A, top panel). Subsequently, cells were grown for seven days in the presence of solvent (DMSO) or ruxolitinib (300 nM). Our previous experiments suggest that this concentration is sufficient to significantly, but not completely, impair viability (not shown) and cell growth (Figure 2A) in parental cells, whereas mutant expressing cells are unaffected in a three day culture. Sequencing of genomic DNA revealed that seven days after treatment with ruxolitinib, more than half of the sequence material contained the E985K or Y931C mutation, but not the control treated cells (Figure 3A, bottom panel). We also confirmed the efficacy of ruxolitinib at this concentration by measuring changes in phosphorylation of the JAK2 target STAT5. Ruxolitinib failed to inhibit phosphorylation of STAT5 at its activation site in both of the resistant cell lines, but not in JAK2V617F expressing cells (Figure 3B). These data would support our findings that both mutations specifically cause ruxolitinib resistance at low doses.
Figure 3. Characterization of ruxolitinib resistant JAK2V617F mutations.
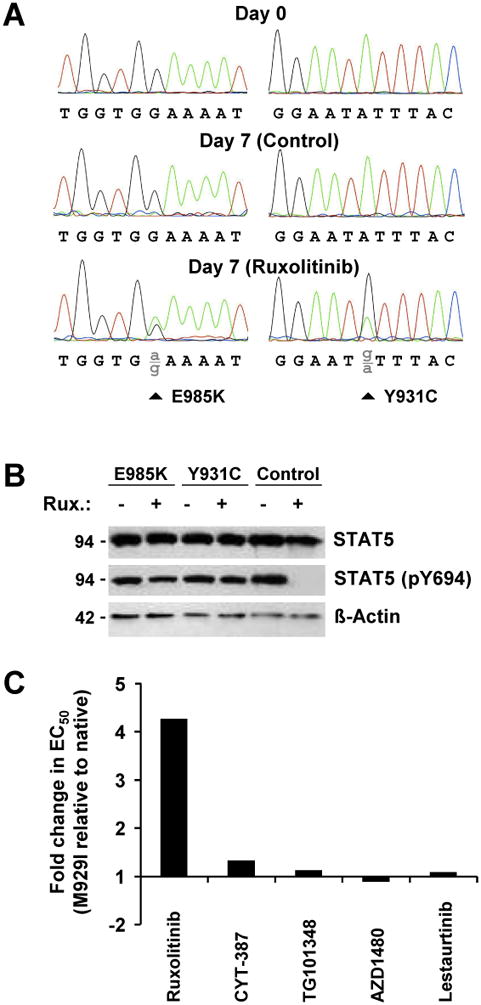
A, genomic DNAs from a polyclonal population of BaF3.EpoR.JAK2V617F cells, containing 1% of JAK2V617F mutant expressing cells were analyzed at day 0 and day 7 after treatment with either DMSO (control) or ruxolitinib (300nM) for the presence of E985K and Y931C substitution (arrows indicate position of corresponding base substitution). Partial chromatograms of the forward strand are shown. B, expression of STAT5, phospho-Y694 STAT5 and β-actin was determined by immunoblotting in BaF3.EpoR cells expressing either JAK2V617F (control) and cells containing the additional E985K or Y931C mutation. Cells were either treated with DMSO or 300 nM ruxolitinib. C, relative changes in EC50 values were determined in response to ruxolitinib for BaF3.EpoR.JAK2V617F.M929I cells, relative to cells expressing native JAK2V617F.
The ‘gatekeeper’ M929I mutation specifically alters ruxolitinib sensitivity
Previously, mutations of the so called ‘gatekeeper’ site in the hinge region of various tyrosine kinases, including ABL (T315), EGFR (T790), KIT (T670) and PDGFRα (T674), were associated with strong in vitro and in vivo resistance to their respective inhibitors 19-21, 23. Our screen did not reveal prominent mutations at this site that could be detected with our approach. Structural analysis (not shown) and sequence alignment (Table 1) indicate that M929 in human and murine JAK2 was homologous to the T315I gatekeeper site in ABL and other tyrosine kinases. In these kinases the valine or threonine residues were commonly mutated into either isoleucine or methionine. In JAK2, this site already contained a methionine residue in the ‘gatekeeper’ position and we therefore mutated it into isoleucine. Similar to the experiments above, we determined the dose dependent reduction in growth in response to various JAK2 inhibitors and calculated EC50 values (Figure 3C). As expected, we did not observe any change in sensitivity of the M929I mutation towards CYT-387, TG101348, AZD1480 or lestaurtinib. Interestingly, this assay demonstrated that the M929I mutation only displayed resistance to ruxolitinib (4.3-fold increase in EC50). The sidechain of M929 does not have apparent polar contacts with ruxolitinib, but is at the far end of the hydrophobic groove that binds the kinase inhibitors and may influence the correct positioning of the drug in the hydrophobic binding pocket.
Table 1.
Sequence alignment of the ‘gatekeeper’ region of tyrosine kinases with common mutations that confer drug resistance compared to JAK2.
| Tyrosine kinase | Protein sequence | ‘Gatekeeper’ mutation |
|---|---|---|
| ABL | PFYIIT315EFMTYGNLLDYLR | T315I 20 |
| EGFR | TVQLIT790QLMPFGCLLDYVR | T790M 21 |
| KIT | PTLVIT670EYCCYGDLLNFLR | T670I 23 |
| PDGFRα | PIYIIT674EYCFYGDLVNYLH | T674I 19 |
| hJAK2 | NLKLIM929EYLPYGSLRDYLQ | |
| mJAK2 | --R---929------------- |
Discussion
Secondary resistance is a major obstacle in the treatment of cancers that are transformed by tyrosine kinase oncogenes. Resistant mutations frequently occur at the drug binding site of the targeted kinases 19-23. In this study, we identified five different point mutations in the kinase domain of JAK2V617F in an in vitro screen that conferred resistance to the ATP competitive JAK2 inhibitor ruxolitinib and cross-resistance to CYT-387, TG101348, AZD1480 and lestaurtinib. These point mutations affected the sensitivity to ruxolitinib and offered a growth advantage to cells during treatment, compared to native JAK2V617F expressing cells. Even though our results were obtained with JAK2V617F, it is likely that other activated forms of JAK2 or oncogenes that lead to activation of JAK2 may as well be susceptible to mutations that cause resistance. Additional activated forms of JAK2 include oncogenic fusions, such as PCM1-JAK2 as a consequence of a recurrent t(8;9)(p21;p24) or point mutations at sites different from V617, such as the R683G mutation in Down syndrome children with B-progenitor acute lymphoblastic leukemias (B-ALL), additional JAK2 point mutations in pediatric or adult B-ALL and others 29-32. Further, oncogenic cytokine receptors, including CRLF2 in B-ALL can lead to constitutive JAK2 signaling 32. There may be substantial overlap in JAK2 signaling and analogous mutations in the JAK2 kinase domain would be predicted to cause drug resistance similar to the results observed in our study.
The docking analysis of ruxolitinib to the JAK2 kinase domain suggests that the interaction within the binding pocket may be similar among different inhibitors, which would explain cross-resistance. One would expect any mutation that weakens the hydrophobic interactions or pushes a charged sidechain into the middle of the binding pocket to lead to resistance. The Y931C mutation may disrupt hydrophobic interactions between Y931 and the ring structures of the inhibitor, along with other hydrophobic interactions, which are likely required to hold the inhibitor in the binding pocket, eventually weakening the inhibitor binding. This mutation may also change the mainchain conformation in the hinge region, which could disrupt polar contacts that the inhibitor makes with the mainchain atoms in the hinge region. Loss of possible π–π interaction between Y931 and pyrazole ring structure may also result in easy expulsion of the inhibitor from the pocket. The large charged sidechain of the G935R mutation may reduce or prevent entry of inhibitors. The positive charge may result in inhibitor expulsion due to charge-charge repulsion with the amine groups in the inhibitor. We hypothesize that the R938L and I960V mutations change the mainchain conformation in a way that effect the receptor binding and affinity, due to their proximity to the binding pocket. The E985K mutation may disturb the water-inhibitor interactions in the pocket or may disturb the hydrophobic pocket in a way to reduce or prevent inhibitor binding.
This screen identified a limited number of mutations that resulted in drug resistance. There are additional amino acids involved in drug interactions and mutations in any of these amino acids in the N-terminal lobe (A880, L855, V863, V911), C-terminal lobe (L983, R980, N981), activation loop (D994) or hinge region (Y931, L932) would have the potential to change the affinity of ruxolitinib or related JAK2 inhibitors to the binding pocket and thus alter sensitivity. The mechanisms involved may be similar between JAK2 inhibitors. Nevertheless, our data also suggest that there are differences between ruxolitinib and the other JAK2 inhibitors. Introduction of the M929I ‘gatekeeper’ mutation specifically affected ruxolitinib sensitivity. This mutation is homologous to the T315I mutation in BCR-ABL, which causes strong ABL inhibitor resistance in chronic myelogenous leukemia 20, 22. The small change in sensitivity for ruxolitinib (4-fold increase in EC50) may be a result of the bulky methionine residue already present in this location and the change to isoleucine is rather modest. Thus, the isoleucine residue may provide little hindrance for the overall binding of specific JAK2 inhibitors, with the exception of ruxolitinib.
In addition, activating mutations in the ABL tyrosine kinase have been implicated in resistance mechanisms towards imatinib 33. Mutations in the kinase domain were not only found to confer resistance but also led to constitutive activation of ABL itself. The activating V617F mutation in the pseudokinase domain does not cause apparent resistance to kinase inhibitors, but there are other activating sites in the pseudokinase domain 34. A screen for JAK1 gain-of-function mutation suggests that homologous activating mutation in the pseudokinase domain may not result in drug resistance 35. This is in contrast to activating mutations in the JAK1 kinase domain, which can confer resistance. Interestingly, one of these JAK1 kinase domain substitutions was also introduced into JAK2. This Y931C mutation is identical to one of the mutations identified in our screen and resulted in factor independent growth as well as JAK2 inhibitor resistance 35. These results do not exclude the possibility that additional mutations outside of the kinase domain may decrease sensitivity for JAK2 inhibitors but our in vitro results hint at mutations in this domain at additional sites as a potential major cause for secondary resistance.
JAK2 inhibitors have shown promising results during their initial clinical trials in MPN patients, but their mechanism of action is still not entirely understood. Even through inhibition of JAK2 plays a major role in the clinical response, there are also effects independent of JAK2 mutation 7, 8. It has been suggested that ruxolitinib may target cytokine signaling though inhibition of JAK2 as well as JAK1 7. Thus, combination of highly specific JAK2 inhibitors with JAK1 inhibitors may be beneficial for MPN patients. Expanded clinical trials and clinical practice will show whether secondary resistance occurs in MPNs, but lessons learned from imatinib resistance in chronic myelogenous leukemia suggest that increased oxidative stress may play a major factor in this process 36, 37. At least in cell line models, JAK2V617F is associated with increased levels of reactive oxygen species (ROS) 26, 38, further underlining the need to carefully monitor the mutational status of JAK2 (and JAK1) in patients that fail to respond to ruxolitinib and other JAK2 inhibitors. Our study may help to identify patients that fail to respond to novel JAK2 inhibitors and require alternative targeted therapies. In particular drugs that target JAK2 maturation (e.g. HSP90 inhibitors 39) or inhibit JAK2 downstream signaling (e.g. Pim kinase inhibitors 6, 40) would be of interest and deserve consideration in this patient group.
Acknowledgments
Financial support: This work is supported in part by National Institutes of Health grant CA134660-04, M.S.)
References
- 1.Levine RL, Gilliland DG. Myeloproliferative disorders. Blood. 2008;112:2190–2198. doi: 10.1182/blood-2008-03-077966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.James C, Ugo V, Le Couedic JP, Staerk J, Delhommeau F, Lacout C, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005;434:1144–1148. doi: 10.1038/nature03546. [DOI] [PubMed] [Google Scholar]
- 3.Lucet IS, Fantino E, Styles M, Bamert R, Patel O, Broughton SE, et al. The structural basis of Janus kinase 2 inhibition by a potent and specific pan-Janus kinase inhibitor. Blood. 2006;107:176–183. doi: 10.1182/blood-2005-06-2413. [DOI] [PubMed] [Google Scholar]
- 4.Williams NK, Bamert RS, Patel O, Wang C, Walden PM, Wilks AF, et al. Dissecting specificity in the Janus kinases: the structures of JAK-specific inhibitors complexed to the JAK1 and JAK2 protein tyrosine kinase domains. J Mol Biol. 2009;387:219–232. doi: 10.1016/j.jmb.2009.01.041. [DOI] [PubMed] [Google Scholar]
- 5.Lu X, Levine R, Tong W, Wernig G, Pikman Y, Zarnegar S, et al. Expression of a homodimeric type I cytokine receptor is required for JAK2V617F-mediated transformation. Proc Natl Acad Sci U S A. 2005;102:18962–18967. doi: 10.1073/pnas.0509714102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wernig G, Gonneville JR, Crowley BJ, Rodrigues MS, Reddy MM, Hudon HE, et al. The Jak2V617F oncogene associated with myeloproliferative diseases requires a functional FERM domain for transformation and for expression of the Myc and Pim proto-oncogenes. Blood. 2008;111:3751–3759. doi: 10.1182/blood-2007-07-102186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verstovsek S, Kantarjian H, Mesa RA, Pardanani AD, Cortes-Franco J, Thomas DA, et al. Safety and efficacy of INCB018424, a JAK1 and JAK2 inhibitor, in myelofibrosis. N Engl J Med. 2010;363:1117–1127. doi: 10.1056/NEJMoa1002028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pardanani A, Gotlib JR, Jamieson C, Cortes JE, Talpaz M, Stone RM, et al. Safety and efficacy of TG101348, a selective JAK2 inhibitor, in myelofibrosis. J Clin Oncol. 2011;29:789–796. doi: 10.1200/JCO.2010.32.8021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tefferi A, Pardanani A. JAK inhibitors in myeloproliferative neoplasms: rationale, current data and perspective. Blood Rev. 2011 doi: 10.1016/j.blre.2011.1006.1002. [DOI] [PubMed] [Google Scholar]
- 10.Hedvat M, Huszar D, Herrmann A, Gozgit JM, Schroeder A, Sheehy A, et al. The JAK2 inhibitor AZD1480 potently blocks Stat3 signaling and oncogenesis in solid tumors. Cancer Cell. 2009;16:487–497. doi: 10.1016/j.ccr.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pardanani A, Lasho T, Smith G, Burns CJ, Fantino E, Tefferi A. CYT387, a selective JAK1/JAK2 inhibitor: in vitro assessment of kinase selectivity and preclinical studies using cell lines and primary cells from polycythemia vera patients. Leukemia. 2009;23:1441–1445. doi: 10.1038/leu.2009.50. [DOI] [PubMed] [Google Scholar]
- 12.Quintas-Cardama A, Vaddi K, Liu P, Manshouri T, Li J, Scherle PA, et al. Preclinical characterization of the selective JAK1/2 inhibitor INCB018424: therapeutic implications for the treatment of myeloproliferative neoplasms. Blood. 2010;115:3109–3117. doi: 10.1182/blood-2009-04-214957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tyner JW, Bumm TG, Deininger J, Wood L, Aichberger KJ, Loriaux MM, et al. CYT387, a novel JAK2 inhibitor, induces hematologic responses and normalizes inflammatory cytokines in murine myeloproliferative neoplasms. Blood. 2010;115:5232–5240. doi: 10.1182/blood-2009-05-223727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wernig G, Kharas MG, Okabe R, Moore SA, Leeman DS, Cullen DE, et al. Efficacy of TG101348, a selective JAK2 inhibitor, in treatment of a murine model of JAK2V617F-induced polycythemia vera. Cancer Cell. 2008;13:311–320. doi: 10.1016/j.ccr.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 15.George DJ, Dionne CA, Jani J, Angeles T, Murakata C, Lamb J, et al. Sustained in vivo regression of Dunning H rat prostate cancers treated with combinations of androgen ablation and Trk tyrosine kinase inhibitors, CEP-751 (KT-6587) or CEP-701 (KT-5555) Cancer Res. 1999;59:2395–2401. [PubMed] [Google Scholar]
- 16.Hexner EO, Serdikoff C, Jan M, Swider CR, Robinson C, Yang S, et al. Lestaurtinib (CEP701) is a JAK2 inhibitor that suppresses JAK2/STAT5 signaling and the proliferation of primary erythroid cells from patients with myeloproliferative disorders. Blood. 2008;111:5663–5671. doi: 10.1182/blood-2007-04-083402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levis M, Allebach J, Tse KF, Zheng R, Baldwin BR, Smith BD, et al. A FLT3-targeted tyrosine kinase inhibitor is cytotoxic to leukemia cells in vitro and in vivo. Blood. 2002;99:3885–3891. doi: 10.1182/blood.v99.11.3885. [DOI] [PubMed] [Google Scholar]
- 18.Strock CJ, Park JI, Rosen M, Dionne C, Ruggeri B, Jones-Bolin S, et al. CEP-701 and CEP-751 inhibit constitutively activated RET tyrosine kinase activity and block medullary thyroid carcinoma cell growth. Cancer Res. 2003;63:5559–5563. [PubMed] [Google Scholar]
- 19.Cools J, Stover EH, Boulton CL, Gotlib J, Legare RD, Amaral SM, et al. PKC412 overcomes resistance to imatinib in a murine model of FIP1L1-PDGFRalpha-induced myeloproliferative disease. Cancer Cell. 2003;3:459–469. doi: 10.1016/s1535-6108(03)00108-9. [DOI] [PubMed] [Google Scholar]
- 20.Gorre ME, Mohammed M, Ellwood K, Hsu N, Paquette R, Rao PN, et al. Clinical resistance to STI-571 cancer therapy caused by BCR-ABL gene mutation or amplification. Science. 2001;293:876–880. doi: 10.1126/science.1062538. [DOI] [PubMed] [Google Scholar]
- 21.Pao W, Miller VA, Politi KA, Riely GJ, Somwar R, Zakowski MF, et al. Acquired resistance of lung adenocarcinomas to gefitinib or erlotinib is associated with a second mutation in the EGFR kinase domain. PLoS Med. 2005;2:e73. doi: 10.1371/journal.pmed.0020073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schindler T, Bornmann W, Pellicena P, Miller WT, Clarkson B, Kuriyan J. Structural mechanism for STI-571 inhibition of abelson tyrosine kinase. Science. 2000;289:1938–1942. doi: 10.1126/science.289.5486.1938. [DOI] [PubMed] [Google Scholar]
- 23.Tamborini E, Bonadiman L, Greco A, Albertini V, Negri T, Gronchi A, et al. A new mutation in the KIT ATP pocket causes acquired resistance to imatinib in a gastrointestinal stromal tumor patient. Gastroenterology. 2004;127:294–299. doi: 10.1053/j.gastro.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 24.Bikadi Z, Hazai E. Application of the PM6 semi-empirical method to modeling proteins enhances docking accuracy of AutoDock. J Cheminform. 2009;1:15. doi: 10.1186/1758-2946-1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morris GM, Goodsell DS, Halliday RS, Huey R, Hart WE, Belew RK, et al. Automated docking using a Lamarckian genetic algorithm and an empirical binding free energy function. J Comput Chem. 1998;19:1639–1662. [Google Scholar]
- 26.Walz C, Crowley BJ, Hudon HE, Gramlich JL, Neuberg DS, Podar K, et al. Activated Jak2 with the V617F point mutation promotes G1/S phase transition. J Biol Chem. 2006;281:18177–18183. doi: 10.1074/jbc.M600064200. [DOI] [PubMed] [Google Scholar]
- 27.Azam M, Latek RR, Daley GQ. Mechanisms of autoinhibition and STI-571/imatinib resistance revealed by mutagenesis of BCR-ABL. Cell. 2003;112:831–843. doi: 10.1016/s0092-8674(03)00190-9. [DOI] [PubMed] [Google Scholar]
- 28.Ray A, Cowan-Jacob SW, Manley PW, Mestan J, Griffin JD. Identification of BCR-ABL point mutations conferring resistance to the Abl kinase inhibitor AMN107 (nilotinib) by a random mutagenesis study. Blood. 2007;109:5011–5015. doi: 10.1182/blood-2006-01-015347. [DOI] [PubMed] [Google Scholar]
- 29.Bercovich D, Ganmore I, Scott LM, Wainreb G, Birger Y, Elimelech A, et al. Mutations of JAK2 in acute lymphoblastic leukaemias associated with Down's syndrome. Lancet. 2008;372:1484–1492. doi: 10.1016/S0140-6736(08)61341-0. [DOI] [PubMed] [Google Scholar]
- 30.Mullighan CG, Zhang J, Harvey RC, Collins-Underwood JR, Schulman BA, Phillips LA, et al. JAK mutations in high-risk childhood acute lymphoblastic leukemia. Proc Natl Acad Sci U S A. 2009;106:9414–9418. doi: 10.1073/pnas.0811761106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reiter A, Walz C, Watmore A, Schoch C, Blau I, Schlegelberger B, et al. The t(8;9)(p22;p24) is a recurrent abnormality in chronic and acute leukemia that fuses PCM1 to JAK2. Cancer Res. 2005;65:2662–2667. doi: 10.1158/0008-5472.CAN-04-4263. [DOI] [PubMed] [Google Scholar]
- 32.Yoda A, Yoda Y, Chiaretti S, Bar-Natan M, Mani K, Rodig SJ, et al. Functional screening identifies CRLF2 in precursor B-cell acute lymphoblastic leukemia. Proc Natl Acad Sci U S A. 2010;107:252–257. doi: 10.1073/pnas.0911726107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Azam M, Seeliger MA, Gray NS, Kuriyan J, Daley GQ. Activation of tyrosine kinases by mutation of the gatekeeper threonine. Nat Struct Mol Biol. 2008;15:1109–1118. doi: 10.1038/nsmb.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhao L, Dong H, Zhang CC, Kinch L, Osawa M, Iacovino M, et al. A JAK2 interdomain linker relays Epo receptor engagement signals to kinase activation. J Biol Chem. 2009;284:26988–26998. doi: 10.1074/jbc.M109.011387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hornakova T, Springuel L, Devreux J, Dusa A, Constantinescu SN, Knoops L, et al. Oncogenic JAK1 and JAK2-activating mutations resistant to ATP-competitive inhibitors. Haematologica. 2011;96:845–853. doi: 10.3324/haematol.2010.036350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koptyra M, Cramer K, Slupianek A, Richardson C, Skorski T. BCR/ABL promotes accumulation of chromosomal aberrations induced by oxidative and genotoxic stress. Leukemia. 2008;22:1969–1972. doi: 10.1038/leu.2008.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sattler M, Verma S, Shrikhande G, Byrne CH, Pride YB, Winkler T, et al. The BCR/ABL tyrosine kinase induces production of reactive oxygen species in hematopoietic cells. J Biol Chem. 2000;275:24273–24278. doi: 10.1074/jbc.M002094200. [DOI] [PubMed] [Google Scholar]
- 38.Reddy MM, Fernandes MS, Salgia R, Levine RL, Griffin JD, Sattler M. NADPH oxidases regulate cell growth and migration in myeloid cells transformed by oncogenic tyrosine kinases. Leukemia. 2011;25:281–289. doi: 10.1038/leu.2010.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marubayashi S, Koppikar P, Taldone T, Abdel-Wahab O, West N, Bhagwat N, et al. HSP90 is a therapeutic target in JAK2-dependent myeloproliferative neoplasms in mice and humans. J Clin Invest. 2010;120:3578–3593. doi: 10.1172/JCI42442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Swords R, Kelly K, Carew J, Nawrocki S, Mahalingam D, Sarantopoulos J, et al. The Pim Kinases: New Targets for Drug Development. Curr Drug Targets. 2011 doi: 10.2174/1389211217771934501. e-pub ahead of print 21 July 2011. [DOI] [PubMed] [Google Scholar]