Abstract
Tuberous sclerosis complex (TSC) is a rare inherited disease that affects many organs and tissues, which explains the diversity of its clinical manifestations. This disease is often diagnosed at an early age when cutaneous angiofibromas, epilepsy and mental retardation are associated. The hepatic involvement in this phakomatosis is an uncommon location. In this context, we report the case of a tuberous sclerosis revealed in adulthood by abdominal pain and distension related to renal and hepatic angiomyolipomas associated with typical skin lesions.
Background
Tuberous sclerosis complex (TSC) is an autosomal dominant inherited disease, characterised by the presence of hamartomatous lesions in multiple organs. The typical clinical manifestations include: angiofibromas, epilepsy and mental retardation. Also, hamartomas can involve other viscera such as kidneys, eyes, lungs and heart.1 Symptomatic hepatic angiomyolipomas have been reported as an exceptional manifestation of this disease.2
It seems useful to sensitise all clinicians to this complication of TSC by reporting a case observed in our institution.
Case presentation
A 47-year-old woman was admitted to our internal medicine department for abdominal pain and distension lasting for 4 months. She has an apparent good state (BMI 25.5 kg/m2) with no fever or weight loss. On clinical examination, abdominal distension and umbilical hernia were noted. Hepatomegaly was detected without splenomegaly. A tender firm mass in the left flank reaching the umbilicus was found. The cardiopulmonary examination was normal. A skin examination showed angiofibromas in the nasolabial fold and shagreen patch lesions in the lumbosacral region. These skin lesions are evolving since the age of 5. Otherwise, she has no history of generalised seizures or mental retardation.
Investigations
Laboratory findings on admission revealed a normal white cell count (8600/mm3), normocytic anaemia (haemoglobin 10 g/dL) and thrombocytosis (664 000/mm3). The erythrocyte sedimentation rate was elevated (105 mm). The C reactive protein was high (25 mg/L) and also the level of plasma fibrinogen (6.05 g/L). Biochemical analysis revealed glutamyltranspeptidase 60 U/L without hepatic cytolysis or hepatic failure. There was an elevated creatinine level 159 µmol/L and the creatinine clearance by Cockcroft and Gault formula was estimated to be 41 mL/mn. Other biochemical findings were within normal limits.
Abdominal ultrasonographic examination confirmed hepatomegaly of 20 cm. There was hyperechogenic, heterogenous round formation in the seventh segment of the liver measuring 10 cm. This formation was hypervascularised with colour Doppler. There were also many rounded centimetric cavities in the liver. The spleen was normal. The kidneys are greatly increased in size with a poor-defined and hyperechogenic contour.
Chest and abdominal CT showed pulmonary multiple cystic lesions with aeric centre and thin wall of different sizes. The liver was grossly enlarged (longitudinal diameter 20 cm). There were multiple hypodense masses located in the liver without any compression of other organs. The largest lesion measured 9 cm in greatest dimension and is located between the segments VI and VII. The aspect of these lesions may evoke angiomyolipomas (figure 1). The kidneys are greatly increased in size with a bilateral renal pelvic dilation. There were multiple cystic formations associated with fat density areas in favour of angiomyolipoma.
Figure 1.
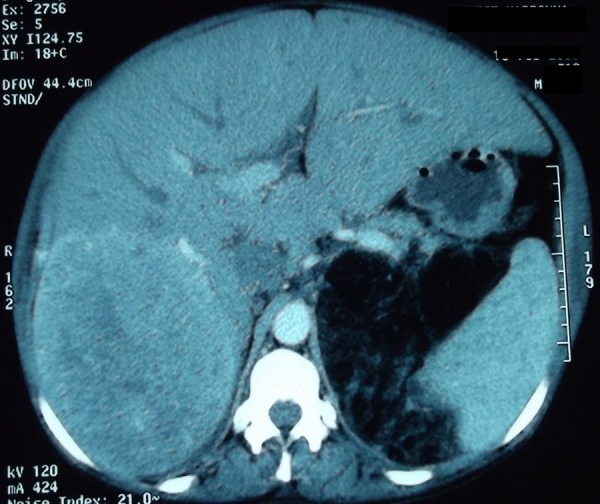
Multiple hypodense masses located in the liver and the largest lesion measured 9 cm in greatest dimension.
The head CT showed multiple calcified subependymal nodules. The ophthalmological examination was normal.
The diagnosis of TSC was made due to the association between more than two major features according to the diagnostic criteria for TSC.3 These major criteria in our observation include facial angiofibroma, shagreen patches, subependymal nodules and renal angiomyolipoma.3
Also, according to the radiological aspect of the liver mass and given the clinical context, we excluded the possible diagnosis of hepatic neoplasm and we made the diagnosis of hepatic angiomyolipomas which may be included in the diagnosis of TSC.
Outcome and follow-up
During the past 4 years, the evolution was stable clinically and biologically. We do not note deterioration in hepatic function. The renal function was stable.
Discussion
The interesting aspect of this report is that hepatic involvement inaugurates TSC. Our observation is also exceptional because the diagnosis of this genetic disorder was made later at the age of 47 years, and multiorgan systems were involved in our paucisymptomatic patient, including skin, brain, lungs, kidneys and liver. Our patient had typical cutaneous lesions such as facial angiofibroma and shagreen patches which constitute the most classic lesions reported in this disease.1 Cerebral CT showed calcification of multiple subependymal nodules which are typical lesions of TSC and contributed to making our diagnosis.1 3 However, neurological symptoms have not been noted. There was no mental retardation or epilepsy. The pulmonary lesions were also asymptomatic despite the presence of cyst formation in chest CT.
Renal angiomyolipomas are the most frequent renal manifestation, occurring in 80% of all the cases.1 Renal angiomyolipoma can be revealed by flank pain or renal failure like in our observation. It can be complicated by anaemia, haematuria, proteinuria, hypertension and end-stage renal failure. The renal function test remained stable in our case.4
Hepatic angiomyolipomas are the less common location in TSC. It has been reported only in 6–10% of cases.4 In the literature, only few cases of symptomatic hepatic angiomyolipomas like in our observation have been reported.2 5 This hepatic involvement can be revealed as in our case by abdominal pain, distension and hepatomegaly.2
This hepatic location can be complicated by malnutrition or mechanical compression as described by Dumortier et al.6
MRI is better than CT scan to diagnose angiomyolipoma. The typical lesions are hypointense in T1-weighted dynamic sequences and hyperintense in T2-weighted images after gadolinium administration.5 However, in some cases, hepatic biopsy will be proposed to exclude malignancy. In our observation neither MRI nor hepatic biopsy were made. Referring to the clinical context, the diagnosis of hepatic location of TSC can be retained. In addition, the absence of any symptomatology in the past 4 years is in favour of our diagnosis.
Anaemia noted in our case can be attributed to micro-bleeding and inflammation caused by tumoral lesions.4
There is no standardised approach proposed in hepatic angiomyolipoma. Surgical resection or liver transplantation may be proposed in cases complicated by compression or haemorrhage.6 In our case, there were no complications. There was no indication for surgery because the patient was stable.
In our case, genetic testing for TSC is not available. New therapeutic options are proposed based on the molecular genetic findings. TSC is characterised by mammalian target of rapamycin (mTOR) activation and growth of benign tumours. That is why early mTOR inhibition may prevent the development of TSC lesions.7
It is also important to provide appropriate genetic counselling and evaluation of the family members in order to detect the disease early.
Learning points.
Tuberous sclerosis complex (TSC) can be diagnosed in advanced age.
Physicians should bear in mind hepatic angiomyolipoma as a differential diagnosis among patients with hepatic masses.
When TSC is clinically suspected, investigations including head tomography, thoracic and abdominal CT will be made to research other asymptomatic locations.
Footnotes
Contributors: All the authors have read the manuscript and have approved this submission.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rosser T, Panigraphy A, McClintock W. The diverse clinical manifestations of tuberous sclerosis complex/a review. Sem Ped Neurol 2006;13:27–36 [DOI] [PubMed] [Google Scholar]
- 2.Lenci I, Angelico M, Tisone G, et al. Massive hepatic angiomyolipoma in a young woman with tuberous sclerosis complex: significant clinical improvement during tamoxifen treatment. J Hepatol 2008;48:1026–9 [DOI] [PubMed] [Google Scholar]
- 3.Roach ES, Gomez MR, Northup H. Tuberous sclerosis complex consensus conference: revised clinical diagnostic criteria. J Child Neurol 1998;13:624–8 [DOI] [PubMed] [Google Scholar]
- 4.Ben Hamida F, Gorsane I, Gharbi C, et al. Renal manifestations in tuberous sclerosis. Rev Med Int 2006;27:836–42 [DOI] [PubMed] [Google Scholar]
- 5.Tang LH, Hui P, Garcia-Tsao G, et al. Multiple angiomyolipomata of the liver: a case report. Mod Pathol 2002;15:167–71 [DOI] [PubMed] [Google Scholar]
- 6.Dumortier J, Guillaud O, Walter T, et al. Liver transplantation for multiple angiomyolipomas complicating tuberous sclerosis complex. Gastroenterol Clin Biol 2010;34:494–8 [DOI] [PubMed] [Google Scholar]
- 7.Katulskak K, Borkowska J, Jozwiak S. possible prevention of tuberous sclerosis complex lesions. Pediatrics 2013;132:e239–42 [DOI] [PubMed] [Google Scholar]


