Abstract
The current study prospectively examines the predictive relationship of trait dissociation, assessed during academy training, to PTSD symptoms assessed at 12 months of active police duty in relatively young and healthy police academy recruits (N = 180). The roles of pre-academy trauma exposure, exposure to life-threatening critical incidents during police duty, and peritraumatic dissociation at the time of the officer’s worst critical incident were also examined. Utilizing path analytic techniques, greater trait dissociation, assessed during academy training, was predictive of both peritraumatic dissociation, and PTSD symptoms assessed at 12 months of police service. Moreover, after accounting for trait dissociation and peritraumatic dissociation, the relationship of previous trauma to later PTSD symptoms was no longer significant, demonstrating that the effect of previous trauma on later vulnerability to PTSD symptoms in this sample may be mediated by both trait and peritraumatic dissociation.
Keywords: Dissociation, traumatic stress, police officers
Delineating predictors of posttraumatic stress disorder (PTSD) is of particular importance for groups at high risk of trauma exposure, such as police officers. Police officers are often repeatedly exposed to critical incident stressors (Brown et al., 1999; Carlier et al., 1997; McCaslin et al., 2006; Robinson et al., 1997), placing them at risk for developing trauma-related distress, including PTSD. The incidence of current duty-related PTSD in police officers has been found to vary between 7% and 19% in previous studies (Carlier et al., 1997; Gersons, 1989; Robinson et al., 1997). In a recent study of 157 officers from an elite unit of Brazilian police, 8.9% met criteria for PTSD and an additional 16% for subsyndromal PTSD (Maia et al., 2007). Because the nature of their job requires high performance in the face of repeated potentially traumatizing events, police officers are an important group in which to understand risk and resilience to PTSD.
Adult survivors of childhood abuse or maltreatment have been found to be at increased risk for PTSD after subsequent trauma exposure during adulthood (e.g., Bremner et al., 1993; Nishith et al., 2000; Yehuda et al., 2001; Zlotnick et al., 1996). History of childhood trauma has also been associated with greater dissociative symptoms in adulthood, including feelings of detachment, blunted emotional responsiveness, reduced awareness of surroundings, derealization, and depersonalization (e.g., Bosch et al., 2003; Briere, 2006; Briere et al., 1988; Chu et al., 1990; Dancu et al., 1996; Nash et al., 1993) Moreover, previous trauma history also predicted higher dissociative symptoms in soldiers early in military training and again later in response to intense training stressors (Morgan et al., 2007). Based on these findings, it has been suggested that dissociative symptoms develop as a trauma-related psychological reaction or alternatively, as a maladaptive way of coping with trauma-related distress.
Although it has been suggested that the presence of dissociative symptoms places one at higher risk for the development of psychopathology after a subsequent trauma (e.g., Foa et al., 1996; Koopman et al., 1994; Marmar et al., 1994; Spiegel, 1991; Terr, 1991; Weiss et al., 1995), the nature of the relationship of dissociation to PTSD has been debated. Some earlier studies posit that greater trait dissociation is a preexisting risk factor for PTSD (e.g., Murray et al., 2002), whereas others suggest that dissociation may be a state-related condition associated with the development of PTSD symptomatology. Halligan and Yehuda examined self-reported dissociation as a risk factor for PTSD in adult children of Holocaust survivors (Halligan et al., 2002). Greater dissociative symptoms were found in adult children with current PTSD, but not among those without PTSD or those with only the risk factor of parental PTSD. It was concluded that the dissociative symptoms did not constitute a risk factor for the development of PTSD but were most related to having PTSD itself. These findings are consistent with those from a longitudinal study of police officers which assessed trait dissociation, PTSD symptoms, and general psychological health in both the early stages of police training and at 1-year follow-up (Hodgins et al., 2001). In this sample, once baseline PTSD symptoms, assessed by self-report during academy training, were accounted for, baseline levels of trait dissociation did not predict subsequent PTSD symptomatology.
Further support for the proposal that PTSD may determine dissociative symptoms was provided by Carlier et al. (1996) who reported that full or partial PTSD symptoms measured at 3 months after a traumatic experience in police officers predicted greater dissociative tendencies at 12 months, whereas this relationship was not significant for those without PTSD symptoms (Carlier et al., 1996). Finally, Ginzburg et al. (2006) reported that levels of PTSD and dissociation changed together over time in a sample of individuals who had experienced a myocardial infarction (Ginzburg et al., 2006). Those who were identified as having PTSD showed an increase in the level of dissociation. Those without PTSD showed no such increase, suggesting that the development of dissociative symptoms was driven by the development of PTSD. It should be noted that not everyone who develops PTSD will necessarily also have co-occurring dissociative symptoms and it has been suggested that it is a subtype of individuals with PTSD that will also have elevated current dissociation (Waelde et al., 2005).
Although studies are mixed regarding the cause and effect relationships between PTSD and dissociative symptoms, there is evidence to suggest that a general tendency to dissociate in adulthood, which may be influenced by early trauma experiences, can influence responses to other traumatic stressors later in life. In other words, it is possible that those with higher trait dissociation may also be more likely to dissociate at the time of later trauma (i.e., peritraumatic dissociation). Peritraumatic dissociation, the presence of dissociative experiences during or immediately after trauma exposure, has been shown to be strongly predictive of PTSD symptoms in Vietnam combat veterans (Bremner et al., 1992; Marmar et al., 1994), emergency responders (Marmar et al., 2006), road traffic accident survivors (Fullerton et al., 2000; Murray et al., 2002), survivors of a large-scale firestorm (Koopman et al., 1994), and among female childhood sexual abuse survivors (Johnson et al., 2001). In a recent meta-analysis, peritraumatic dissociation was found to be the strongest predictor of PTSD among the variables examined (Ozer et al., 2003). In sum, trait dissociation may influence the level of peritraumatic dissociative reactions, which then can place an individual at higher risk for the development of PTSD.
It is difficult to tease apart the complex relationship of dissociative symptoms to PTSD but regardless of whether dissociative symptoms are a preexisting risk factor for PTSD, develop as a component of PTSD, or emerge as a way of coping with PTSD, they are important to understand because their presence may impede recovery from PTSD. Simeon et al. (2005) found that persistent dissociation immediately after the World Trade Center disaster, measured retrospectively at 1-year follow-up, was predictive of less improvement in posttraumatic stress over the first year (Simeon et al., 2005). Furthermore, greater peritraumatic dissociation was significantly related to higher re-experiencing and avoidance symptoms after treatment in 28 female assault survivors (Zoellner et al., 2002).
There are few studies that prospectively examine the relationship between dissociation and PTSD. Prospective studies can help to determine whether dissociative tendencies are the result of trauma exposure or whether dissociative tendencies represent a “trait” that may be a preexisting risk factor for both peritraumatic dissociation and for PTSD, or alternatively whether greater dissociative tendencies result from trauma exposure, PTSD or both (Butler et al., 1996). The current study prospectively examines the relationship of pre-academy trauma exposure, trait dissociation assessed during academy training, and peritraumatic dissociation assessed at 12 months of active police duty, with PTSD symptoms at 12 months of police service in relatively young and healthy police academy recruits assessed during training and reassessed during the first year of police. The following hypothesis was tested using path analytic techniques: greater trait dissociation during academy training would predict greater PTSD symptoms at 12 months of police service, after accounting for exposure to traumatic events before entering the academy and peritraumatic dissociation at the time of the officer’s worst critical incident during the first year of service. We also tested the following secondary hypotheses: (1) greater pre-academy trauma exposure would predict greater levels of trait dissociation during academy training; (2) greater trait dissociation during academy training would predict greater peritraumatic dissociation at the time of the officer’s worst critical incident during the first 12 months of police service; and (3) greater peritraumatic dissociation during the officers worst critical incident in the first year of police service would predict greater PTSD symptoms at 12 months of service.
METHODS
Participants
This study examines the role of trait dissociation in the subsequent development of PTSD in 180 participants evaluated as part of a larger prospective and longitudinal study of police officer stress and health, approved by the University of California Human Subjects Committee and Institutional Review Board. Participants were recruited from 4 urban police departments, the New York Police Department and 3 departments in the San Francisco Bay Area (Oakland, Oakland Police Department; San Francisco, San Francisco Police Department; and San Jose, San Jose Police Department) during police academy training. Academy trainees were introduced to the study by study personnel during academy training classes. The study presentation included the distribution of a letter from the commissioner or police chief of the affiliated department, a letter from the study team, a description of the study procedures, a contact number, and a participation form. In addition to in-person presentations, informational flyers were posted at each academy which provided contact information for the study team. Academy trainees with previous experience in combat, law enforcement, or emergency services were excluded from the baseline component of the study.
Procedures
Baseline assessments were conducted during police academy training. Before assessment, participating officers gave consent to participate after receiving a thorough explanation of the study procedures. Participants were also given a description of the Federal Certificate of Confidentiality obtained for the study, assuring that any information obtained under the auspices of this study is protected and could not be disclosed to department personnel, nor subpoenaed in either criminal or civil court.
This report presents findings on selected predictors, focused on trait and peritraumatic dissociation, in the first 180 academy recruits enrolled in an ongoing prospective longitudinal cohort study. The participants completed baseline assessments during academy training and follow-up assessments after the first year of police service. Data collection in the full cohort is ongoing with a goal of enrolling 400 recruits assessed on a comprehensive set of biological and behavioral predictors during training and followed during the first 7 years of police service.
Measures
Demographics
The age, gender, ethnicity, marital status, and education of each participant were collected.
Life Stressor Checklist-Revised
The Life Stressor Checklist-Revised, a 30-item screening measure of stressful events across the lifespan, was given as a self-report measure for lifetime exposure to stressful life events such as physical assault, sexual assault, being robbed or mugged, and the catastrophic death of a loved one (Wolfe et al., 1996). Previous trauma history was defined as the number of events endorsed from a list of 9 life threatening events taken from the Life Stressor Checklist-Revised, where the participant also believed they could have been killed or seriously harmed, including sexual and/or physical assault, serious disaster, serious physical and mental illness, physical neglect, and for women, abortion or miscarriage.
Dissociative Experiences Scale
The Dissociative Experiences Scale (DES), a 28-item self-report questionnaire, is a measure of trait dissociation used with both normal and clinical populations. The DES total score is the mean of all items and ranges from 0 to 100 and for each item, participants rate the percentage of time (i.e., 0%–100%) they experience each symptom. Good internal consistency and construct validity have been reported for the DES (Bernstein et al., 1986). The DES has also been found to have good test-retest reliability and internal consistency in a clinical sample (Dubester et al., 1995).
Critical Incident History Questionnaire
The Critical Incident History Questionnaire (CIHQ) is a 34-item self-report measure designed to produce a measure of cumulative exposure to critical incidents (Brunet et al., 1998; Weiss et al., 1999). Participants tabulate the number of times (frequency of exposure) that they have personally experienced each of the 34 critical incidents in the line of duty. In this study, those events that had potential to be life threatening or to cause serious injury were summed.
Peritraumatic Dissociation Questionnaire
The Peritraumatic Dissociation Questionnaire (PDEQ) is a 10-item measure of dissociative symptoms (e.g., altered time perception or depersonalization) experienced during or immediately after a traumatic event. Several studies have found the PDEQ to have high internal consistency and support its reliability and convergent and divergent validity (Marmar et al., 2004; Marmar et al., 1997). The participants rated each item with respect to their most disturbing traumatic event on a 5-point scale from (1 = not at all true to 5 = extremely true) and the mean score of all the items was used as the total score. This questionnaire was completed to the officer’s self-identified most distressing critical incident in the first 12 months of active police duty.
Mississippi Combat Scale-Civilian Version
The Mississippi Combat Scale-Civilian Version (MCS-CV) is a 35-item measure that assesses PTSD-related symptoms of intrusion, avoidance, hyperarousal, and other difficulties since the time of critical incident or trauma exposure (Keane et al., 1988; Norris et al., 1996). The civilian version has been used to assess PTSD symptoms in nonveteran controls in the National Vietnam Veterans Readjustment Study (NVVRS; Kulka et al., 1990), and in emergency services personnel after a disaster (Marmar et al., 1996; Weiss et al., 1995). For this study, the participants were asked how much they have experienced each item, “since beginning police service.” It has been reported in several papers that, when factor analyzed, the reverse scored items of the MCS-CV comprise 1 factor, raising the question of whether these items are inherently different from the unreflected items and whether this may influence results (Inkelas et al., 2000). Analyses for this article were rerun using only the unreflected items of the MCS-CV and this did not significantly change the results. Therefore, we report the analyses utilizing the full MCS-CV scale.
Data Analysis
Path analysis was performed using SPSS AMOS 7.0 software (Arbuckle, 2006). These analyses used the maximum likelihood method of parameter estimation. Direct and indirect effects were estimated using a series of hierarchically nested multiple regression analyses predicting PTSD symptoms at 12 months of police service. Variables were entered into the model in the following order: (1) previous trauma as measured by the LSC, (2) trait dissociation as assessed by the DES, (3) critical incident exposure as assessed by the CIHQ, and (4) peritraumatic dissociation during the officers’ self-identified worst critical incident as assessed by the PDEQ.
RESULTS
Participant Characteristics
At baseline, the police officers in this sample were an average of 27.24 (SD = 4.70) years old, and 87.2% (n = 157) were men. The ethnic distribution was as follows: 46.6% Caucasian, 19.9% Latino, 15.3% Asian American/Pacific Islander, 8.0% African American, and 10.2% other or multiple ethnicities. More than half were unmarried (77.3%) and most completed at least some college (89.3% completed a 2– 4-year college degree, 5.1% had completed a graduate degree).
No current axis I psychopathology at baseline was reported for any recruits using the Structured Clinical Interview for DSM-IV, version 2.0 (SCID I-NP) (First et al., 1996). Lifetime SCID I-NP diagnoses for the total sample (N = 180) were as follows: depression (MDD or depression NOS): 19/180 (10.6%); PTSD: 1/180 (0.6%); alcohol abuse: 21/180 (11.7%); alcohol dependency: 7/180 (3.9%); alcohol abuse or dependency: 25/180 (13.9%); and any psychiatric disorder: 40/180 (22.2%). There were 5 cases of any alcohol disorder comorbid with depression. There were no diagnoses of bipolar disorder or other anxiety disorders.
Preliminary Analyses
Variables were examined for normality. Scores on the following variables were skewed and kurtotic: DES (s = 3.6, k = 17.2), PDEQ (s = 1.8, k = 2.8), and CIHQ (s = 3.7, k = 17.7); therefore, statistical analyses were carried out on the log-transformed values of these variables (DESlog, PDEQlog, and CIHQlog). Age and gender were not significantly related to PTSD symptoms and were therefore not included in later analyses. The number of life-threatening traumatic events experienced by the officers before entering the academy ranged from 0 to 3, with 41.2% experiencing no previous trauma, 30.6% experiencing 1 event, 19.4% experiencing 2 events, and 8.8% experiencing 3 events.
Path Analysis
A model assessing direct and indirect pathways was estimated. Means and standard deviations of the variables used in the path analysis are shown in Table 1. A matrix of correlations for the predictor variables is presented in Table 2. Figure 1 illustrates the associations among variables with partial correlation coefficients (β weights) given for each path. The results of the path analysis indicate 3 significant direct pathways to PTSD. These pathways are from (1) trait dissociation (β = 0.18), (2) peritraumatic dissociation (β = .21), and critical incident exposure (β = 0.21). Three indirect paths were also present: (1) an indirect effect of trait dissociation on the relationship between previous life-threatening trauma exposure and PTSD symptoms, with trait dissociation accounting for the majority of the effect, (2) an indirect effect of peritraumatic dissociation on the relationship between critical incident exposure and PTSD symptoms, and (3) an indirect effect of peritraumatic dissociation on the relationship between trait dissociation and PTSD symptoms. Together, the pathways account for 19% of the variance in PTSD symptoms. Table 3 provides information on all of the direct and indirect effects for the model. The overall model yielded strong fit indices (χ2 = 1.279, p = 0.528; comparative fit index = 1.00; and the root mean square error of approximation = 0.000, LO 90 = 0.000 to HI 90 = 0.134).
TABLE 1.
Means and Standard Deviations for Variables used in the Path Analysis (N = 170–180)
| Variable | N | M(SD) |
|---|---|---|
| PTSD Symptoms | 180 | 60.34 (10.76) |
| Prior Trauma | 170 | .96 (.98), Range = 0–3 |
| Trait Dissociation | 176 | 6.34 (7.63) |
| Peritraumatic Dissociation | 174 | 1.40 (.56) |
| Critical Incident Exposure | 180 | 5.62 (9.71), Range = 0–66 |
TABLE 2.
Correlation Matrix of Predictors of MCS-CV PTSD Symptoms (N = 170–180)
| PTSD Symptoms | Prior Trauma | Trait Dissociation (log) | Peritraumatic Dissociation (log) | Critical Incident Exposure (log) | |
|---|---|---|---|---|---|
| PTSD Symptoms | — | .200** | .252*** | .313*** | .275*** |
| Prior Trauma | — | .226** | .090 | .077 | |
| Trait Dissociation (log) | — | .188* | .046 | ||
| Peritraumatic Dissociation (log) | — | .266*** | |||
| Critical Incident Exposure (log) | — |
p < 0.01;
p < 0.001;
p < 0.05.
Because of missing data, N varies from 170–180.
FIGURE 1.
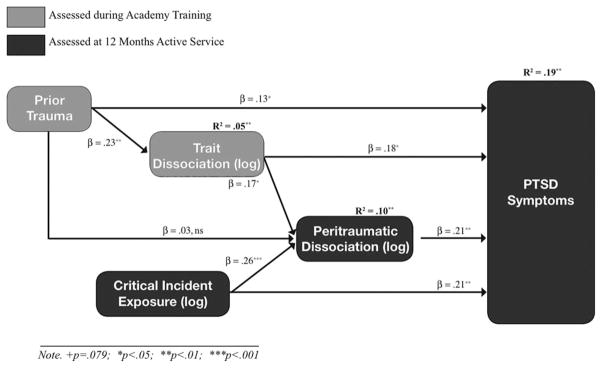
Path model predicting PTSD symptoms (n = 170).
TABLE 3.
Direct and Indirect Effects for the Path Model of PTSD Symptoms
| Causal Variable | Endogenous Variables
|
|||||
|---|---|---|---|---|---|---|
| Trait Dissociation
|
Peritraumatic Diss.
|
PTSD Symptoms
|
||||
| St. | SE | St. | SE | St. | SE | |
| Prior Trauma | ||||||
| Direct effect | 0.23*** | 0.07 | 0.03 | 0.08 | 0.13† | 0.07 |
| Total indirect effects | — | — | 0.04* | 0.02 | 0.06* | 0.03 |
| Total effect | 0.23*** | 0.07 | 0.07 | 0.07 | 0.18* | 0.07 |
| Trait Dissociation | ||||||
| Direct effect | — | — | 0.17* | 0.08 | 0.18** | 0.07 |
| Total indirect effects | — | — | — | — | 0.04* | 0.02 |
| Total effect | — | — | 0.17* | 0.08 | 0.22** | 0.07 |
| Critical Incident Exposure | ||||||
| Direct effect | — | — | 0.26*** | 0.07 | 0.21*** | 0.07 |
| Total indirect effects | — | — | — | — | 0.05*** | 0.03 |
| Total effect | — | — | 0.26*** | 0.07 | 0.27*** | 0.07 |
| Peritraumatic Dissociation | ||||||
| Direct effect | — | — | — | — | 0.21** | 0.07 |
| Total indirect effects | — | — | — | — | — | — |
| Total effect | — | — | — | — | 0.21** | 0.07 |
p < 0.05;
p < 0.01;
p <.001.
p = 0.081.
St. = Standardized β; SE = standard error for standardized effects.
DISCUSSION
Greater trait dissociation, assessed during academy training, was predictive of both peritraumatic dissociation and PTSD symptoms assessed at 12 months of police service. Trait dissociation continued to be a strong predictor of PTSD symptoms even in the presence of previous trauma exposure and peritraumatic dissociation. This finding is also consistent with a previous cross-sectional study of emergency service workers from our group which found that both trait dissociation and peritraumatic dissociation accounted for unique variance in PTSD symptoms after controlling for other variables such as years of experience, trauma exposure, adjustment, locus of control, and social support (Weiss et al., 1995). Further, there was evidence that a portion of the effect of trait dissociation on PTSD was mediated by peritraumatic dissociation to the officer’s worst incident assessed at 12 months. In other words, those who endorsed a greater baseline tendency to dissociate during academy training were more likely to experience greater peritraumatic dissociation at the time of their worst critical incident, and, in turn, greater peritraumatic dissociation predicted higher risk of PTSD symptoms at 12 months of police service.
In this sample of police academy recruits, consistent with previous studies, previous trauma exposure seems to place one at risk for developing greater trait dissociative symptoms, even among those who do not have a diagnosis of PTSD. After accounting for trait dissociation and peritraumatic dissociation, the relationship of previous trauma to later PTSD symptoms was no longer significant, demonstrating that the effect of previous trauma on later vulnerability to PTSD symptoms may be mediated by both trait and peritraumatic dissociation. Critical incident exposure during the first year of police service was also found to predict PTSD symptoms and this effect was partially, but not completely, mediated by peritraumatic dissociation.
Although our results indicate that previous traumatic experiences are predictive of greater trait dissociative symptoms, it should be noted that because we did not include a self-report continuous PTSD symptom measure at baseline, we could not determine whether any of the officers were experiencing subthreshold levels of PTSD symptoms. Moreover, although those with higher trait dissociation may be more prone to experience greater peritraumatic dissociation at the time of later trauma exposure than those low on trait dissociation, peritraumatic dissociation did not fully mediate the relationship between trait dissociation and PTSD. This suggests that individuals with higher preexisting dissociative symptoms may be at higher risk for PTSD after subsequent trauma exposure for a number of other reasons. It is possible that they are less likely to employ adaptive coping strategies in the aftermath of a traumatic event or that they may be more vulnerable to the effects of other psychological or biological variables that may co-occur with greater dissociative symptomatology.
Individual differences in neuroendocrine responses to stress have also been found to be related to symptoms of dissociation reported under stress. Among soldiers in training, exposure to the stress of mock captivity and confinement resulted in significant increases in symptoms of dissociation in all subjects (Morgan et al., 2007). Moreover, in an earlier report on the same sample of subjects, elite soldiers were found to have significantly lower stress-induced symptoms of dissociation when compared with general troop soldiers (Morgan et al., 2001a). These same elite soldiers also exhibited higher stress induced levels of the neurotransmitter neuropeptide Y (NPY) (Morgan et al., 2002; Morgan et al., 2001b). This study replicated findings from animal studies, which have shown that NPY reduces anxiety and animal freezing behavior and implicate NPY as a potential factor in determining vulnerability to stress-induced symptoms of dissociation.
Level of trait dissociation may have important implications for performance. In a study of Army Special Forces soldiers, stress-induced symptoms of dissociation during training were negatively related to military performance scores (Morgan et al., 2007), specifically ability to concentrate on performance and “presence of mind.” It was suggested that the relationship of greater dissociation and poorer performance may be mediated through dissociation’s effect on brain areas involved in functions such as attention, concentration, working memory, and spatial mapping.
Our study had a number of strengths such as measuring these constructs in a young healthy population and collection of prospective data. This study also had several limitations: (1) although academy recruits were screened for axis I disorders including PTSD, we did not administer a self-report measure of continuous PTSD symptoms during academy training at baseline; (2) trait dissociation was not reassessed at 1 year to measure whether there were changes following further critical incident exposure and the development of PTSD symptoms.
CONCLUSIONS
In sum, greater trait dissociation symptoms, assessed during academy training, was predictive of both peritraumatic dissociation and PTSD symptoms assessed at 12 months of police service. Moreover, after accounting for trait dissociation and peritraumatic dissociation, the relationship of previous trauma to later PTSD symptoms was no longer significant, demonstrating that the effect of previous trauma on later vulnerability to PTSD symptoms may be mediated by both trait and peritraumatic dissociation.
Given the current findings, longer-term observation of participating officers in the cohort should give more precise insight on the impact of trait dissociation on peritraumatic distress and the development of PTSD over time. Systematic examination of neuroimaging and neuroendocrine characteristics would shed further light on the relationship between baseline physiological and psychological characteristics related to trait dissociation and the development of PTSD.
Acknowledgments
This research was supported by National Institute of Mental Health grant (R01-MH056350-07) (to C.R.M.).
References
- Arbuckle JL. Amos (Version 7.0) Chicago (IL): SPSS; 2006. [Google Scholar]
- Bernstein E, Putnam F. Development, reliability and validity of a dissociation scale. J Nerv Ment Dis. 1986;174:727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- Bosch LVD, Verheul R, Langeland W, Brink WVD. Trauma, dissociation and posttraumatic stress disorder in female borderline patients with and without substance abuse problems. Aust NZ J Psychiatry. 2003;37:549–555. doi: 10.1046/j.1440-1614.2003.01199.x. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Southwick S, Brett E, Fontana A, Rosenheck R, Charney DS. Dissociation and posttraumatic stress disorder in Vietnam combat veterans. Am J Psychiatry. 1992;149:328–332. doi: 10.1176/ajp.149.3.328. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Southwick SM, Johnson DR, Yehuda R, Charney DS. Childhood physical abuse and combat-related posttraumatic stress disorder in Vietnam veterans. Am J Psychiatry. 1993;150:235–239. doi: 10.1176/ajp.150.2.235. [DOI] [PubMed] [Google Scholar]
- Briere J. Dissociative symptoms and trauma exposure: Specificity, affect dysregulation and posttraumatic stress. J Nerv Ment Dis. 2006;194:78–82. doi: 10.1097/01.nmd.0000198139.47371.54. [DOI] [PubMed] [Google Scholar]
- Briere J, Runtz M. Symptomatology associated with childhood sexual victimization in a nonclinical adult sample. Child Abuse Negl. 1988;12:51–59. doi: 10.1016/0145-2134(88)90007-5. [DOI] [PubMed] [Google Scholar]
- Brown H, Prescott R. Applied Mixed Models in Medicine. Statistics in Practice. Chichester; New York: J. Wiley, Sons; 1999. p. xx.p. 408. [Google Scholar]
- Brunet A, Weiss D, Best SR, Liberman A, Fagan J, Marmar CR. International Society for Traumatic Stress Studies. Washington, DC: 1998. Assessing recurring traumatic exposure: The critical incident history questionnaire. [Google Scholar]
- Butler L, Duran R, Jasiukaitis P. Hypnotizability and traumatic experience: A diathesis-stress model of dissociative symptomatology. Am J Psychiatry. 1996;153:42–63. doi: 10.1176/ajp.153.8.A42. [DOI] [PubMed] [Google Scholar]
- Carlier IVE, Lamberts RD, Fouwels AJ, Gersons BPR. PTSD in relation to dissociation in traumatized police officers. Am J Psychiatry. 1996;153:1325–1328. doi: 10.1176/ajp.153.10.1325. [DOI] [PubMed] [Google Scholar]
- Carlier IVE, Lamberts RD, Gersons BPR. Risk factors for posttraumatic stress symptomatology in police officers: A prospective analysis. J Nerv Ment Dis. 1997;185:498–506. doi: 10.1097/00005053-199708000-00004. [DOI] [PubMed] [Google Scholar]
- Chu JA, Dill DL. Dissociative symptoms in relation to childhood physical and sexual abuse. Am J Psychiatry. 1990;147:887–892. doi: 10.1176/ajp.147.7.887. [DOI] [PubMed] [Google Scholar]
- Dancu CV, Riggs DS, Hearst-Ikeda D, Shoyer BG, Foa EB. Dissociative experiences and posttraumatic stress disorder among female victims of criminal assault and rape. J Trauma Stress. 1996;9:253–267. doi: 10.1007/BF02110659. [DOI] [PubMed] [Google Scholar]
- Dubester K, Braun B. Psychometric properties of the dissociative experiences scale. J Nerv Ment Dis. 1995;183:231–235. doi: 10.1097/00005053-199504000-00008. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis 1 Disorders-Non-Patient Edition (SCID-I/NP, Version 2.0) New York (NY): Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Foa EB, Hearst-Ikeda D. Emotional dissociation in response to trauma: An information-processing approach. In: Michelson LK, Ray WJ, editors. Handbook of Dissociation: Theoretical, Empirical and Clinical Perspectives. New York (NY): Plenum Press; 1996. pp. 207–224. [Google Scholar]
- Fullerton C, Ursano R, Epstein R, Crowley B, Vance K, Kao T, Baum A. Peritraumatic dissociation following motor vehicle accidents: Relationship to prior trauma and prior major depression. J Nerv Ment Dis. 2000;188:267–272. doi: 10.1097/00005053-200005000-00003. [DOI] [PubMed] [Google Scholar]
- Gersons BP. Patterns of PTSD among police officers following shooting incidents: A two-dimensional model and treatment implications. J Trauma Stress. 1989;2:247–257. [Google Scholar]
- Ginzburg K, Solomon Z, Dekel R, Bleich A. Longitudinal study of acute stress disorder, posttraumatic stress disorder and dissociation following myocardial infarction. J Nerv Ment Dis. 2006;194:945–950. doi: 10.1097/01.nmd.0000249061.65454.54. [DOI] [PubMed] [Google Scholar]
- Halligan SL, Yehuda R. Assessing dissociation as a risk factor for posttraumatic stress disorder: A study of adult offspring of holocaust survivors. J Nerv Ment Dis. 2002;190:429–36. doi: 10.1097/00005053-200207000-00002. [DOI] [PubMed] [Google Scholar]
- Hodgins G, Creamer M, Bell R. Risk factors for post-trauma reactions in police officers: A longitudinal study. J Nerv Ment Dis. 2001;189:541–547. doi: 10.1097/00005053-200108000-00007. [DOI] [PubMed] [Google Scholar]
- Inkelas M, Loux LA, Bourque LB, Widawski M, Nguyen LH. Dimensionality and reliability of the Civilian Mississippi Scale for PTSD in a postearthquake community. J Trauma Stress. 2000;13:149–167. doi: 10.1023/A:1007733217042. [DOI] [PubMed] [Google Scholar]
- Johnson D, Pike J, Chard K. Factors predicting PTSD, depression and dissociative severity in female treatment-seeking childhood sexual abuse survivors. Child Abuse Negl. 2001;25:179–198. doi: 10.1016/s0145-2134(00)00225-8. [DOI] [PubMed] [Google Scholar]
- Keane TM, Caddell JM, Taylor KL. Mississippi scale for combat-related posttraumatic stress disorder: Three studies in reliability and validity. J Consult Clin Psychol. 1988;56:85–90. doi: 10.1037//0022-006x.56.1.85. [DOI] [PubMed] [Google Scholar]
- Koopman C, Classen C, Spiegel D. Predictors of posttraumatic stress symptoms among survivors of the Oakland/Berkeley, California, firestorm. Am J Psychiatry. 1994;151:888–894. doi: 10.1176/ajp.151.6.888. [DOI] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. Trauma and the Vietnam War Generation: Report of the Findings From the National Vietnam Veterans Readjustment Study. New York, NY: Brunner/Mazel; 1990. [Google Scholar]
- Maia D, Marmar C, Metzler T, Nobrega A, Berger W, Mendlowicz M, Coutinho E, Figueira I. Post-traumatic stress symptoms in an elite unit of Brazilian police officers: Prevalence and impact on psychosocial functioning and on physical and mental health. J Affect Disord. 2007;97:241–245. doi: 10.1016/j.jad.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Marmar C, McCaslin S, Metzler T, Best S, Weiss D, Fagan J, Liberman A, Pole N, Otte C, Yehuda R, Mohr D, Neylan T. Predictors of posttraumatic stress in police and other first responders. Ann N Y Acad Sci. 2006;1071:1–18. doi: 10.1196/annals.1364.001. [DOI] [PubMed] [Google Scholar]
- Marmar C, Metzler T, Otte C. The Peritraumatic Dissociative Experiences Questionnaire. Assessing Psychological Trauma and PTSD. 2. New York, NY: Guilford Press; 2004. pp. 144–167. [Google Scholar]
- Marmar CR, Weiss DS, Metzler TJ. The peritraumatic dissociative experiences questionnaire. In: Wilson JP, Keane TM, editors. Assessing Psychological Trauma and PTSD: A Handbook for Practitioners. New York (NY): Guilford Press; 1997. pp. 412–428. [Google Scholar]
- Marmar CR, Weiss DS, Metzler TJ, Ronfeldt HM, Foreman C. Stress responses of emergency services personnel to the Loma Prieta earthquake Interstate 880 freeway collapse and control traumatic incidents. J Trauma Stress. 1996;9:63–85. doi: 10.1007/BF02116834. [DOI] [PubMed] [Google Scholar]
- Marmar CR, Weiss DS, Schlenger WE, Fairbank JA, Jordan BK, Kulka RA, Hough RL. Peritraumatic dissociation and posttraumatic stress in male vietnam theater veterans. Am J Psychiatry. 1994;151:902–907. doi: 10.1176/ajp.151.6.902. [DOI] [PubMed] [Google Scholar]
- McCaslin S, Rogers C, Metzler T, Best S, Weiss D, Fagan J, Liberman A, Marmar C. The impact of personal threat on police officers’ responses to critical incident stressors. J Nerv Ment Dis. 2006;194:591–597. doi: 10.1097/01.nmd.0000230641.43013.68. [DOI] [PubMed] [Google Scholar]
- Morgan C, Hazlett G, Wang S, Richardson E, Schnurr P, Southwick S. Symptoms of dissociation in humans experiencing acute, uncontrollable stress: A prospective investigation. Am J Psychiatry. 2001a;158:1239–1247. doi: 10.1176/appi.ajp.158.8.1239. [DOI] [PubMed] [Google Scholar]
- Morgan C, Rasmusson A, Wang S, Hoyt G, Hauger R, Hazlett G. Neuropeptide-Y, cortisol and subjective distress in humans exposed to acute stress: Replication and extension of previous report. Biol Psychiatry. 2002;52:136–142. doi: 10.1016/s0006-3223(02)01319-7. [DOI] [PubMed] [Google Scholar]
- Morgan CA, Southwick SM, Hazlett G, Steffian G. Symptoms of dissociation in healthy military populations: Why and how do war fighters differ in responses to intense stress? In: Vermetten E, Dorahy M, Spiegel D, editors. Traumatic dissociation: Neurobiology and treatment. Washington (DC): American Psychiatric Publishing; 2007. pp. 157–179. [Google Scholar]
- Morgan C, Wang S, Rasmusson A, Hazlett G, Anderson G, Charney D. Relationship among plasma cortisol, catecholamines, neuropeptide Y and human performance during exposure to uncontrollable stress. Psychosom Med. 2001b;63:412–22. doi: 10.1097/00006842-200105000-00010. [DOI] [PubMed] [Google Scholar]
- Murray J, Ehlers A, Mayou R. Dissociation and post-traumatic stress disorder: Two prospective studies of road traffic accident survivors. Br Journal of Psychiatry. 2002;180:363–368. doi: 10.1192/bjp.180.4.363. [DOI] [PubMed] [Google Scholar]
- Nash MR, Hulsey TL, Sexton MC, Harralson TL, Lambert W, Lynch GV. Adult psychopathology associated with a history of childhood sexual abuse: A psychoanalytic perspective. In: Masling JM, Bornstein RF, editors. Psychoanalytic Perspectives on Psychopathology. Empirical Studies of Psychoanalytic Theories. Vol. 4. Washington (DC): American Psychological Association; 1993. pp. 111–137. [Google Scholar]
- Nishith P, Mechanic M, Resic P. Prior interpersonal trauma: The contribution to current PTSD symptoms in female rape victims. J Abnorm Psychol. 2000;109:20–25. [PMC free article] [PubMed] [Google Scholar]
- Norris FH, Perilla JL. The revised Civilian Mississippi Scale for PTSD: Reliability, validity and cross-language stability. J Trauma Stress. 1996;9:285–298. doi: 10.1007/BF02110661. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DL. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychol Bull. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Robinson HM, Sigman MR, Wilson JP. Duty-related stressors and PTSD symptoms in suburban police officers. Psychol Rep. 1997;81:835–845. doi: 10.2466/pr0.1997.81.3.835. [DOI] [PubMed] [Google Scholar]
- Simeon D, Greenberg J, Nelson D, Schmeidler J, Hollander E. Dissociation and posttraumatic stress 1 year after the world trade center disaster: Follow-up of a longitudinal survey. J Clin Psychiatry. 2005;66:231–237. doi: 10.4088/jcp.v66n0212. [DOI] [PubMed] [Google Scholar]
- Spiegel D. Dissociation and trauma. In: Tasman A, Goldfinger SM, editors. American Psychiatric Press Review of Psychiatry. Vol. 10. Washington (DC): American Psychiatric Press; 1991. pp. 261–275. [Google Scholar]
- Terr L. Childhood traumas: An outline and overview. Am J Psychiatry. 1991;148:10–20. doi: 10.1176/ajp.148.1.10. [DOI] [PubMed] [Google Scholar]
- Waelde L, Silvern L, Fairbank J. A Taxometric investigation of dissociation in Vietnam veterans. J Trauma Stress. 2005;18:359–369. doi: 10.1002/jts.20034. [DOI] [PubMed] [Google Scholar]
- Weiss DS, Brunet A, Metzler TJ, Best SR, Fagan JA, Marmar CR. International Society of Traumatic Stress Studies. Miami (FL): 1999. Critical incident exposure in police officers: Frequency, impact and correlates. [Google Scholar]
- Weiss DS, Marmar CR, Metzler TJ, Ronfeldt HM. Predicting symptomatic distress in emergency services personnel. J Consult Clin Psychol. 1995;63:361–368. doi: 10.1037//0022-006x.63.3.361. [DOI] [PubMed] [Google Scholar]
- Wolfe J, Kimerling R, Brown PJ, Chresman KR, Levin K. Psychometric Review of the Life Stressor Checklist-Revised. Measurement of Stress, Trauma and Adaptation. Lutherville (MD): Sidran Press; 1996. pp. 676–679. [Google Scholar]
- Yehuda R, Hallig SL, Grossman R. Childhood trauma and risk for PTSD: Relationship to intergenerational effects of trauma, parental PTSD and cortisol excretion. Dev Psychopathol. 2001;13:733–53. doi: 10.1017/s0954579401003170. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Zakriski AL, Shea MT, Costello E, Begin A, Pearlstein T, Simpson E. The long-term sequelae of sexual abuse: Support for a complex posttraumatic stress disorder. J Trauma Stress. 1996;9:195–205. doi: 10.1007/BF02110655. [DOI] [PubMed] [Google Scholar]
- Zoellner LA, Alvarez-Conrad J, Foa EB. Peritraumatic dissociative experiences, trauma narratives and trauma pathology. J Traumat Stress. 2002;15:49–57. doi: 10.1023/A:1014383228149. [DOI] [PubMed] [Google Scholar]


