Abstract
Objective
To describe the trend in atrial fibrillation (AF) treatment strategies in newly diagnosed AF patients between 1999 and 2008.
Methods
The study was a retrospective cohort study of commercial health plans claims data. Newly diagnosed adult AF patients with ≥1 claim for an AF-related intervention within 12 months of diagnosis were identified. Based on initial treatment, patients were classified into pharmacotherapy or nonpharmacotherapy groups. Pharmacotherapy group was subcategorized into rate-control or rhythm-control groups. Linear regression to assess linear trend and multinomial logistic regression to evaluate factors associated with treatment choice were conducted.
Results
Three thousand ninety-four newly diagnosed AF patients were identified. Eighty percent of these patients were initiated on pharmacotherapy with the majority (84%) receiving rate-control medications only. Relative distribution of the 3 treatment groups remained similar over the study period. However, within the rate-control group, the use of beta blockers increased significantly (P < .001). Treatment with nonpharmacotherapy over rate-control medications was higher in males but lower in patients aged ≥80 (relative risk ratio [RRR]: 1.67, 95% confidence interval [CI]: 1.27–2.20 and RRR: 0.48, 95% CI: 0.30–0.77, respectively). Having stroke and congestive heart failure significantly affected the treatment choice between nonpharmacotherapy and rate-control medications.
Conclusion
Medication therapy, especially rate-control strategies, remains the preferred initial therapy of choice.
Keywords: atrial fibrillation, antiarrhythmic drugs, utilization, retrospective study
Introduction
Atrial fibrillation (AF) is the most prevalent form of cardiac arrhythmia.1–3 AF is marked by disorganization in the electrical activity of the cardiac system. As a result, the heart starts beating at a much faster rate (about 200 beats/min); the rhythm of contraction and relaxation of different chambers of the heart also gets compromised.4
Increasing trend in the prevalence of AF patients in the United States has been reported, with 12 million US population predicted to be affected by 2050.5 Incidence of AF increases with age; in people younger than 55 years, the prevalence of AF is only 0.1% but increases to 9% by the age of 80.1 The mean age of patients with AF is 66.8 in men and 74.6 in women.5 AF is associated with significant health care cost. A 2005 study estimated the treatment cost of AF to be $6.65 billion and approximately 350,000 hospitalizations are attributed to AF annually.6
AF management is broadly divided into rate control which aims to control ventricular rate while letting the AF to continue and rhythm control which aims to restore and maintain sinus rhythm. Rate control is generally achieved by medications such as beta blockers, calcium channel blockers, and digoxin, which are the traditionally used pharmacological agents for controlling ventricular rate. Rhythm control can be achieved either by medications such as type IA, IC, and III antiarrhythmic drugs or by nonpharmacotherapies such as electrical cardioversion, radiofrequency catheter ablation (RFCA), or Cox-Maze procedure.
Previous studies that examined the utilization of treatment options for the management of AF either focused on pharmacotherapy only or did not compare the utilization of pharmacological and nonpharmacological strategies together and are generally dated.2,7–9 Limited information is available on the recent utilization of different strategies, especially ablation techniques which have greatly evolved over the last few decades.1,10,11
In this study, we examined the recent trend in utilization of the initial pharmacological or nonpharmacological treatment received by newly diagnosed AF patients in a nationally representative sample of commercial health plans enrollees.
Methods
Data Source
This study employed a retrospective cohort study design. Data were from a 10% random sample of the PharMetrics Patient-Centric Database (IMS LifeLink™ Health Plan Claims data obtained from PharMetrics, Inc., Watertown, MA) between January 1, 1998 and December 31, 2009. The PharMetrics database is derived from the commercial health plan information of over 98 managed care plans across the United States and contains fully adjudicated medical and prescription claims for over 61 million unique patients.
Atrial Fibrillation Patient Selection
The study cohort consisted of newly diagnosed AF patients between January 1999 and December 2008, identified using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code of 427.31. Patients were required to have at least 2 claims (≥30 days apart but <365 days apart) with a primary diagnosis of AF. Also, one of these claims was required to be an outpatient medical claim. The index date was defined as the date of the first claim with a diagnosis of AF during the study period. Selected patients (1) were aged 18 or above on the index date of AF diagnosis, (2) had 12 months of continuous plan enrollment and pharmacy benefits prior to the index date, and (3) had at least 1 medical or pharmacy claim for an AF-related intervention within 12 months after the index date. Patients were also required to have continuous enrollment and pharmacy benefits prior to the first AF intervention. Patients were excluded if they had any pharmacy claims for rate-control or rhythm-control medications or medical claims for AF-related nonpharmacological treatment during the 12 months prior to the index date (Figure A1). Patients were also excluded if they had any diagnosis for ventricular arrhythmia during the 1 year before and 1 year after the index diagnosis.
Treatment Group
Based on the initial treatment received, patients were classified into pharmacotherapy or nonpharmacotherapy treatment groups. Pharmacotherapy group was further categorized into rate-control (beta blocker, calcium channel blocker, or digoxin) and rhythm-control (type IA, IC, and III anti-arrhythmic drugs) groups. The rhythm-control group consisted of patients on anti-arrhythmic drugs with or without concurrent use of rate-control medication/medications. Medications were identified via generic product identifier (GPI) codes, which are therapeutic classes maintained by MediSpan that define pharmaceutically equivalent drug products. The rate-control medications identified in our database included (beta blocker) acebutolol, atenolol bisoprolol, metoprolol, nadolol, nebivolol, pindolol, propranolol; (calcium channel blocker) diltiazem, verapamil; and digoxin.9,12 The rhythm-control medications included amiodarone, disopyramide, dofetilide, flecainide, procainamide, propafenone, quinidine, and sotalol. The nonpharmacotherapy group included patients who underwent the RFCA, Cox-Maze procedure, or electrical cardioversion as the initial treatment. These procedures were identified using the Current Procedural Terminology (CPT) codes or ICD-9 procedure code. The specific procedure codes used are included in the Appendix (Tables A2 and A3).
Data Analysis
Proportions of patients in each treatment group were calculated by calendar year. Each patient was counted only once in the calendar year of the index diagnosis date. Trends in the utilization of different treatment strategies were analyzed using linear regression models. In addition, we compared patient demographic characteristics (age and gender), geographic region, and AF-related comorbidities (stroke, hypertension, myocardial infarction [MI], diabetes, congestive heart failure [CHF] identified during the 12 months prior to the first AF diagnosis)12,13 across the 3 treatment groups using chi-square test for categorical variables and analysis of variance (ANOVA) for continuous variable. Multivariate multinomial logit regression analysis was applied to determine the factors associated with the choice of the initial treatment of AF. All analysis was conducted using SAS 9.2. A P value of <.05 was considered statistically significant.
Human Subject Protection
This study has been approved by Internal Review Board at the University of Arkansas for Medical Sciences as an exempt study.
Results
From 1999 to 2008, we identified 3094 newly diagnosed adult AF patients who received AF-related interventions within 1 year of the initial AF diagnosis and satisfied other inclusion and exclusion criteria. Most of the newly diagnosed AF patients underwent pharmacotherapy as the initial treatment compared with nonpharmacotherapy (79.57% vs 20.43%). Of the patients who initiated on pharmacotherapy for AF, the majority (83.99%) received rate-control medications only. The time to the initial treatment varied between pharmacotherapy and nonpharmacotherapy treatment groups. Nonpharmacotherapy was initiated at a median time of 51 (interquartile range [IQR]: 114) days compared with approximately 112 (IQR: 187) days in patients initiated on pharmacotherapy.
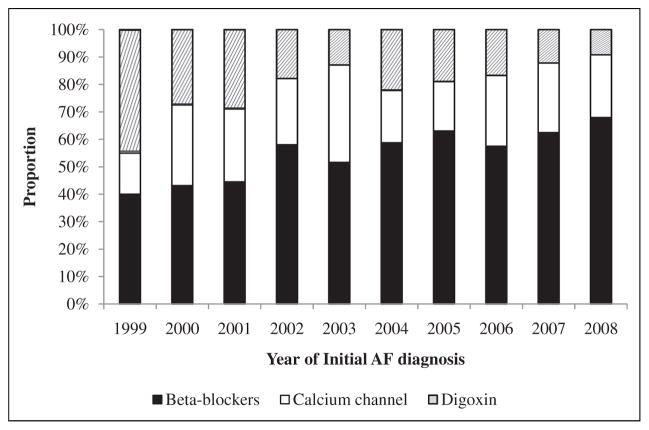
The relative distribution of the 3 types of treatments did not vary significantly during the study period (Figure A2). However, within the rate-control group, use of beta blockers increased significantly from 40% in 1999 to 68% in 2008, with an estimated annual increase of 2.8% over the study period (P < .001; Figure 1). This is accompanied by a significant decrease in the use of digoxin as the initial treatment with an annual decrease of 3.5% a year (Figure 1). For initial nonpharmacotherapy, cardioversion was the most common procedure which was performed in about 85% of the patients in this group; RFCAs accounted for the remaining 15% of the patients. The Maze procedure was only observed since 2006 and increased gradually to about 5%of patients receiving nonpharmacotherapy as the initial treatment in 2008 (Figure A3). The relative distribution of these procedures remained steady over time.
Figure 1.
Rate-control medications used as initial treatment of newly diagnosed artial fibrillation patients: 1999 to 2008.
Table 1 reports the demographic and clinical characteristics of patients by treatment groups. The majority of patients were males (60%). The average age of the patients was 66 (±14.1) at the initial AF diagnosis and more than 80% of them were older than 54 years (Table 1). Patients undergoing nonpharmacotherapy or rhythm-control treatment were significantly (P < .001) younger (63.5 ± 12.6 years and 63.7 ± 14.3 years, respectively) compared with rate-control pharmacotherapy patients (67.2 ± 14.4 years). Nonpharmacotherapy as the initial treatment is more common in patient with CHF (P = .0062) but less among patients with stroke (P = .0116; Table 1).
Table 1.
Baseline Demographic Characteristics of the Newly Diagnosed Atrial Fibrillation Patients Across the Different Treatment Groups
| Total, % | Treatment strategy
|
P valuea | |||
|---|---|---|---|---|---|
| Rate control, % | Rhythm control, % | Nonpharmacotherapy, % | |||
| N | 3094 | 2068 (66.84) | 394 (12.73) | 632 (20.43) | |
| Age group | |||||
| 18–54 | 590 (19.07) | 375 (63.56) | 86 (14.58) | 129 (21.86) | .1456 |
| 55–64 | 910 (29.41) | 550 (60.44) | 125 (13.74) | 235 (25.82) | <.0001 |
| 65–79 | 1026 (33.16) | 700 (68.23) | 129 (12.57) | 197 (19.20) | .4488 |
| ≥80 | 568 (18.36) | 443 (77.99) | 54 (9.51) | 71 (12.50) | <.0001 |
| Gender | |||||
| Female | 1245 (40.24) | 906 (72.77) | 156 (12.53) | 183 (14.70) | <.0001 |
| Male | 1849 (59.76) | 1162 (62.84) | 238 (12.87) | 449 (24.28) | <.0001 |
| Region | |||||
| East | 572 (18.49) | 435 (76.05) | 41 (7.17) | 96 (16.78) | <.0001 |
| Mid-west | 1176 (38.01) | 735 (62.50) | 158 (13.44) | 283 (24.06) | .0001 |
| South | 872 (28.18) | 587 (67.32) | 142 (16.28) | 143 (16.40) | <.0001 |
| West | 474 (15.32) | 311 (65.61) | 53 (11.18) | 110 (23.21) | .1917 |
| Comorbidity | |||||
| Stroke | 135 (4.36) | 101 (74.81) | 19 (14.07) | 15 (11.11) | .0116 |
| Hypertension | 733 (23.69) | 507 (69.17) | 86 (11.73) | 140 (19.10) | .0737 |
| Diabetes | 263 (8.50) | 171 (65.02) | 28 (10.65) | 64 (24.33) | .2838 |
| MI | 426 (13.77) | 270 (63.38) | 54 (12.68) | 102 (23.94) | .2493 |
| CHF | 292 (9.44) | 177 (60.62) | 33 (11.30) | 82 (28.08) | .0062 |
Abbreviations: CHF, congestive heart failure; MI, myocardial infarction.
P values from chi-square tests.
Table 2 reported the adjusted relative risk ratios (RRRs) from the multivariate multinomial regression exploring the potential patient demographic and clinical factors associated with the initial treatment choice received. Compared with the eastern region, patients in other regions were approximately twice as likely to receive rhythm-control therapy over rate-control treatment. On the other hand, nonpharmacotherapy was favored over rate control in patients who were male or with a history of CHF. But having a history of stroke decreased the likelihood of receiving nonpharmacotherapy as the initial treatment over rate-control medications. Also, compared with patients aged 18 to 54, patients 80 years or older were more likely to be treated with rate-control medications than with nonpharmacotherapy.
Table 2.
Results of Multinomial Logistic Regression Model
| Rhythm control versus rate control
|
Nonpharmacotherapy versus rate control
|
|||
|---|---|---|---|---|
| RRR | 95% CI | RRR | 95% CI | |
| Gender (Ref: Female) | ||||
| Male | 1.15 | 0.84–1.58 | 1.67 | 1.27–2.20 |
| Age group (Ref: 18–54) | ||||
| 55–64 | 1.36 | 0.89–2.10 | 1.27 | 0.89–1.80 |
| 65–79 | 0.95 | 0.61–1.48 | 0.97 | 0.68–1.38 |
| ≥80 | 0.72 | 0.42–1.23 | 0.48 | 0.30–0.77 |
| Region (Ref: East) | ||||
| Mid-west | 1.82 | 1.09–3.04 | 1.39 | 0.97–2.00 |
| South | 2.08 | 1.25–3.46 | 0.94 | 0.64–1.39 |
| West | 1.96 | 1.09–3.52 | 1.45 | 0.94–2.24 |
| Comorbidity | ||||
| Stroke | 1.04 | 0.61–1.77 | 0.47 | 0.27–0.84 |
| Hypertension | 0.85 | 0.63–1.17 | 0.80 | 0.62–1.04 |
| Diabetes | 0.87 | 0.56–1.37 | 1.18 | 0.84–1.66 |
| MI | 1.14 | 0.79–1.63 | 1.23 | 0.92–1.65 |
| CHF | 1.09 | 0.72–1.67 | 1.72 | 1.25–2.37 |
| Index year of AF diagnosis (Ref: 1999) | ||||
| 2000 | 0.83 | 0.16–4.33 | 1.03 | 0.20–5.32 |
| 2001 | 0.49 | 0.11–2.13 | 0.40 | 0.09–1.92 |
| 2002 | 0.56 | 0.13–2.40 | 1.35 | 0.32–5.62 |
| 2003 | 0.76 | 0.16–3.53 | 1.44 | 0.32–6.50 |
| 2004 | 0.72 | 0.17–3.01 | 1.52 | 0.37–6.27 |
| 2005 | 0.79 | 0.19–3.20 | 1.74 | 0.43–7.08 |
| 2006 | 0.71 | 0.18–2.81 | 1.33 | 0.33–5.36 |
| 2007 | 0.59 | 0.15–2.36 | 1.56 | 0.39–6.22 |
| 2008 | 0.62 | 0.16–2.43 | 1.24 | 0.31–4.91 |
Abbreviations: CHF, congestive heart failure; MI, myocardial infarction; RRR, relative risk ratio; CI, confidence interval; AF, atrial fibrillation.
Discussion
In this retrospective cohort study, we examined the trends in the use of different treatment options for newly diagnosed AF patients between 1999 and 2008. Medication use was the preferred initial strategy for AF management than nonpharmacotherapies. Although no significant changes in the trend were observed in the relative utilization of the 3 broad treatment options, within-class variation were significant for rate-control medication group with significant increases in the use of beta blockers over time.
We found rate-control medications were used most frequently as the initial therapy in the newly diagnosed AF patients in our analysis. This finding is consistent with the current guideline recommendations.14 The landmark clinical trials published around 2000 found no statistically significant difference between rate-control and rhythm-control medications in improving AF-related symptoms and survival rates; but rhythm-control medications had higher risk of adverse events.15
However, we did not find a significant increase over time in the overall rate-control medication use as the initial treatment. This finding is contrary to a study using the Canadian registry of new-onset AF patients, which found an increasing trend in the rate-control medication use compared with the rhythm-control medications from approximately 35% in 1999 to approximately 52% by 2007.12 Consistent with this Canadian study, we found a decline in the use of digoxin, which may be attributable to the evidence on its inefficacy to control ventricular rate.12 The updated 2006 American Heart Association guideline also recommended against the use of digoxin.14 This decrease in digoxin use was offset by a significant increase in the use of beta blockers, which has proven effectiveness in AF management.12
Interestingly, among users of nonpharmacotherapies, a decrease in the relative use of electrical cardioversion accompanied by an increase in RFCA procedures were observed between 1999 and 2003, after which the pattern slightly reversed and remained stable afterward (Figure A3). However, these changes in the relative proportion of nonpharmacotherapies were not statistically significant, which could be a result of small sample size. Future studies using larger databases are needed to further investigate this issue.
Our study showed that nonpharmacotherapy and rhythm-control strategy were used more frequently in comparatively younger population, with a diminishing preference in older population. Male patients were more likely to receive nonpharmacotherapy than rate-control medications. These results are consistent with other studies that found higher utilization of these nonpharmacotherapies in younger patients and in male patient population.16 For instance, a study of Medicare enrollees in the fiscal years 2001 to 2006 reported that RFCA was performed more in males than in females, and the majority of patients were younger than 75 years with decreased use associated with increasing age.3 Another study investigated the trends in characteristics of patients undergoing catheter ablation over a 7-year period from 1999 to 2005 and found that on average, 77% patients undergoing catheter ablation were male and were comparatively younger (55 ± 11 years) than nonablated patients (67 ± 11 years).17 Study by Dagre et al also reported that women undergo electrical cardioversion or catheter ablation less frequently compared to men.18 Such a gender difference may be attributable to lower referral rate against undergoing invasive treatment of women.17 The gender difference in the initial choice of therapy especially involving nonpharmacotherapies calls for further research.
We found differences across regions in the choice of initial therapy. Compared with patients in the eastern region, those in the Midwest, West, or South were significantly more likely to receive rhythm-control medications over rate-control medications as the initial treatment. Similar regional difference was found in another study.9 Such regional difference may reflect the difference in disease prevalence as cardiovascular diseases are more prevalent in the Midwest and South,19 and a previous study has found that cardiologists are more likely to prescribe rhythm-control medications than primary care physicians.9
Hypertension was the most common comorbidity (23.7%) associated with the study population followed by MI (13.8%), CHF (9.4%), and diabetes (8.5%), whereas stroke (4.4%) was the least common of the comorbidities that were studied. Similar results were seen in the study by Harley et al where hypertension was found to be the most prevalent comorbid condition (50.4%) and stroke was among the least common comorbid condition (4.6%).13 We found initial treatment choices were affected by the presence of stroke and CHF. Stroke patients were less likely to undergo nonpharmacotherapy than rate-control medications, but patients with CHF were more likely to receive nonpharmacotherapy than rate-control medication. Electrical cardioversion is a commonly used procedure to restore normal sinus rhythm in heart failure patients particularly those with marginal left ventricular function.20 However, conversion success may depend on the degree of heart failure treatment; pretreatment with medications such as beta blockers increased conversion success but amiodar-one did not affect conversion success.20 Results from the Atrial Fibrillation and Congestive Heart Failure (AF-CHF) trial suggested rate control should be considered as a primary approach for patients with AF and heart failure.21
Limitations
The PharMetrics claims data are representative of commercially insured population and therefore, results of this study may not generalize to other noncommercial populations. As a general limitation of claim database, newly diagnosed AF patients were identified by the first medical encounter and may not be the initial presentation of AF, given that many AF patients has minimal or no associated symptoms and may not be seeking medical attention at the earliest onset of the disease. No inpatient pharmacy claims were available in the PharMetrics database. Therefore, medications initiated during inpatient visits were not counted. Also, the ICD-9-CM procedure codes and CPT codes used to identify nonpharmacotherapy treatment are not specific to AF; apart from AF, these procedures may also be performed to treat other type of cardiac arrhythmia and therefore, we may have overidentified patients who underwent nonpharmacotherapy as the initial treatment for newly diagnosed AF. However, there are no validated codes for AF-related procedures. We excluded patients with ventricular arrhythmias and required at least 2 claims with AF as the primary diagnosis, which granted greater ascertainment of identifying true AF patients undergoing intervention for AF management but may have erred on being less sensitive.
Conclusion
The overall initial management of AF did not change over the study period. The medication therapy, as opposed to nonpharmacotherapy options, was the preferred choice for the initial management of AF patients. Greater use of ventricular rate-control strategy as the initial therapy compared with other treatment strategies as seen in this study is consistent with the current literature and guideline recommendation. The finding that nonpharmacotherapies were not the preferred initial therapy of choice may be due to the reluctance of patients to go for invasive procedures. Nonpharmacotherapies were more prevalent among younger patients. Gender and regional differences in the choice of the initial treatment were found in this study as well as in the previous literature, which warrants further study.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: No funding was sought out. The use of IMS Life Link Health Plans data used for this study purpose was supported by the University of Arkansas Center for Clinical and Translational Research (National Institutes of Health [NIH] Grant # UL1RR029884). Chenghui Li received funding support from Norvartis Pharmaceuticals Corportation for an unrelated study on gout. We are grateful to Dr Bradley C. Martin for his valuable comments and suggestions which have greatly improved this study.
Appendix A
Figure A1.
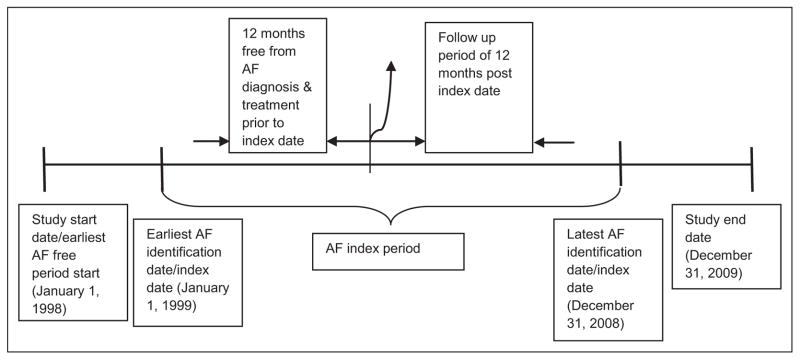
Study time line.
Figure A2.
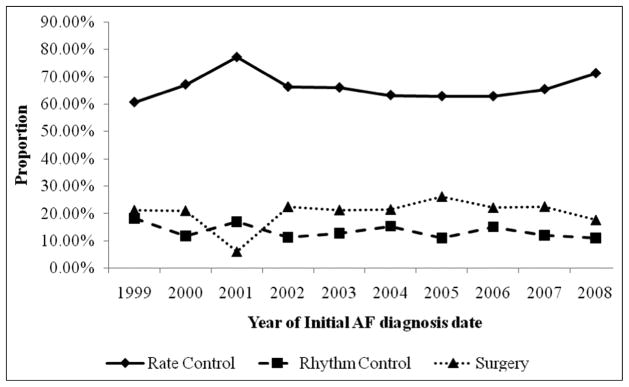
Trend in the choice of initial treatment strategies for newly diagnosed atrial fibrillation: 1999 to 2008.
Figure A3.
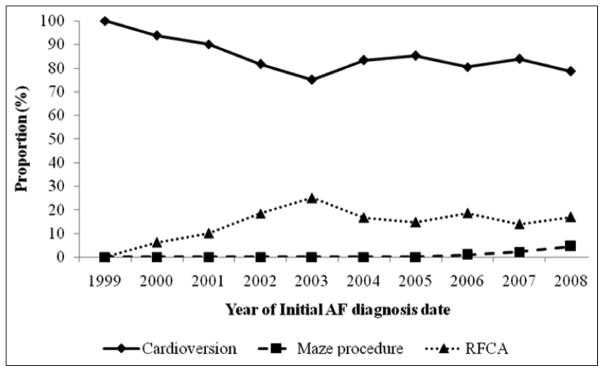
Nonpharmacotherapy used as initial treatment of newly diagnosed atrial fibrillation: 1999 to 2008.
Table A1.
| S no. | Code | ICD/CPT | Description |
|---|---|---|---|
| 1 | 433.xx-436.xx, 437.0, 437.1 | ICD-9-CM | Stroke or intracranial event |
| 2 | 401.xx, 362.11, 402.xx, 404.xx, 437.2 | ICD-9-CM | Hypertension |
| 3 | 250.xx | ICD-9-CM | Diabetes |
| 4 | 410.xx-414.xx | ICD-9-CM | Ischemic heart disease (including myocardial infarction) |
| 5 | 428.0 | ICD-9-CM | Congestive heart failure |
Abbreviations: ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; CPT, Current Procedural Terminology.
Table A2.
| S. no. | Code | ICD/CPT | Description |
|---|---|---|---|
| 1 | 93650 | CPT | Intracardiac catheter ablation of atrioventricular node function, atrioventricular conduction for creation of complete heart block, with or without temporary pacemaker placement |
| 2 | 93651 | CPT | Intracardiac catheter ablation of arrhythmogenic focus; for treatment of supraventricular tachycardia by ablation of fast or slow atrioventricular pathways, accessory atrioventricular connections or other atrial foci, singly or in combination |
| 3 | 37.34 | ICD procedure code | Catheter ablation of lesion or tissues of heart |
Abbreviations: ICD, International Classification of Diseases; CPT, Current Procedural Terminology.
Table A3.
| S. no. | Code | CPT | Description |
|---|---|---|---|
| 1 | 33255 | CPT | Operative tissue ablation and reconstruction of atria, extensive (eg, Maze procedure); without cardiopulmonary bypass |
| 2 | 33256 | CPT | Operative tissue ablation and reconstruction of atria, extensive (eg, Maze procedure); with cardiopulmonary bypass |
| 3 | 33254 | CPT | Operative tissue ablation and reconstruction of atria, limited (eg, modified Maze procedure) |
| 4 | 33266 | CPT | Endoscopy, surgical; operative tissue ablation and reconstruction of atria, extensive (eg, Maze procedure), without cardiopulmonary bypass |
| 5 | 33265 | CPT | Endoscopy, surgical; operative tissue ablation and reconstruction of atria, limited (eg, modified Maze procedure), without cardiopulmonary bypass |
| 6 | 33258 | CPT | Operative tissue ablation and reconstruction of atria, performed at the time of other cardiac procedure/procedures, extensive (eg, Maze procedure), without cardiopulmonary bypass |
| 7 | 33259 | CPT | Operative tissue ablation and reconstruction of atria, performed at the time of other cardiac procedure/procedures, extensive (eg, Maze procedure), with cardiopulmonary bypass |
| 8 | 33257 | CPT | Operative tissue ablation and reconstruction of atria, performed at the time of other cardiac procedure/procedures, limited (eg, modified Maze procedure) |
| 9 | 92960 | CPT | Cardioversion |
| 10 | 92961 | CPT | Cardioversion |
Abbreviations: CPT, Current Procedural Terminology.
Footnotes
Reprints and permission: sagepub.com/journalsPermissions.nav
All authors have read and approved the content of this manuscript. This submission represents original work and is not under review for publication anywhere else. An earlier version of the abstract has been accepted for poster presentation and was presented at the 16th Annual International Society for Pharmacoeconomics and Outcomes Research in Baltimore, Maryland, May 21–25, 2011.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Ip S, Terasawa T, Balk EM, et al. Comparative Effectiveness Review No. 15. Rockville, MD: Agency for Healthcare Research and Quality; Jul, 2009. [Accessed on October 15, 2011]. Comparative Effectiveness of Radiofrequency Catheter Ablation for Atrial Fibrillation. (Prepared by Tufts Medical Center Evidence-based Practice Center under Contract No. 290-02-0022.) Available at: www.effectivehealthcare.ahrq.gov/reports/final.cfm. [PubMed] [Google Scholar]
- 2.Fang MC, Stafford RS, Ruskin JN, et al. National trends in anti-arrhythmic and antithrombotic medication use in atrial fibrillation. Arch Intern Med. 2004;164(1):55–60. doi: 10.1001/archinte.164.1.55. [DOI] [PubMed] [Google Scholar]
- 3.Ellis ER, Culler SD, Simon AW, et al. Trends in utilization and complications of catheter ablation for atrial fibrillation in medicare beneficiaries. Heart Rhythm. 2009;6(9):1267–1273. doi: 10.1016/j.hrthm.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. [Accessed October 20, 2010];Atrial Fibrillation & Flutter. http://wwwhrspatientsorg/patients/heart_disorders/atrial_fibrillation/defaultasp [serial online] 2010;
- 5. [Accessed October 15, 2010];Atrial Fibrillation Fact Sheet. http://wwwcdcgov/dhdsp/data_s-tatistics/fact_sheets/docs/fs_atrial_fibrillationpdf [serial online] 2010;
- 6.Coyne KS, Paramore C, Grandy S, et al. Assessing the direct costs of treating nonvalvular atrial fibrillation in the United States. Value Health. 2006;9(5):348–356. doi: 10.1111/j.1524-4733.2006.00124.x. [DOI] [PubMed] [Google Scholar]
- 7.Allen LaPointe NM, Governale L, Watkins J, et al. Outpatient use of anticoagulants, rate-controlling drugs, and antiarrhythmic drugs for atrial fibrillation. Am Heart J. 2007;154(5):893–898. doi: 10.1016/j.ahj.2007.06.035. [DOI] [PubMed] [Google Scholar]
- 8.Reiffel JA, Kowey PR, Myerburg R, et al. Practice patterns among United States cardiologists for managing adults with atrial fibrillation (from the AFFECTS Registry) Am J Cardiol. 2010;105(8):1122–1129. doi: 10.1016/j.amjcard.2009.11.046. [DOI] [PubMed] [Google Scholar]
- 9.Stafford RS, Robson DC, Misra B, et al. Rate control and sinus rhythm maintenance in atrial fibrillation: national trends in medication use, 1980–1996. Arch Intern Med. 1998;158(19):2144–2148. doi: 10.1001/archinte.158.19.2144. [DOI] [PubMed] [Google Scholar]
- 10.Oral H, Scharf C, Chugh A, et al. Catheter ablation for paroxysmal atrial fibrillation: segmental pulmonary vein ostial ablation versus left atrial ablation. Circulation. 2003;108(19):2355–2360. doi: 10.1161/01.CIR.0000095796.45180.88. [DOI] [PubMed] [Google Scholar]
- 11.Cappato R, Calkins H, Chen SA, et al. Worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation. 2005;111(9):1100–1105. doi: 10.1161/01.CIR.0000157153.30978.67. [DOI] [PubMed] [Google Scholar]
- 12.Andrade JG, Connolly SJ, Dorian P, et al. Antiarrhythmic use from 1991 to 2007: insights from the Canadian Registry of Atrial Fibrillation (CARAF I and II) Heart Rhythm. 2010;7(9):1171–1177. doi: 10.1016/j.hrthm.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 13.Harley CR, Riedel AA, Hauch O, et al. Anticoagulation therapy in patients with chronic atrial fibrillation: a retrospective claims data analysis. Curr Med Res Opin. 2005;21(2):215–222. doi: 10.1185/030079904X20321. [DOI] [PubMed] [Google Scholar]
- 14.Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation-executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients with Atrial Fibrillation) Eur Heart J. 2006;27(16):1979–2030. doi: 10.1093/eurheartj/ehl176. [DOI] [PubMed] [Google Scholar]
- 15.Wyse DG, Waldo AL, DiMarco JP, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347(23):1825–1833. doi: 10.1056/NEJMoa021328. [DOI] [PubMed] [Google Scholar]
- 16.Riesgo A, Sant E, Benito L, et al. Sex differences in the treatment of patients with atrial fibrillation: population-based study in a local health district. Rev Esp Cardiol. 2011;64(3):233–236. doi: 10.1016/j.recesp.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Gerstenfeld EP, Callans D, Dixit S, et al. Characteristics of patients undergoing atrial fibrillation ablation: trends over a seven-year period 1999–2005. J Cardiovasc Electrophysiol. 2007;18(1):23–28. doi: 10.1111/j.1540-8167.2006.00662.x. [DOI] [PubMed] [Google Scholar]
- 18.Dagres N, Nieuwlaat R, Vardas PE, et al. Gender-related differences in presentation, treatment, and outcome of patients with atrial fibrillation in Europe: a report from the Euro heart survey on atrial fibrillation. J Am Coll Cardiol. 2007;49(5):572–577. doi: 10.1016/j.jacc.2006.10.047. [DOI] [PubMed] [Google Scholar]
- 19.Rich DQ, Gaziano JM, Kurth T. Geographic patterns in overall and specific cardiovascular disease incidence in apparently healthy men in the United States. Stroke. 2007;38(8):2221–2227. doi: 10.1161/STROKEAHA.107.483719. [DOI] [PubMed] [Google Scholar]
- 20.Boldt LH, Rolf S, Huemer M, et al. Optimal heart failure therapy and successful cardioversion in heart failure patients with atrial fibrillation. Am Heart J. 2008;155(5):890–895. doi: 10.1016/j.ahj.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 21.Roy D, Talajic M, Dubuc M, et al. Atrial fibrillation and congestive heart failure. Curr Opin Cardiol. 2009;24(1):29–34. doi: 10.1097/hco.0b013e32831c8c58. [DOI] [PubMed] [Google Scholar]
- 22.Wattigney WA, Mensah GA, Croft JB. Increased atrial fibrillation mortality: United States, 1980–1998. Am J Epidemiol. 2002;155(9):819–826. doi: 10.1093/aje/155.9.819. [DOI] [PubMed] [Google Scholar]
- 23. [Accessed October 25, 2010];CPT Code/Relative Value Search. https://catalogama-assnorg/Catalog/cpt/cpt_searchjsp [serial online] 2010;
- 24.Ishak JK, Proskorovsky I, Guo S, et al. Persistence With Antiarrhythmics and the Impact on Atrial Fibrillation-Related Outcomes. Am J Pharm Benefits. 2009;1(4):193–200. [Google Scholar]
- 25.Boccuzzi SJ, Martin J, Stephenson J, et al. Retrospective study of total healthcare costs associated with chronic nonvalvular atrial fibrillation and the occurrence of a first transient ischemic attack, stroke or major bleed. Curr Med Res Opin. 2009;25(12):2853–2864. doi: 10.1185/03007990903196422. [DOI] [PubMed] [Google Scholar]