Abstract
Purpose
We sought to estimate the pooled current prevalence of posttraumatic stress disorder (PTSD) among rescue workers and to determine the variables implicated in the heterogeneity observed among the prevalences of individual studies.
Methods
A systematic review covering studies reporting on the PTSD prevalence in rescue teams was conducted following four sequential steps: (1) research in specialized online databases, (2) review of abstracts and selection of studies, (3) review of reference list, and (4) contact with authors and experts. Prevalence data from all studies were pooled using random effects model. Multivariate meta-regression models were fitted to identify variables related to the prevalences heterogeneity.
Results
A total of 28 studies, reporting on 40 samples with 20,424 rescuers, were selected. The worldwide pooled current prevalence was 10%. Meta-regression modeling in studies carried out in the Asian continent had, on average, higher estimated prevalences than those from Europe, but not higher than the North American estimates. Studies of ambulance personnel also showed higher estimated PTSD prevalence than studies with firefighters and police officers.
Conclusions
Rescue workers in general have a pooled current prevalence of PTSD that is much higher than that of the general population. Ambulance personnel and rescuers from Asia may be more susceptible to PTSD. These results indicate the need for improving pre-employment strategies to select the most resilient individuals for rescue work, to implement continuous preventive measures for personnel, and to promote educational campaigns about PTSD and its therapeutic possibilities.
Keywords: Posttraumatic stress disorder, Prevalence, Rescue workers, Disaster, Meta-analysis
Introduction
Rescue worker can be defined as any person who professionally or voluntarily engages in activities devoted to providing out-of-hospital acute medical care; transportation to definitive care; freeing persons or animals from danger to life or well-being in accidents, fires, bombings, floods, earthquakes, other disasters and life-threatening conditions. As a consequence of these activities, rescue workers have a high exposure to traumatic events [1, 2]. Exposure to a traumatic event is criterion A1 of the Diagnostic and Statistical Manual of Mental Disorders, 4th edition revised (DSM-IV-TR) [3] and the sine qua non condition for the diagnosis of posttraumatic stress disorder (PTSD). A traumatic event is defined by the DSM-IV-TR as experiencing, witnessing, or being confronted with at least one event that involves actual or threatened death or serious injury, or a threat to the physical integrity of self or others. The occupational routine of rescue workers includes the provision of emergency medical assistance to severely injured people, searching for and recovering victims from wreckages and firefights, all of which qualify as traumatic according to DSM-IV-TR criterion A1. Because the risk of developing PTSD increases with the number of traumatic events experienced [4], rescuers are a high risk group for PTSD.
The prevalence of PTSD in rescue workers and its correlates have been intensively investigated since the disorder was first included in the DSM-III [5] in 1980. However, PTSD prevalence is known to vary widely across occupational groups, and rescue workers are not a homogeneous category, encompassing occupations as distinct as firefighters, ambulance personnel, police officers, and canine search and rescue teams. Not surprisingly, PTSD prevalence figures in these groups were found to vary widely from 0% [6] to 46% [7]. The prevalence of PTSD can differ nearly fourfold across occupational groups, even when different types of rescue workers are deployed to the same disaster [8].
Besides occupation, the nature, the severity, and the repetition of the exposure to traumatic events may influence the prevalence of PTSD. For example, among disaster workers involved in rescue efforts after an airplane crash, high prevalence of PTSD was associated with previous experience with disasters, high exposure to the traumatic event and assisting survivors [9]. Furthermore, a variety of factors have been associated with increased risk for PTSD in specific occupational groups of rescuer workers: unmarried status among ambulance personnel [10], lower social support and training levels among canine search and rescue handlers [11], and longer job experience and number of distressing missions among firefighters [12]. Moreover, national and cultural factors are supposed to affect the prevalence of PTSD in rescue workers [13]. Accordingly, it has been proposed that because developing countries show higher rates of interpersonal violence as compared to developed ones, PTSD prevalence would be higher in rescuers from the former than from the latter [14].
However, in spite of the many studies published on the prevalence of PTSD in rescue workers, there is a dearth of systematic reviews which could help identify, appraise, and synthesize the highly heterogeneous research evidence available in this field. Although all rescuers conceivably suffer from repeated occupational exposure to traumatic events and are, thus, considered a high-risk group for PTSD, the worldwide pooled prevalence of PTSD in rescuers in general or across different occupational groups is still unknown. Furthermore, no other study has yet identified the variables that account for the high variability in the published prevalences. Therefore, in order to fill the existing lacunae in psychiatric knowledge, we conducted a meta-analysis of epidemiologic studies on the prevalence of PTSD in rescue workers to calculate the pooled worldwide current prevalence of PTSD in this population as a whole and for each of the different occupational groups that are involved in this kind of work. Further, we also sought to determine the methodological, sociodemographic, and work- and trauma-related variables that account for the large variability in reported prevalence estimates.
Method
Search strategy and study selection
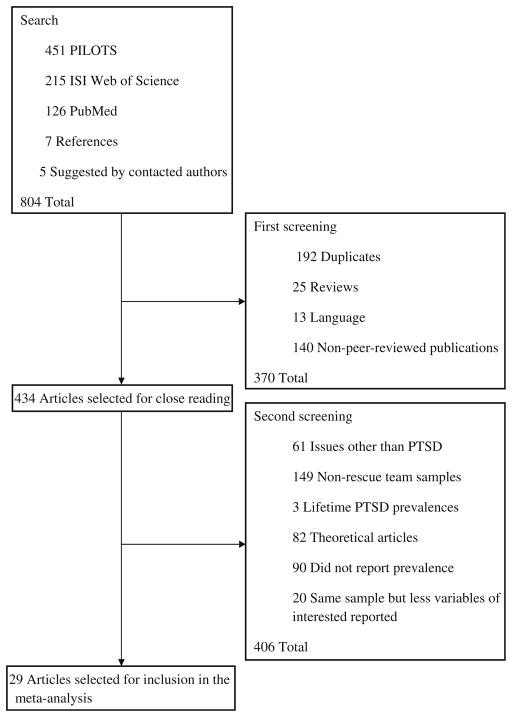
We performed a computerized systematic literature search of the ISI Web of Science, PubMed and PILOTS databases for studies reporting on the prevalence of PTSD in rescue workers until September 2008, without language restrictions and combining the following thesaurus terms and free-text searches: PTSD, posttraumatic stress disorder*, firefighter*, ambulance personnel*, emergency personnel*, paramedic*, urban fire service*, rescue*, ambulance service*, ambulance worker*, disaster-worker*, divers, emergency service*, and helper*. The asterisks mean that all terms beginning with these roots were searched (Fig. 1). As each database has a specific thesaurus system, we employed the following search strategy with respect to controlled vocabularies: (1) ISI Web of Science, we used the field TS (topic), which includes title, abstract, and keywords; (2) PubMed, we used the fields title and medical subject headings (MeSH), the controlled vocabulary used for indexing articles; and (3) PILOTS, the keywords were utilized for the search, which includes title, abstract, and descriptors (controlled vocabulary). Studies were considered for inclusion if they provided original data on the prevalence of PTSD in ambulance personnel, canine handlers, firefighters, rescue workers (when the precise occupational group studied was not spelled out by the authors), or police officers. Unlike other occupational groups, police officers are not primarily engaged in rescue work as defined herein during their regular activities. Considering the focus of the present study, articles reporting on PTSD prevalence among policemen were included only if they were conducted after a rescue operation resulting from a major disaster. Articles investigating other less studied occupational groups, namely recovery workers, body handlers and military medical workers, were not included in this review because their activities do not typically involve rescuing living human beings or due to their possible involvement in war experiences. Studies based on combined samples of rescue workers which included at least one of these occupational groups were also excluded. We identified additional studies by hand searching the references of the original and review articles retrieved, as well as by personal contact with scientific authorities in the field of the epidemiology of PTSD. Five of them were asked whether they were aware of unpublished or ongoing studies, but only two provided timely feedback to our questions. In a first screening of titles and abstracts of all identified papers, the first author (W.B.) excluded duplicated studies retrieved from more than one database, reviews, articles published in languages other than English, as well as non-peer-reviewed publications. In a second screening, the same author scrutinized the full text of the remaining studies and excluded those that only investigated issues other than PTSD, were conducted on non-rescue team samples, assessed only lifetime PTSD prevalences, and those that failed to report prevalence estimates, as well as theoretical articles. Although there are many relevant studies reporting on prevalences of PTSD based on the Impact of Event Scale (IES) [15–22] and on the 12-item General Health Questionnaire (GHQ-12) [23, 24], we decided to exclude studies based on these instruments, because the GHQ-12 is a screening instrument developed to identify general psychological distress [25, 26], rather than specific symptoms of PTSD, and the IES was designed to tap into intrusive and avoidance symptoms, two commonly reported psychological responses to trauma, do not assesses an entire PTSD symptoms cluster, namely hyperarousal [27]. Therefore these instruments do not reflect the current DSM criteria for PTSD. In Fig. 1, these studies were included under the category “did not report prevalence”. Further, whenever different studies presenting data on the same sample were identified (as characterized by coincidences in authorship, number of participants, sociodemographic and clinical characteristics of the sample, and prevalence estimates), only the study reporting the higher number of independent variables of interest for this review was taken into consideration. When a paper failed to mention one or more of the independent variables analyzed in this review but otherwise satisfied the inclusion criteria, an e-mail was sent to the author asking about the missing data. Many of these contacted authors provided relevant additional information and suggested other articles, which were also considered for inclusion.
Fig. 1.
Flow diagram of studies search and selection
We followed the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines [28] for reporting meta-analyses and systematic reviews, and our search strategy and the results obtained are described in Fig. 1.
Data extraction and investigated variables
Data were extracted from full-text articles by the first author (W.B.) and were reviewed by two others (M.V.M. and E.S.F.C.). Diverse categorical and continuous independent variables were investigated in this review and grouped into four classes as follows:
Methodology-related
Year of publication of the study; response rate; type of instrument employed (i.e., self-report vs. interview); diagnostic criteria for PTSD (i.e., studies employing a cut-off value from self-report instruments vs. those using self-report instruments based on the DSM criteria, and vs. those using interviews based on DSM criteria); and requirement of impairment for the diagnosis of PTSD (i.e., assessed whether the studies required DSM criterion F, which refers to impairment in social, occupational, or other important areas of functioning). Although the DSM also includes an impairment criterion for diagnosing PTSD, relatively few studies have consistently probed this issue for identifying probable cases of PTSD.
Sociodemographic-related
Geographic location (i.e., continent where the study was conducted); level of economic development of the country where the study was conducted (according to the International Monetary Fund classification [29]); mean age of rescue workers at the time of the assessment; percentage of men; and percentage of married or cohabiting subjects.
Work-related
Occupational group [i.e., ambulance personnel, firefighters, police officers exposed to a major disaster and “other rescue teams” (the latter including samples where more than one occupational group were grouped together and studies in which the occupational group was not specified by the original authors)], type of work [i.e., professional vs. non-professional (the latter comprising volunteers and/or trainees) vs. unspecified/mixed samples], and average length of service as rescuers at the time of the assessment.
Trauma-related
Exposure to the same major disaster (i.e., rescuers deployed to a specific major catastrophe such as an earthquake, vs. exposure to routine work-related traumatic events) and nature of the major disaster (i.e., no exposure to a major disaster vs. exposure to a human-made disaster vs. exposure to a natural disaster).
Whenever a study reported results for more than one type of rescue workers (e.g., professional vs. volunteer firefighters), all of them were included in the statistical analysis as separate categories. In longitudinal studies, only the baseline measurements were used in the analyses.
Meta-analytical procedures
Prevalence data from all samples were pooled using a random effects model. We used the Q statistic, which follows a chi-square distribution, as a formal test for homogeneity [30]. Heterogeneity was also evaluated using I2 statistics [31], which describe the proportion of variability in the effect estimate due to heterogeneity rather than chance. We dealt with heterogeneity initially through an exploratory subgroup analysis carried out to pool prevalence estimates according to the four classes of variables mentioned above. In order to further evaluate the role of each variable for the observed heterogeneity among prevalence estimates, we fitted meta-regression models for the logit-transformed prevalence as the dependent variable. These models evaluate the contribution of one or more covariates to the dependent variable, taking into account the sample size of the study. The transformation was done to overcome the problem of asymmetry in the distribution of the dependent variable. The strategy for selecting the candidate independent variables for the final model was carried out as suggested by [32]: (1) the process started with careful univariate analysis for each variable; (2) those with P values <0.25 were selected to enter in a multivariate model; and (3) finally, only those with P values <0.10 were retained in the final model in order to avoid unrealistically large estimated coefficients and/or estimated standard errors due to overfitting. We considered values of P ≤ 0.05 as statistically significant and those between 0.05 and 0.10 as having borderline statistical significance.
Statistical analysis was performed with Stata 10.0 using metan and metareg commands.
Results
We screened a total of 804 abstracts published in the last 45 years. After applying the inclusion/exclusion criteria, 29 studies were selected. However, one study [33] that used an unspecified diagnostic interview for PTSD and reported an unusually high current prevalence of 85.7% among a non-representative group of self-selected police officers was considered an outlier and excluded from the analyses. Our final pool of studies comprised 28 articles, with 40 samples and 20,424 rescue workers from 14 countries of all continents [6, 8–10, 12, 34–56] (these studies were included in the meta-analysis).
The random effects model analysis showed that rescue workers as a unified category have a high pooled current worldwide prevalence of PTSD: 10.0% (95% CI: 8.1–11.9%). However, the I2 statistic and chi-square test for heterogeneity confirmed that rescue workers are an extremely heterogeneous group (I2 = 95% and χ2 = 869.92; df = 39; P <0.001, respectively), with a variety of variables influencing the prevalence of PTSD.
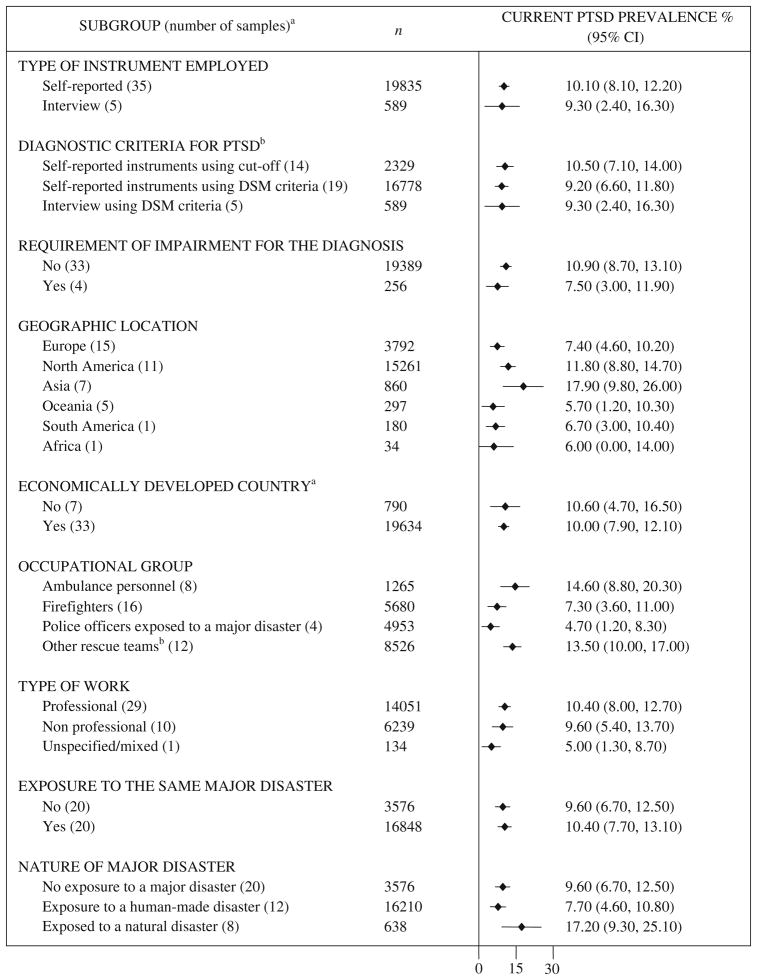
The subgroup analysis for categorical variables is presented in Fig. 2. Stratification by the variables “requirement of impairment for the diagnosis of PTSD” (χ2 = 18.31; df = 2; P <0.001), “geographic location” (χ2 = 13.39; df = 5; P = 0.02), “occupational group” (χ2 = 16.37; df = 3; P = 0.001) and “type of work” (χ2 = 5.93; df = 2; P = 0.05) provided different prevalence estimates.
Fig. 2.
Current pooled prevalence of PTSD in rescue workers according to sociodemographic, methodological, work and trauma-related categorical variables
Note. PTSD=Posttraumatic stress disorder; CI=Confidence interval.
aThe number of samples and the n reported in each subgroup vary because of the data available from the selected studies. aAccording to the International Monetary Fund. bIncludes samples comprising more than one occupational group and unspecified rescue teams.
In order to further explore the role of each variable in the prevalence heterogeneity, meta-regression models were fitted for the logit of the PTSD prevalence, including both categorical and continuous variables. According to the univariate meta-regression analysis (Table 1), “geographic location”, “occupational group” and “average age of rescue workers at assessment” significantly influence the prevalence of PTSD among rescue workers. Considering that positive meta-regression coefficients express an increased prevalence compared to the reference group, studies carried out on the Asian continent had, on average, the highest prevalence estimates. This difference is statistically significant when compared to Europe (β = 1.10; P = 0.02), but not to North America (β = 0.57; P = 0.21). Ambulance personnel had a higher average PTSD prevalence compared to firefighters (β = −0.80; P = 0.04) and police officers exposed to a major disaster (β = −1.22; P = 0.04). For the continuous variables, a younger mean age of rescue workers at assessment was inversely associated with a higher PTSD prevalence (β = −0.05; P = 0.04).
Table 1.
Univariate meta-regression of the logit of PTSD prevalence, according to methodological, sociodemographic, work and trauma-related characteristics
| Variable | Coefficient (β) | 95% CI | P value |
|---|---|---|---|
| Methodology-related | |||
| Year of publication of the study | −0.05 | −0.12 to 0.02 | 0.15 |
| Response rate | 0.01 | −0.007 to 0.04 | 0.18 |
| Type of instrument employed | |||
| Self-reported | Reference | ||
| Interview | 0.10 | −0.94 to 1.14 | 0.84 |
| Diagnostic criteria for PTSD | |||
| Self-reported instruments using cut-off | Reference | ||
| Self-reported instruments using DSM criteria | −0.12 | −0.86 to 0.62 | 0.74 |
| Interviews using DSM criteria | 0.07 | −1.09 to 1.23 | 0.91 |
| Requirement of impairment for the diagnosis of PTSD | |||
| No | Reference | ||
| Yes | −0.20 | −1.30 to 0.89 | 0.71 |
| Sociodemographic-related | |||
| Geographic location | |||
| Europe | Reference | ||
| North America* | 0.54 | −0.20 to 1.28 | 0.15 |
| Asia* | 1.10 | 0.21 to 2.00 | 0.02 |
| Oceania | 0.001 | −1.10 to 1.10 | 0.99 |
| South America | −0.03 | −1.91 to 1.84 | 0.97 |
| Africa | −0.15 | −2.51 to 2.20 | 0.90 |
| Economically developed countrya | |||
| No | Reference | ||
| Yes | −0.05 | −0.93 to 0.84 | 0.90 |
| Mean age of rescue workers at the time of the assessment | −0.05 | −0.09 to −0.003 | 0.04 |
| Percentage of men | −0.003 | −0.03 to 0.02 | 0.81 |
| Percentage of married or cohabiting | 0.005 | −0.01 to 0.02 | 0.61 |
| Work-related | |||
| Occupational group | |||
| Ambulance personnel | Reference | ||
| Firefighters | −0.80 | −1.59 to −0.02 | 0.04 |
| Police officers exposed to a major disaster | −1.22 | −2.35 to −0.08 | 0.04 |
| Others rescue teamsb | −0.04 | −0.85 to 0.76 | 0.91 |
| Type of work | |||
| Professional | Reference | ||
| Non professional | −0.09 | −0.89 to 0.71 | 0.83 |
| Unspecified/mixed | −0.72 | −2.77 to 1.32 | 0.48 |
| Average length of service as rescuers at the time of the assessment | −0.04 | −0.14 to 0.07 | 0.47 |
| Trauma-related | |||
| Exposure to the same major disaster | |||
| No | Reference | ||
| Yes | 0.14 | −0.50 to 0.78 | 0.66 |
| Nature of major disaster | |||
| No exposure to a major disaster | Reference | ||
| Exposure to a human-made disaster | −0.24 | −0.93 to 0.45 | 0.49 |
| Exposure to a natural disaster | 0.76 | −0.05 to 1.56 | 0.07 |
CI confidence interval
According to International Monetary Fund
Includes samples comprising more than one occupational group and unspecified rescue teams
North America (reference) versus Asia: coefficient = 0.57; 95% CI: −0.34 to 1.47; P = 0.21
Finally, when the categorical and continuous variables selected in the univariate meta-regression analysis were entered in the multivariate model, the only variables that remained significantly associated with the pooled current prevalence of PTSD among rescue workers were “geographic location” and “occupational group”’ (Table 2). As observed in the univariate analysis, studies carried out on the Asian continent had, on average, higher prevalence estimates compared to those from Europe (β = 1.04; P = 0.04), but not to those from North America (β = 0.69; P = 0.13). Studies with ambulance personnel also showed higher PTSD prevalence estimates compared to studies with firefighters and police officers exposed to major disasters (β = −0.90; P = 0.04 and β = −1.29; p = 0.03, respectively). Adjusted R2 values showed that these two variables explain 27% of the between-studies variance (heterogeneity).
Table 2.
Multivariate meta-regression of the logit of PTSD prevalence, according to methodological, sociodemographic, work and trauma-related characteristics: final model
| Variable | Coefficient (b) | 95% CI | P value |
|---|---|---|---|
| Sociodemographic-related | |||
| Geographic location | |||
| Europe | Reference | ||
| North America* | 0.36 | −0.40 to 1.11 | 0.34 |
| Asia* | 1.04 | 0.03 to 2.05 | 0.04 |
| Oceania | 0.009 | −1.06 to 1.08 | 0.99 |
| South America | −0.79 | −2.64 to 1.07 | 0.39 |
| Africa | −0.004 | −2.30 to 2.29 | 0.99 |
| Work-related | |||
| Occupational group | |||
| Ambulance personnel | Reference | ||
| Firefighters | −0.90 | −1.75 to −0.06 | 0.04 |
| Police officers exposed to a major disaster | −1.29 | −2.14 to −0.13 | 0.03 |
| Other rescue teams | −0.62 | −1.55 to 0.31 | 0.22 |
| Constant | −1.85 | −2.61 to −1.08 | <0.001 |
Tau2 = 0.5094; I2 residuals = 88.34%; Adjusted R2 = 27.0%
Comparison of North America (reference) versus Asia: coefficient = 0.69; 95% CI: −0.22 to 1.59; P = 0.13
It also important to notice that response rate was also associated with the heterogeneity of prevalence estimates, even when controlling for occupational group (β = 0.02; 95% CI = 0.0–0.04; P = 0.05). This result means that prevalence estimates increased as response rates improved. Nevertheless, response rate was not included in the final model because otherwise the number of samples would have decreased from 40 to 27 due to missing information.
Discussion
Our literature review and meta-analysis showed that the pooled current worldwide prevalence of PTSD in rescue workers in general is 10%. Meta-regression modeling found higher prevalence estimates in studies conducted in Asia and among ambulance personnel.
Although several researchers have described rescue operations as an occupational hazard for the development of PTSD [9, 57], this is the first study to estimate the pooled PTSD prevalence among these professionals and to determine its correlates. The current prevalence we found, 10%, is higher than both 1.3–3.5% reported in the general population from diverse countries [58–61] and the 3–6% described in UK veterans returning from the Iraq War [62]. However, it is comparable to the 2–17% prevalence estimates found in US Vietnam and Iraq veterans [62, 63] and lower than the 19–39% found in direct disaster victims [64]. These comparisons confirm that rescue workers are a high-risk group for the development of PTSD. However, even the high PTSD prevalence found in the present study probably underestimates the real magnitude of the problem, because traumatized rescue workers have increased sick leaves and tend to retire prematurely [10, 65], thus becoming unavailable for studies that investigate only active workers.
Although we have described the prevalence of PTSD in rescuers in general, these workers were found to be highly heterogeneous regarding sociodemographic characteristics, assigned duties, and type and frequency of exposure to traumatic events. They comprised different occupational groups that are thought to be associated with varying levels of risk for developing PTSD. Our results support previous observations that ambulance personnel have the highest prevalence of PTSD among all occupational groups of rescuers, and police officers had the lowest [66]. This difference in prevalence estimates may be explained by the fact that ambulance personnel are exposed to greater pressure and stress at work than other rescue teams [67]. They respond to more emergency calls than police officers and firefighters combined [41] and have closer contact with the victims, a fact that may foster the process of identification and potentially increase the feelings of guilt when they fail in their attempts to help them [68]. However, because police officers are required to carry firearms during their duty hours, they may be submitted to different selection criteria, which can lead to a more psychologically resilient workforce. This requirement can also make police officers more prone to underreport psychological problems than other rescuers for fear that they will be judged as unfit to perform their job responsibilities [8]. It is noteworthy that our results refer only to police officers exposed to a major disaster, and therefore may not be generalizable to all police force members.
We also found that rescuers from Asia had higher prevalence estimates of PTSD than rescuers from Europe. However, six out of the seven Asian samples were assessed after an earthquake. Because earthquakes are the natural disasters most capable of causing widespread destruction, and consequently, result in major human and economic losses [69], they are also conceivably the most traumatizing events. In addition, Asia has been repeatedly hit by the deadliest natural disasters (including earthquakes) on earth for years [70]. It is conceivable that the exposure of almost all samples of rescuers from Asia to disasters of such magnitude can account, at least partially, for the higher PTSD prevalence observed in these workers. In addition, other variables may contribute to the higher PTSD prevalence found among Asian rescuers as compared to Europeans. For instance, differences in financial compensation policies and in the amount and type of psychological support provided could influence rescuer’s resilience.
Some of our negative results warrant further consideration. First, we found no association between gender composition and the prevalence of PTSD. It may seem counterintuitive, because female gender has been consistently associated with the risk of developing PTSD in the general population [71]. However, studies with military and police officers also have failed to find an increased risk for PTSD in females [72]. It is conceivable that some characteristics shared by militaries, police officers and rescuers, such as rigorous selection and training, tend to decrease the impact of gender-related differences in the risk for developing PTSD. It is, therefore, not unlikely that the increased risk for PTSD reported in women from general population might be better explained by factors other than genetic or biological differences. Nevertheless, it must be noted, that in 3/4 of the studies reviewed, males comprised at least 85% of the sample, a fact that reduced the power needed for detecting gender effects.
The second negative finding was the lack of differences between the prevalence estimates of PTSD in samples of professionals versus non-professional rescuers (i.e., trainees and volunteers). This result differs from some [8, 48], but not all [39] studies directly comparing samples of professionals and trainees/volunteers exposed to a same disaster. Given the evidence that training is a key factor for fostering resilience in rescue workers, we speculate that the lack of differences in the two groups might be driven by a bias toward the self-selection of highly resilient volunteers. Many professional rescuers depend on their jobs to support themselves and their families and may refuse to quit their jobs even when suffering from PTSD. On the other hand, volunteer rescuers have no need to get involved in rescuer activities and do it exclusively because of their desire to help.
Third, we found no significant differences between the prevalences of PTSD in rescuers from developed and developing countries. However, 97% of the participants included in this review were from studies conducted in developed countries. This fact not only prevented us from reaching any definitive conclusion about the differences in the prevalence of PTSD between rescuers from developed and developing countries, but also points out the need for more scientific research in poorer countries.
Fourth, we found that the prevalence of PTSD in rescue workers investigated after the exposure to the same major disaster were not significantly different from that of rescuers investigated in their daily occupational routine, where they are repeatedly exposed to traumatic events of less magnitude, but not necessarily to a major disaster. A possible explanation for this counterintuitive finding can be found in the “buffering hypothesis”, according to which social support received during times of intense stress may reduce the psychological impact of traumatic events [73]. It is conceivable that major disasters, as compared to relatively minor, isolated incidents, may activate social networks to a greater degree, providing rescue workers with increased social support. This finding, taken together with the high prevalence of PTSD reported in the present study, highlights the importance of implementing continuous effective preventive measures for PTSD, such as stepped collaborative care and cognitive behavioral therapy for acute stress disorder [74], in the work environment of rescue workers instead of only in the aftermath of a disaster.
Limitations
Our findings should be interpreted within the context of some limitations. First, our literature search was performed in only three electronic databases, a fact that may have precluded us from identifying all studies on this topic. Nevertheless, the chosen databases are among the most relevant and representative sources in the field of mental health, including PILOTS, which is the largest database of publications on PTSD in the world (http://www.ptsd.va.gov). Further, we also performed hand searching and had direct contact with authors and experts. Even if any study was left aside by our search, it is unlike to have a large influence on our conclusions. Second, in an attempt to reduce the heterogeneity and to base our results on the best scientific evidence available we decided to be very rigorous in our studies selection. This approach restricted our pool of papers to 29 studies, and it is conceivable that other relevant papers were left out of this analysis. Third, in spite the rigorous studies selection, we still found a high heterogeneity, which warrants caution in interpreting our findings. Fourth, our search strategy covered only peer-reviewed literature, a decision that may have increased the possibility of reporting biases. Fifth, our final model explained only 27% of the heterogeneity in PTSD prevalence. Although we have assessed a considerable number of variables in this review, the role of many well-known correlates of PTSD, such as neuroticism, lack of social support [64], working hours and the deployment schedules of individuals from different countries could not be investigated due to the lack of specific data in the retrieved studies and this may account for at least part of the observed heterogeneity.
Despite these limitations, we were able to demonstrate that rescue workers in general have a pooled current prevalence of PTSD that is much higher than that of the general population and that ambulance personnel and rescuers from Asia may be more susceptible to PTSD. These results indicate the need for improving pre-employment strategies to select the most resilient individuals for rescue work, to implement continuous preventive measures for personnel, and to promote educational campaigns about PTSD and its therapeutic possibilities in order to help rescuers become more aware of this disorder and make them more comfortable to talk about it and seek treatment. In addition, the high heterogeneity found in our analysis points out the need for more refined research studies which should adopt stricter criteria for identifying rescue workers, a standardized definition of epidemiological terms such as “current prevalence” (e.g., symptoms present in the last month or in the last 6 months), and more representative sampling of rescue workers.
Additional studies are also necessary to address other relevant issues such as the prevalence of partial PTSD and burnout, and what are the most effective measures to prevent PTSD and other disorders in this population.
Acknowledgments
This work was supported by CNPq (Nacional Research Council)—Federal Government of Brazil, FAPERJ—Programa de Apoio ás Instituições de Ensino e Pesquisa (Projeto E-6/110.324/2007), and Confederação Nacional do Comércio de Bens, Serviços e Turismo (CNC). Drs. Berger, Coutinho, Figueira and Mendlowicz were partially supported by grants from CNPq. Dr. Marmar was partially supported by grant R01-MH056350-06 from the National Institute of Mental Health. Dr. Neylan was partially supported by the NIMH grants: MH057157 and MH73978.
Contributor Information
William Berger, Email: wberger@globo.com, Institute of Psychiatry, Universidade Federal do Rio de Janeiro (IPUB-UFRJ), Rua Almirante Saddock de Sá, 290/402 Ipanema, Rio de Janeiro, RJ 22411-040, Brazil, Department of Psychiatry, University of California, San Francisco (UCSF), San Francisco, CA, USA, San Francisco Department of Veterans Affairs Medical Center (DVAMC), Psychiatry Service, San Francisco, CA, USA.
Evandro Silva Freire Coutinho, Department of Epidemiology, Escola Nacional de Saúde Pública (ENSP-FIOCRUZ), Rio de Janeiro, RJ, Brazil.
Ivan Figueira, Institute of Psychiatry, Universidade Federal do Rio de Janeiro (IPUB-UFRJ), Rua Almirante Saddock de Sá, 290/402 Ipanema, Rio de Janeiro, RJ 22411-040, Brazil.
Carla Marques-Portella, Institute of Psychiatry, Universidade Federal do Rio de Janeiro (IPUB-UFRJ), Rua Almirante Saddock de Sá, 290/402 Ipanema, Rio de Janeiro, RJ 22411-040, Brazil.
Mariana Pires Luz, Institute of Psychiatry, Universidade Federal do Rio de Janeiro (IPUB-UFRJ), Rua Almirante Saddock de Sá, 290/402 Ipanema, Rio de Janeiro, RJ 22411-040, Brazil.
Thomas C. Neylan, Department of Psychiatry, University of California, San Francisco (UCSF), San Francisco, CA, USA, San Francisco Department of Veterans Affairs Medical Center (DVAMC), Psychiatry Service, San Francisco, CA, USA
Charles R. Marmar, Department of Psychiatry, University of California, San Francisco (UCSF), San Francisco, CA, USA, San Francisco Department of Veterans Affairs Medical Center (DVAMC), Psychiatry Service, San Francisco, CA, USA
Mauro Vitor Mendlowicz, Institute of Psychiatry, Universidade Federal do Rio de Janeiro (IPUB-UFRJ), Rua Almirante Saddock de Sá, 290/402 Ipanema, Rio de Janeiro, RJ 22411-040, Brazil, Department of Psychiatry and Mental Health, Universidade Federal Fluminense (MSM-UFF), Niterói, RJ, Brazil.
References
- 1.Marmar CR, McCaslin SE, Metzler TJ, Best S, Weiss DS, Fagan J, Liberman A, Pole N, Otte C, Yehuda R, Mohr D, Neylan T. Predictors of posttraumatic stress in police and other first responders. Blackwell; Oxford: 2006. pp. 1–18. [DOI] [PubMed] [Google Scholar]
- 2.Norris FH. Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. J Consult Clin Psychol. 1992;60:409–418. doi: 10.1037//0022-006x.60.3.409. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. American Psychiatric Press; Washington: 2000. Revised. [Google Scholar]
- 4.Neuner F, Schauer M, Karunakara U, Klaschik C, Robert C, Elbert T. Psychological trauma and evidence for enhanced vulnerability for posttraumatic stress disorder trough previous trauma among West Nile refugees. BMC Psychiatry. 2004;4:34. doi: 10.1186/1471-244X-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3. American Psychiatric Press; Washinton: 1980. [Google Scholar]
- 6.Morren M, Yzermans CJ, van Nispen RMA, Wevers SJM. The health of volunteer firefighters three years after a technological disaster. J Occup Health. 2005;47:523–532. doi: 10.1539/joh.47.523. [DOI] [PubMed] [Google Scholar]
- 7.Stewart SH, Mitchell TL, Wright KD, Loba P. The relations of PTSD symptoms to alcohol use and coping drinking in volunteers who responded to the Swissair Flight 111 airline disaster. J Anxiety Disord. 2004;18:51–68. doi: 10.1016/j.janxdis.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 8.Perrin MA, DiGrande L, Wheeler K, Thorpe L, Farfel M, Brackbill R. Differences in PTSD prevalence and associated risk factors among world trade center disaster rescue and recovery workers. Am J Psychiatry. 2007;164:1385–1394. doi: 10.1176/appi.ajp.2007.06101645. [DOI] [PubMed] [Google Scholar]
- 9.Fullerton CS, Ursano RJ, Wang LM. Acute stress disorder, posttraumatic stress disorder, and depression in disaster or rescue workers. Am J Psychiatry. 2004;161:1370–1376. doi: 10.1176/appi.ajp.161.8.1370. [DOI] [PubMed] [Google Scholar]
- 10.Berger W, Figueira I, Maurat AM, Bucassio EP, Vieira I, Jardirn SR, Coutinho ESE, Mari JJ, Mendlowicz MV. Partial and full PTSD in Brazilian ambulance workers: prevalence and impact on health and on quality of life. J Trauma Stress. 2007;20:637–642. doi: 10.1002/jts.20242. [DOI] [PubMed] [Google Scholar]
- 11.Alvarez J, Hunt M. Risk and resilience in canine search and rescue handlers after 9/11. J Trauma Stress. 2005;18:497–505. doi: 10.1002/jts.20058. [DOI] [PubMed] [Google Scholar]
- 12.Wagner D, Heinrichs M, Ehlert U. Prevalence of symptoms of posttraumatic stress disorder in German professional firefighters. Am J Psychiatry. 1998;155:1727–1732. doi: 10.1176/ajp.155.12.1727. [DOI] [PubMed] [Google Scholar]
- 13.DiMaggio C, Galea S. The behavioral consequences of terrorism: a meta-analysis. Acad Emerg Med. 2006;13:559–566. doi: 10.1197/j.aem.2005.11.083. [DOI] [PubMed] [Google Scholar]
- 14.Ward CL, Lombard CJ, Gwebushe N. Critical incident exposure in South African emergency services personnel: prevalence and associated mental health issues. Emerg Med J. 2006;23:226–231. doi: 10.1136/emj.2005.025908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Alexander DAF, Klein S. Ambulance personnel and critical incidents: impact of accident and emergency work on mental health and emotional well-being. Br J Psychiatry. 2001;178:76–81. doi: 10.1192/bjp.178.1.76. [DOI] [PubMed] [Google Scholar]
- 17.Bryant RA, Harvey AG. Posttraumatic stress reactions in volunteer firefighters. J Trauma Stress. 1996;9:51–62. doi: 10.1007/BF02116833. [DOI] [PubMed] [Google Scholar]
- 18.Corneil W, Beaton RD, Murphy SA, Johnson C, Pike K. Exposure to traumatic incidents and prevalence of posttraumatic stress symptomatology in urban firefighters in two countries. J Occup Health Psychol. 1999;4:131–141. doi: 10.1037//1076-8998.4.2.131. [DOI] [PubMed] [Google Scholar]
- 19.Ersland S, Weisaeth L, Sund A. The stress upon rescuers involved in an oil rig disaster: “Alexander L. Kielland” 1980. Acta Psychiatr Scand Suppl. 1989;355:38–49. doi: 10.1111/j.1600-0447.1989.tb05252.x. [DOI] [PubMed] [Google Scholar]
- 20.Grieger TA, Staab JP, Cardena E, McCarroll JE, Brandt GT, Fullerton CS, Ursano RI. Acute stress disorder and subsequent posttraumatic stress disorder in a group of exposed disaster workers. Depress Anxiety. 2000;11:183–184. doi: 10.1002/1520-6394(2000)11:4<183::AID-DA7>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 21.Jonsson A, Segesten K. Daily stress and concept of self in Swedish ambulance personnel. Prehosp Disaster Med. 2004;19:226–234. doi: 10.1017/s1049023x00001825. [DOI] [PubMed] [Google Scholar]
- 22.van der Ploeg E, Kleber RJ. Acute and chronic job stressors among ambulance personnel: predictors of health symptoms. Occup Environ Med. 2003;60:i40–i46. doi: 10.1136/oem.60.suppl_1.i40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldberg DP, Williams P. A user’s guide to the General Health Questionnarie. NFER-Nelson; Windsor: 1988. [Google Scholar]
- 24.McFarlane AC. Long-term psychiatric morbidity after a natural disaster: implications for disaster planners and emergency services. Med J Aust. 1986;145:561–563. [PubMed] [Google Scholar]
- 25.Goldberg DP, Blackwel B. Psychiatric illness in general practice—a detailed study using a new method of case identification. Br Med J. 1970;2:439–443. doi: 10.1136/bmj.2.5707.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salama-Younes M, Montazeri A, Ismail A, Roncin C. Factor structure and internal consistency of the 12-item General Health Questionnaire (GHQ-12) and the Subjective Vitality Scale (VS), and the relationship between them: a study from France. Health Qual Life Outcomes. 2009;7:22. doi: 10.1186/1477-7525-7-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu KK, Chan KS. The development of the Chinese version of Impact of Event Scale—revised (CIES-R) Soc Psychiatry Psychiatr Epidemiol. 2003;38:94–98. doi: 10.1007/s00127-003-0611-x. [DOI] [PubMed] [Google Scholar]
- 28.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB Meta-analysis Of Observational Studies in Epidemiology Group. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 29.International Monetary Fund. World Economic Outlook Database—WEO Groups and Aggregates Information. 2008 http://www.imf.org/external/pubs/ft/weo/2008/01/weodata/groups.htm#oem.
- 30.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Wiley; West Sussex: 2009. [Google Scholar]
- 31.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 32.Hosmer DW, Lemeshow S. Applied logistic regression. Wiley; New York: 2000. [Google Scholar]
- 33.Sims A, Sims D. The phenomenology of post-traumatic stress disorder: a symptomatic study of 70 victims of psychological trauma. Psychopathology. 1998;31:96–112. doi: 10.1159/000029029. [DOI] [PubMed] [Google Scholar]
- 34.Andrews L, Joseph S, Shevlin M, Troop N. Confirmatory factor analysis of posttraumatic stress symptoms in emergency personnel: an examination of seven alternative models. Personal Individ Differ. 2006;41:213–224. [Google Scholar]
- 35.Bennett P, Williams Y, Page N, Hood K, Woollard M. Levels of mental health problems among UK emergency ambulance workers. Emerg Med J. 2004;21:235–236. doi: 10.1136/emj.2003.005645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bryant RA, Sutherland K, Guthrie RM. Impaired specific autobiographical memory as a risk factor for posttraumatic stress after trauma. J Abnorm Psychol. 2007;116:837–841. doi: 10.1037/0021-843X.116.4.837. [DOI] [PubMed] [Google Scholar]
- 37.Chen YS, Chen MC, Chou FHC, Sun FC, Chen PC, Tsai KY, Chao SS. The relationship between quality of life and posttraumatic stress disorder or major depression for firefighters in Kaohsiung, Taiwan. Qual Life Res. 2007;16:1289–1297. doi: 10.1007/s11136-007-9248-7. [DOI] [PubMed] [Google Scholar]
- 38.Clohessy S, Ehlers A. PTSD symptoms, response to intrusive memories and coping in ambulance service workers. Br J Clin Psychol. 1999;38:251–265. doi: 10.1348/014466599162836. [DOI] [PubMed] [Google Scholar]
- 39.Dean PG, Gow KM, Shakespeare-Finch J. Counting the cost: psychological distress in career and auxiliary firefighters. Australas J Disaster Trauma Stud. 2003;1:1–13. [Google Scholar]
- 40.Del Ben KS, Scotti JR, Chen YC, Fortson BL. Prevalence of posttraumatic stress disorder symptoms in firefighters. Work Stress. 2006;20:37–48. [Google Scholar]
- 41.Di Fiorino M, Massimetti G, Nencioni M, Paoli RA. Full and subthreshold Post-Traumatic Stress Disorder seven years after a flooding in rescue squads. Bridging East West Psychiatry. 2004;2:18–25. [Google Scholar]
- 42.Dudek B, Koniarek J. Relationship between sense of coherence and post-traumatic stress disorder symptoms among firefighters. Int J Occup Med Environ Health. 2000;13:299–305. [PubMed] [Google Scholar]
- 43.Durham TW, McCammon SL, Allison EJ. The psychological impact of disaster on rescue personnel. Ann Emerg Med. 1985;14:664–668. doi: 10.1016/s0196-0644(85)80884-2. [DOI] [PubMed] [Google Scholar]
- 44.Gabriel R, Ferrando L, Corton ES, Mingote C, Garcia-Camba E, Liria AF, Galea S. Psychopathological consequences after a terrorist attack: an epidemiological study among victims, the general population, and police officers. Eur Psychiatry. 2007;22:339–346. doi: 10.1016/j.eurpsy.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 45.Grevin F. Posttraumatic stress disorder, ego defense mechanisms, and empathy among urban paramedics. Psychol Rep. 1996;79:483–495. doi: 10.2466/pr0.1996.79.2.483. [DOI] [PubMed] [Google Scholar]
- 46.Guo YJ, Chen CH, Lu ML, Tan HKL, Lee HW, Wang TN. Posttraumatic stress disorder among professional and nonprofessional rescuers involved in an earthquake in Taiwan. Psychiatry Res. 2004;127:35–41. doi: 10.1016/j.psychres.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 47.Guthrie RM, Bryant RA. Extinction learning before trauma and subsequent posttraumatic stress. Psychosomat Med. 2006;68:307–311. doi: 10.1097/01.psy.0000208629.67653.cc. [DOI] [PubMed] [Google Scholar]
- 48.Hagh-Shenas H, Goodarzi MA, Dehbozorgi G, Farashbandi H. Psychological consequences of the bam earthquake on professional and nonprofessional helpers. J Trauma Stress. 2005;18:477–483. doi: 10.1002/jts.20055. [DOI] [PubMed] [Google Scholar]
- 49.Haslam C, Mallon K. A preliminary investigation of post-traumatic stress symptoms among firefighters. Work Stress. 2003;17:277–285. [Google Scholar]
- 50.Heinrichs M, Wagner D, Schoch W, Soravia LM, Hellhammer DH, Ehlert U. Predicting posttraumatic stress symptoms from pretraumatic risk factors: a 2-year prospective follow-up study in firefighters. Am J Psychiatry. 2005;162:2276–2286. doi: 10.1176/appi.ajp.162.12.2276. [DOI] [PubMed] [Google Scholar]
- 51.Huizink AC, Slottje P, Witteveen AB, Bijlsma JA, Twisk JWR, Smidt N, Bramsen I, van Mechelen W, Van Der Ploeg HM, Bouter LM, Smid T. Long term health complaints following the Amsterdam Air Disaster in police officers and fire-fighters. Occup Environ Med. 2006;63:657–662. doi: 10.1136/oem.2005.024687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lowery K, Stokes MA. Role of peer support and emotional expression on posttraumatic stress disorder in student paramedics. J Trauma Stress. 2005;18:171–179. doi: 10.1002/jts.20016. [DOI] [PubMed] [Google Scholar]
- 53.Ozen S, Sir A. Frequency of PTSD in a group of search, rescue workers two months after 2003 Bingol (Turkey) earthquake. J Nerv Ment Dis. 2004;192:573–575. doi: 10.1097/01.nmd.0000135573.47316.67. [DOI] [PubMed] [Google Scholar]
- 54.Renck B, Weisaeth L, Skarbo S. Stress reactions in police officers after a disaster rescue operation. Nord J Psychiatry. 2002;56:7–14. doi: 10.1080/08039480252803855. [DOI] [PubMed] [Google Scholar]
- 55.Seedat S, La Grange H, Niehaus D, Stein DJ. Stress and resilience in South African firefighters. S Afr Med J. 2003;93:236–238. [PubMed] [Google Scholar]
- 56.Weiss DS, Marmar CR, Metzler TJ, Ronfeldt HM. Predicting symptomatic distress in emergency services personnel. J Consult Clin Psychol. 1995;63:361–368. doi: 10.1037//0022-006x.63.3.361. [DOI] [PubMed] [Google Scholar]
- 57.Long ME, Meyer DL, Jacobs GA. Psychological distress among American Red Cross disaster workers responding to the terrorist attacks of September 11, 2001. Psychiatry Res. 2007;149:303–308. doi: 10.1016/j.psychres.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 58.Creamer M, Burgees P, McFarlane AC. Post-traumatic stress disorder: findings from the Australian National Survey of Mental Health and Well-being. Psychol Med. 2001;3:1237–1247. doi: 10.1017/s0033291701004287. [DOI] [PubMed] [Google Scholar]
- 59.de Vries GJ, Olff M. The lifetime prevalence of traumatic events and posttraumatic stress disorder in the Netherlands. J Trauma Stress. 2009;22:259–267. doi: 10.1002/jts.20429. [DOI] [PubMed] [Google Scholar]
- 60.Eun HJ, Lee SM, Kim TH. The epidemiological study of posttraumatic stress disorder in an urban area. J Korean Neuropsychiatr Assoc. 2001;40:581–591. [Google Scholar]
- 61.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry. 2010;44:4–19. doi: 10.3109/00048670903393597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thompson WW, Gottesman II, Zalewski C. Reconciling disparate prevalence rates of PTSD in large samples of US male Vietnam veterans and their controls. BMC Psychiatry. 2006;6:19. doi: 10.1186/1471-244X-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev. 2005;27:78–91. doi: 10.1093/epirev/mxi003. [DOI] [PubMed] [Google Scholar]
- 65.North CS, Tivis L, McMillen JC, Pfefferbaum B, Cox J, Spitznagel EL, Bunch KP, Schorr J, Smith EM. Coping, functioning, and adjustment of rescue workers after the Oklahoma City bombing. J Trauma Stress. 2002;15:171–175. doi: 10.1023/A:1015286909111. [DOI] [PubMed] [Google Scholar]
- 66.Marmar CR, Weiss DS, Metzler TJ, Ronfeldt HM, Foreman C. Stress responses of emergency services personnel to the Loma Prieta earthquake Interstate 880 freeway collapse and control traumatic incidents. J Trauma Stress. 1996;9:63–85. doi: 10.1007/BF02116834. [DOI] [PubMed] [Google Scholar]
- 67.Young KM, Cooper CL. Occupational stress in the ambulance service: a diagnostic study. J Manag Psychol. 1995;10:29–36. doi: 10.1108/09552069710184418. [DOI] [PubMed] [Google Scholar]
- 68.Jonsson A, Segesten K. Guilt, shame and need for a container: a study of post-traumatic stress among ambulance personnel. Accid Emerg Nurs. 2004;12:215–223. doi: 10.1016/j.aaen.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 69.Shafique M, Van Der Meijde A, Kerle N, Van Der Meer F, Khan MA. Predicting topographic aggravation of seismic ground shaking by applying geospatial tools. J Himal Earth Sci. 2008;41:33–43. [Google Scholar]
- 70.Udomratn P. Mental health and the psychosocial consequences of natural disasters in Asia. Int Rev Psychiatry. 2008;20:441–444. doi: 10.1080/09540260802397487. [DOI] [PubMed] [Google Scholar]
- 71.Tolin DF, Foa EB. Sex differences in trauma and post-traumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- 72.Lilly MM, Pole N, Best SR, Metzler T, Marmar CR. Gender and PTSD: what can we learn from female police officers? J Anxiety Disord. 2009;23:767–774. doi: 10.1016/j.janxdis.2009.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Koopman C, Hermanson K, Diamond S, Angell K, Spiegel D. Social support, life stress, pain and emotional adjustment to advanced breast cancer. Psychooncology. 1998;7:101–111. doi: 10.1002/(SICI)1099-1611(199803/04)7:2<101::AID-PON299>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 74.Feldner MT, Monson CM, Friedman MJ. A critical analysis of approaches to targeted PTSD prevention: current status and theoretically derived future directions. Behav Modif. 2007;31:80–116. doi: 10.1177/0145445506295057. [DOI] [PubMed] [Google Scholar]