Abstract
AIM: To report a meta-analysis of the studies that compared the laparoscopic with the open approach for colon cancer resection.
METHODS: Forty-seven manuscripts were reviewed, 33 of which employed for meta-analysis according to the PRISMA guidelines. The results were differentiated according to the study design (prospective randomized trials vs case-control series) and according to the tumor’s location. Outcome measures included: (1) short-term results (operating times, blood losses, bowel function recovery, post-operative pain, return to the oral intake, complications and hospital stay); (2) oncological adequateness (number of nodes harvested in the surgical specimens); and (3) long-term results (including the survivals’ rates and incidence of incisional hernias) and (4) costs.
RESULTS: Meta-analysis of trials provided evidences in support of the laparoscopic procedures for a several short-term outcomes including: a lower blood loss, an earlier recovery of the bowel function, an earlier return to the oral intake, a shorter hospital stay and a lower morbidity rate. Opposite the operating time has been confirmed shorter in open surgery. The same trend has been reported investigating case-control series and cancer by sites, even though there are some concerns regarding the power of the studies in this latter field due to the small number of trials and the small sample of patients enrolled. The two approaches were comparable regarding the mean number of nodes harvested and long-term results, even though these variables were documented reviewing the literature but were not computable for meta-analysis. The analysis of the costs documented lower costs for the open surgery, however just few studies investigated the incidence of post-operative hernias.
CONCLUSION: Laparoscopy is superior for the majority of short-term results. Future studies should better differentiate these approaches on the basis of tumors’ location and the post-operative hernias.
Keywords: Laparoscopy, Colon resection, Colon cancer, Meta-analysis, Evidence-based medicine
Core tip: This is a comprehensive meta-analysis of studies investigating laparoscopic resection in comparison with the open surgery for colon cancer, with the aim of evidencing short term and long term results of the surgical approaches. Results were provided according to the study designs (randomized trials, case control series) and according to the tumor’s location.
INTRODUCTION
Colon cancer remains a major health and social issue affecting in the US more than 100000 new patients/year[1]; the surgical resection remains the standard of care for treating and staging non-metastatic colon cancer. During the last twenty years several progresses were made for improving the treatments, the survivals and the quality of life of cancer patients; the main innovation in the surgical technique was that outbreak of the laparoscopy. The use of laparoscopy for colon resection has been introduced in 1991[2,3]. Initial concerns (including e.g., a long training/learning curve, the possible development of port-site metastasis and an inadequate oncologic resection[4-7]) were subsequently surmounted; indeed in recent years a number of studies recognized the adequateness of the laparoscopic approach along with a number of short-term functional benefits and equivalent long-term results. Nevertheless, the scientific literature in this field is quite heterogeneous regarding the study design adopted (randomized/non-randomized studies), objectives and outcome measures (short-term and log-term results, costs analysis), population enrolled (colon and/or rectal cancer patients), thus it might be difficult for clinicians and surgeons to summarize results and “take at home” univocal messages.
The aim of this manuscript is to review the studies comparing the laparoscopic and the open approach for colon cancer differentiating results by: (1) prospective randomized trials; (2) case-control series (including prospective and retrospective studies); and (3) the comparison of these techniques according to the tumor’s location. This type of differentiation is seldom conducted and might implement the analysis and help the readers in understanding the results. Moreover we focused our investigation on the costs’ analyses provided in the series and trials that were herein reviewed. Indeed, the goal of this paper is to divulgate a comprehensible meta-analysis of the evidences by each category of investigation and to provide a message of clinical use for clinicians and surgeons committed in the care of colon cancer patients.
MATERIALS AND METHODS
Data source and search strategies
This investigation has been conducted adhering at the PRISMA Statements for review and meta-analysis (Figure 1, Table 1). We conducted a systematic review of the literature by searching PubMed database for all the published series and trials comparing the laparoscopic and open surgical approach for colon cancer from 1995 to December 2012. Keywords: “laparoscopic vs open colectomy” AND “colon cancer”, languages: “English”, limit to “human” including clinical trials and comparative studies. We also included references from the retrieved publications. Duplicate references were removed by manual search.
Figure 1.
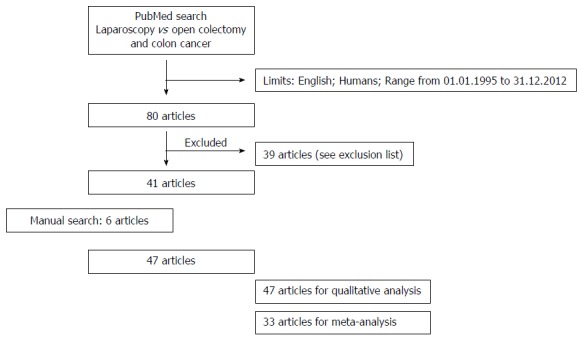
Study design. Study design according to the PRISMA statement for systematic reviews and meta-analysis.
Table 1.
Exclusion list of the manuscripts
| No. | Author | Ref. | Cause of exclusion |
| 1 | Sasaki J | J Nippon Med Sch 2012; 79:259-66 | Different outcome measure |
| 2 | Turagava J | N Z Med J 2012; 125: 17-26 | Only laparoscopy group |
| 3 | Poulsen M | J Gastrointest Surg 2012; 16: 1554-1558 | Only laparoscopy group |
| 4 | Roscio F | Int J Surg 2012; 10: 290-295 | Only laparoscopy group |
| 5 | Wang G | Hepatogastroenterology 2012; 59: 2158-2163 | Only laparoscopy group |
| 6 | Rottoli M | Surg Endosc 2012; 26: 1971-1976 | Different outcome measure |
| 7 | Campos FG | Surg Laparosc Endosc Percutan Tech 2011; 21: 327-333 | Exclusively familial polyposis patients |
| 8 | Panait L | Chirurgia (Bocur) 2011; 106: 475-478 | Only laparoscopy group |
| 9 | Hendren S | Dis Colon Rectum 2011; 54: 1362-1367 | Different outcome measure |
| 10 | Issa N | J Gastrointest Surg 2011; 15: 2011-2015 | Only laparoscopy group |
| 11 | McNicol FJ | Colorect Dis 2012; 14: 458-462 | Rectal cancers |
| 12 | Fujii S | Hepatogastroenterology 2011; 58: 406-410 | Only laparoscopy group |
| 13 | Akmal Y | Surg Endosc 2011; 25: 2967-2971 | Only laparoscopy group |
| 14 | Senthil M | Arch Surg 2010; 145: 840-843 | Different outcome measure |
| 15 | Han SA | Int J Colorect Dis 2010; 25: 631-638 | Different outcome measure |
| 16 | Park IJ | J Gastrointest Surg 2009; 13: 960-965 | Emergency resections |
| 17 | Heise CP | Dis Colon Rectum 2008; 51: 1790-1794 | Rectal cancers |
| 18 | Strhölein MA | Dis Colon Rectum 2008; 51: 385-391 | Rectal cancers |
| 19 | Moloo H | Dis Colon Rectum 2008; 51: 173-180 | Only laparoscopy group |
| 20 | Zhang H | Minim Invasiv Ther allied Technol 2007; 16: 187-191 | Rectal cancers |
| 21 | Polle SW | Surg Endosc 2007; 21:1301-1307 | Rectal cancers |
| 22 | Hasegawa H | Surg Endosc 2007; 21: 920-924 | Rectal cancers |
| 23 | Del Rio P | Minerva Chir 2006; 61: 923-927 | Only laparoscopy group |
| 24 | Schlachta CM | Surg Endosc 2007; 21: 396-369 | Only laparoscopy group |
| 25 | Wong DC | Tech Coloproctol 2006; 10: 37-42 | Rectal cancers |
| 26 | Moloo H | Dis Colon Rectum 2006; 49: 213-218 | Only laparoscopy group |
| 27 | Larson DW | Dis Colon Rectum 2005; 48: 1845-1850 | Rectal cancers |
| 28 | Kuhry E | Surg Endosc 2005; 19: 687-692 | Different outcome measure |
| 29 | Adaki Y | Hepatogastroenterology 2003; 50: 1348-1351 | Different outcome measure |
| 30 | Dunker MS | Dis Colon Rectum 2003; 46: 1238-1244 | Different outcome measure |
| 31 | Pasupathy S | Tech Coloproctol 2001; 5: 19-22 | Rectal cancers |
| 32 | Weeks JC | JAMA 2002; 287: 321-328 | Different outcome measure |
| 33 | Nelson H | Swiss Surg 2001; 7: 248-251 | Different outcome measure |
| 34 | Delgrado S | Dis Colon Rectum 2001; 44: 638-646 | Different outcome measure |
| 35 | Brown SR | Dis Colon Rectum 2001; 44: 397-400 | Rectal cancers |
| 36 | Marcello PW | Dis Colon Rectum 2000; 43: 604-608 | Rectal cancers |
| 37 | Hewitt PM | Dis Colon Rectum 1998; 41: 901-909 | Different outcome measure |
| 38 | Fukushima R | Dis Colon Rectum 1996; 39 (Suppl): S29-34 | Different outcome measure |
| 39 | Bokey EL | Dis Colon Rectum 1996; 39 (Suppl): S29-34 | Only laparoscopy group |
Authors of this study were blinded to authors’ and journals’ name while reviewing the series, and did not have any contacts with the authors of the included papers. We did not consider any journal’s scores (e.g., journal’s Impact Factors) of the published series as exclusion criteria for this review.
Study design and selection of papers
Each paper retrieved was assessed for inclusion or exclusion for this manuscript, by revision of the titles and the abstracts. Published series with the aim to investigate exclusively rectal carcinomas and/or non cancer-diseases (i.e., laparoscopic proctocolectomies for ulcerative colitis or diverticulitis) were excluded (Figure 1). Conversely manuscripts including few rectal cancers (or few non-malignant diseases) into the series, along with the other colon cancer localizations were included into this review.
Hand-assisted and totally laparoscopy procedures were considered altogether into the laparoscopic group, whereas all the open procedures (midline or transverse incisions) were considered as open resections.
All selected papers were categorized into the following sub-groups: (1) randomized studies; and (2) non-randomized studies (including prospective and retrospective case-control series).
Furthermore we identified those researches that investigated the comparison of these two approaches according to the tumor’s location (i.e., right side colectomies, left side colectomies and transverse resections) and highlighted within these groups the comparison of the costs derived by these two approaches.
Outcome measures
Whenever possible we collected data regarding: study design, population and power of the study, types of surgical procedure. We considered as short-term outcome measures: operating times (measured in minutes), blood loss (measured in milliliter), bowel function recovery (defined by the passage of the first flatus/stool; measured in days), post-operative pain (defined as the usage of analgesic -measured in days- and/or the score obtained by the visual analogue scale), return to the oral intake (usually liquid diet; measured in days), morbidity defined by peri-operative complications and hospital stay (measured in days).
Of note, since complications were often reported using different modalities (e.g., major vs minor complications, rate of adverse events etc.), we extrapolated the overall morbidity rate in each category (laparoscopic and open surgery) reported in all the investigated series.
The oncologic adequateness was recorded whenever considered by the authors as the mean number of lymph nodes harvested in the surgical specimen. Mean follow-up (months) was recorded and long-term outcome measures were considered as the rate of relapses, the survivals and the incidence of incisional hernias. The costs analysis has been conducted recording the overall hospital costs for both procedures, providing results in US dollars, in order to analyze a single currency.
We did not considered conversion surgery, since it might bias the results of the open surgery procedures. On the same extent we did not consider the hospital volume, since it is seldom reported, even though the learning curves and the volume of patients might vary short-term results and costs.
A first analysis has been conducted reviewing papers in each category (prospective-randomized trials; case control series; studies investigating cancer by sites) and highlighting in each article were the evidences stand for (e.g., significant statistical analyses supporting laparoscopy or open surgery) for the different outcome measures (e.g., considering the operating time, blood losses etc.). Moreover and whenever computable we provided a meta-analysis of the results.
Statistical analysis
Continuous variables were analysed using means, medians and standard deviations, whereas categorical variables were analysed using frequencies and percents. Statistical analyses and Meta-analysis were performed using MedCalc for Windows, version 10.2.0.0 (MedCalc Software, MariaKerke, Belgium). In order to provide significant results, a meta-analysis has been conducted for all variables in different categories (prospective-randomized trials; case control series; studies investigating cancer by sites) whenever at least 3 studies provided data computable.
The Mantel-Haenszel method was used for calculating the weighted summary Odds ratio under the fixed effects model. Next the heterogeneity statistic is incorporated to calculate the summary odds ratio under the random effects model. The total odds ratio with 95%CI is given both for the Fixed effects model and the Random effects model. If the value 1 is not within the 95%CI, then the Odds ratio is statistically significant at the 5% level (P < 0.05).
For meta-analysis of studies with a continuous measure (comparison of means between treated cases and controls), the Hedges g statistic was used as a formulation for the standardized mean difference (SMD) under the fixed effects model. Next the heterogeneity statistic is incorporated to calculate the summary standardized mean difference under the random effects model. If the value 0 is not within the 95%CI, then the SMD is statistically significant at the 5% level (P < 0.05).
Statistical heterogeneity of the results of the trials was assessed on the basis of a test of heterogeneity (standard chi-squared test on N degrees of freedom where N equals the number of trials contributing data minus one). Three possible causes for heterogeneity were pre-specified: (1) differing response according to difference in the quality of the trial; (2) differing response according to sample size; and (3) differing response according to clinical heterogeneity. If the test of heterogeneity is statistically significant (P < 0.05) then more emphasis should be placed on the random effects model.
RESULTS
Figure 1 outlines the study design. PubMed search provided 80 results, however 39 studies were excluded due to different outcome measures (e.g., investigations aimed to outline the quality of life or the immunological response), due to the evaluation of the laparoscopy procedures per se (missing the open surgery group) or evaluating rectal cancer patients (see exclusion list). All the 47 articles retrieved were included in the systematic review, however only 33 articles provided data computable for meta-analysis.
Randomized controlled trials
Figure 2 outlines results of this analysis. 11 studies were included for review[8-18] from 1995 to 2012, including overall 2992 patients in the laparoscopy group and 2717 in the open surgery group. Of note 4 studies enrolled less than 50 patients/arm[8,10-11,13]. The systematic review of the manuscripts documented a number of benefits of the laparoscopic procedure for the vast majority of the short-term outcome measures (bowel function recovery, return to the oral intake, post-operative pain, blood loss and hospital stay), whereas it was documented a longer operating time comparing the open approach. Of note, all the studies - with the exclusion of the first trial conducted by Lacy and co-authors in 1995[8] - reported a comparable morbidity rate within the two approaches. Similarly the mean count of the nodes harvested (LNH) in the surgical specimens were similar in the 3 studies investigating this variable[8-9,15], and the survivals were reported homogeneous in the vast majority of the studies[11,12,14,17,18], with the sole exception of the trial conducted by Lacy in 2002[9]. It seems important to highlight that only two randomized trials investigated the incidence of post-operative hernias[10,14], reporting a comparable rate of events (Figure 2A).
Figure 2.
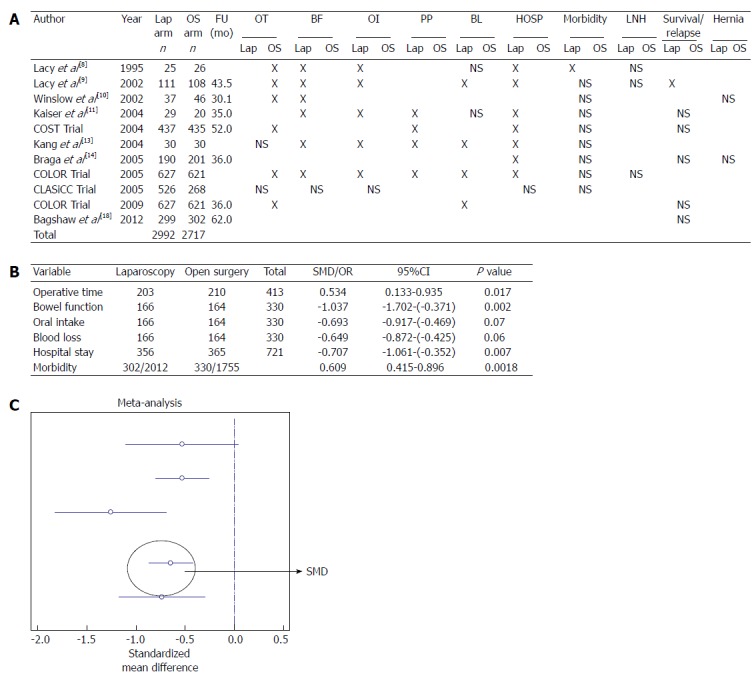
Randomized studies. A: Randomized trails comparing laparoscopy and open surgery. X in the table refers to a statistical association provided in the studies; B: Meta-analysis of the out-come measures; C: Forest plot graph regarding studies investigating blood loss. Lap arm: Laparoscopy arm; OS arm: Open surgery arm; FU: Mean follow-up; OT: Operative time; BF: Bowel function; OI: Oral intake; PP: Post-operative Pain; BL: Blood loss; HOSP: Hospital stay; LNH: Lymph node harvest; NS: Not significant.
Meta-analysis conducted on 9 studies in this group[8-16] confirmed the evidences of the short-term outcome measures in favour of the laparoscopy (bowel function recovery, return to the oral intake, blood loss and hospital stay), plus it documented a better morbidity rate for the laparoscopy group (OR = 0.609; 95%CI: 0.415-0.896). Conversely the operating time has been confirmed shortly in the open procedure group (Figure 2B and C).
Case-control studies
Figure 3 reports data from this analysis. 16 case-control studies were included, counting overall 3819 patients in the laparoscopy group and 6990 in the open surgery group[19-34]. The vast majority of these studies agree in reporting shorter operating time in the open surgery group comparing with the laparoscopic procedures, with the exceptions of the studies conducted by Saba, Bilimoira and de Campos Lobato that provided homogeneous results[19,27,30]. All studies investigating the bowel function recovery recognized a benefit for the laparoscopy procedure[19,21-22,24,26]; similarly the investigation of the return to the oral intake provided homogeneous results in the 2 studies that investigated this outcome measure[19,29].
Figure 3.
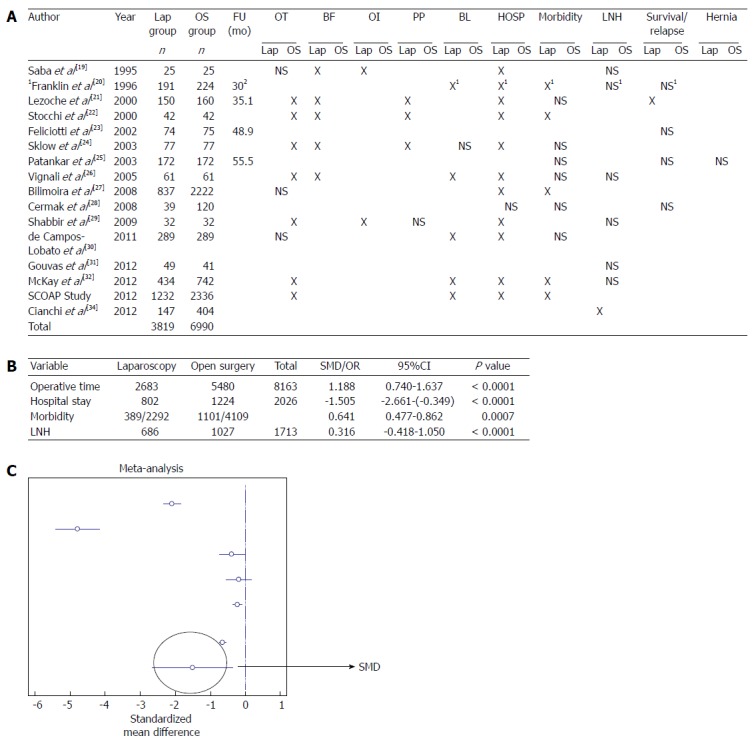
Non-randomized studies. A: Case-control studies comparing laparoscopy and open surgery. X in the table refers to a statistical association provided in the studies; B: Meta-analysis of the out-come measures; C: Forest plot graph regarding studies investigating hospital stay. 1Statistic analysis not performed; 2Significant difference of follow-up according to the stage of the disease. Lap: Laparoscopy; OS: Open surgery; FU: Mean follow-up; OT: Operative time; BF: Bowel function; OI: Oral intake; PP: Post-operative Pain; BL: Blood loss; HOSP: Hospital stay; LNH: Lymph node harvest; NS: Not significant.
Even if Shabbir reported a similar use of analgesic in the post-operatory recovery[22], the other studies reported significant benefits associated with the laparoscopic procedure in this field[21,22,24]. A significant reduction in the blood loss for the patients undergone laparoscopy has been reported by all the authors[20,26,30,32,33], with the sole exception of Slow[24]. The hospital stay has been reported in favour of the laparoscopy group in all the studies, with the exclusion of the series investigated by Cermak et al[28] in 2008. The study of the morbidity rate provided dis-homogeneous results: even though some studies documented some benefits in the laparoscopy group[20,22,27,32,33], others documented comparable results between the 2 approaches[21,24-26,28,30]. Notably, Cianchi in 2012 highlighted a better LNH in the laparoscopy group[34], whereas the others reported homogeneous results.
Similarly, with the exception of Lezoche et al[21], the authors reported comparable survival rates within these 2 approaches. Seems important to highlight that the vast majority of the studies did not investigate the rate of post-operative hernias, with the sole exception of Pantankar in 2008[25] that reported similar results in the 2 groups.
A meta-analysis has been conducted for 11 studies in this category[20-22,24-28,30,32,33], Figure 3B. The operative time has been reported longer in the laparoscopy group, whereas this procedure showed a shorter hospital stay, Figure 3C. Interestingly the meta-analysis provided also in this category of studies some evidences regarding a lower rate of morbidity in the post-operative period following a laparoscopy operation (OR = 0.644; 95%CI: 0.447-0.862). The analysis of the LNH variable was not of statistical value (95%CI: -0.418-1.050).
Right-sided colectomies
We identified 10 studies in this category[24,35-43], involving 427 laparoscopy patients and 485 open colectomy patients, Figure 4. Overall we included 8 case-control series[24,35-38,41-43] and 2 randomized trials[39,40]. Of note the open surgical approach (midline vs transverse incisions) has been categorized exclusively in 4 studies[39,40,42,43]. All the studies analysed documented homogeneous results regarding the hospital stay (statistically better associated with the laparoscopy approach), LNH and survival rate (comparable results between the 2 procedures). Discordant data were documented for the operating time: even though the vast majority of the authors reported a shorter operation in the open group, the studies conducted by Zheng in 2005 and by Nakamura in 2009 documented comparable results[36,41]. The bowel function recovery has been reported shorter in the laparoscopy group in the studies conducted by Lezoche, Slow, Zeng, Chung and Tanis[24,35,36,39,43], whereas other 2 articles provided similar recoveries for both groups[37,38]. Three studies reported comparable results within the 2 surgical approaches regarding the return to the oral intake[36,37,43]; opposite Tong, Chung and Braga[38-40] reported results in favour of the laparoscopy group. Zeng, Chung and Slow (exclusively in patients < 75 years old)[24,36,39] reported a lower use of analgesics in the laparoscopy group, whereas Lohsiriwat and Tanis failed in reporting a statistical association[37,43]. Within the laparoscopy procedures, all the authors with the exceptions of Lohsiriwat and Tong[37,38], documented lower blood losses. Also in this category, the investigation of the rate of post-operative hernias has been conducted in a single study[42].
Figure 4.
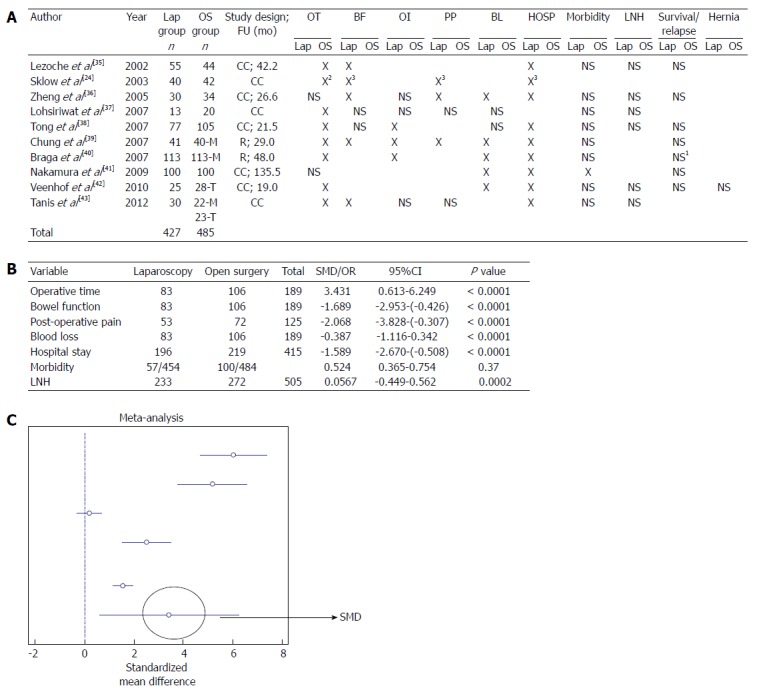
Right sided colectomies. A: Studies comparing right-side laparoscopy colectomy and open surgery. X in the table refers to a statistical association provided in the studies; B: Meta-analysis of the out-come measures; C: Forest plot graph regarding studies investigating operative time. 1Statistic analysis not performed; 2Exclusively if patients > 75 years old; 3Exclusively if patients < 75 years old. Lap: Laparoscopy; OS: Open surgery; M: Midline incision; T: transverse incision R: Randomized, CC: Case-control; FU: Mean follow-up; OT: Operative time; BF: Bowel function; OI: Oral intake; PP: Post-operative Pain; BL: Blood loss; HOSP: Hospital stay; LNH: Lymph node harvest; NS: Not significant.
A meta-analysis has been conducted or 9 manuscripts[24,35-42] within this category, Figure 4B. Significant evidences were highlighted for the laparoscopy procedures regarding the bowel function recovery, post-operative pain, blood losses, hospital stay and interestingly for the morbidity rate (OR = 0.524; 95%CI: 0.365-0.754). Also in this category the investigation of the LNH variable was not of statistical value (95%CI: -0.4149-0.562). Conversely the operating time has been confirmed shorter in the open surgery group, Figure 4C.
Left-sided colon cancers
Seven studies were included in this category[24,35,44-48], encompassing 1608 patients undergone laparoscopy and 9981 patients undergone open surgical resections, Figure 5. Three studies were randomized[44,45,47], the remaining were case-control studies. It seems important to highlight that 3 studies enrolled less than 50 patients/arm[24,47,48]. The analyses of the bowel function recovery, the return to the oral intake, the post-operative pain and the survival rates provided homogeneous results among studies (benefits for the laparoscopy patients for the short-term outcome measures, comparable results between the 2 approaches for long term survivals). The operating time has been reported in favour of the open approach in all the studies with the exception of Cheung et al[47]. Conversely the analysis of the blood losses was in favour of the laparoscopy procedures in all the researches, excluding the article by Leung et al[44]. A shorter hospital stay has been reported statistically associated to the laparoscopy procedure in all the studies with the sole exclusion of the report by Cheung et al[47].
Figure 5.
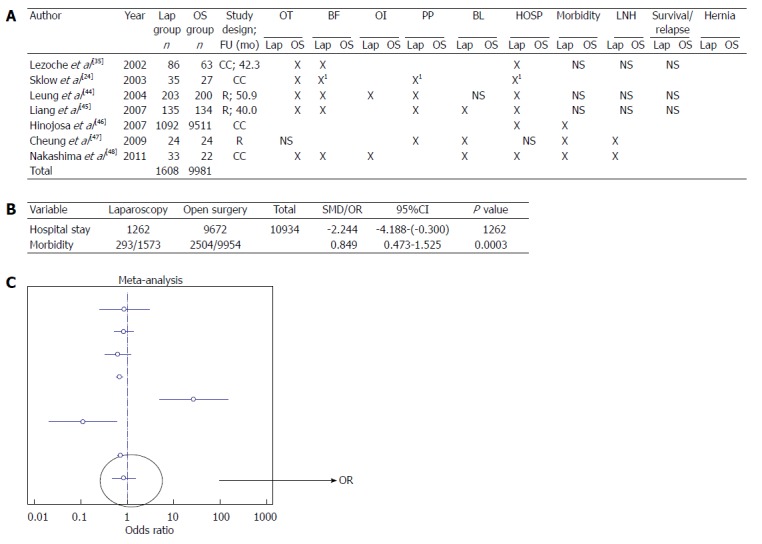
Left sided colectomies. A: Studies comparing left-side laparoscopy colectomy and open surgery. X in the table refers to a statistical association provided in the studies; B: Meta-analysis of the out-come measures; C: Forest plot graph regarding studies investigating morbidity rate. 1Exclusively if patients > 75 years old. Lap: Laparoscopy; OS: Open surgery; M: Midline incision; T: transverse incision R: Randomized, CC: Case-control; FU: Mean follow-up; OT: Operative time; BF: Bowel function; OI: Oral intake; PP: Post-operative Pain; BL: Blood loss; HOSP: Hospital stay; LNH: Lymph node harvest; NS: Not significant.
Interestingly the analysis of the morbidity rate provided discordant data: 3 studies reported benefits for the laparoscopy procedure[46-48], whereas other 3 studies reported comparable results[35,44,45]. Notably the analysis of the LNH reported homogeneous results among different studies, with the exceptions of Cheung and Nakashima[47,48].
A meta-analysis has been provided including all the 7 studies, but it was computable for only two variables (Figure 5B) and interestingly both the hospital stay and the morbidity rate were confirmed in favour of the laparoscopy group, Figure 5C.
Transverse colon cancers
Three studies were included in this category of investigation[49-51], including 124 patients in the laparoscopy group and 141 in the open surgery group, Figure 6. All the studies were case-controls series with some concerns regarding the power of the analyses due to the small samples enrolled. These studies reported homogeneous results in favour of the laparoscopy procedures for the bowel function recovery and the intra-operative blood loss. Notably all the studies documented similar morbidity rates for both surgical approaches. The studies conducted by Kim et al[49] and by Fernández-Cebrián et al[51] documented comparable operating times, whereas Akiyoshi et al[50] reported benefits in this field in the open surgery group. Fernández-Cebrián et al[51] documented comparable results within the 2 procedures regarding the return to the oral intake, whereas the others documented a statistical correlation with the laparoscopy procedure[49,50]. The hospital stay has been reported comparable by Kim and by Fernández-Cebrián[49,51], whereas Akiyoshi et al[50] reported a shorter hospitalization in the laparoscopy group. The analysis of the LNH reported similar results between the surgical procedures in the studies conducted by Kim et al[49] and by Fernández-Cebrián et al[51], whereas Akiyoshi et al[50] documented a higher mean number of nodes harvested in the open surgery group. None of these studies investigated the survivals or the incidence of post-operative hernias.
Figure 6.
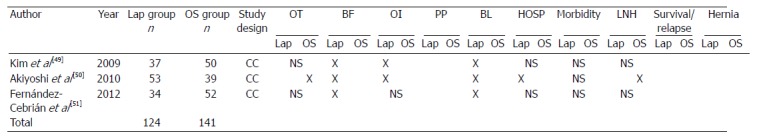
Transverse colectomies. Studies comparing transverse laparoscopy colectomy and open surgery. X in the table refers to a statistical association provided in the studies. Lap: Laparoscopy; OS: Open surgery; M: Midline incision; T: transverse incision; R: Randomized; CC: Case-control; OT: Operative time; BF: Bowel function; OI: Oral intake; PP: Post-operative Pain; BL: Blood loss; HOSP: Hospital stay; LNH: Lymph node harvest; NS: Not significant.
It was not possible to computable data for meta-analysis within this category of investigation.
Costs analysis
Nine studies were included in this investigation[19,29,36,44-46,52-54], including 3 randomized trials[44,45,52], Figure 7. The overall number of patients pooled in the laparoscopy group has been of 102763; otherwise 72264 patients were included in the open surgery group. Costs were expressed or converted whenever necessary in United States dollars. Overall laparoscopy procedures provided costs ranging from $4000 to $41000; conversely the open surgery expenses were ranging from $1800 to $43000. 4 studies were meta-analysed[36,44-46]. Results of the meta-analysis confirmed a significant reduction of the costs in the open surgery group comparing with laparoscopy (SMD = 4.843; 95%CI: 3.031-6.656), Figure 7B and C.
Figure 7.
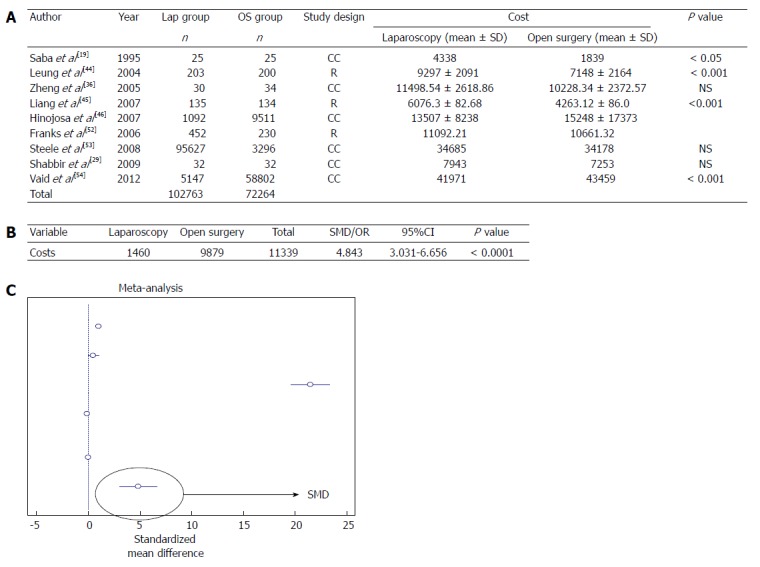
Costs analysis. A: Studies comparing laparoscopy and open surgery: analysis of the costs; B: Meta-analysis; C: Forest plot graph. Lap: Laparoscopy; OS: Open surgery; NS: Not significant; R: Randomized; CC: Case-control.
DISCUSSION
The primary goal of this manuscript was to divulgate the evidences obtained reviewing 47 manuscripts in this field, 33 of which provided data computable for meta-analysis; the results were categorized on the basis of the study design (randomized trials, case-control series) and on the basis of the tumor locations. Moreover we conducted an analysis of the costs derived by the two surgical procedures. Our results are in agreement with that of other meta-analyses in this field documenting better short-term results in the laparoscopy groups comparing with the open surgery procedures[55,56], even though it is associated with a significant longer operative time.
We considered any complications provided by different studies in the “morbidity rate” outcome measure, since it was very difficult to provide homogeneous results reviewing studies in this field; indeed authors considered different complications in the analyzed studies (infections, bleeding etc.). The interpretation of results, however, might be implemented if future studies could stratify the severity of adverse events using standard classifications (e.g., the Clavien’s classification)[57].
Nevertheless, the laparoscopy procedure for colon cancer resection has been reported oncologically safe[58,59]. The same results were reporting analysing exclusively right-sided colectomies[60]. In the field of the evaluation of resections by cancers’ site, we noted that still to-date few studies compared the right-side colectomy by transverse incisions with the laparoscopy procedures; indeed as highlighted by Tanis et al[43] the short-term results obtained by the transverse incisions are often between laparoscopy and the midline approach. It is our opinion that this field of studies should be implemented. Moreover in the field of left-side colectomies the some series pool left-sided and recto-sigmoid cancers[45,46], thus it is often difficult to differentiate “pure” colectomies from the recto-sigmoid resections. Of note just 4 studies out of the 47 reviewed, investigated the rate of post-operative hernias, providing homogeneous results comparing the 2 methodologies[11,14,25,42], thus also this field of investigation should be implemented by incoming studies.
Take at home messages
Short term outcome measures including: a lower blood loss, an earlier recovery of the bowel function, an earlier return to the oral intake, a shorter hospital stay and a lower morbidity rate were statistically associated to the laparoscopic procedures in randomized trials. Opposite the operating time has been confirmed shorter in the open surgery group.
Even though the majority of the trials reported a statistical association with less post-operative pain in the laparoscopic group, this data was not computable on meta-analysis, similarly the comparable results of the LNH within the 2 procedures was documented at the review but not computable at the meta-analysis.
This trend has been confirmed analyzing case-control series and cancer by sites, even though there are some concerns regarding the power of the studies in this latter field due to the small number of trials and the small sample of patients often enrolled.
The analysis of the costs documented lower costs for the open surgery procedures, however seems important to highlight that just few studies investigated the incidence of post-operative hernia. The analysis of the post-operative hernia could add important information; indeed a re-intervention might substantially implement the costs and might put into question the cost-effectiveness of the procedure.
COMMENTS
Background
Colon cancer is a major health issue. Over the last twenty years several progresses were made for improving the treatment and the quality of life of cancer patients, and the main innovation in the field of colon cancer surgical technique was that outbreak of the laparoscopy procedures (minimally-invasive treatments).
Research frontiers
Several studies recognized the adequateness of the laparoscopic approach along with a number of short-term functional benefits and equivalent long-term results comparing to “open” approach. Nevertheless, the scientific literature in this field is quite heterogeneous, thus it might be difficult for clinicians and surgeons to summarize results and “take at home” univocal messages.
Innovations and breakthroughs
The goal of this paper is to divulgate a comprehensible meta-analysis of the evidences and to provide a message of clinical use for clinicians and surgeons committed in the care of colon cancer patients.
Applications
The results are in agreement with that of other meta-analyses in this field documenting better short-term results in the laparoscopy groups comparing with the open surgery procedures, even though it is associated with a significant longer operative time.
Peer review
This is a comprehensive review and meta-analysis of laparoscopic vs open colectomy for colon cancer. It’s well-written with a solid analysis.
Footnotes
Supported by The PhD University Grant program “Clinical and Experimental Research Methodologies in Oncology” provided by the Faculty of Medicine and Psychology University of Rome “La Sapienza” to La Torre M
P- Reviewers: Gayet B, Sing RF S- Editor: Zhai HH L- Editor: A E- Editor: Zhang DN
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Fowler DL, White SA. Laparoscopy-assisted sigmoid resection. Surg Laparosc Endosc. 1991;1:183–188. [PubMed] [Google Scholar]
- 3.Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy) Surg Laparosc Endosc. 1991;1:144–150. [PubMed] [Google Scholar]
- 4.Jacquet P, Averbach AM, Jacquet N. Abdominal wall metastasis and peritoneal carcinomatosis after laparoscopic-assisted colectomy for colon cancer. Eur J Surg Oncol. 1995;21:568–570. doi: 10.1016/s0748-7983(95)97564-0. [DOI] [PubMed] [Google Scholar]
- 5.Akle CA. Early parietal recurrence of adenocarcinoma of the colon after laparoscopic colectomy. Port site metastasis after laparascopic colorectal surgery for cure of malignancy. Br J Surg. 1996;83:427. doi: 10.1002/bjs.1800830353. [DOI] [PubMed] [Google Scholar]
- 6.Wexner SD, Cohen SM. Port site metastases after laparoscopic colorectal surgery for cure of malignancy. Br J Surg. 1995;82:295–298. doi: 10.1002/bjs.1800820305. [DOI] [PubMed] [Google Scholar]
- 7.Ramos JM, Gupta S, Anthone GJ, Ortega AE, Simons AJ, Beart RW. Laparoscopy and colon cancer. Is the port site at risk? A preliminary report. Arch Surg. 1994;129:897–89; discussion 900. doi: 10.1001/archsurg.1994.01420330011001. [DOI] [PubMed] [Google Scholar]
- 8.Lacy AM, García-Valdecasas JC, Piqué JM, Delgado S, Campo E, Bordas JM, Taurá P, Grande L, Fuster J, Pacheco JL. Short-term outcome analysis of a randomized study comparing laparoscopic vs open colectomy for colon cancer. Surg Endosc. 1995;9:1101–1105. doi: 10.1007/BF00188996. [DOI] [PubMed] [Google Scholar]
- 9.Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224–2229. doi: 10.1016/S0140-6736(02)09290-5. [DOI] [PubMed] [Google Scholar]
- 10.Winslow ER, Fleshman JW, Birnbaum EH, Brunt LM. Wound complications of laparoscopic vs open colectomy. Surg Endosc. 2002;16:1420–1425. doi: 10.1007/s00464-002-8837-3. [DOI] [PubMed] [Google Scholar]
- 11.Kaiser AM, Kang JC, Chan LS, Vukasin P, Beart RW. Laparoscopic-assisted vs. open colectomy for colon cancer: a prospective randomized trial. J Laparoendosc Adv Surg Tech A. 2004;14:329–334. doi: 10.1089/lap.2004.14.329. [DOI] [PubMed] [Google Scholar]
- 12.Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050–2059. doi: 10.1056/NEJMoa032651. [DOI] [PubMed] [Google Scholar]
- 13.Kang JC, Chung MH, Chao PC, Yeh CC, Hsiao CW, Lee TY, Jao SW. Hand-assisted laparoscopic colectomy vs open colectomy: a prospective randomized study. Surg Endosc. 2004;18:577–581. doi: 10.1007/s00464-003-8148-3. [DOI] [PubMed] [Google Scholar]
- 14.Braga M, Frasson M, Vignali A, Zuliani W, Civelli V, Di Carlo V. Laparoscopic vs. open colectomy in cancer patients: long-term complications, quality of life, and survival. Dis Colon Rectum. 2005;48:2217–2223. doi: 10.1007/s10350-005-0185-7. [DOI] [PubMed] [Google Scholar]
- 15.Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477–484. doi: 10.1016/S1470-2045(05)70221-7. [DOI] [PubMed] [Google Scholar]
- 16.Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718–1726. doi: 10.1016/S0140-6736(05)66545-2. [DOI] [PubMed] [Google Scholar]
- 17.Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10:44–52. doi: 10.1016/S1470-2045(08)70310-3. [DOI] [PubMed] [Google Scholar]
- 18.Bagshaw PF, Allardyce RA, Frampton CM, Frizelle FA, Hewett PJ, McMurrick PJ, Rieger NA, Smith JS, Solomon MJ, Stevenson AR. Long-term outcomes of the australasian randomized clinical trial comparing laparoscopic and conventional open surgical treatments for colon cancer: the Australasian Laparoscopic Colon Cancer Study trial. Ann Surg. 2012;256:915–919. doi: 10.1097/SLA.0b013e3182765ff8. [DOI] [PubMed] [Google Scholar]
- 19.Saba AK, Kerlakian GM, Kasper GC, Hearn AT. Laparoscopic assisted colectomies versus open colectomy. J Laparoendosc Surg. 1995;5:1–6. doi: 10.1089/lps.1995.5.1. [DOI] [PubMed] [Google Scholar]
- 20.Franklin ME, Rosenthal D, Abrego-Medina D, Dorman JP, Glass JL, Norem R, Diaz A. Prospective comparison of open vs. laparoscopic colon surgery for carcinoma. Five-year results. Dis Colon Rectum. 1996;39:S35–S46. doi: 10.1007/BF02053804. [DOI] [PubMed] [Google Scholar]
- 21.Lezoche E, Feliciotti F, Paganini AM, Guerrieri M, Campagnacci R, De Sanctis A. Laparoscopic colonic resections versus open surgery: a prospective non-randomized study on 310 unselected cases. Hepatogastroenterology. 2000;47:697–708. [PubMed] [Google Scholar]
- 22.Stocchi L, Nelson H, Young-Fadok TM, Larson DR, Ilstrup DM. Safety and advantages of laparoscopic vs. open colectomy in the elderly: matched-control study. Dis Colon Rectum. 2000;43:326–332. doi: 10.1007/BF02258297. [DOI] [PubMed] [Google Scholar]
- 23.Feliciotti F, Paganini AM, Guerrieri M, Sanctis A, Campagnacci R, Lezoche E. Results of laparoscopic vs open resections for colon cancer in patients with a minimum follow-up of 3 years. Surg Endosc. 2002;16:1158–1161. doi: 10.1007/s00464-001-8333-1. [DOI] [PubMed] [Google Scholar]
- 24.Sklow B, Read T, Birnbaum E, Fry R, Fleshman J. Age and type of procedure influence the choice of patients for laparoscopic colectomy. Surg Endosc. 2003;17:923–929. doi: 10.1007/s00464-002-8949-9. [DOI] [PubMed] [Google Scholar]
- 25.Patankar SK, Larach SW, Ferrara A, Williamson PR, Gallagher JT, DeJesus S, Narayanan S. Prospective comparison of laparoscopic vs. open resections for colorectal adenocarcinoma over a ten-year period. Dis Colon Rectum. 2003;46:601–611. doi: 10.1007/s10350-004-6616-z. [DOI] [PubMed] [Google Scholar]
- 26.Vignali A, Di Palo S, Tamburini A, Radaelli G, Orsenigo E, Staudacher C. Laparoscopic vs. open colectomies in octogenarians: a case-matched control study. Dis Colon Rectum. 2005;48:2070–2075. doi: 10.1007/s10350-005-0147-0. [DOI] [PubMed] [Google Scholar]
- 27.Bilimoria KY, Bentrem DJ, Merkow RP, Nelson H, Wang E, Ko CY, Soper NJ. Laparoscopic-assisted vs. open colectomy for cancer: comparison of short-term outcomes from 121 hospitals. J Gastrointest Surg. 2008;12:2001–2009. doi: 10.1007/s11605-008-0568-x. [DOI] [PubMed] [Google Scholar]
- 28.Cermak K, Thill V, Simoens CH, Smets D, Ngongang CH, da Costa PM. Surgical resection for colon cancer: laparoscopic assisted vs. open colectomy. Hepatogastroenterology. 2008;55:412–417. [PubMed] [Google Scholar]
- 29.Shabbir A, Roslani AC, Wong KS, Tsang CB, Wong HB, Cheong WK. Is laparoscopic colectomy as cost beneficial as open colectomy? ANZ J Surg. 2009;79:265–270. doi: 10.1111/j.1445-2197.2009.04857.x. [DOI] [PubMed] [Google Scholar]
- 30.de Campos-Lobato LF, Alves-Ferreira PC, Geisler DP, Kiran RP. Benefits of laparoscopy: does the disease condition that indicated colectomy matter? Am Surg. 2011;77:527–533. [PubMed] [Google Scholar]
- 31.Gouvas N, Pechlivanides G, Zervakis N, Kafousi M, Xynos E. Complete mesocolic excision in colon cancer surgery: a comparison between open and laparoscopic approach. Colorectal Dis. 2012;14:1357–1364. doi: 10.1111/j.1463-1318.2012.03019.x. [DOI] [PubMed] [Google Scholar]
- 32.McKay GD, Morgan MJ, Wong SK, Gatenby AH, Fulham SB, Ahmed KW, Toh JW, Hanna M, Hitos K. Improved short-term outcomes of laparoscopic versus open resection for colon and rectal cancer in an area health service: a multicenter study. Dis Colon Rectum. 2012;55:42–50. doi: 10.1097/DCR.0b013e318239341f. [DOI] [PubMed] [Google Scholar]
- 33.Kwon S, Billingham R, Farrokhi E, Florence M, Herzig D, Horvath K, Rogers T, Steele S, Symons R, Thirlby R, et al. Adoption of laparoscopy for elective colorectal resection: a report from the Surgical Care and Outcomes Assessment Program. J Am Coll Surg. 2012;214:909–18.e1. doi: 10.1016/j.jamcollsurg.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cianchi F, Cortesini C, Trallori G, Messerini L, Novelli L, Comin CE, Qirici E, Bonanomi A, Macrì G, Badii B, et al. Adequacy of lymphadenectomy in laparoscopic colorectal cancer surgery: a single-centre, retrospective study. Surg Laparosc Endosc Percutan Tech. 2012;22:33–37. doi: 10.1097/SLE.0b013e31824332dc. [DOI] [PubMed] [Google Scholar]
- 35.Lezoche E, Feliciotti F, Paganini AM, Guerrieri M, De Sanctis A, Minervini S, Campagnacci R. Laparoscopic vs open hemicolectomy for colon cancer. Surg Endosc. 2002;16:596–602. doi: 10.1007/s00464-001-9053-2. [DOI] [PubMed] [Google Scholar]
- 36.Zheng MH, Feng B, Lu AG, Li JW, Wang ML, Mao ZH, Hu YY, Dong F, Hu WG, Li DH, et al. Laparoscopic versus open right hemicolectomy with curative intent for colon carcinoma. World J Gastroenterol. 2005;11:323–326. doi: 10.3748/wjg.v11.i3.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lohsiriwat V, Lohsiriwat D, Chinswangwatanakul V, Akaraviputh T, Lert-Akyamanee N. Comparison of short-term outcomes between laparoscopically-assisted vs. transverse-incision open right hemicolectomy for right-sided colon cancer: a retrospective study. World J Surg Oncol. 2007;5:49. doi: 10.1186/1477-7819-5-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tong DK, Law WL. Laparoscopic versus open right hemicolectomy for carcinoma of the colon. JSLS. 2007;11:76–80. [PMC free article] [PubMed] [Google Scholar]
- 39.Chung CC, Ng DC, Tsang WW, Tang WL, Yau KK, Cheung HY, Wong JC, Li MK. Hand-assisted laparoscopic versus open right colectomy: a randomized controlled trial. Ann Surg. 2007;246:728–733. doi: 10.1097/SLA.0b013e318123fbdf. [DOI] [PubMed] [Google Scholar]
- 40.Braga M, Frasson M, Vignali A, Zuliani W, Di Carlo V. Open right colectomy is still effective compared to laparoscopy: results of a randomized trial. Ann Surg. 2007;246:1010–1014; discussion 1014-1015. doi: 10.1097/SLA.0b013e31815c4065. [DOI] [PubMed] [Google Scholar]
- 41.Nakamura T, Onozato W, Mitomi H, Naito M, Sato T, Ozawa H, Hatate K, Ihara A, Watanabe M. Retrospective, matched case-control study comparing the oncologic outcomes between laparoscopic surgery and open surgery in patients with right-sided colon cancer. Surg Today. 2009;39:1040–1045. doi: 10.1007/s00595-009-4011-z. [DOI] [PubMed] [Google Scholar]
- 42.Veenhof AA, Van Der Pas MH, Van Der Peet DL, Bonjer HJ, Meijerink WJ, Cuesta MA, Engel AF. Laparoscopic versus transverse Incision right colectomy for colon carcinoma. Colorectal Dis. 2010:Epub ahead of print. doi: 10.1111/j.1463-1318.2010.02413.x. [DOI] [PubMed] [Google Scholar]
- 43.Tanis E, van Geloven AA, Bemelman WA, Wind J. A comparison of short-term outcome after laparoscopic, transverse, and midline right-sided colectomy. Int J Colorectal Dis. 2012;27:797–802. doi: 10.1007/s00384-011-1404-4. [DOI] [PubMed] [Google Scholar]
- 44.Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, Lai PB, Lau WY. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet. 2004;363:1187–1192. doi: 10.1016/S0140-6736(04)15947-3. [DOI] [PubMed] [Google Scholar]
- 45.Liang JT, Huang KC, Lai HS, Lee PH, Jeng YM. Oncologic results of laparoscopic versus conventional open surgery for stage II or III left-sided colon cancers: a randomized controlled trial. Ann Surg Oncol. 2007;14:109–117. doi: 10.1245/s10434-006-9135-4. [DOI] [PubMed] [Google Scholar]
- 46.Hinojosa MW, Murrell ZA, Konyalian VR, Mills S, Nguyen NT, Stamos MJ. Comparison of laparoscopic vs open sigmoid colectomy for benign and malignant disease at academic medical centers. J Gastrointest Surg. 2007;11:1423–1429; discussion 1429-1430. doi: 10.1007/s11605-007-0269-x. [DOI] [PubMed] [Google Scholar]
- 47.Cheung HY, Chung CC, Tsang WW, Wong JC, Yau KK, Li MK. Endolaparoscopic approach vs conventional open surgery in the treatment of obstructing left-sided colon cancer: a randomized controlled trial. Arch Surg. 2009;144:1127–1132. doi: 10.1001/archsurg.2009.216. [DOI] [PubMed] [Google Scholar]
- 48.Nakashima M, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Noaki R, Yamakawa K, Nagasue Y, et al. Colon cancer in the splenic flexure: comparison of short-term outcomes of laparoscopic and open colectomy. Surg Laparosc Endosc Percutan Tech. 2011;21:415–418. doi: 10.1097/SLE.0b013e31823aca96. [DOI] [PubMed] [Google Scholar]
- 49.Kim HJ, Lee IK, Lee YS, Kang WK, Park JK, Oh ST, Kim JG, Kim YH. A comparative study on the short-term clinicopathologic outcomes of laparoscopic surgery versus conventional open surgery for transverse colon cancer. Surg Endosc. 2009;23:1812–1817. doi: 10.1007/s00464-009-0348-z. [DOI] [PubMed] [Google Scholar]
- 50.Akiyoshi T, Kuroyanagi H, Fujimoto Y, Konishi T, Ueno M, Oya M, Yamaguchi T. Short-term outcomes of laparoscopic colectomy for transverse colon cancer. J Gastrointest Surg. 2010;14:818–823. doi: 10.1007/s11605-010-1182-2. [DOI] [PubMed] [Google Scholar]
- 51.Fernández-Cebrián JM, Gil Yonte P, Jimenez-Toscano M, Vega L, Ochando F. Laparoscopic colectomy for transverse colon carcinoma: a surgical challenge but oncologically feasible. Colorectal Dis. 2013;15:e79–e83. doi: 10.1111/codi.12067. [DOI] [PubMed] [Google Scholar]
- 52.Franks PJ, Bosanquet N, Thorpe H, Brown JM, Copeland J, Smith AM, Quirke P, Guillou PJ. Short-term costs of conventional vs laparoscopic assisted surgery in patients with colorectal cancer (MRC CLASICC trial) Br J Cancer. 2006;95:6–12. doi: 10.1038/sj.bjc.6603203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Steele SR, Brown TA, Rush RM, Martin MJ. Laparoscopic vs open colectomy for colon cancer: results from a large nationwide population-based analysis. J Gastrointest Surg. 2008;12:583–591. doi: 10.1007/s11605-007-0286-9. [DOI] [PubMed] [Google Scholar]
- 54.Vaid S, Tucker J, Bell T, Grim R, Ahuja V. Cost analysis of laparoscopic versus open colectomy in patients with colon cancer: results from a large nationwide population database. Am Surg. 2012;78:635–641. [PubMed] [Google Scholar]
- 55.Abraham NS, Young JM, Solomon MJ. Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg. 2004;91:1111–1124. doi: 10.1002/bjs.4640. [DOI] [PubMed] [Google Scholar]
- 56.Tilney HS, Lovegrove RE, Purkayastha S, Heriot AG, Darzi AW, Tekkis PP. Laparoscopic vs open subtotal colectomy for benign and malignant disease. Colorectal Dis. 2006;8:441–450. doi: 10.1111/j.1463-1318.2006.00959.x. [DOI] [PubMed] [Google Scholar]
- 57.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bonjer HJ, Hop WC, Nelson H, Sargent DJ, Lacy AM, Castells A, Guillou PJ, Thorpe H, Brown J, Delgado S, et al. Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg. 2007;142:298–303. doi: 10.1001/archsurg.142.3.298. [DOI] [PubMed] [Google Scholar]
- 59.Korolija D, Tadić S, Simić D. Extent of oncological resection in laparoscopic vs. open colorectal surgery: meta-analysis. Langenbecks Arch Surg. 2003;387:366–371. doi: 10.1007/s00423-002-0335-5. [DOI] [PubMed] [Google Scholar]
- 60.Rondelli F, Trastulli S, Avenia N, Schillaci G, Cirocchi R, Gullà N, Mariani E, Bistoni G, Noya G. Is laparoscopic right colectomy more effective than open resection? A meta-analysis of randomized and nonrandomized studies. Colorectal Dis. 2012;14:e447–e469. doi: 10.1111/j.1463-1318.2012.03054.x. [DOI] [PubMed] [Google Scholar]


