Description
Superior vena cava syndrome is characterised by dyspnoea, headache, facial oedema, and venous distention in the neck, upper chest and arms. These symptoms are bilateral.
A 47-year-old woman reported the appearance of venous ectasias in the right side of her chest, face and neck. The patient was affected by systemic lupus erythematous with antiphospholipid syndrome and end-stage renal disease. She was on haemodialysis via a right subclavian central venous silicone, double-lumen, tunnelled catheter (central venous catheter, CVC) because of a previous thrombosis of arteriovenous fistula. Although this type of CVC has a higher risk of complications (ie, thrombosis), the reason of this choice was not clear, since the patient was treated at another haemodialysis service.
At physical examination, the patient's clinical condition was discrete; right side of the face appeared slightly swollen; distension of the right external jugular vein and superficial ectasic veins of the right hemithorax were present (figure 1). Ultrasound scan showed a fibrotic right internal jugular vein, without Doppler signal. Neck and chest CT confirmed the lack of contrast enhancement of the right internal jugular vein in its distal tract (5.5 cm) until the confluence with the subclavian vein (figures 2A, B) and the presence of multiple ectasic veins of the subcutaneous tissue of the right anterior chest wall and neck (figures 3 and 4). The CVC was passing through the brachiocephalic vein to the right atrium.
Figure 1.

Distension of the right external jugular vein and superficial ectasic veins of the right chest and neck.
Figure 2.

(A) Coronal CT scan reconstruction showing the thrombosis of the right internal jugular vein; (B) sagittal CT scan reconstruction showing the length of the venous occlusion (54.81 mm).
Figure 3.

Superficial ectasic veins of the right chest, shoulder and neck.
Figure 4.
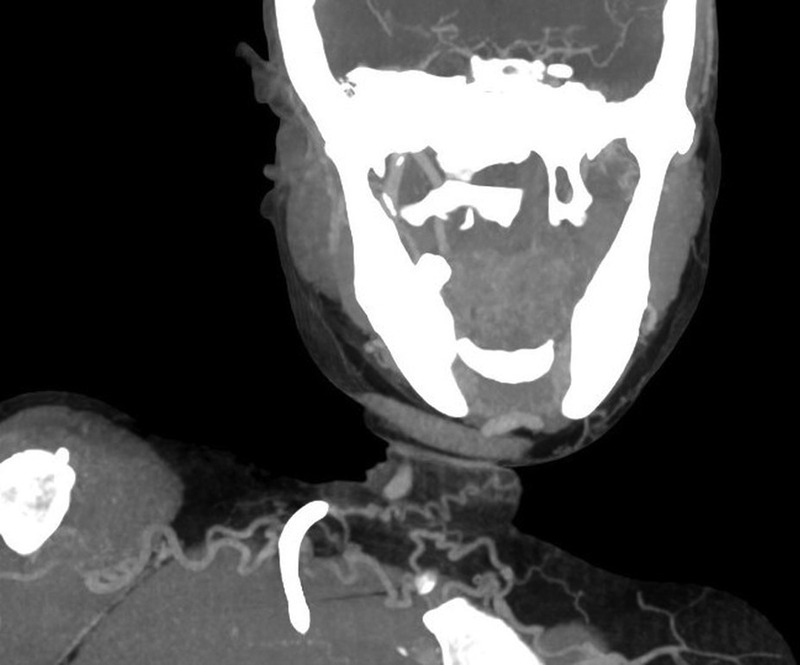
Coronal CT scan reconstruction showing multiple ectasic veins of the subcutaneous tissue of the right anterior chest wall.
These findings were consistent with a CVC-related thrombosis of the internal jugular vein with a compensatory collateral circulation through the external homolateral jugular vein.
Jugular thrombosis represents a possible complication of CVC implant.1–3 The pathogenesis is multifactorial, being related to insertion-related vessel damage, infusion-related endothelium damage and mechanical irritation to the vessel's wall. Most CVC-related thromboses are subclinical with consequent development of collateral circulation.1 2
It is conceivable that, in our patient, the thrombophilic condition (antiphospholipid syndrome) promoted this complication.
Learning points.
Superior vena cava syndrome typically has bilateral signs and symptoms frequently due to infiltration or compression of the vein.
Monolateral symptoms always recognise a local cause of thrombosis.
Central venous catheter-related thrombosis count for 6/10 000 hospital admissions.
Footnotes
Contributors: All authors managed the patient and took part in the writing and revising process of the paper.
Competing interests: None.
Patient consent: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mai C, Hunt D. Upper-extremity deep venous thrombosis: a review. Am J Med 2011;124:402–7 [DOI] [PubMed] [Google Scholar]
- 2.Spiezia L, Simioni P. Upper extremity deep vein thrombosis. Intern Emerg Med 2010;5:103–9 [DOI] [PubMed] [Google Scholar]
- 3.McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med 2003;20:1123–33 [DOI] [PubMed] [Google Scholar]


